Temporomandibular joint dysfunction (TMD, TMJD) is an umbrella term covering
pain
Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, ...
and dysfunction of the
muscles of mastication
There are four classical muscles of mastication. During mastication, three muscles of mastication (''musculi masticatorii'') are responsible for adduction of the jaw, and one (the lateral pterygoid) helps to abduct it. All four move the jaw late ...
(the muscles that move the jaw) and the
temporomandibular joints (the joints which connect the
mandible to the
skull). The most important feature is pain, followed by restricted mandibular movement,
and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to
quality of life;
[ ] this is because the symptoms can become chronic and difficult to manage.
In this article, the term ''temporomandibular disorder'' is taken to mean any disorder that affects the temporomandibular joint, and ''temporomandibular joint dysfunction'' (here also abbreviated to TMD) is taken to mean symptomatic (e.g. pain, limitation of movement, clicking) dysfunction of the temporomandibular joint. However, there is no single, globally accepted term or definition
concerning this topic.
TMDs have a range of causes and often co-occur with a number of overlapping medical conditions, including headaches, fibromyalgia, back pain, and irritable bowel. However, these factors are poorly understood,
and there is disagreement as to their relative importance. There are many treatments available,
although there is a general lack of evidence for any treatment in TMD, and no widely accepted treatment protocol. Common treatments include provision of occlusal splints, psychosocial interventions like
cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. CBT focuses on challenging and changing cognitive distortions (suc ...
, physical therapy, and
pain medication
An analgesic drug, also called simply an analgesic (American English), analgaesic (British English), pain reliever, or painkiller, is any member of the group of drugs used to achieve relief from pain (that is, analgesia or pain management). It i ...
or others. Most sources agree that no irreversible treatment should be carried out for TMD.
About 20% to 30% of the adult population are affected to some degree.
[ ] Usually people affected by TMD are between 20 and 40 years of age,
and it is more common in females than males.
TMD is the second most frequent cause of
orofacial pain
Orofacial pain is a general term covering any pain which is felt in the mouth, jaws and the face. Orofacial pain is a common symptom, and there are many causes.
Orofacial Pain (OFP) is the specialty of dentistry that encompasses the diagnosis, ma ...
after dental pain (i.e.
toothache).
Classification
TMD is considered by some to be one of the 4 major symptom complexes in chronic orofacial pain, along with
burning mouth syndrome,
atypical facial pain and
atypical odontalgia.
[ ] TMD has been considered as a type of
musculoskeletal,
,
or
rheumatological disorder.
It has also been called a
functional
Functional may refer to:
* Movements in architecture:
** Functionalism (architecture)
** Form follows function
* Functional group, combination of atoms within molecules
* Medical conditions without currently visible organic basis:
** Functional sy ...
pain syndrome,
and a
psychogenic disorder.
Others consider TMD a "central sensitivity syndrome", in reference to evidence that TMD might be caused by a
centrally mediated sensitivity to pain.
It is hypothesized that there is a great deal of similarity between TMD and other pain syndromes like
fibromyalgia
Fibromyalgia (FM) is a medical condition defined by the presence of chronic widespread pain, fatigue, waking unrefreshed, cognitive symptoms, lower abdominal pain or cramps, and depression. Other symptoms include insomnia and a general hyp ...
,
irritable bowel syndrome,
interstitial cystitis, headache, chronic lower
back pain and chronic
neck pain. These disorders have also been theorized to be caused by centrally mediated sensitivity to pain, and furthermore they often occur together.
Definitions and terminology
Frequently, TMD has been treated as a single
syndrome, but the prevailing modern view is that TMD is a cluster of related disorders with many common features.
Indeed, some have suggested that, in the future, the term ''TMD'' may be discarded as the different causes are fully identified and separated into different conditions.
Sometimes, "temporomandibular joint dysfunction" is described as the most common form of temporomandibular disorder,
[ ] whereas many other sources use the term ''temporomandibular disorder'' synonymously, or instead of the term ''temporomandibular joint dysfunction''. In turn, the term ''temporomandibular disorder'' is defined as "musculoskeletal disorders affecting the temporomandibular joints and their associated musculature. It is a collective term which represents a diverse group of pathologies involving the temporomandibular joint, the muscles of mastication, or both".
Another definition of temporomandibular disorders is "a group of conditions with similar signs and symptoms that affect the temporomandibular joints, the muscles of mastication, or both."
''Temporomandibular disorder'' is a term that creates confusion since it refers to a group of similarly symptomatic conditions, whilst many sources use the term ''temporomandibular disorders'' as a vague description, rather than a specific syndrome, and refer to any condition which may affect the temporomandibular joints (see table). The temporomandibular joint is susceptible to a huge range of diseases, some rarer than others, and there is no implication that all of these will cause any symptoms or limitation in function at all.
The preferred terms in medical publications is to an extent influenced by geographic location. For example, in the
United Kingdom, the term ''pain dysfunction syndrome'' is in common use.
In the United States, the term ''temporomandibular disorder'' is generally favored. The American Academy of Orofacial Pain uses ''temporomandibular disorder'', whilst the
National Institute of Dental and Craniofacial Research
The National Institute of Dental and Craniofacial Research (NIDCR) is a branch of the U.S. National Institutes of Health. The institute aims to improve the oral, dental, and craniofacial health through research and the distribution of important he ...
uses ''temporomandibular joint disorder''.
A more complete list of synonyms for this topic is extensive, with some being more commonly used than others. In addition to those already mentioned, examples include ''temporomandibular joint pain dysfunction syndrome'', ''temporomandibular pain dysfunction syndrome'', ''temporomandibular joint syndrome'', ''temporomandibular dysfunction syndrome'', ''temporomandibular dysfunction'', ''temporomandibular disorder'', ''temporomandibular syndrome'', ''facial arthromyalgia'', ''myofacial pain dysfunction syndrome'', ''craniomandibular dysfunction'' (CMD), ''myofacial pain dysfunction'', ''masticatory myalgia'', ''mandibular dysfunction'', and ''Costen's syndrome''.
The lack of standardization in terms is not restricted to medical papers. Notable internationally recognized sources vary in both their preferred term, and their offered definition. For example:
By cause and symptoms
It has been suggested that TMD may develop following physical trauma, particularly
whiplash injury, although the evidence for this is not conclusive. This type of TMD is sometimes termed "posttraumatic TMD" (pTMD) to distinguish it from TMD of unknown cause, sometimes termed "
idiopathic TMD" (iTMD).
Sometimes muscle-related (myogenous) TMD (also termed myogenous TMD, or TMD secondary to myofascial pain and dysfunction) is distinguished from joint-related TMD (also termed arthogenous TMD, or TMD secondary to true articular disease), based upon whether the muscles of mastication or the TMJs themselves are predominantly involved. This classification, which effectively divides TMD into 2 syndromes, is followed by the American Academy of Orofacial Pain.
However, since most people with TMD could be placed into both of these groups, which makes a single diagnosis difficult when this classification is used. The Research Diagnostic Criteria (RDC/TMD) allows for multiple diagnoses in an attempt to overcome the problems with other classifications. RDC/TMD considers temporomandibular disorders in 2 axes; axis I is the physical aspects, and axis II involves assessment of psychological status, mandibular function and TMD-related psychosocial disability.
Axis I is further divided into 3 general groups. Group I are muscle disorders, group II are disc displacements and group III are joint disorders,
although it is common for people with TMD to fit into more than one of these groups.
By duration
Sometimes distinction is made between acute TMD, where symptoms last for less than 3 months, and chronic TMD, where symptoms last for more than 3 months.
Not much is known about acute TMD since these individuals do not typically attend in
secondary care (hospital).
Signs and symptoms
Signs and symptoms of temporomandibular joint disorder vary in their presentation. The symptoms will usually involve more than one of the various components of the masticatory system,
muscle
Skeletal muscles (commonly referred to as muscles) are organs of the vertebrate muscular system and typically are attached by tendons to bones of a skeleton. The muscle cells of skeletal muscles are much longer than in the other types of muscl ...
s,
nerves,
tendons
A tendon or sinew is a tough, high-tensile-strength band of dense fibrous connective tissue that connects muscle to bone. It is able to transmit the mechanical forces of muscle contraction to the skeletal system without sacrificing its ability ...
,
ligaments,
bones,
connective tissue
Connective tissue is one of the four primary types of animal tissue, along with epithelial tissue, muscle tissue, and nervous tissue. It develops from the mesenchyme derived from the mesoderm the middle embryonic germ layer. Connective tiss ...
, or the
teeth.
The three classically described, cardinal signs and symptoms of TMD are:
* Pain and tenderness on
palpation in the muscles of mastication, or of the joint itself (preauricular pain – pain felt just in front of the ear). Pain is the defining feature of TMD and is usually aggravated by manipulation or function,
such as when chewing, clenching,
or yawning, and is often worse upon waking. The character of the pain is usually dull or aching, poorly localized,
and intermittent, although it can sometimes be constant. The pain is more usually unilateral (located on one side) rather than bilateral.
It is rarely severe.
* Limited range of mandibular movement,
which may cause difficulty eating or even talking. There may be locking of the jaw, or stiffness in the jaw muscles and the joints, especially present upon waking.
There may also be incoordination, asymmetry or deviation of mandibular movement.
* Noises from the joint during mandibular movement, which may be intermittent.
Joint noises may be described as clicking,
popping,
or crepitus (grating).
TMJ dysfunction is commonly associated with symptoms affecting cervical spine dysfunction and altered head and cervical spine posture.
Other signs and symptoms have also been described, although these are less common and less significant than the cardinal signs and symptoms listed above. Examples include:
* Headache (possibly),
e.g. pain in the
occipital region
The occipital bone () is a cranial dermal bone and the main bone of the occiput (back and lower part of the skull). It is trapezoidal in shape and curved on itself like a shallow dish. The occipital bone overlies the occipital lobes of the cereb ...
(the back of the head), or the forehead;
or other types of facial pain including
migraine
Migraine (, ) is a common neurological disorder characterized by recurrent headaches. Typically, the associated headache affects one side of the head, is pulsating in nature, may be moderate to severe in intensity, and could last from a few hou ...
,
.
or
myofascial pain
Myofascial pain syndrome (MPS), also known as chronic myofascial pain (CMP), is a syndrome characterized by chronic pain in multiple myofascial trigger points ("knots") and fascial (connective tissue) constrictions. It can appear in any body part ...
.
* Pain elsewhere, such as the teeth
or neck.
*
Diminished auditory acuity (hearing loss).
*
Tinnitus (occasionally).
* Dizziness.
* Sensation of malocclusion (feeling that the teeth do not meet together properly).
Causes
TMD is a symptom complex (i.e. a group of symptoms occurring together and characterizing a particular disease), which is thought to be caused by multiple, poorly understood factors,
but the exact etiology is unknown.
There are factors which appear to predispose to TMD (genetic, hormonal, anatomical), factors which may precipitate it (trauma, occlusal changes, parafunction), and also factors which may prolong it (stress and again parafunction).
Overall, two hypotheses have dominated research into the causes of TMD, namely a psychosocial model and a theory of occlusal dysharmony.
Interest in occlusal factors as a causative factor in TMD was especially widespread in the past, and the theory has since fallen out of favor and become controversial due to lack of evidence.
Disc displacement
In people with TMD, it has been shown that the lower head of
lateral pterygoid contracts during mouth closing (when it should relax), and is often tender to palpation. To theorize upon this observation, some have suggested that due to a tear in the back of the joint capsule, the articular disc may be displaced forwards (anterior disc displacement), stopping the upper head of lateral pterygoid from acting to stabilize the disc as it would do normally. As a biologic compensatory mechanism, the lower head tries to fill this role, hence the abnormal muscle activity during mouth closure. There is some evidence that anterior disc displacement is present in a proportion of TMD cases. Anterior disc displacement with reduction refers to abnormal forward movement of the disc during opening which reduces upon closing. Anterior disc displacement without reduction refers to an abnormal forward, bunched-up position of the articular disc which does not reduce. In this latter scenario, the disc is not intermediary between the condyle and the articular fossa as it should be, and hence the articular surfaces of the bones themselves are exposed to a greater degree of wear (which may predispose to osteoarthritis in later life).
Degenerative joint disease
The general term "degenerative joint disease" refers to arthritis (both
osteoarthritis and
rheumatoid arthritis) and arthrosis. The term arthrosis may cause confusion since in the specialized TMD literature it means something slightly different from in the wider medical literature. In medicine generally, arthrosis can be a nonspecific term for a joint, any disease of a joint (or specifically degenerative joint disease), and is also used as a synonym for osteoarthritis. In the specialized literature that has evolved around TMD research, arthrosis is differentiated from arthritis by the presence of low and no inflammation respectively.
Both are however equally degenerative.
The TMJs are sometimes described as one of the most used joints in the body. Over time, either with normal use or with parafunctional use of the joint, wear and degeneration can occur, termed osteoarthritis. Rheumatoid arthritis, an
autoimmune joint disease, can also affect the TMJs. Degenerative joint diseases may lead to defects in the shape of the tissues of the joint, limitation of function (e.g. restricted mandibular movements), and joint pain.
Psychosocial factors
Emotional stress (anxiety, depression, anger) may increase pain by causing
autonomic,
visceral
In biology, an organ is a collection of tissues joined in a structural unit to serve a common function. In the hierarchy of life, an organ lies between tissue and an organ system. Tissues are formed from same type cells to act together in a ...
and skeletal activity and by reduced inhibition via the descending pathways of the
limbic system
The limbic system, also known as the paleomammalian cortex, is a set of brain structures located on both sides of the thalamus, immediately beneath the medial temporal lobe of the cerebrum primarily in the forebrain.Schacter, Daniel L. 2012. ''Ps ...
. The interactions of these biological systems have been described as a vicious "anxiety-pain-tension" cycle which is thought to be frequently involved in TMD. Put simply, stress and anxiety cause grinding of teeth and sustained muscular contraction in the face. This produces pain which causes further anxiety which in turn causes prolonged muscular spasm at trigger points,
vasoconstriction,
ischemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems wi ...
and release of pain mediators. The pain discourages use of the masticatory system (a similar phenomenon in other chronic pain conditions is termed "fear avoidance" behavior), which leads to reduced muscle flexibility, tone, strength and endurance. This manifests as limited mouth opening and a sensation that the teeth are not fitting properly.
Persons with TMD have a higher prevalence of psychological disorders than people without TMD.
People with TMD have been shown to have higher levels of anxiety,
depression, somatization and
sleep deprivation
Sleep deprivation, also known as sleep insufficiency or sleeplessness, is the condition of not having adequate duration and/or quality of sleep to support decent alertness, performance, and health. It can be either chronic or acute and may vary ...
, and these could be considered important
risk factors for the development of TMD.
In the 6 months before the onset, 50–70% of people with TMD report experiencing stressful life events (e.g. involving work, money, health or relationship loss). It has been postulated that such events induce anxiety and cause increased jaw muscle activity. Muscular hyperactivity has also been shown in people with TMD whilst taking examinations or watching horror films.
Others argue that a link between muscular hyperactivity and TMD has not been convincingly demonstrated, and that emotional distress may be more of a consequence of pain rather than a cause.
Bruxism
Bruxism is an oral
parafunctional activity where there is excessive clenching and grinding of the teeth. It can occur during sleep or whilst awake. The cause of bruxism itself is not completely understood, but psychosocial factors appear to be implicated in awake bruxism and
dopamine
Dopamine (DA, a contraction of 3,4-dihydroxyphenethylamine) is a neuromodulatory molecule that plays several important roles in cells. It is an organic compound, organic chemical of the catecholamine and phenethylamine families. Dopamine const ...
rgic dysfunction and other
central nervous system mechanisms may be involved in sleep bruxism. If TMD pain and limitation of mandibular movement are greatest upon waking, and then slowly resolve throughout the day, this may indicate sleep bruxism. Conversely, awake bruxism tends to cause symptoms that slowly get worse throughout the day, and there may be no pain at all upon waking.
The relationship of bruxism with TMD is debated. Many suggest that sleep bruxism can be a causative or contributory factor to pain symptoms in TMD.
Indeed, the symptoms of TMD overlap with those of bruxism.
Others suggest that there is no strong association between TMD and bruxism.
A systematic review investigating the possible relationship concluded that when self-reported bruxism is used to diagnose bruxism, there is a positive association with TMD pain, and when more strict diagnostic criteria for bruxism are used, the association with TMD symptoms is much lower.
Self-reported bruxism is probably a poor method of identifying bruxism.
There are also very many people who grind their teeth and who do not develop TMD.
Bruxism and other parafunctional activities may play a role in perpetuating symptoms in some cases.
Other parafunctional habits such as pen chewing, lip and cheek biting (which may manifest as
morsicatio buccarum or
linea alba), are also suggested to contribute to the development of TMD.
Other parafunctional activities might include jaw thrusting, excessive gum chewing,
nail biting and eating very hard foods.
Trauma
Trauma, both micro and macrotrauma, is sometimes identified as a possible cause of TMD; however, the evidence for this is not strong.
Prolonged mouth opening (hyper-extension) is also suggested as a possible cause. It is thought that this leads to microtrauma and subsequent muscular hyperactivity. This may occur during dental treatment, with oral
intubation whilst under a
general anesthetic
General anaesthetics (or anesthetics, see spelling differences) are often defined as compounds that induce a loss of consciousness in humans or loss of righting reflex in animals. Clinical definitions are also extended to include an induced coma ...
, during singing or wind instrument practice (really these can be thought of as parafunctional activities).
Damage may be incurred during violent yawning, laughing,
road traffic accidents, sports injuries, interpersonal violence, or during dental treatment,
(such as
tooth extraction).
It has been proposed that a link exists between
whiplash injuries (sudden neck hyper-extension usually occurring in road traffic accidents), and the development of TMD. This has been termed "post-traumatic TMD", to separate it from "
idiopathic TMD".
Despite multiple studies having been performed over the years, the cumulative evidence has been described as conflicting, with moderate evidence that TMD can occasionally follow whiplash injury.
The research that suggests a link appears to demonstrate a low to moderate
incidence of TMD following whiplash injury, and that pTMD has a poorer response to treatment than TMD which has not developed in relation to trauma.
Occlusal factors
Occlusal factors as an etiologic factor in TMD is a controversial topic.
Abnormalities of occlusion (problems with the bite) are often blamed for TMD but there is no evidence that these factors are involved.
Occlusal abnormalities are incredibly common, and most people with occlusal abnormalities do not have TMD.
Although occlusal features may affect observed electrical activity in masticatory muscles,
there are no
statistically significant
In statistical hypothesis testing, a result has statistical significance when it is very unlikely to have occurred given the null hypothesis (simply by chance alone). More precisely, a study's defined significance level, denoted by \alpha, is the p ...
differences in the number of occlusal abnormalities in people with TMD and in people without TMD.
There is also no evidence for a causal link between orthodontic treatment and TMD.
The modern, mainstream view is that the vast majority of people with TMD, occlusal factors are not related.
Theories of occlusal factors in TMD are largely of historical interest. A causal relationship between occlusal factors and TMD was championed by Ramfjord in the 1960s.
[ ] A small minority of dentists continue to prescribe occlusal adjustments in the belief that this will prevent or treat TMD despite the existence of systematic reviews of the subject which state that there is no evidence for such practices,
and the vast majority of opinion being that no irreversible treatment should be carried out in TMD (see
Occlusal adjustment).
Genetic factors
TMD does not obviously run in families like a genetic disease. It has been suggested that a genetic predisposition for developing TMD (and chronic pain syndromes generally) could exist. This has been postulated to be explained by variations of the gene which codes for the enzyme
catechol-O-methyl transferase (COMT) which may produce 3 different
phenotypes with regards pain sensitivity. COMT (together with
monoamine oxidase
Monoamine oxidases (MAO) () are a family of enzymes that catalyze the oxidation of monoamines, employing oxygen to clip off their amine group. They are found bound to the outer membrane of mitochondria in most cell types of the body. The first ...
) is involved in breaking down
catecholamines (e.g.
dopamine
Dopamine (DA, a contraction of 3,4-dihydroxyphenethylamine) is a neuromodulatory molecule that plays several important roles in cells. It is an organic compound, organic chemical of the catecholamine and phenethylamine families. Dopamine const ...
,
epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and ...
, and
norepinephrine). The variation of the COMT gene which produces less of this enzyme is associated with a high sensitivity to pain. Females with this variation, are at 2–3 times greater risk of developing TMD than females without this variant. However this theory is controversial since there is conflicting evidence.
Hormonal factors
Since females are more often affected by TMD than males, the
female sex hormone
Sex hormones, also known as sex steroids, gonadocorticoids and gonadal steroids, are steroid hormones that interact with vertebrate steroid hormone receptors. The sex hormones include the androgens, estrogens, and progestogens. Their effects are ...
estrogen has been suggested to be involved.
The results of one study suggested that the periods of highest pain in TMD can be correlated with rapid periods of change in the circulating estrogen level. Low estrogen was also correlated to higher pain.
In the
menstrual cycle
The menstrual cycle is a series of natural changes in hormone production and the structures of the uterus and ovaries of the female reproductive system that make pregnancy possible. The ovarian cycle controls the production and release of eggs a ...
, estrogen levels fluctuate rapidly during
ovulation, and also rapidly increases just before menstruation and rapidly decreases during menstruation.
Post-menopausal
Menopause, also known as the climacteric, is the time in women's lives when menstrual periods stop permanently, and they are no longer able to bear children. Menopause usually occurs between the age of 47 and 54. Medical professionals often d ...
females who are treated with
hormone replacement therapy are more likely to develop TMD, or may experience an exacerbation if they already had TMD. Several possible mechanisms by which estrogen might be involved in TMD symptoms have been proposed. Estrogen may play a role in modulating joint inflammation,
nociceptive neuron
A nociceptor ("pain receptor" from Latin ''nocere'' 'to harm or hurt') is a sensory neuron that responds to damaging or potentially damaging stimuli by sending "possible threat" signals to the spinal cord and the brain. The brain creates the sens ...
s in the trigeminal nerve, muscle reflexes to pain and
μ-opioid receptor
The μ-opioid receptors (MOR) are a class of opioid receptors with a high affinity for enkephalins and beta-endorphin, but a low affinity for dynorphins. They are also referred to as μ(''mu'')-opioid peptide (MOP) receptors. The prototypical � ...
s.
Possible associations
TMD has been suggested to be associated with other conditions or factors, with varying degrees of evidence and some more commonly than others. E.g. It has been shown that 75% of people with TMD could also be diagnosed with fibromyalgia, since they met the diagnostic criteria, and that conversely, 18% of people with fibromyalgia met diagnostic criteria for TMD.
A possible link between many of these chronic pain conditions has been hypothesized to be due to shared pathophysiological mechanisms, and they have been collectively termed "central sensitivity syndromes",
although other apparent associations cannot be explained in this manner. Recently a plethora of research has substantiated a causal relationship between TMD and Obstructive Sleep Apnea (OSA). Severe TMD restricts oral airway opening, and can result in a retrognathic posture that results in glossal blockage of the oropharynx as the tongue relaxes in sleep. This mechanism is exacerbated by alcohol consumption, as well as other chemicals that result in reduced myotonic status of the oropharynx.
* Obstructive sleep apnea.
* Headache.
* Chronic neck pain.
* Chronic back pain.
* Systemic joint laxity.
*
Rheumatoid arthritis.
* Irritable bowel syndrome.
* Interstitial cystitis.
* Regular
scuba diving.
Pathophysiology
Anatomy and physiology
Temporomandibular joints
The temporomandibular joints are the dual articulation of the mandible with the skull. Each TMJ is classed as a "ginglymoarthrodial" joint since it is both a
ginglymus (hinging joint) and an
arthrodial (sliding) joint,
and involves the condylar process of the mandible below, and the articular fossa (or glenoid fossa) of the
temporal bone above. Between these articular surfaces is the articular disc (or meniscus), which is a biconcave, transversely oval disc composed of dense fibrous connective tissue. Each TMJ is covered by a fibrous capsule. There are tight fibers connecting the mandible to the disc, and loose fibers which connect the disc to the temporal bone, meaning there are in effect 2 joint capsules, creating an upper joint space and a lower joint space, with the articular disc in between. The
synovial membrane
The synovial membrane (also known as the synovial stratum, synovium or stratum synoviale) is a specialized connective tissue that lines the inner surface of capsules of synovial joints and tendon sheath. It makes direct contact with the fibrous ...
of the TMJ lines the inside of the fibrous capsule apart from the articular surfaces and the disc. This membrane secretes
synovial fluid
Synovial fluid, also called synovia, elp 1/sup> is a viscous, non-Newtonian fluid found in the cavities of synovial joints. With its egg white–like consistency, the principal role of synovial fluid is to reduce friction between the articular ...
, which is both a lubricant to fill the joint spaces, and a means to convey nutrients to the tissues inside the joint. Behind the disc is loose vascular tissue termed the "bilaminar region" which serves as a posterior attachment for the disc and also fills with blood to fill the space created when the head of the condyle translates down the articular eminence.
Due to its concave shape, sometimes the articular disc is described as having an anterior band, intermediate zone and a posterior band.
When the mouth is opened, the initial movement of the mandibular condyle is rotational, and this involves mainly the lower joint space, and when the mouth is opened further, the movement of the condyle is translational, involving mainly the upper joint space.
This translation movement is achieved by the condylar head sliding down the articular eminence, which constitutes the front border of the articular fossa.
The function of the articular eminence is to limit the forwards movement of the condyle.
The ligament directly associated with the TMJ is the
temporomandibular ligament
The temporomandibular ligament, also known as the external lateral ligament, is a ligament that connects the lower articular tubercle of the zygomatic arch to the lateral and posterior border of the neck of the mandible. It prevents posterior disp ...
, also termed the lateral ligament, which really is a thickening of the lateral aspect of the fibrous capsule.
The
stylomandibular ligament
The stylomandibular ligament is the thickened posterior portion of the investing cervical fascia around the neck. It extends from near the apex of the styloid process of the temporal bone to the angle and posterior border of the angle of the man ...
and the
sphenomandibular ligament
The sphenomandibular ligament (internal lateral ligament) is one of the three ligaments of the temporomandibular joint. It is situated medially to - and generally separate from - the articular capsule of the joint. Superiorly, it is attached to the ...
are not directly associated with the joint capsule. Together, these ligaments act to restrict the extreme movements of the joint.
Muscles of mastication
The muscles of mastication are paired on each side and work together to produce the movements of the mandible. The main muscles involved are the masseter, temporalis and medial and lateral pterygoid muscles.
File:Gray383.png, Left medial and lateral pterygoid muscles
File:Gray382.png, Left temporalis muscle
File:Gray378 (masseter highlight).png, Left masseter muscle (red highlight)
They can be thought of in terms of the directions they move the mandible, with most being involved in more than one type of movement due to the variation in the orientation of muscle fibers within some of these muscles.
* Protrusion – Lateral and medial pterygoid.
* Retraction – Posterior fibers of temporalis (and the digastric and geniohyoid muscles to a lesser extent).
* Elevation – Anterior and middle fibers of temporalis, the superficial and deep fibers of masseter and the medial pterygoid.
* Lateral movements – Medial and lateral pterygoid (the ipsilateral temporalis and the pterygoid muscles of the contralateral side pull the mandible to the ipsilateral side).
Each lateral pterygoid muscle is composed of 2 heads, the upper or superior head and the lower or inferior head. The lower head
originates from the lateral surface of the
lateral pterygoid plate and
inserts at a depression on the neck of mandibular condyle, just below the articular surface, termed the
pterygoid fovea
The pterygoid fovea (occasionally called the pterygoid pit or the pterygoid depression) is located on the mandible. It is a concave surface on the medial side of the neck of the condyloid process of the mandible. It is located posterior to the m ...
. The upper head originates from the infratemporal surface and the infratemporal crest of the greater wing of the
sphenoid bone
The sphenoid bone is an unpaired bone of the neurocranium. It is situated in the middle of the skull towards the front, in front of the basilar part of occipital bone, basilar part of the occipital bone. The sphenoid bone is one of the seven bones ...
. The upper head also inserts at the fovea, but a part may be attached directly to the joint capsule and to the anterior and medial borders of the articular disc.
The 2 parts of lateral pterygoid have different actions. The lower head contracts during mouth opening, and the upper head contracts during mouth closing. The function of the lower head is to steady the articular disc as it moves back with the condyle into the articular fossa. It is relaxed during mouth closure.
Mechanisms of symptoms
Joint noises
Noises from the TMJs are a symptom of dysfunction of these joints. The sounds commonly produced by TMD are usually described as a "click" or a "pop" when a single sound is heard and as "crepitation" or "crepitus" when there are multiple, grating, rough sounds. Most joint sounds are due to internal derangement of the joint, which is instability or abnormal position of the articular disc.
Clicking often accompanies either jaw opening or closing, and usually occurs towards the end of the movement. The noise indicates that the articular disc has suddenly moved to and from a temporarily displaced position (disk displacement with reduction) to allow completion of a phase of movement of the mandible.
If the disc displaces and does not reduce (move back into position) this may be associated with locking. Clicking alone is not diagnostic of TMD since it is present in high proportion of the general population, mostly in people who have no pain.
Crepitus often indicates arthritic changes in the joint, and may occur at any time during mandibular movement, especially lateral movements.
Perforation of the disc may also cause crepitus.
Due to the proximity of the TMJ to the
ear canal
The ear canal (external acoustic meatus, external auditory meatus, EAM) is a pathway running from the outer ear to the middle ear. The adult human ear canal extends from the pinna to the eardrum and is about in length and in diameter.
Struc ...
, joint noises are perceived to be much louder to the individual than to others. Often people with TMD are surprised that what sounds to them like very loud noises cannot be heard at all by others next to them. However, it is occasionally possible for loud joint noises to be easily heard by others in some cases and this can be a source of embarrassment e.g. when eating in company.
Pain
Pain symptoms in TMD can be thought of as originating from the joint (arthralgia), or from the muscles (myofascial), or both. There is a poor correlation between TMD pain severity and evidence of tissue pathology.
Generally, degenerative joint changes are associated with greater pain.
=Myofascial pain
=
Pain originating from the muscles of mastication as a result of abnormal muscular function or hyperactivity. The muscular pain is frequently, but not always, associated with daytime clenching or nocturnal bruxism.
Limitation of mandibular movement
The jaw deviates to the affected side during opening,
and restricted mouth opening usually signifies that both TMJs are involved, but severe
trismus rarely occurs. If the greatest reduction in movement occurs upon waking then this may indicate that there is concomitant sleep bruxism. In other cases the limitation in movement gets worse throughout the day.
The jaw may lock entirely.
Limitation of mandibular movement itself may lead to further problems involving the TMJs and the muscles of mastication. Changes in the synovial membrane may lead to a reduction in lubrication of the joint and contribute to degenerative joint changes.
The muscles become weak, and
fibrosis may occur. All these factors may lead to a further limitation of jaw movement and increase in pain.
Degenerative joint disease, such as osteoarthritis or organic degeneration of the articular surfaces, recurrent fibrous or bony ankylosis, developmental abnormality, or pathologic lesions within the TMJ.
Myofascial pain syndrome
Myofascial pain syndrome (MPS), also known as chronic myofascial pain (CMP), is a syndrome characterized by chronic pain in multiple myofascial trigger points ("knots") and fascial (connective tissue) constrictions. It can appear in any body part ...
.
=Referred TMD pain
=
Sometimes TMD pain can radiate or be referred from its cause (i.e. the TMJ or the muscles of mastication) and be felt as headaches, earache or toothache.
Due to the proximity of the ear to the temporomandibular joint, TMJ pain can often be confused with ear pain.
The pain may be
referred in around half of all patients and experienced as
otalgia (earache).
Conversely, TMD is an important possible cause of
secondary otalgia. Treatment of TMD may then significantly reduce symptoms of otalgia and
tinnitus, as well as
atypical facial pain.
Despite some of these findings, some researchers question whether TMJD therapy can reduce symptoms in the ear, and there is currently an ongoing debate to settle the controversy.
Diagnosis
Pain is the most common reason for people with TMD to seek medical advice.
Joint noises may require
auscultation
Auscultation (based on the Latin verb ''auscultare'' "to listen") is listening to the internal sounds of the body, usually using a stethoscope. Auscultation is performed for the purposes of examining the circulatory and respiratory systems (hea ...
with a
stethoscope
The stethoscope is a medical device for auscultation, or listening to internal sounds of an animal or human body. It typically has a small disc-shaped resonator that is placed against the skin, and one or two tubes connected to two earpieces. ...
to detect.
Clicks of the joint may also be palpated, over the joint itself in the preauricular region, or via a finger inserted in the external acoustic meatus,
which lies directly behind the TMJ.
The
differential diagnosis
In healthcare, a differential diagnosis (abbreviated DDx) is a method of analysis of a patient's history and physical examination to arrive at the correct diagnosis. It involves distinguishing a particular disease or condition from others that p ...
is with degenerative joint disease (e.g. osteoarthritis),
rheumatoid arthritis,
temporal arteritis,
otitis media
Otitis media is a group of inflammatory diseases of the middle ear. One of the two main types is acute otitis media (AOM), an infection of rapid onset that usually presents with ear pain. In young children this may result in pulling at the ear, ...
,
parotitis, mandibular
osteomyelitis,
Eagle syndrome,
trigeminal neuralgia,
oromandibular dystonia, deafferentation pains, and
psychogenic pain.
Diagnostic criteria
Various diagnostic systems have been described. Some consider the Research Diagnostic Criteria method the gold standard.
Abbreviated to "RDC/TMD", this was first introduced in 1992 by Dworkin and LeResche in an attempt to classify temporomandibular disorders by etiology and apply universal standards for research into TMD.
This method involves 2 diagnostic axes, namely axis I, the physical diagnosis, and axis II, the psychologic diagnosis.
Axis I contains 3 different groups which can occur in combinations of 2 or all 3 groups,
(see table).
McNeill 1997 described TMD diagnostic criteria as follows:
* Pain in muscles of mastication, the TMJ, or the periauricular area (around the ear), which is usually made worse by manipulation or function.
* Asymmetric mandibular movement with or without clicking.
* Limitation of mandibular movements.
* Pain present for a minimum of 3 months.
The International Headache Society's diagnostic criteria for "headache or facial pain attributed to temporomandibular joint disorder" is similar to the above:
* A. Recurrent pain in one or more regions of the head or face fulfilling criteria C and D
* B. X-ray, MRI or bone scintigraphy demonstrate TMJ disorder
* C. Evidence that pain can be attributed to the TMJ disorder, based on at least one of the following:
** pain is precipitated by jaw movements or chewing of hard or tough food
** reduced range of or irregular jaw opening
** noise from one or both TMJs during jaw movements
** tenderness of the joint capsule(s) of one or both TMJs
* D. Headache resolves within 3 months, and does not recur, after successful treatment of the TMJ disorder
Medical imaging
The advantages brought about by diagnostic imaging mainly lie within diagnosing TMD of articular origin. Additional benefits of imaging the TMJ are as follows:
* Assess the integrity of anatomical structures in suspicion of disorders
* Staging the extent of any pathology
* Monitoring and staging the progress of disease
* Determining the effects of treatment
When clinical examination alone is unable to bring sufficient detail to ascertain the state of the TMJ, imaging methods can act as an adjuvant to clinical examination in the diagnosis of TMD.
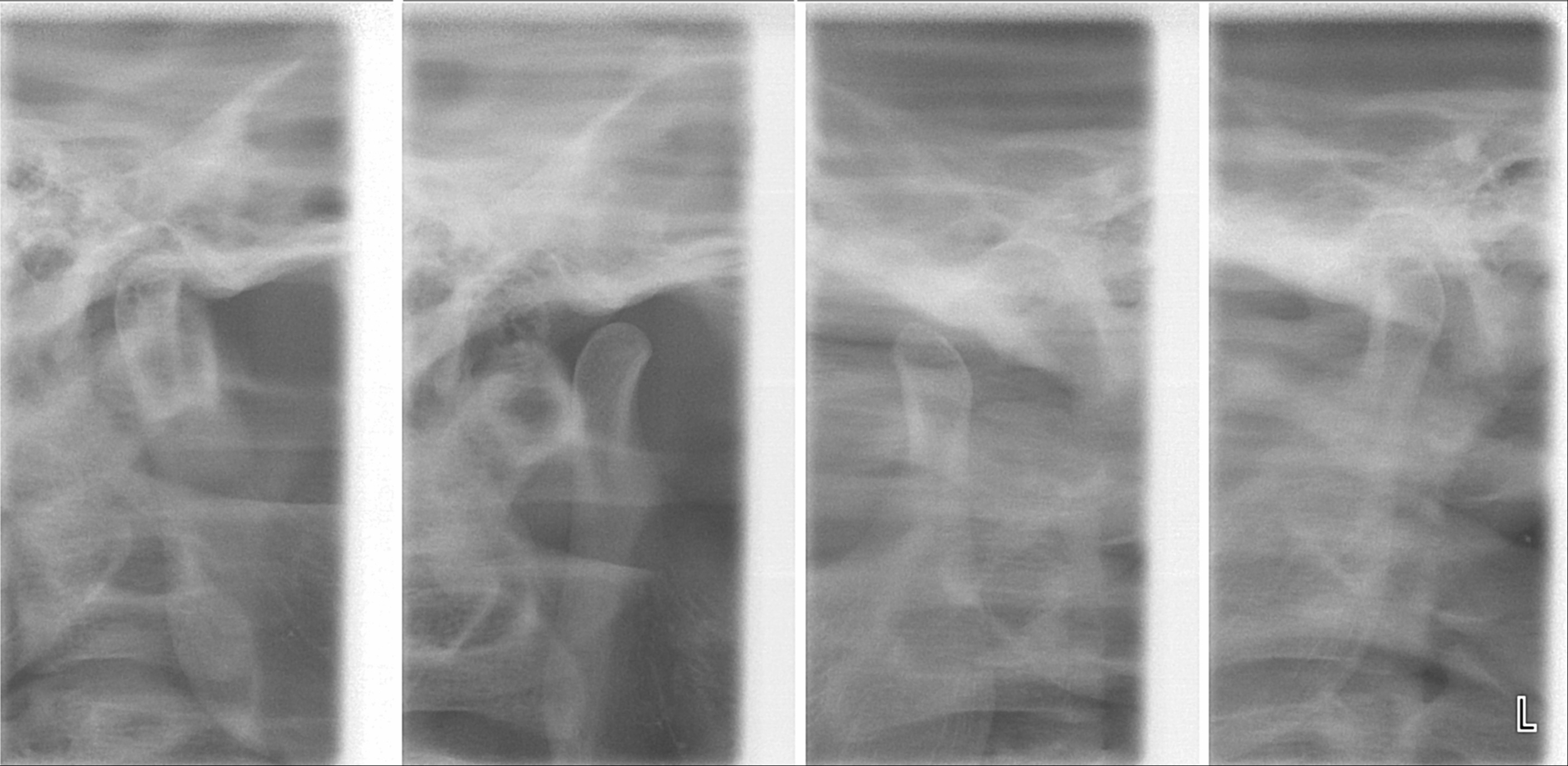
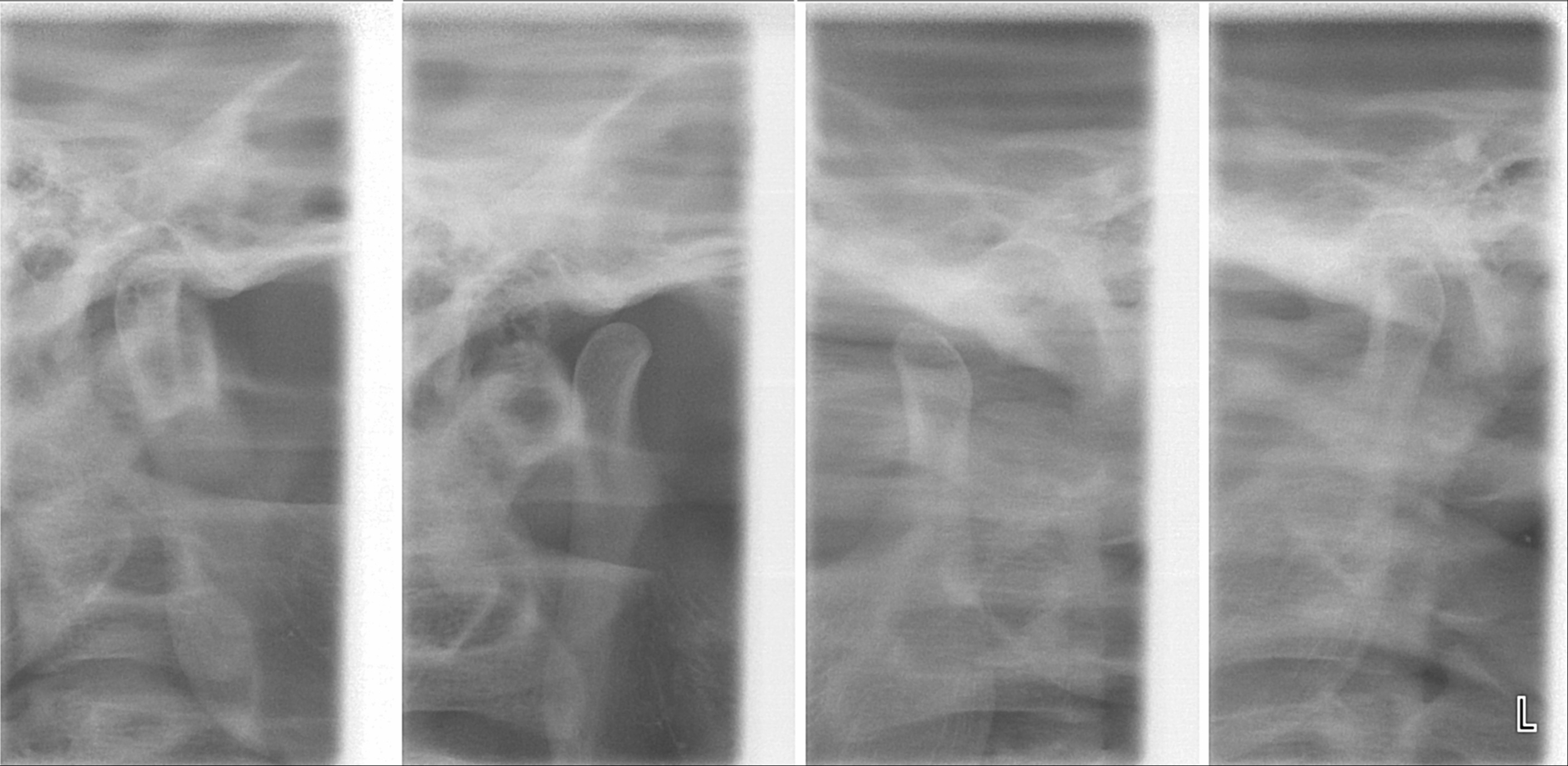
Plain radiography
This method of imaging allows the visualisation of the joint's mineralised areas, therefore excluding the cartilage and soft tissues.
A disadvantage of plain radiography is that images are prone to superimposition from surrounding anatomical structures, thereby complicating radiographic interpretation.
It was concluded that there is no evidence to support the use of plain radiography in the diagnosis of joint erosions and osteophytes.
It is reasonable to conclude that plain film can only be used to diagnose extensive lesions.
Panoramic tomography
The distortion brought about by panoramic imaging decreases its overall reliability. Data concluded from a systematic review showed that only extensive erosions and large osteophytes can be detected by panoramic imaging.
Computerised tomography (CT)
Studies have shown that tomography of the TMJ provided supplementary information that supersedes what is obtainable from clinical examination alone. However, the issues lies in the fact that it is impossible to determine whether certain patient groups would benefit more or less from a radiographic examination.
The main indications of
CT and CBCT examinations are to assess the bony components of the TMJ, specifically the location and extent of any abnormalities present.
The introduction of cone beam computed tomography (CBCT) imaging allowed a lower radiation dose to patients, in comparison to conventional CT. Hintze et al. compared CBCT and CT techniques and their ability to detect morphological TMJ changes. No significant difference was concluded in terms of their diagnostic accuracy.
Magnetic resonance imaging (MRI)
MRI is the optimal choice for the imaging of soft tissues surrounding the TMJ.
It allows three-dimensional evaluation of the axial, coronal and sagittal plane.
It is the gold standard method for assessing disc position and is sensitive for intra-articular degenerative alterations.
Indications for MRI are pre-auricular pain, detection of joint clicking and crepitus, frequent incidents of subluxation and jaw dislocation, limited mouth opening with terminal stiffness, suspicion of neoplastic growth, and osteoarthritic symptoms.
It is also useful for assessing the integrity of neural tissues, which may produce orofacial pain when compressed.
MRI provides evaluation of pathology such as necrosis and oedema all without any exposure to
ionizing radiation
Ionizing radiation (or ionising radiation), including nuclear radiation, consists of subatomic particles or electromagnetic waves that have sufficient energy to ionize atoms or molecules by detaching electrons from them. Some particles can travel ...
.
However, there is a high cost associated with this method of imaging, due to the need for sophisticated facilities.
Caution should be taken in patient selection, as MRI is contraindicated in those with claustrophobic tendencies,
pacemakers and metallic heart valves,
ferromagnetic
Ferromagnetism is a property of certain materials (such as iron) which results in a large observed magnetic permeability, and in many cases a large magnetic coercivity allowing the material to form a permanent magnet. Ferromagnetic materials ...
foreign bodies and pregnant women.
Ultrasound
Where internal TMJ disorders are concerned,
ultrasound (US) imaging can be a useful alternative in assessing the position of the disc
While having significant diagnostic
sensitivity, US has inadequate
specificity when identifying
osteoarthrosis
Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone which affects 1 in 7 adults in the United States. It is believed to be the fourth leading cause of disability in the w ...
. Moreover, it is not accurate enough for the diagnosis of cortical and
articular disc morphology based on the findings done related to morphological alterations.
However, with US, identification of
effusion
In physics and chemistry, effusion is the process in which a gas escapes from a container through a hole of diameter considerably smaller than the mean free path of the molecules. Such a hole is often described as a ''pinhole'' and the escape ...
in individuals with inflammatory conditions associated with pain is possible and confirmed by MRI
US can be a useful alternative in initial investigation of internal TMJ dysfunctions especially in MRI contraindicated individuals
despite its limitations.
in addition to being less costly,
US provides a quick and comfortable real-time imaging without exposing the individual to ionizing radiation
US is commonly assessed in the differential diagnosis of alterations of glandular and neighbouring structures, such as the TMJ and the
masseter muscle. Symptoms of sialendenitis and sialothiasis cases can be confused with
Eagle syndrome, TMD, myofascial and nerve pain, and other pain of the orofacial region.
US assessment is also indicated where there is need to identify the correct position of the joint spaces for infiltrative procedures,
arthrocentesis, and
viscosupplementation
Hyaluronic acid (; abbreviated HA; conjugate acid, conjugate base hyaluronate), also called hyaluronan, is an anion#Anions and cations, anionic, Sulfation, nonsulfated glycosaminoglycan distributed widely throughout connective tissue, connective, ...
. This is due to the fact that US provides a dynamic and real-time location of the component of the joints, while providing adequate lubrication and washing, which can be confirmed by the joint space increase post-treatment.
Management
TMD can be difficult to manage, and since the disorder transcends the boundaries between several health-care disciplines – in particular,
dentistry
Dentistry, also known as dental medicine and oral medicine, is the branch of medicine focused on the teeth, gums, and mouth. It consists of the study, diagnosis, prevention, management, and treatment of diseases, disorders, and conditions o ...
and
neurology, the treatment may often involve multiple approaches and be multidisciplinary.
Most who are involved in treating and researching TMD now agree that any treatment carried out should not permanently alter the jaw or teeth, and should be reversible.
To avoid permanent change,
over-the-counter or
prescription pain medications may be prescribed.
Psychosocial and behavioral interventions
Given the important role that psychosocial factors appear to play in TMD, psychosocial interventions could be viewed to be central to management of the condition.
There is a suggestion that treatment of factors that modulate pain sensitivity such as
mood disorders, anxiety and
fatigue
Fatigue describes a state of tiredness that does not resolve with rest or sleep. In general usage, fatigue is synonymous with extreme tiredness or exhaustion that normally follows prolonged physical or mental activity. When it does not resolve ...
, may be important in the treatment of TMD, which often tends to attempt to address the pain directly.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. CBT focuses on challenging and changing cognitive distortions (suc ...
(CBT) has been used in TMD and has been shown to be efficacious by meta analyses.
is suggested by some to be appropriate for TMD. Studies have suggested that it may even be more beneficial than occlusal splint therapy, and has comparable effects to relaxation techniques.
Relaxation techniques
A relaxation technique (also known as relaxation training) is any method, process, procedure, or activity that helps a person to relax; to attain a state of increased calmness; or otherwise reduce levels of pain, anxiety, stress or anger. Relax ...
include
progressive muscle relaxation
Progressive muscle relaxation (PMR) is a non-pharmacological method of deep muscle relaxation, based on the premise that muscle tension is the body's psychological response to anxiety-provoking thoughts and that muscle relaxation blocks anxiety. ...
,
yoga, and
meditation.
It has been suggested that TMD involves increased sensitivity to external stimuli leading to an increased
sympathetic ("fight or flight") response with cardiovascular and respiratory alterations.
Relaxation techniques cause reduced sympathetic activity, including muscle relaxation and reducing sensitivity to external stimuli, and provoke a general sense of well-being and reduced anxiety.
Devices


Occlusal splint
A mouthguard is a protective device for the mouth that covers the teeth and gums to prevent and reduce injury to the teeth, arches, lips and gums. An effective mouthguard is like a crash helmet for teeth and jaws. It also prevents the jaws com ...
s (also termed bite plates or intra-oral appliances) are often used by dentists to treat TMD. They are usually made of
acrylic
Acrylic may refer to:
Chemicals and materials
* Acrylic acid, the simplest acrylic compound
* Acrylate polymer, a group of polymers (plastics) noted for transparency and elasticity
* Acrylic resin, a group of related thermoplastic or thermosett ...
and can be hard or soft. They can be designed to fit onto the upper teeth or the lower teeth. They may cover all the teeth in one arch (full coverage splint) or only some (partial coverage splint). Splints are also termed according to their intended mechanism, such as the anterior positioning splint or the stabilization splint.
Although occlusal splints are generally considered a reversible treatment,
sometimes partial coverage splints lead to pathologic tooth migration (changes in the position of teeth). Normally splints are only worn during sleep, and therefore probably do nothing for people who engage in parafunctional activities during wakefulness rather than during sleep. There is slightly more evidence for the use of occlusal splints in sleep bruxism than in TMD. A splint can also have a diagnostic role if it demonstrates excessive occlusal wear after a period of wearing it each night. This may confirm the presence of sleep bruxism if it was in doubt. Soft splints are occasionally reported to worsen discomfort related to TMD.
Specific types of occlusal splint are discussed below.
A stabilization splint is a hard acrylic splint that forces the teeth to meet in an "ideal" relationship for the muscles of mastication and the TMJs. It is claimed that this technique reduces abnormal muscular activity and promotes "neuromuscular balance". A stabilization splint is only intended to be used for about 2–3 months.
It is more complicated to construct than other types of splint since a
face bow record is required and significantly more skill on the part of the
dental technician. This kind of splint should be properly fitted to avoid exacerbating the problem and used for brief periods of time. The use of the splint should be discontinued if it is painful or increases existing pain.
[ A systematic review of all the scientific studies investigating the efficacy of stabilization splints concluded the following:
Partial coverage splints are recommended by some experts, but they have the potential to cause unwanted tooth movements, which can occasionally be severe. The mechanism of this tooth movement is that the splint effectively holds some teeth out of contact and puts all the force of the bite onto the teeth which the splint covers. This can cause the covered teeth to be intruded, and those that are not covered to over-erupted. I.e. a partial coverage splint can act as a ]Dahl appliance
The Dahl effect or Dahl concept is used in dentistry where a localized appliance or localized restoration is used to increase the available interocclusal space for restorations.
Concept
A steep incisal guidance angle (the angle formed between ...
. Examples of partial coverage splints include the NTI-TSS ("nociceptive trigeminal inhibitor tension suppression system"), which covers the upper front teeth only. Due to the risks involved with long term use, some discourage the use of any type of partial coverage splint.
Medication
Medication is the main method of managing pain in TMD, mostly because there is little if any evidence of the effectiveness of surgical or dental interventions. Many drugs have been used to treat TMD pain, such as analgesic
An analgesic drug, also called simply an analgesic (American English), analgaesic (British English), pain reliever, or painkiller, is any member of the group of drugs used to achieve relief from pain (that is, analgesia or pain management). It ...
s (pain killers), benzodiazepine
Benzodiazepines (BZD, BDZ, BZs), sometimes called "benzos", are a class of depressant drugs whose core chemical structure is the fusion of a benzene ring and a diazepine ring. They are prescribed to treat conditions such as anxiety disorders, ...
s (e.g. clonazepam, prazepam, diazepam), anticonvulsant
Anticonvulsants (also known as antiepileptic drugs or recently as antiseizure drugs) are a diverse group of pharmacological agents used in the treatment of epileptic seizures. Anticonvulsants are also increasingly being used in the treatment of b ...
s (e.g. gabapentin), muscle relaxants (e.g. cyclobenzaprine
Cyclobenzaprine (sold under the brand name Flexeril, among others) is a medication used for muscle spasms from musculoskeletal conditions of sudden onset. It is not useful in cerebral palsy. It is taken by mouth. Use is not recommended for mor ...
), and others. Analgesics that have been studied in TMD include non-steroidal anti-inflammatory drugs (e.g. piroxicam, diclofenac, naproxen) and cyclo-oxygenase-2 inhibitor
COX-2 inhibitors are a type of nonsteroidal anti-inflammatory drug (NSAID) that directly targets cyclooxygenase-2, COX-2, an enzyme responsible for inflammation and pain. Targeting selectivity for COX-2 reduces the risk of peptic ulceration and i ...
s (e.g. celecoxib).
Topical methyl salicylate and topical capsaicin have also been used.
Other drugs that have been described for use in TMD include glucosamine hydrochloride
Glucosamine (C6H13NO5) is an amino sugar and a prominent precursor in the biochemical synthesis of glycosylated proteins and lipids. Glucosamine is part of the structure of two polysaccharides, chitosan and chitin. Glucosamine is one of the most ...
/chondroitin sulphate
Chondroitin sulfate is a sulfated glycosaminoglycan (GAG) composed of a chain of alternating sugars ( N-acetylgalactosamine and glucuronic acid). It is usually found attached to proteins as part of a proteoglycan. A chondroitin chain can have over ...
and propranolol. Low-doses of anti-muscarinic
A muscarinic receptor antagonist (MRA) is a type of anticholinergic agent that blocks the activity of the muscarinic acetylcholine receptor. The muscarinic receptor is a protein involved in the transmission of signals through certain parts of the ...
tricyclic antidepressant
Tricyclic antidepressants (TCAs) are a class of medications that are used primarily as antidepressants, which is important for the management of depression. They are second-line drugs next to SSRIs. TCAs were discovered in the early 1950s and we ...
s such as amitriptyline,nortriptyline
Nortriptyline, sold under the brand name Pamelor, among others, is a medication used to treat depression. This medicine is used for: neuropathic pain, attention deficit hyperactivity disorder (ADHD), smoking cessation and anxiety. As with many a ...
have also been described.systematic review
A systematic review is a Literature review, scholarly synthesis of the evidence on a clearly presented topic using critical methods to identify, define and assess research on the topic. A systematic review extracts and interprets data from publ ...
carried out in 2010 concluded that there was insufficient evidence to support or not to support the use of these drugs in TMD.opiate
An opiate, in classical pharmacology, is a substance derived from opium. In more modern usage, the term ''opioid'' is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain (including antagonis ...
analgesics has been suggested, although these drugs carry a risk of drug dependence
Substance dependence, also known as drug dependence, is a biopsychological situation whereby an individual's functionality is dependent on the necessitated re-consumption of a psychoactive substance because of an adaptive state that has develope ...
and other side effects.tramadol
Tramadol, sold under the brand name Ultram among others, is an opioid pain medication used to treat moderate to moderately severe pain. When taken by mouth in an immediate-release formulation, the onset of pain relief usually begins within an h ...
, hydrocodone, and methadone.steroid
A steroid is a biologically active organic compound with four rings arranged in a specific molecular configuration. Steroids have two principal biological functions: as important components of cell membranes that alter membrane fluidity; and a ...
s, into the muscles (e.g. the temoralis muscle or its tendon) are also sometimes used. Local anesthetics may provide temporary pain relief, and steroids inhibit pro-inflammatory cytokines.Botulinum toxin
Botulinum toxin, or botulinum neurotoxin (BoNT), is a neurotoxic protein produced by the bacterium ''Clostridium botulinum'' and related species. It prevents the release of the neurotransmitter acetylcholine from axon endings at the neuromusc ...
solution ("Botox") is sometimes used to treat TMD.acetylcholine
Acetylcholine (ACh) is an organic chemical that functions in the brain and body of many types of animals (including humans) as a neurotransmitter. Its name is derived from its chemical structure: it is an ester of acetic acid and choline. Part ...
release at the neuromuscular junction.muscles of facial expression
The facial muscles are a group of striated skeletal muscles supplied by the facial nerve (cranial nerve VII) that, among other things, control facial expression. These muscles are also called mimetic muscles. They are only found in mammals, alth ...
,
Physiotherapy
Physiotherapy
Physical therapy (PT), also known as physiotherapy, is one of the allied health professions. It is provided by physical therapists who promote, maintain, or restore health through physical examination, diagnosis, management, prognosis, patient ...
(physical therapy) is sometimes used as an adjuvant In pharmacology, an adjuvant is a drug or other substance, or a combination of substances, that is used to increase the efficacy or potency of certain drugs. Specifically, the term can refer to:
* Adjuvant therapy in cancer management
* Analgesic ...
to other methods of treatment in TMD.ischemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems wi ...
and subsequent hyperemia in the muscles, and this is hypothesized to inactivate trigger points and disrupt small fibrous adhesions within the muscle that have formed following surgery or muscular shortening due to restricted movement.low level laser therapy
Low-level laser therapy (LLLT), cold laser therapy, or photobiomodulation (PBM) is a form of medicine that applies low-level (low-power) lasers or light-emitting diodes (LEDs) to the surface of the body. Whereas high-power lasers are used in la ...
may help with pain.orofacial pain
Orofacial pain is a general term covering any pain which is felt in the mouth, jaws and the face. Orofacial pain is a common symptom, and there are many causes.
Orofacial Pain (OFP) is the specialty of dentistry that encompasses the diagnosis, ma ...
. MT has been used to restore normal range of motion, promoting circulation, stimulate proprioception, break fibrous adhesions, stimulate synovial fluid production and reduce pain. Exercises and MT are safe and simple interventions that could potentially be beneficial for patients with TMD. No adverse events regarding exercise therapy and manual therapy have been reported.biofeedback
Biofeedback is the process of gaining greater awareness of many physiology, physiological functions of one's own body by using Electronics, electronic or other instruments, and with a goal of being able to Manipulation (psychology), manipulate t ...
to reduce nighttime clenching experience a reduction in TMD.
Occlusal adjustment
This is the adjustment or reorganizing of the existing occlusion, carried out in the belief that this will redistribute forces evenly across the dental arches or achieve a more favorable position of the condyles in the fossae, which is purported to lessen tooth wear, bruxism and TMD, but this is controversial. These techniques are sometimes termed "occlusal rehabilitation" or "occlusal equilibration".
Surgery
Attempts in the last decade to develop surgical treatments based on MRI and CAT scans now receive less attention. These techniques are reserved for the most difficult cases where other therapeutic modalities
Physical therapy (PT), also known as physiotherapy, is one of the allied health professions. It is provided by physical therapists who promote, maintain, or restore health through physical examination, diagnosis, management, prognosis, patien ...
have failed. The American Society of Maxillofacial Surgeons The American Society of Maxillofacial Surgeons (ASMS) is a professional organization focused on the science and practice of surgery of the facial region and craniofacial skeleton. The organization is involved in education, research, and advocacy on ...
recommends a conservative/non-surgical approach first. Only 20% of patients need to proceed to surgery.
Examples of surgical procedures that are used in TMD, some more commonly than others, include arthrocentesis arthroscopy, meniscectomy, disc repositioning, condylotomy or joint replacement. Invasive surgical procedures in TMD may cause symptoms to worsen.
Alternative medicine
Acupuncture
Acupuncture is sometimes used for TMD.
Chiropractic
Chiropractic adjustment
Spinal adjustment and chiropractic adjustment are terms used by chiropractors to describe their approaches to spinal manipulation, as well as some osteopaths, who use the term adjustment. Despite anecdotal success, there is no scientific evidenc ...
s (also termed manipulations or mobilizations) are sometimes used in the belief that this will treat TMD.case report In medicine, a case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports may contain a demographic profile of the patient, but usually describe an unusual or novel occurrence ...
s and a case series of only 9 participants. One review concluded "inconclusive evidence in a favorable direction regarding mobilization and massage for TMD".
Prognosis
It has been suggested that the natural history of TMD is benign and self-limiting,
Epidemiology
TMD mostly affects people in the 20 – 40 age group,
History
Temporomandibular disorders were described as early as ancient Egypt.
References
{{Authority control
Musculoskeletal disorders
Articles containing video clips
Pathology of temporomandibular joints, muscles of mastication and associated structures
Ailments of unknown cause
 Pain is the most common reason for people with TMD to seek medical advice.
Joint noises may require
Pain is the most common reason for people with TMD to seek medical advice.
Joint noises may require 
