MRI on:
[Wikipedia]
[Google]
[Amazon]
Magnetic resonance imaging (MRI) is a
 In most medical applications,
In most medical applications,  MRI requires a magnetic field that is both strong and
MRI requires a magnetic field that is both strong and

 Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 ( spin-lattice; that is, magnetization in the same direction as the static magnetic field) and T2 ( spin-spin; transverse to the static magnetic field).
To create a T1-weighted image, magnetization is allowed to recover before measuring the MR signal by changing the
Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 ( spin-lattice; that is, magnetization in the same direction as the static magnetic field) and T2 ( spin-spin; transverse to the static magnetic field).
To create a T1-weighted image, magnetization is allowed to recover before measuring the MR signal by changing the
 MRI has a wide range of applications in
MRI has a wide range of applications in
 MRI is the investigative tool of choice for neurological cancers over CT, as it offers better visualization of the
MRI is the investigative tool of choice for neurological cancers over CT, as it offers better visualization of the
 Cardiac MRI is complementary to other imaging techniques, such as
Cardiac MRI is complementary to other imaging techniques, such as
 Magnetic resonance
Magnetic resonance
 An
An
A Guided Tour of MRI: An introduction for laypeople
National High Magnetic Field Laboratory
The Basics of MRI
''Underlying physics and technical aspects''.
from the Institute for Magnetic Resonance Safety, Education, and Research (IMRSER)
Royal Institution Lecture – MRI: A Window on the Human Body
* ttps://www.howequipmentworks.com/mri_basics/ How MRI works explained simply using diagrams
Real-time MRI videos: Biomedizinische NMR Forschungs GmbH
* Paul C. Lauterbur
Genesis of the MRI (Magnetic Resonance Imaging) notebook, September 1971
(all pages freely available for download in variety of formats from
digital.sciencehistory.org
{{DEFAULTSORT:Magnetic Resonance Imaging 1973 introductions American inventions Articles containing video clips Cryogenics Radiology Discovery and invention controversies 20th-century inventions Biomagnetics
medical imaging
Medical imaging is the technique and process of imaging the interior of a body for clinical analysis and medical intervention, as well as visual representation of the function of some organs or tissues (physiology). Medical imaging seeks to rev ...
technique used in radiology
Radiology ( ) is the medical discipline that uses medical imaging to diagnose diseases and guide their treatment, within the bodies of humans and other animals. It began with radiography (which is why its name has a root referring to radiat ...
to form pictures of the anatomy
Anatomy () is the branch of biology concerned with the study of the structure of organisms and their parts. Anatomy is a branch of natural science that deals with the structural organization of living things. It is an old science, having its ...
and the physiological
Physiology (; ) is the scientific study of functions and mechanisms in a living system. As a sub-discipline of biology, physiology focuses on how organisms, organ systems, individual organs, cells, and biomolecules carry out the chemical ...
processes of the body. MRI scanners use strong magnetic field
A magnetic field is a vector field that describes the magnetic influence on moving electric charges, electric currents, and magnetic materials. A moving charge in a magnetic field experiences a force perpendicular to its own velocity and to ...
s, magnetic field gradients, and radio wave
Radio waves are a type of electromagnetic radiation with the longest wavelengths in the electromagnetic spectrum, typically with frequencies of 300 gigahertz (GHz) and below. At 300 GHz, the corresponding wavelength is 1 mm (short ...
s to generate images of the organs in the body. MRI does not involve X-rays
An X-ray, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 Picometre, picometers to 10 Nanometre, nanometers, corresponding to frequency, ...
or the use of ionizing radiation
Ionizing radiation (or ionising radiation), including nuclear radiation, consists of subatomic particles or electromagnetic waves that have sufficient energy to ionize atoms or molecules by detaching electrons from them. Some particles can travel ...
, which distinguishes it from CT and PET scan
Positron emission tomography (PET) is a functional imaging technique that uses radioactive substances known as radiotracers to visualize and measure changes in metabolic processes, and in other physiological activities including blood flow, r ...
s. MRI is a medical application of nuclear magnetic resonance
Nuclear magnetic resonance (NMR) is a physical phenomenon in which nuclei in a strong constant magnetic field are perturbed by a weak oscillating magnetic field (in the near field) and respond by producing an electromagnetic signal with a ...
(NMR) which can also be used for imaging in other NMR applications, such as NMR spectroscopy
Nuclear magnetic resonance spectroscopy, most commonly known as NMR spectroscopy or magnetic resonance spectroscopy (MRS), is a spectroscopic technique to observe local magnetic fields around atomic nuclei. The sample is placed in a magnetic fiel ...
.
MRI is widely used in hospitals and clinics for medical diagnosis
Medical diagnosis (abbreviated Dx, Dx, or Ds) is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. The information re ...
, staging
Staging may refer to:
Computing
* Staging (cloud computing), a process used to assemble, test, and review a new solution before it is moved into production and the existing solution is decommissioned
* Staging (data), intermediately storing data ...
and follow-up of disease. Compared to CT, MRI provides better contrast in images of soft-tissues, e.g. in the brain
A brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. It is located in the head, usually close to the sensory organs for senses such as vision. It is the most complex organ in a v ...
or abdomen. However, it may be perceived as less comfortable by patients, due to the usually longer and louder measurements with the subject in a long, confining tube, though "Open" MRI designs mostly relieve this. Additionally, implants and other non-removable metal in the body can pose a risk and may exclude some patients from undergoing an MRI examination safely.
MRI was originally called NMRI (nuclear magnetic resonance imaging), but "nuclear" was dropped to avoid negative associations. Certain atomic nuclei
The atomic nucleus is the small, dense region consisting of protons and neutrons at the center of an atom, discovered in 1911 by Ernest Rutherford based on the 1909 Geiger–Marsden gold foil experiment. After the discovery of the neutron ...
are able to absorb radio frequency
Radio frequency (RF) is the oscillation rate of an alternating electric current or voltage or of a magnetic, electric or electromagnetic field or mechanical system in the frequency range from around to around . This is roughly between the upp ...
energy when placed in an external magnetic field
A magnetic field is a vector field that describes the magnetic influence on moving electric charges, electric currents, and magnetic materials. A moving charge in a magnetic field experiences a force perpendicular to its own velocity and to ...
; the resultant evolving spin polarization
Spin polarization is the degree to which the spin, i.e., the intrinsic angular momentum of elementary particles, is aligned with a given direction. This property may pertain to the spin, hence to the magnetic moment, of conduction electrons in fe ...
can induce a RF signal in a radio frequency coil and thereby be detected. In clinical and research MRI, hydrogen atoms
A hydrogen atom is an atom of the chemical element hydrogen. The Electric charge, electrically neutral atom contains a single positively charged proton and a single negatively charged electron bound to the nucleus by the Coulomb force. Atomic ...
are most often used to generate a macroscopic polarization that is detected by antennas close to the subject being examined. Hydrogen atoms are naturally abundant in humans and other biological organisms, particularly in water
Water (chemical formula ) is an inorganic, transparent, tasteless, odorless, and nearly colorless chemical substance, which is the main constituent of Earth's hydrosphere and the fluids of all known living organisms (in which it acts as a ...
and fat
In nutrition science, nutrition, biology, and chemistry, fat usually means any ester of fatty acids, or a mixture of such chemical compound, compounds, most commonly those that occur in living beings or in food.
The term often refers spec ...
. For this reason, most MRI scans essentially map the location of water and fat in the body. Pulses of radio waves excite the nuclear spin
In atomic physics, the spin quantum number is a quantum number (designated ) which describes the intrinsic angular momentum (or spin angular momentum, or simply spin) of an electron or other particle. The phrase was originally used to describe th ...
energy transition, and magnetic field gradients localize the polarization in space. By varying the parameters of the pulse sequence
In Fourier transform NMR spectroscopy and imaging, a pulse sequence describes a series of radio frequency pulses applied to the sample, such that the free induction decay is related to the characteristic frequencies of the desired signals. After ...
, different contrasts may be generated between tissues based on the relaxation properties of the hydrogen atoms therein.
Since its development in the 1970s and 1980s, MRI has proven to be a versatile imaging technique. While MRI is most prominently used in diagnostic medicine
Medical diagnosis (abbreviated Dx, Dx, or Ds) is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. The information re ...
and biomedical research, it also may be used to form images of non-living objects, such as mummies
A mummy is a dead human or an animal whose soft tissues and organs have been preserved by either intentional or accidental exposure to chemicals, extreme cold, very low humidity, or lack of air, so that the recovered body does not decay furth ...
. Diffusion MRI
Diffusion-weighted magnetic resonance imaging (DWI or DW-MRI) is the use of specific MRI sequences as well as software that generates images from the resulting data that uses the diffusion of water molecules to generate contrast in MR images. It ...
and functional MRI
Functional magnetic resonance imaging or functional MRI (fMRI) measures brain activity by detecting changes associated with blood flow. This technique relies on the fact that cerebral blood flow and neuronal activation are coupled. When an area o ...
extend the utility of MRI to capture neuronal tracts and blood flow respectively in the nervous system, in addition to detailed spatial images. The sustained increase in demand for MRI within health system
Health, according to the World Health Organization, is "a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity".World Health Organization. (2006)''Constitution of the World Health Organiza ...
s has led to concerns about cost effectiveness
Cost-effectiveness analysis (CEA) is a form of economic analysis that compares the relative costs and outcomes (effects) of different courses of action. Cost-effectiveness analysis is distinct from cost–benefit analysis, which assigns a monetar ...
and overdiagnosis
Overdiagnosis is the diagnosis of disease that will never cause symptoms or death during a patient's ordinarily expected lifetime and thus presents no practical threat regardless of being pathologic. Overdiagnosis is a side effect of screening fo ...
.
Mechanism
Construction and physics
hydrogen
Hydrogen is the chemical element with the symbol H and atomic number 1. Hydrogen is the lightest element. At standard conditions hydrogen is a gas of diatomic molecules having the formula . It is colorless, odorless, tasteless, non-toxic, an ...
nuclei, which consist solely of a proton
A proton is a stable subatomic particle, symbol , H+, or 1H+ with a positive electric charge of +1 ''e'' elementary charge. Its mass is slightly less than that of a neutron and 1,836 times the mass of an electron (the proton–electron mass ...
, that are in tissues create a signal that is processed to form an image of the body in terms of the density of those nuclei in a specific region. Given that the protons are affected by fields from other atoms to which they are bonded, it is possible to separate responses from hydrogen in specific compounds.
To perform a study, the person is positioned within an MRI scanner
The physics of magnetic resonance imaging (MRI) concerns fundamental physical considerations of MRI techniques and technological aspects of MRI devices. MRI is a medical imaging technique mostly used in radiology and nuclear medicine in order t ...
that forms a strong magnetic field
A magnetic field is a vector field that describes the magnetic influence on moving electric charges, electric currents, and magnetic materials. A moving charge in a magnetic field experiences a force perpendicular to its own velocity and to ...
around the area to be imaged. First, energy from an oscillating
Oscillation is the repetitive or periodic variation, typically in time, of some measure about a central value (often a point of equilibrium) or between two or more different states. Familiar examples of oscillation include a swinging pendulum ...
magnetic field is temporarily applied to the patient at the appropriate resonance
Resonance describes the phenomenon of increased amplitude that occurs when the frequency of an applied periodic force (or a Fourier component of it) is equal or close to a natural frequency of the system on which it acts. When an oscillatin ...
frequency. Scanning with X and Y gradient coils causes a selected region of the patient to experience the exact magnetic field required for the energy to be absorbed. The atoms are excited by a radio frequency
Radio frequency (RF) is the oscillation rate of an alternating electric current or voltage or of a magnetic, electric or electromagnetic field or mechanical system in the frequency range from around to around . This is roughly between the upp ...
(RF) pulse and the resultant signal is measured by a receiving coil. The RF signal may be processed to deduce position information by looking at the changes in RF level and phase caused by varying the local magnetic field using gradient coils. As these coils are rapidly switched during the excitation and response to perform a moving line scan, they create the characteristic repetitive noise of an MRI scan as the windings move slightly due to magnetostriction
Magnetostriction (cf. electrostriction) is a property of magnetic materials that causes them to change their shape or dimensions during the process of magnetization. The variation of materials' magnetization due to the applied magnetic field change ...
. The contrast between different tissues is determined by the rate at which excited atoms return to the equilibrium state
Thermodynamic equilibrium is an axiomatic concept of thermodynamics. It is an internal state of a single thermodynamic system, or a relation between several thermodynamic systems connected by more or less permeable or impermeable walls. In thermod ...
. Exogenous
In a variety of contexts, exogeny or exogeneity () is the fact of an action or object originating externally. It contrasts with endogeneity or endogeny, the fact of being influenced within a system.
Economics
In an economic model, an exogeno ...
contrast agent
A contrast agent (or contrast medium) is a substance used to increase the contrast of structures or fluids within the body in medical imaging. Contrast agents absorb or alter external electromagnetism or ultrasound, which is different from radiop ...
s may be given to the person to make the image clearer.
The major components of an MRI scanner are the main magnet
A magnet is a material or object that produces a magnetic field. This magnetic field is invisible but is responsible for the most notable property of a magnet: a force that pulls on other ferromagnetic materials, such as iron, steel, nickel, ...
, which polarizes the sample, the shim coils for correcting shifts in the homogeneity
Homogeneity and heterogeneity are concepts often used in the sciences and statistics relating to the uniformity of a substance or organism. A material or image that is homogeneous is uniform in composition or character (i.e. color, shape, siz ...
of the main magnetic field, the gradient system which is used to localize the region to be scanned and the RF system, which excites the sample and detects the resulting NMR signal. The whole system is controlled by one or more computers.
 MRI requires a magnetic field that is both strong and
MRI requires a magnetic field that is both strong and uniform
A uniform is a variety of clothing worn by members of an organization while participating in that organization's activity. Modern uniforms are most often worn by armed forces and paramilitary organizations such as police, emergency services, se ...
to a few parts per million across the scan volume. The field strength of the magnet is measured in teslas – and while the majority of systems operate at 1.5 T, commercial systems are available between 0.2 and 7 T. Whole-body MRI systems for research application operate in e.g. 9.4T, 10.5T, 11.7T. Even higher field whole-body MRI systems e.g. 14 T and beyond are in conceptual proposal or in engineering design. Most clinical magnets are superconducting
Superconductivity is a set of physical properties observed in certain materials where Electrical resistance and conductance, electrical resistance vanishes and magnetic field, magnetic flux fields are expelled from the material. Any material e ...
magnets, which require liquid helium
Liquid helium is a physical state of helium at very low temperatures at standard atmospheric pressures. Liquid helium may show superfluidity.
At standard pressure, the chemical element helium exists in a liquid form only at the extremely low temp ...
to keep them at low temperatures. Lower field strengths can be achieved with permanent magnets, which are often used in "open" MRI scanners for claustrophobic
Claustrophobia is the fear of confined spaces. It can be triggered by many situations or stimuli, including elevators, especially when crowded to capacity, windowless rooms, and hotel rooms with closed doors and sealed windows. Even bedrooms with ...
patients. Lower field strengths are also used in a portable MRI scanner approved by the FDA in 2020. Recently, MRI has been demonstrated also at ultra-low fields, i.e., in the microtesla-to-millitesla range, where sufficient signal quality is made possible by prepolarization (on the order of 10–100 mT) and by measuring the Larmor precession
In physics, Larmor precession (named after Joseph Larmor) is the precession of the magnetic moment of an object about an external magnetic field. The phenomenon is conceptually similar to the precession of a tilted classical gyroscope in an extern ...
fields at about 100 microtesla with highly sensitive superconducting quantum interference devices (SQUID
True squid are molluscs with an elongated soft body, large eyes, eight arms, and two tentacles in the superorder Decapodiformes, though many other molluscs within the broader Neocoleoidea are also called squid despite not strictly fitting t ...
s).
T1 and T2

 Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 ( spin-lattice; that is, magnetization in the same direction as the static magnetic field) and T2 ( spin-spin; transverse to the static magnetic field).
To create a T1-weighted image, magnetization is allowed to recover before measuring the MR signal by changing the
Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 ( spin-lattice; that is, magnetization in the same direction as the static magnetic field) and T2 ( spin-spin; transverse to the static magnetic field).
To create a T1-weighted image, magnetization is allowed to recover before measuring the MR signal by changing the repetition time
The physics of magnetic resonance imaging (MRI) concerns fundamental Physics, physical considerations of Magnetic resonance imaging, MRI techniques and technological aspects of MRI devices. MRI is a medical imaging technique mostly used in radi ...
(TR). This image weighting is useful for assessing the cerebral cortex, identifying fatty tissue, characterizing focal liver lesions, and in general, obtaining morphological information, as well as for post-contrast imaging.
To create a T2-weighted image, magnetization is allowed to decay before measuring the MR signal by changing the echo time In magnetic resonance, a spin echo or Hahn echo is the refocusing of spin magnetisation by a pulse of resonant electromagnetic radiation. Modern nuclear magnetic resonance (NMR) and magnetic resonance imaging (MRI) make use of this effect.
The N ...
(TE). This image weighting is useful for detecting edema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's Tissue (biology), tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels t ...
and inflammation, revealing white matter lesions, and assessing zonal anatomy in the prostate
The prostate is both an Male accessory gland, accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found only in some mammals. It differs between species anatomically, ...
and uterus
The uterus (from Latin ''uterus'', plural ''uteri'') or womb () is the organ in the reproductive system of most female mammals, including humans that accommodates the embryonic and fetal development of one or more embryos until birth. The uter ...
.
The standard display of MRI images is to represent fluid characteristics in black and white
Black-and-white (B&W or B/W) images combine black and white in a continuous spectrum, producing a range of shades of grey.
Media
The history of various visual media began with black and white, and as technology improved, altered to color. ...
images, where different tissues turn out as follows:
= Diagnostics =
Usage by organ or system
 MRI has a wide range of applications in
MRI has a wide range of applications in medical diagnosis
Medical diagnosis (abbreviated Dx, Dx, or Ds) is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. The information re ...
and more than 25,000 scanners are estimated to be in use worldwide. MRI affects diagnosis and treatment in many specialties although the effect on improved health outcomes is disputed in certain cases.
MRI is the investigation of choice in the preoperative staging
Staging may refer to:
Computing
* Staging (cloud computing), a process used to assemble, test, and review a new solution before it is moved into production and the existing solution is decommissioned
* Staging (data), intermediately storing data ...
of rectal
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the sigmoid colon) at the le ...
and prostate cancer
Prostate cancer is cancer of the prostate. Prostate cancer is the second most common cancerous tumor worldwide and is the fifth leading cause of cancer-related mortality among men. The prostate is a gland in the male reproductive system that sur ...
and has a role in the diagnosis, staging, and follow-up of other tumors, as well as for determining areas of tissue for sampling in biobanking.
Neuroimaging
 MRI is the investigative tool of choice for neurological cancers over CT, as it offers better visualization of the
MRI is the investigative tool of choice for neurological cancers over CT, as it offers better visualization of the posterior cranial fossa
The posterior cranial fossa is part of the cranial cavity, located between the foramen magnum and tentorium cerebelli. It contains the brainstem and cerebellum.
This is the most inferior of the fossae. It houses the cerebellum, medulla and pons. ...
, containing the brainstem
The brainstem (or brain stem) is the posterior stalk-like part of the brain that connects the cerebrum with the spinal cord. In the human brain the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is cont ...
and the cerebellum
The cerebellum (Latin for "little brain") is a major feature of the hindbrain of all vertebrates. Although usually smaller than the cerebrum, in some animals such as the mormyrid fishes it may be as large as or even larger. In humans, the cerebel ...
. The contrast provided between grey
Grey (more common in British English) or gray (more common in American English) is an intermediate color between black and white. It is a neutral or achromatic color, meaning literally that it is "without color", because it can be composed o ...
and white matter
White matter refers to areas of the central nervous system (CNS) that are mainly made up of myelinated axons, also called tracts. Long thought to be passive tissue, white matter affects learning and brain functions, modulating the distribution ...
makes MRI the best choice for many conditions of the central nervous system
The central nervous system (CNS) is the part of the nervous system consisting primarily of the brain and spinal cord. The CNS is so named because the brain integrates the received information and coordinates and influences the activity of all par ...
, including demyelinating disease
A demyelinating disease is any disease of the nervous system in which the myelin sheath of neurons is damaged. This damage impairs the conduction of signals in the affected nerves. In turn, the reduction in conduction ability causes deficiency i ...
s, dementia
Dementia is a disorder which manifests as a set of related symptoms, which usually surfaces when the brain is damaged by injury or disease. The symptoms involve progressive impairments in memory, thinking, and behavior, which negatively affe ...
, cerebrovascular disease
Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The ...
, infectious diseases
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable dise ...
, Alzheimer's disease
Alzheimer's disease (AD) is a neurodegeneration, neurodegenerative disease that usually starts slowly and progressively worsens. It is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in short-term me ...
and epilepsy
Epilepsy is a group of non-communicable neurological disorders characterized by recurrent epileptic seizures. Epileptic seizures can vary from brief and nearly undetectable periods to long periods of vigorous shaking due to abnormal electrical ...
. Since many images are taken milliseconds apart, it shows how the brain responds to different stimuli, enabling researchers to study both the functional and structural brain abnormalities in psychological disorders. MRI also is used in guided stereotactic surgery
Stereotactic surgery is a minimally invasive form of surgical intervention that makes use of a three-dimensional coordinate system to locate small targets inside the body and to perform on them some action such as ablation, biopsy, lesion, injec ...
and radiosurgery
Radiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. Like other forms of radiation therapy (also called radiotherapy), it is usually u ...
for treatment of intracranial tumors, arteriovenous malformations, and other surgically treatable conditions using a device known as the N-localizer
The N-localizer is a device that enables guidance of stereotactic surgery or radiosurgery using tomographic images that are obtained via computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET). The N-local ...
. New tools that implement artificial intelligence in healthcare
Artificial intelligence in healthcare is an overarching term used to describe the use of machine-learning algorithms and software, or artificial intelligence (AI), to mimic human cognition in the analysis, presentation, and comprehension of compl ...
have demonstrated higher image quality and morphometric analysis in neuroimaging
Neuroimaging is the use of quantitative (computational) techniques to study the structure and function of the central nervous system, developed as an objective way of scientifically studying the healthy human brain in a non-invasive manner. Incre ...
with the application of a denoising system.
The record for the highest spatial resolution of a whole intact brain (postmortem) is 100 microns, from Massachusetts General Hospital. The data was published in NATURE on 30 October 2019.
Cardiovascular
 Cardiac MRI is complementary to other imaging techniques, such as
Cardiac MRI is complementary to other imaging techniques, such as echocardiography
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart.
It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Echocardiography has become routinely used in t ...
, cardiac CT, and nuclear medicine
Nuclear medicine or nucleology is a medical specialty involving the application of radioactive substances in the diagnosis and treatment of disease. Nuclear imaging, in a sense, is "radiology done inside out" because it records radiation emitting ...
. It can be used to assess the structure and the function of the heart. Its applications include assessment of myocardial ischemia and viability, cardiomyopathies
Cardiomyopathy is a group of diseases that affect the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. A ...
, myocarditis
Myocarditis, also known as inflammatory cardiomyopathy, is an acquired cardiomyopathy due to inflammation of the heart muscle. Symptoms can include shortness of breath, chest pain, decreased ability to exercise, and an irregular heartbeat. The ...
, iron overload
Iron overload or hemochromatosis (also spelled ''haemochromatosis'' in British English) indicates increased total accumulation of iron in the body from any cause and resulting organ damage. The most important causes are hereditary haemochromatosi ...
, vascular diseases, and congenital heart disease
A congenital heart defect (CHD), also known as a congenital heart anomaly and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital heart defect is classed as a cardiovascular ...
.
Musculoskeletal
Applications in the musculoskeletal system include spinal imaging, assessment ofjoint
A joint or articulation (or articular surface) is the connection made between bones, ossicles, or other hard structures in the body which link an animal's skeletal system into a functional whole.Saladin, Ken. Anatomy & Physiology. 7th ed. McGraw ...
disease, and soft tissue tumors. Also, MRI techniques can be used for diagnostic imaging of
systemic muscle diseases including genetic muscle diseases.
Swallowing movement of throat and oesophagus can cause motion artifact over the imaged spine. Therefore, a saturation pulse applied over this region the throat and oesophagus can help to avoid this artifact. Motion artifact arising due to pumping of the heart can be reduced by timing the MRI pulse according to heart cycles. Blood vessels flow artifacts can be reduced by applying saturation pulses above and below the region of interest.
Liver and gastrointestinal
Hepatobiliary
The biliary tract, (biliary tree or biliary system) refers to the liver, gallbladder and bile ducts, and how they work together to make, store and secrete bile. Bile consists of water, electrolytes, bile acids, cholesterol, phospholipids and ...
MR is used to detect and characterize lesions of the liver
The liver is a major Organ (anatomy), organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the Protein biosynthesis, synthesis of proteins and biochemicals necessary for ...
, pancreas
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e. it has both an end ...
, and bile duct
A bile duct is any of a number of long tube-like structures that carry bile, and is present in most vertebrates.
Bile is required for the digestion of food and is secreted by the liver into passages that carry bile toward the hepatic duct. It ...
s. Focal or diffuse disorders of the liver may be evaluated using diffusion-weighted, opposed-phase imaging and dynamic contrast enhancement sequences. Extracellular contrast agents are used widely in liver MRI, and newer hepatobiliary contrast agents also provide the opportunity to perform functional biliary imaging. Anatomical imaging of the bile ducts is achieved by using a heavily T2-weighted sequence in magnetic resonance cholangiopancreatography (MRCP). Functional imaging of the pancreas is performed following administration of secretin
Secretin is a hormone that regulates water homeostasis throughout the body and influences the environment of the duodenum by regulating secretions in the stomach, pancreas, and liver. It is a peptide hormone produced in the S cells of the duode ...
. MR enterography provides non-invasive assessment of inflammatory bowel disease and small bowel tumors. MR-colonography may play a role in the detection of large polyps in patients at increased risk of colorectal cancer.
Angiography
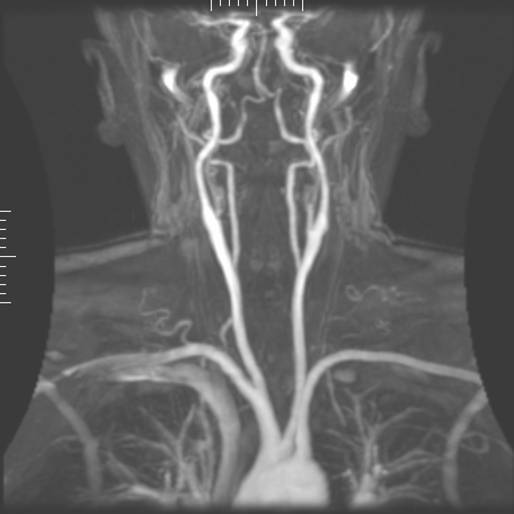
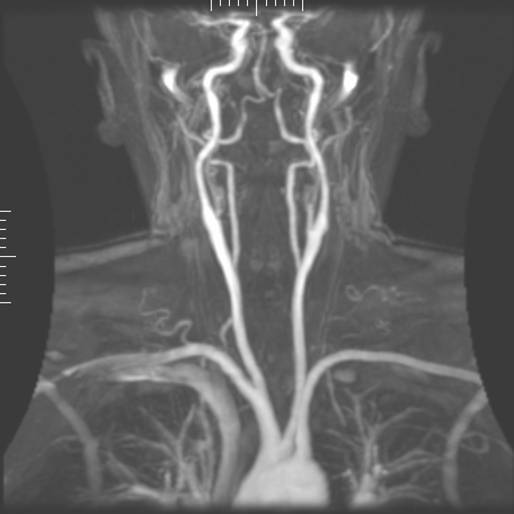 Magnetic resonance
Magnetic resonance angiography
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. Modern angiography is performe ...
(MRA) generates pictures of the arteries to evaluate them for stenosis
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
(abnormal narrowing) or aneurysm
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus (s ...
s (vessel wall dilatations, at risk of rupture). MRA is often used to evaluate the arteries of the neck and brain, the thoracic and abdominal aorta, the renal arteries, and the legs (called a "run-off"). A variety of techniques can be used to generate the pictures, such as administration of a paramagnetic
Paramagnetism is a form of magnetism whereby some materials are weakly attracted by an externally applied magnetic field, and form internal, induced magnetic fields in the direction of the applied magnetic field. In contrast with this behavior, d ...
contrast agent (gadolinium
Gadolinium is a chemical element with the symbol Gd and atomic number 64. Gadolinium is a silvery-white metal when oxidation is removed. It is only slightly malleable and is a ductile rare-earth element. Gadolinium reacts with atmospheric oxygen ...
) or using a technique known as "flow-related enhancement" (e.g., 2D and 3D time-of-flight sequences), where most of the signal on an image is due to blood that recently moved into that plane (see also FLASH MRI
Fast low angle shot magnetic resonance imaging (FLASH MRI) is a particular sequence of magnetic resonance imaging. It is a gradient echo sequence which combines a low-flip angle radio-frequency excitation of the nuclear magnetic resonance signal ( ...
).
Techniques involving phase accumulation (known as phase contrast angiography) can also be used to generate flow velocity maps easily and accurately. Magnetic resonance venography (MRV) is a similar procedure that is used to image veins. In this method, the tissue is now excited inferiorly, while the signal is gathered in the plane immediately superior to the excitation plane—thus imaging the venous blood that recently moved from the excited plane.
Contrast agents
MRI for imaging anatomical structures or blood flow do not require contrast agents since the varying properties of the tissues or blood provide natural contrasts. However, for more specific types of imaging,exogenous
In a variety of contexts, exogeny or exogeneity () is the fact of an action or object originating externally. It contrasts with endogeneity or endogeny, the fact of being influenced within a system.
Economics
In an economic model, an exogeno ...
contrast agents may be given intravenously
Intravenous therapy (abbreviated as IV therapy) is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutrie ...
, orally, or intra-articularly. Most contrast agents are either paramagnetic (e.g.: gadolinium, manganese, europium), and are used to shorten T1 in the tissue they accumulate in, or super-paramagnetic (SPIONs), and are used to shorten T2 and T2* in healthy tissue reducing its signal intensity (negative contrast agents). The most commonly used intravenous contrast agents are based on chelate
Chelation is a type of bonding of ions and molecules to metal ions. It involves the formation or presence of two or more separate coordinate bonds between a polydentate (multiple bonded) ligand and a single central metal atom. These ligands are ...
s of gadolinium
Gadolinium is a chemical element with the symbol Gd and atomic number 64. Gadolinium is a silvery-white metal when oxidation is removed. It is only slightly malleable and is a ductile rare-earth element. Gadolinium reacts with atmospheric oxygen ...
, which is highly paramagnetic. In general, these agents have proved safer than the iodinated contrast agents used in X-ray radiography or CT. Anaphylactoid reactions
Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the follow ...
are rare, occurring in approx. 0.03–0.1%. Of particular interest is the lower incidence of nephrotoxicity, compared with iodinated agents, when given at usual doses—this has made contrast-enhanced MRI scanning an option for patients with renal impairment, who would otherwise not be able to undergo contrast-enhanced CT.
Gadolinium-based contrast reagents are typically octadentate complexes of gadolinium(III). The complex is very stable (log K > 20) so that, in use, the concentration of the un-complexed Gd3+ ions should be below the toxicity limit. The 9th place in the metal ion's coordination sphere
In coordination chemistry, the first coordination sphere refers to the array of molecules and ions (the ligands) directly attached to the central metal atom. The second coordination sphere consists of molecules and ions that attached in various ...
is occupied by a water molecule which exchanges rapidly with water molecules in the reagent molecule's immediate environment, affecting the magnetic resonance relaxation time
In the physical sciences, relaxation usually means the return of a perturbed system into equilibrium.
Each relaxation process can be categorized by a relaxation time τ. The simplest theoretical description of relaxation as function of time ' ...
. For details see MRI contrast agent
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI). The most commonly used compounds for contrast enhancement are gadolinium-based. Such MRI contrast agents shorten ...
.
In December 2017, the Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a List of United States federal agencies, federal agency of the United States Department of Health and Human Services, Department of Health and Human Services. The FDA is respon ...
(FDA) in the United States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territorie ...
announced in a drug safety communication that new warnings were to be included on all gadolinium-based contrast agents (GBCAs). The FDA also called for increased patient education and requiring gadolinium contrast vendors to conduct additional animal and clinical studies to assess the safety of these agents.
Although gadolinium agents have proved useful for patients with kidney impairment, in patients with severe kidney failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as eit ...
requiring dialysis there is a risk of a rare but serious illness, nephrogenic systemic fibrosis
Nephrogenic systemic fibrosis is a rare syndrome that involves fibrosis of skin, joints, eyes, and internal organs. NSF is caused by exposure to gadolinium in gadolinium-based MRI contrast agents (GBCAs) in patients with impaired kidney function. ...
, which may be linked to the use of certain gadolinium-containing agents. The most frequently linked is gadodiamide
Gadodiamide, sold under the brand name Omniscan, is a gadolinium-based MRI contrast agent (GBCA), used in magnetic resonance imaging (MRI) procedures to assist in the visualization of blood vessels.
Medical uses
Gadodiamide is a contrast med ...
, but other agents have been linked too. Although a causal link has not been definitively established, current guidelines in the United States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territorie ...
are that dialysis patients should only receive gadolinium agents where essential and that dialysis should be performed as soon as possible after the scan to remove the agent from the body promptly.
In Europe, where more gadolinium-containing agents are available, a classification of agents according to potential risks has been released. In 2008, a new contrast agent named gadoxetate, brand name Eovist (US) or Primovist (EU), was approved for diagnostic use: This has the theoretical benefit of a dual excretion path.
Sequences
AnMRI sequence
An MRI sequence in magnetic resonance imaging (MRI) is a particular setting of pulse sequences and pulsed field gradients, resulting in a particular image appearance.
A multiparametric MRI is a combination of two or more sequences, and/or includin ...
is a particular setting of radiofrequency pulses and gradients, resulting in a particular image appearance. The T1 and T2 weighting can also be described as MRI sequences.
Other specialized configurations
Magnetic resonance spectroscopy
Magnetic resonance spectroscopy
Nuclear magnetic resonance spectroscopy, most commonly known as NMR spectroscopy or magnetic resonance spectroscopy (MRS), is a spectroscopic technique to observe local magnetic fields around atomic nuclei. The sample is placed in a magnetic fiel ...
(MRS) is used to measure the levels of different metabolites
In biochemistry, a metabolite is an intermediate or end product of metabolism.
The term is usually used for small molecules. Metabolites have various functions, including fuel, structure, signaling, stimulatory and inhibitory effects on enzymes, c ...
in body tissues, which can be achieved through a variety of single voxel or imaging-based techniques. The MR signal produces a spectrum of resonances that corresponds to different molecular arrangements of the isotope being "excited". This signature is used to diagnose certain metabolic disorders, especially those affecting the brain, and to provide information on tumor metabolism
Metabolism (, from el, μεταβολή ''metabolē'', "change") is the set of life-sustaining chemical reactions in organisms. The three main functions of metabolism are: the conversion of the energy in food to energy available to run cell ...
.
Magnetic resonance spectroscopic imaging (MRSI) combines both spectroscopic and imaging methods to produce spatially localized spectra from within the sample or patient. The spatial resolution is much lower (limited by the available SNR), but the spectra in each voxel contains information about many metabolites. Because the available signal is used to encode spatial and spectral information, MRSI requires high SNR achievable only at higher field strengths (3 T and above). The high procurement and maintenance costs of MRI with extremely high field strengths inhibit their popularity. However, recent compressed sensing
Compressed sensing (also known as compressive sensing, compressive sampling, or sparse sampling) is a signal processing technique for efficiently acquiring and reconstructing a Signal (electronics), signal, by finding solutions to Underdetermined ...
-based software algorithms (''e.g.'', SAMV) have been proposed to achieve super-resolution
Super-resolution imaging (SR) is a class of techniques that enhance (increase) the resolution of an imaging system. In optical SR the diffraction limit of systems is transcended, while in geometrical SR the resolution of digital imaging sensors i ...
without requiring such high field strengths.
Real-time MRI
Real-time MRI
Real-time magnetic resonance imaging (RT-MRI) refers to the continuous monitoring ("filming") of moving objects in real time. Because MRI is based on time-consuming scanning of k-space, real-time MRI was possible only with low image quality or ...
refers to the continuous imaging of moving objects (such as the heart) in real time. One of the many different strategies developed since the early 2000s is based on radial FLASH MRI
Fast low angle shot magnetic resonance imaging (FLASH MRI) is a particular sequence of magnetic resonance imaging. It is a gradient echo sequence which combines a low-flip angle radio-frequency excitation of the nuclear magnetic resonance signal ( ...
, and iterative reconstruction
Iterative reconstruction refers to iterative algorithms used to reconstruct 2D and 3D images in certain imaging techniques.
For example, in computed tomography an image must be reconstructed from projections of an object. Here, iterative recons ...
. This gives a temporal resolution of 20–30 ms for images with an in-plane resolution of 1.5–2.0 mm. Balanced steady-state free precession (bSSFP) imaging has a better image contrast between the blood pool and myocardium than the FLASH MRI
Fast low angle shot magnetic resonance imaging (FLASH MRI) is a particular sequence of magnetic resonance imaging. It is a gradient echo sequence which combines a low-flip angle radio-frequency excitation of the nuclear magnetic resonance signal ( ...
, yet it will produce severe banding artifact when the B0 inhomogeneity is strong. Real-time MRI
Real-time magnetic resonance imaging (RT-MRI) refers to the continuous monitoring ("filming") of moving objects in real time. Because MRI is based on time-consuming scanning of k-space, real-time MRI was possible only with low image quality or ...
is likely to add important information on diseases of the heart and the joints, and in many cases may make MRI examinations easier and more comfortable for patients, especially for the patients who cannot hold their breathings or who have arrhythmia.
Interventional MRI
The lack of harmful effects on the patient and the operator make MRI well-suited forinterventional radiology
Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs bo ...
, where the images produced by an MRI scanner guide minimally invasive procedures. Such procedures use no ferromagnetic
Ferromagnetism is a property of certain materials (such as iron) which results in a large observed magnetic permeability, and in many cases a large magnetic coercivity allowing the material to form a permanent magnet. Ferromagnetic materials ...
instruments.
A specialized growing subset of interventional MRI is intraoperative MRI
Intraoperative magnetic resonance imaging (iMRI) refers to an operating room configuration that enables surgeons to image the patient via an MRI scanner while the patient is undergoing surgery, particularly brain surgery. iMRI reduces the risk of ...
, in which an MRI is used in surgery. Some specialized MRI systems allow imaging concurrent with the surgical procedure. More typically, the surgical procedure is temporarily interrupted so that MRI can assess the success of the procedure or guide subsequent surgical work.
Magnetic resonance guided focused ultrasound
In guided therapy,high-intensity focused ultrasound
High-intensity focused ultrasound (HIFU) is a non-invasive therapeutic technique that uses non-ionizing ultrasonic waves to heat or ablate tissue. HIFU can be used to increase the flow of blood or lymph or to destroy tissue, such as tumors, via ...
(HIFU) beams are focused on a tissue, that are controlled using MR thermal imaging. Due to the high energy at the focus, the temperature rises to above 65 °C
The degree Celsius is the unit of temperature on the Celsius scale (originally known as the centigrade scale outside Sweden), one of two temperature scales used in the International System of Units (SI), the other being the Kelvin scale. The ...
(150 °F) which completely destroys the tissue. This technology can achieve precise ablation
Ablation ( la, ablatio – removal) is removal or destruction of something from an object by vaporization, chipping, erosion, erosive processes or by other means. Examples of ablative materials are described below, and include spacecraft materi ...
of diseased tissue. MR imaging provides a three-dimensional view of the target tissue, allowing for the precise focusing of ultrasound energy. The MR imaging provides quantitative, real-time, thermal images of the treated area. This allows the physician to ensure that the temperature generated during each cycle of ultrasound energy is sufficient to cause thermal ablation within the desired tissue and if not, to adapt the parameters to ensure effective treatment.
Multinuclear imaging
Hydrogen has the most frequently imagednucleus
Nucleus ( : nuclei) is a Latin word for the seed inside a fruit. It most often refers to:
*Atomic nucleus, the very dense central region of an atom
*Cell nucleus, a central organelle of a eukaryotic cell, containing most of the cell's DNA
Nucle ...
in MRI because it is present in biological tissues in great abundance, and because its high gyromagnetic ratio
In physics, the gyromagnetic ratio (also sometimes known as the magnetogyric ratio in other disciplines) of a particle or system is the ratio of its magnetic moment to its angular momentum, and it is often denoted by the symbol , gamma. Its SI u ...
gives a strong signal. However, any nucleus with a net nuclear spin
In atomic physics, the spin quantum number is a quantum number (designated ) which describes the intrinsic angular momentum (or spin angular momentum, or simply spin) of an electron or other particle. The phrase was originally used to describe th ...
could potentially be imaged with MRI. Such nuclei include helium-3
Helium-3 (3He see also helion) is a light, stable isotope of helium with two protons and one neutron (the most common isotope, helium-4, having two protons and two neutrons in contrast). Other than protium (ordinary hydrogen), helium-3 is the ...
, lithium-7
Naturally occurring lithium (3Li) is composed of two stable isotope ratio, stable isotopes, lithium-6 and lithium-7, with the latter being far more abundant on Earth. Both of the natural Isotope, isotopes have an unexpectedly low nuclear bindin ...
, carbon-13
Carbon-13 (13C) is a natural, stable isotope of carbon with a nucleus containing six protons and seven neutrons. As one of the environmental isotopes, it makes up about 1.1% of all natural carbon on Earth.
Detection by mass spectrometry
A mass ...
, fluorine
Fluorine is a chemical element with the symbol F and atomic number 9. It is the lightest halogen and exists at standard conditions as a highly toxic, pale yellow diatomic gas. As the most electronegative reactive element, it is extremely reacti ...
-19, oxygen-17
Oxygen-17 (17O) is a low-abundance, natural, stable isotope of oxygen (0.0373% in seawater; approximately twice as abundant as deuterium).
As the only stable isotope of oxygen possessing a nuclear spin (+5/2) and a favorable characteristic of fi ...
, sodium
Sodium is a chemical element with the symbol Na (from Latin ''natrium'') and atomic number 11. It is a soft, silvery-white, highly reactive metal. Sodium is an alkali metal, being in group 1 of the periodic table. Its only stable iso ...
-23, phosphorus
Phosphorus is a chemical element with the symbol P and atomic number 15. Elemental phosphorus exists in two major forms, white phosphorus and red phosphorus, but because it is highly reactive, phosphorus is never found as a free element on Ear ...
-31 and xenon-129. 23Na and 31P are naturally abundant in the body, so they can be imaged directly. Gaseous isotopes such as 3He or 129Xe must be hyperpolarized and then inhaled as their nuclear density is too low to yield a useful signal under normal conditions. 17O and 19F can be administered in sufficient quantities in liquid form (e.g. 17O-water) that hyperpolarization is not a necessity. Using helium or xenon has the advantage of reduced background noise, and therefore increased contrast for the image itself, because these elements are not normally present in biological tissues.
Moreover, the nucleus of any atom that has a net nuclear spin and that is bonded to a hydrogen atom could potentially be imaged via heteronuclear magnetization transfer MRI that would image the high-gyromagnetic-ratio hydrogen nucleus instead of the low-gyromagnetic-ratio nucleus that is bonded to the hydrogen atom. In principle, heteronuclear magnetization transfer MRI could be used to detect the presence or absence of specific chemical bonds.
Multinuclear imaging is primarily a research technique at present. However, potential applications include functional imaging and imaging of organs poorly seen on 1H MRI (e.g., lungs and bones) or as alternative contrast agents. Inhaled hyperpolarized 3He can be used to image the distribution of air spaces within the lungs. Injectable solutions containing 13C or stabilized bubbles of hyperpolarized 129Xe have been studied as contrast agents for angiography and perfusion imaging. 31P can potentially provide information on bone density and structure, as well as functional imaging of the brain. Multinuclear imaging holds the potential to chart the distribution of lithium in the human brain, this element finding use as an important drug for those with conditions such as bipolar disorder.
Molecular imaging by MRI
MRI has the advantages of having very high spatial resolution and is very adept at morphological imaging and functional imaging. MRI does have several disadvantages though. First, MRI has a sensitivity of around 10−3 mol/L to 10−5 mol/L, which, compared to other types of imaging, can be very limiting. This problem stems from the fact that the population difference between the nuclear spin states is very small at room temperature. For example, at 1.5 teslas, a typical field strength for clinical MRI, the difference between high and low energy states is approximately 9 molecules per 2 million. Improvements to increase MR sensitivity include increasing magnetic field strength and hyperpolarization via optical pumping or dynamic nuclear polarization. There are also a variety of signal amplification schemes based on chemical exchange that increase sensitivity. To achieve molecular imaging of disease biomarkers using MRI, targeted MRIcontrast agent
A contrast agent (or contrast medium) is a substance used to increase the contrast of structures or fluids within the body in medical imaging. Contrast agents absorb or alter external electromagnetism or ultrasound, which is different from radiop ...
s with high specificity and high relaxivity (sensitivity) are required. To date, many studies have been devoted to developing targeted-MRI contrast agents to achieve molecular imaging by MRI. Commonly, peptides, antibodies, or small ligands, and small protein domains, such as HER-2 affibodies, have been applied to achieve targeting. To enhance the sensitivity of the contrast agents, these targeting moieties are usually linked to high payload MRI contrast agents or MRI contrast agents with high relaxivities. A new class of gene targeting MR contrast agents has been introduced to show gene action of unique mRNA and gene transcription factor proteins. These new contrast agents can trace cells with unique mRNA, microRNA and virus; tissue response to inflammation in living brains. The MR reports change in gene expression with positive correlation to TaqMan analysis, optical and electron microscopy.
Parallel MRI
It takes time to gather MRI data using sequential applications of magnetic field gradients. Even for the most streamlined ofMRI sequence
An MRI sequence in magnetic resonance imaging (MRI) is a particular setting of pulse sequences and pulsed field gradients, resulting in a particular image appearance.
A multiparametric MRI is a combination of two or more sequences, and/or includin ...
s, there are physical and physiologic limits to the rate of gradient switching. Parallel MRI circumvents these limits by gathering some portion of the data simultaneously, rather than in a traditional sequential fashion. This is accomplished using arrays of radiofrequency (RF) detector coils, each with a different 'view' of the body. A reduced set of gradient steps is applied, and the remaining spatial information is filled in by combining signals from various coils, based on their known spatial sensitivity patterns. The resulting acceleration is limited by the number of coils and by the signal to noise ratio (which decreases with increasing acceleration), but two- to four-fold accelerations may commonly be achieved with suitable coil array configurations, and substantially higher accelerations have been demonstrated with specialized coil arrays. Parallel MRI may be used with most MRI sequence
An MRI sequence in magnetic resonance imaging (MRI) is a particular setting of pulse sequences and pulsed field gradients, resulting in a particular image appearance.
A multiparametric MRI is a combination of two or more sequences, and/or includin ...
s.
After a number of early suggestions for using arrays of detectors to accelerate imaging went largely unremarked in the MRI field, parallel imaging saw widespread development and application following the introduction of the SiMultaneous Acquisition of Spatial Harmonics (SMASH) technique in 1996–7. The SENSitivity Encoding (SENSE) and Generalized Autocalibrating Partially Parallel Acquisitions (GRAPPA) techniques are the parallel imaging methods in most common use today. The advent of parallel MRI resulted in extensive research and development in image reconstruction and RF coil design, as well as in a rapid expansion of the number of receiver channels available on commercial MR systems. Parallel MRI is now used routinely for MRI examinations in a wide range of body areas and clinical or research applications.
Quantitative MRI
Most MRI focuses on qualitative interpretation of MR data by acquiring spatial maps of relative variations in signal strength which are "weighted" by certain parameters. Quantitative methods instead attempt to determine spatial maps of accurate tissue relaxometry parameter values or magnetic field, or to measure the size of certain spatial features. Examples of quantitative MRI methods are: * T1-mapping (notably used incardiac magnetic resonance imaging
Cardiac magnetic resonance imaging (cardiac MRI), also known as cardiovascular MRI, is a magnetic resonance imaging (MRI) technology used for non-invasive assessment of the function and structure of the cardiovascular system. Conditions in which it ...
)
* T2-mapping
* Quantitative susceptibility mapping (QSM)
* Quantitative fluid flow MRI (i.e. some cerebrospinal fluid flow MRI
Cerebrospinal fluid (CSF) flow MRI is used to assess pulsatile CSF flow both qualitatively and quantitatively. Time-resolved 2D phase-contrast MRI with velocity encoding is the most common method for CSF analysis. CSF Fluid Flow MRI detects back ...
)
* Magnetic resonance elastography (MRE)
Quantitative MRI aims to increase the reproducibility
Reproducibility, also known as replicability and repeatability, is a major principle underpinning the scientific method. For the findings of a study to be reproducible means that results obtained by an experiment or an observational study or in a ...
of MR images and interpretations, but has historically require longer scan times.
Quantitative MRI (or qMRI) sometimes more specifically refers to multi-parametric quantitative MRI, the mapping of multiple tissue relaxometry parameters in a single imaging session.
Efforts to make multi-parametric quantitative MRI faster have produced sequences which map multiple parameters simultaneously, either by building separate encoding methods for each parameter into the sequence,
or by fitting MR signal evolution to a multi-parameter model.
Safety
MRI is, in general, a safe technique, although injuries may occur as a result of failed safety procedures or human error.Contraindications
In medicine, a contraindication is a condition that serves as a reason not to take a certain medical treatment due to the harm that it would cause the patient. Contraindication is the opposite of indication, which is a reason to use a certain tre ...
to MRI include most cochlear implant
A cochlear implant (CI) is a surgically implanted neuroprosthesis that provides a person who has moderate-to-profound sensorineural hearing loss with sound perception. With the help of therapy, cochlear implants may allow for improved speech und ...
s and cardiac pacemakers
350px, Image showing the cardiac pacemaker or SA node, the primary pacemaker within the electrical_conduction_system_of_the_heart">SA_node,_the_primary_pacemaker_within_the_electrical_conduction_system_of_the_heart.
The_muscle_contraction.htm ...
, shrapnel
Shrapnel may refer to:
Military
* Shrapnel shell, explosive artillery munitions, generally for anti-personnel use
* Shrapnel (fragment), a hard loose material
Popular culture
* ''Shrapnel'' (Radical Comics)
* ''Shrapnel'', a game by Adam C ...
, and metallic foreign bodies
A foreign body (FB) is any object originating outside the body of an organism. In machinery, it can mean any unwanted intruding object.
Most references to foreign bodies involve propulsion through natural orifices into hollow organs.
Foreign bo ...
in the eyes
Eyes are organs of the visual system. They provide living organisms with vision, the ability to receive and process visual detail, as well as enabling several photo response functions that are independent of vision. Eyes detect light and conve ...
. Magnetic resonance imaging in pregnancy appears to be safe, at least during the second and third trimesters
Pregnancy is the time during which one or more offspring develops ( gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.
Pregnancy usually occurs by sexual intercourse, but ca ...
if done without contrast agents. Since MRI does not use any ionizing radiation, its use is generally favored in preference to CT when either modality could yield the same information. Some patients experience claustrophobia and may require sedation or shorter MRI protocols. Amplitude and rapid switching of gradient coils during image acquisition may cause peripheral nerve stimulation.
MRI uses powerful magnets and can therefore cause magnetic materials
A magnet is a material or object that produces a magnetic field. This magnetic field is invisible but is responsible for the most notable property of a magnet: a force that pulls on other ferromagnetic materials, such as iron, steel, nickel, ...
to move at great speeds, posing a projectile risk, and may cause fatal accidents. However, as millions of MRIs are performed globally each year, fatalities are extremely rare.
Overuse
Medical societies issue guidelines for when physicians should use MRI on patients and recommend against overuse. MRI can detect health problems or confirm a diagnosis, but medical societies often recommend that MRI not be the first procedure for creating a plan to diagnose or manage a patient's complaint. A common case is to use MRI to seek a cause oflow back pain
Low back pain (LBP) or lumbago is a common disorder involving the muscles, nerves, and bones of the back, in between the lower edge of the ribs and the lower fold of the buttocks. Pain can vary from a dull constant ache to a sudden sharp feeli ...
; the American College of Physicians
The American College of Physicians (ACP) is a national organization of internists, who specialize in the diagnosis, treatment, and care of adults.Sokanu "What is an Internist?" Retrieved October 20, 2014 With 161,000 members, ACP is the largest ...
, for example, recommends against this procedure as unlikely to result in a positive outcome for the patient.
Artifacts
 An
An MRI artifact An MRI artifact is a visual artifact (an anomaly seen during visual representation) in magnetic resonance imaging (MRI). It is a feature appearing in an image that is not present in the original object. Many different artifacts can occur
during MRI, ...
is a visual artifact
Visual artifacts (also artefacts) are artifact (error), anomalies apparent during visual representation as in digital graphics and other forms of imagery, especially photography and microscopy.
In digital graphics
* Image quality#Image quality f ...
, that is, an anomaly during visual representation. Many different artifacts can occur during magnetic resonance imaging (MRI), some affecting the diagnostic quality, while others may be confused with pathology. Artifacts can be classified as patient-related, signal processing-dependent and hardware (machine)-related.
Non-medical use
MRI is used industrially mainly for routine analysis of chemicals. Thenuclear magnetic resonance
Nuclear magnetic resonance (NMR) is a physical phenomenon in which nuclei in a strong constant magnetic field are perturbed by a weak oscillating magnetic field (in the near field) and respond by producing an electromagnetic signal with a ...
technique is also used, for example, to measure the ratio between water and fat in foods, monitoring of flow of corrosive fluids in pipes, or to study molecular structures such as catalysts.
Being non-invasive and non-damaging, MRI can be used to study the anatomy of plants, their water transportation processes and water balance. It is also applied to veterinary radiology for diagnostic purposes. Outside this, its use in zoology is limited due to the high cost; but it can be used on many species.
In palaeontology it is used to examine the structure of fossils.
Forensic
Forensic science, also known as criminalistics, is the application of science to Criminal law, criminal and Civil law (legal system), civil laws, mainly—on the criminal side—during criminal investigation, as governed by the legal standard ...
imaging provides graphic documentation of an autopsy
An autopsy (post-mortem examination, obduction, necropsy, or autopsia cadaverum) is a surgical procedure that consists of a thorough examination of a corpse by dissection to determine the cause, mode, and manner of death or to evaluate any di ...
, which manual autopsy does not. CT scanning provides quick whole-body imaging of skeletal and parenchyma
Parenchyma () is the bulk of functional substance in an animal organ or structure such as a tumour. In zoology it is the name for the tissue that fills the interior of flatworms.
Etymology
The term ''parenchyma'' is New Latin from the word π ...
l alterations, whereas MRI imaging gives better representation of soft tissue pathology
Pathology is the study of the causes and effects of disease or injury. The word ''pathology'' also refers to the study of disease in general, incorporating a wide range of biology research fields and medical practices. However, when used in ...
. But MRI is more expensive, and more time-consuming to utilize. Moreover, the quality of MR imaging deteriorates below 10 °C.
History
In 1971 atStony Brook University
Stony Brook University (SBU), officially the State University of New York at Stony Brook, is a public research university in Stony Brook, New York. Along with the University at Buffalo, it is one of the State University of New York system's ...
, Paul Lauterbur applied magnetic field gradients in all three dimensions and a back-projection technique to create NMR images. He published the first images of two tubes of water in 1973 in the journal ''Nature'', followed by the picture of a living animal, a clam, and in 1974 by the image of the thoracic cavity of a mouse. Lauterbur called his imaging method zeugmatography, a term which was replaced by (N)MR imaging. In the late 1970s, physicists Peter Mansfield
Sir Peter Mansfield (9 October 1933 – 8 February 2017) was an English physicist who was awarded the 2003 Nobel Prize in Physiology or Medicine, shared with Paul Lauterbur, for discoveries concerning Magnetic Resonance Imaging (MRI). Mansfie ...
and Paul Lauterbur
Paul Christian Lauterbur (May 6, 1929 – March 27, 2007) was an American chemist who shared the Nobel Prize in Physiology or Medicine in 2003 with Peter Mansfield for his work which made the development of magnetic resonance imaging (MRI) poss ...
developed MRI-related techniques, like the echo-planar imaging (EPI) technique.
Advances in semiconductor
A semiconductor is a material which has an electrical resistivity and conductivity, electrical conductivity value falling between that of a electrical conductor, conductor, such as copper, and an insulator (electricity), insulator, such as glas ...
technology were crucial to the development of practical MRI, which requires a large amount of computational power. This was made possible by the rapidly increasing number of transistors
upright=1.4, gate (G), body (B), source (S) and drain (D) terminals. The gate is separated from the body by an insulating layer (pink).
A transistor is a semiconductor device used to Electronic amplifier, amplify or electronic switch, switch e ...
on a single integrated circuit
An integrated circuit or monolithic integrated circuit (also referred to as an IC, a chip, or a microchip) is a set of electronic circuits on one small flat piece (or "chip") of semiconductor material, usually silicon. Large numbers of tiny ...
chip. Mansfield and Lauterbur were awarded the 2003 Nobel Prize in Physiology or Medicine
The Nobel Prize in Physiology or Medicine is awarded yearly by the Nobel Assembly at the Karolinska Institute for outstanding discoveries in physiology or medicine. The Nobel Prize is not a single prize, but five separate prizes that, accord ...
for their "discoveries concerning magnetic resonance imaging".
See also
* Amplified magnetic resonance imaging *Electron paramagnetic resonance
Electron paramagnetic resonance (EPR) or electron spin resonance (ESR) spectroscopy is a method for studying materials that have unpaired electrons. The basic concepts of EPR are analogous to those of nuclear magnetic resonance (NMR), but the spin ...
* High-definition fiber tracking
* High-resolution computed tomography
High-resolution computed tomography (HRCT) is a type of computed tomography (CT) with specific techniques to enhance image resolution. It is used in the diagnosis of various health problems, though most commonly for lung disease, by assessing t ...
* History of neuroimaging
The first neuroimaging technique ever is the so-called 'human circulation balance' invented by Angelo Mosso in the 1880s and able to non-invasively measure the redistribution of blood during emotional and intellectual activity.
Then, in the early ...
* International Society for Magnetic Resonance in Medicine
The International Society for Magnetic Resonance in Medicine is a "multi-disciplinary nonprofit association that promotes innovation, development, and application of magnetic resonance techniques in medicine and biology throughout the world".
The ...
* Jemris Jemris is an open source MRI sequence design and simulation framework written in C++.
It was designed to most generally and numerically integrate the Bloch equation in a single-core or parallel fashion for protons over a time course of a sequence ...
* List of neuroimaging software
Neuroimaging software is used to study the structure and function of the brain. To see an NIH Blueprint for Neuroscience Research funded clearinghouse of many of these software applications, as well as hardware, etc. go to the NITRC web site.
* 3 ...
* Magnetic immunoassay
Magnetic immunoassay (MIA) is a type of diagnostic immunoassay using magnetic beads as labels in lieu of conventional enzymes (ELISA), radioisotopes (RIA) or fluorescent moieties ( fluorescent immunoassays) to detect a specified analyte. MIA involv ...
* Magnetic particle imaging Magnetic particle imaging (MPI) is an emerging non-invasive tomographic technique that directly detects superparamagnetic nanoparticle tracers. The technology has potential applications in diagnostic imaging and material science. Currently, it i ...
* Magnetic resonance elastography
* ''Magnetic Resonance Imaging'' (journal)
* Magnetic resonance microscopy
Magnetic resonance microscopy (MRM, μMRI) is magnetic resonance imaging (MRI) at a microscopic level down to the scale of microns. The first definition of MRM was MRI having voxel resolutions of better than 100 μm.
Nomenclature
Magnetic r ...
* Nobel Prize controversies – Physiology or medicine
* Rabi cycle
In physics, the Rabi cycle (or Rabi flop) is the cyclic behaviour of a two-level quantum system in the presence of an oscillatory driving field. A great variety of physical processes belonging to the areas of quantum computing, condensed matter, ...
* Robinson oscillator
The Robinson oscillator is an electronic oscillator circuit originally devised for use in the field of continuous wave (CW) nuclear magnetic resonance (NMR). It was a development of the marginal oscillator. Strictly one should distinguish between ...
* Sodium MRI
Sodium MRI (also known as 23 Na-MRI) is a specialised magnetic resonance imaging technique that uses strong magnetic fields, magnetic field gradients, and radio waves to generate images of the distribution of sodium in the body, as opposed to mo ...
* Virtopsy
Virtopsy is a virtual alternative to a traditional autopsy, conducted with scanning and imaging technology. The name is a portmanteau of "virtual" and "autopsy" and is a trademark registered to Richard Dirnhofer (de), the former head of the Insti ...
References
Further reading
* * * * * * * * * * * * * * * * * *External links
*A Guided Tour of MRI: An introduction for laypeople
National High Magnetic Field Laboratory
The Basics of MRI
''Underlying physics and technical aspects''.
from the Institute for Magnetic Resonance Safety, Education, and Research (IMRSER)
Royal Institution Lecture – MRI: A Window on the Human Body
* ttps://www.howequipmentworks.com/mri_basics/ How MRI works explained simply using diagrams
Real-time MRI videos: Biomedizinische NMR Forschungs GmbH
* Paul C. Lauterbur
Genesis of the MRI (Magnetic Resonance Imaging) notebook, September 1971
(all pages freely available for download in variety of formats from
Science History Institute
The Science History Institute is an institution that preserves and promotes understanding of the history of science. Located in Philadelphia, Pennsylvania, it includes a library, museum, archive, research center and conference center.
It was fo ...
Digital Collections adigital.sciencehistory.org
{{DEFAULTSORT:Magnetic Resonance Imaging 1973 introductions American inventions Articles containing video clips Cryogenics Radiology Discovery and invention controversies 20th-century inventions Biomagnetics