Radiation therapy or radiotherapy, often abbreviated RT, RTx, or XRT, is a therapy using
ionizing radiation, generally provided as part of cancer treatment to control or kill
malignant
Malignancy () is the tendency of a medical condition to become progressively worse.
Malignancy is most familiar as a characterization of cancer. A ''malignant'' tumor contrasts with a non-cancerous ''benign'' tumor in that a malignancy is not s ...
cells and normally delivered by a
linear accelerator
A linear particle accelerator (often shortened to linac) is a type of particle accelerator that accelerates charged subatomic particles or ions to a high speed by subjecting them to a series of oscillating electric potentials along a linear ...
. Radiation therapy may be curative in a number of types of cancer if they are localized to one area of the body. It may also be used as part of
adjuvant therapy, to prevent tumor recurrence after surgery to remove a primary malignant tumor (for example, early stages of breast cancer). Radiation therapy is synergistic with
chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs ( chemotherapeutic agents or alkylating agents) as part of a standardized chemotherapy regimen. Chemothe ...
, and has been used before, during, and after chemotherapy in susceptible cancers. The subspecialty of oncology concerned with radiotherapy is called radiation oncology. A physician who practices in this subspecialty is a
radiation oncologist
A radiation oncologist is a specialist physician who uses ionizing radiation (such as megavoltage X-rays or radionuclides) in the treatment of cancer. Radiation oncology is one of the three primary specialties, the other two being surgical and ...
.
Radiation therapy is commonly applied to the cancerous tumor because of its ability to control cell growth. Ionizing radiation works by damaging the
DNA of cancerous tissue leading to
cellular death. To spare normal tissues (such as skin or organs which radiation must pass through to treat the tumor), shaped radiation beams are aimed from several angles of exposure to intersect at the tumor, providing a much larger
absorbed dose there than in the surrounding healthy tissue. Besides the tumour itself, the radiation fields may also include the draining lymph nodes if they are clinically or radiologically involved with the tumor, or if there is thought to be a risk of subclinical malignant spread. It is necessary to include a margin of normal tissue around the tumor to allow for uncertainties in daily set-up and internal tumor motion. These uncertainties can be caused by internal movement (for example, respiration and bladder filling) and movement of external skin marks relative to the tumor position.
Radiation oncology is the medical specialty concerned with prescribing radiation, and is distinct from
radiology, the use of radiation in
medical imaging and
diagnosis. Radiation may be prescribed by a
radiation oncologist
A radiation oncologist is a specialist physician who uses ionizing radiation (such as megavoltage X-rays or radionuclides) in the treatment of cancer. Radiation oncology is one of the three primary specialties, the other two being surgical and ...
with intent to cure ("curative") or for adjuvant therapy. It may also be used as
palliative treatment
Palliative care (derived from the Latin root , or 'to cloak') is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Wit ...
(where cure is not possible and the aim is for local disease control or symptomatic relief) or as therapeutic treatment (where the therapy has survival benefit and can be curative). It is also common to combine radiation therapy with
surgery, chemotherapy,
hormone therapy,
immunotherapy
Immunotherapy or biological therapy is the treatment of disease by activating or suppressing the immune system. Immunotherapies designed to elicit or amplify an immune response are classified as ''activation immunotherapies,'' while immunotherap ...
or some mixture of the four. Most common cancer types can be treated with radiation therapy in some way.
The precise treatment intent (curative, adjuvant,
neoadjuvant therapeutic, or palliative) will depend on the tumor type, location, and stage, as well as the general health of the patient.
Total body irradiation (TBI) is a radiation therapy technique used to prepare the body to receive a
bone marrow transplant
Hematopoietic stem-cell transplantation (HSCT) is the transplantation of multipotent hematopoietic stem cells, usually derived from bone marrow, peripheral blood, or umbilical cord blood in order to replicate inside of a patient and to produce ...
.
Brachytherapy, in which a
radioactive source
A radioactive source is a known quantity of a radionuclide which emits ionizing radiation; typically one or more of the radiation types gamma rays, alpha particles, beta particles, and neutron radiation.
Sources can be used for irradiation, where ...
is placed inside or next to the area requiring treatment, is another form of radiation therapy that minimizes exposure to healthy tissue during procedures to treat cancers of the breast, prostate and other organs. Radiation therapy has several applications in non-malignant conditions, such as the treatment of
trigeminal neuralgia
Trigeminal neuralgia (TN or TGN), also called Fothergill disease, tic douloureux, or trifacial neuralgia is a long-term pain disorder that affects the trigeminal nerve, the nerve responsible for sensation in the face and motor functions such as ...
,
acoustic neuromas
A vestibular schwannoma (VS), also called acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve that passes from the inner ear to the brain. The tumor originates when Schwann cells that form the insulating myelin sheat ...
, severe
thyroid eye disease,
pterygium
Pterygium (plural ''pterygia'' or ''pterygiums'') refers to any wing-like triangular membrane occurring in the neck, eyes, knees, elbows, ankles or digits.
The term comes from the Greek word ''pterygion'' meaning "wing".
Types
* Popliteal pter ...
,
pigmented villonodular synovitis, and prevention of
keloid scar growth, vascular
restenosis
Restenosis is the recurrence of stenosis, a narrowing of a blood vessel, leading to restricted blood flow. Restenosis usually pertains to an artery or other large blood vessel that has become narrowed, received treatment to clear the blockage and s ...
, and
heterotopic ossification. The use of radiation therapy in non-malignant conditions is limited partly by worries about the risk of radiation-induced cancers.
Medical uses
Different cancers respond to radiation therapy in different ways.
The response of a cancer to radiation is described by its radiosensitivity.
Highly radiosensitive cancer cells are rapidly killed by modest doses of radiation. These include
leukemias
Leukemia ( also spelled leukaemia and pronounced ) is a group of blood cancers that usually begin in the bone marrow and result in high numbers of abnormal blood cells. These blood cells are not fully developed and are called ''blasts'' or '' ...
, most
lymphomas and
germ cell tumors.
The majority of
epithelial cancers
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bl ...
are only moderately radiosensitive, and require a significantly higher dose of radiation (60-70 Gy) to achieve a radical cure.
Some types of cancer are notably radioresistant, that is, much higher doses are required to produce a radical cure than may be safe in clinical practice.
Renal cell cancer
Renal cell carcinoma (RCC) is a kidney cancer that originates in the lining of the proximal convoluted tubule, a part of the very small tubes in the kidney that transport primary urine. RCC is the most common type of kidney cancer in adults, res ...
and
melanoma are generally considered to be radioresistant but radiation therapy is still a palliative option for many patients with metastatic melanoma. Combining radiation therapy with
immunotherapy
Immunotherapy or biological therapy is the treatment of disease by activating or suppressing the immune system. Immunotherapies designed to elicit or amplify an immune response are classified as ''activation immunotherapies,'' while immunotherap ...
is an active area of investigation and has shown some promise for melanoma and other cancers.
It is important to distinguish the radiosensitivity of a particular tumor, which to some extent is a laboratory measure, from the radiation "curability" of a cancer in actual clinical practice. For example, leukemias are not generally curable with radiation therapy, because they are disseminated through the body. Lymphoma may be radically curable if it is localised to one area of the body. Similarly, many of the common, moderately radioresponsive tumors are routinely treated with curative doses of radiation therapy if they are at an early stage. For example,
non-melanoma skin cancer,
head and neck cancer,
breast cancer
Breast cancer is cancer that develops from breast tissue. Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, milk rejection, fluid coming from the nipple, a newly inverted nipple, or a r ...
,
non-small cell lung cancer
Non-small-cell lung cancer (NSCLC) is any type of epithelial lung cancer other than small-cell lung carcinoma (SCLC). NSCLC accounts for about 85% of all lung cancers. As a class, NSCLCs are relatively insensitive to chemotherapy, compared to s ...
,
cervical cancer,
anal cancer
Anal cancer is a cancer which arises from the anus, the distal opening of the gastrointestinal tract. Symptoms may include bleeding from the anus or a lump near the anus. Other symptoms may include pain, itchiness, or discharge from the anus. A ...
, and
prostate cancer. With the exception of oligometastatic disease,
metastatic
Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, then, ...
cancers are incurable with radiation therapy because it is not possible to treat the whole body.
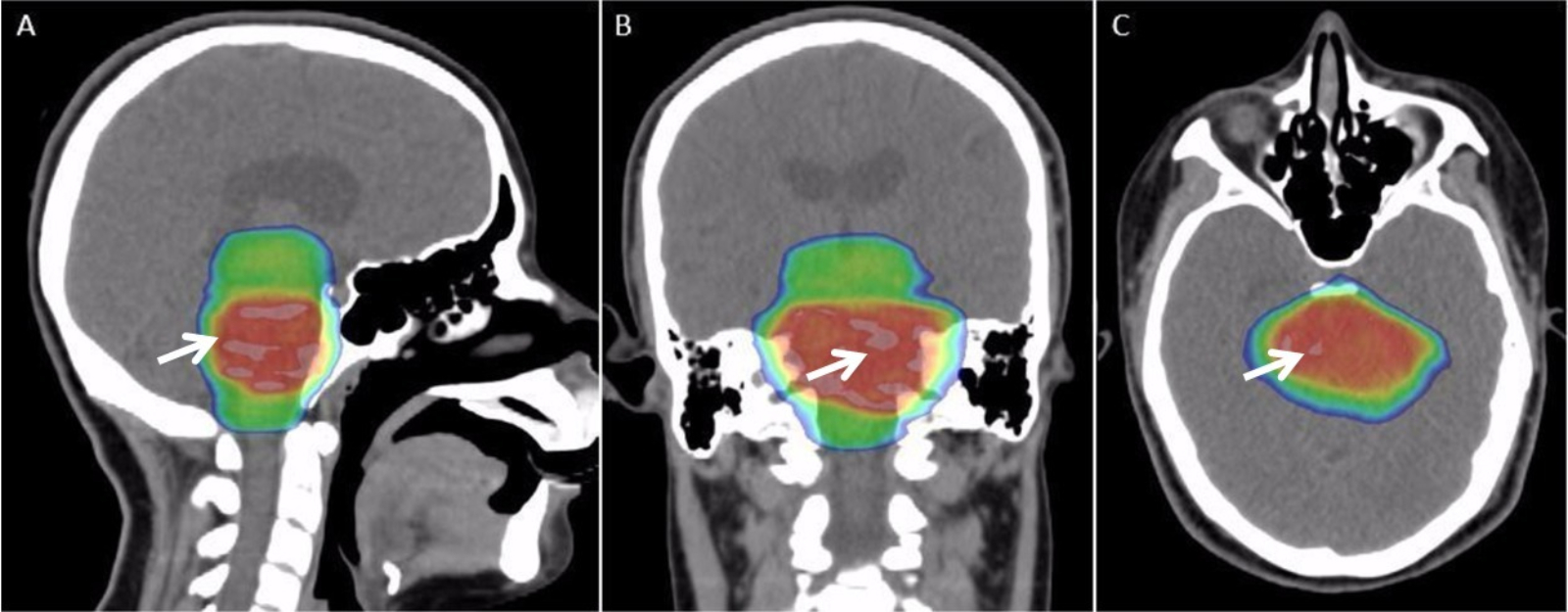
Modern radiation therapy relies on a CT scan to identify the tumor and surrounding normal structures and to perform dose calculations for the creation of a complex radiation treatment plan. The patient receives small skin marks to guide the placement of treatment fields.
[Camphausen KA, Lawrence RC]
"Principles of Radiation Therapy"
in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds
Cancer Management: A Multidisciplinary Approach
. 11 ed. 2008. Patient positioning is crucial at this stage as the patient will have to be placed in an identical position during each treatment. Many patient positioning devices have been developed for this purpose, including masks and cushions which can be molded to the patient. Image-guided radiation therapy (IGRT) is a method that uses imaging to correct for positional errors of each treatment session.
The response of a tumor to radiation therapy is also related to its size. Due to complex
radiobiology
Radiobiology (also known as radiation biology, and uncommonly as actinobiology) is a field of clinical and basic medical sciences that involves the study of the action of ionizing radiation on living things, especially health effects of radiation. ...
, very large tumors respond less well to radiation than smaller tumors or microscopic disease. Various strategies are used to overcome this effect. The most common technique is surgical resection prior to radiation therapy. This is most commonly seen in the treatment of breast cancer with
wide local excision
A wide local excision (WLE) is a surgical procedure to remove a small area of diseased or problematic tissue with a margin of normal tissue. This procedure is commonly performed on the breast and to skin lesions, but can be used on any area of the ...
or
mastectomy
Mastectomy is the medical term for the surgical removal of one or both breasts, partially or completely. A mastectomy is usually carried out to treat breast cancer. In some cases, women believed to be at high risk of breast cancer have the operat ...
followed by
adjuvant radiation therapy
Adjuvant therapy, also known as adjunct therapy, adjuvant care, or augmentation therapy, is a therapy that is given in addition to the primary or initial therapy to maximize its effectiveness. The surgeries and complex treatment regimens used in ...
. Another method is to shrink the tumor with
neoadjuvant chemotherapy prior to radical radiation therapy. A third technique is to enhance the radiosensitivity of the cancer by giving certain drugs during a course of radiation therapy. Examples of radiosensitizing drugs include
cisplatin
Cisplatin is a chemotherapy medication used to treat a number of cancers. These include testicular cancer, ovarian cancer, cervical cancer, breast cancer, bladder cancer, head and neck cancer, esophageal cancer, lung cancer, mesothelioma, ...
,
nimorazole
Nimorazole (INN) is a nitroimidazole anti-infective. It is also being investigated for the treatment of head and neck cancer
Head and neck cancer develops from tissues in the lip and oral cavity (mouth), larynx (throat), salivary glands, nose, ...
, and
cetuximab
Cetuximab, sold under the brand name Erbitux, is an epidermal growth factor receptor (EGFR) inhibitor medication used for the treatment of metastatic colorectal cancer and head and neck cancer. Cetuximab is a chimeric (mouse/human) monoclonal a ...
.
The impact of radiotherapy varies between different types of cancer and different groups. For example, for breast cancer after
breast-conserving surgery
Breast-conserving surgery (BCS) refers to an operation that aims to remove breast cancer while avoiding a mastectomy. Different forms of this operation include: lumpectomy (tylectomy), wide local excision, segmental resection, and quadrantectom ...
, radiotherapy has been found to halve the rate at which the disease recurs. In pancreatic cancer, radiotherapy has increased survival times for inoperable tumors.
Side effects
Radiation therapy is in itself painless. Many low-dose
palliative treatments (for example, radiation therapy to bony
metastases
Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, then ...
) cause minimal or no side effects, although short-term pain flare-up can be experienced in the days following treatment due to oedema compressing nerves in the treated area. Higher doses can cause varying side effects during treatment (acute side effects), in the months or years following treatment (long-term side effects), or after re-treatment (cumulative side effects). The nature, severity, and longevity of side effects depends on the organs that receive the radiation, the treatment itself (type of radiation, dose,
fractionation
Fractionation is a separation process in which a certain quantity of a mixture (of gases, solids, liquids, enzymes, or isotopes, or a suspension) is divided during a phase transition, into a number of smaller quantities (fractions) in which the ...
, concurrent chemotherapy), and the patient.
Most side effects are predictable and expected. Side effects from radiation are usually limited to the area of the patient's body that is under treatment. Side effects are dose- dependent; for example higher doses of head and neck radiation can be associated with
cardiovascular
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, tha ...
complications,
thyroid dysfunction, and
pituitary
In vertebrate anatomy, the pituitary gland, or hypophysis, is an endocrine gland, about the size of a chickpea and weighing, on average, in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain. The hypoph ...
axis dysfunction. Modern radiation therapy aims to reduce side effects to a minimum and to help the patient understand and deal with side effects that are unavoidable.
The main side effects reported are fatigue and skin irritation, like a mild to moderate sun burn. The fatigue often sets in during the middle of a course of treatment and can last for weeks after treatment ends. The irritated skin will heal, but may not be as elastic as it was before.
Acute side effects
; Nausea and vomiting
:This is not a general side effect of radiation therapy, and mechanistically is associated only with treatment of the stomach or abdomen (which commonly react a few hours after treatment), or with radiation therapy to certain nausea-producing structures in the head during treatment of certain head and neck tumors, most commonly the
vestibules of the inner ears. As with any distressing treatment, some patients vomit immediately during radiotherapy, or even in anticipation of it, but this is considered a psychological response. Nausea for any reason can be treated with antiemetics.
; Damage to the
epithelial surfaces
:Epithelial surfaces may sustain damage from radiation therapy. Depending on the area being treated, this may include the skin, oral mucosa, pharyngeal, bowel mucosa and ureter. The rates of onset of damage and recovery from it depend upon the turnover rate of epithelial cells. Typically the skin starts to become pink and sore several weeks into treatment. The reaction may become more severe during the treatment and for up to about one week following the end of radiation therapy, and the skin may break down. Although this
moist desquamation
Moist desquamation is a description of the clinical pattern seen as a consequence of radiation exposure where the skin thins and then begins to weep because of loss of integrity of the epithelial barrier and decreased oncotic pressure. Typically t ...
is uncomfortable, recovery is usually quick. Skin reactions tend to be worse in areas where there are natural folds in the skin, such as underneath the female breast, behind the ear, and in the groin.
; Mouth, throat and stomach sores
:If the head and neck area is treated, temporary soreness and ulceration commonly occur in the mouth and throat.
If severe, this can affect swallowing, and the patient may need painkillers and nutritional support/food supplements. The esophagus can also become sore if it is treated directly, or if, as commonly occurs, it receives a dose of collateral radiation during treatment of lung cancer. When treating liver malignancies and metastases, it is possible for collateral radiation to cause gastric, stomach or duodenal ulcers This collateral radiation is commonly caused by non-targeted delivery (reflux) of the radioactive agents being infused. Methods, techniques and devices are available to lower the occurrence of this type of adverse side effect.
; Intestinal discomfort
:The lower bowel may be treated directly with radiation (treatment of rectal or anal cancer) or be exposed by radiation therapy to other pelvic structures (prostate, bladder, female genital tract). Typical symptoms are soreness, diarrhoea, and nausea. Nutritional interventions may be able to help with diarrhoea associated with radiotherapy.
Studies in people having pelvic radiotherapy as part of anticancer treatment for a primary pelvic cancer found that changes in dietary fat, fibre and lactose during radiotherapy reduced diarrhoea at the end of treatment.
; Swelling
:As part of the general
inflammation
Inflammation (from la, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molec ...
that occurs, swelling of soft tissues may cause problems during radiation therapy. This is a concern during treatment of brain tumors and brain metastases, especially where there is pre-existing raised
intracranial pressure
Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury ( mmHg) and at rest, is normally 7–15 mmHg for a supine adult ...
or where the tumor is causing near-total obstruction of a
lumen (e.g.,
trachea or main
bronchus
A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi pronounced (BRAN-KAI) to branch from the trachea at the carina are the right main bronchus and the left main bronchu ...
). Surgical intervention may be considered prior to treatment with radiation. If surgery is deemed unnecessary or inappropriate, the patient may receive
steroids during radiation therapy to reduce swelling.
; Infertility
:The
gonads
A gonad, sex gland, or reproductive gland is a mixed gland that produces the gametes and sex hormones of an organism. Female reproductive cells are egg cells, and male reproductive cells are sperm. The male gonad, the testicle, produces sper ...
(ovaries and testicles) are very sensitive to radiation. They may be unable to produce
gametes
A gamete (; , ultimately ) is a haploid cell that fuses with another haploid cell during fertilization in organisms that reproduce sexually. Gametes are an organism's reproductive cells, also referred to as sex cells. In species that produce ...
following direct exposure to most normal treatment doses of radiation. Treatment planning for all body sites is designed to minimize, if not completely exclude dose to the gonads if they are not the primary area of treatment.
Late side effects
Late side effects occur months to years after treatment and are generally limited to the area that has been treated. They are often due to damage of blood vessels and connective tissue cells. Many late effects are reduced by fractionating treatment into smaller parts.
;
Fibrosis
Fibrosis, also known as fibrotic scarring, is a pathological wound healing in which connective tissue replaces normal parenchymal tissue to the extent that it goes unchecked, leading to considerable tissue remodelling and the formation of perma ...
: Tissues which have been irradiated tend to become less elastic over time due to a diffuse scarring process.
; Epilation
: Epilation (hair loss) may occur on any hair bearing skin with doses above 1 Gy. It only occurs within the radiation field/s. Hair loss may be permanent with a single dose of 10 Gy, but if the dose is fractionated permanent hair loss may not occur until dose exceeds 45 Gy.
; Dryness
: The salivary glands and tear glands have a radiation tolerance of about 30
Gy in 2 Gy fractions, a dose which is exceeded by most radical head and neck cancer treatments. Dry mouth (
xerostomia
Xerostomia, also known as dry mouth, is dryness in the mouth, which may be associated with a change in the composition of saliva, or reduced salivary flow, or have no identifiable cause.
This symptom is very common and is often seen as a side eff ...
) and dry eyes (
xerophthalmia) can become irritating long-term problems and severely reduce the patient's
quality of life. Similarly,
sweat glands in treated skin (such as the
armpit
The axilla (also, armpit, underarm or oxter) is the area on the human body directly under the shoulder joint. It includes the axillary space, an anatomical space within the shoulder girdle between the arm and the thoracic cage, bounded superior ...
) tend to stop working, and the naturally moist vaginal
mucosa is often dry following pelvic irradiation.
;
Lymphedema
: Lymphedema, a condition of localized fluid retention and tissue swelling, can result from damage to the lymphatic system sustained during radiation therapy. It is the most commonly reported complication in breast radiation therapy patients who receive adjuvant axillary radiotherapy following surgery to clear the axillary lymph nodes .
; Cancer
: Radiation is a potential cause of cancer, and secondary malignancies are seen in some patients. Cancer survivors are already more likely than the general population to develop malignancies due to a number of factors including lifestyle choices, genetics, and previous radiation treatment. It is difficult to directly quantify the rates of these secondary cancers from any single cause. Studies have found radiation therapy as the cause of secondary malignancies for only a small minority of patients. New techniques such as proton beam therapy and
carbon ion radiotherapy
Particle therapy is a form of external beam radiotherapy using beams of energetic neutrons, protons, or other heavier positive ions for cancer treatment. The most common type of particle therapy as of August 2021 is proton therapy.
In contrast ...
which aim to reduce dose to healthy tissues will lower these risks. It starts to occur 4–6 years following treatment, although some haematological malignancies may develop within 3 years. In the vast majority of cases, this risk is greatly outweighed by the reduction in risk conferred by treating the primary cancer even in pediatric malignancies which carry a higher burden of secondary malignancies.
;
Cardiovascular disease
: Radiation can increase the risk of heart disease and death as observed in previous breast cancer RT regimens. Therapeutic radiation increases the risk of a subsequent cardiovascular event (i.e., heart attack or stroke) by 1.5 to 4 times a person's normal rate, aggravating factors included.
The increase is dose dependent, related to the RT's dose strength, volume and location.
: Cardiovascular late side effects have been termed radiation-induced heart disease (RIHD) and radiation-induced vascular disease (RIVD).
Symptoms are dose dependent and include
cardiomyopathy,
myocardial fibrosis,
valvular heart disease
Valvular heart disease is any cardiovascular disease process involving one or more of the four valves of the heart (the aortic and mitral valves on the left side of heart and the pulmonic and tricuspid valves on the right side of heart). These ...
,
coronary artery disease,
heart arrhythmia
Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adult ...
and
peripheral artery disease
Peripheral artery disease (PAD) is an abnormal narrowing of arteries other than those that supply the heart or brain. When narrowing occurs in the heart, it is called coronary artery disease, and in the brain, it is called cerebrovascular dis ...
. Radiation-induced fibrosis, vascular
cell damage
Cell damage (also known as cell injury) is a variety of changes of stress that a cell suffers due to external as well as internal environmental changes. Amongst other causes, this can be due to physical, chemical, infectious, biological, nutrition ...
and
oxidative stress
Oxidative stress reflects an imbalance between the systemic manifestation of reactive oxygen species and a biological system's ability to readily detoxify the reactive intermediates or to repair the resulting damage. Disturbances in the normal ...
can lead to these and other late side effect symptoms.
Most radiation-induced cardiovascular diseases occur 10 or more years post treatment, making causality determinations more difficult.
; Cognitive decline
: In cases of radiation applied to the head radiation therapy may cause
cognitive decline
Dementia is a disorder which manifests as a set of related symptoms, which usually surfaces when the brain is damaged by injury or disease. The symptoms involve progressive impairments in memory, thinking, and behavior, which negatively affec ...
. Cognitive decline was especially apparent in young children, between the ages of 5 to 11. Studies found, for example, that the IQ of 5-year-old children declined each year after treatment by several IQ points.
;
Radiation enteropathy

: The gastrointestinal tract can be damaged following abdominal and pelvic radiotherapy.
Atrophy, fibrosis and vascular changes produce
malabsorption
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety ...
,
diarrhea,
steatorrhea and
bleeding
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vag ...
with
bile acid diarrhea
Bile acid malabsorption (BAM), known also as bile acid diarrhea, is a cause of several gut-related problems, the main one being chronic diarrhea. It has also been called bile acid-induced diarrhea, cholerheic or choleretic enteropathy, bile salt di ...
and
vitamin B12 malabsorption commonly found due to ileal involvement.
Pelvic radiation disease includes
radiation proctitis
Radiation proctitis or radiation proctopathy is condition characterized by damage to the rectum after exposure to x-rays or other ionizing radiation as a part of radiation therapy. Radiation proctopathy may occur as acute inflammation called "acu ...
, producing bleeding, diarrhoea and urgency,
and can also cause radiation cystitis when the bladder is affected.
; Radiation-induced
polyneuropathy
: Radiation treatments may damage nerves near the target area or within the delivery path as nerve tissue is also
radiosensitive.
Nerve damage from ionizing radiation occurs in phases, the initial phase from microvascular injury, capillary damage and
nerve demyelination.
Subsequent damage occurs from vascular constriction and
nerve compression due to
uncontrolled fibrous tissue growth caused by radiation.
Radiation-induced polyneuropathy
ICD-10-CM Code G62.82 occurs in approximately 1–5% of those receiving radiation therapy.
: Depending upon the irradiated zone, late effect neuropathy may occur in either the
central nervous system
The central nervous system (CNS) is the part of the nervous system consisting primarily of the brain and spinal cord. The CNS is so named because the brain integrates the received information and coordinates and influences the activity of all p ...
(CNS) or the
peripheral nervous system
The peripheral nervous system (PNS) is one of two components that make up the nervous system of bilateral animals, with the other part being the central nervous system (CNS). The PNS consists of nerves and ganglia, which lie outside the brain ...
(PNS). In the CNS for example, cranial nerve injury typically presents as a visual acuity loss 1–14 years post treatment.
In the PNS, injury to the plexus nerves presents as radiation-induced brachial plexopathy or
radiation-induced lumbosacral plexopathy appearing up to 3 decades post treatment.
;Radiation necrosis
:Radiation
necrosis is the death of healthy tissue near the irradiated site. It is a type of
coagulative necrosis Coagulative necrosis is a type of accidental cell death typically caused by ischemia or infarction. In coagulative necrosis, the architectures of dead tissue are preserved for at least a couple of days. It is believed that the injury denatures stru ...
that occurs because the radiation directly or indirectly damages blood vessels in the area, which reduces the blood supply to the remaining healthy tissue, causing it to die by
ischemia, similar to what happens in an
ischemic stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop funct ...
.
Because it is an indirect effect of the treatment, it occurs months to decades after radiation exposure.
Cumulative side effects
Cumulative effects from this process should not be confused with long-term effects – when short-term effects have disappeared and long-term effects are subclinical, reirradiation can still be problematic. These doses are calculated by the radiation oncologist and many factors are taken into account before the subsequent radiation takes place.
Effects on reproduction
During the first two weeks after
fertilization, radiation therapy is lethal but not
teratogenic.
/ref> High doses of radiation during pregnancy induce congenital anomaly, anomalies, impaired growth and intellectual disability
Intellectual disability (ID), also known as general learning disability in the United Kingdom and formerly mental retardation, Rosa's Law, Pub. L. 111-256124 Stat. 2643(2010). is a generalized neurodevelopmental disorder characterized by signif ...
, and there may be an increased risk of childhood leukemia and other tumours in the offspring.[
In males previously having undergone radiotherapy, there appears to be no increase in genetic defects or congenital malformations in their children conceived after therapy.][ However, the use of ]assisted reproductive technologies
Assisted reproductive technology (ART) includes medical procedures used primarily to address infertility. This subject involves procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation of gametes ...
and micromanipulation techniques might increase this risk.[
]
Effects on pituitary system
Hypopituitarism
Hypopituitarism is the decreased (''hypo'') secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is know ...
commonly develops after radiation therapy for sellar and parasellar neoplasms, extrasellar brain tumours, head and neck tumours, and following whole body irradiation for systemic malignancies.[ Radiation-induced hypopituitarism mainly affects growth hormone and ]gonadal hormone
Sex hormones, also known as sex steroids, gonadocorticoids and gonadal steroids, are steroid hormones that interact with vertebrate steroid hormone receptors. The sex hormones include the androgens, estrogens, and progestogens. Their effects are ...
s.thyroid stimulating hormone
Thyroid-stimulating hormone (also known as thyrotropin, thyrotropic hormone, or abbreviated TSH) is a pituitary hormone that stimulates the thyroid gland to produce thyroxine (T4), and then triiodothyronine (T3) which stimulates the metabolism of ...
(TSH) deficiencies are the least common among people with radiation-induced hypopituitarism.[ Changes in ]prolactin
Prolactin (PRL), also known as lactotropin, is a protein best known for its role in enabling mammals to produce milk. It is influential in over 300 separate processes in various vertebrates, including humans. Prolactin is secreted from the pit ...
-secretion is usually mild, and vasopressin deficiency appears to be very rare as a consequence of radiation.[
]
Radiation therapy accidents
There are rigorous procedures in place to minimise the risk of accidental overexposure of radiation therapy to patients. However, mistakes do occasionally occur; for example, the radiation therapy machine Therac-25 was responsible for at least six accidents between 1985 and 1987, where patients were given up to one hundred times the intended dose; two people were killed directly by the radiation overdoses. From 2005 to 2010, a hospital in Missouri
Missouri is a state in the Midwestern region of the United States. Ranking 21st in land area, it is bordered by eight states (tied for the most with Tennessee): Iowa to the north, Illinois, Kentucky and Tennessee to the east, Arkansas t ...
overexposed 76 patients (most with brain cancer) during a five-year period because new radiation equipment had been set up incorrectly.
Although medical errors are exceptionally rare, radiation oncologists, medical physicists and other members of the radiation therapy treatment team are working to eliminate them. ASTRO has launched a safety initiative called
Target Safely
that, among other things, aims to record errors nationwide so that doctors can learn from each and every mistake and prevent them from happening. ASTRO also publishes a list of questions for patients to ask their doctors about radiation safety to ensure every treatment is as safe as possible.
Use in non-cancerous diseases
 Radiation therapy is used to treat early stage Dupuytren's disease and
Radiation therapy is used to treat early stage Dupuytren's disease and Ledderhose disease
Plantar fascial fibromatosis, also known as Ledderhose's disease, Morbus Ledderhose, and plantar fibromatosis, is a relatively uncommon non-malignant thickening of the feet's deep connective tissue, or fascia. In the beginning, where nodules start ...
. When Dupuytren's disease is at the nodules and cords stage or fingers are at a minimal deformation stage of less than 10 degrees, then radiation therapy is used to prevent further progress of the disease. Radiation therapy is also used post surgery in some cases to prevent the disease continuing to progress. Low doses of radiation are used typically three gray of radiation for five days, with a break of three months followed by another phase of three gray of radiation for five days.
Technique
Mechanism of action
Radiation therapy works by damaging the DNA of cancerous cells and can cause them to undergo mitotic catastrophe. This DNA damage is caused by one of two types of energy, photon
A photon () is an elementary particle that is a quantum of the electromagnetic field, including electromagnetic radiation such as light and radio waves, and the force carrier for the electromagnetic force. Photons are massless, so they a ...
or charged particle
In physics, a charged particle is a particle with an electric charge. It may be an ion, such as a molecule or atom with a surplus or deficit of electrons relative to protons. It can also be an electron or a proton, or another elementary pa ...
. This damage is either direct or indirect ionization
Ionization, or Ionisation is the process by which an atom or a molecule acquires a negative or positive charge by gaining or losing electrons, often in conjunction with other chemical changes. The resulting electrically charged atom or molecul ...
of the atoms which make up the DNA chain. Indirect ionization happens as a result of the ionization of water, forming free radicals, notably hydroxyl radicals, which then damage the DNA.
In photon therapy, most of the radiation effect is through free radicals. Cells have mechanisms for repairing single-strand DNA damage and double-stranded DNA damage. However, double-stranded DNA breaks are much more difficult to repair, and can lead to dramatic chromosomal abnormalities and genetic deletions. Targeting double-stranded breaks increases the probability that cells will undergo cell death
Cell death is the event of a biological cell ceasing to carry out its functions. This may be the result of the natural process of old cells dying and being replaced by new ones, as in programmed cell death, or may result from factors such as d ...
. Cancer cells are generally less differentiated and more stem cell-like; they reproduce more than most healthy differentiated cells, and have a diminished ability to repair sub-lethal damage. Single-strand DNA damage is then passed on through cell division; damage to the cancer cells' DNA accumulates, causing them to die or reproduce more slowly.
One of the major limitations of photon radiation therapy is that the cells of solid tumors become deficient in oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements as ...
. Solid tumors can outgrow their blood supply, causing a low-oxygen state known as hypoxia. Oxygen is a potent radiosensitizer, increasing the effectiveness of a given dose of radiation by forming DNA-damaging free radicals. Tumor cells in a hypoxic environment may be as much as 2 to 3 times more resistant to radiation damage than those in a normal oxygen environment.
Much research has been devoted to overcoming hypoxia including the use of high pressure oxygen tanks, hyperthermia therapy
Hyperthermia therapy ''(or hyperthermia, or thermotherapy)'' is a type of medical treatment in which body tissue is exposed to temperatures above body temperature, in the region of 40–45 °C (104–113 °F). Hyperthermia is usually ...
(heat therapy which dilates blood vessels to the tumor site), blood substitutes that carry increased oxygen, hypoxic cell radiosensitizer drugs such as misonidazole
Misonidazole is a radiosensitizer that was investigated in clinical trials. It was used in these trials for radiation therapy
Radiation therapy or radiotherapy, often abbreviated RT, RTx, or XRT, is a therapy using ionizing radiation, general ...
and metronidazole, and hypoxic cytotoxins (tissue poisons), such as tirapazamine
Tirapazamine (SR-4233) is an experimental anticancer drug that is activated to a toxic radical only at very low levels of oxygen ( hypoxia). Such levels are common in human solid tumors, a phenomenon known as tumor hypoxia. Thus, tirapazamine is ...
. Newer research approaches are currently being studied, including preclinical and clinical investigations into the use of an oxygen diffusion-enhancing compound An oxygen diffusion-enhancing compound is any substance that increases the availability of oxygen in body tissues by influencing the molecular structure of water in blood plasma and thereby promoting the movement (diffusion) of oxygen through plas ...
such as trans sodium crocetinate (TSC) as a radiosensitizer.
Charged particles such as protons and boron, carbon
Carbon () is a chemical element with the symbol C and atomic number 6. It is nonmetallic and tetravalent—its atom making four electrons available to form covalent chemical bonds. It belongs to group 14 of the periodic table. Carbon mak ...
, and neon ions can cause direct damage to cancer cell DNA through high-LET ( linear energy transfer) and have an antitumor effect independent of tumor oxygen supply because these particles act mostly via direct energy transfer usually causing double-stranded DNA breaks. Due to their relatively large mass, protons and other charged particles have little lateral side scatter in the tissue – the beam does not broaden much, stays focused on the tumor shape, and delivers small dose side-effects to surrounding tissue. They also more precisely target the tumor using the Bragg peak effect. See proton therapy for a good example of the different effects of intensity-modulated radiation therapy (IMRT) vs. charged particle therapy. This procedure reduces damage to healthy tissue between the charged particle radiation source and the tumor and sets a finite range for tissue damage after the tumor has been reached. In contrast, IMRT's use of uncharged particles causes its energy to damage healthy cells when it exits the body. This exiting damage is not therapeutic, can increase treatment side effects, and increases the probability of secondary cancer induction. This difference is very important in cases where the close proximity of other organs makes any stray ionization very damaging (example: head and neck cancers). This X-ray exposure is especially bad for children, due to their growing bodies, and while depending on a multitude of factors, they are around 10 times more sensitive to developing secondary malignancies after radiotherapy as compared to adults.
Dose
The amount of radiation used in photon radiation therapy is measured in grays (Gy), and varies depending on the type and stage of cancer being treated. For curative cases, the typical dose for a solid epithelial tumor ranges from 60 to 80 Gy, while lymphomas are treated with 20 to 40 Gy.
Preventive (adjuvant) doses are typically around 45–60 Gy in 1.8–2 Gy fractions (for breast, head, and neck cancers.) Many other factors are considered by radiation oncologist
A radiation oncologist is a specialist physician who uses ionizing radiation (such as megavoltage X-rays or radionuclides) in the treatment of cancer. Radiation oncology is one of the three primary specialties, the other two being surgical and ...
s when selecting a dose, including whether the patient is receiving chemotherapy, patient comorbidities, whether radiation therapy is being administered before or after surgery, and the degree of success of surgery.
Delivery parameters of a prescribed dose are determined during treatment planning (part of dosimetry Radiation dosimetry in the fields of health physics and radiation protection is the measurement, calculation and assessment of the ionizing radiation dose absorbed by an object, usually the human body. This applies both internally, due to ingested ...
). Treatment planning is generally performed on dedicated computers using specialized treatment planning software. Depending on the radiation delivery method, several angles or sources may be used to sum to the total necessary dose. The planner will try to design a plan that delivers a uniform prescription dose to the tumor and minimizes dose to surrounding healthy tissues.
In radiation therapy, three-dimensional dose distributions may be evaluated using the dosimetry Radiation dosimetry in the fields of health physics and radiation protection is the measurement, calculation and assessment of the ionizing radiation dose absorbed by an object, usually the human body. This applies both internally, due to ingested ...
technique known as gel dosimetry Gel dosimeters, also called Fricke gel dosimeters, are manufactured from radiation sensitive chemicals that, upon irradiation with ionising radiation, undergo a fundamental change in their properties as a function of the absorbed radiation dose.
Ov ...
.
Fractionation
The total dose is fractionated (spread out over time) for several important reasons. Fractionation allows normal cells time to recover, while tumor cells are generally less efficient in repair between fractions. Fractionation also allows tumor cells that were in a relatively radio-resistant phase of the cell cycle during one treatment to cycle into a sensitive phase of the cycle before the next fraction is given. Similarly, tumor cells that were chronically or acutely hypoxic (and therefore more radioresistant) may reoxygenate between fractions, improving the tumor cell kill.
Fractionation regimens are individualised between different radiation therapy centers and even between individual doctors. In North America, Australia, and Europe, the typical fractionation schedule for adults is 1.8 to 2 Gy per day, five days a week. In some cancer types, prolongation of the fraction schedule over too long can allow for the tumor to begin repopulating, and for these tumor types, including head-and-neck and cervical squamous cell cancers, radiation treatment is preferably completed within a certain amount of time. For children, a typical fraction size may be 1.5 to 1.8 Gy per day, as smaller fraction sizes are associated with reduced incidence and severity of late-onset side effects in normal tissues.
In some cases, two fractions per day are used near the end of a course of treatment. This schedule, known as a concomitant boost regimen or hyperfractionation, is used on tumors that regenerate more quickly when they are smaller. In particular, tumors in the head-and-neck demonstrate this behavior.
Patients receiving palliative radiation to treat uncomplicated painful bone metastasis should not receive more than a single fraction of radiation.[, which cites
* ] A single treatment gives comparable pain relief and morbidity outcomes to multiple-fraction treatments, and for patients with limited life expectancy, a single treatment is best to improve patient comfort.
Schedules for fractionation
One fractionation schedule that is increasingly being used and continues to be studied is hypofractionation. This is a radiation treatment in which the total dose of radiation is divided into large doses. Typical doses vary significantly by cancer type, from 2.2 Gy/fraction to 20 Gy/fraction, the latter being typical of stereotactic treatments (stereotactic ablative body radiotherapy, or SABR – also known as SBRT, or stereotactic body radiotherapy) for subcranial lesions, or SRS (stereotactic radiosurgery) for intracranial lesions. The rationale of hypofractionation is to reduce the probability of local recurrence by denying clonogenic cells the time they require to reproduce and also to exploit the radiosensitivity of some tumors. In particular, stereotactic treatments are intended to destroy clonogenic cells by a process of ablation – ''i.e.'' the delivery of a dose intended to destroy clonogenic cells directly, rather than to interrupt the process of clonogenic cell division repeatedly (apoptosis), as in routine radiotherapy.
Estimation of dose based on target sensitivity
Different cancer types have different radiation sensitivity. While predicting the sensitivity based on genomic or proteomic analyses of biopsy samples has proven challenging, the predictions of radiation effect on individual patients from genomic signatures of intrinsic cellular radiosensitivity have been shown to associate with clinical outcome. An alternative approach to genomics and proteomics was offered by the discovery that radiation protection in microbes is offered by non-enzymatic complexes of manganese
Manganese is a chemical element with the symbol Mn and atomic number 25. It is a hard, brittle, silvery metal, often found in minerals in combination with iron. Manganese is a transition metal with a multifaceted array of industrial alloy use ...
and small organic metabolites. The content and variation of manganese (measurable by electron paramagnetic resonance) were found to be good predictors of radiosensitivity, and this finding extends also to human cells. An association was confirmed between total cellular manganese contents and their variation, and clinically inferred radioresponsiveness in different tumor cells, a finding that may be useful for more precise radiodosages and improved treatment of cancer patients.
Types
Historically, the three main divisions of radiation therapy are:
* external beam radiation therapy (EBRT or XRT) or teletherapy;
* brachytherapy or sealed source radiation therapy; and
* systemic radioisotope therapy or unsealed source radiotherapy
Radionuclide therapy (RNT, also known as unsealed source radiotherapy or molecular radiotherapy) uses radioactive substances called radiopharmaceuticals to treat medical conditions, particularly cancer. These are introduced into the body by vario ...
.
The differences relate to the position of the radiation source; external is outside the body, brachytherapy uses sealed radioactive sources placed precisely in the area under treatment, and systemic radioisotopes are given by infusion or oral ingestion. Brachytherapy can use temporary or permanent placement of radioactive sources. The temporary sources are usually placed by a technique called afterloading. In afterloading a hollow tube or applicator is placed surgically in the organ to be treated, and the sources are loaded into the applicator after the applicator is implanted. This minimizes radiation exposure to health care personnel.
Particle therapy is a special case of external beam radiation therapy where the particles are protons or heavier ions
An ion () is an atom or molecule with a net electrical charge.
The charge of an electron is considered to be negative by convention and this charge is equal and opposite to the charge of a proton, which is considered to be positive by conven ...
.
A review of radiation therapy randomised clinical trials from 2018 to 2021 found many practice-changing data and new concepts that emerge from RCTs, identifying techniques that improve the therapeutic ratio, techniques that lead to more tailored treatments, stressing the importance of patient satisfaction, and identifying areas that require further study.
External beam radiation therapy
The following three sections refer to treatment using X-rays.
Conventional external beam radiation therapy
 Historically conventional external beam radiation therapy (2DXRT) was delivered via two-dimensional beams using kilovoltage therapy X-ray units, medical linear accelerators that generate high-energy X-rays, or with machines that were similar to a linear accelerator in appearance, but used a sealed radioactive source like the one shown above.
Historically conventional external beam radiation therapy (2DXRT) was delivered via two-dimensional beams using kilovoltage therapy X-ray units, medical linear accelerators that generate high-energy X-rays, or with machines that were similar to a linear accelerator in appearance, but used a sealed radioactive source like the one shown above.
Stereotactic radiation
Stereotactic radiation is a specialized type of external beam radiation therapy. It uses focused radiation beams targeting a well-defined tumor using extremely detailed imaging scans. Radiation oncologists perform stereotactic treatments, often with the help of a neurosurgeon for tumors in the brain or spine.
There are two types of stereotactic radiation. Stereotactic radiosurgery (SRS) is when doctors use a single or several stereotactic radiation treatments of the brain or spine. Stereotactic body radiation therapy (SBRT) refers to one or several stereotactic radiation treatments with the body, such as the lungs.
Some doctors say an advantage to stereotactic treatments is that they deliver the right amount of radiation to the cancer in a shorter amount of time than traditional treatments, which can often take 6 to 11 weeks. Plus treatments are given with extreme accuracy, which should limit the effect of the radiation on healthy tissues. One problem with stereotactic treatments is that they are only suitable for certain small tumors.
Stereotactic treatments can be confusing because many hospitals call the treatments by the name of the manufacturer rather than calling it SRS or SBRT. Brand names for these treatments include Axesse, Cyberknife, Gamma Knife, Novalis, Primatom, Synergy, X-Knife, TomoTherapy, Trilogy and Truebeam
Varian Medical Systems is an American radiation oncology treatments and software maker based in Palo Alto, California. Their medical devices include linear accelerators (LINACs) and software for treating cancer and other medical conditions with ...
. This list changes as equipment manufacturers continue to develop new, specialized technologies to treat cancers.
Virtual simulation, and 3-dimensional conformal radiation therapy
The planning of radiation therapy treatment has been revolutionized by the ability to delineate tumors and adjacent normal structures in three dimensions using specialized CT and/or MRI scanners and planning software.
Virtual simulation, the most basic form of planning, allows more accurate placement of radiation beams than is possible using conventional X-rays, where soft-tissue structures are often difficult to assess and normal tissues difficult to protect.
An enhancement of virtual simulation is 3-dimensional conformal radiation therapy (3DCRT), in which the profile of each radiation beam is shaped to fit the profile of the target from a beam's eye view (BEV) using a multileaf collimator (MLC) and a variable number of beams. When the treatment volume conforms to the shape of the tumor, the relative toxicity of radiation to the surrounding normal tissues is reduced, allowing a higher dose of radiation to be delivered to the tumor than conventional techniques would allow.[
]
Intensity-modulated radiation therapy (IMRT)
 Intensity-modulated radiation therapy (IMRT) is an advanced type of high-precision radiation that is the next generation of 3DCRT.
Intensity-modulated radiation therapy (IMRT) is an advanced type of high-precision radiation that is the next generation of 3DCRT.optimization
Mathematical optimization (alternatively spelled ''optimisation'') or mathematical programming is the selection of a best element, with regard to some criterion, from some set of available alternatives. It is generally divided into two subfi ...
and treatment simulation ( Treatment Planning). The radiation dose is consistent with the 3-D shape of the tumor by controlling, or modulating, the radiation beam's intensity. The radiation dose intensity is elevated near the gross tumor volume while radiation among the neighboring normal tissues is decreased or avoided completely. This results in better tumor targeting, lessened side effects, and improved treatment outcomes than even 3DCRT.
3DCRT is still used extensively for many body sites but the use of IMRT is growing in more complicated body sites such as CNS, head and neck, prostate, breast, and lung. Unfortunately, IMRT is limited by its need for additional time from experienced medical personnel. This is because physicians must manually delineate the tumors one CT image at a time through the entire disease site which can take much longer than 3DCRT preparation. Then, medical physicists and dosimetrists must be engaged to create a viable treatment plan. Also, the IMRT technology has only been used commercially since the late 1990s even at the most advanced cancer centers, so radiation oncologists who did not learn it as part of their residency programs must find additional sources of education before implementing IMRT.
Proof of improved survival benefit from either of these two techniques over conventional radiation therapy (2DXRT) is growing for many tumor sites, but the ability to reduce toxicity is generally accepted. This is particularly the case for head and neck cancers in a series of pivotal trials performed by Professor Christopher Nutting
Christopher M. Nutting (born 5 April 1968) is a British Professor of Clinical Oncology and medical consultant, specializing in head and neck cancers, who has helped develop Intensity-Modulated Radiotherapy (IMRT), an advanced form of Radiation t ...
of the Royal Marsden Hospital. Both techniques enable dose escalation, potentially increasing usefulness. There has been some concern, particularly with IMRT,
Volumetric modulated arc therapy (VMAT)
Volumetric modulated arc therapy (VMAT) is a radiation technique introduced in 2007nasopharyngeal
The pharynx (plural: pharynges) is the part of the throat behind the mouth and nasal cavity, and above the oesophagus and trachea (the tubes going down to the stomach and the lungs). It is found in vertebrates and invertebrates, though its struct ...
, oropharyngeal
The pharynx (plural: pharynges) is the part of the throat behind the mouth and nasal cavity, and above the oesophagus and trachea (the tubes going down to the stomach and the lungs). It is found in vertebrates and invertebrates, though its struct ...
and hypopharyngeal carcinomas VMAT provides equivalent or better protection of the organ at risk (OAR).
Temporally feathered radiation therapy (TFRT)
Temporally feathered radiation therapy (TFRT) is a radiation technique introduced in 2018
Automated planning
Automated treatment planning has become an integrated part of radiotherapy treatment planning. There are in general two approaches of automated planning. 1) Knowledge based planning where the treatment planning system has a library of high quality plans, from which it can predict the target and dose-volume histogram of the organ at risk. 2) The other approach is commonly called protocol based planning, where the treatment planning system tried to mimic an experienced treatment planner and through an iterative process evaluates the plan quality from on the basis of the protocol.
Particle therapy
In particle therapy ( proton therapy being one example), energetic ionizing particles (protons or carbon ions) are directed at the target tumor. The dose increases while the particle penetrates the tissue, up to a maximum (the Bragg peak) that occurs near the end of the particle's range, and it then drops to (almost) zero. The advantage of this energy deposition profile is that less energy is deposited into the healthy tissue surrounding the target tissue.
Auger therapy
Auger therapy
Auger therapy is a form of radiation therapy for the treatment of cancer which relies on low-energy electrons (emitted by the Auger effect) to damage cancer cells, rather than the high-energy radiation used in traditional radiation therapy. Simil ...
(AT) makes use of a very high dose
Motion compensation
In many types of external beam radiotherapy, motion can negatively impact the treatment delivery by moving target tissue out of, or other healthy tissue into, the intended beam path. Some form of patient immobilisation is common, to prevent the large movements of the body during treatment, however this cannot prevent all motion, for example as a result of breathing. Several techniques have been developed to account for motion like this. Deep inspiration breath-hold (DIBH) is commonly used for breast treatments where it is important to avoid irradiating the heart. In DIBH the patient holds their breath after breathing in to provide a stable position for the treatment beam to be turned on. This can be done automatically using an external monitoring system such as a spirometer
A spirometer is an apparatus for measuring the volume of air inspired and expired by the lungs. A spirometer measures ventilation, the movement of air into and out of the lungs. The spirogram will identify two different types of abnormal ventilat ...
or a camera and markers. The same monitoring techniques, as well as 4DCT imaging, can also be for respiratory gated treatment, where the patient breathes freely and the beam is only engaged at certain points in the breathing cycle. Other techniques include using 4DCT imaging to plan treatments with margins that account for motion, and active movement of the treatment couch, or beam, to follow motion.
Contact X-ray brachytherapy
Contact X-ray brachytherapy (also called "CXB", "electronic brachytherapy" or the "Papillon Technique") is a type of radiation therapy using kilovoltage X-ray
An X-ray, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 picometers to 10 nanometers, corresponding to frequencies in the range 30&nb ...
s applied close to the tumour to treat rectal cancer
Colorectal cancer (CRC), also known as bowel cancer, colon cancer, or rectal cancer, is the development of cancer from the colon or rectum (parts of the large intestine). Signs and symptoms may include blood in the stool, a change in bowel ...
. The process involves inserting the X-ray tube
An X-ray tube is a vacuum tube that converts electrical input power into X-rays. The availability of this controllable source of X-rays created the field of radiography, the imaging of partly opaque objects with penetrating radiation. In contrast ...
through the anus into the rectum and placing it against the cancerous tissue, then high doses of X-rays are emitted directly into the tumor
A neoplasm () is a type of abnormal and excessive growth of tissue. The process that occurs to form or produce a neoplasm is called neoplasia. The growth of a neoplasm is uncoordinated with that of the normal surrounding tissue, and persists ...
at two weekly intervals. It is typically used for treating early rectal cancer in patients who may not be candidates for surgery.[
]
Brachytherapy (sealed source radiotherapy)
 Brachytherapy is delivered by placing radiation source(s) inside or next to the area requiring treatment. Brachytherapy is commonly used as an effective treatment for cervical,
Brachytherapy is delivered by placing radiation source(s) inside or next to the area requiring treatment. Brachytherapy is commonly used as an effective treatment for cervical,[
] prostate,[
] breast,[
] and skin cancer[
] and can also be used to treat tumours in many other body sites.[
]
In brachytherapy, radiation sources are precisely placed directly at the site of the cancerous tumour. This means that the irradiation only affects a very localized area – exposure to radiation of healthy tissues further away from the sources is reduced. These characteristics of brachytherapy provide advantages over external beam radiation therapy – the tumour can be treated with very high doses of localized radiation, whilst reducing the probability of unnecessary damage to surrounding healthy tissues.[
] A course of brachytherapy can often be completed in less time than other radiation therapy techniques. This can help reduce the chance of surviving cancer cells dividing and growing in the intervals between each radiation therapy dose.
Radionuclide therapy
Radionuclide therapy (also known as systemic radioisotope therapy, radiopharmaceutical therapy, or molecular radiotherapy), is a form of targeted therapy. Targeting can be due to the chemical properties of the isotope such as radioiodine which is specifically absorbed by the thyroid gland a thousandfold better than other bodily organs. Targeting can also be achieved by attaching the radioisotope to another molecule or antibody to guide it to the target tissue. The radioisotopes are delivered through infusion
Infusion is the process of extracting chemical compounds or flavors from plant material in a solvent such as water, oil or alcohol, by allowing the material to remain suspended in the solvent over time (a process often called steeping). An in ...
(into the bloodstream) or ingestion. Examples are the infusion of metaiodobenzylguanidine (MIBG) to treat neuroblastoma, of oral iodine-131 to treat thyroid cancer or thyrotoxicosis
Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormones by the thyroid gland. Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidism. ...
, and of hormone-bound lutetium-177 and yttrium-90
Yttrium-90 () is an isotope of yttrium. Yttrium-90 has found a wide range of uses in radiation therapy to treat some forms of cancer.
Decay
undergoes β− decay to zirconium-90 with a half-life of 64.1 hours and a decay energy of 2.28 M ...
to treat neuroendocrine tumors
Neuroendocrine tumors (NETs) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They most commonly occur in the intestine, where they are often called carcinoid tumors, but they are also found in the pancreas, lun ...
( peptide receptor radionuclide therapy).
Another example is the injection of radioactive yttrium-90 or holmium-166 microspheres into the hepatic artery
The common hepatic artery is a short blood vessel that supplies oxygenated blood to the liver, pylorus of the stomach, duodenum, pancreas, and gallbladder.
It arises from the celiac artery and has the following branches:
Additional images
...
to radioembolize liver tumors or liver metastases. These microspheres are used for the treatment approach known as selective internal radiation therapy
Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer. It is general ...
. The microspheres are approximately 30 µm in diameter (about one-third of a human hair) and are delivered directly into the artery supplying blood to the tumors. These treatments begin by guiding a catheter
In medicine, a catheter (/ˈkæθətər/) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgi ...
up through the femoral artery in the leg, navigating to the desired target site and administering treatment. The blood feeding the tumor will carry the microspheres directly to the tumor enabling a more selective approach than traditional systemic chemotherapy. There are currently three different kinds of microspheres: SIR-Spheres, TheraSphere and QuiremSpheres.
A major use of systemic radioisotope therapy is in the treatment of bone metastasis
Bone metastasis, or osseous metastatic disease, is a category of cancer metastases that results from primary tumor invasion to bone. Bone-originating primary tumors such as osteosarcoma, chondrosarcoma, and Ewing's sarcoma are rare; the most com ...
from cancer. The radioisotopes travel selectively to areas of damaged bone, and spare normal undamaged bone. Isotopes commonly used in the treatment of bone metastasis are radium-223
Radium-223 (223Ra, Ra-223) is an isotope of radium with an 11.4-day half-life. It was discovered in 1905 by T. Godlewski, a Polish chemist from Kraków, and was historically known as actinium X (AcX). Radium-223 dichloride is an alpha particle- ...
, strontium-89
Strontium-89 () is a radioactive isotope of strontium produced by nuclear fission, with a half-life of 50.57 days. It undergoes β− decay into yttrium-89. Strontium-89 has an application in medicine.
History
It was used for the first time by ...
and samarium (153Sm) lexidronam.
In 2002, the United States Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food s ...
(FDA) approved ibritumomab tiuxetan
Ibritumomab tiuxetan (pronounced ), sold under the trade name Zevalin, is a monoclonal antibody radioimmunotherapy treatment for non-Hodgkin's lymphoma. The drug uses the monoclonal mouse IgG1 antibody ibritumomab in conjunction with the chelator ...
(Zevalin), which is an anti-CD20
B-lymphocyte antigen CD20 or CD20 is expressed on the surface of all B-cells beginning at the pro-B phase ( CD45R+, CD117+) and progressively increasing in concentration until maturity.
In humans CD20 is encoded by the ''MS4A1'' gene.
This gene ...
monoclonal antibody
A monoclonal antibody (mAb, more rarely called moAb) is an antibody produced from a cell Lineage made by cloning a unique white blood cell. All subsequent antibodies derived this way trace back to a unique parent cell.
Monoclonal antibodies ...
conjugated to yttrium-90.
In 2003, the FDA approved the tositumomab/iodine (131I) tositumomab regimen (Bexxar), which is a combination of an iodine-131 labelled and an unlabelled anti-CD20 monoclonal antibody.
These medications were the first agents of what is known as radioimmunotherapy, and they were approved for the treatment of refractory non-Hodgkin's lymphoma
Non-Hodgkin lymphoma (NHL), also known as non-Hodgkin's lymphoma, is a group of hematological malignancy, blood cancers that includes all types of lymphomas except Hodgkin lymphomas. Symptoms include lymphadenopathy, enlarged lymph nodes, fever ...
.
Intraoperative radiotherapy
Intraoperative radiation therapy (IORT) is applying therapeutic levels of radiation to a target area, such as a cancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal b ...
tumor, while the area is exposed during surgery.
Rationale
The rationale for IORT is to deliver a high dose of radiation precisely to the targeted area with minimal exposure of surrounding tissues which are displaced or shielded during the IORT. Conventional radiation techniques such as external beam radiotherapy (EBRT) following surgical removal of the tumor have several drawbacks: The tumor bed where the highest dose should be applied is frequently missed due to the complex localization of the wound cavity even when modern radiotherapy planning is used. Additionally, the usual delay between the surgical removal of the tumor and EBRT may allow a repopulation of the tumor cells. These potentially harmful effects can be avoided by delivering the radiation more precisely to the targeted tissues leading to immediate sterilization of residual tumor cells. Another aspect is that wound fluid has a stimulating effect on tumor cells. IORT was found to inhibit the stimulating effects of wound fluid.
History
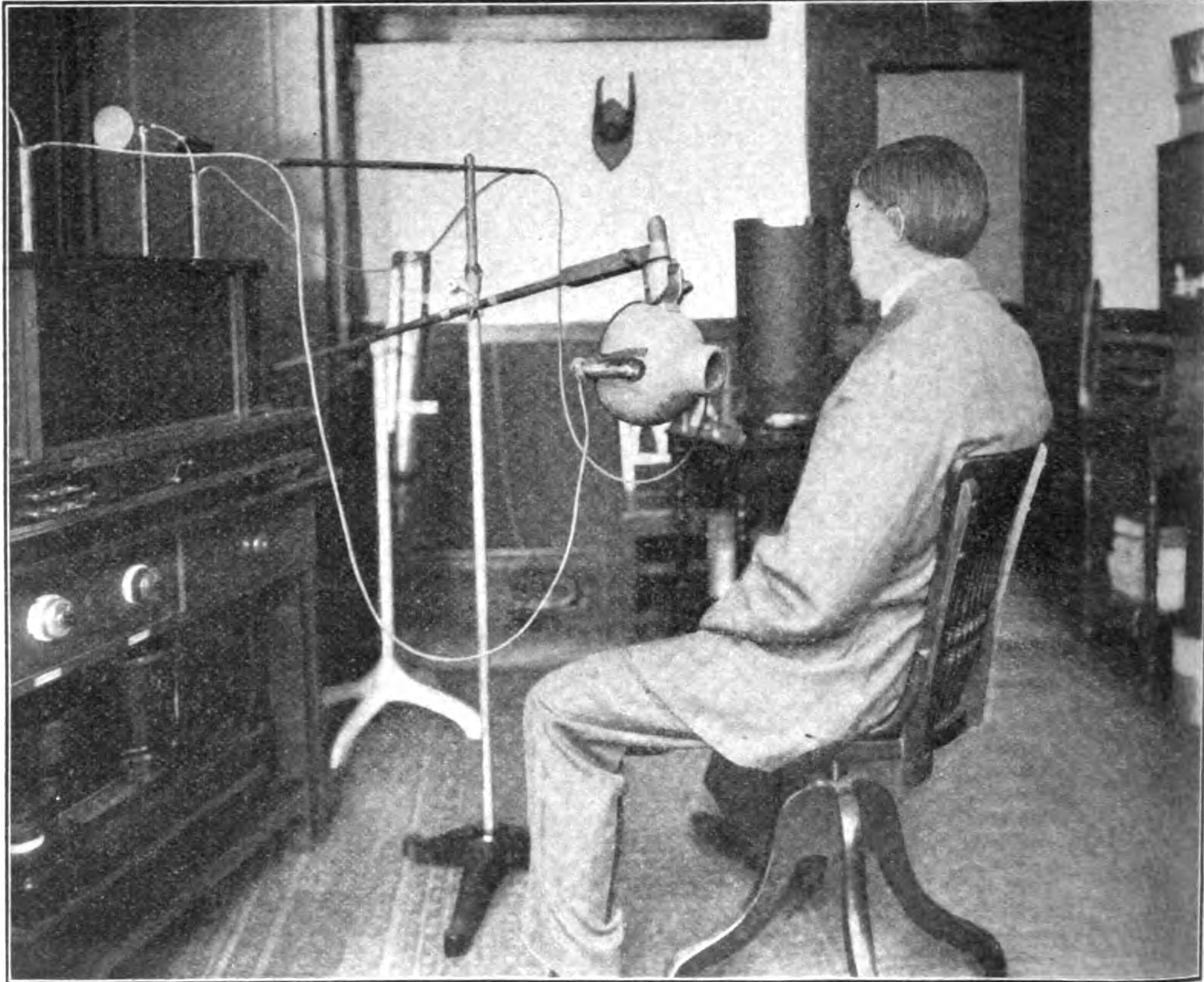 Medicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of X-rays in 1895 by Wilhelm Röntgen.
Medicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of X-rays in 1895 by Wilhelm Röntgen.Nobel Prize
The Nobel Prizes ( ; sv, Nobelpriset ; no, Nobelprisen ) are five separate prizes that, according to Alfred Nobel's will of 1895, are awarded to "those who, during the preceding year, have conferred the greatest benefit to humankind." Alfr ...
–winning scientist Marie Curie (1867–1934), who discovered the radioactive elements polonium
Polonium is a chemical element with the symbol Po and atomic number 84. Polonium is a chalcogen. A rare and highly radioactive metal with no stable isotopes, polonium is chemically similar to selenium and tellurium, though its metallic character ...
and radium in 1898. This began a new era in medical treatment and research.X-ray tube
An X-ray tube is a vacuum tube that converts electrical input power into X-rays. The availability of this controllable source of X-rays created the field of radiography, the imaging of partly opaque objects with penetrating radiation. In contrast ...
. External beam radiotherapy (teletherapy) began at the turn of the century with relatively low voltage (<150 kV) X-ray machines. It was found that while superficial tumors could be treated with low voltage X-rays, more penetrating, higher energy beams were required to reach tumors inside the body, requiring higher voltages. Orthovoltage X-rays, which used tube voltages of 200-500 kV, began to be used during the 1920s. To reach the most deeply buried tumors without exposing intervening skin and tissue to dangerous radiation doses required rays with energies of 1 MV or above, called "megavolt" radiation. Producing megavolt X-rays required voltages on the X-ray tube of 3 to 5 million volts, which required huge expensive installations. Megavoltage X-ray units were first built in the late 1930s but because of cost were limited to a few institutions. One of the first, installed at St. Bartholomew's hospital, London in 1937 and used until 1960, used a 30 foot long X-ray tube and weighed 10 tons. Radium produced megavolt gamma rays, but was extremely rare and expensive due to its low occurrence in ores. In 1937 the entire world supply of radium for radiotherapy was 50 grams, valued at £800,000, or $50 million in 2005 dollars.
The invention of the nuclear reactor
A nuclear reactor is a device used to initiate and control a fission nuclear chain reaction or nuclear fusion reactions. Nuclear reactors are used at nuclear power plants for electricity generation and in nuclear marine propulsion. Heat fr ...
in the Manhattan Project during World War 2 made possible the production of artificial radioisotope
A radionuclide (radioactive nuclide, radioisotope or radioactive isotope) is a nuclide that has excess nuclear energy, making it unstable. This excess energy can be used in one of three ways: emitted from the nucleus as gamma radiation; transferr ...
s for radiotherapy. Cobalt therapy
Cobalt therapy is the medical use of gamma rays from the radioisotope cobalt-60 to treat conditions such as cancer. Beginning in the 1950s, cobalt-60 was widely used in external beam radiotherapy (teletherapy) machines, which produced a beam ...
, teletherapy machines using megavolt gamma rays emitted by cobalt-60, a radioisotope produced by irradiating ordinary cobalt metal in a reactor, revolutionized the field between the 1950s and the early 1980s. Cobalt machines were relatively cheap, robust and simple to use, although due to its 5.27 year half-life the cobalt had to be replaced about every 5 years.
Medical linear particle accelerator
A linear particle accelerator (often shortened to linac) is a type of particle accelerator that accelerates charged subatomic particles or ions to a high speed by subjecting them to a series of oscillating electric potentials along a linear b ...
s, developed since the 1940s, began replacing X-ray and cobalt units in the 1980s and these older therapies are now declining. The first medical linear accelerator was used at the Hammersmith Hospital in London in 1953.
See also
* Beam spoiler
* Cancer and nausea
* Fast neutron therapy
* Neutron capture therapy of cancer
* Particle beam
A particle beam is a stream of charged or neutral particles. In particle accelerators, these particles can move with a velocity close to the speed of light. There is a difference between the creation and control of charged particle beams and ne ...
* Radiation therapist
* Selective internal radiation therapy
Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer. It is general ...
* Treatment of cancer
Cancer can be treated by surgery, chemotherapy, radiation therapy, hormonal therapy, targeted therapy (including immunotherapy such as monoclonal antibody therapy) and synthetic lethality, most commonly as a series of separate treatments ...
References
Further reading
*
*
*
* McGarry, M (2002). ''Radiation therapy in Treatment''. AUSG Books.
*
External links
;Information
Human Health Campus The official website of the International Atomic Energy Agency dedicated to Professionals in Radiation Medicine. This site is managed by the Division of Human Health, Department of Nuclear Sciences and Applications
RT Answers – ASTRO: patient information site
The Radiation Therapy Oncology Group: an organisation for radiation oncology research
RadiologyInfo
-The radiology information resource for patients: Radiation Therapy
Source of cancer stem cells' resistance to radiation
explained on YouTube.
Cancer Management Handbook: Principles of Radiation Therapy
Biologically equivalent dose calculator
Radiobiology Treatment Gap Compensator Calculator
;About the profession
PROS (Paediatric Radiation Oncology Society)
American Society for Radiation Oncology – ASTRO: the official site for radiation oncologists
European Society for Therapeutic Radiology and Oncology
Who does what in Radiation Oncology?
– Responsibilities of the various personnel within Radiation Oncology in the United States
;Accidents and QA
Verification of dose calculations in radiation therapy
{{Authority control
Radioactivity
Radiation health effects
Medical physics
Radiobiology
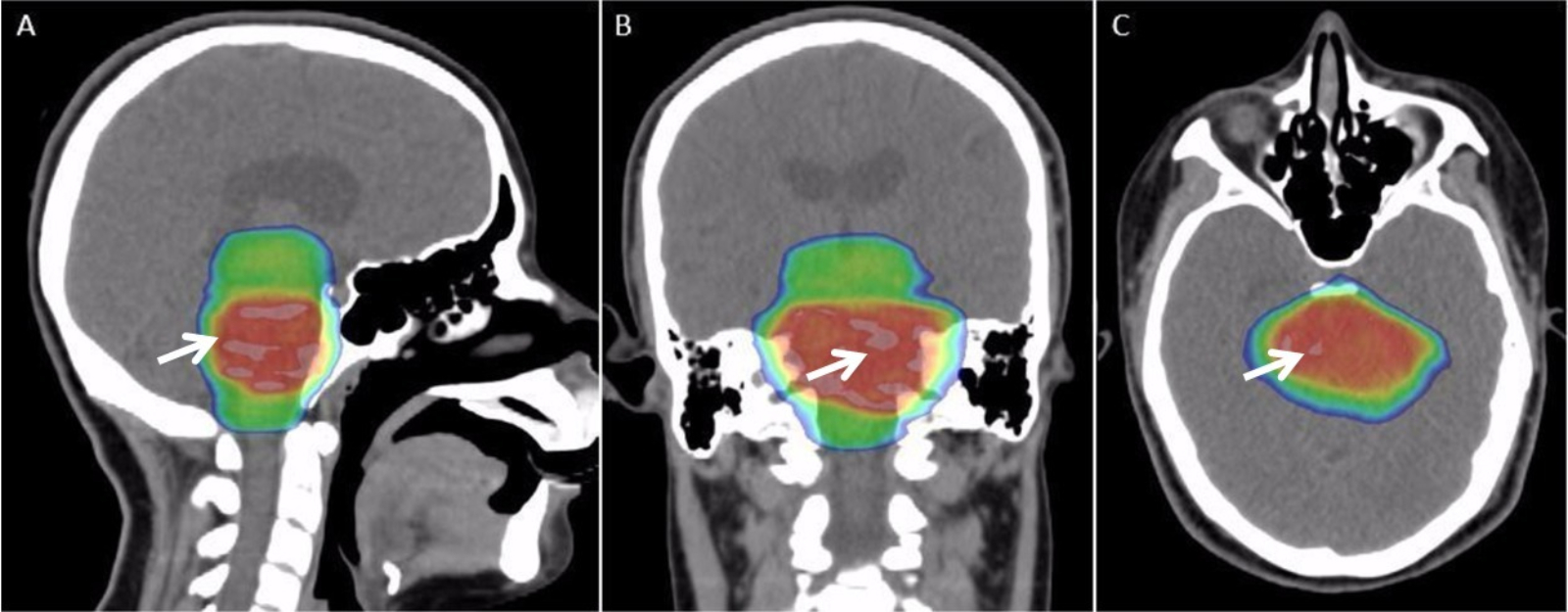 Different cancers respond to radiation therapy in different ways.
The response of a cancer to radiation is described by its radiosensitivity.
Highly radiosensitive cancer cells are rapidly killed by modest doses of radiation. These include
Different cancers respond to radiation therapy in different ways.
The response of a cancer to radiation is described by its radiosensitivity.
Highly radiosensitive cancer cells are rapidly killed by modest doses of radiation. These include  : The gastrointestinal tract can be damaged following abdominal and pelvic radiotherapy. Atrophy, fibrosis and vascular changes produce
: The gastrointestinal tract can be damaged following abdominal and pelvic radiotherapy. Atrophy, fibrosis and vascular changes produce  Radiation therapy is used to treat early stage Dupuytren's disease and
Radiation therapy is used to treat early stage Dupuytren's disease and  Intensity-modulated radiation therapy (IMRT) is an advanced type of high-precision radiation that is the next generation of 3DCRT. IMRT also improves the ability to conform the treatment volume to concave tumor shapes, for example when the tumor is wrapped around a vulnerable structure such as the spinal cord or a major organ or blood vessel. Computer-controlled X-ray accelerators distribute precise radiation doses to malignant tumors or specific areas within the tumor. The pattern of radiation delivery is determined using highly tailored computing applications to perform
Intensity-modulated radiation therapy (IMRT) is an advanced type of high-precision radiation that is the next generation of 3DCRT. IMRT also improves the ability to conform the treatment volume to concave tumor shapes, for example when the tumor is wrapped around a vulnerable structure such as the spinal cord or a major organ or blood vessel. Computer-controlled X-ray accelerators distribute precise radiation doses to malignant tumors or specific areas within the tumor. The pattern of radiation delivery is determined using highly tailored computing applications to perform  Brachytherapy is delivered by placing radiation source(s) inside or next to the area requiring treatment. Brachytherapy is commonly used as an effective treatment for cervical,
prostate,
breast,
and skin cancer
and can also be used to treat tumours in many other body sites.
In brachytherapy, radiation sources are precisely placed directly at the site of the cancerous tumour. This means that the irradiation only affects a very localized area – exposure to radiation of healthy tissues further away from the sources is reduced. These characteristics of brachytherapy provide advantages over external beam radiation therapy – the tumour can be treated with very high doses of localized radiation, whilst reducing the probability of unnecessary damage to surrounding healthy tissues.
A course of brachytherapy can often be completed in less time than other radiation therapy techniques. This can help reduce the chance of surviving cancer cells dividing and growing in the intervals between each radiation therapy dose.
As one example of the localized nature of breast brachytherapy, the SAVI device delivers the radiation dose through multiple catheters, each of which can be individually controlled. This approach decreases the exposure of healthy tissue and resulting side effects, compared both to external beam radiation therapy and older methods of breast brachytherapy.
Brachytherapy is delivered by placing radiation source(s) inside or next to the area requiring treatment. Brachytherapy is commonly used as an effective treatment for cervical,
prostate,
breast,
and skin cancer
and can also be used to treat tumours in many other body sites.
In brachytherapy, radiation sources are precisely placed directly at the site of the cancerous tumour. This means that the irradiation only affects a very localized area – exposure to radiation of healthy tissues further away from the sources is reduced. These characteristics of brachytherapy provide advantages over external beam radiation therapy – the tumour can be treated with very high doses of localized radiation, whilst reducing the probability of unnecessary damage to surrounding healthy tissues.
A course of brachytherapy can often be completed in less time than other radiation therapy techniques. This can help reduce the chance of surviving cancer cells dividing and growing in the intervals between each radiation therapy dose.
As one example of the localized nature of breast brachytherapy, the SAVI device delivers the radiation dose through multiple catheters, each of which can be individually controlled. This approach decreases the exposure of healthy tissue and resulting side effects, compared both to external beam radiation therapy and older methods of breast brachytherapy.
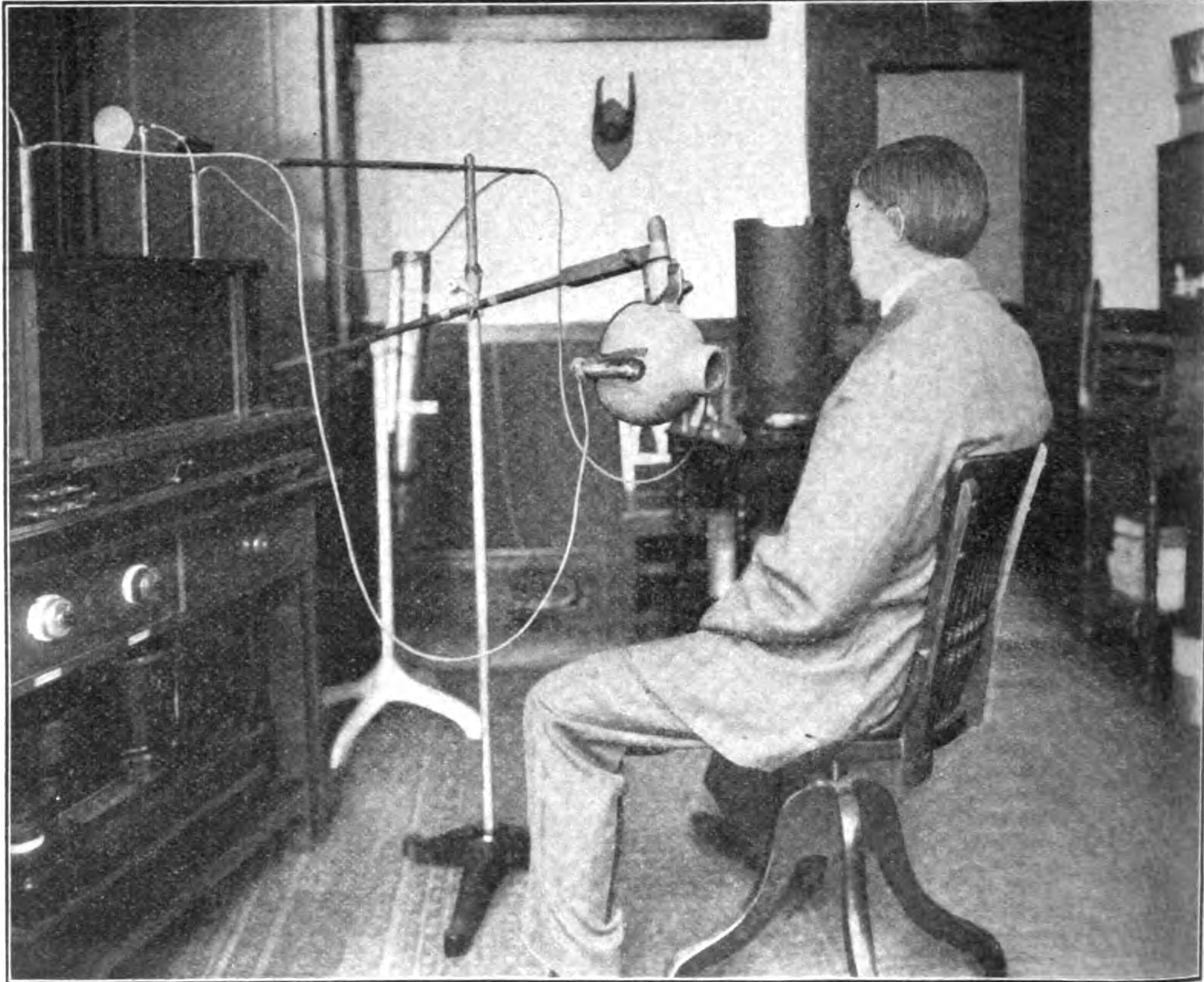 Medicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of X-rays in 1895 by Wilhelm Röntgen. Emil Grubbe of Chicago was possibly the first American physician to use X-rays to treat cancer, beginning in 1896.
The field of radiation therapy began to grow in the early 1900s largely due to the groundbreaking work of
Medicine has used radiation therapy as a treatment for cancer for more than 100 years, with its earliest roots traced from the discovery of X-rays in 1895 by Wilhelm Röntgen. Emil Grubbe of Chicago was possibly the first American physician to use X-rays to treat cancer, beginning in 1896.
The field of radiation therapy began to grow in the early 1900s largely due to the groundbreaking work of