Pneumonia on:
[Wikipedia]
[Google]
[Amazon]
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry
 Pneumonia is due to infections caused primarily by
Pneumonia is due to infections caused primarily by
 Bacteria are the most common cause of
Bacteria are the most common cause of
 In adults, viruses account for about one third of pneumonia cases, and in children for about 15% of them. Commonly implicated agents include rhinoviruses, coronaviruses,
In adults, viruses account for about one third of pneumonia cases, and in children for about 15% of them. Commonly implicated agents include rhinoviruses, coronaviruses,
 Pneumonia frequently starts as an
Pneumonia frequently starts as an

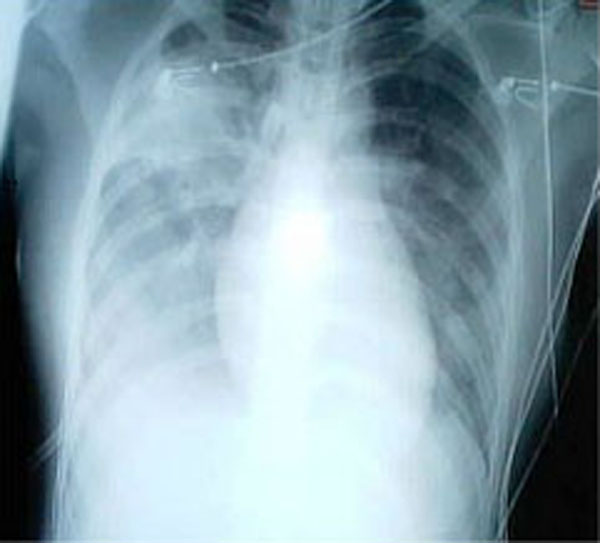
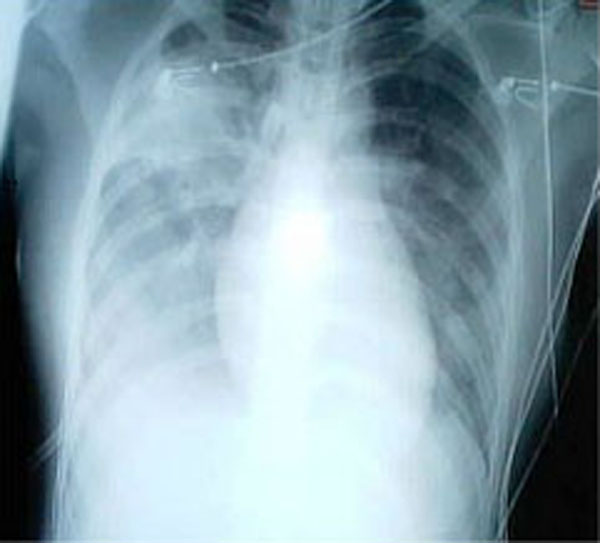
 A chest radiograph is frequently used in diagnosis. In people with mild disease, imaging is needed only in those with potential complications, those not having improved with treatment, or those in which the cause is uncertain. If a person is sufficiently sick to require hospitalization, a chest radiograph is recommended. Findings do not always match the severity of disease and do not reliably separate between bacterial and viral infection.
X-ray presentations of pneumonia may be classified as
A chest radiograph is frequently used in diagnosis. In people with mild disease, imaging is needed only in those with potential complications, those not having improved with treatment, or those in which the cause is uncertain. If a person is sufficiently sick to require hospitalization, a chest radiograph is recommended. Findings do not always match the severity of disease and do not reliably separate between bacterial and viral infection.
X-ray presentations of pneumonia may be classified as
File:UOTW 34 - Ultrasound of the Week 1.webm, Pneumonia seen by ultrasound
File:UOTW 34 - Ultrasound of the Week 2.webm, Pneumonia seen by ultrasound
File:UOTW 34 - Ultrasound of the Week 3.jpg, Pneumonia seen by ultrasound
File:RtPneuKidMark.png, Right middle lobe pneumonia in a child as seen on plain X-ray
 In pneumonia, a collection of fluid may form in the space that surrounds the lung. Occasionally, microorganisms will infect this fluid, causing an
In pneumonia, a collection of fluid may form in the space that surrounds the lung. Occasionally, microorganisms will infect this fluid, causing an

 Pneumonia is a common illness affecting approximately 450 million people a year and occurring in all parts of the world. It is a major cause of death among all age groups resulting in 4 million deaths (7% of the world's total death) yearly. Rates are greatest in children less than five, and adults older than 75 years. It occurs about five times more frequently in the developing world than in the
Pneumonia is a common illness affecting approximately 450 million people a year and occurring in all parts of the world. It is a major cause of death among all age groups resulting in 4 million deaths (7% of the world's total death) yearly. Rates are greatest in children less than five, and adults older than 75 years. It occurs about five times more frequently in the developing world than in the
 Pneumonia has been a common disease throughout human history. The word is from Greek πνεύμων (pneúmōn) meaning "lung". The symptoms were described by
Pneumonia has been a common disease throughout human history. The word is from Greek πνεύμων (pneúmōn) meaning "lung". The symptoms were described by
cough
A cough is a sudden expulsion of air through the large breathing passages that can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three ph ...
, chest pain, fever
Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point. There is not a single agreed-upon upper limit for normal temperature with sources using val ...
, and difficulty breathing. The severity of the condition is variable.
Pneumonia is usually caused by infection with virus
A virus is a submicroscopic infectious agent that replicates only inside the living cells of an organism. Viruses infect all life forms, from animals and plants to microorganisms, including bacteria and archaea.
Since Dmitri Ivanovsk ...
es or bacteria
Bacteria (; singular: bacterium) are ubiquitous, mostly free-living organisms often consisting of one Cell (biology), biological cell. They constitute a large domain (biology), domain of prokaryotic microorganisms. Typically a few micrometr ...
, and less commonly by other microorganisms. Identifying the responsible pathogen can be difficult. Diagnosis is often based on symptoms and physical examination. Chest X-rays, blood tests, and culture of the sputum may help confirm the diagnosis. The disease may be classified by where it was acquired, such as community- or hospital-acquired or healthcare-associated pneumonia.
Risk factors for pneumonia include cystic fibrosis, chronic obstructive pulmonary disease (COPD), sickle cell disease
Sickle cell disease (SCD) is a group of blood disorders typically inherited from a person's parents. The most common type is known as sickle cell anaemia. It results in an abnormality in the oxygen-carrying protein haemoglobin found in red b ...
, asthma, diabetes, heart failure, a history of smoking, a poor ability to cough (such as following a stroke), and a weak immune system.
Vaccines to prevent certain types of pneumonia (such as those caused by ''Streptococcus pneumoniae
''Streptococcus pneumoniae'', or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic (under aerobic conditions) or beta-hemolytic (under anaerobic conditions), aerotolerant anaerobic member of the genus Streptococcus. They ar ...
'' bacteria, linked to influenza, or linked to COVID-19) are available. Other methods of prevention include hand washing
Hand washing (or handwashing), also known as hand hygiene, is the act of cleaning one's hands with soap or handwash and water to remove viruses/bacteria/microorganisms, dirt, grease, or other harmful and unwanted substances stuck to the hands ...
to prevent infection, not smoking, and social distancing.
Treatment depends on the underlying cause. Pneumonia believed to be due to bacteria is treated with antibiotics. If the pneumonia is severe, the affected person is generally hospitalized. Oxygen therapy may be used if oxygen levels are low.
Each year, pneumonia affects about 450 million people globally (7% of the population) and results in about 4 million deaths. With the introduction of antibiotics and vaccines in the 20th century, survival has greatly improved. Nevertheless, pneumonia remains a leading cause of death in developing countries, and also among the very old, the very young, and the chronically ill. Pneumonia often shortens the period of suffering among those already close to death and has thus been called "the old man's friend".
Signs and symptoms
People with infectious pneumonia often have aproductive cough
A cough is a sudden expulsion of air through the large breathing passages that can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three phas ...
, fever
Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point. There is not a single agreed-upon upper limit for normal temperature with sources using val ...
accompanied by shaking chills, shortness of breath, sharp or stabbing chest pain during deep breaths, and an increased rate of breathing. In elderly people, confusion may be the most prominent sign.
The typical signs and symptoms in children under five are fever, cough, and fast or difficult breathing. Fever is not very specific, as it occurs in many other common illnesses and may be absent in those with severe disease, malnutrition or in the elderly. In addition, a cough is frequently absent in children less than 2 months old. More severe signs and symptoms in children may include blue-tinged skin, unwillingness to drink, convulsions, ongoing vomiting, extremes of temperature, or a decreased level of consciousness.
Bacterial and viral cases of pneumonia usually result in similar symptoms. Some causes are associated with classic, but non-specific, clinical characteristics. Pneumonia caused by ''Legionella
''Legionella'' is a genus of pathogenic gram-negative bacteria that includes the species '' L. pneumophila'', causing legionellosis (all illnesses caused by ''Legionella'') including a pneumonia-type illness called Legionnaires' disease and a mil ...
'' may occur with abdominal pain, diarrhea, or confusion. Pneumonia caused by ''Streptococcus pneumoniae
''Streptococcus pneumoniae'', or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic (under aerobic conditions) or beta-hemolytic (under anaerobic conditions), aerotolerant anaerobic member of the genus Streptococcus. They ar ...
'' is associated with rusty colored sputum. Pneumonia caused by '' Klebsiella'' may have bloody sputum often described as "currant jelly". Bloody sputum (known as hemoptysis
Hemoptysis is the coughing up of blood or blood-stained mucus from the bronchi, larynx, trachea, or lungs. In other words, it is the airway bleeding. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia, a ...
) may also occur with tuberculosis, Gram-negative pneumonia, lung abscesses and more commonly acute bronchitis. Pneumonia caused by ''Mycoplasma pneumoniae
''Mycoplasma pneumoniae'' is a very small bacterium in the class Mollicutes. It is a human pathogen that causes the disease mycoplasma pneumonia, a form of atypical bacterial pneumonia related to cold agglutinin disease. ''M. pneumoniae'' is c ...
'' may occur in association with swelling of the lymph nodes in the neck, joint pain
Arthralgia (from Greek ''arthro-'', joint + ''-algos'', pain) literally means ''joint pain''. Specifically, arthralgia is a symptom of injury, infection, illness (in particular arthritis), or an allergic reaction to medication.
According to MeSH, ...
, or a middle ear infection. Viral pneumonia presents more commonly with wheezing than bacterial pneumonia. Pneumonia was historically divided into "typical" and "atypical" based on the belief that the presentation predicted the underlying cause. However, evidence has not supported this distinction, therefore it is no longer emphasized.
Cause
 Pneumonia is due to infections caused primarily by
Pneumonia is due to infections caused primarily by bacteria
Bacteria (; singular: bacterium) are ubiquitous, mostly free-living organisms often consisting of one Cell (biology), biological cell. They constitute a large domain (biology), domain of prokaryotic microorganisms. Typically a few micrometr ...
or virus
A virus is a submicroscopic infectious agent that replicates only inside the living cells of an organism. Viruses infect all life forms, from animals and plants to microorganisms, including bacteria and archaea.
Since Dmitri Ivanovsk ...
es and less commonly by fungi and parasites
Parasitism is a close relationship between species, where one organism, the parasite, lives on or inside another organism, the host, causing it some harm, and is adapted structurally to this way of life. The entomologist E. O. Wilson ha ...
. Although more than 100 strains of infectious agents have been identified, only a few are responsible for the majority of cases. Mixed infections with both viruses and bacteria may occur in roughly 45% of infections in children and 15% of infections in adults. A causative agent may not be isolated in about half of cases despite careful testing. In an active population-based surveillance for community-acquired pneumonia requiring hospitalization in five hospitals in Chicago and Nashville from January 2010 through June 2012, 2259 patients were identified who had radiographic evidence of pneumonia and specimens that could be tested for the responsible pathogen. Most patients (62%) had no detectable pathogens in their sample, and unexpectedly, respiratory viruses were detected more frequently than bacteria. Specifically, 23% had one or more viruses, 11% had one or more bacteria, 3% had both bacterial and viral pathogens, and 1% had a fungal or mycobacterial infection. "The most common pathogens were human rhinovirus
The rhinovirus (from the grc, ῥίς, rhis "nose", , romanized: "of the nose", and the la, vīrus) is the most common viral infectious agent in humans and is the predominant cause of the common cold. Rhinovirus infection proliferates in tem ...
(in 9% of patients), influenza virus (in 6%), and ''Streptococcus pneumoniae'' (in 5%)."
The term ''pneumonia'' is sometimes more broadly applied to any condition resulting in inflammation of the lungs (caused for example by autoimmune diseases, chemical burns or drug reactions); however, this inflammation is more accurately referred to as pneumonitis
Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris (e.g., animal dander), aspiration, herbicide ...
.
Factors that predispose to pneumonia include smoking, immunodeficiency, alcoholism, chronic obstructive pulmonary disease, sickle cell disease
Sickle cell disease (SCD) is a group of blood disorders typically inherited from a person's parents. The most common type is known as sickle cell anaemia. It results in an abnormality in the oxygen-carrying protein haemoglobin found in red b ...
(SCD), asthma, chronic kidney disease, liver disease
Liver disease, or hepatic disease, is any of many diseases of the liver. If long-lasting it is termed chronic liver disease. Although the diseases differ in detail, liver diseases often have features in common.
Signs and symptoms
Some of the si ...
, and biological aging. Additional risks in children include not being breastfed
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that brea ...
, exposure to cigarette smoke and other air pollution, malnutrition, and poverty. The use of acid-suppressing medications – such as proton-pump inhibitors
Proton-pump inhibitors (PPIs) are a class of medications that cause a profound and prolonged reduction of stomach acid production. They do so by irreversibly inhibiting the stomach's H+/K+ ATPase proton pump.
They are the most potent inhibitors ...
or H2 blockers
H2 antagonists, sometimes referred to as H2RAs and also called H2 blockers, are a class of medications that block the action of histamine at the histamine H2 receptors of the parietal cells in the stomach. This decreases the production of sto ...
– is associated with an increased risk of pneumonia. Approximately 10% of people who require mechanical ventilation develop ventilator-associated pneumonia, and people with a gastric feeding tube have an increased risk of developing aspiration pneumonia
Aspiration pneumonia is a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs. Signs and symptoms often include fever and cough of relatively rapid onset. Complications may inc ...
. For people with certain variants of the FER gene, the risk of death is reduced in sepsis caused by pneumonia. However, for those with TLR6 variants, the risk of getting Legionnaires' disease is increased.
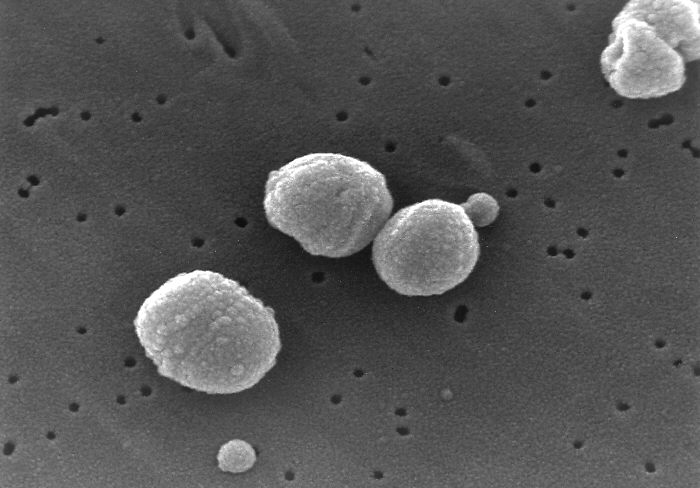
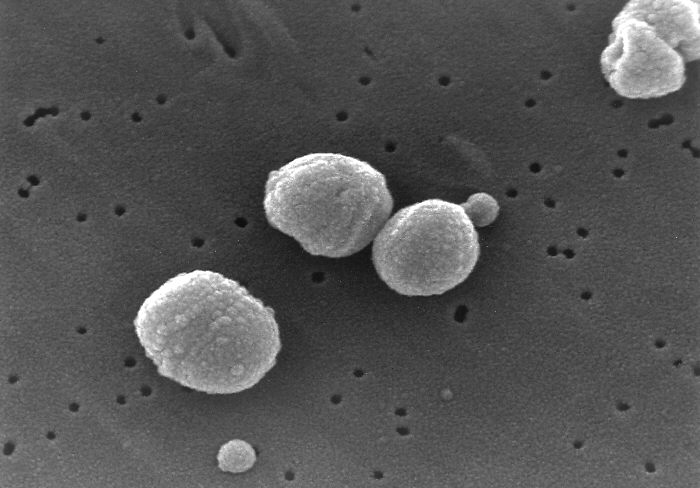
Bacteria
 Bacteria are the most common cause of
Bacteria are the most common cause of community-acquired pneumonia
Community-acquired pneumonia (CAP) refers to pneumonia (any of several lung diseases) contracted by a person outside of the healthcare system. In contrast, hospital-acquired pneumonia (HAP) is seen in patients who have recently visited a hospital ...
(CAP), with ''Streptococcus pneumoniae
''Streptococcus pneumoniae'', or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic (under aerobic conditions) or beta-hemolytic (under anaerobic conditions), aerotolerant anaerobic member of the genus Streptococcus. They ar ...
'' isolated in nearly 50% of cases. Other commonly isolated bacteria include '' Haemophilus influenzae'' in 20%, ''Chlamydophila pneumoniae
''Chlamydia pneumoniae'' is a species of ''Chlamydia'', an obligate intracellular bacterium that infects humans and is a major cause of pneumonia. It was known as the Taiwan acute respiratory agent (TWAR) from the names of the two original isola ...
'' in 13%, and ''Mycoplasma pneumoniae
''Mycoplasma pneumoniae'' is a very small bacterium in the class Mollicutes. It is a human pathogen that causes the disease mycoplasma pneumonia, a form of atypical bacterial pneumonia related to cold agglutinin disease. ''M. pneumoniae'' is c ...
'' in 3% of cases; '' Staphylococcus aureus''; ''Moraxella catarrhalis
''Moraxella catarrhalis'' is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the inf ...
''; and '' Legionella pneumophila''. A number of drug-resistant versions of the above infections are becoming more common, including drug-resistant ''Streptococcus pneumoniae'' (DRSP) and methicillin-resistant ''Staphylococcus aureus'' (MRSA).
The spreading of organisms is facilitated by certain risk factors. Alcoholism is associated with ''Streptococcus pneumoniae'', anaerobic organisms, and ''Mycobacterium tuberculosis''; smoking facilitates the effects of ''Streptococcus pneumoniae'', ''Haemophilus influenzae'', ''Moraxella catarrhalis'', and ''Legionella pneumophila''. Exposure to birds is associated with ''Chlamydia psittaci
''Chlamydia psittaci'' is a lethal intracellular parasite, intracellular bacterial species that may cause Endemism, endemic Bird, avian chlamydiosis, epizootic outbreaks in mammals, and respiratory psittacosis in humans. Potential hosts include ...
''; farm animals with '' Coxiella burnetti''; aspiration of stomach contents with anaerobic organisms; and cystic fibrosis with '' Pseudomonas aeruginosa'' and ''Staphylococcus aureus''. ''Streptococcus pneumoniae'' is more common in the winter, and it should be suspected in persons aspirating a large number of anaerobic organisms.
Viruses
 In adults, viruses account for about one third of pneumonia cases, and in children for about 15% of them. Commonly implicated agents include rhinoviruses, coronaviruses,
In adults, viruses account for about one third of pneumonia cases, and in children for about 15% of them. Commonly implicated agents include rhinoviruses, coronaviruses, influenza virus
''Orthomyxoviridae'' (from Greek ὀρθός, ''orthós'' 'straight' + μύξα, ''mýxa'' 'mucus') is a family of negative-sense RNA viruses. It includes seven genera: ''Alphainfluenzavirus'', ''Betainfluenzavirus'', '' Gammainfluenzavirus'', ' ...
, respiratory syncytial virus
Respiratory syncytial virus (RSV), also called human respiratory syncytial virus (hRSV) and human orthopneumovirus, is a common, contagious virus that causes infections of the respiratory tract. It is a negative-sense, single-stranded RNA virus. ...
(RSV), adenovirus, and parainfluenza
Human parainfluenza viruses (HPIVs) are the viruses that cause human parainfluenza. HPIVs are a paraphyletic group of four distinct single-stranded RNA viruses belonging to the '' Paramyxoviridae'' family. These viruses are closely associated wit ...
. Herpes simplex virus rarely causes pneumonia, except in groups such as newborns, persons with cancer, transplant recipients, and people with significant burns. After organ transplantation
Organ transplantation is a medical procedure in which an organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organs may be transpor ...
or in otherwise immunocompromised
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that a ...
persons, there are high rates of cytomegalovirus pneumonia. Those with viral infections may be secondarily infected with the bacteria ''Streptococcus pneumoniae'', ''Staphylococcus aureus'', or ''Haemophilus influenzae'', particularly when other health problems are present. Different viruses predominate at different times of the year; during flu season
Flu season is an annually recurring time period characterized by the prevalence of an outbreak of influenza (flu). The season occurs during the cold half of the year in each hemisphere. It takes approximately two days to show symptoms. Influen ...
, for example, influenza may account for more than half of all viral cases. Outbreaks of other viruses also occur occasionally, including hantaviruses
''Orthohantavirus'' is a genus of single-stranded, enveloped, negative-sense RNA viruses in the family '' Hantaviridae'' within the order ''Bunyavirales''. Members of this genus may be called orthohantaviruses or simply hantaviruses.
Orthohantav ...
and coronaviruses. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can also result in pneumonia.
Fungi
Fungal pneumonia is uncommon, but occurs more commonly in individuals with weakened immune systems due to AIDS, immunosuppressive drugs, or other medical problems. It is most often caused by ''Histoplasma capsulatum
''Histoplasma capsulatum'' is a species of dimorphic fungus. Its sexual form is called ''Ajellomyces capsulatus''. It can cause pulmonary and disseminated histoplasmosis.
''H. capsulatum'' is "distributed worldwide, except in Antarctica, but m ...
'', '' Blastomyces'', '' Cryptococcus neoformans'', '' Pneumocystis jiroveci'' ( pneumocystis pneumonia, or PCP), and ''Coccidioides immitis
''Coccidioides immitis'' is a pathogenic fungus that resides in the soil in certain parts of the southwestern United States, northern Mexico, and a few other areas in the Western Hemisphere.
Epidemiology
''C. immitis'', along with its relati ...
''. Histoplasmosis
Histoplasmosis is a fungal infection caused by '' Histoplasma capsulatum''. Symptoms of this infection vary greatly, but the disease affects primarily the lungs. Occasionally, other organs are affected; called disseminated histoplasmosis, it can ...
is most common in the Mississippi River basin
The Mississippi River is the second-longest river and chief river of the second-largest drainage system in North America, second only to the Hudson Bay drainage system. From its traditional source of Lake Itasca in northern Minnesota, it f ...
, and coccidioidomycosis
Coccidioidomycosis (, ), commonly known as cocci, Valley fever, as well as California fever, desert rheumatism, or San Joaquin Valley fever, is a mammalian fungal disease caused by '' Coccidioides immitis'' or ''Coccidioides posadasii''. Coccid ...
is most common in the Southwestern United States. The number of cases of fungal pneumonia has been increasing in the latter half of the 20th century due to increasing travel and rates of immunosuppression in the population. For people infected with HIV/AIDS
Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual ...
, PCP is a common opportunistic infection.
Parasites
A variety of parasites can affect the lungs, including '' Toxoplasma gondii'', '' Strongyloides stercoralis'', '' Ascaris lumbricoides'', and ''Plasmodium malariae
''Plasmodium malariae'' is a parasitic protozoan that causes malaria in humans. It is one of several species of ''Plasmodium'' parasites that infect other organisms as pathogens, also including ''Plasmodium falciparum'' and ''Plasmodium vivax'' ...
''.Murray and Nadel (2010). Chapter 37. These organisms typically enter the body through direct contact with the skin, ingestion, or via an insect vector. Except for '' Paragonimus westermani'', most parasites do not specifically affect the lungs but involve the lungs secondarily to other sites. Some parasites, in particular those belonging to the ''Ascaris'' and ''Strongyloides'' genera, stimulate a strong eosinophilic
Eosinophilic (Greek suffix -phil-, meaning ''loves eosin'') is the staining of tissues, cells, or organelles after they have been washed with eosin, a dye.
Eosin is an acidic dye for staining cell cytoplasm, collagen, and muscle fibers. ''E ...
reaction, which may result in eosinophilic pneumonia
Eosinophilic pneumonia is a disease in which an eosinophil, a type of white blood cell, accumulates in the lungs. These cells cause disruption of the normal air spaces (alveoli) where oxygen is extracted from the atmosphere. Several different kin ...
. In other infections, such as malaria, lung involvement is due primarily to cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrin ...
-induced systemic inflammation. In the developed world
A developed country (or industrialized country, high-income country, more economically developed country (MEDC), advanced country) is a sovereign state that has a high quality of life, developed economy and advanced technological infrastruct ...
, these infections are most common in people returning from travel or in immigrants. Around the world, parasitic pneumonia is most common in the immunodeficient.
Noninfectious
Idiopathic interstitial pneumonia or noninfectious pneumonia is a class ofdiffuse lung disease
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium (the tissue and space around the alveoli (air sacs)) of the lungs. It concerns alveolar epithelium, pulmon ...
s. They include diffuse alveolar damage, organizing pneumonia
Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles ( bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pn ...
, nonspecific interstitial pneumonia, lymphocytic interstitial pneumonia
Lymphocytic interstitial pneumonia (LIP) is a syndrome secondary to autoimmune and other lymphoproliferative disorders. Symptoms include fever, cough, and shortness of breath. Lymphocytic interstitial pneumonia applies to disorders associated w ...
, desquamative interstitial pneumonia, respiratory bronchiolitis interstitial lung disease
Respiratory bronchiolitis is a lung disease associated with tobacco smoking. Topic Completed: 1 July 2020. Minor changes: 1 July 2020 In pathology, it is defined by the presence of "smoker's macrophages". When manifesting significant clinical sympt ...
, and usual interstitial pneumonia. Lipoid pneumonia is another rare cause due to lipids entering the lung. These lipids can either be inhaled or spread to the lungs from elsewhere in the body.
Mechanisms
 Pneumonia frequently starts as an
Pneumonia frequently starts as an upper respiratory tract infection
An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx or trachea. This commonly includes nasal obstruction, sore thro ...
that moves into the lower respiratory tract. It is a type of pneumonitis (lung inflammation). The normal flora of the upper airway give protection by competing with pathogens for nutrients. In the lower airways, reflexes of the glottis, actions of complement proteins and immunoglobulins are important for protection. Micro aspiration of contaminated secretions can infect the lower airways and cause pneumonia. The progress of pneumonia is determined by the virulence of the organism; the amount of organism required to start an infection; and the body's immune response against the infection.
Bacterial
Most bacteria enter the lungs via small aspirations of organisms residing in the throat or nose. Half of normal people have these small aspirations during sleep. While the throat always contains bacteria, potentially infectious ones reside there only at certain times and under certain conditions. A minority of types of bacteria such as '' Mycobacterium tuberculosis'' and '' Legionella pneumophila'' reach the lungs via contaminated airborne droplets. Bacteria can also spread via the blood. Once in the lungs, bacteria may invade the spaces between cells and between alveoli, where the macrophages andneutrophil
Neutrophils (also known as neutrocytes or heterophils) are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying ...
s (defensive white blood cells) attempt to inactivate the bacteria. The neutrophils also release cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrin ...
s, causing a general activation of the immune system. This leads to the fever, chills, and fatigue common in bacterial pneumonia. The neutrophils, bacteria, and fluid from surrounding blood vessels fill the alveoli, resulting in the consolidation seen on chest X-ray.
Viral
Viruses may reach the lung by a number of different routes. Respiratory syncytial virus is typically contracted when people touch contaminated objects and then touch their eyes or nose.Murray and Nadel (2010). Chapter 31. Other viral infections occur when contaminated airborne droplets are inhaled through the nose or mouth. Once in the upper airway, the viruses may make their way into the lungs, where they invade the cells lining the airways, alveoli, or lung parenchyma. Some viruses such as measles and herpes simplex may reach the lungs via the blood. The invasion of the lungs may lead to varying degrees of cell death. When the immune system responds to the infection, even more lung damage may occur. Primarily white blood cells, mainly mononuclear cells, generate the inflammation. As well as damaging the lungs, many viruses simultaneously affect other organs and thus disrupt other body functions. Viruses also make the body more susceptible to bacterial infections; in this way, bacterial pneumonia can occur at the same time as viral pneumonia.Diagnosis
Pneumonia is typically diagnosed based on a combination of physical signs and often a chest X-ray. In adults with normal vital signs and a normal lung examination, the diagnosis is unlikely. However, the underlying cause can be difficult to confirm, as there is no definitive test able to distinguish between bacterial and non-bacterial cause. The overall impression of a physician appears to be at least as good as decision rules for making or excluding the diagnosis.Diagnosis in children
The World Health Organization has defined pneumonia in children clinically based on either acough
A cough is a sudden expulsion of air through the large breathing passages that can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three ph ...
or difficulty breathing and a rapid respiratory rate, chest indrawing, or a decreased level of consciousness. A rapid respiratory rate is defined as greater than 60 breaths per minute in children under 2 months old, greater than 50 breaths per minute in children 2 months to 1 year old, or greater than 40 breaths per minute in children 1 to 5 years old.
In children, low oxygen levels and lower chest indrawing are more sensitive than hearing chest crackles
Crackles are the clicking, rattling, or crackling noises that may be made by one or both lungs of a human with a respiratory disease during inhalation. They are usually heard only with a stethoscope ("on auscultation"). Pulmonary crackles are a ...
with a stethoscope or increased respiratory rate. Grunting and nasal flaring may be other useful signs in children less than five years old.
Lack of wheezing is an indicator of ''Mycoplasma pneumoniae
''Mycoplasma pneumoniae'' is a very small bacterium in the class Mollicutes. It is a human pathogen that causes the disease mycoplasma pneumonia, a form of atypical bacterial pneumonia related to cold agglutinin disease. ''M. pneumoniae'' is c ...
'' in children with pneumonia, but as an indicator it is not accurate enough to decide whether or not macrolide
The Macrolides are a class of natural products that consist of a large macrocyclic lactone ring to which one or more deoxy sugars, usually cladinose and desosamine, may be attached. The lactone rings are usually 14-, 15-, or 16-membered. Ma ...
treatment should be used. The presence of chest pain in children with pneumonia doubles the probability of ''Mycoplasma pneumoniae''.
Diagnosis in adults
In general, in adults, investigations are not needed in mild cases. There is a very low risk of pneumonia if all vital signs and auscultation are normal.C-reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin- ...
(CRP) may help support the diagnosis. For those with CRP less than 20 mg/L without convincing evidence of pneumonia, antibiotics are not recommended.
Procalcitonin may help determine the cause and support decisions about who should receive antibiotics. Antibiotics are encouraged if the procalcitonin level reaches 0.25 μg/L, strongly encouraged if it reaches 0.5 μg/L, and strongly discouraged if the level is below 0.10 μg/L. In people requiring hospitalization, pulse oximetry
Pulse oximetry is a noninvasive method for monitoring a person's oxygen saturation. Peripheral oxygen saturation (SpO2) readings are typically within 2% accuracy (within 4% accuracy in 95% of cases) of the more accurate (and invasive) reading o ...
, chest radiography and blood tests – including a complete blood count, serum electrolytes
An electrolyte is a medium containing ions that is electrically conducting through the movement of those ions, but not conducting electrons. This includes most soluble salts, acids, and bases dissolved in a polar solvent, such as water. Upon d ...
, C-reactive protein level, and possibly liver function tests – are recommended.
The diagnosis of influenza-like illness can be made based on the signs and symptoms; however, confirmation of an influenza infection requires testing. Thus, treatment is frequently based on the presence of influenza in the community or a rapid influenza test.
Physical exam
Physical examination may sometimes reveallow blood pressure
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure (the top number) and the di ...
, high heart rate, or low oxygen saturation
Oxygen saturation (symbol SO2) is a relative measure of the concentration of oxygen that is dissolved or carried in a given medium as a proportion of the maximal concentration that can be dissolved in that medium at the given temperature. It ca ...
. The respiratory rate may be faster than normal, and this may occur a day or two before other signs. Examination of the chest may be normal, but it may show decreased expansion on the affected side. Harsh breath sounds from the larger airways that are transmitted through the inflamed lung are termed bronchial breathing and are heard on auscultation with a stethoscope. Crackles
Crackles are the clicking, rattling, or crackling noises that may be made by one or both lungs of a human with a respiratory disease during inhalation. They are usually heard only with a stethoscope ("on auscultation"). Pulmonary crackles are a ...
(rales) may be heard over the affected area during inspiration. Percussion may be dulled over the affected lung, and increased, rather than decreased, vocal resonance Vocal resonance may be defined as "the process by which the basic product of phonation is enhanced in timbre and/or intensity by the air-filled cavities through which it passes on its way to the outside air." Throughout the vocal literature, various ...
distinguishes pneumonia from a pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
.
Imaging

 A chest radiograph is frequently used in diagnosis. In people with mild disease, imaging is needed only in those with potential complications, those not having improved with treatment, or those in which the cause is uncertain. If a person is sufficiently sick to require hospitalization, a chest radiograph is recommended. Findings do not always match the severity of disease and do not reliably separate between bacterial and viral infection.
X-ray presentations of pneumonia may be classified as
A chest radiograph is frequently used in diagnosis. In people with mild disease, imaging is needed only in those with potential complications, those not having improved with treatment, or those in which the cause is uncertain. If a person is sufficiently sick to require hospitalization, a chest radiograph is recommended. Findings do not always match the severity of disease and do not reliably separate between bacterial and viral infection.
X-ray presentations of pneumonia may be classified as lobar pneumonia
Lobar pneumonia is a form of pneumonia characterized by inflammatory exudate within the intra-alveolar space resulting in consolidation that affects a large and continuous area of the lobe of a lung.
It is one of three anatomic classifications ...
, bronchopneumonia
Bronchopneumonia is a subtype of pneumonia. It is the acute inflammation of the bronchi, accompanied by inflamed patches in the nearby lobules of the lungs. citing: Webster's New World College Dictionary, Fifth Edition, Copyright 2014
It is ofte ...
, lobular pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of ...
, and interstitial pneumonia. Bacterial, community-acquired pneumonia classically show lung consolidation of one lung segmental lobe, which is known as lobar pneumonia. However, findings may vary, and other patterns are common in other types of pneumonia. Aspiration pneumonia may present with bilateral opacities primarily in the bases of the lungs and on the right side. Radiographs of viral pneumonia may appear normal, appear hyper-inflated, have bilateral patchy areas, or present similar to bacterial pneumonia with lobar consolidation. Radiologic findings may not be present in the early stages of the disease, especially in the presence of dehydration, or may be difficult to interpret in the obese
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's we ...
or those with a history of lung disease. Complications such as pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
may also be found on chest radiographs. Laterolateral chest radiographs can increase the diagnostic accuracy of lung consolidation and pleural effusion.
A CT scan can give additional information in indeterminate cases. CT scans can also provide more details in those with an unclear chest radiograph (for example occult pneumonia in chronic obstructive pulmonary disease) and can exclude pulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream ( embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathin ...
and fungal pneumonia and detect lung abscess in those who are not responding to treatments. However, CT scans are more expensive, have a higher dose of radiation, and cannot be done at bedside.
Lung ultrasound may also be useful in helping to make the diagnosis. Ultrasound is radiation free and can be done at bedside. However, ultrasound requires specific skills to operate the machine and interpret the findings. It may be more accurate than chest X-ray.
Microbiology
In people managed in the community, determining the causative agent is not cost-effective and typically does not alter management. For people who do not respond to treatment,sputum culture
A sputum culture is a test to detect and identify bacteria or fungi that infect the lungs or breathing passages. Sputum is a thick fluid produced in the lungs and in the adjacent airways. Normally, fresh morning sample is preferred for the bac ...
should be considered, and culture for '' Mycobacterium tuberculosis'' should be carried out in persons with a chronic productive cough. Microbiological evaluation is also indicated in severe pneumonia, alcoholism, asplenia, immunosuppression, HIV infection, and those being empirically treated for MRSA of pseudomonas. Although positive blood culture and pleural fluid
The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication be ...
culture definitively establish the diagnosis of the type of micro-organism involved, a positive sputum culture has to be interpreted with care for the possibility of colonisation
Colonization, or colonisation, constitutes large-scale population movements wherein migrants maintain strong links with their, or their ancestors', former country – by such links, gain advantage over other inhabitants of the territory. When ...
of respiratory tract. Testing for other specific organisms may be recommended during outbreaks, for public health reasons. In those hospitalized for severe disease, both sputum and blood cultures
A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia ...
are recommended, as well as testing the urine for antigens to ''Legionella'' and ''Streptococcus''. Viral infections, can be confirmed via detection of either the virus or its antigens with culture or polymerase chain reaction (PCR), among other techniques. ''Mycoplasma'', ''Legionella'', ''Streptococcus'', and ''Chlamydia'' can also be detected using PCR techniques on bronchoalveolar lavage and nasopharyngeal swab
A nasopharyngeal swab is a device used for collecting a sample of nasal secretions from the back of the nose and throat. The sample is then analyzed for the presence of organisms or other clinical markers for disease. This diagnostic method is c ...
. The causative agent is determined in only 15% of cases with routine microbiological tests.
Classification
Pneumonitis
Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris (e.g., animal dander), aspiration, herbicide ...
refers to lung inflammation; pneumonia refers to pneumonitis, usually due to infection but sometimes non-infectious, that has the additional feature of pulmonary consolidation. Pneumonia is most commonly classified by where or how it was acquired: community-acquired, aspiration, healthcare-associated, hospital-acquired, and ventilator-associated pneumonia. It may also be classified by the area of the lung affected: lobar pneumonia
Lobar pneumonia is a form of pneumonia characterized by inflammatory exudate within the intra-alveolar space resulting in consolidation that affects a large and continuous area of the lobe of a lung.
It is one of three anatomic classifications ...
, bronchial pneumonia and acute interstitial pneumonia; or by the causative organism. Pneumonia in children may additionally be classified based on signs and symptoms as non-severe, severe, or very severe.
The setting in which pneumonia develops is important to treatment, as it correlates to which pathogens are likely suspects, which mechanisms are likely, which antibiotics are likely to work or fail, and which complications can be expected based on the person's health status.
Community
Community-acquired pneumonia (CAP) is acquired in the community, outside of health care facilities. Compared with healthcare-associated pneumonia, it is less likely to involve multidrug-resistant bacteria. Although the latter are no longer rare in CAP, they are still less likely.Healthcare
Health care–associated pneumonia (HCAP) is an infection associated with recent exposure to the health care system, including hospitals, outpatient clinics,nursing home
A nursing home is a facility for the residential care of elderly or disabled people. Nursing homes may also be referred to as skilled nursing facility (SNF) or long-term care facilities. Often, these terms have slightly different meanings to i ...
s, dialysis centers, chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs ( chemotherapeutic agents or alkylating agents) as part of a standardized chemotherapy regimen. Chemothe ...
treatment, or home care. HCAP is sometimes called MCAP (medical care–associated pneumonia).
People may become infected with pneumonia in a hospital; this is defined as pneumonia not present at the time of admission (symptoms must start at least 48 hours after admission). It is likely to involve hospital-acquired infection
A hospital-acquired infection, also known as a nosocomial infection (from the Greek , meaning "hospital"), is an infection that is acquired in a hospital or other health care facility. To emphasize both hospital and nonhospital settings, it is so ...
s, with higher risk of multidrug-resistant pathogens. People in a hospital often have other medical conditions, which may make them more susceptible to pathogens in the hospital.
Ventilator-associated pneumonia occurs in people breathing with the help of mechanical ventilation. Ventilator-associated pneumonia is specifically defined as pneumonia that arises more than 48 to 72 hours after endotracheal intubation.
Differential diagnosis
Several diseases can present with similar signs and symptoms to pneumonia, such as: chronic obstructive pulmonary disease, asthma, pulmonary edema, bronchiectasis, lung cancer, and pulmonary emboli. Unlike pneumonia, asthma and COPD typically present with wheezing, pulmonary edema presents with an abnormal electrocardiogram, cancer and bronchiectasis present with a cough of longer duration, and pulmonary emboli present with acute onset sharp chest pain and shortness of breath. Mild pneumonia should be differentiated fromupper respiratory tract infection
An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx or trachea. This commonly includes nasal obstruction, sore thro ...
(URTI). Severe pneumonia should be differentiated from acute heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, ...
. Pulmonary infiltrates that resolved after giving mechanical ventilation should point to heart failure and atelectasis rather than pneumonia. For recurrent pneumonia, underlying lung cancer, metastasis
Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, then ...
, tuberculosis, a foreign bodies, immunosuppression, and hypersensitivity should be suspected.
Prevention
Prevention includes vaccination, environmental measures, and appropriate treatment of other health problems. It is believed that, if appropriate preventive measures were instituted globally, mortality among children could be reduced by 400,000; and, if proper treatment were universally available, childhood deaths could be decreased by another 600,000.Vaccination
Vaccination prevents against certain bacterial and viral pneumonias both in children and adults. Influenza vaccines are modestly effective at preventing symptoms of influenza, The Center for Disease Control and Prevention (CDC) recommends yearly influenza vaccination for every person 6 months and older. Immunizing health care workers decreases the risk of viral pneumonia among their patients. Vaccinations against '' Haemophilus influenzae'' and ''Streptococcus pneumoniae
''Streptococcus pneumoniae'', or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic (under aerobic conditions) or beta-hemolytic (under anaerobic conditions), aerotolerant anaerobic member of the genus Streptococcus. They ar ...
'' have good evidence to support their use. There is strong evidence for vaccinating children under the age of 2 against ''Streptococcus pneumoniae'' (pneumococcal conjugate vaccine
Pneumococcal conjugate vaccine is a pneumococcal vaccine and a conjugate vaccine used to protect infants, young children, and adults against disease caused by the bacterium ''Streptococcus pneumoniae'' (pneumococcus). It contains purified capsul ...
). Vaccinating children against ''Streptococcus pneumoniae'' has led to a decreased rate of these infections in adults, because many adults acquire infections from children. A ''Streptococcus pneumoniae'' vaccine is available for adults, and has been found to decrease the risk of invasive pneumococcal disease
''Streptococcus pneumoniae'', or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic (under aerobic conditions) or beta-hemolytic (under anaerobic conditions), aerotolerant anaerobic member of the genus Streptococcus. They ar ...
by 74%, but there is insufficient evidence to suggest using the pneumococcal vaccine to prevent pneumonia or death in the general adult population. The CDC recommends that young children and adults over the age of 65 receive the pneumococcal vaccine, as well as older children or younger adults who have an increased risk of getting pneumococcal disease. The pneumococcal vaccine has been shown to reduce the risk of community acquired pneumonia in people with chronic obstructive pulmonary disease, but does not reduce mortality or the risk of hospitalization for people with this condition. People with COPD are recommended by a number of guidelines to have a pneumococcal vaccination. Other vaccines for which there is support for a protective effect against pneumonia include pertussis
Whooping cough, also known as pertussis or the 100-day cough, is a highly contagious bacterial disease. Initial symptoms are usually similar to those of the common cold with a runny nose, fever, and mild cough, but these are followed by two or t ...
, varicella, and measles.
Medications
When influenza outbreaks occur, medications such as amantadine orrimantadine
Rimantadine ( INN, sold under the trade name 'Flumadine'') is an orally administered antiviral drug used to treat, and in rare cases prevent, influenzavirus A infection. When taken within one to two days of developing symptoms, rimantadine can s ...
may help prevent the condition, but they are associated with side effects. Zanamivir
Zanamivir is a medication used to treat and prevent influenza caused by influenza A and influenza B viruses. It is a neuraminidase inhibitor and was developed by the Australian biotech firm Biota Holdings. It was licensed to Glaxo in 1990 and ap ...
or oseltamivir decrease the chance that people who are exposed to the virus will develop symptoms; however, it is recommended that potential side effects are taken into account.
Other
Smoking cessation
Smoking cessation, usually called quitting smoking or stopping smoking, is the process of discontinuing tobacco smoking. Tobacco smoke contains nicotine, which is addictive and can cause dependence. As a result, nicotine withdrawal often m ...
and reducing indoor air pollution, such as that from cooking indoors with wood, crop residues or dung, are both recommended. Smoking appears to be the single biggest risk factor for pneumococcal pneumonia
Pneumococcal pneumonia is a type of bacterial pneumonia that is caused by Streptococcus pneumoniae (pneumococcus). It is the most common bacterial pneumonia found in adults, the most common type of community-acquired pneumonia, and one of the ...
in otherwise-healthy adults. Hand hygiene and coughing into one's sleeve may also be effective preventative measures. Wearing surgical masks by the sick may also prevent illness.
Appropriately treating underlying illnesses (such as HIV/AIDS
Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual ...
, diabetes mellitus, and malnutrition) can decrease the risk of pneumonia. In children less than 6 months of age, exclusive breast feeding reduces both the risk and severity of disease. In people with HIV/AIDS and a CD4 count of less than 200 cells/uL the antibiotic trimethoprim/sulfamethoxazole
Trimethoprim/sulfamethoxazole, sold under the brand name Bactrim among others, is a fixed-dose combination antibiotic medication used to treat a variety of bacterial infections. It consists of one part trimethoprim to five parts sulfamethoxa ...
decreases the risk of '' Pneumocystis pneumonia'' and is also useful for prevention in those that are immunocompromised but do not have HIV.
Testing pregnant women for Group B Streptococcus and ''Chlamydia trachomatis
''Chlamydia trachomatis'' (), commonly known as chlamydia, is a bacterium that causes chlamydia, which can manifest in various ways, including: trachoma, lymphogranuloma venereum, nongonococcal urethritis, cervicitis, salpingitis, pelvic infla ...
'', and administering antibiotic treatment, if needed, reduces rates of pneumonia in infants; preventive measures for HIV transmission from mother to child may also be efficient. Suctioning the mouth and throat of infants with meconium-stained amniotic fluid has not been found to reduce the rate of aspiration pneumonia
Aspiration pneumonia is a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs. Signs and symptoms often include fever and cough of relatively rapid onset. Complications may inc ...
and may cause potential harm, thus this practice is not recommended in the majority of situations. In the frail elderly good oral health care may lower the risk of aspiration pneumonia, even though there is no good evidence that one approach to mouth care is better than others in preventing nursing home acquired pneumonia. Zinc supplementation in children 2 months to five years old appears to reduce rates of pneumonia.
For people with low levels of vitamin C in their diet or blood, taking vitamin C supplements may be suggested to decrease the risk of pneumonia, although there is no strong evidence of benefit. There is insufficient evidence to recommend that the general population take vitamin C to prevent or treat pneumonia.
For adults and children in the hospital who require a respirator, there is no strong evidence indicating a difference between heat and moisture exchanger
Heat and moisture exchangers (HME) are devices used in mechanically ventilated patients intended to help prevent complications due to "drying of the respiratory mucosa, such as mucus plugging and endotracheal tube (ETT) occlusion." HMEs are one ...
s and heated humidifiers for preventing pneumonia. There is tentative evidence that laying flat on the back compared to semi-raised increases pneumonia risks in people who are intubated.
Management
Antibiotics
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention o ...
by mouth, rest, simple analgesics
An analgesic drug, also called simply an analgesic (American English), analgaesic (British English), pain reliever, or painkiller, is any member of the group of drugs used to achieve relief from pain (that is, analgesia or pain management). It ...
, and fluids usually suffice for complete resolution. However, those with other medical conditions, the elderly, or those with significant trouble breathing may require more advanced care. If the symptoms worsen, the pneumonia does not improve with home treatment, or complications occur, hospitalization may be required. Worldwide, approximately 7–13% of cases in children result in hospitalization, whereas in the developed world between 22 and 42% of adults with community-acquired pneumonia are admitted. The CURB-65 score is useful for determining the need for admission in adults. If the score is 0 or 1, people can typically be managed at home; if it is 2, a short hospital stay or close follow-up is needed; if it is 3–5, hospitalization is recommended. In children those with respiratory distress or oxygen saturations of less than 90% should be hospitalized. The utility of chest physiotherapy in pneumonia has not yet been determined. Over-the-counter cough medicine
Cold medicines are a group of medications taken individually or in combination as a treatment for the symptoms of the common cold and similar conditions of the upper respiratory tract. The term encompasses a broad array of drugs, including ...
has not been found to be effective, nor has the use of zinc
Zinc is a chemical element with the symbol Zn and atomic number 30. Zinc is a slightly brittle metal at room temperature and has a shiny-greyish appearance when oxidation is removed. It is the first element in group 12 (IIB) of the periodi ...
in children. There is insufficient evidence for mucolytics. There is no strong evidence to recommend that children who have non-measles related pneumonia take vitamin A supplements. Vitamin D, as of 2018 is of unclear benefit in children.
Pneumonia can cause severe illness in a number of ways, and pneumonia with evidence of organ dysfunction may require intensive care unit admission for observation and specific treatment. The main impact is on the respiratory and the circulatory system. Respiratory failure
Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise ...
not responding to normal oxygen therapy may require heated humidified high-flow therapy delivered through nasal cannulae, non-invasive ventilation
Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alter ...
, or in severe cases invasive ventilation through an endotracheal tube. Regarding circulatory problems as part of sepsis, evidence of poor blood flow or low blood pressure is initially treated with 30 mL/kg of crystalloid infused intravenously. In situations where fluids alone are ineffective, vasopressor medication may be required.
For adults with moderate or severe acute respiratory distress syndrome (ARDS) undergoing mechanical ventilation, there is a reduction in mortality when people lie on their front for at least 12 hours a day. However, this increases the risk of endotracheal tube obstruction and pressure sores.
Bacterial
Antibiotics improve outcomes in those with bacterial pneumonia. The first dose of antibiotics should be given as soon as possible. Increased use of antibiotics, however, may lead to the development of antimicrobial resistant strains of bacteria. Antibiotic choice depends initially on the characteristics of the person affected, such as age, underlying health, and the location the infection was acquired. Antibiotic use is also associated with side effects such as nausea, diarrhea, dizziness, taste distortion, or headaches. In the UK, treatment before culture results withamoxicillin
Amoxicillin is an antibiotic medication used to treat a number of bacterial infections. These include middle ear infection, strep throat, pneumonia, skin infections, and urinary tract infections among others. It is taken by mouth, or less c ...
is recommended as the first line for community-acquired pneumonia
Community-acquired pneumonia (CAP) refers to pneumonia (any of several lung diseases) contracted by a person outside of the healthcare system. In contrast, hospital-acquired pneumonia (HAP) is seen in patients who have recently visited a hospital ...
, with doxycycline or clarithromycin
Clarithromycin, sold under the brand name Biaxin among others, is an antibiotic used to treat various bacterial infections. This includes strep throat, pneumonia, skin infections, '' H. pylori'' infection, and Lyme disease, among others. Clarith ...
as alternatives. In North America, amoxicillin, doxycycline, and in some areas a macrolide
The Macrolides are a class of natural products that consist of a large macrocyclic lactone ring to which one or more deoxy sugars, usually cladinose and desosamine, may be attached. The lactone rings are usually 14-, 15-, or 16-membered. Ma ...
(such as azithromycin or erythromycin) is the first-line outpatient treatment in adults. In children with mild or moderate symptoms, amoxicillin taken by mouth is the first line. The use of fluoroquinolones in uncomplicated cases is discouraged due to concerns about side-effects and generating resistance in light of there being no greater benefit.
For those who require hospitalization and caught their pneumonia in the community the use of a β-lactam such as cephazolin
Cefazolin, also known as cefazoline and cephazolin, is a first-generation cephalosporin antibiotic used for the treatment of a number of bacterial infections. Specifically it is used to treat cellulitis, urinary tract infections, pneumonia, endo ...
plus macrolide
The Macrolides are a class of natural products that consist of a large macrocyclic lactone ring to which one or more deoxy sugars, usually cladinose and desosamine, may be attached. The lactone rings are usually 14-, 15-, or 16-membered. Ma ...
such as azithromycin is recommended. A fluoroquinolone
A quinolone antibiotic is a member of a large group of broad-spectrum bacteriocidals that share a bicyclic core structure related to the substance 4-quinolone. They are used in human and veterinary medicine to treat bacterial infections, as wel ...
may replace azithromycin but is less preferred. Antibiotics by mouth and by injection appear to be similarly effective in children with severe pneumonia.
The duration of treatment has traditionally been seven to ten days, but increasing evidence suggests that shorter courses (3–5 days) may be effective for certain types of pneumonia and may reduce the risk of antibiotic resistance. Research in children showed that a shorter, 3-day course of amoxicillin was as effective as a longer, 7-day course for treating pneumonia in this population. For pneumonia that is associated with a ventilator caused by non-fermenting Gram-negative bacilli (NF-GNB), a shorter course of antibiotics increases the risk that the pneumonia will return. Recommendations for hospital-acquired pneumonia
Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48–72 hours after being admitted. It is thus distinguished from community-acquired pneumonia. It is usually caused by ...
include third- and fourth-generation cephalosporins
The cephalosporins (sg. ) are a class of β-lactam antibiotics originally derived from the fungus ''Acremonium'', which was previously known as ''Cephalosporium''.
Together with cephamycins, they constitute a subgroup of β-lactam antibiotics ...
, carbapenems, fluoroquinolone
A quinolone antibiotic is a member of a large group of broad-spectrum bacteriocidals that share a bicyclic core structure related to the substance 4-quinolone. They are used in human and veterinary medicine to treat bacterial infections, as wel ...
s, aminoglycoside
Aminoglycoside is a medicinal and bacteriologic category of traditional Gram-negative antibacterial medications that inhibit protein synthesis and contain as a portion of the molecule an amino-modified glycoside (sugar). The term can also refer ...
s, and vancomycin. These antibiotics are often given intravenously
Intravenous therapy (abbreviated as IV therapy) is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutrie ...
and used in combination. In those treated in hospital, more than 90% improve with the initial antibiotics. For people with ventilator-acquired pneumonia, the choice of antibiotic therapy will depend on the person's risk of being infected with a strain of bacteria that is multi-drug resistant
Multiple drug resistance (MDR), multidrug resistance or multiresistance is antimicrobial resistance shown by a species of microorganism to at least one antimicrobial drug in three or more antimicrobial categories. Antimicrobial categories ar ...
. Once clinically stable, intravenous antibiotics should be switched to oral antibiotics. For those with ''Methicillin resistant Staphylococcus aureus
Methicillin-resistant ''Staphylococcus aureus'' (MRSA) is a group of Gram-positive bacteria that are genetically distinct from other strains of ''Staphylococcus aureus''. MRSA is responsible for several difficult-to-treat infections in humans. ...
'' (MRSA) or ''Legionella'' infections, prolonged antibiotics may be beneficial.
The addition of corticosteroids to standard antibiotic treatment appears to improve outcomes, reducing death and morbidity for adults with severe community acquired pneumonia, and reducing death for adults and children with non-severe community acquired pneumonia. A 2017 review therefore recommended them in adults with severe community acquired pneumonia. A 2019 guideline however recommended against their general use, unless refractory shock was present. Side effects associated with the use of corticosteroids include high blood sugar. There is some evidence that adding corticosteroids to the standard PCP pneumonia treatment may be beneficial for people who are infected with HIV.
The use of granulocyte colony stimulating factor (G-CSF) along with antibiotics does not appear to reduce mortality and routine use for treating pneumonia is not supported by evidence.
Viral
Neuraminidase inhibitors Neuraminidase inhibitors (NAIs) are a class of drugs which block the neuraminidase enzyme. They are a commonly used antiviral drug type against influenza. Viral neuraminidases are essential for influenza reproduction, facilitating viral budding from ...
may be used to treat viral pneumonia caused by influenza viruses (influenza A
'' A virus'' (''IAV'') causes influenza in birds and some mammals, and is the only species of the genus ''Alphainfluenzavirus'' of the virus family ''Orthomyxoviridae''. Strains of all subtypes of influenza A virus have been isolated from wild ...
and influenza B). No specific antiviral medications are recommended for other types of community acquired viral pneumonias including SARS coronavirus, adenovirus, hantavirus
''Orthohantavirus'' is a genus of single-stranded, enveloped, negative-sense RNA viruses in the family '' Hantaviridae'' within the order ''Bunyavirales''. Members of this genus may be called orthohantaviruses or simply hantaviruses.
Orthohantav ...
, and parainfluenza
Human parainfluenza viruses (HPIVs) are the viruses that cause human parainfluenza. HPIVs are a paraphyletic group of four distinct single-stranded RNA viruses belonging to the '' Paramyxoviridae'' family. These viruses are closely associated wit ...
virus. Influenza A may be treated with rimantadine
Rimantadine ( INN, sold under the trade name 'Flumadine'') is an orally administered antiviral drug used to treat, and in rare cases prevent, influenzavirus A infection. When taken within one to two days of developing symptoms, rimantadine can s ...
or amantadine, while influenza A or B may be treated with oseltamivir, zanamivir
Zanamivir is a medication used to treat and prevent influenza caused by influenza A and influenza B viruses. It is a neuraminidase inhibitor and was developed by the Australian biotech firm Biota Holdings. It was licensed to Glaxo in 1990 and ap ...
or peramivir
Peramivir (trade name Rapivab) is an antiviral drug developed by BioCryst Pharmaceuticals for the treatment of influenza. Peramivir is a neuraminidase inhibitor, acting as a transition-state analogue inhibitor of influenza neuraminidase and th ...
. These are of most benefit if they are started within 48 hours of the onset of symptoms. Many strains of H5N1
Influenza A virus subtype H5N1 (A/H5N1) is a subtype of the influenza A virus which can cause illness in humans and many other animal species. A bird-adapted strain of H5N1, called HPAI A(H5N1) for highly pathogenic avian influenza virus of type ...
influenza A, also known as avian influenza
Avian influenza, known informally as avian flu or bird flu, is a variety of influenza caused by viruses adapted to birds.
or "bird flu", have shown resistance to rimantadine and amantadine. The use of antibiotics in viral pneumonia is recommended by some experts, as it is impossible to rule out a complicating bacterial infection. The British Thoracic Society
The British Thoracic Society (BTS) was formed in 1982 by the amalgamation of the British Thoracic Association and the Thoracic Society. It is a registered charity and a company limited by guarantee.
Function
The society's main charitable objecti ...
recommends that antibiotics be withheld in those with mild disease. The use of corticosteroids is controversial.
Aspiration
In general, aspiration pneumonitis is treated conservatively with antibiotics indicated only foraspiration pneumonia
Aspiration pneumonia is a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs. Signs and symptoms often include fever and cough of relatively rapid onset. Complications may inc ...
. The choice of antibiotic will depend on several factors, including the suspected causative organism and whether pneumonia was acquired in the community or developed in a hospital setting. Common options include clindamycin, a combination of a beta-lactam antibiotic
β-lactam antibiotics (beta-lactam antibiotics) are antibiotics that contain a beta-lactam ring in their chemical
structure. This includes penicillin derivatives (penams), cephalosporins and cephamycins (cephems), monobactams, carbapenems and ...
and metronidazole, or an aminoglycoside
Aminoglycoside is a medicinal and bacteriologic category of traditional Gram-negative antibacterial medications that inhibit protein synthesis and contain as a portion of the molecule an amino-modified glycoside (sugar). The term can also refer ...
.
Corticosteroids are sometimes used in aspiration pneumonia, but there is limited evidence to support their effectiveness.
Follow-up
TheBritish Thoracic Society
The British Thoracic Society (BTS) was formed in 1982 by the amalgamation of the British Thoracic Association and the Thoracic Society. It is a registered charity and a company limited by guarantee.
Function
The society's main charitable objecti ...
recommends that a follow-up chest radiograph be taken in people with persistent symptoms, smokers, and people older than 50. American guidelines vary, from generally recommending a follow-up chest radiograph to not mentioning any follow-up.
Prognosis
With treatment, most types of bacterial pneumonia will stabilize in 3–6 days. It often takes a few weeks before most symptoms resolve. X-ray findings typically clear within four weeks and mortality is low (less than 1%). In the elderly or people with other lung problems, recovery may take more than 12 weeks. In persons requiring hospitalization, mortality may be as high as 10%, and in those requiring intensive care it may reach 30–50%. Pneumonia is the most commonhospital-acquired infection
A hospital-acquired infection, also known as a nosocomial infection (from the Greek , meaning "hospital"), is an infection that is acquired in a hospital or other health care facility. To emphasize both hospital and nonhospital settings, it is so ...
that causes death.Murray and Nadel (2010). Chapter 32. Before the advent of antibiotics, mortality was typically 30% in those that were hospitalized. However, for those whose lung condition deteriorates within 72 hours, the problem is usually due to sepsis. If pneumonia deteriorates after 72 hours, it could be due to nosocomial infection
A hospital-acquired infection, also known as a nosocomial infection (from the Greek , meaning "hospital"), is an infection that is acquired in a hospital or other health care facility. To emphasize both hospital and nonhospital settings, it is so ...
or excerbation of other underlying comorbidities. About 10% of those discharged from hospital are readmitted due to underlying co-morbidities such as heart, lung, or neurological disorders, or due to new onset of pneumonia.
Complications may occur in particular in the elderly and those with underlying health problems. This may include, among others: empyema
An empyema () is a collection or gathering of pus within a naturally existing anatomical cavity. For example, pleural empyema is empyema of the pleural cavity. It must be differentiated from an abscess, which is a collection of pus in a newly fo ...
, lung abscess, bronchiolitis obliterans, acute respiratory distress syndrome, sepsis, and worsening of underlying health problems.Cunha (2010). pp. 6–18.
Clinical prediction rules
Clinical prediction rules have been developed to more objectively predict outcomes of pneumonia. These rules are often used to decide whether to hospitalize the person. * Pneumonia severity index (or ''PSI Score'') * CURB-65 score, which takes into account the severity of symptoms, any underlying diseases, and agePleural effusion, empyema, and abscess
 In pneumonia, a collection of fluid may form in the space that surrounds the lung. Occasionally, microorganisms will infect this fluid, causing an
In pneumonia, a collection of fluid may form in the space that surrounds the lung. Occasionally, microorganisms will infect this fluid, causing an empyema
An empyema () is a collection or gathering of pus within a naturally existing anatomical cavity. For example, pleural empyema is empyema of the pleural cavity. It must be differentiated from an abscess, which is a collection of pus in a newly fo ...
. To distinguish an empyema from the more common simple parapneumonic effusion, the fluid may be collected with a needle (thoracentesis
Thoracentesis , also known as thoracocentesis (from Greek ''thōrax'' 'chest, thorax'—GEN ''thōrakos''—and ''kentēsis'' 'pricking, puncture'), pleural tap, needle thoracostomy, or needle decompression (often used term), is an invasive med ...
), and examined. If this shows evidence of empyema, complete drainage of the fluid is necessary, often requiring a drainage catheter. In severe cases of empyema, surgery may be needed. If the infected fluid is not drained, the infection may persist, because antibiotics do not penetrate well into the pleural cavity. If the fluid is sterile, it must be drained only if it is causing symptoms or remains unresolved.
In rare circumstances, bacteria in the lung will form a pocket of infected fluid called a lung abscess. Lung abscesses can usually be seen with a chest X-ray but frequently require a chest CT scan to confirm the diagnosis. Abscesses typically occur in aspiration pneumonia
Aspiration pneumonia is a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs. Signs and symptoms often include fever and cough of relatively rapid onset. Complications may inc ...
, and often contain several types of bacteria. Long-term antibiotics are usually adequate to treat a lung abscess, but sometimes the abscess must be drained by a surgeon or radiologist.
Respiratory and circulatory failure
Pneumonia can cause respiratory failure by triggering acute respiratory distress syndrome (ARDS), which results from a combination of infection and inflammatory response. The lungs quickly fill with fluid and become stiff. This stiffness, combined with severe difficulties extracting oxygen due to the alveolar fluid, may require long periods of mechanical ventilation for survival. Other causes of circulatory failure arehypoxemia
Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the bod ...
, inflammation, and increased coagulability.
Sepsis is a potential complication of pneumonia but usually occurs in people with poor immunity or hyposplenism. The organisms most commonly involved are ''Streptococcus pneumoniae'', ''Haemophilus influenzae'', and ''Klebsiella pneumoniae''. Other causes of the symptoms should be considered such as a myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may ...
or a pulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream ( embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathin ...
.Cunha (2010). pp. 250–51.
Epidemiology
developed world
A developed country (or industrialized country, high-income country, more economically developed country (MEDC), advanced country) is a sovereign state that has a high quality of life, developed economy and advanced technological infrastruct ...
. Viral pneumonia accounts for about 200 million cases. In the United States, as of 2009, pneumonia is the 8th leading cause of death.
Children
In 2008, pneumonia occurred in approximately 156 million children (151 million in the developing world and 5 million in the developed world). In 2010, it resulted in 1.3 million deaths, or 18% of all deaths in those under five years, of which 95% occurred in the developing world. Countries with the greatest burden of disease include India (43 million), China (21 million) and Pakistan (10 million). It is the leading cause of death among children in low income countries. Many of these deaths occur in thenewborn
An infant or baby is the very young offspring of human beings. ''Infant'' (from the Latin word ''infans'', meaning 'unable to speak' or 'speechless') is a formal or specialised synonym for the common term ''baby''. The terms may also be used to ...
period. The World Health Organization estimates that one in three newborn infant deaths is due to pneumonia. Approximately half of these deaths can be prevented, as they are caused by the bacteria for which an effective vaccine is available. In 2011, pneumonia was the most common reason for admission to the hospital after an emergency department visit in the U.S. for infants and children.
History
 Pneumonia has been a common disease throughout human history. The word is from Greek πνεύμων (pneúmōn) meaning "lung". The symptoms were described by
Pneumonia has been a common disease throughout human history. The word is from Greek πνεύμων (pneúmōn) meaning "lung". The symptoms were described by Hippocrates
Hippocrates of Kos (; grc-gre, Ἱπποκράτης ὁ Κῷος, Hippokrátēs ho Kôios; ), also known as Hippocrates II, was a Greek physician of the classical period who is considered one of the most outstanding figures in the history o ...
(–370 BC): "Peripneumonia, and pleuritic affections, are to be thus observed: If the fever be acute, and if there be pains on either side, or in both, and if expiration be if cough be present, and the sputa expectorated be of a blond or livid color, or likewise thin, frothy, and florid, or having any other character different from the common... When pneumonia is at its height, the case is beyond remedy if he is not purged, and it is bad if he has dyspnoea, and urine that is thin and acrid, and if sweats come out about the neck and head, for such sweats are bad, as proceeding from the suffocation, rales, and the violence of the disease which is obtaining the upper hand." However, Hippocrates referred to pneumonia as a disease "named by the ancients". He also reported the results of surgical drainage of empyemas. Maimonides (1135–1204 AD) observed: "The basic symptoms that occur in pneumonia and that are never lacking are as follows: acute fever, sticking pleuritic
Pleurisy, also known as pleuritis, is inflammation of the membranes that surround the lungs and line the chest cavity (pleurae). This can result in a sharp chest pain while breathing. Occasionally the pain may be a constant dull ache. Other sym ...
pain in the side, short rapid breaths, serrated pulse
In medicine, a pulse represents the tactile arterial palpation of the cardiac cycle (heartbeat) by trained fingertips. The pulse may be palpated in any place that allows an artery to be compressed near the surface of the body, such as at the n ...
and cough."Maimonides, ''Fusul Musa'' ("''Pirkei Moshe''"). This clinical description is quite similar to those found in modern textbooks, and it reflected the extent of medical knowledge through the Middle Ages
In the history of Europe, the Middle Ages or medieval period lasted approximately from the late 5th to the late 15th centuries, similar to the post-classical period of global history. It began with the fall of the Western Roman Empire ...
into the 19th century.
Edwin Klebs was the first to observe bacteria in the airways of persons having died of pneumonia in 1875. Initial work identifying the two common bacterial causes, ''Streptococcus pneumoniae'' and ''Klebsiella pneumoniae'', was performed by Carl Friedländer
Carl Friedländer (19 November 1847, Brieg (Brzeg), Silesia – 13 May 1887, Meran (Merano), County of Tyrol) was a German pathologist and microbiologist who helped discover the bacterial cause of pneumonia in 1882. He also first described t ...
and Albert Fraenkel in 1882 and 1884, respectively. Friedländer's initial work introduced the Gram stain
In microbiology and bacteriology, Gram stain (Gram staining or Gram's method), is a method of staining used to classify bacterial species into two large groups: gram-positive bacteria and gram-negative bacteria. The name comes from the Danish b ...
, a fundamental laboratory test still used today to identify and categorize bacteria. Christian Gram
Hans Christian Joachim Gram (13 September 1853 – 14 November 1938) was a Danish bacteriologist noted for his development of the Gram stain, still a standard technique to classify bacteria and make them more visible under a microscope.
Early ...
's paper describing the procedure in 1884 helped to differentiate the two bacteria, and showed that pneumonia could be caused by more than one microorganism. In 1887, Jaccond demonstrated pneumonia may be caused by opportunistic bacteria always present in the lung.
Sir William Osler, known as "the father of modern medicine", appreciated the death and disability caused by pneumonia, describing it as the "captain of the men of death" in 1918, as it had overtaken tuberculosis as one of the leading causes of death in this time. This phrase was originally coined by John Bunyan
John Bunyan (; baptised 30 November 162831 August 1688) was an English writer and Puritan preacher best remembered as the author of the Christian allegory ''The Pilgrim's Progress,'' which also became an influential literary model. In addition ...
in reference to "consumption" (tuberculosis). Osler also described pneumonia as "the old man's friend" as death was often quick and painless when there were much slower and more painful ways to die.
Viral pneumonia was first described by Hobart Reimann in 1938. Reimann, Chairman of the Department of Medicine at Jefferson Medical College, had established the practice of routinely typing the pneumococcal organism in cases where pneumonia presented. Out of this work, the distinction between viral and bacterial strains was noticed.
Several developments in the 1900s improved the outcome for those with pneumonia. With the advent of penicillin and other antibiotics, modern surgical techniques, and intensive care in the 20th century, mortality from pneumonia, which had approached 30%, dropped precipitously in the developed world. Vaccination of infants against '' Haemophilus influenzae'' type B began in 1988 and led to a dramatic decline in cases shortly thereafter. Vaccination against ''Streptococcus pneumoniae'' in adults began in 1977, and in children in 2000, resulting in a similar decline.
Society and culture
Awareness
Due to the relatively low awareness of the disease, 12 November was declared as the annual World Pneumonia Day, a day for concerned citizens and policy makers to take action against the disease, in 2009.Costs
The global economic cost of community-acquired pneumonia has been estimated at $17 billion annually. Other estimates are considerably higher. In 2012 the estimated aggregate costs of treating pneumonia in the United States were $20 billion; the median cost of a single pneumonia-related hospitalization is over $15,000. According to data released by the Centers for Medicare and Medicaid Services, average 2012 hospital charges for inpatient treatment of uncomplicated pneumonia in the U.S. were $24,549 and ranged as high as $124,000. The average cost of an emergency room consult for pneumonia was $943 and the average cost for medication was $66. Aggregate annual costs of treating pneumonia in Europe have been estimated at €10 billion.References
Footnotes CitationsBibliography
* *External links
{{Authority control Articles containing video clips Coronavirus-associated diseases Infectious diseases Respiratory and cardiovascular disorders specific to the perinatal period Wikipedia medicine articles ready to translate (full) Wikipedia emergency medicine articles ready to translate