Schizophrenia on:
[Wikipedia]
[Google]
[Amazon]
Schizophrenia is a
 Schizophrenia is a
Schizophrenia is a
 An estimated 70% of those with schizophrenia have cognitive deficits, and these are most pronounced in early onset and late-onset illness. These are often evident long before the onset of illness in the prodromal stage, and may be present in early adolescence, or childhood. They are a core feature but not considered to be core symptoms, as are positive and negative symptoms. However, their presence and degree of dysfunction is taken as a better indicator of functionality than the presentation of core symptoms. Cognitive deficits become worse at first episode psychosis but then return to baseline, and remain fairly stable over the course of the illness.
The deficits in cognition are seen to drive the negative psychosocial outcome in schizophrenia, and are claimed to equate to a possible reduction in IQ from the norm of 100 to 70–85. Cognitive deficits may be of neurocognition (nonsocial) or of
An estimated 70% of those with schizophrenia have cognitive deficits, and these are most pronounced in early onset and late-onset illness. These are often evident long before the onset of illness in the prodromal stage, and may be present in early adolescence, or childhood. They are a core feature but not considered to be core symptoms, as are positive and negative symptoms. However, their presence and degree of dysfunction is taken as a better indicator of functionality than the presentation of core symptoms. Cognitive deficits become worse at first episode psychosis but then return to baseline, and remain fairly stable over the course of the illness.
The deficits in cognition are seen to drive the negative psychosocial outcome in schizophrenia, and are claimed to equate to a possible reduction in IQ from the norm of 100 to 70–85. Cognitive deficits may be of neurocognition (nonsocial) or of
 The first-line treatment for schizophrenia is an antipsychotic. The first-generation antipsychotics, now called
The first-line treatment for schizophrenia is an antipsychotic. The first-generation antipsychotics, now called
 Schizophrenia has great human and economic costs. It decreases life expectancy by between 20 and 28 years. This is primarily because of its association with heart disease, diabetes,
Schizophrenia has great human and economic costs. It decreases life expectancy by between 20 and 28 years. This is primarily because of its association with heart disease, diabetes,
 In 2017, the Global Burden of Disease Study estimated there were 1.1 million new cases; in 2022 the World Health Organization (WHO) reported a total of 24 million cases globally. Schizophrenia affects around 0.3–0.7% of people at some point in their life. In areas of conflict this figure can rise to between 4.0 and 6.5%. It occurs 1.4 times more frequently in males than females and typically appears earlier in men.
Worldwide, schizophrenia is the most common
In 2017, the Global Burden of Disease Study estimated there were 1.1 million new cases; in 2022 the World Health Organization (WHO) reported a total of 24 million cases globally. Schizophrenia affects around 0.3–0.7% of people at some point in their life. In areas of conflict this figure can rise to between 4.0 and 6.5%. It occurs 1.4 times more frequently in males than females and typically appears earlier in men.
Worldwide, schizophrenia is the most common
 Accounts of a schizophrenia-like
Accounts of a schizophrenia-like
 In the 1930s a number of shock procedures which induced seizures (convulsions) or comas were used to treat schizophrenia. Insulin shock involved injecting large doses of insulin to induce comas, which in turn produced hypoglycemia and convulsions. The use of electricity to induce seizures was in use as
In the 1930s a number of shock procedures which induced seizures (convulsions) or comas were used to treat schizophrenia. Insulin shock involved injecting large doses of insulin to induce comas, which in turn produced hypoglycemia and convulsions. The use of electricity to induce seizures was in use as
 In 2002, the term for schizophrenia in Japan was changed from to to reduce stigma. The new name, also interpreted as "integration disorder", was inspired by the biopsychosocial model. A similar change was made in South Korea in 2012 to attunement disorder.
In the United States, the annual cost of schizophrenia – including direct costs (outpatient, inpatient, drugs, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment) – was estimated at $62.7 billion for the year 2002. In the UK the cost in 2016 was put at £11.8 billion per year with a third of that figure directly attributable to the cost of hospital, social care and treatment.
In 2002, the term for schizophrenia in Japan was changed from to to reduce stigma. The new name, also interpreted as "integration disorder", was inspired by the biopsychosocial model. A similar change was made in South Korea in 2012 to attunement disorder.
In the United States, the annual cost of schizophrenia – including direct costs (outpatient, inpatient, drugs, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment) – was estimated at $62.7 billion for the year 2002. In the UK the cost in 2016 was put at £11.8 billion per year with a third of that figure directly attributable to the cost of hospital, social care and treatment.
mental disorder
A mental disorder, also referred to as a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. Such features may be persistent, relapsing and remitt ...
characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucination
A hallucination is a perception in the absence of an external stimulus that has the qualities of a real perception. Hallucinations are vivid, substantial, and are perceived to be located in external objective space. Hallucination is a combinati ...
s (typically hearing voices), delusions, and disorganized thinking. Other symptoms include social withdrawal, decreased emotional expression, and apathy. Symptoms typically develop gradually, begin during young adulthood, and in many cases never become resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a history that includes the person's reported experiences, and reports of others familiar with the person. To be diagnosed with schizophrenia, symptoms and functional impairment need to be present for six months ( DSM-5) or one month (ICD-11
The ICD-11 is the eleventh revision of the International Classification of Diseases (ICD). It replaces the ICD-10 as the global standard for recording health information and causes of death. The ICD is developed and annually updated by the World H ...
). Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders
A mood disorder, also known as an affective disorder, is any of a group of conditions of mental and behavioral disorder where a disturbance in the person's mood is the main underlying feature. The classification is in the ''Diagnostic and Stat ...
, anxiety disorders, and obsessive–compulsive disorder
Obsessive–compulsive disorder (OCD) is a mental and behavioral disorder in which an individual has intrusive thoughts and/or feels the need to perform certain routines repeatedly to the extent where it induces distress or impairs general ...
.
About 0.3% to 0.7% of people are diagnosed with schizophrenia during their lifetime. In 2017, there were an estimated 1.1 million new cases and in 2022 a total of 24 million cases globally. Males are more often affected and on average have an earlier onset. The causes of schizophrenia include genetic and environmental factors. Genetic factors include a variety of common and rare genetic variants. Possible environmental factors include being raised in a city, cannabis use during adolescence, infections, the ages of a person's mother or father, and poor nutrition during pregnancy.
About half of those diagnosed with schizophrenia will have a significant improvement over the long term with no further relapses, and a small proportion of these will recover completely. The other half will have a lifelong impairment. In severe cases people may be admitted to hospitals. Social problems such as long-term unemployment, poverty, homelessness, exploitation, and victimization are commonly correlated with schizophrenia. Compared to the general population, people with schizophrenia have a higher suicide rate (about 5% overall) and more physical health problems, leading to an average decrease in life expectancy by 20 to 28 years. In 2015, an estimated 17,000 deaths were linked to schizophrenia.
The mainstay of treatment is antipsychotic medication, along with counseling, job training, and social rehabilitation. Up to a third of people do not respond to initial antipsychotics, in which case clozapine
Clozapine is a psychiatric medication and is the first atypical antipsychotic (also called second-generation antipsychotic). It is primarily used to treat people with schizophrenia and schizoaffective disorders who have had an inadequate respo ...
may be used. In a network comparative meta-analysis of 15 antipsychotic drugs, clozapine was significantly more effective than all other drugs, although clozapine's heavily multimodal action may cause more side effects. In situations where doctors judge that there is a risk of harm to self or others, they may impose short involuntary hospitalization. Long-term hospitalization is used on a small number of people with severe schizophrenia. In some countries where supportive services are limited or unavailable, long-term hospital stays are more common.
Signs and symptoms
 Schizophrenia is a
Schizophrenia is a mental disorder
A mental disorder, also referred to as a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. Such features may be persistent, relapsing and remitt ...
characterized by significant alterations in perception, thoughts
In their most common sense, the terms thought and thinking refer to conscious cognitive processes that can happen independently of sensory stimulation. Their most paradigmatic forms are judging, reasoning, concept formation, problem solving, an ...
, mood, and behavior. Symptoms are described in terms of positive
Positive is a property of positivity and may refer to:
Mathematics and science
* Positive formula, a logical formula not containing negation
* Positive number, a number that is greater than 0
* Plus sign, the sign "+" used to indicate a posi ...
, negative, and cognitive symptoms. The positive symptoms of schizophrenia are the same for any psychosis and are sometimes referred to as psychotic symptoms. These may be present in any of the different psychoses, and are often transient making early diagnosis of schizophrenia problematic. Psychosis noted for the first time in a person who is later diagnosed with schizophrenia is referred to as a first-episode psychosis (FEP).
Positive symptoms
Positive symptoms are those symptoms that are not normally experienced, but are present in people during a psychotic episode in schizophrenia. They include delusions,hallucination
A hallucination is a perception in the absence of an external stimulus that has the qualities of a real perception. Hallucinations are vivid, substantial, and are perceived to be located in external objective space. Hallucination is a combinati ...
s, and disorganized thoughts and speech, typically regarded as manifestations of psychosis. Hallucinations occur at some point in the lifetimes of 80% of those with schizophrenia and most commonly involve the sense of hearing
Hearing, or auditory perception, is the ability to perceive sounds through an organ, such as an ear, by detecting vibrations as periodic changes in the pressure of a surrounding medium. The academic field concerned with hearing is audit ...
(most often hearing voices) but can sometimes involve any of the other senses of taste, sight, smell, and touch
In physiology, the somatosensory system is the network of neural structures in the brain and body that produce the perception of touch ( haptic perception), as well as temperature ( thermoception), body position (proprioception), and pain. It ...
. The frequency of hallucinations involving multiple senses is double the rate of those involving only one sense. They are also typically related to the content of the delusional theme. Delusions are bizarre or persecutory
Persecution is the systematic mistreatment of an individual or group by another individual or group. The most common forms are religious persecution, racism, and political persecution, though there is naturally some overlap between these terms ...
in nature. Distortions of self-experience such as feeling as if one's thoughts or feelings are not really one's own, to believing that thoughts are being inserted into one's mind, sometimes termed passivity phenomena, are also common. Thought disorders can include thought blocking, and disorganized speech. Positive symptoms generally respond well to medication, and become reduced over the course of the illness, perhaps related to the age-related decline in dopamine activity.
Negative symptoms
Negative symptoms are deficits of normal emotional responses, or of other thought processes. The five recognized domains of negative symptoms are: blunted affect – showing flat expressions or little emotion; alogia – a poverty of speech; anhedonia – an inability to feel pleasure; asociality – the lack of desire to form relationships, and avolition – a lack of motivation and apathy. Avolition and anhedonia are seen as motivational deficits resulting from impaired reward processing. Reward is the main driver of motivation and this is mostly mediated by dopamine. It has been suggested that negative symptoms are multidimensional and they have been categorised into two subdomains of apathy or lack of motivation, and diminished expression. Apathy includes avolition, anhedonia, and social withdrawal; diminished expression includes blunt affect, and alogia. Sometimes diminished expression is treated as both verbal and non-verbal. Apathy accounts for around 50 percent of the most often found negative symptoms and affects functional outcome and subsequent quality of life. Apathy is related to disrupted cognitive processing affecting memory and planning including goal-directed behaviour. The two subdomains have suggested a need for separate treatment approaches. A lack of distress – relating to a reduced experience of depression and anxiety is another noted negative symptom. A distinction is often made between those negative symptoms that are inherent to schizophrenia, termed primary; and those that result from positive symptoms, from the side effects of antipsychotics, substance use disorder, and social deprivation – termed secondary negative symptoms. Negative symptoms are less responsive to medication and the most difficult to treat. However, if properly assessed, secondary negative symptoms are amenable to treatment. Scales for specifically assessing the presence of negative symptoms, and for measuring their severity, and their changes have been introduced since the earlier scales such as the PANNS that deals with all types of symptoms. These scales are the ''Clinical Assessment Interview for Negative Symptoms'' (CAINS), and the ''Brief Negative Symptom Scale'' (BNSS) also known as second-generation scales. In 2020, ten years after its introduction, a cross-cultural study of the use of BNSS found valid and reliablepsychometric
Psychometrics is a field of study within psychology concerned with the theory and technique of measurement. Psychometrics generally refers to specialized fields within psychology and education devoted to testing, measurement, assessment, and ...
evidence for the five-domain structure cross-culturally. The BNSS is designed to assess both the presence and severity and change of negative symptoms of the five recognized domains, and the additional item of reduced normal distress. BNSS can register changes in negative symptoms concerning psychosocial and pharmacological intervention trials. BNSS has also been used to study a proposed non-D2 treatment called SEP-363856. Findings supported the favouring of five domains over the two-dimensional proposition.
Cognitive symptoms
 An estimated 70% of those with schizophrenia have cognitive deficits, and these are most pronounced in early onset and late-onset illness. These are often evident long before the onset of illness in the prodromal stage, and may be present in early adolescence, or childhood. They are a core feature but not considered to be core symptoms, as are positive and negative symptoms. However, their presence and degree of dysfunction is taken as a better indicator of functionality than the presentation of core symptoms. Cognitive deficits become worse at first episode psychosis but then return to baseline, and remain fairly stable over the course of the illness.
The deficits in cognition are seen to drive the negative psychosocial outcome in schizophrenia, and are claimed to equate to a possible reduction in IQ from the norm of 100 to 70–85. Cognitive deficits may be of neurocognition (nonsocial) or of
An estimated 70% of those with schizophrenia have cognitive deficits, and these are most pronounced in early onset and late-onset illness. These are often evident long before the onset of illness in the prodromal stage, and may be present in early adolescence, or childhood. They are a core feature but not considered to be core symptoms, as are positive and negative symptoms. However, their presence and degree of dysfunction is taken as a better indicator of functionality than the presentation of core symptoms. Cognitive deficits become worse at first episode psychosis but then return to baseline, and remain fairly stable over the course of the illness.
The deficits in cognition are seen to drive the negative psychosocial outcome in schizophrenia, and are claimed to equate to a possible reduction in IQ from the norm of 100 to 70–85. Cognitive deficits may be of neurocognition (nonsocial) or of social cognition
Social cognition is a sub-topic of various branches of psychology that focuses on how people process, store, and apply information about other people and social situations. It focuses on the role that cognitive processes play in social interacti ...
. Neurocognition is the ability to receive and remember information, and includes verbal fluency, memory, reason
Reason is the capacity of consciously applying logic by drawing conclusions from new or existing information, with the aim of seeking the truth. It is closely associated with such characteristically human activities as philosophy, science, ...
ing, problem solving, speed of processing, and auditory and visual perception. Verbal memory
Verbal memory is a term used in cognitive psychology which refers to memory of words and other abstractions involving language.
Verbal encoding
Verbal encoding refers to the interpretation of verbal stimuli. Verbal encoding appears to be strongly ...
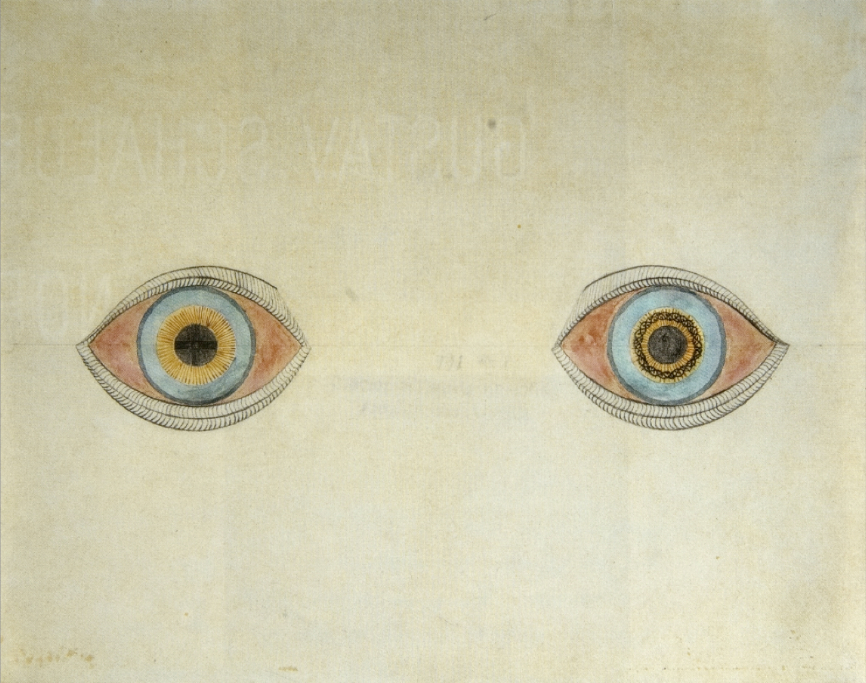
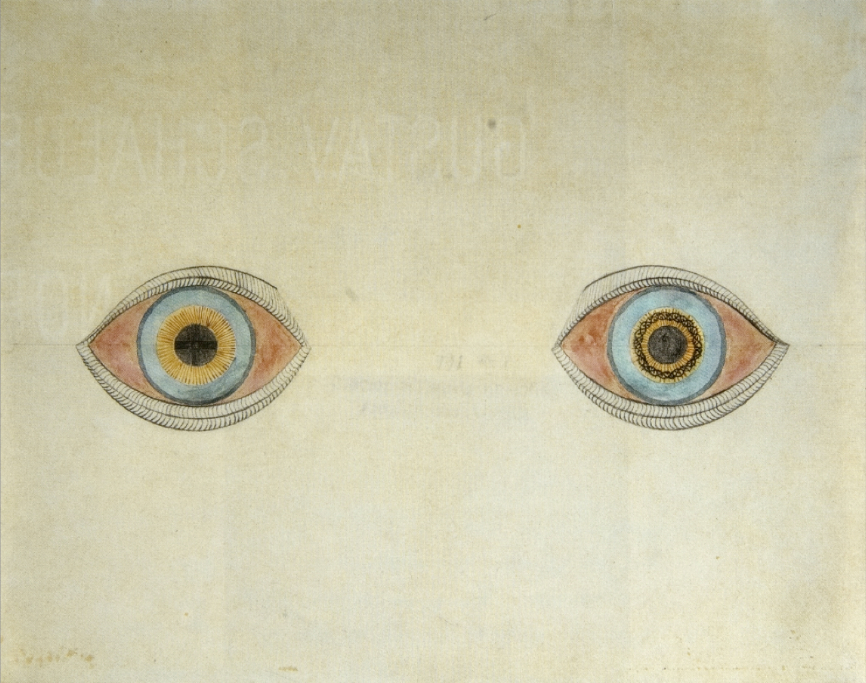
and attention are seen to be the most affected. Verbal memory impairment is associated with a decreased level of semantic processing (relating meaning to words). Another memory impairment is that of episodic memory. An impairment in visual perception that is consistently found in schizophrenia is that of visual backward masking. Visual processing
Visual processing is a term that is used to refer to the brain's ability to use and interpret visual information from the world around us. The process of converting light energy into a meaningful image is a complex process that is facilitated by ...
impairments include an inability to perceive complex visual illusion
Within visual perception, an optical illusion (also called a visual illusion) is an illusion caused by the visual system and characterized by a visual percept that arguably appears to differ from reality. Illusions come in a wide variety; the ...
s. Social cognition is concerned with the mental operations needed to interpret, and understand the self and others in the social world. This is also an associated impairment, and facial emotion perception is often found to be difficult. Facial perception is critical for ordinary social interaction. Cognitive impairments do not usually respond to antipsychotics, and there are a number of interventions that are used to try to improve them; cognitive remediation therapy is of particular help.
Neurological soft signs of clumsiness and loss of fine motor movement are often found in schizophrenia, which may resolve with effective treatment of FEP.
Onset
Onset typically occurs between the late teens and early 30s, with the peak incidence occurring in males in the early to mid twenties, and in females in the late twenties. Onset before the age of 17 is known as early-onset, and before the age of 13, as can sometimes occur, is known as childhood schizophrenia or very early-onset. Onset can occur between the ages of 40 and 60, known as late-onset schizophrenia. Onset over the age of 60, which may be difficult to differentiate as schizophrenia, is known as very-late-onset schizophrenia-like psychosis. Late onset has shown that a higher rate of females are affected; they have less severe symptoms and need lower doses of antipsychotics. The tendency for earlier onset in males is later seen to be balanced by a post-menopausal increase in the development in females. Estrogen produced pre-menopause has a dampening effect on dopamine receptors but its protection can be overridden by a genetic overload. There has been a dramatic increase in the numbers of older adults with schizophrenia. Onset may happen suddenly or may occur after the slow and gradual development of a number of signs and symptoms, a period known as the prodromal stage. Up to 75% of those with schizophrenia go through a prodromal stage. The negative and cognitive symptoms in the prodrome stage can precede FEP (first episode psychosis) by many months and up to five years. The period from FEP and treatment is known as the duration of untreated psychosis (DUP) which is seen to be a factor in functional outcome. The prodromal stage is the high-risk stage for the development of psychosis. Since the progression to first episode psychosis is not inevitable, an alternative term is often preferred of at risk mental state. Cognitive dysfunction at an early age impacts a young person's usual cognitive development. Recognition and early intervention at the prodromal stage would minimize the associated disruption to educational and social development and has been the focus of many studies.Risk factors
Schizophrenia is described as a neurodevelopmental disorder with no precise boundary, or single cause, and is thought to develop fromgene–environment interaction
Gene–environment interaction (or genotype–environment interaction or G×E) is when two different genotypes respond to environmental variation in different ways. A norm of reaction is a graph that shows the relationship between genes and envi ...
s with involved vulnerability factors. The interactions of these risk factor
In epidemiology, a risk factor or determinant is a variable associated with an increased risk of disease or infection.
Due to a lack of harmonization across disciplines, determinant, in its more widely accepted scientific meaning, is often ...
s are complex, as numerous and diverse insults
An insult is an expression or statement (or sometimes behavior) which is disrespectful or scornful. Insults may be intentional or accidental. An insult may be factual, but at the same time pejorative, such as the word " inbred".
Jocular exc ...
from conception to adulthood can be involved. A genetic predisposition on its own, without interacting environmental factors, will not give rise to the development of schizophrenia. The genetic component means that prenatal brain development is disturbed, and environmental influence affects the postnatal development of the brain. Evidence suggests that genetically susceptible children are more likely to be vulnerable to the effects of environmental risk factors.
Genetic
Estimates of the heritability of schizophrenia are between 70% and 80%, which implies that 70% to 80% of the individual differences in risk to schizophrenia is associated with genetics. These estimates vary because of the difficulty in separating genetic and environmental influences, and their accuracy has been queried. The greatest risk factor for developing schizophrenia is having afirst-degree relative
A first-degree relative (FDR) is a person's parent (father or mother), full sibling (brother or sister) or child. It constitutes a category of family members that largely overlaps with the term nuclear family, but without spouses.
If the persons ...
with the disease (risk is 6.5%); more than 40% of identical twins
Twins are two offspring produced by the same pregnancy.MedicineNet > Definition of TwinLast Editorial Review: 19 June 2000 Twins can be either ''monozygotic'' ('identical'), meaning that they develop from one zygote, which splits and forms two em ...
of those with schizophrenia are also affected. If one parent is affected the risk is about 13% and if both are affected the risk is nearly 50%. However, the ''DSM-5'' indicates that most people with schizophrenia have no family history of psychosis. Results of candidate gene
The candidate gene approach to conducting genetic association studies focuses on associations between genetic variation within pre-specified genes of interest, and phenotypes or disease states. This is in contrast to genome-wide association studies ...
studies of schizophrenia have generally failed to find consistent associations, and the genetic loci identified by genome-wide association studies
In genomics, a genome-wide association study (GWA study, or GWAS), also known as whole genome association study (WGA study, or WGAS), is an observational study of a genome-wide set of genetic variants in different individuals to see if any varian ...
explain only a small fraction of the variation in the disease.
Many genes are known to be involved in schizophrenia, each with small effect and unknown transmission and expression
Expression may refer to:
Linguistics
* Expression (linguistics), a word, phrase, or sentence
* Fixed expression, a form of words with a specific meaning
* Idiom, a type of fixed expression
* Metaphorical expression, a particular word, phrase, o ...
. The summation of these effect sizes into a polygenic risk score can explain at least 7% of the variability in liability for schizophrenia. Around 5% of cases of schizophrenia are understood to be at least partially attributable to rare copy number variation
Copy number variation (CNV) is a phenomenon in which sections of the genome are repeated and the number of repeats in the genome varies between individuals. Copy number variation is a type of structural variation: specifically, it is a type of ...
s (CNVs); these structural variation Genomic structural variation is the variation in structure of an organism's chromosome. It consists of many kinds of variation in the genome of one species, and usually includes microscopic and submicroscopic types, such as deletions, duplications, ...
s are associated with known genomic disorders involving deletions at 22q11.2 (DiGeorge syndrome
DiGeorge syndrome, also known as 22q11.2 deletion syndrome, is a syndrome caused by a microdeletion on the long arm of chromosome 22. While the symptoms can vary, they often include congenital heart problems, specific facial features, frequent i ...
) and 17q12 ( 17q12 microdeletion syndrome), duplications at 16p11.2 (most frequently found) and deletions at 15q11.2 ( Burnside–Butler syndrome). Some of these CNVs increase the risk of developing schizophrenia by as much as 20-fold, and are frequently comorbid with autism and intellectual disabilities.
The genes CRHR1
Corticotropin-releasing hormone receptor 1 (CRHR1) is a protein, also known as CRF1, with the latter (CRF1) now being the IUPHAR-recommended name. In humans, CRF1 is encoded by the ''CRHR1'' gene at region 17q21.31, beside micrototubule-associate ...
and CRHBP
Corticotropin-releasing factor-binding protein is a protein that in humans is encoded by the ''CRHBP'' gene
In biology, the word gene (from , ; "...Wilhelm Johannsen coined the word gene to describe the Mendelian units of heredity..." mea ...
are associated with the severity of suicidal behavior. These genes code for stress response proteins needed in the control of the HPA axis HPA may refer to:
Organizations
* Harry Potter Alliance, a charity
* Halifax Port Authority, Canada
* Hamburg Port Authority, Germany
* Hawaii Preparatory Academy, a school in Hawaii, US
* Health Protection Agency, UK
* Heerespersonalamt, the Ger ...
, and their interaction can affect this axis. Response to stress can cause lasting changes in the function of the HPA axis possibly disrupting the negative feedback mechanism, homeostasis
In biology, homeostasis (British also homoeostasis) (/hɒmɪə(ʊ)ˈsteɪsɪs/) is the state of steady internal, physical, and chemical conditions maintained by living systems. This is the condition of optimal functioning for the organism and ...
, and the regulation of emotion leading to altered behaviors.
The question of how schizophrenia could be primarily genetically influenced, given that people with schizophrenia have lower fertility rates, is a paradox. It is expected that genetic variants that increase the risk of schizophrenia would be selected against due to their negative effects on reproductive fitness. A number of potential explanations have been proposed, including that allele
An allele (, ; ; modern formation from Greek ἄλλος ''állos'', "other") is a variation of the same sequence of nucleotides at the same place on a long DNA molecule, as described in leading textbooks on genetics and evolution.
::"The chro ...
s associated with schizophrenia risk confers a fitness advantage in unaffected individuals. While some evidence has not supported this idea, others propose that a large number of alleles each contributing a small amount can persist.
A meta-analysis found that oxidative DNA damage was significantly increased in schizophrenia.
Environmental
Environmental factors, each associated with a slight risk of developing schizophrenia in later life includeoxygen deprivation
Asphyxia or asphyxiation is a condition of deficient supply of oxygen to the body which arises from abnormal breathing. Asphyxia causes generalized hypoxia, which affects primarily the tissues and organs. There are many circumstances that can ...
, infection, prenatal maternal stress, and malnutrition in the mother during prenatal development. A risk is associated with maternal obesity, in increasing oxidative stress
Oxidative stress reflects an imbalance between the systemic manifestation of reactive oxygen species and a biological system's ability to readily detoxify the reactive intermediates or to repair the resulting damage. Disturbances in the normal ...
, and dysregulating the dopamine and serotonin pathways. Both maternal stress and infection have been demonstrated to alter fetal neurodevelopment through an increase of pro-inflammatory cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrin ...
s. There is a slighter risk associated with being born in the winter or spring possibly due to vitamin D deficiency
Vitamin D deficiency or hypovitaminosis D is a vitamin D level that is below normal. It most commonly occurs in people when they have inadequate exposure to sunlight, particularly sunlight with adequate ultraviolet B rays (UVB). Vitamin D defic ...
or a prenatal viral infection
A viral disease (or viral infection) occurs when an organism's body is invaded by pathogenic viruses, and infectious virus particles (virions) attach to and enter susceptible cells.
Structural Characteristics
Basic structural characteristics, ...
. Other infections during pregnancy or around the time of birth that have been linked to an increased risk include infections by '' Toxoplasma gondii'' and ''Chlamydia
Chlamydia, or more specifically a chlamydia infection, is a sexually transmitted infection caused by the bacterium '' Chlamydia trachomatis''. Most people who are infected have no symptoms. When symptoms do appear they may occur only several we ...
''. The increased risk is about five to eight percent. Viral infections of the brain during childhood are also linked to a risk of schizophrenia during adulthood.
Adverse childhood experiences Adverse childhood experiences (ACEs) encompass various forms of physical and emotional abuse, neglect, and household dysfunction experienced in childhood. The harms of ACEs can be long-lasting, affecting people even in their adulthood. ACEs have be ...
(ACEs), severe forms of which are classed as childhood trauma, range from being bullied or abused, to the death of a parent. Many adverse childhood experiences can cause toxic stress and increase the risk of psychosis. Chronic trauma, including ACEs, can promote lasting inflammatory dysregulation throughout the nervous system. It is suggested that early stress may contribute to the development of schizophrenia through these alterations in the immune system. Schizophrenia was the last diagnosis to benefit from the link made between ACEs and adult mental health outcomes.
Living in an urban environment
An urban area, built-up area or urban agglomeration is a human settlement with a high population density and infrastructure of built environment. Urban areas are created through urbanization and are categorized by urban morphology as cities, ...
during childhood or as an adult has consistently been found to increase the risk of schizophrenia by a factor of two, even after taking into account drug use, ethnic group, and size of social group
In the social sciences, a social group can be defined as two or more people who interact with one another, share similar characteristics, and collectively have a sense of unity. Regardless, social groups come in a myriad of sizes and varieties ...
. A possible link between the urban environment and pollution has been suggested to be the cause of the elevated risk of schizophrenia. Other risk factors include social isolation
Social isolation is a state of complete or near-complete lack of contact between an individual and society. It differs from loneliness, which reflects temporary and involuntary lack of contact with other humans in the world. Social isolation ...
, immigration related to social adversity and racial discrimination, family dysfunction, unemployment, and poor housing conditions. Having a father older than 40 years, or parents younger than 20 years are also associated with schizophrenia.
Substance use
About half of those with schizophrenia userecreational drugs
Recreation is an activity of leisure, leisure being discretionary time. The "need to do something for recreation" is an essential element of human biology and psychology. Recreational activities are often done for enjoyment, amusement, or pleasur ...
, including cannabis, tobacco, and alcohol excessively. Use of stimulants such as amphetamine and cocaine can lead to a temporary stimulant psychosis, which presents very similarly to schizophrenia. Rarely, alcohol use can also result in a similar alcohol-related psychosis. Drugs may also be used as coping mechanisms by people who have schizophrenia, to deal with depression, anxiety, boredom, and loneliness
Loneliness is an unpleasant emotional response to perceived isolation. Loneliness is also described as social paina psychological mechanism which motivates individuals to seek social connections. It is often associated with a perceived lack ...
. The use of cannabis and tobacco are not associated with the development of cognitive deficits, and sometimes a reverse relationship is found where their use improves these symptoms. However, substance use disorders are associated with an increased risk of suicide, and a poor response to treatment.
Cannabis use may be a contributory factor in the development of schizophrenia, potentially increasing the risk of the disease in those who are already at risk. The increased risk may require the presence of certain genes within an individual. Its use is associated with doubling the rate.
Mechanism
The mechanisms of schizophrenia are unknown, and a number of models have been put forward to explain the link between altered brain function and schizophrenia.The prevailing model of schizophrenia is that of a neurodevelopmental disorder, and the underlying changes that occur before symptoms become evident are seen as arising from the interaction between genes and the environment. Extensive studies support this model. Maternal infections, malnutrition and complications during pregnancy andchildbirth
Childbirth, also known as labour and delivery, is the ending of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million births glob ...
are known risk factors for the development of schizophrenia, which usually emerges between the ages of 18–25, a period that overlaps with certain stages of neurodevelopment. Gene-environment interactions lead to deficits in the neural circuitry that affect sensory and cognitive functions.
The common dopamine and glutamate models proposed are not mutually exclusive; each is seen to have a role in the neurobiology of schizophrenia. The most common model put forward was the dopamine hypothesis of schizophrenia, which attributes psychosis to the mind's faulty interpretation of the misfiring of dopaminergic neurons. This has been directly related to the symptoms of delusions and hallucinations. Abnormal dopamine signaling has been implicated in schizophrenia based on the usefulness of medications that affect the dopamine receptor and the observation that dopamine levels are increased during acute psychosis. A decrease in D1 receptors in the dorsolateral prefrontal cortex may also be responsible for deficits in working memory.
The glutamate hypothesis of schizophrenia links alterations between glutamatergic neurotransmission and the neural oscillation
Neural oscillations, or brainwaves, are rhythmic or repetitive patterns of neural activity in the central nervous system. Neural tissue can generate oscillatory activity in many ways, driven either by mechanisms within individual neurons or by ...
s that affect connections between the thalamus and the cortex. Studies have shown that a reduced expression of a glutamate receptor – NMDA receptor, and glutamate blocking drugs such as phencyclidine
Phencyclidine or phenylcyclohexyl piperidine (PCP), also known as angel dust among other names, is a dissociative anesthetic mainly used recreationally for its significant mind-altering effects. PCP may cause hallucinations, distorted percept ...
and ketamine can mimic the symptoms and cognitive problems associated with schizophrenia. Post-mortem studies consistently find that a subset of these neurons fail to express GAD67 ( GAD1), in addition to abnormalities in brain morphometry. The subsets of interneurons that are abnormal in schizophrenia are responsible for the synchronizing of neural ensembles needed during working memory tasks. These give the neural oscillations produced as gamma waves that have a frequency of between 30 and 80 hertz
The hertz (symbol: Hz) is the unit of frequency in the International System of Units (SI), equivalent to one event (or cycle) per second. The hertz is an SI derived unit whose expression in terms of SI base units is s−1, meaning that o ...
. Both working memory tasks and gamma waves are impaired in schizophrenia, which may reflect abnormal interneuron functionality. An important process that may be disrupted in neurodevelopment is astrogenesis – the formation of astrocyte
Astrocytes (from Ancient Greek , , "star" + , , "cavity", "cell"), also known collectively as astroglia, are characteristic star-shaped glial cells in the brain and spinal cord. They perform many functions, including biochemical control of e ...
s. Astrocytes are crucial in contributing to the formation and maintenance of neural circuits and it is believed that disruption in this role can result in a number of neurodevelopmental disorders including schizophrenia. Evidence suggests that reduced numbers of astrocytes in deeper cortical layers are assocociated with a diminished expression of EAAT2
Excitatory amino acid transporter 2 (EAAT2) also known as solute carrier family 1 member 2 (SLC1A2) and glutamate transporter 1 (GLT-1) is a protein that in humans is encoded by the ''SLC1A2'' gene. Alternatively spliced transcript variants of thi ...
, a glutamate transporter
Glutamate transporters are a family of neurotransmitter transporter proteins that move glutamate – the principal excitatory neurotransmitter – across a membrane. The family of glutamate transporters is composed of two primary subclasses: the ex ...
in astrocytes; supporting the glutamate hypothesis.
Deficits in executive functions, such as planning, inhibition, and working memory, are pervasive in schizophrenia. Although these functions are separable, their dysfunction in schizophrenia may reflect an underlying deficit in the ability to represent goal related information in working memory, and to utilize this to direct cognition and behavior. These impairments have been linked to a number of neuroimaging and neuropathological abnormalities. For example, functional neuroimaging studies report evidence of reduced neural processing efficiency, whereby the dorsolateral prefrontal cortex is activated to a greater degree to achieve a certain level of performance relative to controls on working memory tasks. These abnormalities may be linked to the consistent post-mortem finding of reduced neuropil
Neuropil (or "neuropile") is any area in the nervous system composed of mostly unmyelinated axons, dendrites and glial cell processes that forms a synaptically dense region containing a relatively low number of cell bodies. The most prevalent an ...
, evidenced by increased pyramidal cell density and reduced dendritic spine density. These cellular and functional abnormalities may also be reflected in structural neuroimaging studies that find reduced grey matter volume in association with deficits in working memory tasks.
Positive symptoms have been linked to cortical thinning in the superior temporal gyrus. Severity of negative symptoms has been linked to reduced thickness in the left medial orbitofrontal cortex
The orbitofrontal cortex (OFC) is a prefrontal cortex region in the frontal lobes of the brain which is involved in the cognitive process of decision-making. In non-human primates it consists of the association cortex areas Brodmann area 11, 1 ...
. Anhedonia, traditionally defined as a reduced capacity to experience pleasure, is frequently reported in schizophrenia. However, a large body of evidence suggests that hedonic responses are intact in schizophrenia, and that what is reported to be anhedonia is a reflection of dysfunction in other processes related to reward. Overall, a failure of reward prediction is thought to lead to impairment in the generation of cognition and behavior required to obtain rewards, despite normal hedonic responses.
Another theory links abnormal brain lateralization to the development of being left-handed which is significantly more common in those with schizophrenia. This abnormal development of hemispheric asymmetry is noted in schizophrenia. Studies have concluded that the link is a true and verifiable effect that may reflect a genetic link between lateralization and schizophrenia.
Bayesian models of brain functioning have been utilized to link abnormalities in cellular functioning to symptoms. Both hallucinations and delusions have been suggested to reflect improper encoding of prior expectations, thereby causing expectation to excessively influence sensory perception and the formation of beliefs. In approved models of circuits that mediate predictive coding
In neuroscience, predictive coding (also known as predictive processing) is a theory of brain function which postulates that the brain is constantly generating and updating a "mental model" of the environment. According to the theory, such a ment ...
, reduced NMDA receptor activation, could in theory result in the positive symptoms of delusions and hallucinations.
Diagnosis
Criteria
Schizophrenia is diagnosed based on criteria in either the '' Diagnostic and Statistical Manual of Mental Disorders'' (DSM) published by the American Psychiatric Association or the International Statistical Classification of Diseases and Related Health Problems (ICD) published by the World Health Organization (WHO). These criteria use the self-reported experiences of the person and reported abnormalities in behavior, followed by apsychiatric assessment
A psychiatric assessment, or psychological screening, is the process of gathering information about a person within a psychiatric service, with the purpose of making a diagnosis. The assessment is usually the first stage of a treatment process, but ...
. The mental status examination is an important part of the assessment. An established tool for assessing the severity of positive and negative symptoms is the Positive and Negative Syndrome Scale (PANSS). This has been seen to have shortcomings relating to negative symptoms, and other scales – the ''Clinical Assessment Interview for Negative Symptoms'' (CAINS), and the ''Brief Negative Symptoms Scale'' (BNSS) have been introduced. The DSM-5, published in 2013, gives a ''Scale to Assess the Severity of Symptom Dimensions'' outlining eight dimensions of symptoms.
DSM-5 states that to be diagnosed with schizophrenia, two diagnostic criteria have to be met over the period of one month, with a significant impact on social or occupational functioning for at least six months. One of the symptoms needs to be either delusions, hallucinations, or disorganized speech. A second symptom could be one of the negative symptoms, or severely disorganized or catatonic behaviour. A different diagnosis of schizophreniform disorder
Schizophreniform disorder is a mental disorder diagnosed when symptoms of schizophrenia are present for a significant portion of time (at least a month), but signs of disturbance are not present for the full six months required for the diagnosis ...
can be made before the six months needed for the diagnosis of schizophrenia.
In Australia the guideline for diagnosis is for six months or more with symptoms severe enough to affect ordinary functioning. In the UK diagnosis is based on having the symptoms for most of the time for one month, with symptoms that significantly affect the ability to work, study, or to carry on ordinary daily living, and with other similar conditions ruled out.
The ICD criteria are typically used in European countries; the DSM criteria are used predominantly in the United States and Canada, and are prevailing in research studies. In practice, agreement between the two systems is high. The current proposal for the ICD-11
The ICD-11 is the eleventh revision of the International Classification of Diseases (ICD). It replaces the ICD-10 as the global standard for recording health information and causes of death. The ICD is developed and annually updated by the World H ...
criteria for schizophrenia recommends adding self-disorder as a symptom.
A major unresolved difference between the two diagnostic systems is that of the requirement in DSM of an impaired functional outcome. WHO for ICD argues that not all people with schizophrenia have functional deficits and so these are not specific for the diagnosis.
Comorbidities
Many people with schizophrenia may have one or more other mental disorders, such aspanic disorder
Panic disorder is a mental and behavioral disorder, specifically an anxiety disorder characterized by reoccurring unexpected panic attacks. Panic attacks are sudden periods of intense fear that may include palpitations, sweating, shaking, short ...
, obsessive–compulsive disorder
Obsessive–compulsive disorder (OCD) is a mental and behavioral disorder in which an individual has intrusive thoughts and/or feels the need to perform certain routines repeatedly to the extent where it induces distress or impairs general ...
, or substance use disorder. These are separate disorders that require treatment. When comorbid with schizophrenia, substance use disorder and antisocial personality disorder both increase the risk for violence. Comorbid substance use disorder also increases risk for suicide.
Sleep disorder
A sleep disorder, or somnipathy, is a medical disorder of an individual's sleep patterns. Some sleep disorders are severe enough to interfere with normal physical, mental, social and emotional functioning. Polysomnography and actigraphy are tests ...
s often co-occur with schizophrenia, and may be an early sign of relapse. Sleep disorders are linked with positive symptoms such as disorganized thinking and can adversely affect cortical plasticity and cognition. The consolidation of memories is disrupted in sleep disorders. They are associated with severity of illness, a poor prognosis, and poor quality of life. Sleep onset and maintenance insomnia is a common symptom, regardless of whether treatment has been received or not. Genetic variations have been found associated with these conditions involving the circadian rhythm, dopamine and histamine metabolism, and signal transduction.
Differential diagnosis
To make a diagnosis of schizophrenia other possible causes of psychosis need to be excluded. Psychotic symptoms lasting less than a month may be diagnosed as brief psychotic disorder, or asschizophreniform disorder
Schizophreniform disorder is a mental disorder diagnosed when symptoms of schizophrenia are present for a significant portion of time (at least a month), but signs of disturbance are not present for the full six months required for the diagnosis ...
. Psychosis is noted in ''Other specified schizophrenia spectrum and other psychotic disorders'' as a DSM-5 category. Schizoaffective disorder
Schizoaffective disorder (SZA, SZD or SAD) is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis is made when the person has symptoms of both schizophrenia (usually psychosis) and a mood disorder: ...
is diagnosed if symptoms of mood disorder are substantially present alongside psychotic symptoms. Psychosis that results from a general medical condition or substance is termed secondary psychosis.
Psychotic symptoms may be present in several other conditions, including bipolar disorder, borderline personality disorder, substance intoxication, substance-induced psychosis
Substance-induced psychosis (commonly known as toxic psychosis or drug-induced psychosis) is a form of psychosis that is attributed to substance use. It is a psychosis that results from the effects of chemicals or drugs, including those produced b ...
, and a number of drug withdrawal syndromes. Non-bizarre delusions are also present in delusional disorder
Delusional disorder is a mental illness in which a person has delusions, but with no accompanying prominent hallucinations, thought disorder, mood disorder, or significant flattening of affect.American Psychiatric Association. (2013). ''Diagnostic ...
, and social withdrawal in social anxiety disorder
Social anxiety disorder (SAD), also known as social phobia, is an anxiety disorder characterized by sentiments of fear and anxiety in social situations, causing considerable distress and impaired ability to function in at least some aspects o ...
, avoidant personality disorder and schizotypal personality disorder. Schizotypal personality disorder has symptoms that are similar but less severe than those of schizophrenia. Schizophrenia occurs along with obsessive–compulsive disorder
Obsessive–compulsive disorder (OCD) is a mental and behavioral disorder in which an individual has intrusive thoughts and/or feels the need to perform certain routines repeatedly to the extent where it induces distress or impairs general ...
(OCD) considerably more often than could be explained by chance, although it can be difficult to distinguish obsessions that occur in OCD from the delusions of schizophrenia. There can be considerable overlap with the symptoms of post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that can develop because of exposure to a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats o ...
.
A more general medical and neurological examination may be needed to rule out medical illnesses which may rarely produce psychotic schizophrenia-like symptoms, such as metabolic disturbance, systemic infection
A systemic disease is one that affects a number of organs and tissues, or affects the body as a whole.
Examples
* Mastocytosis, including mast cell activation syndrome and eosinophilic esophagitis
* Chronic fatigue syndrome
* Systemic vascul ...
, syphilis, HIV-associated neurocognitive disorder, epilepsy, limbic encephalitis, and brain lesions. Stroke, multiple sclerosis, hyperthyroidism, hypothyroidism, and dementias such as Alzheimer's disease, Huntington's disease
Huntington's disease (HD), also known as Huntington's chorea, is a neurodegenerative disease that is mostly inherited. The earliest symptoms are often subtle problems with mood or mental abilities. A general lack of coordination and an uns ...
, frontotemporal dementia, and the Lewy body dementias may also be associated with schizophrenia-like psychotic symptoms. It may be necessary to rule out a delirium, which can be distinguished by visual hallucinations, acute onset and fluctuating level of consciousness, and indicates an underlying medical illness. Investigations are not generally repeated for relapse unless there is a specific ''medical'' indication or possible adverse effects
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. The term complica ...
from antipsychotic medication. In children hallucinations must be separated from typical childhood fantasies. It is difficult to distinguish childhood schizophrenia from autism.
Prevention
Prevention
Prevention may refer to:
Health and medicine
* Preventive healthcare, measures to prevent diseases or injuries rather than curing them or treating their symptoms
General safety
* Crime prevention, the attempt to reduce deter crime and crim ...
of schizophrenia is difficult as there are no reliable markers for the later development of the disorder. It is unclear as of 2011 whether treating patients in the prodrome phase of schizophrenia provides benefits. There is a discrepancy between the growth in the implementation of early intervention programmes for psychosis and the underlying empirical evidence.
There is some evidence as of 2009 that early intervention in those with first-episode psychosis may improve short-term outcomes, but there is little benefit from these measures after five years. Cognitive behavioral therapy may reduce the risk of psychosis in those at high risk after a year and is recommended in this group, by the National Institute for Health and Care Excellence
The National Institute for Health and Care Excellence (NICE) is an executive non-departmental public body of the Department of Health and Social Care in England that publishes guidelines in four areas:
* the use of health technologies withi ...
(NICE). Another preventive measure is to avoid drugs that have been associated with development of the disorder, including cannabis, cocaine, and amphetamines.
Antipsychotics are prescribed following a first-episode psychosis, and following remission a preventive maintenance use is continued to avoid relapse. However, it is recognized that some people do recover following a single episode and that long-term use of antipsychotics will not be needed but there is no way of identifying this group.
Management
The primary treatment of schizophrenia is the use of antipsychotic medications, often in combination with psychosocial interventions and social supports. Community support services including drop-in centers, visits by members of a community mental health team,supported employment
Supported employment refers to service provisions wherein people with disabilities, including intellectual disabilities, mental health, and traumatic brain injury, among others, are assisted with obtaining and maintaining employment. Supported e ...
, and support groups are common. The time between the onset of psychotic symptoms to being given treatment – the duration of untreated psychosis (DUP) – is associated with a poorer outcome in both the short term and the long term.
Voluntary
Voluntary may refer to:
* Voluntary (music)
* Voluntary or volunteer, person participating via volunteering/volunteerism
* Voluntary muscle contraction
See also
* Voluntary action
* Voluntariness, in law and philosophy
* Voluntaryism, reje ...
or involuntary admission to hospital may be imposed by doctors and courts who deem a person to be having a severe episode. In the UK, large mental hospitals termed asylums began to be closed down in the 1950s with the advent of antipsychotics, and with an awareness of the negative impact of long-term hospital stays on recovery. This process was known as deinstitutionalization
Deinstitutionalisation (or deinstitutionalization) is the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability. In the la ...
, and community and supportive services were developed in order to support this change. Many other countries followed suit with the US starting in the 60s. There still remain a smaller group of people who do not improve enough to be discharged. In some countries that lack the necessary supportive and social services, long-term hospital stays are more usual.
Medication
 The first-line treatment for schizophrenia is an antipsychotic. The first-generation antipsychotics, now called
The first-line treatment for schizophrenia is an antipsychotic. The first-generation antipsychotics, now called typical antipsychotics
Typical antipsychotics (also known as major tranquilizers, and first generation antipsychotics) are a class of antipsychotic drugs first developed in the 1950s and used to treat psychosis (in particular, schizophrenia). Typical antipsychotics ma ...
, are dopamine antagonists that block D2 receptors, and affect the neurotransmission
Neurotransmission (Latin: ''transmissio'' "passage, crossing" from ''transmittere'' "send, let through") is the process by which signaling molecules called neurotransmitters are released by the axon terminal of a neuron (the presynaptic neuron), ...
of dopamine. Those brought out later, the second-generation antipsychotics known as atypical antipsychotics
The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs (antipsychotic drugs in general are also known as major tranquilizers and ne ...
, can also have effect on another neurotransmitter, serotonin. Antipsychotics can reduce the symptoms of anxiety within hours of their use but for other symptoms they may take several days or weeks to reach their full effect. They have little effect on negative and cognitive symptoms, which may be helped by additional psychotherapies and medications. There is no single antipsychotic suitable for first-line treatment for everyone, as responses and tolerances vary between people. Stopping medication may be considered after a single psychotic episode where there has been a full recovery with no symptoms for twelve months. Repeated relapses worsen the long-term outlook and the risk of relapse following a second episode is high, and long-term treatment is usually recommended.
About half of those with schizophrenia will respond favourably to antipsychotics, and have a good return of functioning. However, positive symptoms persist in up to a third of people. Following two trials of different antipsychotics over six weeks, that also prove ineffective, they will be classed as having treatment resistant schizophrenia (TRS), and clozapine
Clozapine is a psychiatric medication and is the first atypical antipsychotic (also called second-generation antipsychotic). It is primarily used to treat people with schizophrenia and schizoaffective disorders who have had an inadequate respo ...
will be offered. Clozapine is of benefit to around half of this group although it has the potentially serious side effect of agranulocytosis (lowered white blood cell count) in less than 4% of people.
About 30 to 50 percent of people with schizophrenia do not accept that they have an illness or comply with their recommended treatment. For those who are unwilling or unable to take medication regularly, long-acting injections of antipsychotics may be used, which reduce the risk of relapse to a greater degree than oral medications. When used in combination with psychosocial interventions, they may improve long-term adherence to treatment.
Adverse effects
Extrapyramidal symptoms
Extrapyramidal symptoms (EPS) are symptoms that are archetypically associated with the extrapyramidal system of the brain's cerebral cortex. When such symptoms are caused by medications or other drugs, they are also known as extrapyramidal side ...
, including akathisia
Akathisia is a movement disorder characterized by a subjective feeling of inner restlessness accompanied by mental distress and an inability to sit still. Usually, the legs are most prominently affected. Those affected may fidget, rock back a ...
, are associated with all commercially available antipsychotic to varying degrees. There is little evidence that second generation antipsychotics have reduced levels of extrapyramidical symptoms compared to typical antipsychotics. Tardive dyskinesia
Tardive dyskinesia (TD) is a disorder that results in involuntary repetitive body movements, which may include grimacing, sticking out the tongue or smacking the lips. Additionally, there may be rapid jerking movements or slow writhing movemen ...
can occur due to long-term use of antipsychotics, developing after months or years of use. The antipsychotic clozapine
Clozapine is a psychiatric medication and is the first atypical antipsychotic (also called second-generation antipsychotic). It is primarily used to treat people with schizophrenia and schizoaffective disorders who have had an inadequate respo ...
is also associated with thromboembolism (including pulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream ( embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathin ...
), myocarditis, and cardiomyopathy.
Psychosocial interventions
A number of psychosocial interventions that include several types of psychotherapy may be useful in the treatment of schizophrenia such as: family therapy, group therapy, cognitive remediation therapy (CRT), cognitive behavioral therapy (CBT), and metacognitive training. Skills training, and help with substance use, and weight management – often needed as a side effect of an antipsychotic – are also offered. In the US, interventions for first episode psychosis have been brought together in an overall approach known as coordinated speciality care (CSC) and also includes support for education. In the UK ''care across all phases'' is a similar approach that covers many of the treatment guidelines recommended. The aim is to reduce the number of relapses and stays in hospital. Other support services for education, employment, and housing are usually offered. For people with severe schizophrenia, and discharged from a stay in hospital, these services are often brought together in an integrated approach to offer support in the community away from the hospital setting. In addition to medicine management, housing, and finances, assistance is given for more routine matters such as help with shopping and using public transport. This approach is known as assertive community treatment (ACT) and has been shown to achieve positive results in symptoms, social functioning and quality of life. Another more intense approach is known as ''intensive care management'' (ICM). ICM is a stage further than ACT and emphasises support of high intensity in smaller caseloads, (less than twenty). This approach is to provide long-term care in the community. Studies show that ICM improves many of the relevant outcomes including social functioning. Some studies have shown little evidence for the effectiveness of CBT in either reducing symptoms or preventing relapse. However, other studies have found that CBT does improve overall psychotic symptoms (when in use with medication) and it has been recommended in Canada, but has been seen to have no effect on social function, relapse, or quality of life. In the UK it is recommended as an add-on therapy in the treatment of schizophrenia. Arts therapies are seen to improve negative symptoms in some people, and are recommended by NICE in the UK. This approach is criticised as having not been well-researched, and arts therapies are not recommended in Australian guidelines for example.Peer support
Peer support occurs when people provide knowledge, experience, emotional, social or practical help to each other. It commonly refers to an initiative consisting of trained supporters (although it can be provided by peers without training), and can ...
, in which people with personal experience of schizophrenia, provide help to each other, is of unclear benefit.
Other
Exercise including aerobic exercise has been shown to improve positive and negative symptoms, cognition, working memory, and improve quality of life. Exercise has also been shown to increase the volume of thehippocampus
The hippocampus (via Latin from Greek , ' seahorse') is a major component of the brain of humans and other vertebrates. Humans and other mammals have two hippocampi, one in each side of the brain. The hippocampus is part of the limbic system, ...
in those with schizophrenia. A decrease in hippocampal volume is one of the factors linked to the development of the disease. However, there still remains the problem of increasing motivation for, and maintaining participation in physical activity. Supervised sessions are recommended. In the UK healthy eating advice is offered alongside exercise programs.
An inadequate diet is often found in schizophrenia, and associated vitamin deficiencies including those of folate
Folate, also known as vitamin B9 and folacin, is one of the B vitamins. Manufactured folic acid, which is converted into folate by the body, is used as a dietary supplement and in food fortification as it is more stable during processing an ...
, and vitamin D are linked to the risk factors for the development of schizophrenia and for early death including heart disease. Those with schizophrenia possibly have the worst diet of all the mental disorders. Lower levels of folate and vitamin D have been noted as significantly lower in first episode psychosis. The use of supplemental folate is recommended. A zinc deficiency
Zinc deficiency is defined either as insufficient zinc to meet the needs of the body, or as a serum zinc level below the normal range. However, since a decrease in the serum concentration is only detectable after long-term or severe depletion, s ...
has also been noted. Vitamin B12 is also often deficient and this is linked to worse symptoms. Supplementation with B vitamins has been shown to significantly improve symptoms, and to put in reverse some of the cognitive deficits. It is also suggested that the noted dysfunction in gut microbiota might benefit from the use of probiotics
Probiotics are live microorganisms promoted with claims that they provide health benefits when consumed, generally by improving or restoring the gut microbiota. Probiotics are considered generally safe to consume, but may cause bacteria- host i ...
.
Prognosis
obesity
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's ...
, poor diet, a sedentary lifestyle
Sedentary lifestyle is a Lifestyle (social sciences), lifestyle type, in which one is physically inactive and does little or no physical movement and or exercise. A person living a sedentary lifestyle is often sitting or lying down while enga ...
, and smoking, with an increased rate of suicide playing a lesser role. Side effects of antipsychotics may also increase the risk.
Almost 40% of those with schizophrenia die from complications of cardiovascular disease which is seen to be increasingly associated. An underlying factor of sudden cardiac death may be Brugada syndrome (BrS) – BrS mutations that overlap with those linked with schizophrenia are the calcium channel mutations. BrS may also be drug-induced from certain antipsychotics and antidepressants. Primary polydipsia, or excessive fluid intake, is relatively common in people with chronic schizophrenia. This may lead to hyponatremia
Hyponatremia or hyponatraemia is a low concentration of sodium in the blood. It is generally defined as a sodium concentration of less than 135 mmol/L (135 mEq/L), with severe hyponatremia being below 120 mEq/L. Symptoms can be a ...
which can be life-threatening. Antipsychotics can lead to a dry mouth
Xerostomia, also known as dry mouth, is dryness in the mouth, which may be associated with a change in the composition of saliva, or reduced salivary flow, or have no identifiable cause.
This symptom is very common and is often seen as a side eff ...
, but there are several other factors that may contribute to the disorder; it may reduce life expectancy by 13 per cent. Barriers to improving the mortality rate in schizophrenia are poverty, overlooking the symptoms of other illnesses, stress, stigma, and medication side effects.
Schizophrenia is a major cause of disability. In 2016, it was classed as the 12th most disabling condition. Approximately 75% of people with schizophrenia have ongoing disability with relapses. Some people do recover completely and others function well in society. Most people with schizophrenia live independently with community support. About 85% are unemployed. In people with a first episode of psychosis in schizophrenia a good long-term outcome occurs in 31%, an intermediate outcome in 42% and a poor outcome in 31%. Males are affected more often than females, and have a worse outcome. Studies showing that outcomes for schizophrenia appear better in the developing than the developed world
A developed country (or industrialized country, high-income country, more economically developed country (MEDC), advanced country) is a sovereign state that has a high quality of life, developed economy and advanced technological infrastruct ...
have been questioned. Social problems, such as long-term unemployment, poverty, homelessness, exploitation, stigmatization and victimization are common consequences, and lead to social exclusion.
There is a higher than average suicide rate
The following are lists of countries by suicide rate as published by the World Health Organization (WHO) and other sources.
About one person in 5,000–15,000 dies by suicide every year, with an estimated global rate of 10.5 per 100,000 popula ...
associated with schizophrenia estimated at 5% to 6%, most often occurring in the period following onset or first hospital admission. Several times more (20 to 40%) attempt suicide at least once. There are a variety of risk factors, including male gender, depression, a high IQ, heavy smoking, and substance use. Repeated relapse is linked to an increased risk of suicidal behavior. The use of clozapine
Clozapine is a psychiatric medication and is the first atypical antipsychotic (also called second-generation antipsychotic). It is primarily used to treat people with schizophrenia and schizoaffective disorders who have had an inadequate respo ...
can reduce the risk of suicide, and of aggression.
A strong association between schizophrenia and tobacco smoking has been shown in worldwide studies. Smoking is especially high in those diagnosed with schizophrenia, with estimates ranging from 80 to 90% being regular smokers, as compared to 20% of the general population. Those who smoke tend to smoke heavily, and additionally smoke cigarettes with high nicotine content. Some propose that this is in an effort to improve symptoms. Among people with schizophrenia use of cannabis is also common.
Schizophrenia leads to an increased risk of dementia.
Violence
Most people with schizophrenia are not aggressive, and are more likely to be victims of violence rather than perpetrators. People with schizophrenia are commonly exploited and victimized by violent crime as part of a broader dynamic of social exclusion. People diagnosed with schizophrenia are also subject to forced drug injections, seclusion, and restraint at high rates. The risk of violence by people with schizophrenia is small. There are minor subgroups where the risk is high. This risk is usually associated with a comorbid disorder such as a substance use disorder – in particular alcohol, or with antisocial personality disorder. Substance use disorder is strongly linked, and other risk factors are linked to deficits in cognition and social cognition including facial perception and insight that are in part included in theory of mind impairments. Poor cognitive functioning, decision-making, and facial perception may contribute to making a wrong judgement of a situation that could result in an inappropriate response such as violence. These associated risk factors are also present in antisocial personality disorder which when present as a comorbid disorder greatly increases the risk of violence.Epidemiology
psychotic disorder
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior ...
. The frequency of schizophrenia varies across the world, within countries, and at the local and neighborhood level; this variation in prevalence
In epidemiology, prevalence is the proportion of a particular population found to be affected by a medical condition (typically a disease or a risk factor such as smoking or seatbelt use) at a specific time. It is derived by comparing the number o ...
between studies over time, across geographical locations, and by gender is as high as fivefold.
Schizophrenia causes approximately one percent of worldwide disability adjusted life years and resulted in 17,000 deaths in 2015.
In 2000, WHO found the percentage of people affected and the number of new cases that develop each year is roughly similar around the world, with age-standardized prevalence per 100,000 ranging from 343 in Africa to 544 in Japan and Oceania for men, and from 378 in Africa to 527 in Southeastern Europe for women.
History
Conceptual development
 Accounts of a schizophrenia-like
Accounts of a schizophrenia-like syndrome
A syndrome is a set of medical signs and symptoms which are correlated with each other and often associated with a particular disease or disorder. The word derives from the Greek language, Greek σύνδρομον, meaning "concurrence". When a sy ...
are rare in records before the 19th century; the earliest case reports were in 1797 and 1809. ''Dementia praecox
Dementia praecox (meaning a "premature dementia" or "precocious madness") is a disused psychiatric diagnosis that originally designated a chronic, deteriorating psychotic disorder characterized by rapid cognitive disintegration, usually beginni ...
'', meaning premature dementia, was used by German psychiatrist Heinrich Schüle in 1886, and then in 1891 by Arnold Pick in a case report of hebephrenia. In 1893 Emil Kraepelin
Emil Wilhelm Georg Magnus Kraepelin (; ; 15 February 1856 – 7 October 1926) was a German psychiatrist.
H. J. Eysenck's ''Encyclopedia of Psychology'' identifies him as the founder of modern scientific psychiatry, psychopharmacology and psych ...
used the term in making a distinction, known as the Kraepelinian dichotomy
The Kraepelinian dichotomy is the division of the major endogenous psychoses into the disease concepts of dementia praecox, which was reformulated as schizophrenia by Eugen Bleuler by 1908, and manic-depressive psychosis, which has now been recon ...
, between the two psychoses – dementia praecox, and manic depression (now called bipolar disorder). When it became evident that the disorder was not a degenerative dementia, it was renamed schizophrenia by Eugen Bleuler in 1908.
The word ''schizophrenia'' translates as 'splitting of the mind' and is Modern Latin
New Latin (also called Neo-Latin or Modern Latin) is the revival of Literary Latin used in original, scholarly, and scientific works since about 1500. Modern scholarly and technical nomenclature, such as in zoological and botanical taxonomy a ...
from the Greek
Greek may refer to:
Greece
Anything of, from, or related to Greece, a country in Southern Europe:
*Greeks, an ethnic group.
*Greek language, a branch of the Indo-European language family.
**Proto-Greek language, the assumed last common ancestor ...
words ''schizein'' (σχίζειν, 'to split') and ''phrēn'', (φρήν, 'mind') Its use was intended to describe the separation of function between personality, thinking
In their most common sense, the terms thought and thinking refer to conscious cognitive processes that can happen independently of sensory stimulation. Their most paradigmatic forms are judging, reasoning, concept formation, problem solving, an ...
, memory, and perception.
In the early 20th century, the psychiatrist Kurt Schneider categorized the psychotic symptoms of schizophrenia into two groups – hallucinations and delusions. The hallucinations were listed as specific to auditory and the delusions included thought disorders. These were seen as important symptoms, termed ''first-rank''. The most common first-rank symptom was found to belong to thought disorders. In 2013 the first-rank symptoms were excluded from the DSM-5 criteria; while they may not be useful in diagnosing schizophrenia, they can assist in differential diagnosis.
Subtypes of schizophrenia – classified as paranoid, disorganized, catatonic, undifferentiated, and residual – were difficult to distinguish and are no longer recognized as separate conditions by DSM-5 (2013) or ICD-11
The ICD-11 is the eleventh revision of the International Classification of Diseases (ICD). It replaces the ICD-10 as the global standard for recording health information and causes of death. The ICD is developed and annually updated by the World H ...
.
Breadth of diagnosis
Before the 1960s, nonviolent petty criminals and women were sometimes diagnosed with schizophrenia, categorizing the latter as ill for not performing their duties within patriarchy as wives and mothers. In the mid-to-late 1960s, black men were categorized as "hostile and aggressive" and diagnosed as schizophrenic at much higher rates, their civil rights and Black Power activism labeled as delusions. In the early 1970s in the US, the diagnostic model for schizophrenia was broad and clinically based using DSM II. Schizophrenia was diagnosed far more in the US than in Europe which used the ICD-9 criteria. The US model was criticised for failing to demarcate clearly those people with a mental illness. In 1980 DSM III was published and showed a shift in focus from the clinically based biopsychosocial model to a reason-based medical model. DSM IV brought an increased focus on an evidence-based medical model.Historical treatment
 In the 1930s a number of shock procedures which induced seizures (convulsions) or comas were used to treat schizophrenia. Insulin shock involved injecting large doses of insulin to induce comas, which in turn produced hypoglycemia and convulsions. The use of electricity to induce seizures was in use as
In the 1930s a number of shock procedures which induced seizures (convulsions) or comas were used to treat schizophrenia. Insulin shock involved injecting large doses of insulin to induce comas, which in turn produced hypoglycemia and convulsions. The use of electricity to induce seizures was in use as electroconvulsive therapy
Electroconvulsive therapy (ECT) is a psychiatric treatment where a generalized seizure (without muscular convulsions) is electrically induced to manage refractory mental disorders.Rudorfer, MV, Henry, ME, Sackeim, HA (2003)"Electroconvulsive th ...
(ECT) by 1938.
Psychosurgery, including the lobotomy
A lobotomy, or leucotomy, is a form of neurosurgical treatment for psychiatric disorder or neurological disorder (e.g. epilepsy) that involves severing connections in the brain's prefrontal cortex. The surgery causes most of the connections t ...
and frontal lobotomy – carried out from the 1930s until the 1970s in the United States, and until the 1980s in France – are recognized as a human rights abuse. In the mid-1950s the first typical antipsychotic
Typical antipsychotics (also known as major tranquilizers, and first generation antipsychotics) are a class of antipsychotic drugs first developed in the 1950s and used to treat psychosis (in particular, schizophrenia). Typical antipsychotics ma ...
, chlorpromazine
Chlorpromazine (CPZ), marketed under the brand names Thorazine and Largactil among others, is an antipsychotic medication. It is primarily used to treat psychotic disorders such as schizophrenia. Other uses include the treatment of bipolar di ...
, was introduced, followed in the 1970s by the first atypical antipsychotic
The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs (antipsychotic drugs in general are also known as major tranquilizers and ne ...
, clozapine
Clozapine is a psychiatric medication and is the first atypical antipsychotic (also called second-generation antipsychotic). It is primarily used to treat people with schizophrenia and schizoaffective disorders who have had an inadequate respo ...
.
Political abuse
From the 1960s until 1989, psychiatrists in the USSR and Eastern Bloc diagnosed thousands of people withsluggish schizophrenia
Sluggish schizophrenia or slow progressive schizophrenia (russian: вялотеку́щая шизофрени́я, translit=vyalotekushchaya shizofreniya) was a diagnostic category used in the Soviet Union to describe what was claimed to be a for ...
, without signs of psychosis, based on "the assumption that symptoms would later appear". Now discredited, the diagnosis provided a convenient way to confine political dissidents.
Society and culture
 In 2002, the term for schizophrenia in Japan was changed from to to reduce stigma. The new name, also interpreted as "integration disorder", was inspired by the biopsychosocial model. A similar change was made in South Korea in 2012 to attunement disorder.
In the United States, the annual cost of schizophrenia – including direct costs (outpatient, inpatient, drugs, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment) – was estimated at $62.7 billion for the year 2002. In the UK the cost in 2016 was put at £11.8 billion per year with a third of that figure directly attributable to the cost of hospital, social care and treatment.
In 2002, the term for schizophrenia in Japan was changed from to to reduce stigma. The new name, also interpreted as "integration disorder", was inspired by the biopsychosocial model. A similar change was made in South Korea in 2012 to attunement disorder.
In the United States, the annual cost of schizophrenia – including direct costs (outpatient, inpatient, drugs, and long-term care) and non-healthcare costs (law enforcement, reduced workplace productivity, and unemployment) – was estimated at $62.7 billion for the year 2002. In the UK the cost in 2016 was put at £11.8 billion per year with a third of that figure directly attributable to the cost of hospital, social care and treatment.
Cultural depictions
The book '' A Beautiful Mind'' chronicled the life ofJohn Forbes Nash
John Forbes Nash Jr. (June 13, 1928 – May 23, 2015) was an American mathematician who made fundamental contributions to game theory, real algebraic geometry, differential geometry, and partial differential equations. Nash and fellow g ...
who had been diagnosed with schizophrenia and won the Nobel Memorial Prize in Economic Sciences
The Nobel Memorial Prize in Economic Sciences, officially the Sveriges Riksbank Prize in Economic Sciences in Memory of Alfred Nobel ( sv, Sveriges riksbanks pris i ekonomisk vetenskap till Alfred Nobels minne), is an economics award administered ...
. The book was made into a film with the same name; an earlier documentary film was '' A Brilliant Madness''.
In 1964 a case study
A case study is an in-depth, detailed examination of a particular case (or cases) within a real-world context. For example, case studies in medicine may focus on an individual patient or ailment; case studies in business might cover a particular fi ...
of three males diagnosed with schizophrenia who each had the delusional belief that they were Jesus Christ was published as ''The Three Christs of Ypsilanti
''The Three Christs of Ypsilanti'' (1964) is a book-length psychiatric case study by Milton Rokeach, concerning his experiment on a group of three males with paranoid schizophrenia at Ypsilanti State Hospital in Ypsilanti, Michigan. The book deta ...
''; a film with the title '' Three Christs'' was released in 2020.
Media coverage reinforces public perception of an association between schizophrenia and violence; in film, people with schizophrenia are highly likely to be portrayed as a danger to others. In the UK guidelines for reporting conditions and award campaigns have shown a reduction in negative reporting since 2013.
Research directions
A 2015 Cochrane review found unclear evidence of benefit from brain stimulation techniques to treat the positive symptoms of schizophrenia, in particular auditory verbal hallucinations (AVHs). Most studies focus ontranscranial direct-current stimulation
Transcranial direct current stimulation (tDCS) is a form of neuromodulation that uses constant, low direct current delivered via electrodes on the head. It was originally developed to help patients with brain injuries or neuropsychiatric conditio ...
(tDCM), and repetitive transcranial magnetic stimulation (rTMS). Techniques based on focused ultrasound for deep brain stimulation
Deep brain stimulation (DBS) is a neurosurgical procedure involving the placement of a medical device called a neurostimulator, which sends electrical impulses, through implanted electrodes, to specific targets in the brain (the brain nucleus ...
could provide insight for the treatment of AVHs.
The study of potential biomarkers
In biomedical contexts, a biomarker, or biological marker, is a measurable indicator of some biological state or condition. Biomarkers are often measured and evaluated using blood, urine, or soft tissues to examine normal biological processes, pa ...
that would help in diagnosis and treatment of schizophrenia is an active area of research as of 2020. Possible biomarkers include markers of inflammation, neuroimaging, brain-derived neurotrophic factor
Brain-derived neurotrophic factor (BDNF), or abrineurin, is a protein found in the and the periphery. that, in humans, is encoded by the ''BDNF'' gene. BDNF is a member of the neurotrophin family of growth factors, which are related to the canon ...
(BDNF), and speech analysis. Some markers such as C-reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin- ...
are useful in detecting levels of inflammation implicated in some psychiatric disorders but they are not disorder-specific. Other inflammatory cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrin ...
s are found to be elevated in first episode psychosis and acute relapse that are normalized after treatment with antipsychotics, and these may be considered as state markers. Deficits in sleep spindles in schizophrenia may serve as a marker of an impaired thalamocortical circuit, and a mechanism for memory impairment. MicroRNA
MicroRNA (miRNA) are small, single-stranded, non-coding RNA molecules containing 21 to 23 nucleotides. Found in plants, animals and some viruses, miRNAs are involved in RNA silencing and post-transcriptional regulation of gene expression. mi ...
s are highly influential in early neuronal development, and their disruption is implicated in several CNS disorders; circulating microRNAs (cimiRNAs) are found in body fluids such as blood and cerebrospinal fluid, and changes in their levels are seen to relate to changes in microRNA levels in specific regions of brain tissue. These studies suggest that cimiRNAs have the potential to be early and accurate biomarkers in a number of disorders including schizophrenia.
Explanatory notes
References
External links
* {{Featured article 1900s neologisms Psychosis