Bacterial Meningitis on:
[Wikipedia]
[Google]
[Amazon]
Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the
 In adults, the most common symptom of meningitis is a severe headache, occurring in almost 90% of cases of bacterial meningitis, followed by neck stiffness (the inability to flex the neck forward passively due to increased neck muscle tone and stiffness). The classic triad of diagnostic signs consists of neck stiffness, sudden high fever, and
In adults, the most common symptom of meningitis is a severe headache, occurring in almost 90% of cases of bacterial meningitis, followed by neck stiffness (the inability to flex the neck forward passively due to increased neck muscle tone and stiffness). The classic triad of diagnostic signs consists of neck stiffness, sudden high fever, and
 Additional problems may occur in the early stage of the illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may trigger
Additional problems may occur in the early stage of the illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may trigger
 The types of bacteria that cause bacterial meningitis vary according to the infected individual's age group.
* In
The types of bacteria that cause bacterial meningitis vary according to the infected individual's age group.
* In

 A lumbar puncture is done by positioning the person, usually lying on the side, applying
A lumbar puncture is done by positioning the person, usually lying on the side, applying
 Meningitis can be diagnosed after death has occurred. The findings from a post mortem are usually a widespread inflammation of the
Meningitis can be diagnosed after death has occurred. The findings from a post mortem are usually a widespread inflammation of the
meninges
In anatomy, the meninges (, ''singular:'' meninx ( or ), ) are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in ...
. The most common symptoms are fever, headache, and neck stiffness. Other symptoms include confusion
In medicine, confusion is the quality or state of being bewildered or unclear. The term "acute mental confusion"
or altered consciousness
Consciousness, at its simplest, is sentience and awareness of internal and external existence. However, the lack of definitions has led to millennia of analyses, explanations and debates by philosophers, theologians, linguisticians, and scien ...
, nausea, vomiting, and an inability to tolerate light or loud noises. Young children often exhibit only nonspecific symptoms, such as irritability, drowsiness, or poor feeding. A non-blanching rash (a rash that does not fade when a glass is rolled over it) may also be present.
The inflammation may be caused by infection with viruses, bacteria or other microorganisms. Non-infectious causes include malignancy
Malignancy () is the tendency of a medical condition to become progressively worse.
Malignancy is most familiar as a characterization of cancer. A ''malignant'' tumor contrasts with a non-cancerous ''benign'' tumor in that a malignancy is not s ...
( cancer), subarachnoid haemorrhage
Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consci ...
, chronic inflammatory disease (sarcoidosis
Sarcoidosis (also known as ''Besnier-Boeck-Schaumann disease'') is a disease involving abnormal collections of inflammatory cells that form lumps known as granulomata. The disease usually begins in the lungs, skin, or lymph nodes. Less commonly a ...
) and certain drugs. Meningitis can be life-threatening because of the inflammation's proximity to the brain and spinal cord; therefore, the condition is classified as a medical emergency. A lumbar puncture, in which a needle is inserted into the spinal canal
The spinal canal (or vertebral canal or spinal cavity) is the canal that contains the spinal cord within the vertebral column. The spinal canal is formed by the vertebrae through which the spinal cord passes. It is a process of the dorsal body ...
to collect a sample of cerebrospinal fluid
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
CSF is produced by specialised ependymal cells in the choroid plexus of the ventricles of the b ...
(CSF), can diagnose or exclude meningitis.
Some forms of meningitis are preventable by immunization with the meningococcal
''Neisseria meningitidis'', often referred to as meningococcus, is a Gram-negative bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia, a life-threatening sepsis. The bacterium is referred to as a ...
, mumps
MUMPS ("Massachusetts General Hospital Utility Multi-Programming System"), or M, is an imperative, high-level programming language with an integrated transaction processing key–value database. It was originally developed at Massachusetts Gener ...
, pneumococcal
''Streptococcus pneumoniae'', or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic (under aerobic conditions) or beta-hemolytic (under anaerobic conditions), aerotolerant anaerobic member of the genus Streptococcus. They are ...
, and Hib vaccines. Giving antibiotic
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention ...
s to people with significant exposure to certain types of meningitis may also be useful. The first treatment in acute meningitis consists of promptly giving antibiotics and sometimes antiviral drug
Antiviral drugs are a class of medication used for treating viral infections. Most antivirals target specific viruses, while a broad-spectrum antiviral is effective against a wide range of viruses. Unlike most antibiotics, antiviral drugs do ...
s. Corticosteroid
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involve ...
s can also be used to prevent complications from excessive inflammation. Meningitis can lead to serious long-term consequences such as deafness
Deafness has varying definitions in cultural and medical contexts. In medical contexts, the meaning of deafness is hearing loss that precludes a person from understanding spoken language, an audiological condition. In this context it is written ...
, epilepsy, hydrocephalus
Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary i ...
, or cognitive deficit
Cognitive deficit is an inclusive term to describe any characteristic that acts as a barrier to the cognition process.
The term may describe
* deficits in overall intelligence (as with intellectual disabilities),
* specific and restricted defici ...
s, especially if not treated quickly.
In 2019, meningitis was prevalent in about 7.7 million people worldwide. This resulted in 236,000 deaths, down from 433,000 deaths in 1990. With appropriate treatment, the risk of death in bacterial meningitis is less than 15%. Outbreaks of bacterial meningitis occur between December and June each year in an area of sub-Saharan Africa known as the meningitis belt. Smaller outbreaks may also occur in other areas of the world. The word meningitis comes from the Greek μῆνιγξ ''meninx'', "membrane", and the medical suffix ''-itis'', "inflammation".
Signs and symptoms
Clinical features
 In adults, the most common symptom of meningitis is a severe headache, occurring in almost 90% of cases of bacterial meningitis, followed by neck stiffness (the inability to flex the neck forward passively due to increased neck muscle tone and stiffness). The classic triad of diagnostic signs consists of neck stiffness, sudden high fever, and
In adults, the most common symptom of meningitis is a severe headache, occurring in almost 90% of cases of bacterial meningitis, followed by neck stiffness (the inability to flex the neck forward passively due to increased neck muscle tone and stiffness). The classic triad of diagnostic signs consists of neck stiffness, sudden high fever, and altered mental status
An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment.
A mildly depressed level of consciousne ...
; however, all three features are present in only 44–46% of bacterial meningitis cases. If none of the three signs are present, acute meningitis is extremely unlikely. Other signs commonly associated with meningitis include photophobia
Photophobia is a medical symptom of abnormal intolerance to visual perception of light. As a medical symptom photophobia is not a morbid fear or phobia, but an experience of discomfort or pain to the eyes due to light exposure or by presence of ...
(intolerance to bright light) and phonophobia
Phonophobia, also called ligyrophobia or sonophobia, is a fear of or aversion to loud sounds (for example fireworks)—a type of specific phobia. It is a very rare phobia which is often the symptom of hyperacusis. Sonophobia can refer to the hype ...
(intolerance to loud noises). Small children often do not exhibit the aforementioned symptoms, and may only be irritable and look unwell. The fontanelle
A fontanelle (or fontanel) (colloquially, soft spot) is an anatomical feature of the infant human skull comprising soft membranous gaps ( sutures) between the cranial bones that make up the calvaria of a fetus or an infant. Fontanelles allow f ...
(the soft spot on the top of a baby's head) can bulge in infants aged up to 6 months. Other features that distinguish meningitis from less severe illnesses in young children are leg pain, cold extremities, and an abnormal skin color.
Nuchal rigidity
Neck stiffness, stiff neck and nuchal rigidity are terms often used interchangeably to describe the medical condition when one experiences discomfort or pain when trying to turn, move, or flex the neck. Possible causes include muscle strain or spr ...
occurs in 70% of bacterial meningitis in adults. Other signs include the presence of positive Kernig's sign
Kernig's sign is a test used in physical examination to look for evidence of irritation of the meninges. The test involves flexing the thighs at the hip, and the knees, at 90 degree angles, and assessing whether subsequent extension of the knee i ...
or Brudziński sign. Kernig's sign is assessed with the person lying supine
In grammar, a supine is a form of verbal noun used in some languages. The term is most often used for Latin, where it is one of the four principal parts of a verb. The word refers to a position of lying on one's back (as opposed to 'prone' ...
, with the hip and knee flexed to 90 degrees. In a person with a positive Kernig's sign, pain limits passive extension of the knee. A positive Brudzinski's sign occurs when flexion of the neck causes involuntary flexion of the knee and hip. Although Kernig's sign and Brudzinski's sign are both commonly used to screen for meningitis, the sensitivity of these tests is limited. They do, however, have very good specificity for meningitis: the signs rarely occur in other diseases. Another test, known as the "jolt accentuation maneuver" helps determine whether meningitis is present in those reporting fever and headache. A person is asked to rapidly rotate the head horizontally; if this does not make the headache worse, meningitis is unlikely.
Other problems can produce symptoms similar to those above, but from non-meningitic causes. This is called meningism or pseudomeningitis.
Meningitis caused by the bacterium '' Neisseria meningitidis'' (known as "meningococcal meningitis") can be differentiated from meningitis with other causes by a rapidly spreading petechial rash, which may precede other symptoms. The rash consists of numerous small, irregular purple or red spots ("petechiae") on the trunk, lower extremities, mucous membranes, conjunctiva, and (occasionally) the palms of the hands or soles of the feet. The rash is typically non-blanching; the redness does not disappear when pressed with a finger or a glass tumbler. Although this rash is not necessarily present in meningococcal meningitis, it is relatively specific for the disease; it does, however, occasionally occur in meningitis due to other bacteria. Other clues on the cause of meningitis may be the skin signs of hand, foot and mouth disease
Hand, foot, and mouth disease (HFMD) is a common infection caused by a group of enteroviruses. It typically begins with a fever and feeling generally unwell. This is followed a day or two later by flat discolored spots or bumps that may bli ...
and genital herpes
Genital herpes is an infection by the herpes simplex virus (HSV) of the genitals. Most people either have no or mild symptoms and thus do not know they are infected. When symptoms do occur, they typically include small blisters that break open ...
, both of which are associated with various forms of viral meningitis.
Early complications
 Additional problems may occur in the early stage of the illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may trigger
Additional problems may occur in the early stage of the illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may trigger sepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is follo ...
, a systemic inflammatory response syndrome
Systemic inflammatory response syndrome (SIRS) is an inflammatory state affecting the whole body. It is the body's response to an infectious or noninfectious insult. Although the definition of SIRS refers to it as an "inflammatory" response, i ...
of falling blood pressure, fast heart rate, high or abnormally low temperature, and rapid breathing. Very low blood pressure may occur at an early stage, especially but not exclusively in meningococcal meningitis; this may lead to insufficient blood supply to other organs. Disseminated intravascular coagulation, the excessive activation of blood clotting
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechan ...
, may obstruct blood flow
Hemodynamics or haemodynamics are the dynamics of blood flow. The circulatory system is controlled by homeostatic mechanisms of autoregulation, just as hydraulic circuits are controlled by control systems. The hemodynamic response continuously ...
to organs and paradoxically increase the bleeding risk. Gangrene of limbs can occur in meningococcal disease. Severe meningococcal and pneumococcal infections may result in hemorrhaging of the adrenal gland
The adrenal glands (also known as suprarenal glands) are endocrine glands that produce a variety of hormones including adrenaline and the steroids aldosterone and cortisol. They are found above the kidneys. Each gland has an outer cortex which ...
s, leading to Waterhouse-Friderichsen syndrome, which is often fatal.
The brain tissue may swell, pressure inside the skull may increase and the swollen brain may herniate through the skull base. This may be noticed by a decreasing level of consciousness
An altered level of consciousness is any measure of arousal other than normal. Level of consciousness (LOC) is a measurement of a person's arousability and responsiveness to stimuli from the environment.
A mildly depressed level of consciousne ...
, loss of the pupillary light reflex, and abnormal posturing
Abnormal posturing is an involuntary flexion or extension of the arms and legs, indicating severe brain injury. It occurs when one set of muscles becomes incapacitated while the opposing set is not, and an external stimulus such as pain caus ...
. The inflammation of the brain tissue may also obstruct the normal flow of CSF around the brain (hydrocephalus
Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary i ...
). Seizure
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with los ...
s may occur for various reasons; in children, seizures are common in the early stages of meningitis (in 30% of cases) and do not necessarily indicate an underlying cause. Seizures may result from increased pressure and from areas of inflammation in the brain tissue. Focal seizures
Focal seizures (also called partial seizures and localized seizures) are seizures which affect initially only one hemisphere of the brain. The brain is divided into two hemispheres, each consisting of four lobes – the frontal, temporal, parie ...
(seizures that involve one limb or part of the body), persistent seizures, late-onset seizures and those that are difficult to control with medication indicate a poorer long-term outcome.
Inflammation of the meninges may lead to abnormalities of the cranial nerves
Cranial nerves are the nerves that emerge directly from the brain (including the brainstem), of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and f ...
, a group of nerves arising from the brain stem
The brainstem (or brain stem) is the posterior stalk-like part of the brain that connects the cerebrum with the spinal cord. In the human brain the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is conti ...
that supply the head and neck area and which control, among other functions, eye movement, facial muscles, and hearing. Visual symptoms and hearing loss may persist after an episode of meningitis. Inflammation of the brain (encephalitis
Encephalitis is inflammation of the brain. The severity can be variable with symptoms including reduction or alteration in consciousness, headache, fever, confusion, a stiff neck, and vomiting. Complications may include seizures, hallucinations, ...
) or its blood vessels (cerebral vasculitis
Cerebral vasculitis (sometimes the word angiitis is used instead of "vasculitis") is vasculitis (inflammation of the blood vessel wall) involving the brain and occasionally the spinal cord. It affects all of the vessels: very small blood vessels ( ...
), as well as the formation of blood clots
A thrombus (plural thrombi), colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cr ...
in the veins ( cerebral venous thrombosis), may all lead to weakness, loss of sensation, or abnormal movement or function of the part of the body supplied by the affected area of the brain.
Causes
Meningitis is typically caused by an infection with microorganisms. Most infections are due to viruses, with bacteria, fungi, andprotozoa
Protozoa (singular: protozoan or protozoon; alternative plural: protozoans) are a group of single-celled eukaryotes, either free-living or parasitic, that feed on organic matter such as other microorganisms or organic tissues and debris. Histo ...
being the next most common causes. It may also result from various non-infectious causes. The term ''aseptic meningitis
Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, mycob ...
'' refers to cases of meningitis in which no bacterial infection can be demonstrated. This type of meningitis is usually caused by viruses but it may be due to bacterial infection that has already been partially treated, when bacteria disappear from the meninges, or pathogens infect a space adjacent to the meninges (e.g. sinusitis
Sinusitis, also known as rhinosinusitis, is inflammation of the mucous membranes that line the sinuses resulting in symptoms that may include thick nasal mucus, a plugged nose, and facial pain. Other signs and symptoms may include fever, hea ...
). Endocarditis (an infection of the heart valves which spreads small clusters of bacteria through the bloodstream) may cause aseptic meningitis. Aseptic meningitis may also result from infection with spirochetes, a group of bacteria that includes '' Treponema pallidum'' (the cause of syphilis
Syphilis () is a sexually transmitted infection caused by the bacterium ''Treponema pallidum'' subspecies ''pallidum''. The signs and symptoms of syphilis vary depending in which of the four stages it presents (primary, secondary, latent, and ...
) and ''Borrelia burgdorferi
''Borrelia burgdorferi'' is a bacterial species of the spirochete class in the genus ''Borrelia'', and is one of the causative agents of Lyme disease in humans. Along with a few similar genospecies, some of which also cause Lyme disease, it make ...
'' (known for causing Lyme disease). Meningitis may be encountered in cerebral malaria
Malaria is a Mosquito-borne disease, mosquito-borne infectious disease that affects humans and other animals. Malaria causes Signs and symptoms, symptoms that typically include fever, fatigue (medical), tiredness, vomiting, and headaches. In se ...
(malaria infecting the brain) or amoebic meningitis, meningitis due to infection with amoebae
An amoeba (; less commonly spelled ameba or amœba; plural ''am(o)ebas'' or ''am(o)ebae'' ), often called an amoeboid, is a type of cell or unicellular organism with the ability to alter its shape, primarily by extending and retracting pseudopo ...
such as ''Naegleria fowleri
''Naegleria fowleri'', colloquially known as a "brain-eating amoeba", is a species of the genus ''Naegleria'', belonging to the phylum Percolozoa, which is technically not classified as true amoeba, but a shapeshifting amoeboflagellate excava ...
'', contracted from freshwater sources.
Bacterial
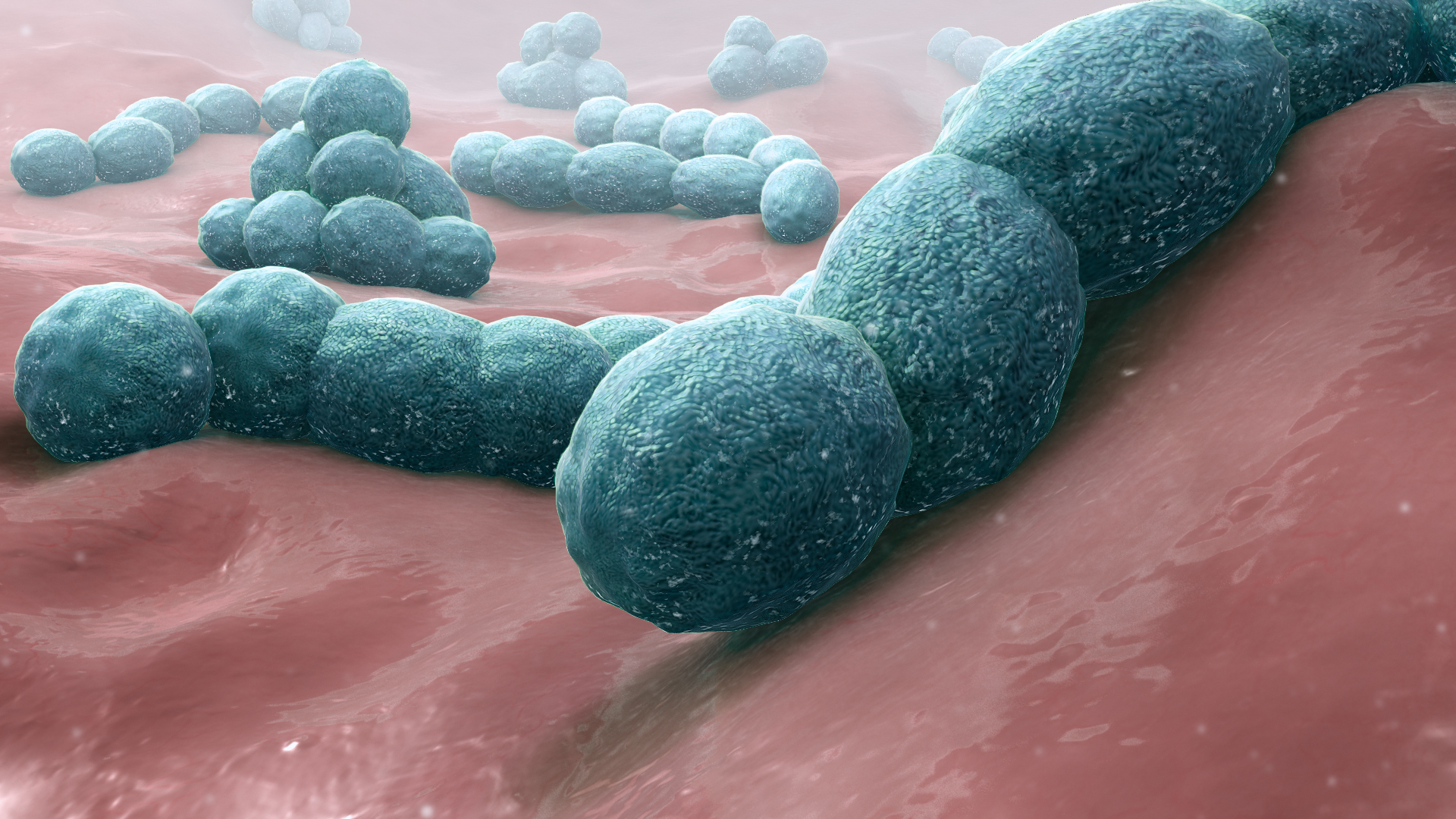
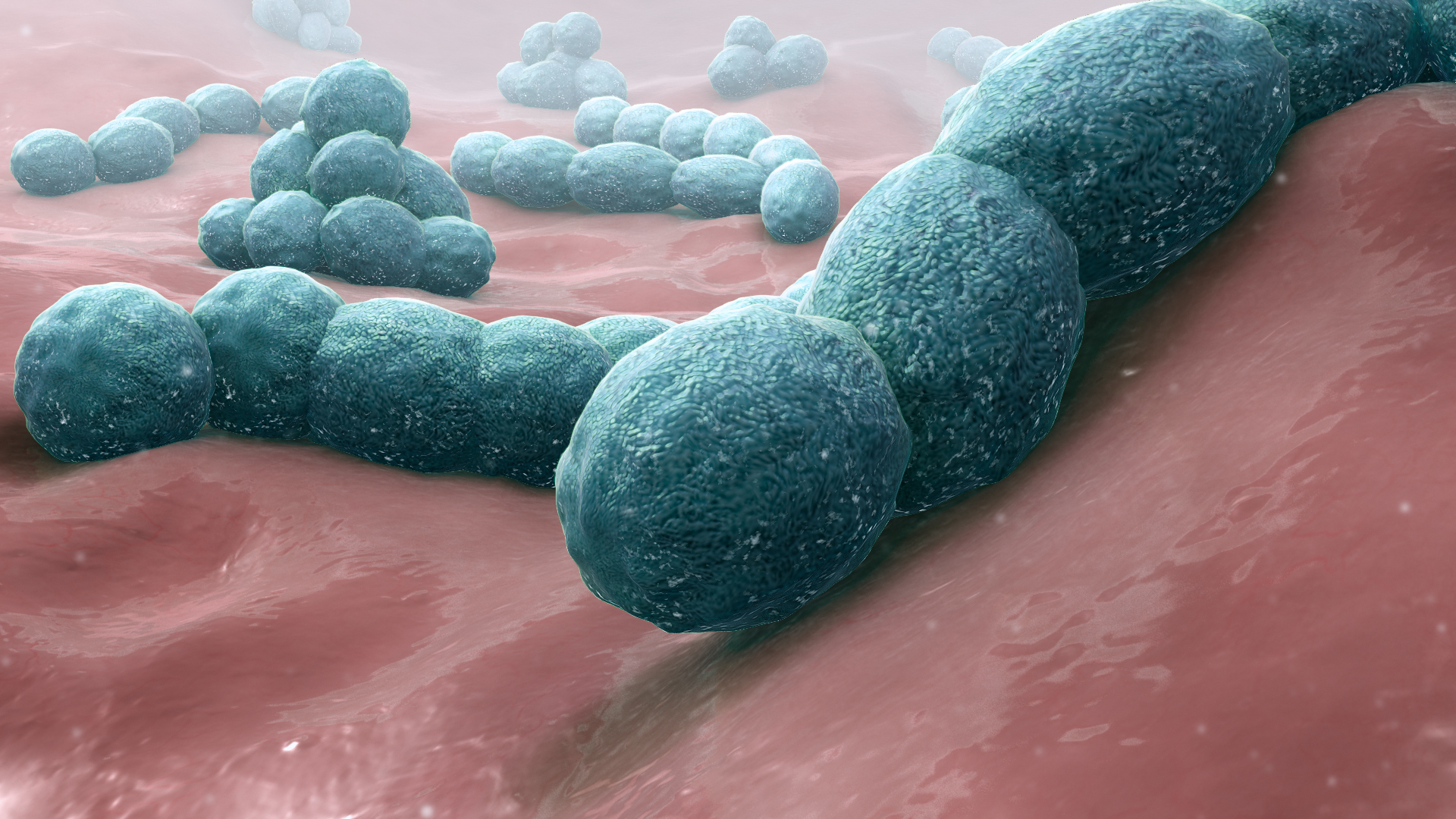 The types of bacteria that cause bacterial meningitis vary according to the infected individual's age group.
* In
The types of bacteria that cause bacterial meningitis vary according to the infected individual's age group.
* In premature babies
Preterm birth, also known as premature birth, is the birth of a baby at fewer than 37 weeks gestational age, as opposed to full-term delivery at approximately 40 weeks. Extreme preterm is less than 28 weeks, very early preterm birth is between ...
and newborns
An infant or baby is the very young offspring of human beings. ''Infant'' (from the Latin word ''infans'', meaning 'unable to speak' or 'speechless') is a formal or specialised synonym for the common term ''baby''. The terms may also be used t ...
up to three months old, common causes are '' group B streptococci'' (subtypes III which normally inhabit the vagina and are mainly a cause during the first week of life) and bacteria that normally inhabit the digestive tract
The gastrointestinal tract (GI tract, digestive tract, alimentary canal) is the tract or passageway of the digestive system that leads from the mouth to the anus. The GI tract contains all the major organs of the digestive system, in humans and ...
such as ''Escherichia coli
''Escherichia coli'' (),Wells, J. C. (2000) Longman Pronunciation Dictionary. Harlow ngland Pearson Education Ltd. also known as ''E. coli'' (), is a Gram-negative, facultative anaerobic, rod-shaped, coliform bacterium of the genus '' Esc ...
'' (carrying the K1 antigen). '' Listeria monocytogenes'' (serotype IVb) can be contracted when consuming improperly prepared food such as dairy products, produce and deli meats, and may cause meningitis in the newborn.
* Older children are more commonly affected by '' Neisseria meningitidis'' (meningococcus) and '' Streptococcus pneumoniae'' (serotypes 6, 9, 14, 18 and 23) and those under five by ''Haemophilus influenzae'' type B (in countries that do not offer vaccination).
* In adults, ''Neisseria meningitidis'' and ''Streptococcus pneumoniae'' together cause 80% of bacterial meningitis cases. Risk of infection with ''Listeria monocytogenes'' is increased in people over 50 years old. The introduction of pneumococcal vaccine has lowered rates of pneumococcal meningitis in both children and adults.
Recent skull trauma
Trauma most often refers to:
*Major trauma, in physical medicine, severe physical injury caused by an external source
*Psychological trauma, a type of damage to the psyche that occurs as a result of a severely distressing event
*Traumatic inju ...
potentially allows nasal cavity bacteria to enter the meningeal space. Similarly, devices in the brain and meninges, such as cerebral shunt
A cerebral shunt is a device permanently implanted inside the head and body to drain excess fluid away from the brain. They are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If ...
s, extraventricular drains or Ommaya reservoir
An Ommaya reservoir is an intraventricular catheter system that can be used for the aspiration of cerebrospinal fluid or for the delivery of drugs (e.g. chemotherapy) into the cerebrospinal fluid. It consists of a catheter in one lateral ventricle ...
s, carry an increased risk of meningitis. In these cases, people are more likely to be infected with Staphylococci
''Staphylococcus'' is a genus of Gram-positive bacteria in the family Staphylococcaceae from the order Bacillales. Under the microscope, they appear spherical ( cocci), and form in grape-like clusters. ''Staphylococcus'' species are faculta ...
, Pseudomonas
''Pseudomonas'' is a genus of Gram-negative, Gammaproteobacteria, belonging to the family Pseudomonadaceae and containing 191 described species. The members of the genus demonstrate a great deal of metabolic diversity and consequently are able to ...
, and other Gram-negative bacteria. These pathogens are also associated with meningitis in people with an impaired immune system. An infection in the head and neck area, such as otitis media
Otitis media is a group of inflammatory diseases of the middle ear. One of the two main types is acute otitis media (AOM), an infection of rapid onset that usually presents with ear pain. In young children this may result in pulling at the ear, ...
or mastoiditis
Mastoiditis is the result of an infection that extends to the air cells of the skull behind the ear. Specifically, it is an inflammation of the mucosal lining of the mastoid antrum and mastoid air cell system inside the mastoid process. The m ...
, can lead to meningitis in a small proportion of people. Recipients of cochlear implant
A cochlear implant (CI) is a surgically implanted neuroprosthesis that provides a person who has moderate-to-profound sensorineural hearing loss with sound perception. With the help of therapy, cochlear implants may allow for improved speech unde ...
s for hearing loss are more at risk for pneumococcal meningitis.
Tuberculous meningitis, which is meningitis caused by ''Mycobacterium tuberculosis
''Mycobacterium tuberculosis'' (M. tb) is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis. First discovered in 1882 by Robert Koch, ''M. tuberculosis'' has an unusual, waxy coating on its ...
'', is more common in people from countries in which tuberculosis is endemic, but is also encountered in people with immune problems, such as AIDS
Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual ma ...
.
Recurrent bacterial meningitis may be caused by persisting anatomical defects, either congenital
A birth defect, also known as a congenital disorder, is an abnormal condition that is present at birth regardless of its cause. Birth defects may result in disabilities that may be physical, intellectual, or developmental. The disabilities can ...
or acquired, or by disorders of the immune system. Anatomical defects allow continuity between the external environment and the nervous system. The most common cause of recurrent meningitis is a skull fracture, particularly fractures that affect the base of the skull or extend towards the sinuses and petrous pyramids. Approximately 59% of recurrent meningitis cases are due to such anatomical abnormalities, 36% are due to immune deficiencies (such as complement deficiency
Complement deficiency is an immunodeficiency of absent or suboptimal functioning of one of the complement system proteins. Because of redundancies in the immune system, many complement disorders are never diagnosed. Some studies estimate that less ...
, which predisposes especially to recurrent meningococcal meningitis), and 5% are due to ongoing infections in areas adjacent to the meninges.
Viral
Viruses that cause meningitis includeenterovirus
''Enterovirus'' is a genus of positive-sense single-stranded RNA viruses associated with several human and mammalian diseases. Enteroviruses are named by their transmission-route through the intestine ('enteric' meaning intestinal).
Serologic ...
es, herpes simplex virus (generally type 2, which produces most genital sores; less commonly type 1), varicella zoster virus
Varicella-zoster virus (VZV), also known as human herpesvirus 3 (HHV-3, HHV3) or ''Human alphaherpesvirus 3'' ( taxonomically), is one of nine known herpes viruses that can infect humans. It causes chickenpox (varicella) commonly affecting chi ...
(known for causing chickenpox
Chickenpox, also known as varicella, is a highly contagious disease caused by the initial infection with varicella zoster virus (VZV). The disease results in a characteristic skin rash that forms small, itchy blisters, which eventually scab ...
and shingles), mumps virus
The mumps virus (MuV) is the virus that causes mumps. MuV contains a single-stranded, negative-sense genome made of ribonucleic acid (RNA). Its genome is about 15,000 nucleotides in length and contains seven genes that encode nine proteins. The ...
, HIV
The human immunodeficiency viruses (HIV) are two species of ''Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune ...
, LCMV
Lymphocytic choriomeningitis (LCM) is a rodent-borne viral infectious disease that presents as aseptic meningitis, encephalitis or meningoencephalitis. Its causative agent is ''lymphocytic choriomeningitis mammarenavirus'' (LCMV), a member of th ...
, Arboviruses
Arbovirus is an informal name for any virus that is transmitted by arthropod vectors. The term ''arbovirus'' is a portmanteau word (''ar''thropod-''bo''rne ''virus''). ''Tibovirus'' (''ti''ck-''bo''rne ''virus'') is sometimes used to more spe ...
(acquired from a mosquito or other insect), and the Influenza virus. Mollaret's meningitis
Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis ...
is a chronic recurrent form of herpes meningitis; it is thought to be caused by herpes simplex virus type 2.
Fungal
There are a number of risk factors forfungal meningitis
Fungal meningitis refers to meningitis caused by a fungal infection.
Signs and symptoms
Symptoms of fungal meningitis are generally similar to those of other types of meningitis, and include: a fever, stiff neck, severe headache, photophobia ...
, including the use of immunosuppressant
Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are drugs that inhibit or prevent activity of the immune system.
Classification
Immunosuppressive drugs can be classified in ...
s (such as after organ transplantation), HIV/AIDS, and the loss of immunity associated with aging. It is uncommon in those with a normal immune system but has occurred with medication contamination. Symptom onset is typically more gradual, with headaches and fever being present for at least a couple of weeks before diagnosis. The most common fungal meningitis is cryptococcal meningitis
Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When th ...
due to ''Cryptococcus neoformans
''Cryptococcus neoformans'' is an encapsulated yeast belonging to the class Tremellomycetes and an obligate aerobe that can live in both plants and animals. Its teleomorph is a filamentous fungus, formerly referred to ''Filobasidiella neoformans ...
''. In Africa, cryptococcal meningitis is now the most common cause of meningitis in multiple studies, and it accounts for 20–25% of AIDS-related deaths in Africa. Other less common fungal pathogens which can cause meningitis include: ''Coccidioides immitis
''Coccidioides immitis'' is a pathogenic fungus that resides in the soil in certain parts of the southwestern United States, northern Mexico, and a few other areas in the Western Hemisphere.
Epidemiology
''C. immitis'', along with its rela ...
'', ''Histoplasma capsulatum
''Histoplasma capsulatum'' is a species of dimorphic fungus. Its sexual form is called ''Ajellomyces capsulatus''. It can cause pulmonary and disseminated histoplasmosis.
''H. capsulatum'' is "distributed worldwide, except in Antarctica, but ...
'', ''Blastomyces dermatitidis
''Blastomyces dermatitidis'' is a dimorphic fungus that causes blastomycosis, an invasive and often serious fungal infection found occasionally in humans and other animals. It lives in soil and wet, decaying wood, often in an area close to a wat ...
'', and '' Candida'' species.
Parasitic
A parasitic cause is often assumed when there is a predominance ofeosinophils
Eosinophils, sometimes called eosinophiles or, less commonly, acidophils, are a variety of white blood cells (WBCs) and one of the immune system components responsible for combating multicellular parasites and certain infections in vertebrates. ...
(a type of white blood cell) in the CSF. The most common parasites implicated are ''Angiostrongylus cantonensis
''Angiostrongylus cantonensis'' is a parasitic nematode (roundworm) that causes angiostrongyliasis, the most common cause of eosinophilic meningitis in Southeast Asia and the Pacific Basin. The nematode commonly resides in the pulmonary arterie ...
'', ''Gnathostoma spinigerum
''Gnathostoma spinigerum'' is a parasitic nematode that causes gnathostomiasis in humans, also known as its clinical manifestations are '' creeping eruption'', ''larva migrans'', ''Yangtze edema'', ''Choko-Fuschu Tua chid'' and ''wandering swelli ...
'', '' Schistosoma'', as well as the conditions cysticercosis
Cysticercosis is a tissue infection caused by the young form of the pork tapeworm. People may have few or no symptoms for years. In some cases, particularly in Asia, solid lumps of between one and two centimetres may develop under the skin. Aft ...
, toxocariasis
Toxocariasis is an illness of humans caused by the dog roundworm (''Toxocara canis'') and, less frequently, the cat roundworm ('' Toxocara cati'').https://academic.oup.com/ajcp/article/142/suppl_1/A104/1771175 Eosinophilic Pseudoleukemia Due to T ...
, baylisascariasis
''Baylisascaris procyonis'', also known by the common name of raccoon roundworm, is a roundworm nematode, found ubiquitously in raccoons, the definitive hosts. It is named after H. A. Baylis, who studied them in the 1920s–30s, and Greek '' ask ...
, paragonimiasis, and a number of rarer infections and noninfective conditions.
Non-infectious
Meningitis may occur as the result of several non-infectious causes: spread of cancer to the meninges ('' malignant or neoplastic meningitis'') and certain drugs (mainly non-steroidal anti-inflammatory drugs,antibiotic
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention ...
s and intravenous immunoglobulins). It may also be caused by several inflammatory conditions, such as sarcoidosis
Sarcoidosis (also known as ''Besnier-Boeck-Schaumann disease'') is a disease involving abnormal collections of inflammatory cells that form lumps known as granulomata. The disease usually begins in the lungs, skin, or lymph nodes. Less commonly a ...
(which is then called neurosarcoidosis
Neurosarcoidosis (sometimes shortened to neurosarcoid) refers to a type of sarcoidosis, a condition of unknown cause featuring granulomas in various tissues, in this type involving the central nervous system (brain and spinal cord). Neurosarcoidosi ...
), connective tissue disorders such as systemic lupus erythematosus
Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Commo ...
, and certain forms of vasculitis (inflammatory conditions of the blood vessel wall), such as Behçet's disease
Behçet's disease (BD) is a type of inflammatory disorder which affects multiple parts of the body. The most common symptoms include painful sores on the mucous membranes of the mouth and other parts of the body, inflammation of parts of the e ...
. Epidermoid cyst
An epidermoid cyst or epidermal inclusion cyst is a benign cyst usually found on the skin. The cyst develops out of ectodermal tissue. Histologically, it is made of a thin layer of squamous epithelium.
Signs and symptoms
The epidermoid cyst may ...
s and dermoid cyst
A dermoid cyst is a teratoma of a cystic nature that contains an array of developmentally mature, solid tissues. It frequently consists of skin, hair follicles, and sweat glands, while other commonly found components include clumps of long hair ...
s may cause meningitis by releasing irritant matter into the subarachnoid space. Rarely, migraine may cause meningitis, but this diagnosis is usually only made when other causes have been eliminated.
Mechanism
The meninges comprise three membranes that, together with thecerebrospinal fluid
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
CSF is produced by specialised ependymal cells in the choroid plexus of the ventricles of the b ...
, enclose and protect the brain and spinal cord (the central nervous system
The central nervous system (CNS) is the part of the nervous system consisting primarily of the brain and spinal cord. The CNS is so named because the brain integrates the received information and coordinates and influences the activity of all par ...
). The pia mater
Pia mater ( or ),Entry "pia mater"
in
arachnoid mater The arachnoid mater (or simply arachnoid) is one of the three meninges, the protective membranes that cover the brain and spinal cord. It is so named because of its resemblance to a spider web. The arachnoid mater is a derivative of the neural ...
(so named because of its spider-web-like appearance) is a loosely fitting sac on top of the pia mater. The in
arachnoid mater The arachnoid mater (or simply arachnoid) is one of the three meninges, the protective membranes that cover the brain and spinal cord. It is so named because of its resemblance to a spider web. The arachnoid mater is a derivative of the neural ...
subarachnoid space
In anatomy, the meninges (, ''singular:'' meninx ( or ), ) are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in ...
separates the arachnoid and pia mater membranes and is filled with cerebrospinal fluid. The outermost membrane, the dura mater, is a thick durable membrane, which is attached to both the arachnoid membrane and the skull.
In bacterial meningitis, bacteria reach the meninges by one of two main routes: through the bloodstream (hematogenous spread) or through direct contact between the meninges and either the nasal cavity or the skin. In most cases, meningitis follows invasion of the bloodstream by organisms that live on mucosal surfaces such as the nasal cavity. This is often in turn preceded by viral infections, which break down the normal barrier provided by the mucosal surfaces. Once bacteria have entered the bloodstream, they enter the subarachnoid space
In anatomy, the meninges (, ''singular:'' meninx ( or ), ) are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in ...
in places where the blood–brain barrier
The blood–brain barrier (BBB) is a highly selective semipermeable border of endothelial cells that prevents solutes in the circulating blood from ''non-selectively'' crossing into the extracellular fluid of the central nervous system where neu ...
is vulnerable – such as the choroid plexus
The choroid plexus, or plica choroidea, is a plexus of cells that arises from the tela choroidea in each of the ventricles of the brain. Regions of the choroid plexus produce and secrete most of the cerebrospinal fluid (CSF) of the central nervo ...
. Meningitis occurs in 25% of newborns with bloodstream infections due to group B streptococci; this phenomenon is much less common in adults. Direct contamination of the cerebrospinal fluid may arise from indwelling devices, skull fractures, or infections of the nasopharynx or the nasal sinuses that have formed a tract with the subarachnoid space (see above); occasionally, congenital defects of the dura mater can be identified.
The large-scale inflammation that occurs in the subarachnoid space during meningitis is not a direct result of bacterial infection but can rather largely be attributed to the response of the immune system to the entry of bacteria into the central nervous system
The central nervous system (CNS) is the part of the nervous system consisting primarily of the brain and spinal cord. The CNS is so named because the brain integrates the received information and coordinates and influences the activity of all par ...
. When components of the bacterial cell membrane are identified by the immune cells of the brain (astrocyte
Astrocytes (from Ancient Greek , , "star" + , , "cavity", "cell"), also known collectively as astroglia, are characteristic star-shaped glial cells in the brain and spinal cord. They perform many functions, including biochemical control of endo ...
s and microglia
Microglia are a type of neuroglia (glial cell) located throughout the brain and spinal cord. Microglia account for about 7% of cells found within the brain. As the resident macrophage cells, they act as the first and main form of active immune de ...
), they respond by releasing large amounts of cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autoc ...
s, hormone-like mediators that recruit other immune cells and stimulate other tissues to participate in an immune response. The blood–brain barrier becomes more permeable, leading to "vasogenic" cerebral edema (swelling of the brain due to fluid leakage from blood vessels). Large numbers of white blood cells enter the CSF, causing inflammation of the meninges and leading to "interstitial" edema (swelling due to fluid between the cells). In addition, the walls of the blood vessels themselves become inflamed (cerebral vasculitis), which leads to decreased blood flow and a third type of edema, "cytotoxic" edema. The three forms of cerebral edema all lead to increased intracranial pressure
Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury ( mmHg) and at rest, is normally 7–15 mmHg for a supine adult. ...
; together with the lowered blood pressure often encountered in sepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is follo ...
, this means that it is harder for blood to enter the brain; consequently brain cell
Brain cells make up the functional tissue of the brain. The rest of the brain tissue is structural or connective called the stroma which includes blood vessels. The two main types of cells in the brain are neurons, also known as nerve cells, an ...
s are deprived of oxygen and undergo apoptosis
Apoptosis (from grc, ἀπόπτωσις, apóptōsis, 'falling off') is a form of programmed cell death that occurs in multicellular organisms. Biochemical events lead to characteristic cell changes (morphology) and death. These changes includ ...
(programmed cell death
Programmed cell death (PCD; sometimes referred to as cellular suicide) is the death of a cell (biology), cell as a result of events inside of a cell, such as apoptosis or autophagy. PCD is carried out in a biological process, which usually confers ...
).
It is recognized that administration of antibiotics may initially worsen the process outlined above, by increasing the amount of bacterial cell membrane products released through the destruction of bacteria. Particular treatments, such as the use of corticosteroids
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involv ...
, are aimed at dampening the immune system's response to this phenomenon.
Diagnosis
Diagnosing meningitis as promptly as possible can improve outcomes. There is no specific sign or symptom that can diagnose meningitis and a lumbar puncture (spinal tap) to examine the cerebrospinal fluid is recommended for diagnosis. Lumbar puncture is contraindicated if there is a mass in the brain (tumor or abscess) or theintracranial pressure
Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury ( mmHg) and at rest, is normally 7–15 mmHg for a supine adult. ...
(ICP) is elevated, as it may lead to brain herniation
Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the t ...
. If someone is at risk for either a mass or raised ICP (recent head injury, a known immune system problem, localizing neurological signs, or evidence on examination of a raised ICP), a CT or MRI
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves ...
scan is recommended prior to the lumbar puncture. – formal guideline at This applies in 45% of all adult cases.
There are no physical tests that can rule out or determine if a person has meningitis. The jolt accentuation test is not specific or sensitive enough to completely rule out meningitis.
If someone is suspected of having meningitis, blood test
A blood test is a laboratory analysis performed on a blood sample that is usually extracted from a vein in the arm using a hypodermic needle, or via fingerprick. Multiple tests for specific blood components, such as a glucose test or a choleste ...
s are performed for markers of inflammation (e.g. C-reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin-6 ...
, complete blood count
A complete blood count (CBC), also known as a full blood count (FBC), is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and pla ...
), as well as blood cultures. If a CT or MRI is required before LP, or if LP proves difficult, professional guidelines suggest that antibiotics should be administered first to prevent delay in treatment, especially if this may be longer than 30 minutes. Often, CT or MRI scans are performed at a later stage to assess for complications of meningitis.
In severe forms of meningitis, monitoring of blood electrolytes may be important; for example, hyponatremia is common in bacterial meningitis. The cause of hyponatremia, however, is controversial and may include dehydration, the inappropriate secretion of the antidiuretic hormone
Human vasopressin, also called antidiuretic hormone (ADH), arginine vasopressin (AVP) or argipressin, is a hormone synthesized from the AVP gene as a peptide prohormone in neurons in the hypothalamus, and is converted to AVP. It then travel ...
(SIADH), or overly aggressive intravenous fluid administration.
Lumbar puncture

 A lumbar puncture is done by positioning the person, usually lying on the side, applying
A lumbar puncture is done by positioning the person, usually lying on the side, applying local anesthetic
A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general a ...
, and inserting a needle into the dural sac
Dural is a suburb of Sydney, in the state of New South Wales, Australia 36 kilometres north-west of the Sydney central business district in the local government areas of Hornsby Shire and The Hills Shire. Dural is part of the Hills District. ...
(a sac around the spinal cord) to collect cerebrospinal fluid (CSF). When this has been achieved, the "opening pressure" of the CSF is measured using a manometer. The pressure is normally between 6 and 18 cm water (cmH2O); in bacterial meningitis the pressure is usually elevated. In cryptococcal meningitis
Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When th ...
, intracranial pressure is markedly elevated. The initial appearance of the fluid may prove an indication of the nature of the infection: cloudy CSF indicates higher levels of protein, white and red blood cells and/or bacteria, and therefore may suggest bacterial meningitis.
The CSF sample is examined for presence and types of white blood cells, red blood cells, protein content and glucose level. Gram staining of the sample may demonstrate bacteria in bacterial meningitis, but absence of bacteria does not exclude bacterial meningitis as they are only seen in 60% of cases; this figure is reduced by a further 20% if antibiotics were administered before the sample was taken. Gram staining is also less reliable in particular infections such as listeriosis
Listeriosis is a bacterial infection most commonly caused by ''Listeria monocytogenes'', although '' L. ivanovii'' and '' L. grayi'' have been reported in certain cases. Listeriosis can cause severe illness, including severe sepsis, meni ...
. Microbiological culture of the sample is more sensitive (it identifies the organism in 70–85% of cases) but results can take up to 48 hours to become available. The type of white blood cell predominantly present (see table) indicates whether meningitis is bacterial (usually neutrophil-predominant) or viral (usually lymphocyte-predominant), although at the beginning of the disease this is not always a reliable indicator. Less commonly, eosinophils predominate, suggesting parasitic or fungal etiology, among others.
The concentration of glucose in CSF is normally above 40% of that in blood. In bacterial meningitis it is typically lower; the CSF glucose level is therefore divided by the Blood sugar, blood glucose (CSF glucose to serum glucose ratio). A ratio ≤0.4 is indicative of bacterial meningitis; in the newborn, glucose levels in CSF are normally higher, and a ratio below 0.6 (60%) is therefore considered abnormal. High levels of lactic acid, lactate in CSF indicate a higher likelihood of bacterial meningitis, as does a higher white blood cell count. If lactate levels are less than 35 mg/dl and the person has not previously received antibiotics then this may rule out bacterial meningitis.
Various other specialized tests may be used to distinguish between different types of meningitis. A latex agglutination test may be positive in meningitis caused by '' Streptococcus pneumoniae'', '' Neisseria meningitidis'', ''Haemophilus influenzae'', ''Escherichia coli
''Escherichia coli'' (),Wells, J. C. (2000) Longman Pronunciation Dictionary. Harlow ngland Pearson Education Ltd. also known as ''E. coli'' (), is a Gram-negative, facultative anaerobic, rod-shaped, coliform bacterium of the genus '' Esc ...
'' and ''Streptococcus agalactiae, group B streptococci''; its routine use is not encouraged as it rarely leads to changes in treatment, but it may be used if other tests are not diagnostic. Similarly, the Limulus amebocyte lysate, limulus lysate test may be positive in meningitis caused by Gram-negative bacteria, but it is of limited use unless other tests have been unhelpful. Polymerase chain reaction (PCR) is a technique used to amplify small traces of bacterial DNA in order to detect the presence of bacterial or viral DNA in cerebrospinal fluid; it is a highly sensitive and specific test since only trace amounts of the infecting agent's DNA is required. It may identify bacteria in bacterial meningitis and may assist in distinguishing the various causes of viral meningitis (enterovirus
''Enterovirus'' is a genus of positive-sense single-stranded RNA viruses associated with several human and mammalian diseases. Enteroviruses are named by their transmission-route through the intestine ('enteric' meaning intestinal).
Serologic ...
, herpes simplex virus, herpes simplex virus 2 and mumps in those not vaccinated for this). Serology (identification of antibodies to viruses) may be useful in viral meningitis. If tuberculous meningitis is suspected, the sample is processed for Ziehl–Neelsen stain, which has a low sensitivity, and tuberculosis culture, which takes a long time to process; PCR is being used increasingly. Diagnosis of cryptococcal meningitis can be made at low cost using an India ink stain of the CSF; however, testing for cryptococcal antigen in blood or CSF is more sensitive.
A diagnostic and therapeutic difficulty is "partially treated meningitis", where there are meningitis symptoms after receiving antibiotics (such as for presumptive sinusitis
Sinusitis, also known as rhinosinusitis, is inflammation of the mucous membranes that line the sinuses resulting in symptoms that may include thick nasal mucus, a plugged nose, and facial pain. Other signs and symptoms may include fever, hea ...
). When this happens, CSF findings may resemble those of viral meningitis, but antibiotic treatment may need to be continued until there is definitive positive evidence of a viral cause (e.g. a positive enterovirus PCR).
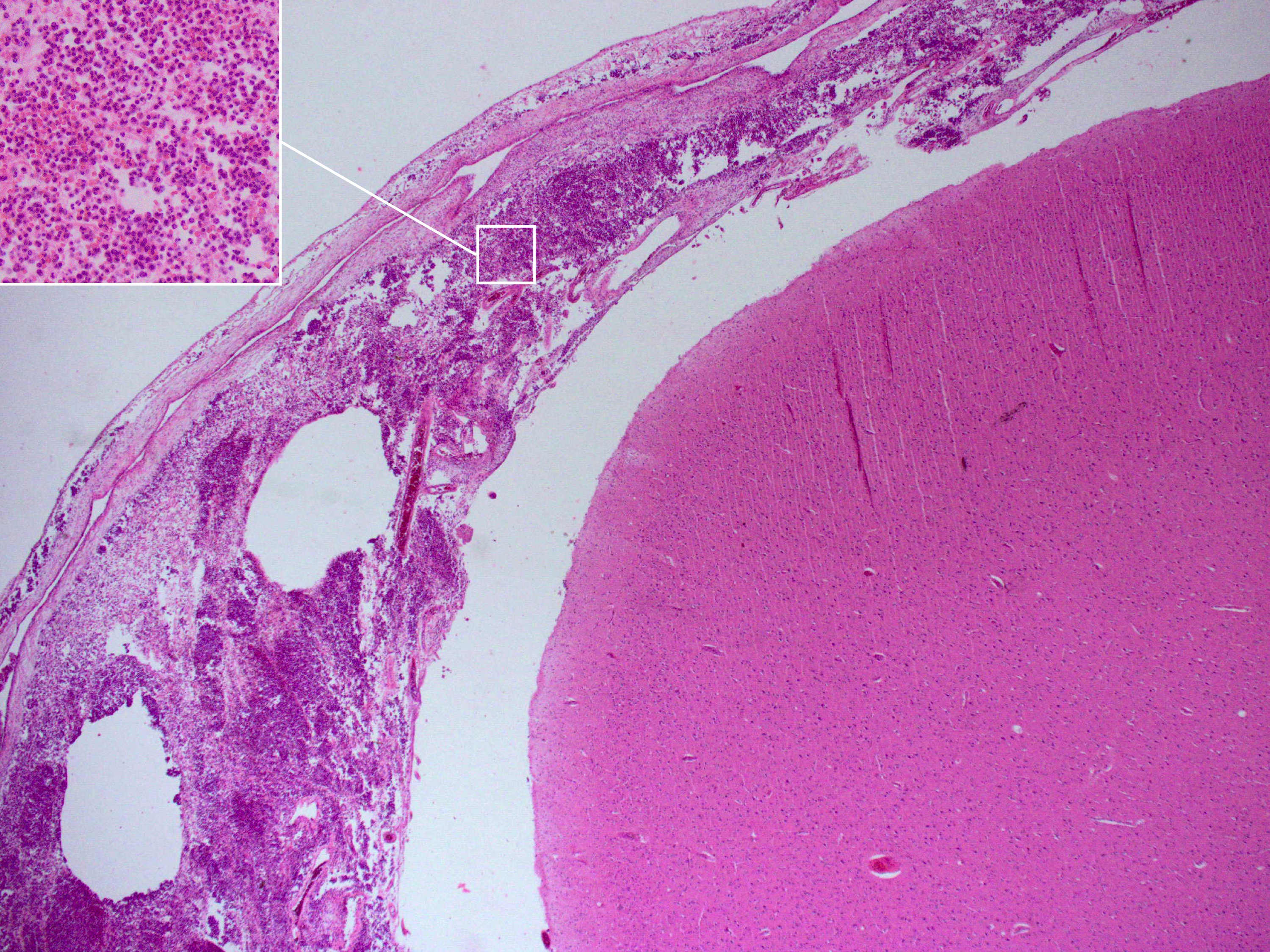
Postmortem
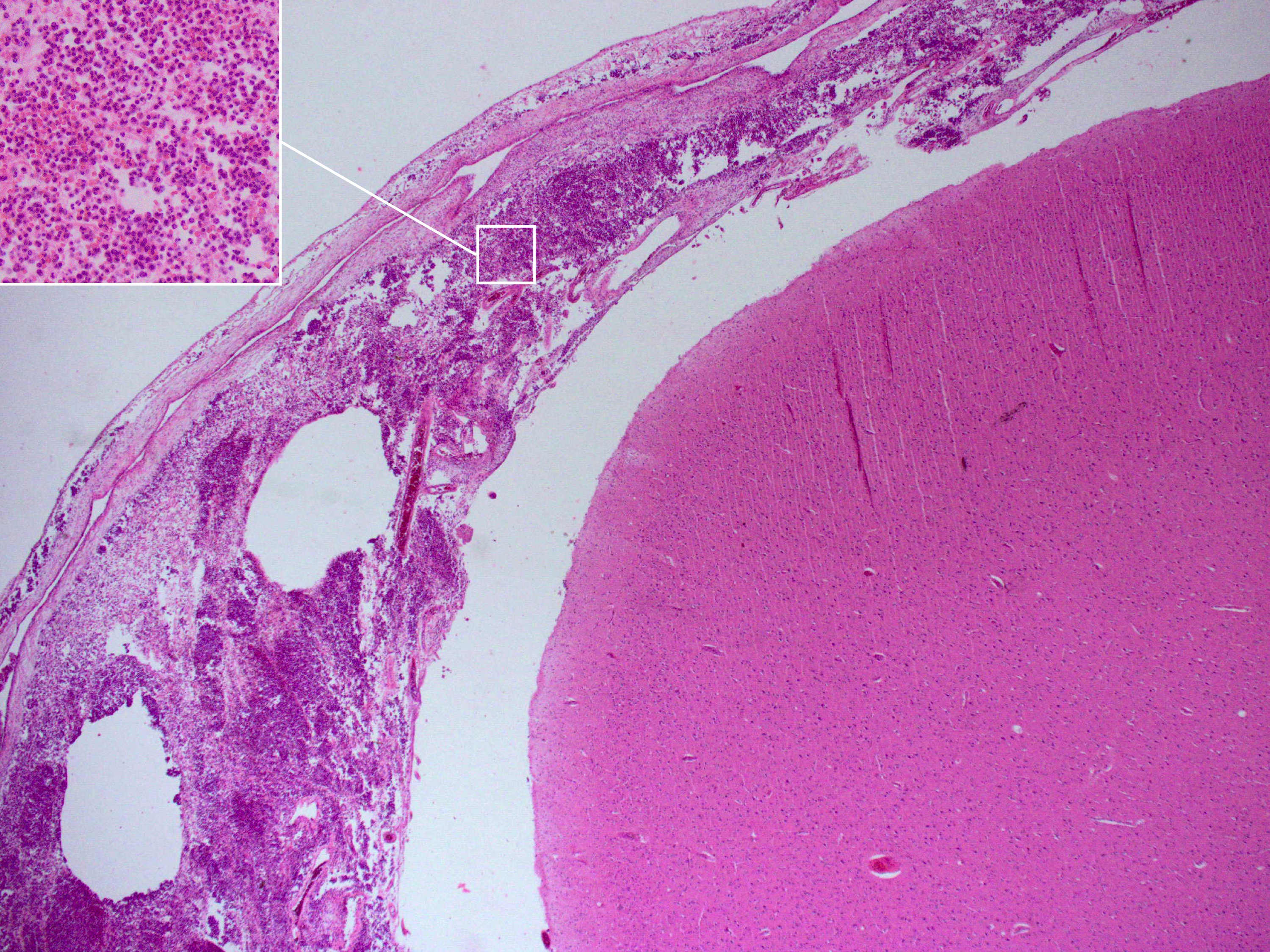 Meningitis can be diagnosed after death has occurred. The findings from a post mortem are usually a widespread inflammation of the
Meningitis can be diagnosed after death has occurred. The findings from a post mortem are usually a widespread inflammation of the pia mater
Pia mater ( or ),Entry "pia mater"
in
spinal cord, may be surrounded with pus – as may the meningeal vessels.
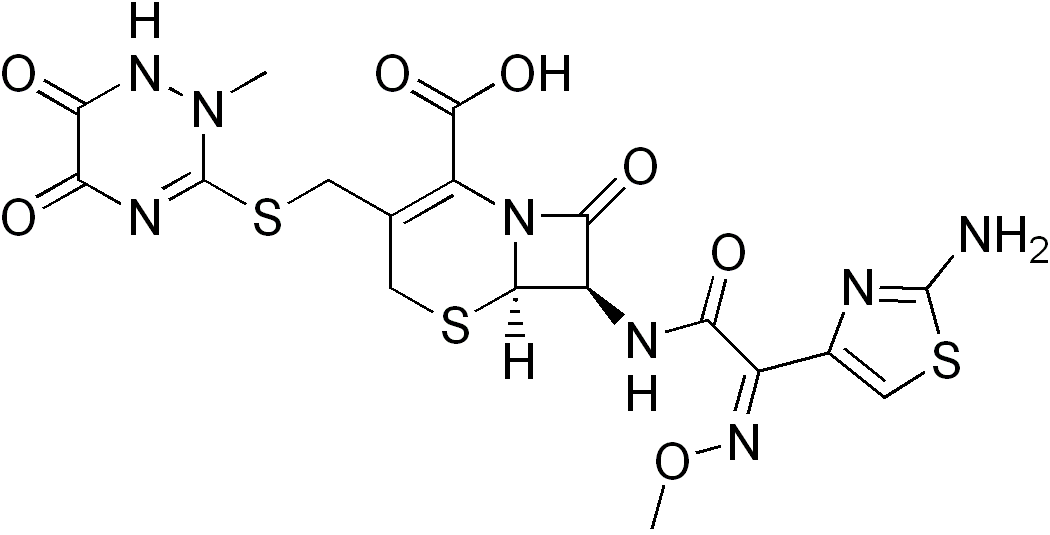 Empiric antibiotics (treatment without exact diagnosis) should be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place and population. For instance, in the United Kingdom, empirical treatment consists of a third-generation cefalosporin such as cefotaxime or ceftriaxone. In the US, where resistance to cefalosporins is increasingly found in streptococci, addition of vancomycin to the initial treatment is recommended. Chloramphenicol, either alone or in combination with ampicillin, however, appears to work equally well.
Empirical therapy may be chosen on the basis of the person's age, whether the infection was preceded by a head injury, whether the person has undergone recent neurosurgery and whether or not a cerebral shunt is present. In young children and those over 50 years of age, as well as those who are immunocompromised, the addition of ampicillin is recommended to cover '' Listeria monocytogenes''. Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens. The results of the CSF microbiological culture, culture generally take longer to become available (24–48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics. For an antibiotic to be effective in meningitis it must not only be active against the pathogenic bacterium but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis. Most of the antibiotics used in meningitis have not been tested directly on people with meningitis in clinical trials. Rather, the relevant knowledge has mostly derived from laboratory studies in rabbits. Tuberculous meningitis requires prolonged treatment with antibiotics. While tuberculosis of the lungs is typically treated for six months, those with tuberculous meningitis are typically treated for a year or longer.
Empiric antibiotics (treatment without exact diagnosis) should be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place and population. For instance, in the United Kingdom, empirical treatment consists of a third-generation cefalosporin such as cefotaxime or ceftriaxone. In the US, where resistance to cefalosporins is increasingly found in streptococci, addition of vancomycin to the initial treatment is recommended. Chloramphenicol, either alone or in combination with ampicillin, however, appears to work equally well.
Empirical therapy may be chosen on the basis of the person's age, whether the infection was preceded by a head injury, whether the person has undergone recent neurosurgery and whether or not a cerebral shunt is present. In young children and those over 50 years of age, as well as those who are immunocompromised, the addition of ampicillin is recommended to cover '' Listeria monocytogenes''. Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens. The results of the CSF microbiological culture, culture generally take longer to become available (24–48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics. For an antibiotic to be effective in meningitis it must not only be active against the pathogenic bacterium but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis. Most of the antibiotics used in meningitis have not been tested directly on people with meningitis in clinical trials. Rather, the relevant knowledge has mostly derived from laboratory studies in rabbits. Tuberculous meningitis requires prolonged treatment with antibiotics. While tuberculosis of the lungs is typically treated for six months, those with tuberculous meningitis are typically treated for a year or longer.
 Untreated, bacterial meningitis is almost always fatal. Viral meningitis, in contrast, tends to resolve spontaneously and is rarely fatal. With treatment, Mortality rate, mortality (risk of death) from bacterial meningitis depends on the age of the person and the underlying cause. Of newborns, 20–30% may die from an episode of bacterial meningitis. This risk is much lower in older children, whose mortality is about 2%, but rises again to about 19–37% in adults.
Risk of death is predicted by various factors apart from age, such as the pathogen and the time it takes for the pathogen to be cleared from the cerebrospinal fluid, the severity of the generalized illness, a decreased level of consciousness or an abnormally low count of white blood cells in the CSF. Meningitis caused by ''H. influenzae'' and meningococci has a better prognosis than cases caused by group B streptococci, coliforms and ''S. pneumoniae''. In adults, too, meningococcal meningitis has a lower mortality (3–7%) than pneumococcal disease.
In children there are several potential disabilities which may result from damage to the nervous system, including sensorineural hearing loss, epilepsy, Learning disability, learning and behavioral difficulties, as well as Intellectual disability, decreased intelligence. These occur in about 15% of survivors. Some of the hearing loss may be reversible. In adults, 66% of all cases emerge without disability. The main problems are
Untreated, bacterial meningitis is almost always fatal. Viral meningitis, in contrast, tends to resolve spontaneously and is rarely fatal. With treatment, Mortality rate, mortality (risk of death) from bacterial meningitis depends on the age of the person and the underlying cause. Of newborns, 20–30% may die from an episode of bacterial meningitis. This risk is much lower in older children, whose mortality is about 2%, but rises again to about 19–37% in adults.
Risk of death is predicted by various factors apart from age, such as the pathogen and the time it takes for the pathogen to be cleared from the cerebrospinal fluid, the severity of the generalized illness, a decreased level of consciousness or an abnormally low count of white blood cells in the CSF. Meningitis caused by ''H. influenzae'' and meningococci has a better prognosis than cases caused by group B streptococci, coliforms and ''S. pneumoniae''. In adults, too, meningococcal meningitis has a lower mortality (3–7%) than pneumococcal disease.
In children there are several potential disabilities which may result from damage to the nervous system, including sensorineural hearing loss, epilepsy, Learning disability, learning and behavioral difficulties, as well as Intellectual disability, decreased intelligence. These occur in about 15% of survivors. Some of the hearing loss may be reversible. In adults, 66% of all cases emerge without disability. The main problems are

 Although meningitis is a notifiable disease in many countries, the exact incidence (epidemiology), incidence rate is unknown. In 2013 meningitis resulted in 303,000 deaths – down from 464,000 deaths in 1990. In 2010 it was estimated that meningitis resulted in 420,000 deaths, excluding
Although meningitis is a notifiable disease in many countries, the exact incidence (epidemiology), incidence rate is unknown. In 2013 meningitis resulted in 303,000 deaths – down from 464,000 deaths in 1990. In 2010 it was estimated that meningitis resulted in 420,000 deaths, excluding
Meningitis
Centers for Disease Control and Prevention (CDC) {{Authority control Meningitis, Disorders causing seizures Medical emergencies Acute pain Wikipedia medicine articles ready to translate (full) Medical triads Wikipedia infectious disease articles ready to translate
in
spinal cord, may be surrounded with pus – as may the meningeal vessels.
Prevention
For some causes of meningitis, protection can be provided in the long term through vaccination, or in the short term withantibiotic
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention ...
s. Some behavioral measures may also be effective.
Behavioral
Bacterial and viral meningitis are contagious, but neither is as contagious as the common cold or flu. Both can be transmitted through droplets of respiratory secretions during close contact such as kissing, sneezing or coughing on someone, but bacterial meningitis cannot be spread by only breathing the air where a person with meningitis has been. Viral meningitis is typically caused by enteroviruses, and is most commonly spread through fecal contamination. The risk of infection can be decreased by changing the behavior that led to transmission.Vaccination
Since the 1980s, many countries have included Hib vaccine, immunization against ''Haemophilus influenzae'' type B in their routine childhood vaccination schemes. This has practically Eradication of infectious diseases, eliminated this pathogen as a cause of meningitis in young children in those countries. In the countries in which the disease burden is highest, however, the vaccine is still too expensive. Similarly, immunization against mumps has led to a sharp fall in the number of cases of mumps meningitis, which prior to vaccination occurred in 15% of all cases of mumps. Meningococcal vaccine, Meningococcus vaccines exist against groups A, B, C, W135 and Y. In countries where the vaccine for meningococcus group C was introduced, cases caused by this pathogen have decreased substantially. A quadrivalent vaccine now exists, which combines four vaccines with the exception of B; immunization with this ACW135Y vaccine is now a visa requirement for taking part in Hajj. Development of a vaccine against group B meningococci has proved much more difficult, as its surface proteins (which would normally be used to make a vaccine) only elicit a weak Immunogenicity, response from the immune system, or cross-react with normal human proteins. Still, some countries (New Zealand, Cuba, Norway and Chile) have developed vaccines against local strains of group B meningococci; some have shown good results and are used in local immunization schedules. Two new vaccines, both approved in 2014, are effective against a wider range of group B meningococci strains. In Africa, until recently, the approach for prevention and control of meningococcal epidemics was based on early detection of the disease and emergency reactive mass vaccination of the at-risk population with bivalent A/C or trivalent A/C/W135 polysaccharide vaccines, though the introduction of MenAfriVac (meningococcus group A vaccine) has demonstrated effectiveness in young people and has been described as a model for product development partnerships in resource-limited settings. Routine vaccination against ''Streptococcus pneumoniae'' with the pneumococcal conjugate vaccine (PCV), which is active against seven common serotypes of this pathogen, significantly reduces the incidence of pneumococcal meningitis. The pneumococcal polysaccharide vaccine, which covers 23 strains, is only administered to certain groups (e.g. those who have had a splenectomy, the surgical removal of the spleen); it does not elicit a significant immune response in all recipients, e.g. small children. Childhood vaccination with Bacillus Calmette-Guérin has been reported to significantly reduce the rate of tuberculous meningitis, but its waning effectiveness in adulthood has prompted a search for a better vaccine.Antibiotics
Short-term antibiotic prophylaxis is another method of prevention, particularly of meningococcal meningitis. In cases of meningococcal meningitis, preventative treatment in close contacts with antibiotics (e.g. rifampicin, ciprofloxacin or ceftriaxone) can reduce their risk of contracting the condition, but does not protect against future infections. Resistance to rifampicin has been noted to increase after use, which has caused some to recommend considering other agents. While antibiotics are frequently used in an attempt to prevent meningitis in those with a basilar skull fracture there is not enough evidence to determine whether this is beneficial or harmful. This applies to those with or without a CSF leak.Management
Meningitis is potentially life-threatening and has a high mortality rate if untreated; delay in treatment has been associated with a poorer outcome. Thus, treatment with wide-spectrum antibiotics should not be delayed while confirmatory tests are being conducted. If meningococcal disease is suspected in primary care, guidelines recommend that benzylpenicillin be administered before transfer to hospital. Intravenous fluid, Intravenous fluids should be administered if hypotension (low blood pressure) or shock (circulatory), shock are present. It is not clear whether intravenous fluid should be given routinely or whether this should be restricted. Given that meningitis can cause a number of early severe complications, regular medical review is recommended to identify these complications early and to admit the person to an intensive care unit if deemed necessary. Mechanical ventilation may be needed if the level of consciousness is very low, or if there is evidence of respiratory failure. If there are signs of raised intracranial pressure, measures to monitor the pressure may be taken; this would allow the optimization of the cerebral perfusion pressure and various treatments to decrease the intracranial pressure with medication (e.g. mannitol). Seizures are treated with anticonvulsants. Hydrocephalus (obstructed flow of CSF) may require insertion of a temporary or long-term drainage device, such as acerebral shunt
A cerebral shunt is a device permanently implanted inside the head and body to drain excess fluid away from the brain. They are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If ...
. The osmotic therapy, glycerol, has an unclear effect on mortality but may decrease hearing problems.
Bacterial meningitis
Antibiotics
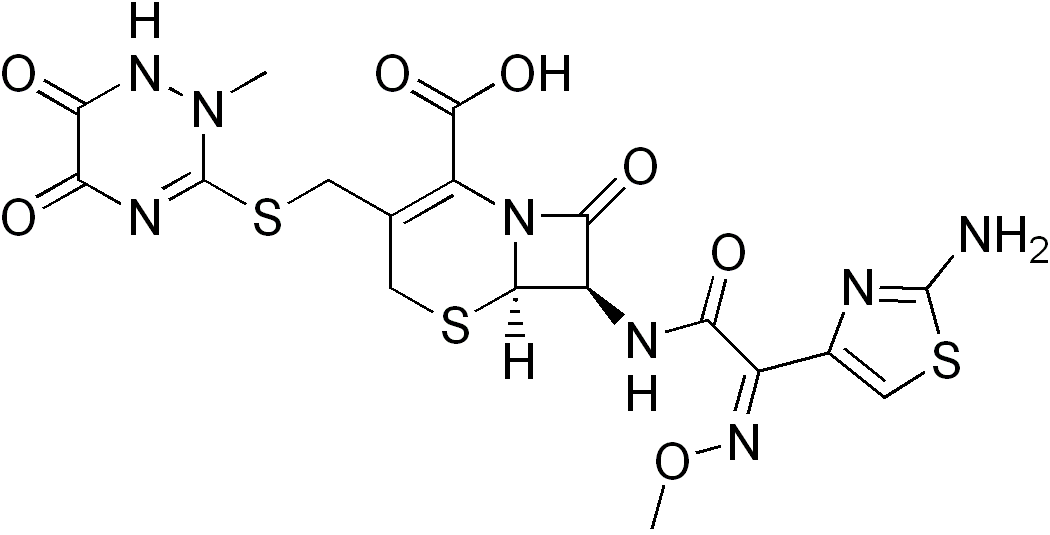 Empiric antibiotics (treatment without exact diagnosis) should be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place and population. For instance, in the United Kingdom, empirical treatment consists of a third-generation cefalosporin such as cefotaxime or ceftriaxone. In the US, where resistance to cefalosporins is increasingly found in streptococci, addition of vancomycin to the initial treatment is recommended. Chloramphenicol, either alone or in combination with ampicillin, however, appears to work equally well.
Empirical therapy may be chosen on the basis of the person's age, whether the infection was preceded by a head injury, whether the person has undergone recent neurosurgery and whether or not a cerebral shunt is present. In young children and those over 50 years of age, as well as those who are immunocompromised, the addition of ampicillin is recommended to cover '' Listeria monocytogenes''. Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens. The results of the CSF microbiological culture, culture generally take longer to become available (24–48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics. For an antibiotic to be effective in meningitis it must not only be active against the pathogenic bacterium but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis. Most of the antibiotics used in meningitis have not been tested directly on people with meningitis in clinical trials. Rather, the relevant knowledge has mostly derived from laboratory studies in rabbits. Tuberculous meningitis requires prolonged treatment with antibiotics. While tuberculosis of the lungs is typically treated for six months, those with tuberculous meningitis are typically treated for a year or longer.
Empiric antibiotics (treatment without exact diagnosis) should be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place and population. For instance, in the United Kingdom, empirical treatment consists of a third-generation cefalosporin such as cefotaxime or ceftriaxone. In the US, where resistance to cefalosporins is increasingly found in streptococci, addition of vancomycin to the initial treatment is recommended. Chloramphenicol, either alone or in combination with ampicillin, however, appears to work equally well.
Empirical therapy may be chosen on the basis of the person's age, whether the infection was preceded by a head injury, whether the person has undergone recent neurosurgery and whether or not a cerebral shunt is present. In young children and those over 50 years of age, as well as those who are immunocompromised, the addition of ampicillin is recommended to cover '' Listeria monocytogenes''. Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens. The results of the CSF microbiological culture, culture generally take longer to become available (24–48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics. For an antibiotic to be effective in meningitis it must not only be active against the pathogenic bacterium but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis. Most of the antibiotics used in meningitis have not been tested directly on people with meningitis in clinical trials. Rather, the relevant knowledge has mostly derived from laboratory studies in rabbits. Tuberculous meningitis requires prolonged treatment with antibiotics. While tuberculosis of the lungs is typically treated for six months, those with tuberculous meningitis are typically treated for a year or longer.
Fluid Therapy
Fluid given intravenously are an essential part of treatment of bacterial meningitis. There is no difference in terms of mortality or acute severe neurological complications in children given a maintenance regimen over restricted-fluid regimen, but evidence is in favor of the maintenance regimen in terms of emergence of chronic severe neurological complications.Steroids
Additional treatment with corticosteroids (usually dexamethasone) has shown some benefits, such as a reduction of hearing loss, and better short term neurological outcomes in adolescents and adults from World Bank high-income economy, high-income countries with low rates of HIV. Some research has found reduced rates of death while other research has not. They also appear to be beneficial in those with tuberculosis meningitis, at least in those who are HIV negative. Professional guidelines therefore recommend the commencement of dexamethasone or a similar corticosteroid just before the first dose of antibiotics is given, and continued for four days. Given that most of the benefit of the treatment is confined to those with pneumococcal meningitis, some guidelines suggest that dexamethasone be discontinued if another cause for meningitis is identified. The likely mechanism is suppression of overactive inflammation. Additional treatment with corticosteroids have a different role in children than in adults. Though the benefit of corticosteroids has been demonstrated in adults as well as in children from high-income countries, their use in children from Poverty, low-income countries is not supported by the evidence; the reason for this discrepancy is not clear. Even in high-income countries, the benefit of corticosteroids is only seen when they are given prior to the first dose of antibiotics, and is greatest in cases of ''H. influenzae'' meningitis, the incidence of which has decreased dramatically since the introduction of the Hib vaccine. Thus, corticosteroids are recommended in the treatment of pediatric meningitis if the cause is ''H. influenzae'', and only if given prior to the first dose of antibiotics; other uses are controversial.Viral meningitis
Viral meningitis typically only requires supportive therapy; most viruses responsible for causing meningitis are not amenable to specific treatment. Viral meningitis tends to run a more benign course than bacterial meningitis. Herpes simplex virus andvaricella zoster virus
Varicella-zoster virus (VZV), also known as human herpesvirus 3 (HHV-3, HHV3) or ''Human alphaherpesvirus 3'' ( taxonomically), is one of nine known herpes viruses that can infect humans. It causes chickenpox (varicella) commonly affecting chi ...
may respond to treatment with antiviral drugs such as aciclovir, but there are no clinical trials that have specifically addressed whether this treatment is effective. Mild cases of viral meningitis can be treated at home with conservative measures such as fluid, bedrest, and analgesics.
Fungal meningitis
Fungal meningitis, such ascryptococcal meningitis
Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When th ...
, is treated with long courses of high dose Antifungal drug, antifungals, such as amphotericin B and flucytosine. Raised intracranial pressure is common in fungal meningitis, and frequent (ideally daily) lumbar punctures to relieve the pressure are recommended, or alternatively a lumbar drain.
Prognosis
deafness
Deafness has varying definitions in cultural and medical contexts. In medical contexts, the meaning of deafness is hearing loss that precludes a person from understanding spoken language, an audiological condition. In this context it is written ...
(in 14%) and Developmental disability, cognitive impairment (in 10%).
Tuberculous meningitis in children continues to be associated with a significant risk of death even with treatment (19%), and a significant proportion of the surviving children have ongoing neurological problems. Just over a third of all cases survives with no problems.
Epidemiology

cryptococcal meningitis
Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When th ...
.
Bacterial meningitis occurs in about 3 people per 100,000 annually in Western world, Western countries. Population-wide studies have shown that viral meningitis is more common, at 10.9 per 100,000, and occurs more often in the summer. In Brazil, the rate of bacterial meningitis is higher, at 45.8 per 100,000 annually. Sub-Saharan Africa has been plagued by large epidemics of meningococcal meningitis for over a century, leading to it being labeled the "meningitis belt". Epidemics typically occur in the dry season (December to June), and an epidemic wave can last two to three years, dying out during the intervening rainy seasons. Attack rates of 100–800 cases per 100,000 are encountered in this area, which is poorly served by Health care, medical care. These cases are predominantly caused by meningococci. The largest epidemic ever recorded in history swept across the entire region in 1996–1997, causing over 250,000 cases and 25,000 deaths.
Meningococcal disease occurs in epidemics in areas where many people live together for the first time, such as army barracks during mobilization, university and college campuses and the annual Hajj pilgrimage. Although the pattern of epidemic cycles in Africa is not well understood, several factors have been associated with the development of epidemics in the meningitis belt. They include: medical conditions (immunological susceptibility of the population), demographic conditions (travel and large population displacements), socioeconomic conditions (overcrowding and poor living conditions), climatic conditions (drought and dust storms), and concurrent infections (acute respiratory infections).
There are significant differences in the local distribution of causes for bacterial meningitis. For instance, while ''N. meningitides'' groups B and C cause most disease episodes in Europe, group A is found in Asia and continues to predominate in Africa, where it causes most of the major epidemics in the meningitis belt, accounting for about 80% to 85% of documented meningococcal meningitis cases.
History
Some suggest that Hippocrates may have realized the existence of meningitis, and it seems that meningism was known to pre-Renaissance physicians such as Avicenna. The description of tuberculous meningitis, then called "dropsy in the brain", is often attributed to Edinburgh physician Robert Whytt, Sir Robert Whytt in a posthumous report that appeared in 1768, although the link with tuberculosis and its pathogen was not made until the next century. It appears that epidemic meningitis is a relatively recent phenomenon. The first recorded major outbreak occurred in Geneva in 1805. Several other epidemics in Europe and the United States were described shortly afterward, and the first report of an epidemic in Africa appeared in 1840. African epidemics became much more common in the 20th century, starting with a major epidemic sweeping Nigeria and Ghana in 1905–1908. The first report of bacterial infection underlying meningitis was by the Austrian bacteriologist Anton Weichselbaum, who in 1887 described the ''meningococcus''. Mortality from meningitis was very high (over 90%) in early reports. In 1906, antiserum was produced in horses; this was developed further by the American scientist Simon Flexner and markedly decreased mortality from meningococcal disease. In 1944, penicillin was first reported to be effective in meningitis. The introduction in the late 20th century of ''Haemophilus'' vaccines led to a marked fall in cases of meningitis associated with this pathogen, and in 2002, evidence emerged that treatment with steroids could improve the prognosis of bacterial meningitis. World Meningitis Day is observed on 24 April each year.References
External links
*Meningitis
Centers for Disease Control and Prevention (CDC) {{Authority control Meningitis, Disorders causing seizures Medical emergencies Acute pain Wikipedia medicine articles ready to translate (full) Medical triads Wikipedia infectious disease articles ready to translate