Cardiovascular on:
[Wikipedia]
[Google]
[Amazon]
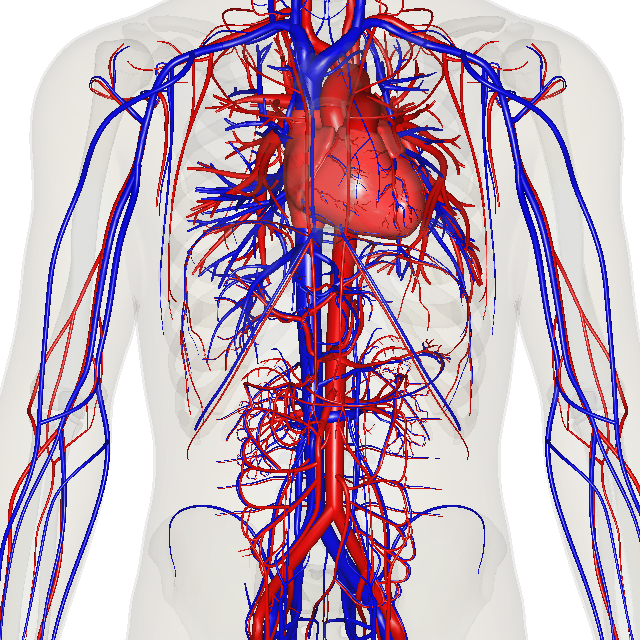
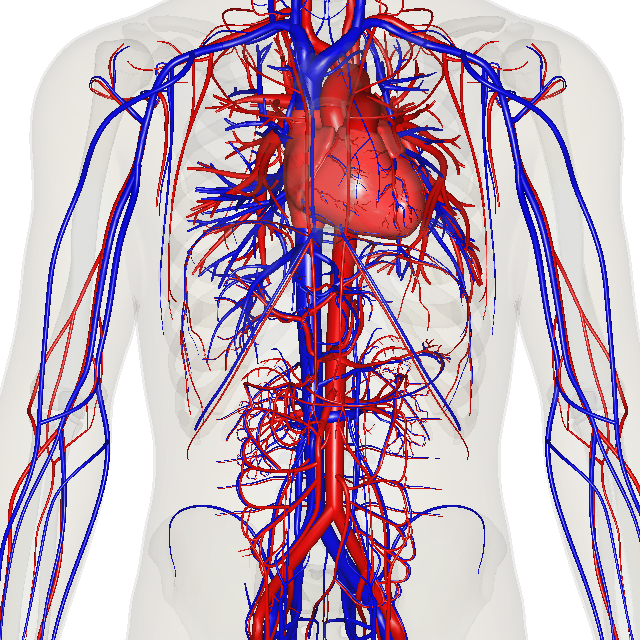
The blood circulatory system is a system of organs that includes the
 The circulatory system includes the
The circulatory system includes the
 The heart pumps blood to all parts of the body providing
The heart pumps blood to all parts of the body providing
 The pulmonary circulation is the portion of the cardiovascular system in which
The pulmonary circulation is the portion of the cardiovascular system in which
 The systemic circulation is a circuit loop that delivers oxygenated blood from the left heart to the rest of the body through the
The systemic circulation is a circuit loop that delivers oxygenated blood from the left heart to the rest of the body through the
 Oxygenated blood enters the systemic circulation when leaving the left ventricle, via the aortic semilunar valve. The first part of the systemic circulation is the aorta, a massive and thick-walled artery. The aorta arches and gives branches supplying the upper part of the body after passing through the aortic opening of the diaphragm at the level of thoracic ten vertebra, it enters the abdomen. Later, it descends down and supplies branches to abdomen, pelvis, perineum and the lower limbs.
The walls of the aorta are elastic. This elasticity helps to maintain the
Oxygenated blood enters the systemic circulation when leaving the left ventricle, via the aortic semilunar valve. The first part of the systemic circulation is the aorta, a massive and thick-walled artery. The aorta arches and gives branches supplying the upper part of the body after passing through the aortic opening of the diaphragm at the level of thoracic ten vertebra, it enters the abdomen. Later, it descends down and supplies branches to abdomen, pelvis, perineum and the lower limbs.
The walls of the aorta are elastic. This elasticity helps to maintain the
 The human arterial system originates from the aortic arches and from the dorsal aortae starting from week 4 of embryonic life. The first and second aortic arches regress and form only the maxillary arteries and stapedial arteries respectively. The arterial system itself arises from aortic arches 3, 4 and 6 (aortic arch 5 completely regresses).
The dorsal aortae, present on the dorsal side of the embryo, are initially present on both sides of the embryo. They later fuse to form the basis for the aorta itself. Approximately thirty smaller arteries branch from this at the back and sides. These branches form the
The human arterial system originates from the aortic arches and from the dorsal aortae starting from week 4 of embryonic life. The first and second aortic arches regress and form only the maxillary arteries and stapedial arteries respectively. The arterial system itself arises from aortic arches 3, 4 and 6 (aortic arch 5 completely regresses).
The dorsal aortae, present on the dorsal side of the embryo, are initially present on both sides of the embryo. They later fuse to form the basis for the aorta itself. Approximately thirty smaller arteries branch from this at the back and sides. These branches form the
 The function and health of the circulatory system and its parts are measured in a variety of manual and automated ways. These include simple methods such as those that are part of the
The function and health of the circulatory system and its parts are measured in a variety of manual and automated ways. These include simple methods such as those that are part of the
 While humans, as well as other
While humans, as well as other

 The circulatory systems of all vertebrates, as well as of
The circulatory systems of all vertebrates, as well as of
 The earliest known writings on the circulatory system are found in the Ebers Papyrus (16th century BCE), an ancient Egyptian medical papyrus containing over 700 prescriptions and remedies, both physical and spiritual. In the
The earliest known writings on the circulatory system are found in the Ebers Papyrus (16th century BCE), an ancient Egyptian medical papyrus containing over 700 prescriptions and remedies, both physical and spiritual. In the
"History of Medicine: Sushruta – the Clinician – Teacher par Excellence"
, ''Indian J Chest Dis Allied Sci'' Vol. 49 pp. 243–244, National Informatics Centre (Government of India). The valves of the heart were discovered by a physician of the Hippocratean school around the 4th century BCE. However, their function was not properly understood then. Because blood pools in the veins after death, arteries look empty. Ancient anatomists assumed they were filled with air and that they were for the transport of air. The Greek physician, Herophilus, distinguished veins from arteries but thought that the pulse was a property of arteries themselves. Greek anatomist Erasistratus observed that arteries that were cut during life bleed. He ascribed the fact to the phenomenon that air escaping from an artery is replaced with blood that enters between veins and arteries by very small vessels. Thus he apparently postulated capillaries but with reversed flow of blood. In 2nd-century AD Finally, the English physician
Finally, the English physician
Circulatory Pathways
in ''Anatomy and Physiology'' by
The Circulatory System
Study on the Manuscript of Paris by Servetus (1546 description of the Pulmonary Circulation) {{DEFAULTSORT:Circulatory System Exercise physiology Angiology
heart
The heart is a muscular Organ (biology), organ in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as ca ...
, blood vessel
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide awa ...
s, and blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the cir ...
which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, that consists of the heart and blood vessels (from Greek ''kardia'' meaning ''heart'', and from Latin ''vascula'' meaning ''vessels''). The circulatory system has two divisions, a systemic circulation or circuit, and a pulmonary circulation or circuit. Some sources use the terms ''cardiovascular system'' and ''vascular system'' interchangeably with the ''circulatory system''.
The network of blood vessels are the great vessels of the heart including large elastic arteries, and large vein
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated ...
s; other arteries, smaller arterioles, capillaries
A capillary is a small blood vessel from 5 to 10 micrometres (μm) in diameter. Capillaries are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the smallest blood vessels in the body: ...
that join with venule
A venule is a very small blood vessel in the microcirculation that allows blood to return from the capillary beds to drain into the larger blood vessels, the veins. Venules range from 7μm to 1mm in diameter. Veins contain approximately 70% of ...
s (small veins), and other veins. The circulatory system is closed in vertebrates, which means that the blood never leaves the network of blood vessels. Some invertebrate
Invertebrates are a paraphyletic group of animals that neither possess nor develop a vertebral column (commonly known as a ''backbone'' or ''spine''), derived from the notochord. This is a grouping including all animals apart from the chorda ...
s such as arthropod
Arthropods (, (gen. ποδός)) are invertebrate animals with an exoskeleton, a segmented body, and paired jointed appendages. Arthropods form the phylum Arthropoda. They are distinguished by their jointed limbs and cuticle made of chiti ...
s have an open circulatory system
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, t ...
. Diploblast
Eumetazoa (), also known as diploblasts, Epitheliozoa, or Histozoa, are a proposed basal animal clade as a sister group of the Porifera (sponges). The basal eumetazoan clades are the Ctenophora and the ParaHoxozoa. Placozoa is now also seen ...
s such as sponges
Sponges, the members of the phylum Porifera (; meaning 'pore bearer'), are a basal animal clade as a sister of the diploblasts. They are multicellular organisms that have bodies full of pores and channels allowing water to circulate through t ...
, and comb jellies
Ctenophora (; ctenophore ; ) comprise a phylum of marine invertebrates, commonly known as comb jellies, that inhabit sea waters worldwide. They are notable for the groups of cilia they use for swimming (commonly referred to as "combs"), and ...
lack a circulatory system.
Blood is a fluid
In physics, a fluid is a liquid, gas, or other material that continuously deforms (''flows'') under an applied shear stress, or external force. They have zero shear modulus, or, in simpler terms, are substances which cannot resist any shear ...
consisting of plasma, red blood cell
Red blood cells (RBCs), also referred to as red cells, red blood corpuscles (in humans or other animals not having nucleus in red blood cells), haematids, erythroid cells or erythrocytes (from Greek ''erythros'' for "red" and ''kytos'' for "hol ...
s, white blood cell
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mult ...
s, and platelets
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby ...
that is circulated around the body carrying oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements ...
and nutrient
A nutrient is a substance used by an organism to survive, grow, and reproduce. The requirement for dietary nutrient intake applies to animals, plants, fungi, and protists. Nutrients can be incorporated into cells for metabolic purposes or excre ...
s to the tissues, and waste materials away. Circulated nutrients include proteins
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, respo ...
and minerals
In geology and mineralogy, a mineral or mineral species is, broadly speaking, a solid chemical compound with a fairly well-defined chemical composition and a specific crystal structure that occurs naturally in pure form.John P. Rafferty, ed ...
, other components transported are gases such as oxygen, and carbon dioxide
Carbon dioxide ( chemical formula ) is a chemical compound made up of molecules that each have one carbon atom covalently double bonded to two oxygen atoms. It is found in the gas state at room temperature. In the air, carbon dioxide is t ...
, hormone
A hormone (from the Greek participle , "setting in motion") is a class of signaling molecules in multicellular organisms that are sent to distant organs by complex biological processes to regulate physiology and behavior. Hormones are required ...
s, and hemoglobin
Hemoglobin (haemoglobin BrE) (from the Greek word αἷμα, ''haîma'' 'blood' + Latin ''globus'' 'ball, sphere' + ''-in'') (), abbreviated Hb or Hgb, is the iron-containing oxygen-transport metalloprotein present in red blood cells (erythroc ...
; providing nourishment, help in the immune system
The immune system is a network of biological processes that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to parasitic worms, as well as cancer cells and objects such as wood splinte ...
to fight diseases
A disease is a particular abnormal condition that negatively affects the structure or function of all or part of an organism, and that is not immediately due to any external injury. Diseases are often known to be medical conditions that a ...
, and in maintaining homeostasis
In biology, homeostasis ( British also homoeostasis) (/hɒmɪə(ʊ)ˈsteɪsɪs/) is the state of steady internal, physical, and chemical conditions maintained by living systems. This is the condition of optimal functioning for the organism and ...
by stabilizing temperature and natural pH.
In vertebrates, complementary to the circulatory system is the lymphatic system
The lymphatic system, or lymphoid system, is an organ system in vertebrates that is part of the immune system, and complementary to the circulatory system. It consists of a large network of lymphatic vessels, lymph nodes, lymphatic or lymphoid ...
. This system carries excess plasma filtered from the capillaries
A capillary is a small blood vessel from 5 to 10 micrometres (μm) in diameter. Capillaries are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the smallest blood vessels in the body: ...
as interstitial fluid between cells, away from the body tissues in an accessory route to return the excess fluid back to the blood circulation as lymph
Lymph (from Latin, , meaning "water") is the fluid that flows through the lymphatic system, a system composed of lymph vessels (channels) and intervening lymph nodes whose function, like the venous system, is to return fluid from the tissues ...
. The passage of lymph takes much longer than that of blood. The lymphatic system is a subsystem that is essential for the functioning of the blood circulatory system; without it the blood would become depleted of fluid. The lymphatic system works together with the immune system. Unlike the closed circulatory system, the lymphatic system is an open system. Some sources describe it as a ''secondary circulatory system''.
The circulatory system can be affected by many cardiovascular disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, hea ...
s. Cardiologist
Cardiology () is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular ...
s are medical professionals which specialise in the heart, and cardiothoracic surgeon
Cardiothoracic surgery is the field of medicine involved in surgical treatment of organs inside the thoracic cavity — generally treatment of conditions of the heart (heart disease), lungs (lung disease), and other pleural or mediastinal stru ...
s specialise in operating on the heart and its surrounding areas. Vascular surgeon
Vascular surgery is a surgical subspecialty in which diseases of the vascular system, or arteries, veins and lymphatic circulation, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty ...
s focus on disorders of the blood vessels, and lymphatic vessels.
Structure
 The circulatory system includes the
The circulatory system includes the heart
The heart is a muscular Organ (biology), organ in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as ca ...
, blood vessel
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide awa ...
s, and blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the cir ...
. The cardiovascular system in all vertebrates, consists of the heart and blood vessels. The circulatory system is further divided into two major circuits – a pulmonary circulation, and a systemic circulation
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, t ...
. The pulmonary circulation is a circuit loop from the right heart taking deoxygenated blood to the lung
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of ...
s where it is oxygenated and returned to the left heart. The systemic circulation is a circuit loop that delivers oxygenated blood from the left heart to the rest of the body, and returns deoxygenated blood back to the right heart via large veins known as the venae cavae
In anatomy, the venae cavae (; singular: vena cava ; ) are two large veins (great vessels) that return deoxygenated blood from the body into the heart. In humans they are the superior vena cava and the inferior vena cava, and both empty into th ...
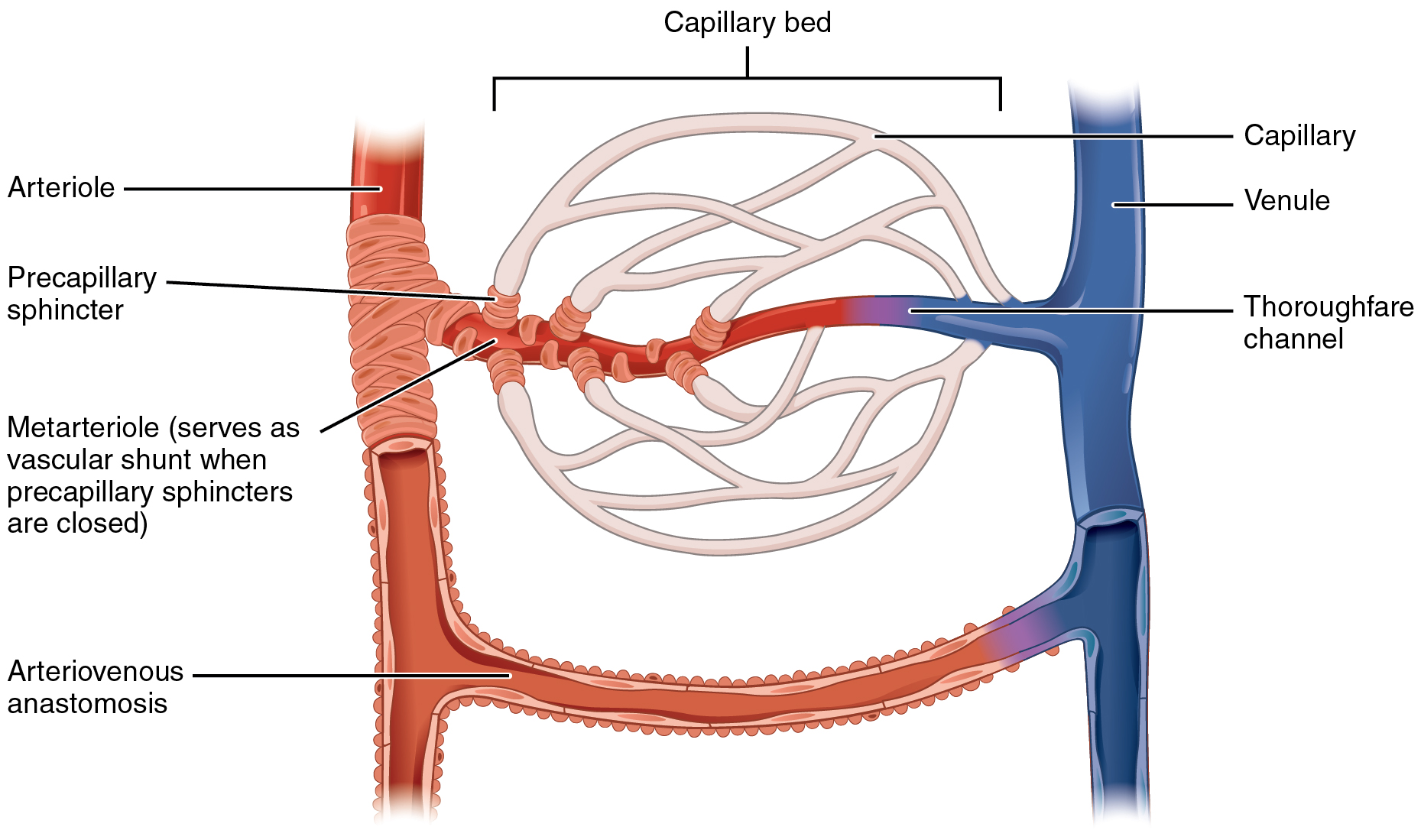
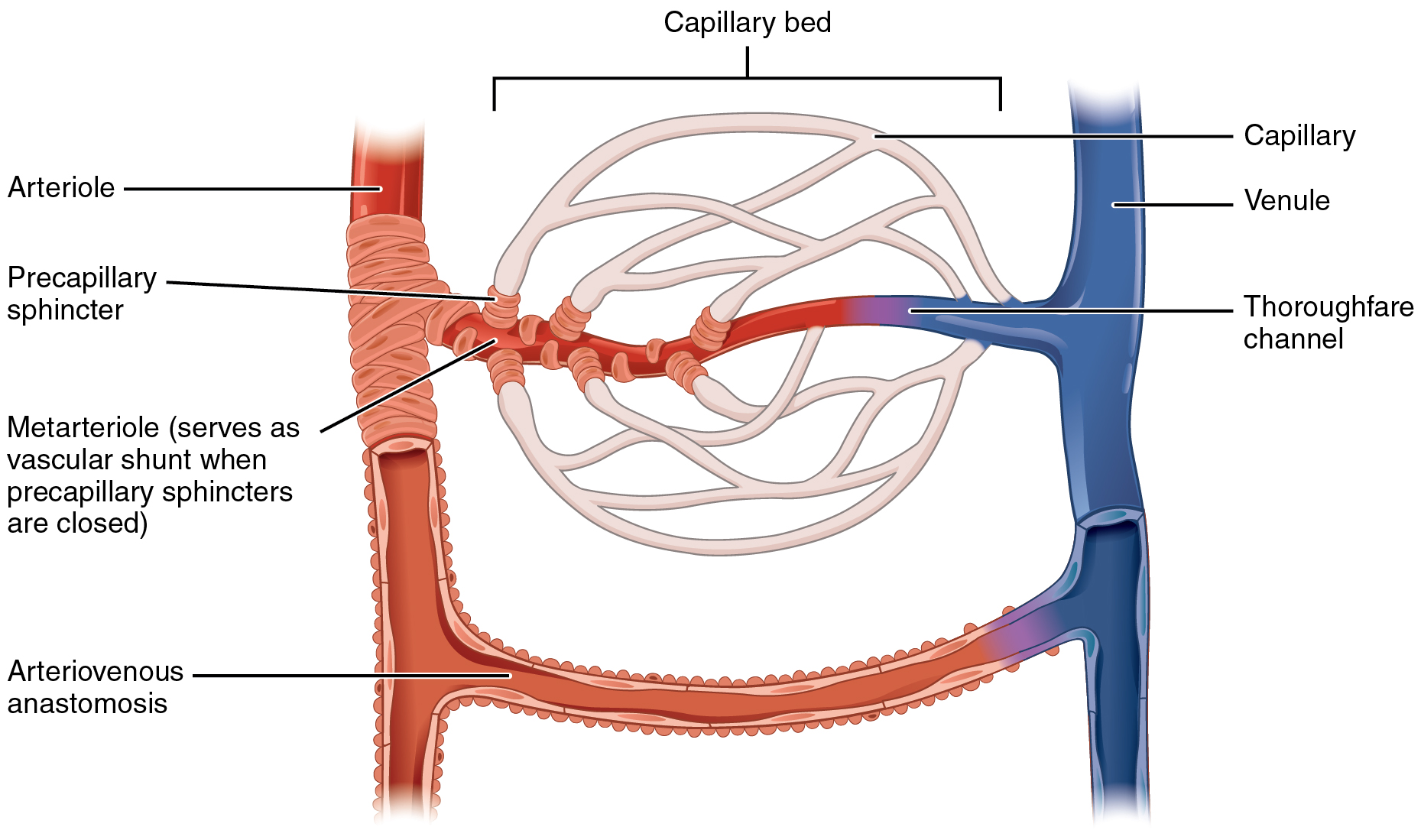
. The systemic circulation can also be defined as two parts – a ''macrocirculation'' and a ''microcirculation
The microcirculation is the circulation of the blood in the smallest blood vessels, the microvessels of the microvasculature present within organ tissues. The microvessels include terminal arterioles, metarterioles, capillaries, and venules. ...
''. An average adult contains five to six quarts (roughly 4.7 to 5.7 liters) of blood, accounting for approximately 7% of their total body weight. Blood consists of plasma, red blood cells
Red blood cells (RBCs), also referred to as red cells, red blood corpuscles (in humans or other animals not having nucleus in red blood cells), haematids, erythroid cells or erythrocytes (from Greek ''erythros'' for "red" and ''kytos'' for "hol ...
, white blood cells
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mult ...
, and platelets
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby ...
. The digestive system
The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion (the tongue, salivary glands, pancreas, liver, and gallbladder). Digestion involves the breakdown of food into smaller and smaller compone ...
also works with the circulatory system to provide the nutrients the system needs to keep the heart
The heart is a muscular Organ (biology), organ in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as ca ...
pumping.
Further circulatory routes are associated, such as the coronary circulation
Coronary circulation is the circulation of blood in the blood vessels that supply the heart muscle (myocardium).
Coronary arteries supply oxygenated blood to the heart muscle. Cardiac veins then drain away the blood after it has been deoxygen ...
to the heart itself, the cerebral circulation to the brain
A brain is an organ (biology), organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. It is located in the head, usually close to the sensory organs for senses such as Visual perception, vision. I ...
, renal circulation
The renal circulation supplies the blood to the kidneys via the renal arteries, left and right, which branch directly from the abdominal aorta. Despite their relatively small size, the kidneys receive approximately 20% of the cardiac output.
Each ...
to the kidney
The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about in length. They receive blood from the paired renal arteries; blo ...
s, and bronchial circulation to the bronchi in the lungs.
The human circulatory system is closed
Closed may refer to:
Mathematics
* Closure (mathematics), a set, along with operations, for which applying those operations on members always results in a member of the set
* Closed set, a set which contains all its limit points
* Closed interval, ...
, meaning that the blood is contained within the vascular network. Nutrients travel through tiny blood vessels of the microcirculation to reach organs. The lymphatic system
The lymphatic system, or lymphoid system, is an organ system in vertebrates that is part of the immune system, and complementary to the circulatory system. It consists of a large network of lymphatic vessels, lymph nodes, lymphatic or lymphoid ...
is an essential subsystem of the circulatory system consisting of a network of lymphatic vessel
The lymphatic vessels (or lymph vessels or lymphatics) are thin-walled vessels (tubes), structured like blood vessels, that carry lymph. As part of the lymphatic system, lymph vessels are complementary to the cardiovascular system. Lymph ves ...
s, lymph nodes
A lymph node, or lymph gland, is a kidney-shaped organ of the lymphatic system and the adaptive immune system. A large number of lymph nodes are linked throughout the body by the lymphatic vessels. They are major sites of lymphocytes that includ ...
, organs, tissues and circulating lymph
Lymph (from Latin, , meaning "water") is the fluid that flows through the lymphatic system, a system composed of lymph vessels (channels) and intervening lymph nodes whose function, like the venous system, is to return fluid from the tissues ...
. This subsystem is an open system. A major function is to carry the lymph, draining and returning interstitial fluid into the lymphatic duct
A lymph duct is a great lymphatic vessel that empties lymph into one of the subclavian veins. There are two lymph ducts in the body—the right lymphatic duct and the thoracic duct. The right lymphatic duct drains lymph from the right upper li ...
s back to the heart for return to the circulatory system. Another major function is working together with the immune system
The immune system is a network of biological processes that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to parasitic worms, as well as cancer cells and objects such as wood splinte ...
to provide defense against pathogen
In biology, a pathogen ( el, πάθος, "suffering", "passion" and , "producer of") in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a g ...
s.
Heart
nutrient
A nutrient is a substance used by an organism to survive, grow, and reproduce. The requirement for dietary nutrient intake applies to animals, plants, fungi, and protists. Nutrients can be incorporated into cells for metabolic purposes or excre ...
s and oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements ...
to every cell, and removing waste products. The left heart pumps oxygenated blood returned from the lungs to the rest of the body in the systemic circulation
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, t ...
. The right heart pumps deoxygenated blood to the lungs in the pulmonary circulation. In the human heart there is one atrium and one ventricle for each circulation, and with both a systemic and a pulmonary circulation there are four chambers in total: left atrium, left ventricle
A ventricle is one of two large chambers toward the bottom of the heart that collect and expel blood towards the peripheral beds within the body and lungs. The blood pumped by a ventricle is supplied by an atrium, an adjacent chamber in the uppe ...
, right atrium and right ventricle
A ventricle is one of two large chambers toward the bottom of the heart that collect and expel blood towards the peripheral beds within the body and lungs. The blood pumped by a ventricle is supplied by an atrium, an adjacent chamber in the uppe ...
. The right atrium is the upper chamber of the right side of the heart. The blood that is returned to the right atrium is deoxygenated (poor in oxygen) and passed into the right ventricle to be pumped through the pulmonary artery to the lungs for re-oxygenation and removal of carbon dioxide. The left atrium receives newly oxygenated blood from the lungs as well as the pulmonary vein which is passed into the strong left ventricle to be pumped through the aorta to the different organs of the body.
Pulmonary circulation
 The pulmonary circulation is the portion of the cardiovascular system in which
The pulmonary circulation is the portion of the cardiovascular system in which oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements ...
-depleted blood is pumped away from the heart, via the pulmonary artery, to the lungs
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either si ...
and returned, oxygenated, to the heart via the pulmonary vein.
Oxygen-deprived blood from the superior and inferior vena cava
In anatomy, the venae cavae (; singular: vena cava ; ) are two large veins (great vessels) that return deoxygenated blood from the body into the heart. In humans they are the superior vena cava and the inferior vena cava, and both empty into th ...
enters the right atrium of the heart and flows through the tricuspid valve (right atrioventricular valve) into the right ventricle, from which it is then pumped through the pulmonary semilunar valve
The pulmonary valve (sometimes referred to as the pulmonic valve) is a valve of the heart that lies between the right ventricle and the pulmonary artery and has three cusps. It is one of the four valves of the heart and one of the two semilunar v ...
into the pulmonary artery to the lungs. Gas exchange
Gas exchange is the physical process by which gases move passively by diffusion across a surface. For example, this surface might be the air/water interface of a water body, the surface of a gas bubble in a liquid, a gas-permeable membrane, or a ...
occurs in the lungs, whereby is released from the blood, and oxygen is absorbed. The pulmonary vein returns the now oxygen-rich blood to the left atrium.
A separate system known as the bronchial circulation supplies blood to the tissue of the larger airways of the lung.
Systemic circulation
 The systemic circulation is a circuit loop that delivers oxygenated blood from the left heart to the rest of the body through the
The systemic circulation is a circuit loop that delivers oxygenated blood from the left heart to the rest of the body through the aorta
The aorta ( ) is the main and largest artery in the human body, originating from the left ventricle of the heart and extending down to the abdomen, where it splits into two smaller arteries (the common iliac arteries). The aorta distributes o ...
. Deoxygenated blood is returned in the systemic circulation to the right heart via two large veins, the inferior vena cava and superior vena cava, where it is pumped from the right atrium into the pulmonary circulation for oxygenation. The systemic circulation can also be defined as having two parts – a macrocirculation and a microcirculation
The microcirculation is the circulation of the blood in the smallest blood vessels, the microvessels of the microvasculature present within organ tissues. The microvessels include terminal arterioles, metarterioles, capillaries, and venules. ...
.
Blood vessels
Theblood vessel
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide awa ...
s of the circulatory system are the arteries
An artery (plural arteries) () is a blood vessel in humans and most animals that takes blood away from the heart to one or more parts of the body (tissues, lungs, brain etc.). Most arteries carry oxygenated blood; the two exceptions are the pu ...
, veins
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated ...
, and capillaries
A capillary is a small blood vessel from 5 to 10 micrometres (μm) in diameter. Capillaries are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the smallest blood vessels in the body: ...
. The large arteries and veins that take blood to, and away from the heart are known as the great vessels.
Arteries
 Oxygenated blood enters the systemic circulation when leaving the left ventricle, via the aortic semilunar valve. The first part of the systemic circulation is the aorta, a massive and thick-walled artery. The aorta arches and gives branches supplying the upper part of the body after passing through the aortic opening of the diaphragm at the level of thoracic ten vertebra, it enters the abdomen. Later, it descends down and supplies branches to abdomen, pelvis, perineum and the lower limbs.
The walls of the aorta are elastic. This elasticity helps to maintain the
Oxygenated blood enters the systemic circulation when leaving the left ventricle, via the aortic semilunar valve. The first part of the systemic circulation is the aorta, a massive and thick-walled artery. The aorta arches and gives branches supplying the upper part of the body after passing through the aortic opening of the diaphragm at the level of thoracic ten vertebra, it enters the abdomen. Later, it descends down and supplies branches to abdomen, pelvis, perineum and the lower limbs.
The walls of the aorta are elastic. This elasticity helps to maintain the blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure ...
throughout the body. When the aorta receives almost five litres of blood from the heart, it recoils and is responsible for pulsating blood pressure. As the aorta branches into smaller arteries, their elasticity goes on decreasing and their compliance goes on increasing.
Capillaries
Arteries branch into small passages called arterioles and then into thecapillaries
A capillary is a small blood vessel from 5 to 10 micrometres (μm) in diameter. Capillaries are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the smallest blood vessels in the body: ...
. The capillaries merge to bring blood into the venous system.
Veins
Capillaries merge intovenule
A venule is a very small blood vessel in the microcirculation that allows blood to return from the capillary beds to drain into the larger blood vessels, the veins. Venules range from 7μm to 1mm in diameter. Veins contain approximately 70% of ...
s, which merge into veins. The venous system
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated ...
feeds into the two major veins: the superior vena cava – which mainly drains tissues above the heart – and the inferior vena cava – which mainly drains tissues below the heart. These two large veins empty into the right atrium of the heart.
Portal veins
The general rule is that arteries from the heart branch out into capillaries, which collect into veins leading back to the heart. Portal veins are a slight exception to this. In humans the only significant example is thehepatic portal vein
The portal vein or hepatic portal vein (HPV) is a blood vessel that carries blood from the gastrointestinal tract, gallbladder, pancreas and spleen to the liver. This blood contains nutrients and toxins extracted from digested contents. Appr ...
which combines from capillaries around the gastrointestinal tract
The gastrointestinal tract (GI tract, digestive tract, alimentary canal) is the tract or passageway of the digestive system that leads from the mouth to the anus. The GI tract contains all the major organs of the digestive system, in humans and ...
where the blood absorbs the various products of digestion; rather than leading directly back to the heart, the hepatic portal vein branches into a second capillary system in the liver
The liver is a major organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the synthesis of proteins and biochemicals necessary for digestion and growth. In humans, it i ...
.
Coronary circulation
The heart itself is supplied with oxygen and nutrients through a small "loop" of the systemic circulation and derives very little from the blood contained within the four chambers. The coronary circulation system provides a blood supply to the heart muscle itself. The coronary circulation begins near the origin of the aorta by twocoronary arteries
The coronary arteries are the arterial blood vessels of coronary circulation, which transport oxygenated blood to the heart muscle. The heart requires a continuous supply of oxygen to function and survive, much like any other tissue or organ ...
: the right coronary artery and the left coronary artery. After nourishing the heart muscle, blood returns through the coronary veins into the coronary sinus
In anatomy, the coronary sinus () is a collection of veins joined together to form a large vessel that collects blood from the heart muscle (myocardium). It delivers deoxygenated blood to the right atrium, as do the superior and inferior vena ...
and from this one into the right atrium. Backflow of blood through its opening during atrial systole
The cardiac cycle is the performance of the human heart from the beginning of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, followin ...
is prevented by the Thebesian valve
In the anatomy of the heart, the valve of the coronary sinus (also called the Thebesian valve, after Adam Christian Thebesius) is a semicircular fold of the lining membrane of the right atrium, at the orifice of the coronary sinus. It is situat ...
. The smallest cardiac veins drain directly into the heart chambers.
Cerebral circulation
The brain has a dual blood supply, an ''anterior'' and a ''posterior circulation'' from arteries at its front and back. The anterior circulation arises from the internal carotid arteries to supply the front of the brain. The posterior circulation arises from the vertebral arteries, to supply the back of the brain andbrainstem
The brainstem (or brain stem) is the posterior stalk-like part of the brain that connects the cerebrum with the spinal cord. In the human brain the brainstem is composed of the midbrain, the pons, and the medulla oblongata. The midbrain is ...
. The circulation from the front and the back join ( anastomise) at the circle of Willis
The circle of Willis (also called Willis' circle, loop of Willis, cerebral arterial circle, and Willis polygon) is a circulatory anastomosis that supplies blood to the brain and surrounding structures in reptiles, birds and mammals, including hu ...
.
Renal circulation
Therenal circulation
The renal circulation supplies the blood to the kidneys via the renal arteries, left and right, which branch directly from the abdominal aorta. Despite their relatively small size, the kidneys receive approximately 20% of the cardiac output.
Each ...
is the blood supply to the kidney
The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about in length. They receive blood from the paired renal arteries; blo ...
s, contains many specialized blood vessels and receives around 20% of the cardiac output. It branches from the abdominal aorta
In human anatomy, the abdominal aorta is the largest artery in the abdominal cavity. As part of the aorta, it is a direct continuation of the descending aorta (of the thorax).
Structure
The abdominal aorta begins at the level of the diaphr ...
and returns blood to the ascending vena cava
In anatomy, the venae cavae (; singular: vena cava ; ) are two large veins (great vessels) that return deoxygenated blood from the body into the heart. In humans they are the superior vena cava and the inferior vena cava, and both empty into th ...
.
Development
The development of the circulatory system starts withvasculogenesis
Vasculogenesis is the process of blood vessel formation, occurring by a '' de novo'' production of endothelial cells. It is sometimes paired with angiogenesis, as the first stage of the formation of the vascular network, closely followed by an ...
in the embryo
An embryo is an initial stage of development of a multicellular organism. In organisms that reproduce sexually, embryonic development is the part of the life cycle that begins just after fertilization of the female egg cell by the male spe ...
. The human arterial and venous systems develop from different areas in the embryo. The arterial system develops mainly from the aortic arches, six pairs of arches that develop on the upper part of the embryo. The venous system arises from three bilateral veins during weeks 4 – 8 of embryogenesis
An embryo is an initial stage of development of a multicellular organism. In organisms that reproduce sexually, embryonic development is the part of the life cycle that begins just after fertilization of the female egg cell by the male spe ...
. Fetal circulation begins within the 8th week of development. Fetal circulation does not include the lungs, which are bypassed via the truncus arteriosus. Before birth the fetus
A fetus or foetus (; plural fetuses, feti, foetuses, or foeti) is the unborn offspring that develops from an animal embryo. Following embryonic development the fetal stage of development takes place. In human prenatal development, fetal dev ...
obtains oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements ...
(and nutrient
A nutrient is a substance used by an organism to survive, grow, and reproduce. The requirement for dietary nutrient intake applies to animals, plants, fungi, and protists. Nutrients can be incorporated into cells for metabolic purposes or excre ...
s) from the mother through the placenta
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate mate ...
and the umbilical cord.
Arteries
 The human arterial system originates from the aortic arches and from the dorsal aortae starting from week 4 of embryonic life. The first and second aortic arches regress and form only the maxillary arteries and stapedial arteries respectively. The arterial system itself arises from aortic arches 3, 4 and 6 (aortic arch 5 completely regresses).
The dorsal aortae, present on the dorsal side of the embryo, are initially present on both sides of the embryo. They later fuse to form the basis for the aorta itself. Approximately thirty smaller arteries branch from this at the back and sides. These branches form the
The human arterial system originates from the aortic arches and from the dorsal aortae starting from week 4 of embryonic life. The first and second aortic arches regress and form only the maxillary arteries and stapedial arteries respectively. The arterial system itself arises from aortic arches 3, 4 and 6 (aortic arch 5 completely regresses).
The dorsal aortae, present on the dorsal side of the embryo, are initially present on both sides of the embryo. They later fuse to form the basis for the aorta itself. Approximately thirty smaller arteries branch from this at the back and sides. These branches form the intercostal arteries
The intercostal arteries are a group of arteries that supply the area between the ribs ("costae"), called the intercostal space. The highest intercostal artery (supreme intercostal artery or superior intercostal artery) is an artery in the hu ...
, arteries of the arms and legs, lumbar arteries and the lateral sacral arteries. Branches to the sides of the aorta will form the definitive renal
The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about in length. They receive blood from the paired renal arteries; bloo ...
, suprarenal and gonadal arteries. Finally, branches at the front of the aorta consist of the vitelline arteries and umbilical arteries
The umbilical artery is a paired artery (with one for each half of the body) that is found in the abdominal and pelvic regions. In the fetus, it extends into the umbilical cord.
Structure Development
The umbilical arteries supply deoxygenated ...
. The vitelline arteries form the celiac, superior
Superior may refer to:
*Superior (hierarchy), something which is higher in a hierarchical structure of any kind
Places
*Superior (proposed U.S. state), an unsuccessful proposal for the Upper Peninsula of Michigan to form a separate state
*Lake ...
and inferior mesenteric arteries of the gastrointestinal tract. After birth, the umbilical arteries will form the internal iliac arteries.
Veins
The human venous system develops mainly from the vitelline veins, the umbilical veins and the cardinal veins, all of which empty into thesinus venosus
The sinus venosus is a large quadrangular cavity which precedes the atrium on the venous side of the chordate heart. In mammals, it exists distinctly only in the embryonic heart, where it is found between the two venae cavae. However, the sinus v ...
.
Function
About 98.5% of the oxygen in a sample of arterial blood in a healthy human, breathing air at sea-level pressure, is chemically combined withhemoglobin
Hemoglobin (haemoglobin BrE) (from the Greek word αἷμα, ''haîma'' 'blood' + Latin ''globus'' 'ball, sphere' + ''-in'') (), abbreviated Hb or Hgb, is the iron-containing oxygen-transport metalloprotein present in red blood cells (erythroc ...
molecules. About 1.5% is physically dissolved in the other blood liquids and not connected to hemoglobin. The hemoglobin molecule is the primary transporter of oxygen in vertebrates.
Clinical significance
Many diseases affect the circulatory system. These include a number ofcardiovascular disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, hea ...
s, affecting the heart and blood vessels; hematologic diseases that affect the blood, such as anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
, and lymphatic disease
Lymphatic disease is a class of disorders which directly affect the components of the lymphatic system.
Examples include Castleman's disease and lymphedema.
__TOC__ Types
Diseases and disorder
Hodgkin's Disease/Hodgkin's Lymphoma
Hodgkin lymphoma ...
s affecting the lymphatic system. Cardiologist
Cardiology () is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular ...
s are medical professionals which specialise in the heart, and cardiothoracic surgeon
Cardiothoracic surgery is the field of medicine involved in surgical treatment of organs inside the thoracic cavity — generally treatment of conditions of the heart (heart disease), lungs (lung disease), and other pleural or mediastinal stru ...
s specialise in operating on the heart and its surrounding areas. Vascular surgeon
Vascular surgery is a surgical subspecialty in which diseases of the vascular system, or arteries, veins and lymphatic circulation, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty ...
s focus on the blood vessels.
Cardiovascular disease
Diseases affecting the cardiovascular system are called ''cardiovascular disease''. Many of these diseases are called "lifestyle disease
Lifestyle diseases can be defined as diseases linked with one's lifestyle. These diseases are non-communicable diseases. They are caused by lack of physical activity , unhealthy eating, alcohol, substance use disorders and smoking tobacco, wh ...
s" because they develop over time and are related to a person's exercise habits, diet, whether they smoke, and other lifestyle choices a person makes. Atherosclerosis
Atherosclerosis is a pattern of the disease arteriosclerosis in which the wall of the artery develops abnormalities, called lesions. These lesions may lead to narrowing due to the buildup of atheromatous plaque. At onset there are usually no s ...
is the precursor to many of these diseases. It is where small atheromatous plaques
An atheroma, or atheromatous plaque, is an abnormal and reversible accumulation of material in the inner layer of an arterial wall.
The material consists of mostly macrophage cells, or debris, containing lipids, calcium and a variable amount o ...
build up in the walls of medium and large arteries. This may eventually grow or rupture to occlude the arteries. It is also a risk factor for acute coronary syndrome
Acute coronary syndrome (ACS) is a syndrome (a set of signs and symptoms) due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally l ...
s, which are diseases that are characterised by a sudden deficit of oxygenated blood to the heart tissue. Atherosclerosis is also associated with problems such as aneurysm
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus ( ...
formation or splitting ("dissection") of arteries.
Another major cardiovascular disease involves the creation of a clot, called a "thrombus". These can originate in veins or arteries. Deep venous thrombosis
Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enla ...
, which mostly occurs in the legs, is one cause of clots in the veins of the legs, particularly when a person has been stationary for a long time. These clots may embolise, meaning travel to another location in the body. The results of this may include pulmonary embolus, transient ischaemic attack
A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of ...
s, or stroke
A stroke is a disease, medical condition in which poor cerebral circulation, blood flow to the brain causes cell death. There are two main types of stroke: brain ischemia, ischemic, due to lack of blood flow, and intracranial hemorrhage, hemorr ...
.
Cardiovascular diseases may also be congenital in nature, such as heart defects or persistent fetal circulation, where the circulatory changes that are supposed to happen after birth do not. Not all congenital changes to the circulatory system are associated with diseases, a large number are anatomical variation
An anatomical variation, anatomical variant, or anatomical variability is a presentation of body structure with morphological features different from those that are typically described in the majority of individuals. Anatomical variations are categ ...
s.
Investigations
 The function and health of the circulatory system and its parts are measured in a variety of manual and automated ways. These include simple methods such as those that are part of the
The function and health of the circulatory system and its parts are measured in a variety of manual and automated ways. These include simple methods such as those that are part of the cardiovascular examination
The cardiovascular examination is a portion of the physical examination that involves evaluation of the cardiovascular system. The exact contents of the examination will vary depending on the presenting complaint but a complete examination will i ...
, including the taking of a person's pulse as an indicator of a person's heart rate, the taking of blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure ...
through a sphygmomanometer or the use of a stethoscope
The stethoscope is a medical device for auscultation, or listening to internal sounds of an animal or human body. It typically has a small disc-shaped resonator that is placed against the skin, and one or two tubes connected to two earpieces. ...
to listen to the heart for murmurs which may indicate problems with the heart's valves. An electrocardiogram can also be used to evaluate the way in which electricity is conducted through the heart.
Other more invasive means can also be used. A cannula or catheter
In medicine, a catheter (/ˈkæθətər/) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgi ...
inserted into an artery may be used to measure pulse pressure or pulmonary wedge pressures. Angiography, which involves injecting a dye into an artery to visualise an arterial tree, can be used in the heart (coronary angiography Coronary () may, as shorthand in English, be used to mean:
* Coronary circulation, the system of arteries and veins in mammals
** Coronary artery disease
**Coronary occlusion
** A myocardial infarction, a heart attack
As adjective
* Referring to t ...
) or brain. At the same time as the arteries are visualised, blockages or narrowings may be fixed through the insertion of stent
In medicine, a stent is a metal or plastic tube inserted into the lumen of an anatomic vessel or duct to keep the passageway open, and stenting is the placement of a stent. A wide variety of stents are used for different purposes, from expandab ...
s, and active bleeds may be managed by the insertion of coils. An MRI may be used to image arteries, called an MRI angiogram. For evaluation of the blood supply to the lungs a CT pulmonary angiogram may be used. Vascular ultrasonography may be used to investigate vascular disease
Vascular disease is a class of diseases of the blood vessels – the arteries and veins of the circulatory system of the body. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood vessels can cause a ...
s affecting the venous system
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated ...
and the arterial system
An artery (plural arteries) () is a blood vessel in humans and most animals that takes blood away from the heart to one or more parts of the body (tissues, lungs, brain etc.). Most arteries carry oxygenated blood; the two exceptions are the pul ...
including the diagnosis of stenosis
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
, thrombosis
Thrombosis (from Ancient Greek "clotting") is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel (a vein or an artery) is injured, the body uses platelets (th ...
or venous insufficiency. An intravascular ultrasound
Intravascular ultrasound (IVUS) or intravascular echocardiography is a medical imaging methodology using a specially designed catheter with a miniaturized ultrasound probe attached to the distal end of the catheter. The proximal end of the cathe ...
using a catheter
In medicine, a catheter (/ˈkæθətər/) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgi ...
is also an option.
Surgery
There are a number of surgical procedures performed on the circulatory system: *Coronary artery bypass surgery
Coronary artery bypass surgery, also known as coronary artery bypass graft (CABG, pronounced "cabbage") is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pai ...
* Coronary stent used in angioplasty
Angioplasty, is also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atheroscle ...
* Vascular surgery
Vascular surgery is a surgical subspecialty in which diseases of the vascular system, or arteries, veins and lymphatic circulation, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialt ...
* Vein stripping
* Cosmetic procedures
Cardiovascular procedures are more likely to be performed in an inpatient setting than in an ambulatory care setting; in the United States, only 28% of cardiovascular surgeries were performed in the ambulatory care setting.
Other animals
 While humans, as well as other
While humans, as well as other vertebrates
Vertebrates () comprise all animal taxa within the subphylum Vertebrata () (chordates with backbones), including all mammals, birds, reptiles, amphibians, and fish. Vertebrates represent the overwhelming majority of the phylum Chordata, with ...
, have a closed blood circulatory system (meaning that the blood never leaves the network of arteries, veins and capillaries), some invertebrate
Invertebrates are a paraphyletic group of animals that neither possess nor develop a vertebral column (commonly known as a ''backbone'' or ''spine''), derived from the notochord. This is a grouping including all animals apart from the chorda ...
groups have an open circulatory system containing a heart but limited blood vessels. The most primitive, diploblastic
Diploblasty is a condition of the blastula in which there are two primary germ layers: the ectoderm and endoderm.
Diploblastic organisms are organisms which develop from such a blastula, and include cnidaria and ctenophora, formerly grouped togeth ...
animal phyla Phyla, the plural of ''phylum'', may refer to:
* Phylum, a biological taxon between Kingdom and Class
* by analogy, in linguistics, a large division of possibly related languages, or a major language family which is not subordinate to another
Phy ...
lack circulatory systems.
An additional transport system, the lymphatic system, which is only found in animals with a closed blood circulation, is an open system providing an accessory route for excess interstitial fluid to be returned to the blood.
The blood vascular system first appeared probably in an ancestor of the triploblasts
The Bilateria or bilaterians are animals with bilateral symmetry as an embryo, i.e. having a left and a right side that are mirror images of each other. This also means they have a head and a tail (anterior-posterior axis) as well as a belly and ...
over 600 million years ago, overcoming the time-distance constraints of diffusion, while endothelium
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the ve ...
evolved in an ancestral vertebrate some 540–510 million years ago.
Open circulatory system
Inarthropod
Arthropods (, (gen. ποδός)) are invertebrate animals with an exoskeleton, a segmented body, and paired jointed appendages. Arthropods form the phylum Arthropoda. They are distinguished by their jointed limbs and cuticle made of chiti ...
s, the open circulatory system is a system in which a fluid in a cavity called the hemocoel bathes the organs directly with oxygen and nutrients, with there being no distinction between blood and interstitial fluid; this combined fluid is called hemolymph
Hemolymph, or haemolymph, is a fluid, analogous to the blood in vertebrates, that circulates in the interior of the arthropod (invertebrate) body, remaining in direct contact with the animal's tissues. It is composed of a fluid plasma in which ...
or haemolymph. Muscular movements by the animal during locomotion can facilitate hemolymph movement, but diverting flow from one area to another is limited. When the heart relaxes, blood is drawn back toward the heart through open-ended pores (ostia).
Hemolymph fills all of the interior hemocoel of the body and surrounds all cells
Cell most often refers to:
* Cell (biology), the functional basic unit of life
Cell may also refer to:
Locations
* Monastic cell, a small room, hut, or cave in which a religious recluse lives, alternatively the small precursor of a monastery w ...
. Hemolymph is composed of water
Water (chemical formula ) is an inorganic, transparent, tasteless, odorless, and nearly colorless chemical substance, which is the main constituent of Earth's hydrosphere and the fluids of all known living organisms (in which it acts as ...
, inorganic
In chemistry, an inorganic compound is typically a chemical compound that lacks carbon–hydrogen bonds, that is, a compound that is not an organic compound. The study of inorganic compounds is a subfield of chemistry known as ''inorganic chemist ...
salts (mostly sodium
Sodium is a chemical element with the symbol Na (from Latin ''natrium'') and atomic number 11. It is a soft, silvery-white, highly reactive metal. Sodium is an alkali metal, being in group 1 of the periodic table. Its only stable ...
, chloride
The chloride ion is the anion (negatively charged ion) Cl−. It is formed when the element chlorine (a halogen) gains an electron or when a compound such as hydrogen chloride is dissolved in water or other polar solvents. Chloride s ...
, potassium
Potassium is the chemical element with the symbol K (from Neo-Latin '' kalium'') and atomic number19. Potassium is a silvery-white metal that is soft enough to be cut with a knife with little force. Potassium metal reacts rapidly with atmos ...
, magnesium
Magnesium is a chemical element with the symbol Mg and atomic number 12. It is a shiny gray metal having a low density, low melting point and high chemical reactivity. Like the other alkaline earth metals (group 2 of the periodic ...
, and calcium
Calcium is a chemical element with the symbol Ca and atomic number 20. As an alkaline earth metal, calcium is a reactive metal that forms a dark oxide-nitride layer when exposed to air. Its physical and chemical properties are most similar ...
), and organic compounds (mostly carbohydrates, protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, res ...
s, and lipid
Lipids are a broad group of naturally-occurring molecules which includes fats, waxes, sterols, fat-soluble vitamins (such as vitamins A, D, E and K), monoglycerides, diglycerides, phospholipids, and others. The functions of lipids in ...
s). The primary oxygen transporter molecule is hemocyanin.
There are free-floating cells, the hemocyte
A blood cell, also called a hematopoietic cell, hemocyte, or hematocyte, is a cell produced through hematopoiesis and found mainly in the blood. Major types of blood cells include red blood cells (erythrocytes), white blood cells (leukocytes) ...
s, within the hemolymph. They play a role in the arthropod immune system
The immune system is a network of biological processes that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to parasitic worms, as well as cancer cells and objects such as wood splinte ...
.

Closed circulatory system
annelid
The annelids (Annelida , from Latin ', "little ring"), also known as the segmented worms, are a large phylum, with over 22,000 extant species including ragworms, earthworms, and leeches. The species exist in and have adapted to various ecol ...
s (for example, earthworm
An earthworm is a terrestrial invertebrate that belongs to the phylum Annelida. They exhibit a tube-within-a-tube body plan; they are externally segmented with corresponding internal segmentation; and they usually have setae on all segments. T ...
s) and cephalopod
A cephalopod is any member of the molluscan class Cephalopoda ( Greek plural , ; "head-feet") such as a squid, octopus, cuttlefish, or nautilus. These exclusively marine animals are characterized by bilateral body symmetry, a prominent head ...
s (squid
True squid are molluscs with an elongated soft body, large eyes, eight arms, and two tentacles in the superorder Decapodiformes, though many other molluscs within the broader Neocoleoidea are also called squid despite not strictly fittin ...
s, octopus
An octopus ( : octopuses or octopodes, see below for variants) is a soft-bodied, eight- limbed mollusc of the order Octopoda (, ). The order consists of some 300 species and is grouped within the class Cephalopoda with squids, cuttlefish, ...
es and relatives) always keep their circulating blood enclosed within heart chambers or blood vessels and are classified as ''closed'', just as in humans. Still, the systems of fish
Fish are Aquatic animal, aquatic, craniate, gill-bearing animals that lack Limb (anatomy), limbs with Digit (anatomy), digits. Included in this definition are the living hagfish, lampreys, and Chondrichthyes, cartilaginous and bony fish as we ...
, amphibian
Amphibians are four-limbed and ectothermic vertebrates of the class Amphibia. All living amphibians belong to the group Lissamphibia. They inhabit a wide variety of habitats, with most species living within terrestrial, fossorial, arbo ...
s, reptile
Reptiles, as most commonly defined are the animals in the class Reptilia ( ), a paraphyletic grouping comprising all sauropsids except birds. Living reptiles comprise turtles, crocodilians, squamates ( lizards and snakes) and rhynchocephalia ...
s, and bird
Birds are a group of warm-blooded vertebrates constituting the class Aves (), characterised by feathers, toothless beaked jaws, the laying of hard-shelled eggs, a high metabolic rate, a four-chambered heart, and a strong yet lightweig ...
s show various stages of the evolution
Evolution is change in the heritable characteristics of biological populations over successive generations. These characteristics are the expressions of genes, which are passed on from parent to offspring during reproduction. Variation ...
of the circulatory system. Closed systems permit blood to be directed to the organs that require it.
In fish, the system has only one circuit, with the blood being pumped through the capillaries of the gill
A gill () is a respiratory organ that many aquatic organisms use to extract dissolved oxygen from water and to excrete carbon dioxide. The gills of some species, such as hermit crabs, have adapted to allow respiration on land provided they ar ...
s and on to the capillaries of the body tissues. This is known as ''single cycle'' circulation. The heart of fish is, therefore, only a single pump (consisting of two chambers).
In amphibians and most reptiles, a double circulatory system is used, but the heart is not always completely separated into two pumps. Amphibians have a three-chambered heart.
In reptiles, the ventricular septum of the heart is incomplete and the pulmonary artery is equipped with a sphincter muscle. This allows a second possible route of blood flow. Instead of blood flowing through the pulmonary artery to the lungs, the sphincter may be contracted to divert this blood flow through the incomplete ventricular septum into the left ventricle and out through the aorta
The aorta ( ) is the main and largest artery in the human body, originating from the left ventricle of the heart and extending down to the abdomen, where it splits into two smaller arteries (the common iliac arteries). The aorta distributes o ...
. This means the blood flows from the capillaries to the heart and back to the capillaries instead of to the lungs. This process is useful to ectothermic
An ectotherm (from the Greek () "outside" and () "heat") is an organism in which internal physiological sources of heat are of relatively small or of quite negligible importance in controlling body temperature.Davenport, John. Animal Life ...
(cold-blooded) animals in the regulation of their body temperature.
Mammals, birds and crocodilia
Crocodilia (or Crocodylia, both ) is an order of mostly large, predatory, semiaquatic reptiles, known as crocodilians. They first appeared 95 million years ago in the Late Cretaceous period ( Cenomanian stage) and are the closest livi ...
ns show complete separation of the heart into two pumps, for a total of four heart chambers; it is thought that the four-chambered heart of birds and crocodilians evolved independently from that of mammals. Double circulatory systems permit blood to be repressurized after returning from the lungs, speeding up delivery of oxygen to tissues.
No circulatory system
Circulatory systems are absent in some animals, includingflatworm
The flatworms, flat worms, Platyhelminthes, or platyhelminths (from the Greek πλατύ, ''platy'', meaning "flat" and ἕλμινς (root: ἑλμινθ-), ''helminth-'', meaning "worm") are a phylum of relatively simple bilaterian, unsegmen ...
s. Their body cavity
A body cavity is any space or compartment, or potential space, in an animal body. Cavities accommodate organs and other structures; cavities as potential spaces contain fluid.
The two largest human body cavities are the ventral body cavity, and ...
has no lining or enclosed fluid. Instead, a muscular pharynx
The pharynx (plural: pharynges) is the part of the throat behind the mouth and nasal cavity, and above the oesophagus and trachea (the tubes going down to the stomach and the lungs). It is found in vertebrates and invertebrates, though its st ...
leads to an extensively branched digestive system
The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion (the tongue, salivary glands, pancreas, liver, and gallbladder). Digestion involves the breakdown of food into smaller and smaller compone ...
that facilitates direct diffusion
Diffusion is the net movement of anything (for example, atoms, ions, molecules, energy) generally from a region of higher concentration to a region of lower concentration. Diffusion is driven by a gradient in Gibbs free energy or chemical ...
of nutrients to all cells. The flatworm's dorso-ventrally flattened body shape also restricts the distance of any cell from the digestive system or the exterior of the organism. Oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements ...
can diffuse from the surrounding water into the cells, and carbon dioxide can diffuse out. Consequently, every cell is able to obtain nutrients, water and oxygen without the need of a transport system.
Some animals, such as jellyfish
Jellyfish and sea jellies are the informal common names given to the medusa-phase of certain gelatinous members of the subphylum Medusozoa, a major part of the phylum Cnidaria. Jellyfish are mainly free-swimming marine animals with umbre ...
, have more extensive branching from their gastrovascular cavity (which functions as both a place of digestion and a form of circulation), this branching allows for bodily fluids to reach the outer layers, since the digestion begins in the inner layers.
History
papyrus
Papyrus ( ) is a material similar to thick paper that was used in ancient times as a writing surface. It was made from the pith of the papyrus plant, '' Cyperus papyrus'', a wetland sedge. ''Papyrus'' (plural: ''papyri'') can also refer to ...
, it acknowledges the connection of the heart to the arteries. The Egyptians thought air came in through the mouth and into the lungs and heart. From the heart, the air travelled to every member through the arteries. Although this concept of the circulatory system is only partially correct, it represents one of the earliest accounts of scientific thought.
In the 6th century BCE, the knowledge of circulation of vital fluids through the body was known to the Ayurvedic
Ayurveda () is an alternative medicine system with historical roots in the Indian subcontinent. The theory and practice of Ayurveda is pseudoscientific. Ayurveda is heavily practiced in India and Nepal, where around 80% of the population repo ...
physician Sushruta
Sushruta, or ''Suśruta'' (Sanskrit: सुश्रुत, IAST: , ) was an ancient Indian physician. The '' Sushruta Samhita'' (''Sushruta's Compendium''), a treatise ascribed to him, is one of the most important surviving ancient treatises o ...
in ancient India
According to consensus in modern genetics, anatomically modern humans first arrived on the Indian subcontinent from Africa between 73,000 and 55,000 years ago. Quote: "Y-Chromosome and Mt-DNA data support the colonization of South Asia by ...
. He also seems to have possessed knowledge of the arteries, described as 'channels' by Dwivedi & Dwivedi (2007).Dwivedi, Girish & Dwivedi, Shridhar (2007)"History of Medicine: Sushruta – the Clinician – Teacher par Excellence"
, ''Indian J Chest Dis Allied Sci'' Vol. 49 pp. 243–244, National Informatics Centre (Government of India). The valves of the heart were discovered by a physician of the Hippocratean school around the 4th century BCE. However, their function was not properly understood then. Because blood pools in the veins after death, arteries look empty. Ancient anatomists assumed they were filled with air and that they were for the transport of air. The Greek physician, Herophilus, distinguished veins from arteries but thought that the pulse was a property of arteries themselves. Greek anatomist Erasistratus observed that arteries that were cut during life bleed. He ascribed the fact to the phenomenon that air escaping from an artery is replaced with blood that enters between veins and arteries by very small vessels. Thus he apparently postulated capillaries but with reversed flow of blood. In 2nd-century AD
Rome
, established_title = Founded
, established_date = 753 BC
, founder = King Romulus ( legendary)
, image_map = Map of comune of Rome (metropolitan city of Capital Rome, region Lazio, Italy).svg
, map_caption ...
, the Greek physician Galen
Aelius Galenus or Claudius Galenus ( el, Κλαύδιος Γαληνός; September 129 – c. AD 216), often Anglicized as Galen () or Galen of Pergamon, was a Greek physician, surgeon and philosopher in the Roman Empire. Considered to be o ...
knew that blood vessels carried blood and identified venous (dark red) and arterial (brighter and thinner) blood, each with distinct and separate functions. Growth and energy were derived from venous blood created in the liver from chyle, while arterial blood gave vitality by containing pneuma (air) and originated in the heart. Blood flowed from both creating organs to all parts of the body where it was consumed and there was no return of blood to the heart or liver. The heart did not pump blood around, the heart's motion sucked blood in during diastole and the blood moved by the pulsation of the arteries themselves.
Galen believed that the arterial blood was created by venous blood passing from the left ventricle to the right by passing through 'pores' in the interventricular septum, air passed from the lungs via the pulmonary artery to the left side of the heart. As the arterial blood was created 'sooty' vapors were created and passed to the lungs also via the pulmonary artery to be exhaled.
In 1025, '' The Canon of Medicine'' by the Persian physician, Avicenna
Ibn Sina ( fa, ابن سینا; 980 – June 1037 CE), commonly known in the West as Avicenna (), was a Persian polymath who is regarded as one of the most significant physicians, astronomers, philosophers, and writers of the Islamic ...
, "erroneously accepted the Greek notion regarding the existence of a hole in the ventricular septum by which the blood traveled between the ventricles." Despite this, Avicenna "correctly wrote on the cardiac cycle
The cardiac cycle is the performance of the human heart from the beginning of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, followin ...
s and valvular function", and "had a vision of blood circulation" in his ''Treatise on Pulse''. While also refining Galen's erroneous theory of the pulse, Avicenna provided the first correct explanation of pulsation: "Every beat of the pulse comprises two movements and two pauses. Thus, expansion : pause : contraction : pause. ..The pulse is a movement in the heart and arteries ... which takes the form of alternate expansion and contraction."
In 1242, the Arabian physician, Ibn al-Nafis described the process of pulmonary circulation in greater, more accurate detail than his predecessors, though he believed, as they did, in the notion of vital spirit ( pneuma), which he believed was formed in the left ventricle. Ibn al-Nafis stated in his ''Commentary on Anatomy in Avicenna's Canon'':
...the blood from the right chamber of the heart must arrive at the left chamber but there is no direct pathway between them. The thick septum of the heart is not perforated and does not have visible pores as some people thought or invisible pores as Galen thought. The blood from the right chamber must flow through the vena arteriosa (pulmonary artery) to the lungs, spread through its substances, be mingled there with air, pass through the arteria venosa ( pulmonary vein) to reach the left chamber of the heart and there form the vital spirit...In addition, Ibn al-Nafis had an insight into what would become a larger theory of the
capillary
A capillary is a small blood vessel from 5 to 10 micrometres (μm) in diameter. Capillaries are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the smallest blood vessels in the bod ...
circulation. He stated that "there must be small communications or pores (''manafidh'' in Arabic) between the pulmonary artery and vein," a prediction that preceded the discovery of the capillary system by more than 400 years. Ibn al-Nafis' theory, however, was confined to blood transit in the lungs and did not extend to the entire body.
Michael Servetus
Michael Servetus (; es, Miguel Serveto as real name; french: Michel Servet; also known as ''Miguel Servet'', ''Miguel de Villanueva'', ''Revés'', or ''Michel de Villeneuve''; 29 September 1509 or 1511 – 27 October 1553) was a Spanish th ...
was the first European to describe the function of pulmonary circulation, although his achievement was not widely recognized at the time, for a few reasons. He firstly described it in the "Manuscript of Paris" (near 1546), but this work was never published. And later he published this description, but in a theological treatise, ''Christianismi Restitutio'', not in a book on medicine. Only three copies of the book survived but these remained hidden for decades, the rest were burned shortly after its publication in 1553 because of persecution of Servetus by religious authorities.
A better known discovery of pulmonary circulation was by Vesalius's successor at Padua
Padua ( ; it, Padova ; vec, Pàdova) is a city and ''comune'' in Veneto, northern Italy. Padua is on the river Bacchiglione, west of Venice. It is the capital of the province of Padua. It is also the economic and communications hub of the ...
, Realdo Colombo
Matteo Realdo Colombo (c. 1515 – 1559) was an Italian professor of anatomy and a surgeon at the University of Padua between 1544 and 1559.
Early life and education
Matteo Realdo Colombo or Realdus Columbus, was born in Cremona, Lombardy, the ...
, in 1559.
 Finally, the English physician
Finally, the English physician William Harvey
William Harvey (1 April 1578 – 3 June 1657) was an English physician who made influential contributions in anatomy and physiology. He was the first known physician to describe completely, and in detail, the systemic circulation and propert ...
, a pupil of Hieronymus Fabricius
Girolamo Fabrici d'Acquapendente, also known as Girolamo Fabrizio or Hieronymus Fabricius (20 May 1533 – 21 May 1619), was a pioneering anatomist and surgeon known in medical science as "The Father of Embryology."
Life and accomplishments ...
(who had earlier described the valves of the veins without recognizing their function), performed a sequence of experiments and published his ''Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus
''Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus'' (Latin, 'An Anatomical Exercise on the Motion of the Heart and Blood in Living Beings'), commonly called ''De Motu Cordis'', is the best-known work of the physician William Harv ...
'' in 1628, which "demonstrated that there had to be a direct connection between the venous and arterial systems throughout the body, and not just the lungs. Most importantly, he argued that the beat of the heart produced a continuous circulation of blood through minute connections at the extremities of the body. This is a conceptual leap that was quite different from Ibn al-Nafis' refinement of the anatomy and bloodflow in the heart and lungs." This work, with its essentially correct exposition, slowly convinced the medical world. However, Harvey was not able to identify the capillary system connecting arteries and veins; these were later discovered by Marcello Malpighi in 1661.
In 1956, André Frédéric Cournand
André Frédéric Cournand (September 24, 1895 – February 19, 1988) was a French-American physician and physiologist.
Biography
Cournand was awarded the Nobel Prize in Physiology or Medicine in 1956 along with Werner Forssmann and Dickinson W. ...
, Werner Forssmann
Werner Theodor Otto Forßmann (Forssmann in English; ; 29 August 1904 – 1 June 1979) was a German researcher and physician from Germany who shared the 1956 Nobel Prize in Medicine (with Andre Frederic Cournand and Dickinson W. Richards) for ...
and Dickinson W. Richards were awarded the Nobel Prize
The Nobel Prizes ( ; sv, Nobelpriset ; no, Nobelprisen ) are five separate prizes that, according to Alfred Nobel's will of 1895, are awarded to "those who, during the preceding year, have conferred the greatest benefit to humankind." Alfr ...
in Medicine "for their discoveries concerning heart catheterization
Cardiac catheterization (heart cath) is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.
A common example of cardiac catheterization is coronary catheterization that ...
and pathological changes in the circulatory system."
In his Nobel lecture, Forssmann credits Harvey as birthing cardiology with the publication of his book in 1628.
In the 1970s, Diana McSherry
Diana McSherry (born 1945) is an American computer scientist and biophysicist. She is known for her research in and development of computer-based systems to analyze heart function. Her system produced computer images of the circulation system and ...
developed computer-based systems to create images of the circulatory system and heart without the need for surgery.
See also
* * * * * * * *References
External links
Circulatory Pathways
in ''Anatomy and Physiology'' by
OpenStax
OpenStax (formerly OpenStax College) is a nonprofit educational technology initiative based at Rice University. Since 2012, OpenStax has created peer-reviewed, openly-licensed textbooks, which are available in free digital formats and for a low c ...
The Circulatory System
Study on the Manuscript of Paris by Servetus (1546 description of the Pulmonary Circulation) {{DEFAULTSORT:Circulatory System Exercise physiology Angiology