Traditional Chinese medicine (TCM) is an
alternative medical practice drawn from
traditional medicine
Traditional medicine (also known as indigenous medicine or folk medicine) comprises medical aspects of traditional knowledge that developed over generations within the folk beliefs of various societies, including indigenous peoples, before the ...
in China. It has been described as "fraught with
pseudoscience
Pseudoscience consists of statements, beliefs, or practices that claim to be both scientific and factual but are incompatible with the scientific method. Pseudoscience is often characterized by contradictory, exaggerated or falsifiability, unfa ...
", with the majority of its treatments having no logical
mechanism of action
In pharmacology, the term mechanism of action (MOA) refers to the specific biochemical interaction through which a drug substance produces its pharmacological effect. A mechanism of action usually includes mention of the specific molecular targe ...
.
Medicine in traditional China encompassed a range of sometimes competing health and healing practices,
folk beliefs
In folkloristics, folk belief or folk-belief is a broad genre of folklore that is often expressed in narratives, customs, rituals, foodways, proverbs, and rhymes. It also includes a wide variety of behaviors, expressions, and beliefs. Examples of ...
,
literati theory and
Confucian philosophy
Confucianism, also known as Ruism or Ru classicism, is a system of thought and behavior originating in ancient China. Variously described as tradition, a philosophy, a religion, a humanistic or rationalistic religion, a way of governing, or ...
,
herbal remedies
Herbal medicine (also herbalism) is the study of pharmacognosy and the use of medicinal plants, which are a basis of traditional medicine. With worldwide research into pharmacology, some herbal medicines have been translated into modern remedies ...
,
food
Food is any substance consumed by an organism for nutritional support. Food is usually of plant, animal, or fungal origin, and contains essential nutrients, such as carbohydrates, fats, proteins, vitamins, or minerals. The substance is inge ...
, diet, exercise, medical specializations, and schools of thought. In the early twentieth century, Chinese cultural and political modernizers worked to eliminate traditional practices as backward and unscientific. Traditional practitioners then selected elements of philosophy and practice and organized them into what they called "Chinese medicine" (''Zhongyi''). In the 1950s, the Chinese government sponsored the integration of Chinese and Western medicine, and in the
Great Proletarian Cultural Revolution
The Cultural Revolution, formally known as the Great Proletarian Cultural Revolution, was a sociopolitical movement in the People's Republic of China (PRC) launched by Mao Zedong in 1966, and lasting until his death in 1976. Its stated goal ...
of the 1960s, promoted Chinese medicine as inexpensive and popular.
After the opening of relations between the United States and China after 1972, there was great interest in the West for what is now called traditional Chinese medicine (TCM).
TCM is said to be based on such texts as ''
Huangdi Neijing
''Huangdi Neijing'' (), literally the ''Inner Canon of the Yellow Emperor'' or ''Esoteric Scripture of the Yellow Emperor'', is an ancient Chinese medical text or group of texts that has been treated as a fundamental doctrinal source for Chines ...
'' (The Inner Canon of the Yellow Emperor), and ''
Compendium of Materia Medica
The ''Bencao gangmu'', known in English as the ''Compendium of Materia Medica'' or ''Great Pharmacopoeia'', is an encyclopedic gathering of medicine, natural history, and Chinese herbology compiled and edited by Li Shizhen and published in the ...
'', a sixteenth-century encyclopedic work, and includes various forms of
herbal medicine
Herbal medicine (also herbalism) is the study of pharmacognosy and the use of medicinal plants, which are a basis of traditional medicine. With worldwide research into pharmacology, some herbal medicines have been translated into modern remed ...
,
acupuncture
Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine (TCM) in which thin needles are inserted into the body. Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientifi ...
,
cupping therapy
Cupping therapy is a form of alternative medicine in which a local suction is created on the skin with the application of heated cups. Its practice mainly occurs in Asia but also in Eastern Europe, the Middle East, and Latin America. Cupping has ...
,
gua sha
''Gua sha'' (), or ''kerokan'' (in Indonesia), is a traditional Chinese medicine (TCM) practice in which a tool is used to scrape people's skin in order to produce light petechiae. Practitioners believe that ''gua sha'' releases unhealthy bodily ...
,
massage (tui na),
bonesetter (die-da),
exercise (qigong), and dietary therapy. TCM is widely used in the
Sinosphere
The East Asian cultural sphere, also known as the Sinosphere, the Sinic world, the Sinitic world, the Chinese cultural sphere, the Chinese character sphere encompasses multiple countries in East Asia and Southeast Asia that were historically ...
. One of the basic tenets is that the body's
vital energy
Vitalism is a belief that starts from the premise that "living organisms are fundamentally different from non-living entities because they contain some non-physical element or are governed by different principles than are inanimate things." Wher ...
(''ch'i'' or ''
qi'') is circulating through channels called
meridians having branches connected to bodily organs and functions.
The concept of vital energy is pseudoscientific. Concepts of the body and of disease used in TCM reflect its ancient origins and its emphasis on dynamic processes over material structure, similar to the
humoral theory
Humorism, the humoral theory, or humoralism, was a system of medicine detailing a supposed makeup and workings of the human body, adopted by Ancient Greek and Roman physicians and philosophers.
Humorism began to fall out of favor in the 1850s ...
of
ancient Greece
Ancient Greece ( el, ß╝Ö╬╗╬╗╬¼Žé, Hell├Īs) was a northeastern Mediterranean civilization, existing from the Greek Dark Ages of the 12thŌĆō9th centuries BC to the end of classical antiquity ( AD 600), that comprised a loose collection of cult ...
and
ancient Rome
In modern historiography, ancient Rome refers to Roman civilisation from the founding of the city of Rome in the 8th century BC to the collapse of the Western Roman Empire in the 5th century AD. It encompasses the Roman Kingdom (753ŌĆō509 B ...
.
The demand for traditional medicines in China has been a major generator of
illegal wildlife smuggling, linked to the
killing and smuggling of endangered animals.
History

Scholars in the history of medicine in China distinguish its doctrines and practice from those of present-day TCM. As
Ian Johnson notes, the term "Traditional Chinese Medicine" was coined by "party propagandists" and first appeared in English in 1955.
Nathan Sivin
Nathan Sivin (11 May 1931 ŌĆō 24 June 2022), also known as Xiwen (), was an American sinologist, historian, essayist, educator, and writer. He taught first at Massachusetts Institute of Technology, then at the University of Pennsylvania until his r ...
criticizes attempts to treat medicine and medical practices in traditional China as if they were a single system. Instead, he says, there were 2,000 years of "medical system in turmoil" and speaks of a "myth of an unchanging medical tradition." He urges that "Traditional medicine translated purely into terms of modern medicine becomes partly nonsensical, partly irrelevant, and partly mistaken; that is also true the other way around, a point easily overlooked." TJ Hinrichs observes that people in modern Western societies divide healing practices into biomedicine for the body, psychology for the mind, and religion for the spirit, but these distinctions are inadequate to describe medical concepts among Chinese historically and to a considerable degree today.
The medical anthropologist
Charles Leslie writes that Chinese, Greco-Arabic, and Indian
traditional medicines were all grounded in systems of correspondence that aligned the organization of society, the universe, and the human body and other forms of life into an "all-embracing order of things." Each of these traditional systems was organized with such qualities as heat and cold, wet and dry, light and darkness, qualities that also align the seasons, compass directions, and the human cycle of birth, growth, and death. They provided, Leslie continued, a "comprehensive way of conceiving patterns that ran through all of nature," and they "served as a classificatory and mnemonic device to observe health problems and to reflect upon, store, and recover empirical knowledge," but they were also "subject to stultifying theoretical elaboration, self-deception, and
dogma
Dogma is a belief or set of beliefs that is accepted by the members of a group without being questioned or doubted. It may be in the form of an official system of principles or doctrines of a religion, such as Roman Catholicism, Judaism, Islam ...
tism."
The doctrines of Chinese medicine are rooted in books such as the ''
Yellow Emperor's Inner Canon'' and the ''
Treatise on Cold Damage'', as well as in cosmological notions such as
yinŌĆōyang and the
five phases
(; Japanese: (); Korean: (); Vietnamese: ''ng┼® h├Ānh'' (õ║öĶĪī)), usually translated as Five Phases or Five Agents, is a fivefold conceptual scheme that many traditional Chinese fields used to explain a wide array of phenomena, from cosmi ...
. The "Documentation of Chinese materia medica" (CMM) dates back to around 1,100 BCE when only a few dozen drugs were described. By the end of the 16th century, the number of drugs documented had reached close to 1,900. And by the end of the last century, published records of CMM had reached 12,800 drugs."
Starting in the 1950s, these precepts were standardized in the People's Republic of China, including attempts to integrate them with modern notions of
anatomy
Anatomy () is the branch of biology concerned with the study of the structure of organisms and their parts. Anatomy is a branch of natural science that deals with the structural organization of living things. It is an old science, having its ...
and
pathology
Pathology is the study of the causes and effects of disease or injury. The word ''pathology'' also refers to the study of disease in general, incorporating a wide range of biology research fields and medical practices. However, when used in ...
. In the 1950s, the Chinese government promoted a systematized form of TCM.
Shang dynasty
Traces of therapeutic activities in China date from the
Shang dynasty
The Shang dynasty (), also known as the Yin dynasty (), was a Chinese royal dynasty founded by Tang of Shang (Cheng Tang) that ruled in the Yellow River valley in the second millennium BC, traditionally succeeding the Xia dynasty and ...
(14thŌĆō11th centuries BCE).
Though the Shang did not have a concept of "medicine" as distinct from other health practices, their
oracular
An oracle is a person or agency considered to provide wise and insightful counsel or prophetic predictions, most notably including precognition of the future, inspired by deities. As such, it is a form of divination.
Description
The word ''or ...
inscriptions on
bones
A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, a ...
and tortoise shells refer to illnesses that affected the Shang royal family: eye disorders, toothaches, bloated abdomen, and such.
Shang elites usually attributed them to curses sent by their ancestors. There is currently no evidence that the Shang nobility used herbal remedies.
Stone and bone needles found in ancient tombs led
Joseph Needham
Noel Joseph Terence Montgomery Needham (; 9 December 1900 ŌĆō 24 March 1995) was a British biochemist, historian of science and sinologist known for his scientific research and writing on the history of Chinese science and technology, in ...
to speculate that acupuncture might have been carried out in the Shang dynasty.
This being said, most historians now make a distinction between medical
lancing (or
bloodletting
Bloodletting (or blood-letting) is the withdrawal of blood from a patient to prevent or cure illness and disease. Bloodletting, whether by a physician or by leeches, was based on an ancient system of medicine in which blood and other bodily flu ...
) and acupuncture in the narrower sense of using metal needles to attempt to treat illnesses by stimulating
points along
circulation channels ("meridians") in accordance with beliefs related to the circulation of "Qi".
The earliest evidence for acupuncture in this sense dates to the second or first century BCE.
Han dynasty
The ''Yellow Emperor's Inner Canon (
Huangdi Nei Jing)'', the oldest received work of Chinese medical theory, was compiled during the
Han dynasty
The Han dynasty (, ; ) was an imperial dynasty of China (202 BC ŌĆō 9 AD, 25ŌĆō220 AD), established by Liu Bang (Emperor Gao) and ruled by the House of Liu. The dynasty was preceded by the short-lived Qin dynasty (221ŌĆō207 BC) and a warr ...
around the first century BCE on the basis of shorter texts from different medical lineages.
Written in the form of dialogues between the legendary
Yellow Emperor
The Yellow Emperor, also known as the Yellow Thearch or by his Chinese name Huangdi (), is a deity ('' shen'') in Chinese religion, one of the legendary Chinese sovereigns and culture heroes included among the mytho-historical Three Soverei ...
and his ministers, it offers explanations on the relation between humans, their environment, and the
cosmos
The cosmos (, ) is another name for the Universe. Using the word ''cosmos'' implies viewing the universe as a complex and orderly system or entity.
The cosmos, and understandings of the reasons for its existence and significance, are studied in ...
, on the contents of the body, on human vitality and pathology, on the symptoms of illness, and on how to make diagnostic and therapeutic decisions in light of all these factors.
Unlike earlier texts like ''
Recipes for Fifty-Two Ailments'', which was excavated in the 1970s from the
Mawangdui tomb that had been sealed in 168 BCE, the ''Inner Canon'' rejected the influence of spirits and the use of magic.
It was also one of the first books in which the cosmological doctrines of Yinyang and the Five Phases were brought to a mature synthesis.
The ''Treatise on Cold Damage Disorders and Miscellaneous Illnesses (Shang Han Lun)'' was collated by
Zhang Zhongjing
Zhang Zhongjing (; 150ŌĆō219), formal name Zhang Ji (), was a Chinese pharmacologist, physician, inventor, and writer of the Eastern Han dynasty and one of the most eminent Chinese physicians during the later years of the Han dynasty. He estab ...
sometime between 196 and 220 CE; at the end of the Han dynasty. Focusing on drug prescriptions rather than acupuncture,
it was the first medical work to combine Yinyang and the Five Phases with drug therapy.
This
formulary was also the earliest public Chinese medical text to group symptoms into clinically useful "patterns" (''zheng'' ) that could serve as targets for therapy. Having gone through numerous changes over time, the formulary now circulates as two distinct books: the ''
Treatise on Cold Damage Disorders'' and the ''
Essential Prescriptions of the Golden Casket'', which were edited separately in the eleventh century, under the
Song dynasty
The Song dynasty (; ; 960ŌĆō1279) was an imperial dynasty of China that began in 960 and lasted until 1279. The dynasty was founded by Emperor Taizu of Song following his usurpation of the throne of the Later Zhou. The Song conquered the rest ...
.
Nanjing
Nanjing (; , Mandarin pronunciation: ), alternately romanized as Nanking, is the capital of Jiangsu province of the People's Republic of China. It is a sub-provincial city, a megacity, and the second largest city in the East China region. T ...
or "Classic of Difficult Issues," originally called "The Yellow Emperor Eighty-one Nan Jing", ascribed to
Bian Que
Bian Que (; 407 ŌĆō 310 BC) was an ancient Chinese figure traditionally said to be the earliest known Chinese physician during the Warring States period. His real name is said to be Qin Yueren (), but his medical skills were so amazing that peop ...
in the
eastern Han dynasty
The Han dynasty (, ; ) was an imperial dynasty of China (202 BC ŌĆō 9 AD, 25ŌĆō220 AD), established by Liu Bang (Emperor Gao) and ruled by the House of Liu. The dynasty was preceded by the short-lived Qin dynasty (221ŌĆō207 BC) and a warr ...
. This book was compiled in the form of question-and-answer explanations. A total of 81 questions have been discussed. Therefore, it is also called "Eighty-One Nan".
The book is based on basic theory and has also analyzed some disease certificates. Questions one to twenty-two is about pulse study, questions twenty-three to twenty-nine is about meridian study, questions thirty to forty-seven is related to urgent illnesses, questions forty-eight to sixty-one is related to serious diseases, questions sixty-two to sixty-eight is related to acupuncture points, and questions sixty-nine to eighty-one is related to the needlepoint methods.
The book is credited as developing its own path, while also inheriting the theories from Huangdi Neijing. The content includes physiology, pathology, diagnosis, treatment contents, and a more essential and specific discussion of pulse diagnosis.
It has become one of the four classics for Chinese medicine practitioners to learn from and has impacted the medical development in China.
''
Shennong Ben Cao Jing
''Shennong Bencaojing'' (also ''Classic of the Materia Medica'' or ''Shen-nong's Herbal Classics'' and ''Shen-nung Pen-tsao Ching''; ) is a Chinese book on agriculture and medicinal plants, traditionally attributed to Shennong. Researchers belie ...
'' is one of the earliest written medical books in China. Written during the Eastern Han Dynasty between 200 and 250 CE, it was the combined effort of practitioners in the Qin and Han Dynasties who summarized, collected and compiled the results of pharmacological experience during their time periods. It was the first systematic summary of Chinese herbal medicine.
Most of the pharmacological theories and compatibility rules and the proposed "seven emotions and harmony" principle have played a role in the practice of medicine for thousands of years.
Therefore, it has been a textbook for medical workers in modern China.
The full text of ''Shennong Ben Cao Jing'' in English can be found online.
[Shen Nong Ben Cao Ling (The Divine Farmers Materia Medica)](_blank)
archive.org
Post-Han dynasty
In the centuries that followed, several shorter books tried to summarize or systematize the contents of the ''Yellow Emperor's Inner Canon''. The ''Canon of Problems'' (probably second century CE) tried to reconcile divergent doctrines from the ''Inner Canon'' and developed a complete medical system centered on needling therapy.
The ''AB Canon of Acupuncture and Moxibustion'' (''Zhenjiu jiayi jing'' , compiled by
Huangfu Mi
Huangfu Mi (215ŌĆō282), courtesy name Shi'an (), was a Chinese physician, essayist, historian, poet, and writer who lived through the late Eastern Han dynasty, Three Kingdoms period and early Western Jin dynasty. He was born in a poor farming fam ...
sometime between 256 and 282 CE) assembled a consistent body of doctrines concerning acupuncture;
whereas the ''Canon of the Pulse'' (''Maijing'' ; c. 280) presented itself as a "comprehensive handbook of diagnostics and therapy."
Around 900ŌĆō1000 AD, Chinese were the first to develop a form of vaccination, known as
variolation
Variolation was the method of inoculation first used to immunize individuals against smallpox (''Variola'') with material taken from a patient or a recently variolated individual, in the hope that a mild, but protective, infection would result. Var ...
or
inoculation
Inoculation is the act of implanting a pathogen or other microorganism. It may refer to methods of artificially inducing immunity against various infectious diseases, or it may be used to describe the spreading of disease, as in "self-inoculati ...
, to prevent
smallpox
Smallpox was an infectious disease caused by variola virus (often called smallpox virus) which belongs to the genus Orthopoxvirus. The last naturally occurring case was diagnosed in October 1977, and the World Health Organization (WHO) c ...
. Chinese physicians had realised that when healthy people were exposed to smallpox scab tissue, they had a smaller chance of being infected by the disease later on. The common methods of inoculation at the time was through crushing smallpox scabs into powder and breathing it through the nose.
Prominent medical scholars of the post-Han period included
Tao Hongjing
Tao Hongjing (456ŌĆō536), courtesy name Tongming, was a Chinese alchemist, astronomer, calligrapher, military general, musician, physician, and pharmacologist, and writer during the Northern and Southern dynasties (420ŌĆō589). A polymathic indiv ...
(456ŌĆō536),
Sun Simiao
Sun Simiao (; died 682) was a Chinese physician and writer of the Sui and Tang dynasty. He was titled as China's King of Medicine (, Yaowang) for his significant contributions to Chinese medicine and tremendous care to his patients.
Books
Sun ...
of the Sui and Tang dynasties,
Zhang Jiegu
Zhang Yuansu Õ╝Āõ║ōń┤Ā (a.k.a. Zhang Jiegu; ca. 1151ŌĆō1234) was one of the most historically influential Traditional Chinese medicine physicians in the period of transition from China's northern Jin dynasty to the Mongolian Yuan dynasty
...
(ŌĆō1234), and
Li Shizhen
Li Shizhen (July 3, 1518 ŌĆō 1593), courtesy name Dongbi, was a Chinese acupuncturist, herbalist, naturalist, pharmacologist, physician, and writer of the Ming dynasty. He is the author of a 27-year work, found in the ''Compendium of M ...
(1518ŌĆō1593).
People's Republic
In 1950,
Chinese Communist Party
The Chinese Communist Party (CCP), officially the Communist Party of China (CPC), is the founding and One-party state, sole ruling party of the China, People's Republic of China (PRC). Under the leadership of Mao Zedong, the CCP emerged victoriou ...
(CCP) chairman
Mao Zedong
Mao Zedong pronounced ; also romanised traditionally as Mao Tse-tung. (26 December 1893 ŌĆō 9 September 1976), also known as Chairman Mao, was a Chinese communist revolutionary who was the founder of the People's Republic of China (PRC) ...
announced support of traditional Chinese medicine, but he did not personally believe in and did not use it.
In 1952, the president of the
Chinese Medical Association
In China, the practice of medicine is a mixture of government, charitable, and private institutions, while many people rely on traditional medicine. Until reforms in the late twentieth and early twenty-first century, physicians were quasi-governm ...
said that, "This One Medicine, will possess a basis in modern natural sciences, will have absorbed the ancient and the new, the Chinese and the foreign, all medical achievementsŌĆöand will be China's New Medicine!"
During the
Cultural Revolution
The Cultural Revolution, formally known as the Great Proletarian Cultural Revolution, was a sociopolitical movement in the People's Republic of China (PRC) launched by Mao Zedong in 1966, and lasting until his death in 1976. Its stated goal ...
(1966ŌĆō1976) the CCP and the government emphasized modernity, cultural identity and China's social and economic reconstruction and contrasted them to the colonial and feudal past. The government established a grassroots health care system as a step in the search for a new national identity and tried to revitalize traditional medicine and made large investments in traditional medicine to try to develop affordable medical care and public health facilities.
The Ministry of Health directed health care throughout China and established primary care units. Chinese physicians trained in Western medicine were required to learn traditional medicine, while traditional healers received training in modern methods. This strategy aimed to integrate modern medical concepts and methods and revitalize appropriate aspects of traditional medicine. Therefore, traditional Chinese medicine was re-created in response to Western medicine.
In 1968, the CCP supported a new system of health care delivery for rural areas. Villages were assigned a
barefoot doctor
Barefoot doctors () were healthcare providers who underwent basic medical training and worked in rural villages in China. They included farmers, folk healers, rural healthcare providers, and recent middle or secondary school graduates who receiv ...
(a medical staff with basic medical skills and knowledge to deal with minor illnesses) responsible for basic medical care. The medical staff combined the values of traditional China with modern methods to provide health and medical care to poor farmers in remote rural areas. The barefoot doctors became a symbol of the Cultural Revolution, for the introduction of modern medicine into villages where traditional Chinese medicine services were used.
In the second decade of the twenty-first century,
Chinese Communist Party
The Chinese Communist Party (CCP), officially the Communist Party of China (CPC), is the founding and One-party state, sole ruling party of the China, People's Republic of China (PRC). Under the leadership of Mao Zedong, the CCP emerged victoriou ...
general secretary
Xi Jinping
Xi Jinping ( ; ; ; born 15 June 1953) is a Chinese politician who has served as the general secretary of the Chinese Communist Party (CCP) and chairman of the Central Military Commission (CMC), and thus as the paramount leader of China, s ...
strongly supported TCM, calling it a "gem". As of May 2011, in order to promote TCM worldwide, China had signed TCM partnership agreements with over 70 countries.
His government pushed to increase its use and the number of TCM-trained doctors and announced that students of TCM would no longer be required to pass examinations in Western medicine. Chinese scientists and researchers, however, expressed concern that TCM training and therapies would receive equal support with Western medicine. They also criticized a reduction in government testing and regulation of the production of TCMs, some of which were toxic. Government censors have removed Internet posts that question TCM.
Hong Kong
At the beginning of
Hong Kong
Hong Kong ( (US) or (UK); , ), officially the Hong Kong Special Administrative Region of the People's Republic of China ( abbr. Hong Kong SAR or HKSAR), is a city and special administrative region of China on the eastern Pearl River Delt ...
's opening up, Western medicine was not yet popular, and Western medicine doctors were mostly foreigners; local residents mostly relied on Chinese medicine practitioners. In 1841, the British government of Hong Kong issued an announcement pledging to govern Hong Kong residents in accordance with all the original rituals, customs and private legal property rights.
As traditional Chinese medicine had always been used in China, the use of traditional Chinese medicine was not regulated.
The establishment in 1870 of the
Tung Wah Hospital
Tung Wah Hospital is a Charitable hospital in Hong Kong under the Tung Wah Group of Hospitals. Located above Possession Point, at 12 Po Yan Street in Sheung Wan, it is the first hospital established in Colonial Hong Kong for the general publi ...
was the first use of Chinese medicine for the treatment in Chinese hospitals providing free medical services.
As the promotion of Western medicine by the British government started from 1940,
Western medicine started being popular among Hong Kong population. In 1959, Hong Kong had researched the use of traditional Chinese medicine to replace Western medicine.
Critique
Historians of science
The history of science covers the development of science from ancient times to the present. It encompasses all three major branches of science: natural, social, and formal.
Science's earliest roots can be traced to Ancient Egypt and Mesop ...
have developed the study of medicine in traditional China into a field with its own scholarly associations, journals, graduate programs, and debates with each other. Many distinguish "medicine in traditional China" from the recent Traditional Chinese Medicine (TCM), which took elements from traditional texts and practices to construct a systematic body. Paul Unschuld, for instance, sees a "departure of TCM from its historical origins." What is called "Traditional Chinese Medicine" and practiced today in China and the West is not thousands of years old, but recently constructed using selected traditional terms, some of which have been taken out of context, some badly misunderstood. He has criticized Chinese and Western popular books for
selective use of evidence, choosing only those works or parts of historical works that seem to lead to modern medicine, ignoring those elements that do not now seem to be effective.
A 2007 editorial the journal ''Nature'' wrote that TCM "remains poorly researched and supported, and most of its treatments have no logical
mechanism of action
In pharmacology, the term mechanism of action (MOA) refers to the specific biochemical interaction through which a drug substance produces its pharmacological effect. A mechanism of action usually includes mention of the specific molecular targe ...
."
Critics say that TCM theory and practice have no basis in
modern science
The history of science covers the development of science from ancient history, ancient times to the present. It encompasses all three major branches of science: natural science, natural, social science, social, and formal science, formal.
Sc ...
, and TCM practitioners do not agree on what diagnosis and treatments should be used for any given person.
A ''
Nature
Nature, in the broadest sense, is the physics, physical world or universe. "Nature" can refer to the phenomenon, phenomena of the physical world, and also to life in general. The study of nature is a large, if not the only, part of science. ...
'' editorial described TCM as "fraught with
pseudoscience
Pseudoscience consists of statements, beliefs, or practices that claim to be both scientific and factual but are incompatible with the scientific method. Pseudoscience is often characterized by contradictory, exaggerated or falsifiability, unfa ...
".
A review of the literature in 2008 found that scientists are "still unable to find a shred of evidence" according to standards of
science-based medicine
''Science-Based Medicine'' is a website and blog with articles covering issues in science and medicine, especially medical scams and practices. Founded in 2008, it is owned and operated by the New England Skeptical Society and run by Steven N ...
for traditional Chinese concepts such as ''qi'', meridians, and acupuncture points,
and that the traditional principles of acupuncture are deeply flawed.
"Acupuncture points and meridians are not a reality", the review continued, but "merely the product of an ancient Chinese philosophy".
In June 2019, the
World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of h ...
included traditional Chinese medicine in a global diagnostic compendium, but a spokesman said this was "not an endorsement of the scientific validity of any Traditional Medicine practice or the efficacy of any Traditional Medicine intervention."
A 2012 review of
cost-effectiveness research for TCM found that studies had low
levels of evidence
A hierarchy of evidence (or levels of evidence) is a heuristic used to rank the relative strength of results obtained from scientific research. There is broad agreement on the relative strength of large-scale, epidemiological studies. More than 8 ...
, with no beneficial outcomes.
Pharmaceutical research on the potential for creating new drugs from traditional remedies has few successful results.
Proponents suggest that research has so far missed key features of the art of TCM, such as unknown interactions between various ingredients and complex interactive biological systems.
One of the basic tenets of TCM is that the body's
vital energy
Vitalism is a belief that starts from the premise that "living organisms are fundamentally different from non-living entities because they contain some non-physical element or are governed by different principles than are inanimate things." Wher ...
(''ch'i'' or ''
qi'') is circulating through channels called
meridians having branches connected to bodily organs and functions.
The concept of vital energy is pseudoscientific. Concepts of the body and of disease used in TCM reflect its ancient origins and its emphasis on dynamic processes over material structure, similar to
Classical humoral theory
Humorism, the humoral theory, or humoralism, was a system of medicine detailing a supposed makeup and workings of the human body, adopted by Ancient Greek and Roman physicians and philosophers.
Humorism began to fall out of favor in the 1850s ...
.
TCM has also been controversial within China. In 2006, the Chinese philosopher
Zhang Gongyao
Zhang Gongyao ( Chinese: Õ╝ĀÕŖ¤ĶĆĆ; Pinyin: ''Zh─üng G┼Źngy├Āo''; born November 10, 1956) is a Chinese philosopher. He is a professor in Department of Philosophy, Central South University, China. He promoted the abolishment of traditional Chinese m ...
triggered a national debate with an article entitled "Farewell to Traditional Chinese Medicine", arguing that TCM was a pseudoscience that should be abolished in public healthcare and academia. The Chinese government however, took the stance that TCM is a science and continued to encourage its development.
There are concerns over a number of potentially toxic plants, animal parts, and mineral Chinese compounds,
as well as the facilitation of disease. Trafficked and farm-raised animals used in TCM are a source of several fatal
zoonotic diseases
A zoonosis (; plural zoonoses) or zoonotic disease is an infectious disease of humans caused by a pathogen (an infectious agent, such as a bacterium, virus, parasite or prion) that has jumped from a non-human (usually a vertebrate) to a human ...
.
There are additional concerns over the illegal trade and transport of endangered species including rhinoceroses and tigers, and the welfare of specially farmed animals, including bears.
Philosophical background
Traditional Chinese medicine (TCM) is a broad range of medicine practices sharing common concepts which have been developed in China and are based on a tradition of more than 2,000 years, including various forms of
herbal medicine
Herbal medicine (also herbalism) is the study of pharmacognosy and the use of medicinal plants, which are a basis of traditional medicine. With worldwide research into pharmacology, some herbal medicines have been translated into modern remed ...
, acupuncture, massage (), exercise (), and dietary therapy.
[Traditional Chinese Medicine, National Center for Complementary and Integrative Health]
Traditional Chinese Medicine: An Introduction
It is primarily used as a complementary alternative medicine approach.
TCM is widely used in China and it is also used in the West.
Its philosophy is based on
Yinyangism (i.e., the combination of Five Phases theory with YinŌĆōYang theory),
which was later absorbed by
Daoism
Taoism (, ) or Daoism () refers to either a school of philosophical thought (ķüōÕ«Č; ''daojia'') or to a religion (ķüōµĢÖ; ''daojiao''), both of which share ideas and concepts of Chinese origin and emphasize living in harmony with the ''Tao'' ...
.
[Liu, Zheng-Cai (1999)]
"A Study of Daoist Acupuncture & Moxibustion"
Blue Poppy Press, first edition. Philosophical texts influenced TCM, mostly by being grounded in the same theories of ''qi, yin-yang'' and ''wuxing'' and microcosm-macrocosm analogies.

Yin and yang
Yin and yang are ancient Chinese concepts which can be traced back to the
Shang dynasty
The Shang dynasty (), also known as the Yin dynasty (), was a Chinese royal dynasty founded by Tang of Shang (Cheng Tang) that ruled in the Yellow River valley in the second millennium BC, traditionally succeeding the Xia dynasty and ...
[Men, J. & Guo, L. (2010]
"A General Introduction to Traditional Chinese Medicine"
Science Press. (1600ŌĆō1100 BCE). They represent two abstract and complementary aspects that every phenomenon in the universe can be divided into.
Primordial analogies for these aspects are the sun-facing (yang) and the shady (yin) side of a hill.
Two other commonly used representational allegories of yin and yang are water and fire.
In the
yinŌĆōyang theory, detailed attributions are made regarding the yin or yang character of things:
The concept of yin and yang is also applicable to the human body; for example, the upper part of the body and the back are assigned to yang, while the lower part of the body is believed to have the yin character.
Yin and yang characterization also extends to the various body functions, and ŌĆō more importantly ŌĆō to disease symptoms (e.g., cold and heat sensations are assumed to be yin and yang symptoms, respectively).
Thus, yin and yang of the body are seen as phenomena whose lack (or over-abundance) comes with characteristic symptom combinations:
* Yin vacuity (also termed "vacuity-heat"): heat sensations, possible sweating at night, insomnia, dry pharynx, dry mouth, dark urine, and a "fine" and rapid pulse.
[Kaptchuck, Ted J. (2000)]
"The Web That Has No Weaver"
2nd edition. Contemporary Books.
* Yang vacuity ("vacuity-cold"): aversion to cold, cold limbs, bright white complexion, long voidings of clear urine, diarrhea, pale and enlarged tongue, and a slightly weak, slow and fine pulse.
TCM also identifies drugs believed to treat these specific symptom combinations, i.e., to reinforce yin and yang.

Strict rules are identified to apply to the relationships between the Five Phases in terms of sequence, of acting on each other, of counteraction, etc.
All these aspects of Five Phases theory constitute the basis of the
z├Āng-fŪö concept, and thus have great influence regarding the TCM model of the body.
Five Phase theory is also applied in diagnosis and therapy.
Correspondences between the body and the universe have historically not only been seen in terms of the Five Elements, but also of the "Great Numbers" ()
For example, the number of acu-points has at times been seen to be 365, corresponding with the number of days in a year; and the number of main meridiansŌĆō12ŌĆōhas been seen as corresponding with the number of rivers flowing through the
ancient Chinese empire.
[''"There are 365 days in the year, while humans have 365 joints r acu-points.. There are 12 channel rivers across the land, while humans have 12 channel"'', A Study of Daoist Acupuncture & Moxibustion, Cheng-Tsai Liu, Liu Zheng-Cai, Ka Hua, p. 40]
Model of the body

TCM "holds that the body's
vital energy
Vitalism is a belief that starts from the premise that "living organisms are fundamentally different from non-living entities because they contain some non-physical element or are governed by different principles than are inanimate things." Wher ...
(''chi'' or ''qi'') circulates through channels, called ''
meridians'', that have branches connected to bodily organs and functions."
Its view of the human body is only marginally concerned with anatomical structures, but focuses primarily on the body's ''functions''
(such as digestion, breathing, temperature maintenance, etc.):
These functions are aggregated and then associated with a primary functional entity ŌĆō for instance, nourishment of the tissues and maintenance of their moisture are seen as connected functions, and the entity postulated to be responsible for these functions is xi─ø (blood).
These functional entities thus constitute ''concepts'' rather than something with biochemical or anatomical properties.
[Ross, Jeremy (1984)]
"Zang Fu, the organ systems of traditional Chinese medicine"
Elsevier. First edition 1984. pp. 12ŌĆō13. "For example, he term
He or HE may refer to:
Language
* He (pronoun), an English pronoun
* He (kana), the romanization of the Japanese kana ŃüĖ
* He (letter), the fifth letter of many Semitic alphabets
* He (Cyrillic), a letter of the Cyrillic script called ''He'' ...
Xue is used rather than Blood, since the latter implies the blood of Western medicine, with its precise parameters of biochemistry and histology. Although Xue and blood share some common attributes, fundamentally, Xue is a different concept."
The primary functional entities used by traditional Chinese medicine are q├¼, xu─ø, the five z├Āng organs, the six fŪö organs, and the meridians which extend through the organ systems.
These are all theoretically interconnected: each z├Āng organ is paired with a fŪö organ, which are nourished by the blood and concentrate qi for a particular function, with meridians being extensions of those functional systems throughout the body.
Concepts of the body and of disease used in TCM are pseudoscientific, similar to
Mediterranean
The Mediterranean Sea is a sea connected to the Atlantic Ocean, surrounded by the Mediterranean Basin and almost completely enclosed by land: on the north by Western and Southern Europe and Anatolia, on the south by North Africa, and on the e ...
humoral theory
Humorism, the humoral theory, or humoralism, was a system of medicine detailing a supposed makeup and workings of the human body, adopted by Ancient Greek and Roman physicians and philosophers.
Humorism began to fall out of favor in the 1850s ...
.
TCM's model of the body is characterized as full of pseudoscience.
Some practitioners no longer consider yin and yang and the idea of an energy flow to apply.
Scientific investigation has not found any
histological
Histology,
also known as microscopic anatomy or microanatomy, is the branch of biology which studies the microscopic anatomy of biological tissues. Histology is the microscopic counterpart to gross anatomy, which looks at larger structures vis ...
or
physiological
Physiology (; ) is the scientific study of functions and mechanisms in a living system. As a sub-discipline of biology, physiology focuses on how organisms, organ systems, individual organs, cells, and biomolecules carry out the chemical ...
evidence for traditional Chinese concepts such as ''qi'', meridians, and acupuncture points. It is a generally held belief within the acupuncture community that acupuncture points and meridians structures are special conduits for electrical signals but no research has established any consistent anatomical structure or function for either acupuncture points or meridians.
The scientific evidence for the anatomical existence of either meridians or acupuncture points is not compelling.
Stephen Barrett
Stephen Joel Barrett (; born 1933) is an American retired psychiatrist, author, co-founder of the National Council Against Health Fraud (NCAHF), and the webmaster of Quackwatch. He runs a number of websites dealing with quackery and health frau ...
of
Quackwatch
Quackwatch is a United States-based website, self-described as a "network of people" founded by Stephen Barrett, which aims to "combat health-related frauds, myths, fads, fallacies, and misconduct" and to focus on "quackery-related information th ...
writes that, "TCM theory and practice are not based upon the body of knowledge related to health, disease, and health care that has been widely accepted by the scientific community. TCM practitioners disagree among themselves about how to diagnose patients and which treatments should go with which diagnoses. Even if they could agree, the TCM theories are so nebulous that no amount of scientific study will enable TCM to offer rational care."
Qi
TCM distinguishes many kinds of qi ().
In a general sense, qi is something that is defined by five "cardinal functions":
[. "" [Physiological functions of qi: 1.) Function of actuation ... 2.) Function of warming ... 3.) Function of defense ... 4.) Function of containment ... 5.) Function of transformation ...]][as seen at ]
# Actuation () ŌĆō of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels. This includes actuation of the functions of the zang-fu organs and meridians.
# Warming () ŌĆō the body, especially the limbs.
# Defense () ŌĆō against
Exogenous Pathogenic Factors
# Containment () ŌĆō of body fluids, i.e., keeping blood, sweat, urine, semen, etc. from leakage or excessive emission.
# Transformation () ŌĆō of food, drink, and breath into qi,
xue (blood), and
jinye ("fluids"), and/or transformation of all of the latter into each other.
Vacuity of qi will be characterized especially by pale complexion, lassitude of spirit, lack of strength, spontaneous sweating, laziness to speak, non-digestion of food, shortness of breath (especially on exertion), and a pale and enlarged tongue.
Qi is believed to be partially generated from food and drink, and partially from air (by breathing). Another considerable part of it is inherited from the parents and will be consumed in the course of life.
TCM uses special terms for qi running inside of the blood vessels and for qi that is distributed in the skin, muscles, and tissues between them. The former is called y├Łng-q├¼ (); its function is to complement xu├© and its nature has a strong yin aspect (although qi in general is considered to be yang).
The latter is called weì-qì (); its main function is defence and it has pronounced yang nature.
Qi is said to circulate in the meridians. Just as the qi held by each of the zang-fu organs, this is considered to be part of the 'principal' qi () of the body
[" [After yuan-qi is created, it disperses over the whole body, to the zang-fu in the interior, to the skin and the space beneath it on the exterior...] as seen in ] (also called , ''true'' qi, or , ''original'' qi).
["" [1. Yuan-qi is also known as "yuan-qi" and "zh─ōn q├¼", is the body's most fundamental and most important (kind of) qi ...] as seen at ]
Xie
In contrast to the majority of other functional entities, or (, "blood") is correlated with a physical form ŌĆō the red liquid running in the blood vessels.
Its concept is, nevertheless, defined by its functions: nourishing all parts and tissues of the body, safeguarding an adequate degree of moisture, and sustaining and soothing both consciousness and sleep.
Typical symptoms of a lack of (usually termed "blood vacuity" []) are described as: Pale-white or withered-yellow complexion, dizziness, flowery vision, palpitations, insomnia, numbness of the extremities; pale tongue; "fine" pulse.
Jinye
Closely related to xu─ø are the j─½ny├© (, usually translated as "body fluids"), and just like xu─ø they are considered to be yin in nature, and defined first and foremost by the functions of nurturing and moisturizing the different structures of the body.
Their other functions are to harmonize yin and yang, and to help with the secretion of waste products.
[" [3.) Functions of the Jinye: ... 3.3.)Harmonizing yin and yang ... 3.4.)Secretion of waste products ...] As seen at: ]
J─½ny├© are ultimately extracted from food and drink, and constitute the raw material for the production of xu─ø; conversely, xu─ø can also be transformed into j─½ny├©.
Their palpable manifestations are all bodily fluids:
tears
Tears are a clear liquid secreted by the lacrimal glands (tear gland) found in the eyes of all land mammals. Tears are made up of water, electrolytes, proteins, lipids, and mucins that form layers on the surface of eyes. The different types of ...
,
sputum,
saliva
Saliva (commonly referred to as spit) is an extracellular fluid produced and secreted by salivary glands in the mouth. In humans, saliva is around 99% water, plus electrolytes, mucus, white blood cells, epithelial cells (from which DNA can be ...
,
gastric acid
Gastric acid, gastric juice, or stomach acid is a digestive fluid formed within the stomach lining. With a pH between 1 and 3, gastric acid plays a key role in digestion of proteins by activating digestive enzymes, which together break down the ...
,
joint fluid,
sweat
Perspiration, also known as sweating, is the production of fluids secreted by the sweat glands in the skin of mammals.
Two types of sweat glands can be found in humans: eccrine glands and apocrine glands. The eccrine sweat glands are distrib ...
,
urine
Urine is a liquid by-product of metabolism in humans and in many other animals. Urine flows from the kidneys through the ureters to the urinary bladder. Urination results in urine being excretion, excreted from the body through the urethra.
Cel ...
, etc.
["" [The (term) jinye comprises all physiological bodily fluids of the zang-fu and tissues, and physiological secretions, gastric juice, intestinal juice, saliva, joint fluid, etc. Customarily, this also includes metabolic products like urine, sweat, tears, etc.] As seen at: ]
Zang-fu
The z├Āng-fŪö () constitute the centre piece of TCM's systematization of bodily functions. Bearing the names of organs, they are, however, only secondarily tied to (rudimentary) anatomical assumptions (the fŪö a little more, the z├Āng much less).
As they are primarily defined by their functions,
they are not equivalent to the anatomical organs; to highlight this fact, their names are usually capitalized.
The term z├Āng () refers to the five entities considered to be yin in nature ŌĆō
Heart
The heart is a muscular organ in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as carbon dioxide t ...
,
Liver
The liver is a major Organ (anatomy), organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the Protein biosynthesis, synthesis of proteins and biochemicals necessary for ...
,
Spleen
The spleen is an organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter. The word spleen comes . ,
Lung
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of t ...
,
Kidney
The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about in length. They receive blood from the paired renal arteries; blood ...
ŌĆō while fŪö () refers to the six yang organs ŌĆō
Small Intestine
The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the p ...
,
Large Intestine
The large intestine, also known as the large bowel, is the last part of the gastrointestinal tract and of the digestive system in tetrapods. Water is absorbed here and the remaining waste material is stored in the rectum as feces before being r ...
,
Gallbladder
In vertebrates, the gallbladder, also known as the cholecyst, is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although ...
,
Urinary Bladder
The urinary bladder, or simply bladder, is a hollow organ in humans and other vertebrates that stores urine from the kidneys before disposal by urination. In humans the bladder is a distensible organ that sits on the pelvic floor. Urine enters ...
,
Stomach
The stomach is a muscular, hollow organ in the gastrointestinal tract of humans and many other animals, including several invertebrates. The stomach has a dilated structure and functions as a vital organ in the digestive system. The stomach i ...
and
S─ünjia┼Ź.
[by citation from the ]Huangdi Neijing
''Huangdi Neijing'' (), literally the ''Inner Canon of the Yellow Emperor'' or ''Esoteric Scripture of the Yellow Emperor'', is an ancient Chinese medical text or group of texts that has been treated as a fundamental doctrinal source for Chines ...
's Suwen: "" [Within the human body's zang-fu, there's yin and yang; the zang are yin, the fu are yang]. As seen at:
The z├Āng's essential functions consist in production and storage of q├¼ and xu─ø; they are said to regulate digestion, breathing, water metabolism, the musculoskeletal system, the skin, the sense organs, aging, emotional processes, and mental activity, among other structures and processes.
The fŪö organs' main purpose is merely to transmit and digest ()
[" [The Six Fu: gallbladder, stomach, small intestine, large intestine, bladder, sanjiao; "transmit and digest"] as seen at ] substances such as waste and food.
Since their concept was developed on the basis of WŪö X├Łng philosophy, each z├Āng is paired with a fŪö, and each z├Āng-fŪö pair is assigned to one of five elemental qualities (i.e., the Five Elements or Five Phases).
These correspondences are stipulated as:
* Fire () = Heart () and Small Intestine () (and, secondarily, S─ünjia┼Ź [, "Triple Burner"] and Pericardium [])
* Earth () = Spleen () and Stomach ()
* Metal () = Lung () and Large Intestine ()
* Water () = Kidney () and Bladder ()
* Wood () = Liver () and Gallbladder ()
The z├Āng-fŪö are also connected to the
twelve standard meridians ŌĆō each yang meridian is attached to a fŪö organ, and five of the yin meridians are attached to a z├Āng.
As there are only five z├Āng but six yin meridians, the sixth is assigned to the
Pericardium
The pericardium, also called pericardial sac, is a double-walled sac containing the heart and the roots of the great vessels. It has two layers, an outer layer made of strong connective tissue (fibrous pericardium), and an inner layer made of ...
, a peculiar entity almost similar to the Heart z├Āng.
Jing-luo

The meridians (, ) are believed to be channels running from the z├Āng-fŪö in the interior (, ) of the body to the limbs and joints ("the surface"
, transporting qi and xu─Ģ.
[" [The jingluo transport qi and blood through the whole body, connecting the zang-fu with limbs and joints, connecting interior with surface, up with down, inside with outside ...] as seen at ] TCM identifies 12 "regular" and 8 "extraordinary" meridians;
the Chinese terms being (, lit. "the Twelve Vessels") and () respectively.
[" [(3.) The Twelve Vessels ... (4.) The Extraordinary Eight Vessels ...] as seen at ] There's also a number of less customary channels branching from the "regular" meridians.
Gender in traditional medicine
''Fuke ''() is the Chinese term for women's medicine (known as
gynecology
Gynaecology or gynecology (see spelling differences) is the area of medicine that involves the treatment of women's diseases, especially those of the reproductive organs. It is often paired with the field of obstetrics, forming the combined are ...
and
obstetrics
Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period. As a medical specialty, obstetrics is combined with gynecology under the discipline known as obstetrics and gynecology (OB/GYN), which is a surgi ...
in modern medicine). However, there are few or no ancient works on it except for Fu Qing-zhu's ''Fu Qing Zhu Nu Ke'' (Fu Qing-zhu's ''Gynecology'').
In traditional China, as in many other cultures, the health and medicine of female bodies was less understood than that of male bodies. Women's bodies were often secondary to male bodies, since women were thought of as the weaker, sicklier sex.
[Furth, Charlotte. ''A Flourishing Yin: Gender in China's Medical History, 960ŌĆō1665''. Berkeley: University of California Press, 1999]
hdl.handle.net
In clinical encounters, women and men were treated differently. Diagnosing women was not as simple as diagnosing men. First, when a woman fell ill, an appropriate adult man was to call the doctor and remain present during the examination, for the woman could not be left alone with the doctor.
The physician would discuss the female's problems and diagnosis only through the male. However, in certain cases, when a woman dealt with complications of pregnancy or birth, older women assumed the role of the formal authority. Men in these situations would not have much power to interfere.
Second, women were often silent about their issues with doctors due to the societal expectation of female modesty when a male figure was in the room.
Third, patriarchal society also caused doctors to call women and children patients "the anonymous category of family members (''Jia Ren'') or household (''Ju Jia'')"
in their journals. This anonymity and lack of conversation between the doctor and woman patient led to the inquiry diagnosis of the Four Diagnostic Methods
being the most challenging. Doctors used a medical doll known as a
Doctor's lady, on which female patients could indicate the location of their symptoms.
Cheng Maoxian (b. 1581), who practiced medicine in Yangzhou, described the difficulties doctors had with the norm of female modesty. One of his case studies was that of Fan Jisuo's teenage daughter, who could not be diagnosed because she was unwilling to speak about her symptoms, since the illness involved discharge from her intimate areas.
As Cheng describes, there were four standard methods of diagnosis ŌĆō looking, asking, listening and smelling and touching (for pulse-taking). To maintain some form of modesty, women would often stay hidden behind curtains and screens. The doctor was allowed to touch enough of her body to complete his examination, often just the pulse taking. This would lead to situations where the symptoms and the doctor's diagnosis did not agree and the doctor would have to ask to view more of the patient.
These social and cultural beliefs were often barriers to learning more about female health, with women themselves often being the most formidable barrier. Women were often uncomfortable talking about their illnesses, especially in front of the male chaperones that attended medical examinations.
Women would choose to omit certain symptoms as a means of upholding their chastity and honor. One such example is the case in which a teenage girl was unable to be diagnosed because she failed to mention her symptom of vaginal discharge.
Silence was their way of maintaining control in these situations, but it often came at the expense of their health and the advancement of female health and medicine. This silence and control were most obviously seen when the health problem was related to the core of Ming ''fuke'', or the sexual body.
It was often in these diagnostic settings that women would choose silence. In addition, there would be a conflict between patient and doctor on the probability of her diagnosis. For example, a woman who thought herself to be past the point of child-bearing age, might not believe a doctor who diagnoses her as pregnant.
This only resulted in more conflict.
Yin yang and gender
Yin and yang were critical to the understanding of women's bodies, but understood only in conjunction with male bodies.
Yin and yang ruled the body, the body being a microcosm of the universe and the earth. In addition, gender in the body was understood as homologous, the two genders operating in synchronization.
Gender was presumed to influence the movement of energy and a well-trained physician would be expected to read the pulse and be able to identify two dozen or more energy flows.
Yin and yang concepts were applied to the feminine and masculine aspects of all bodies, implying that the differences between men and women begin at the level of this energy flow. According to ''Bequeathed Writings of Master Chu'' the male's yang pulse movement follows an ascending path in "compliance
ith cosmic directionso that the cycle of circulation in the body and the Vital Gate are felt...The female's yin pulse movement follows a defending path against the direction of cosmic influences, so that the nadir and the Gate of Life are felt at the inch position of the left hand".
In sum, classical medicine marked yin and yang as high and low on bodies which in turn would be labeled normal or abnormal and gendered either male or female.
Bodily functions could be categorized through systems, not organs. In many drawings and diagrams, the twelve channels and their visceral systems were organized by yin and yang, an organization that was identical in female and male bodies. Female and male bodies were no different on the plane of yin and yang. Their gendered differences were not acknowledged in diagrams of the human body. Medical texts such as the ''
Yuzuan yizong jinjian'' were filled with illustrations of male bodies or androgynous bodies that did not display gendered characteristics.
[Wu, Yi-Li, and . "The Gendered Medical Iconography of the Golden Mirror, Yuzuan Yizong Jinjian , 1742." In ''Imagining Chinese Medicine'', edited by Lo Vivienne, , Barrett Penelope, Dear David, Di Lu, , Reynolds Lois, Yang Dolly, and , 111ŌĆō32. Leiden; Boston: Brill, 2018. .]
As in other cultures, fertility and menstruation dominate female health concerns.
Since male and female bodies were governed by the same forces, traditional Chinese medicine did not recognize the womb as the place of reproduction. The abdominal cavity presented pathologies that were similar in both men and women, which included tumors, growths, hernias, and swellings of the genitals. The "master system," as Charlotte Furth calls it, is the kidney visceral system, which governed reproductive functions. Therefore, it was not the anatomical structures that allowed for pregnancy, but the difference in processes that allowed for the condition of pregnancy to occur.
Pregnancy
Traditional Chinese medicine's dealings with pregnancy are documented from at least the seventeenth century. According to Charlotte Furth, "a pregnancy (in the seventeenth century) as a known bodily experience emerged
..out of the liminality of menstrual irregularity, as uneasy digestion, and a sense of fullness".
These symptoms were common among other illness as well, so the diagnosis of pregnancy often came late in the term. The ''Canon of the Pulse'', which described the use of pulse in diagnosis, stated that pregnancy was "a condition marked by symptoms of the disorder in one whose pulse is normal" or "where the pulse and symptoms do not agree".
Women were often silent about suspected pregnancy, which led to many men not knowing that their wife or daughter was pregnant until complications arrived. Complications through the misdiagnosis and the woman's reluctance to speak often led to medically induced abortions. Cheng, Furth wrote, "was unapologetic about endangering a fetus when pregnancy risked a mother's well being".
The method of abortion was the ingestion of certain herbs and foods. Disappointment at the loss of the fetus often led to family discord.
Postpartum
If the baby and mother survived the term of the pregnancy, childbirth was then the next step. The tools provided for birth were: towels to catch the blood, a container for the placenta, a pregnancy sash to support the belly, and an infant swaddling wrap.
With these tools, the baby was born, cleaned, and swaddled; however, the mother was then immediately the focus of the doctor to replenish her ''qi.''
In his writings, Cheng places a large amount of emphasis on the Four Diagnostic methods to deal with postpartum issues and instructs all physicians to "not neglect any
f the four methods
F, or f, is the sixth Letter (alphabet), letter in the Latin alphabet, used in the English alphabet, modern English alphabet, the alphabets of other western European languages and others worldwide. Its name in English is English alphabet#Let ...
.
The process of birthing was thought to deplete a woman's blood level and ''qi'' so the most common treatments for postpartum were food (commonly garlic and ginseng), medicine, and rest.
[Cheng Maoxian. ''Yi'an'' (casebook). Dated 1633, but Xue Qinghu (1991) states that the original was printed in 1644] This process was followed up by a month check-in with the physician, a practice known as ''zuo yuezi''.
Infertility
Infertility, not very well understood, posed serious social and cultural repercussions. The seventh-century scholar
Sun Simiao
Sun Simiao (; died 682) was a Chinese physician and writer of the Sui and Tang dynasty. He was titled as China's King of Medicine (, Yaowang) for his significant contributions to Chinese medicine and tremendous care to his patients.
Books
Sun ...
is often quoted: "those who have prescriptions for women's distinctiveness take their differences of pregnancy, childbirth and
nternalbursting injuries as their basis."
Even in contemporary ''fu ke'' placing emphasis on reproductive functions, rather than the entire health of the woman, suggests that the main function of ''fu ke'' is to produce children.
Once again, the kidney visceral system governs the "source ''Qi''", which governs the reproductive systems in both sexes. This source ''Qi'' was thought to "be slowly depleted through sexual activity, menstruation and childbirth."
It was also understood that the depletion of source Qi could result from the movement of an external pathology that moved through the outer visceral systems before causing more permanent damage to the home of source Qi, the kidney system. In addition, the view that only very serious ailments ended in the damage of this system means that those who had trouble with their reproductive systems or fertility were seriously ill.
According to traditional Chinese medical texts, infertility can be summarized into different syndrome types. These were spleen and kidney depletion (yang depletion), liver and kidney depletion (yin depletion), blood depletion, phlegm damp, liver oppression, and damp heat. This is important because, while most other issues were complex in Chinese medical physiology, women's fertility issues were simple. Most syndrome types revolved around menstruation, or lack thereof. The patient was entrusted with recording not only the frequency, but also the "volume, color, consistency, and odor of menstrual flow."
This placed responsibility of symptom recording on the patient, and was compounded by the earlier discussed issue of female chastity and honor. This meant that diagnosing female infertility was difficult, because the only symptoms that were recorded and monitored by the physician were the pulse and color of the tongue.
Concept of disease
In general, disease is perceived as a disharmony (or imbalance) in the functions or interactions of yin, yang, qi, xu─Ģ, z├Āng-fŪö, meridians etc. and/or of the interaction between the human body and the environment.
Therapy is based on which "pattern of disharmony" can be identified.
Thus, "pattern discrimination" is the most important step in TCM diagnosis.
It is also known to be the most difficult aspect of practicing TCM.
To determine which pattern is at hand, practitioners will examine things like the color and shape of the tongue, the relative strength of pulse-points, the smell of the breath, the quality of breathing or the sound of the voice.
["Tongue Diagnosis in Chinese Medicine", Giovanni Maciocia, Eastland Press; Revised edition (June 1995)] For example, depending on tongue and pulse conditions, a TCM practitioner might diagnose bleeding from the mouth and nose as: "Liver fire rushes upwards and scorches the Lung, injuring the blood vessels and giving rise to reckless pouring of blood from the mouth and nose."
He might then go on to prescribe
treatments designed to clear heat or supplement the Lung.
Disease entities
In TCM, a disease has two aspects: "b├¼ng" and "zh├©ng".
[Clavey, Steven (1995)]
"Fluid physiology and pathology in traditional Chinese medicine"
Elsevier. 2nd edition, 2003. The former is often translated as "disease entity",
"disease category",
"illness",
or simply "diagnosis".
The latter, and more important one, is usually translated as "pattern"
(or sometimes also as "syndrome"
). For example, the disease entity of a common cold might present with a pattern of
wind-cold in one person, and with the pattern of
wind-heat in another.
From a scientific point of view, most of the disease entities () listed by TCM constitute symptoms.
Examples include headache, cough, abdominal pain, constipation etc.
Since therapy will not be chosen according to the disease entity but according to the pattern, two people with the same disease entity but different patterns will receive different therapy.
Vice versa, people with similar patterns might receive similar therapy even if their disease entities are different. This is called ''yì bìng tóng zhì, tóng bìng yì zhì'' ().
Patterns
In TCM, "pattern" () refers to a "pattern of disharmony" or "functional disturbance" within the functional entities of which the TCM model of the body is composed.
There are disharmony patterns of qi, xu─ø, the body fluids, the z├Āng-fŪö, and the
meridians.
They are ultimately defined by their symptoms and signs (i.e., for example, pulse and tongue findings).
In clinical practice, the identified pattern usually involves a combination of affected entities
[Flaws, Bob (1990)]
"Sticking to the Point"
Blue Poppy Press. 10th Printing, 2007. (compare with
typical examples of patterns). The concrete pattern identified should account for ''all'' the symptoms a person has.
[Flaws, B. & Finney, D. (1996)]
"A handbook of TCM patterns & their treatments"
Blue Poppy Press. 6th Printing 2007.
Six Excesses
The Six Excesses (,
sometimes also translated as "Pathogenic Factors",
[ p. 159] or "Six Pernicious Influences";
with the alternative term of , ŌĆō "Six Evils" or "Six Devils")
are allegorical terms used to describe disharmony patterns displaying certain typical symptoms.
These symptoms resemble the effects of six climatic factors.
In the allegory, these symptoms can occur because one or more of those climatic factors (called , "the six qi")
were able to invade the body surface and to proceed to the interior.
This is sometimes used to draw causal relationships (i.e., prior exposure to wind/cold/etc. is identified as the cause of a disease),
while other authors explicitly deny a direct cause-effect relationship between weather conditions and disease,
pointing out that the Six Excesses are primarily descriptions of a certain combination of symptoms
translated into a pattern of disharmony.
It is undisputed, though, that the Six Excesses can manifest inside the body without an external cause.
In this case, they might be denoted "internal", e.g., "internal wind"
or "internal fire (or heat)".
The Six Excesses and their characteristic clinical signs are:
# Wind (): rapid onset of symptoms, wandering location of symptoms, itching, nasal congestion, "floating" pulse;
tremor, paralysis, convulsion.
# Cold (): cold sensations, aversion to cold, relief of symptoms by warmth, watery/clear excreta, severe pain, abdominal pain, contracture/hypertonicity of muscles, (slimy) white tongue fur, "deep"/"hidden" or "string-like" pulse,
or slow pulse.
# Fire/Heat (): aversion to heat, high fever, thirst, concentrated urine, red face, red tongue, yellow tongue fur, rapid pulse.
(Fire and heat are basically seen to be the same)
# Dampness (): sensation of heaviness, sensation of fullness, symptoms of Spleen dysfunction, greasy tongue fur, "slippery" pulse.
# Dryness (): dry cough, dry mouth, dry throat, dry lips, nosebleeds, dry skin, dry stools.
# Summerheat (): either heat or mixed damp-heat symptoms.
Six-Excesses-patterns can consist of only one or a combination of Excesses (e.g., wind-cold, wind-damp-heat).
They can also transform from one into another.
Typical examples of patterns
For each of the functional entities (qi, xu─Ģ, z├Āng-fŪö, meridians etc.), typical disharmony patterns are recognized; for example: qi vacuity and qi stagnation in the case of qi;
blood vacuity, blood stasis, and blood heat in the case of xu─Ģ;
Spleen qi vacuity, Spleen yang vacuity, Spleen qi vacuity with down-bearing qi, Spleen qi vacuity with lack of blood containment, cold-damp invasion of the Spleen, damp-heat invasion of Spleen and Stomach in case of the Spleen z├Āng;
wind/cold/damp invasion in the case of the meridians.
TCM gives detailed prescriptions of these patterns regarding their typical symptoms, mostly including characteristic tongue and/or pulse findings.
For example:
* "Upflaming Liver fire" (): Headache, red face, reddened eyes, dry mouth, nosebleeds, constipation, dry or hard stools, profuse menstruation, sudden
tinnitus
Tinnitus is the perception of sound when no corresponding external sound is present. Nearly everyone experiences a faint "normal tinnitus" in a completely quiet room; but it is of concern only if it is bothersome, interferes with normal hearin ...
or deafness, vomiting of sour or bitter fluids, expectoration of blood,
irascibility, impatience; red tongue with dry yellow fur; slippery and string-like pulse.
Eight principles of diagnosis
The process of determining which actual pattern is on hand is called (, usually translated as "pattern diagnosis",
"pattern identification"
or "pattern discrimination"
). Generally, the first and most important step in pattern diagnosis is an evaluation of the present signs and symptoms on the basis of the "Eight Principles" ().
These eight principles refer to four pairs of fundamental qualities of a disease: exterior/interior, heat/cold, vacuity/repletion, and yin/yang.
Out of these, heat/cold and vacuity/repletion have the biggest clinical importance.
The yin/yang quality, on the other side, has the smallest importance and is somewhat seen aside from the other three pairs, since it merely presents a general and vague conclusion regarding what other qualities are found.
In detail, the Eight Principles refer to the following:
* ''Yin and yang'' are universal aspects all things can be classified under, this includes diseases in general as well as the Eight Principles' first three couples.
For example, cold is identified to be a yin aspect, while heat is attributed to yang.
Since descriptions of patterns in terms of yin and yang lack complexity and clinical practicality, though, patterns are usually not labeled this way anymore.
Exceptions are vacuity-cold and repletion-heat patterns, who are sometimes referred to as "yin patterns" and "yang patterns" respectively.
* ''Exterior'' () refers to a disease manifesting in the superficial layers of the body ŌĆō skin, hair, flesh, and meridians.
It is characterized by aversion to cold and/or wind, headache, muscle ache, mild fever, a "floating" pulse, and a normal tongue appearance.
* ''Interior'' () refers to disease manifestation in the z├Āng-fŪö, or (in a wider sense) to any disease that can not be counted as exterior.
There are no generalized characteristic symptoms of interior patterns, since they'll be determined by the affected z├Āng or fŪö entity.
* ''Cold'' () is generally characterized by aversion to cold, absence of thirst, and a white tongue fur.
More detailed characterization depends on whether cold is coupled with vacuity or repletion.
* ''Heat'' () is characterized by an absence of aversion to cold, a red and painful throat, a dry tongue fur and a rapid and floating pulse if it falls together with an exterior pattern.
In all other cases, symptoms depend on whether heat is coupled with vacuity or repletion.
* ''Deficiency'' (), can be further differentiated into deficiency of
qi, xu─ø,
yin and yang
Yin and yang ( and ) is a Chinese philosophy, Chinese philosophical concept that describes opposite but interconnected forces. In Chinese cosmology, the universe creates itself out of a primary chaos of material energy, organized into the c ...
, with all their respective characteristic symptoms.
Yin deficiency can also cause "empty-heat".
* ''Excess'' () generally refers to any disease that can't be identified as a deficient pattern, and usually indicates the presence of one of the Six Excesses,
or a pattern of stagnation (of qi, xu─ø, etc.).
[Tierra & Tierra 1998, p. 108] In a concurrent exterior pattern, excess is characterized by the absence of sweating.
After the fundamental nature of a disease in terms of the Eight Principles is determined, the investigation focuses on more specific aspects.
By evaluating the present signs and symptoms against the background of typical disharmony patterns of the various entities, evidence is collected whether or how specific entities are affected.
This evaluation can be done
# in respect of the meridians ()
# in respect of qi ()
# in respect of xu├© ()
# in respect of the body fluids ()
# in respect of the z├Āng-fŪö ()
ŌĆō very similar to this, though less specific, is disharmony pattern description in terms of the Five Elements []
)
There are also three special pattern diagnosis systems used in case of febrile and infectious diseases only ("Six Channel system" or "six division pattern" []; "Wei Qi Ying Xue system" or "four division pattern" []; "San Jiao system" or "three burners pattern" []).
Considerations of disease causes
Although TCM and its concept of disease do not strongly differentiate between cause and effect,
[Ross, Jeremy (1984]
"Zang Fu, the organ systems of traditional Chinese medicine"
Elsevier. First edition 1984. pattern discrimination can include considerations regarding the disease cause; this is called (, "disease-cause pattern discrimination").
There are three fundamental categories of disease causes () recognized:
# external causes: these include the Six Excesses and "Pestilential Qi".
# internal causes: the "Seven Affects" (,
sometimes also translated as "Seven Emotions"
) ŌĆō joy, anger, brooding, sorrow, fear, fright and grief.
These are believed to be able to cause damage to the functions of the z├Āng-f├║, especially of the Liver.
# non-external-non-internal causes: dietary irregularities (especially: too much raw, cold, spicy, fatty or sweet food; voracious eating; too much alcohol),
fatigue, sexual intemperance, trauma, and parasites ().
Diagnostics
In TCM, there are five major diagnostic methods: inspection, auscultation, olfaction, inquiry, and palpation.
These are grouped into what is known as the "Four pillars" of diagnosis, which are Inspection, Auscultation/ Olfaction, Inquiry, and Palpation ().
* Inspection focuses on the face and particularly on the tongue, including analysis of the tongue size, shape, tension, color and coating, and the absence or presence of teeth marks around the edge.
* Auscultation refers to listening for particular sounds (such as wheezing).
* Olfaction refers to attending to body odor.
* Inquiry focuses on the "seven inquiries", which involve asking the person about the regularity, severity, or other characteristics of: chills, fever, perspiration, appetite, thirst, taste, defecation, urination, pain, sleep,
menses
Menstruation (also known as a period, among other colloquial terms) is the regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina. The menstrual cycle is characterized by the rise and fall of horm ...
,
leukorrhea
Leukorrhea or (leucorrhoea British English), also known as fluor albus, is a thick, whitish, yellowish or greenish vaginal discharge.
It has also been referred to as "the whites".
There are many causes of leukorrhea, the usual one being estrogen ...
.
* Palpation which includes feeling the body for tender
A-shi points, and the palpation of the wrist pulses as well as various other pulses, and palpation of the abdomen.
Tongue and pulse
Examination of the tongue and the pulse are among the principal diagnostic methods in TCM. Details of the tongue, including shape, size, color, texture, cracks, teeth marks, as well as tongue coating are all considered as part of
tongue diagnosis. Various regions of the tongue's surface are believed to correspond to the z├Āng-f┼Ł organs. For example, redness on the tip of the tongue might indicate heat in the Heart, while redness on the sides of the tongue might indicate heat in the Liver.
Pulse palpation involves measuring the pulse both at a superficial and at a deep level at three different locations on the
radial artery
In human anatomy, the radial artery is the main artery of the lateral aspect of the forearm.
Structure
The radial artery arises from the bifurcation of the brachial artery in the antecubital fossa. It runs distally on the anterior part of the f ...
(''Cun, Guan, Chi'', located two fingerbreadths from the wrist crease, one fingerbreadth from the wrist crease, and right at the wrist crease, respectively, usually palpated with the index, middle and ring finger) of each arm, for a total of twelve pulses, all of which are thought to correspond with certain z├Āng-f┼Ł. The pulse is examined for several characteristics including rhythm, strength and volume, and described with qualities like "floating, slippery, bolstering-like, feeble, thready and quick"; each of these qualities indicates certain
disease patterns. Learning TCM pulse diagnosis can take several years.
Herbal medicine


The term "herbal medicine" is somewhat misleading in that, while plant elements are by far the most commonly used substances in TCM, other, non-botanic substances are used as well: animal, human, and mineral products are also used.
Thus, the term "medicinal" (instead of herb) may be used,
although there is no scientific evidence that any of these compounds have medicinal effects.
Raw materials
There are roughly 13,000 compounds used in China and over 100,000 TCM recipes recorded in the ancient literature.
Plant elements and extracts are by far the most common elements used.
[Foster, S. & Yue, C. (1992)]
"Herbal emissaries: bringing Chinese herbs to the West"
. Healing Arts Press. In the classic ''Handbook of Traditional Drugs'' from 1941, 517 drugs were listed ŌĆō out of these, 45 were animal parts, and 30 were minerals.
Animal substances
Some animal parts used can be considered rather strange such as cow gallstones,
hornet nests,
es,
and
scorpion
Scorpions are predatory arachnids of the order Scorpiones. They have eight legs, and are easily recognized by a pair of grasping pincers and a narrow, segmented tail, often carried in a characteristic forward curve over the back and always end ...
.
Other examples of animal parts include horn of the antelope or buffalo, deer antlers, testicles and
penis bone of the dog, and snake bile.
Some TCM textbooks still recommend preparations containing animal tissues, but there has been little research to justify the claimed clinical efficacy of many TCM animal products.
Some compounds can include the parts of endangered species, including tiger bones
and
rhinoceros horn
A rhinoceros (; ; ), commonly abbreviated to rhino, is a member of any of the five extant species (or numerous extinct species) of odd-toed ungulates in the family Rhinocerotidae. (It can also refer to a member of any of the extinct species o ...
[''Facts about traditional Chinese medicine (TCM): rhinoceros horn'', Encyclop├”dia Britannica]
Facts about traditional Chinese medicine (TCM): rhinoceros horn, as discussed in rhinoceros (mammal): ŌĆō Britannica Online Encyclopedia
which is used for many ailments (though not as an aphrodisiac as is commonly misunderstood in the West).
The black market in rhinoceros horns (driven not just by TCM but also unrelated status-seeking) has reduced the world's rhino population by more than 90 percent over the past 40 years.
Concerns have also arisen over the use of
pangolin
Pangolins, sometimes known as scaly anteaters, are mammals of the order Pholidota (, from Ancient Greek ŽĢ╬┐╬╗╬╣╬┤ŽēŽäŽīŽé ŌĆō "clad in scales"). The one extant family, the Manidae, has three genera: '' Manis'', '' Phataginus'', and '' Smut ...
scales,
turtle
plastron,
seahorses,
and the
gill plates of
mobula
''Mobula'' is a genus of rays in the family Mobulidae that is found worldwide in tropical and warm, temperate seas. Some authorities consider this to be a subfamily of the Myliobatidae (eagle rays). Their appearance is similar to that of manta r ...
and
manta ray
Manta rays are large rays belonging to the genus ''Mobula'' (formerly its own genus ''Manta''). The larger species, '' M. birostris'', reaches in width, while the smaller, '' M. alfredi'', reaches . Both have triangular Pectoral fin#AnchPect ...
s.
Poachers hunt restricted or endangered species to supply the black market with TCM products.
There is no scientific evidence of efficacy for tiger medicines.
Concern over China considering to legalize the trade in tiger parts prompted the 171-nation
Convention on International Trade in Endangered Species
CITES (shorter name for the Convention on International Trade in Endangered Species of Wild Fauna and Flora, also known as the Washington Convention) is a multilateral treaty to protect endangered plants and animals from the threats of interna ...
(CITES) to endorse a decision opposing the resurgence of trade in tigers.
Fewer than 30,000
saiga antelope
The saiga antelope (, ''Saiga tatarica''), or saiga, is a critically endangered antelope which during antiquity inhabited a vast area of the Eurasian steppe spanning the foothills of the Carpathian Mountains in the northwest and Caucasus in t ...
s remain, which are exported to China for use in traditional fever therapies.
Organized gangs illegally export the horn of the antelopes to China.
The pressures on
seahorse
A seahorse (also written ''sea-horse'' and ''sea horse'') is any of 46 species of small marine fish in the genus ''Hippocampus''. "Hippocampus" comes from the Ancient Greek (), itself from () meaning "horse" and () meaning "sea monster" or " ...
s (''Hippocampus'' spp.) used in traditional medicine is enormous; tens of millions of animals are unsustainably caught annually.
Many species of
syngnathid are currently part of the
IUCN Red List of Threatened Species
The International Union for Conservation of Nature (IUCN) Red List of Threatened Species, also known as the IUCN Red List or Red Data Book, founded in 1964, is the world's most comprehensive inventory of the global conservation status of biologi ...
or national equivalents.
Since TCM recognizes
bear bile
Bears are carnivoran mammals of the family Ursidae. They are classified as caniforms, or doglike carnivorans. Although only eight species of bears are extant, they are widespread, appearing in a wide variety of habitats throughout the Nor ...
as a treatment compound, more than 12,000
asiatic black bears
The Asian black bear (''Ursus thibetanus''), also known as the Asiatic black bear, moon bear and white-chested bear, is a medium-sized bear species native to Asia that is largely adapted to an arboreal lifestyle. It lives in the Himalayas, sout ...
are held in bear farms. The bile is extracted through a permanent hole in the abdomen leading to the
gall bladder
In vertebrates, the gallbladder, also known as the cholecyst, is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although ...
, which can cause severe pain. This can lead to bears trying to kill themselves. As of 2012, approximately 10,000 bears are farmed in China for their bile.
This practice has spurred public outcry across the country.
The bile is collected from live bears via a surgical procedure.
As of March 2020 bear bile as ingredient of ''Tan Re Qing'' injection remains on the list of remedies recommended for treatment of "severe cases" of COVID-19 by National Health Commission of China and the National Administration of Traditional Chinese Medicine.
The
deer penis
In traditional Chinese medicine, a deer penis (; Vietnamese: ''Lß╗Öc p├Łn'') is said to have important therapeutic properties.
Purported properties
In Angang, Taiwan, women are reported to consume deer penis during pregnancy as it is said to ha ...
is believed to have therapeutic benefits according to traditional Chinese medicine. Tiger parts from poached animals include
tiger penis
In traditional Chinese medicine, a tiger penis ( Vietnamese: ''P├Łn hß╗Ģ''; ) is said to have important therapeutic properties. However, there is no scientific proof that tiger penis can be used to treat any medical disorder. The demand for tiger ...
, believed to improve virility, and tiger eyes.
The illegal trade for tiger parts in China has driven the species to near-extinction because of its popularity in traditional medicine.
Laws protecting even
critically endangered species such as the
Sumatran tiger fail to stop the display and sale of these items in open markets.
Shark fin soup
Shark fin soup is a traditional soup or stewed dish served in parts of China, Taiwan, and Southeast Asia. The shark fins provide texture, while the taste comes from the other soup ingredients. It is commonly served at special occasions such as ...
is traditionally regarded in Chinese medicine as beneficial for health in East Asia, and its status as an elite dish has led to huge demand with the increase of affluence in China, devastating shark populations.
The shark fins have been a part of traditional Chinese medicine for centuries.
Shark finning is banned in many countries, but the trade is thriving in Hong Kong and China, where the fins are part of shark fin soup, a dish considered a delicacy, and used in some types of traditional Chinese medicine.
The
tortoise
Tortoises () are reptiles of the family Testudinidae of the order Testudines (Latin: ''tortoise''). Like other turtles, tortoises have a turtle shell, shell to protect from predation and other threats. The shell in tortoises is generally hard, ...
(
freshwater turtle
Turtles are an order of reptiles known as Testudines, characterized by a special shell developed mainly from their ribs. Modern turtles are divided into two major groups, the Pleurodira (side necked turtles) and Cryptodira (hidden necked tu ...
, ''guiban'') and turtle (
Chinese softshell turtle
The Chinese softshell turtle (''Pelodiscus sinensis'') is a species of softshell turtle that is native to China (Inner Mongolia to Guangxi, including Hong Kong) and Taiwan, with records of escapeesŌĆösome of which have established introduced po ...
, ''biejia'') species used in traditional Chinese medicine are raised on farms, while restrictions are made on the accumulation and export of other endangered species.
However, issues concerning the
overexploitation
Overexploitation, also called overharvesting, refers to harvesting a renewable resource to the point of diminishing returns. Continued overexploitation can lead to the destruction of the resource, as it will be unable to replenish. The term app ...
of Asian turtles in China have not been completely solved.
Australian scientists have developed methods to identify medicines containing DNA traces of endangered species.
[DNA may weed out toxic Chinese medicine](_blank)
ŌĆō By Carolyn Herbert ŌĆō Australian Broadcasting Corporation ŌĆō Retrieved 14 April 2012. Finally, although not an endangered species, sharp rises in exports of donkeys and donkey hide from Africa to China to make the traditional remedy ''ejiao'' have prompted export restrictions by some African countries.
Human body parts

Traditional Chinese medicine also includes some human parts: the classic
Materia medica (
Bencao Gangmu
The ''Bencao gangmu'', known in English as the ''Compendium of Materia Medica'' or ''Great Pharmacopoeia'', is an encyclopedic gathering of medicine, natural history, and Chinese herbology compiled and edited by Li Shizhen and published in the ...
) describes (also criticizes) the use of 35 human body parts and
excreta
Excretion is a process in which metabolic waste
is eliminated from an organism. In vertebrates this is primarily carried out by the lungs, kidneys, and skin. This is in contrast with secretion, where the substance may have specific tasks after lea ...
in medicines, including bones, fingernail, hairs, dandruff, earwax, impurities on the teeth, feces, urine, sweat, organs, but most are no longer in use.
[THE HUMAN BODY AS A NEW COMMODITY, Tsuyoshi Awaya, The Review of Tokuyama, June 1999][Commodifying bodies, Nancy Scheper-Hughes, Loïc J. D. Wacquant, 2002]
Human placenta has been used an ingredient in certain traditional Chinese medicines,
including using dried human placenta, known as "Ziheche", to treat infertility, impotence and other conditions.
The consumption of the human placenta is a potential source of infection.
Traditional categorization
The traditional categorizations and classifications that can still be found today are:
* The classification according to the
Four Natures (): hot, warm, cool, or cold (or, neutral in terms of temperature)
and hot and warm herbs are used to treat
cold
Cold is the presence of low temperature, especially in the atmosphere. In common usage, cold is often a subjective perception. A lower bound to temperature is absolute zero, defined as 0.00K on the Kelvin scale, an absolute thermodynamic ...
diseases, while cool and cold herbs are used to treat heat diseases.
* The classification according to the
Five Flavors, (, sometimes also translated as Five Tastes): acrid, sweet, bitter, sour, and salty.
Substances may also have more than one flavor, or none (i.e., a "bland" flavor).
Each of the Five Flavors corresponds to one of z├Āng organs, which in turn corresponds to one of the
Five Phases
(; Japanese: (); Korean: (); Vietnamese: ''ng┼® h├Ānh'' (õ║öĶĪī)), usually translated as Five Phases or Five Agents, is a fivefold conceptual scheme that many traditional Chinese fields used to explain a wide array of phenomena, from cosmi ...
.
A flavor implies certain properties and therapeutic actions of a substance; e.g., saltiness drains downward and softens hard masses, while sweetness is supplementing, harmonizing, and moistening.
* The classification according to the meridian ŌĆō more precisely, the z├Āng-fu organ including its associated meridian ŌĆō which can be expected to be primarily affected by a given compound.
* The categorization according to the specific function mainly include: exterior-releasing
or exterior-resolving,
heat-clearing,
downward-draining,
or precipitating
wind-damp-dispelling,
dampness-transforming,
promoting the movement of water and percolating dampness
or dampness-percolating,
interior-warming,
qi-regulating
or qi-rectifying,
dispersing food accumulation
or food-dispersing,
worm-expelling,
stopping bleeding
or blood-
stanching,
quickening the Blood and dispelling
stasis or blood-quickening,
transforming phlegm, stopping coughing and calming wheezing
or phlegm-transforming and cough- and panting-suppressing,
Spirit-quieting,
calming the liver and expelling wind
or liver-calming and wind-extinguishing
orifice-opening
supplementing
which includes qi-supplementing, blood-nourishing, yin-enriching, and yang-fortifying,
astriction-promoting
or securing and astringing,
vomiting-inducing,
and substances for external application.
[Xu, L. & Wang, W. (2002]
"Chinese materia medica: combinations and applications"
Donica Publishing Ltd. 1st edition.
Efficacy
there were not enough good-quality trials of herbal therapies to allow their effectiveness to be determined.
A high percentage of relevant studies on traditional Chinese medicine are in Chinese databases. Fifty percent of systematic reviews on TCM did not search Chinese databases, which could lead to a bias in the results.
Many systematic reviews of TCM interventions published in Chinese journals are incomplete, some contained errors or were misleading.
The herbs recommended by traditional Chinese practitioners in the US are unregulated.
* A 2013 review found the data too weak to support use of Chinese herbal medicine (CHM) for
benign prostatic hyperplasia
Benign prostatic hyperplasia (BPH), also called prostate enlargement, is a noncancerous increase in size of the prostate gland. Symptoms may include frequent urination, trouble starting to urinate, weak stream, inability to urinate, or loss o ...
.
* A 2013 review found the research on the benefit and safety of CHM for idiopathic sudden sensorineural hearing loss is of poor quality and cannot be relied upon to support their use.
* A 2013
Cochrane review
Cochrane (previously known as the Cochrane Collaboration) is a British international charitable organisation formed to organise medical research findings to facilitate evidence-based choices about health interventions involving health profes ...
found inconclusive evidence that CHM reduces the severity of eczema.
* The traditional medicine ginger, which has shown anti-inflammatory properties in laboratory experiments, has been used to treat
rheumatism
Rheumatism or rheumatic disorders are conditions causing chronic, often intermittent pain affecting the joints or connective tissue. Rheumatism does not designate any specific disorder, but covers at least 200 different conditions, including art ...
, headache and digestive and respiratory issues, though there is no firm evidence supporting these uses.
* A 2012 Cochrane review found no difference in
mortality rate
Mortality rate, or death rate, is a measure of the number of deaths (in general, or due to a specific cause) in a particular population, scaled to the size of that population, per unit of time. Mortality rate is typically expressed in units of de ...
among 640 SARS patients when Chinese herbs were used alongside Western medicine versus Western medicine exclusively, although they concluded some herbs may have improved symptoms and decreased corticosteroid doses.
* A 2012 Cochrane review found insufficient evidence to support the use of TCM for people with adhesive small bowel obstruction.
* A 2011 review found low quality evidence that suggests CHM improves the symptoms of Sjogren's syndrome.
*A 2011 Cochrane review found inconclusive evidence to support the use of TCM herbal medicines for treatment of
hypercholesterolemia
Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood. It is a form of hyperlipidemia (high levels of lipids in the blood), hyperlipoproteinemia (high levels of lipoproteins in the blood), ...
.
* A 2011 Cochrane review did not find improvement in fasting
C-peptide
The connecting peptide, or C-peptide, is a short 31-amino-acid polypeptide that connects insulin's A-chain to its B-chain in the proinsulin molecule. In the context of diabetes or hypoglycemia, a measurement of C-peptide blood serum levels can ...
when compared to
insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism o ...
treatment for
latent autoimmune diabetes
Slowly evolving immune-mediated diabetes, or latent autoimmune diabetes in adults (LADA), is a form of diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level ( hyperglyce ...
in adults after 3 months. It is important to highlight that the studies available to be included in this review presented considerable flaws in quality and design.
* A 2010 review found TCM seems to be effective for the treatment of fibromyalgia but the findings were of insufficient methodological rigor.
* A 2008 Cochrane review found promising evidence for the use of Chinese herbal medicine in relieving
painful menstruation
Dysmenorrhea, also known as period pain, painful periods or menstrual cramps, is pain during menstruation. Its usual onset occurs around the time that menstruation begins. Symptoms typically last less than three days. The pain is usually in the ...
, but the trials assessed were of such low methodological quality that no conclusion could be drawn about the remedies' suitability as a recommendable treatment option.
*
Turmeric
Turmeric () is a flowering plant, ''Curcuma longa'' (), of the ginger family, Zingiberaceae, the rhizomes of which are used in cooking. The plant is a perennial, rhizomatous, herbaceous plant native to the Indian subcontinent and Southeast Asi ...
has been used in traditional Chinese medicine for centuries to treat various conditions.
This includes jaundice and hepatic disorders, rheumatism, anorexia, diabetic wounds, and menstrual complications.
Most of its effects have been attributed to
curcumin
Curcumin is a bright yellow chemical produced by plants of the ''Curcuma longa'' species. It is the principal curcuminoid of turmeric (''Curcuma longa''), a member of the ginger family, Zingiberaceae. It is sold as a herbal supplement, cosmetic ...
.
Research that curcumin shows strong anti-inflammatory and antioxidant activities have instigated mechanism of action studies on the possibility for cancer and inflammatory diseases prevention and treatment.
It also exhibits
immunomodulatory
Immunotherapy or biological therapy is the treatment of disease by activating or suppressing the immune system. Immunotherapies designed to elicit or amplify an immune response are classified as ''activation immunotherapies,'' while immunotherap ...
effects.
* A 2005 Cochrane review found insufficient evidence for the use of CHM in HIV-infected people and people with
AIDS
Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual m ...
.
* A 2010 Cochrane review found insufficient evidence to support the use of Traditional Chinese Herbal Products (THCP) in the treatment of
angina.
* A 2010 Cochrane review found no evidence supporting the use of TCHM for stopping bleeding from
haemorrhoids
Hemorrhoids (or haemorrhoids), also known as piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term ''he ...
. There was some weak evidence of pain relief.
Drug research
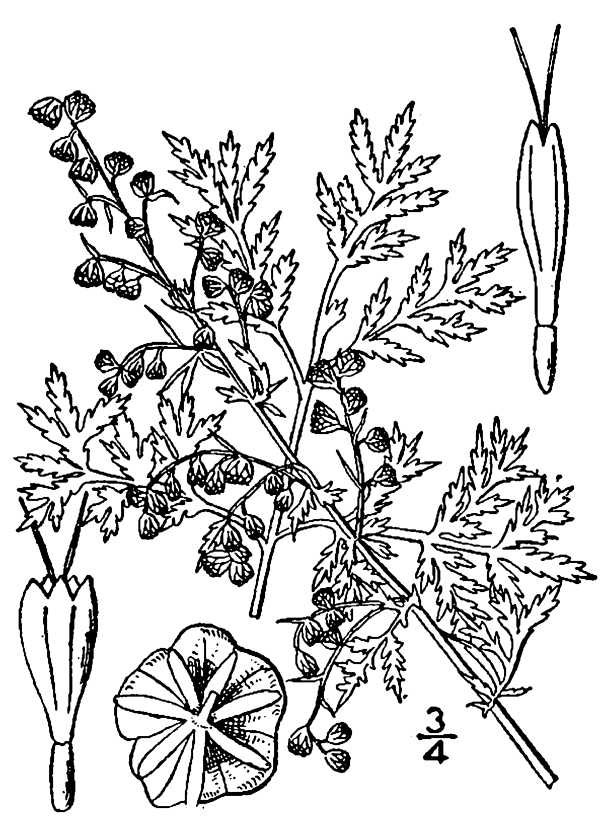
With an eye to the enormous Chinese market, pharmaceutical companies have explored creating new drugs from traditional remedies. The journal ''Nature'' commented that "claims made on behalf of an uncharted body of knowledge should be treated with the customary skepticism that is the bedrock of both science and medicine."
There had been success in the 1970s, however, with the development of the antimalarial drug
artemisinin
Artemisinin () and its semisynthetic derivatives are a group of drugs used in the treatment of malaria due to '' Plasmodium falciparum''. It was discovered in 1972 by Tu Youyou, who shared the 2015 Nobel Prize in Physiology or Medicine for her ...
, which is a processed extract of ''
Artemisia annua
''Artemisia annua'', also known as sweet wormwood, sweet annie, sweet sagewort, annual mugwort or annual wormwood (), is a common type of wormwood native to temperate Asia, but naturalized in many countries including scattered parts of North Am ...
'', a herb traditionally used as a fever treatment.
''Artemisia annua'' has been used by Chinese herbalists in traditional Chinese medicines for 2,000 years. In 1596, Li Shizhen recommended tea made from qinghao specifically to treat malaria symptoms in his ''
Compendium of Materia Medica
The ''Bencao gangmu'', known in English as the ''Compendium of Materia Medica'' or ''Great Pharmacopoeia'', is an encyclopedic gathering of medicine, natural history, and Chinese herbology compiled and edited by Li Shizhen and published in the ...
''. Researcher
Tu Youyou
Tu Youyou (; born 30 December 1930) is a Chinese pharmaceutical chemist and malariologist. She discovered artemisinin (also known as , ) and dihydroartemisinin, used to treat malaria, a breakthrough in twentieth-century tropical medicine, sa ...
discovered that a low-temperature extraction process could isolate an effective antimalarial substance from the plant.
Tu says she was influenced by a traditional Chinese herbal medicine source, ''The Handbook of Prescriptions for Emergency Treatments'', written in 340 by
Ge Hong
Ge Hong (; b. 283 ŌĆō d. 343 or 364), courtesy name Zhichuan (ń©ÜÕĘØ), was a Chinese linguist, Taoist practitioner, philosopher, physician, politician, and writer during the Eastern Jin dynasty. He was the author of '' Essays on Chinese Characte ...
, which states that this herb should be steeped in cold water.
The extracted substance, once subject to detoxification and purification processes, is a usable antimalarial drug
ŌĆō a 2012 review found that artemisinin-based remedies were the most effective drugs for the treatment of malaria.
For her work on malaria, Tu received the 2015
Nobel Prize in Physiology or Medicine
The Nobel Prize in Physiology or Medicine is awarded yearly by the Nobel Assembly at the Karolinska Institute for outstanding discoveries in physiology or medicine. The Nobel Prize is not a single prize, but five separate prizes that, accord ...
. Despite global efforts in combating malaria, it remains a large burden for the population.
Although
WHO
Who or WHO may refer to:
* Who (pronoun), an interrogative or relative pronoun
* Who?, one of the Five Ws in journalism
* World Health Organization
Arts and entertainment Fictional characters
* Who, a creature in the Dr. Seuss book '' Horton He ...
recommends artemisinin-based remedies for treating uncomplicated malaria, but resistance to the drug can no longer be ignored.
Also in the 1970s Chinese researcher
Zhang TingDong
Zhang Tingdong (; born on November 8, 1932) is a Chinese medical scientist, pharmaceutical chemist, and educator at Harbin Medical University, 1st affiliated Hospital, and is best known for discovering of using arsenic trioxide to treat leukemia, ...
and colleagues investigated the potential use of the traditionally used substance
arsenic trioxide
Arsenic trioxide, sold under the brand name Trisenox among others, is an inorganic compound and medication. As an industrial chemical, whose major uses include in the manufacture of wood preservatives, pesticides, and glass. As a medication, i ...
to treat
acute promyelocytic leukemia (APL).
Building on his work, research both in China and the West eventually led to the development of the drug
Trisenox
Arsenic trioxide, sold under the brand name Trisenox among others, is an inorganic compound and medication. As an industrial chemical, whose major uses include in the manufacture of wood preservatives, pesticides, and glass. As a medication, it ...
, which was approved for leukemia treatment by the FDA in 2000.
Huperzine A
Huperzine A is a naturally occurring sesquiterpene alkaloid compound found in the firmoss ''Huperzia serrata'' and in varying quantities in other food ''Huperzia'' species, including ''H. elmeri'', ''H. carinat'', and ''H. aqualupian''. Huperz ...
, an extract from the herb, ''
Huperzia serrata
''Huperzia serrata'', the toothed clubmoss, is a plant known as a firmoss which contains the acetylcholinesterase inhibitor huperzine A
Huperzine A is a naturally occurring sesquiterpene alkaloid compound found in the firmoss ''Huperzia serr ...
'', is under preliminary research as a possible therapeutic for Alzheimer's disease, but poor methodological quality of the research restricts conclusions about its effectiveness.
Ephedrine
Ephedrine is a central nervous system (CNS) stimulant that is often used to prevent low blood pressure during anesthesia. It has also been used for asthma, narcolepsy, and obesity but is not the preferred treatment. It is of unclear benefit in ...
in its natural form, known as ''m├Ī hu├Īng'' () in TCM, has been documented in China since the
Han dynasty
The Han dynasty (, ; ) was an imperial dynasty of China (202 BC ŌĆō 9 AD, 25ŌĆō220 AD), established by Liu Bang (Emperor Gao) and ruled by the House of Liu. The dynasty was preceded by the short-lived Qin dynasty (221ŌĆō207 BC) and a warr ...
(206 BCE ŌĆō 220 CE) as an
antiasthmatic and stimulant.
In 1885, the chemical synthesis of ephedrine was first accomplished by Japanese
organic chemist
Organic chemistry is a subdiscipline within chemistry involving the scientific study of the structure, properties, and reactions of organic compounds and organic materials, i.e., matter in its various forms that contain carbon atoms.Clayden, J. ...
Nagai Nagayoshi based on his research on
Japanese
Japanese may refer to:
* Something from or related to Japan, an island country in East Asia
* Japanese language, spoken mainly in Japan
* Japanese people, the ethnic group that identifies with Japan through ancestry or culture
** Japanese diaspor ...
and Chinese traditional herbal medicines
was first documented in the
Ming dynasty
The Ming dynasty (), officially the Great Ming, was an Dynasties in Chinese history, imperial dynasty of China, ruling from 1368 to 1644 following the collapse of the Mongol Empire, Mongol-led Yuan dynasty. The Ming dynasty was the last ort ...
.
Cost-effectiveness
A 2012 systematic review found there is a lack of available
cost-effectiveness evidence in TCM.
Safety

From the earliest records regarding the use of compounds to today, the toxicity of certain substances has been described in all Chinese materiae medicae.
Since TCM has become more popular in the Western world, there are increasing concerns about the potential toxicity of many traditional Chinese plants, animal parts and minerals.
Traditional Chinese herbal remedies are conveniently available from grocery stores in most Chinese neighborhoods; some of these items may contain toxic ingredients, are imported into the U.S. illegally, and are associated with claims of therapeutic benefit without evidence.
For most compounds, efficacy and toxicity testing are based on traditional knowledge rather than laboratory analysis.
The toxicity in some cases could be confirmed by modern research (i.e., in scorpion); in some cases it could not (i.e., in ''
Curculigo'').
Traditional herbal medicines can contain extremely toxic chemicals and heavy metals, and naturally occurring toxins, which can cause illness, exacerbate pre-existing poor health or result in death.
Botanical misidentification of plants can cause toxic reactions in humans.
The description of some plants used in TCM has changed, leading to unintended poisoning by using the wrong plants.
A concern is also contaminated herbal medicines with microorganisms and fungal toxins, including
aflatoxin
Aflatoxins are various poisonous carcinogens and mutagens that are produced by certain molds, particularly ''Aspergillus'' species. The fungi grow in soil, decaying vegetation and various staple foodstuffs and commodities such as hay, sweetcorn ...
.
Traditional herbal medicines are sometimes contaminated with toxic heavy metals, including lead, arsenic, mercury and cadmium, which inflict serious health risks to consumers.
Also, adulteration of some herbal medicine preparations with conventional drugs which may cause serious adverse effects, such as
corticosteroid
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex of vertebrates, as well as the synthetic analogues of these hormones. Two main classes of corticosteroids, glucocorticoids and mineralocorticoids, are involv ...
s,
phenylbutazone
Phenylbutazone, often referred to as "bute", is a nonsteroidal anti-inflammatory drug (NSAID) for the short-term treatment of pain and fever in animals.
In the United States and United Kingdom, it is no longer approved for human use (except in th ...
,
phenytoin
Phenytoin (PHT), sold under the brand name Dilantin among others, is an anti-seizure medication. It is useful for the prevention of tonic-clonic seizures (also known as grand mal seizures) and focal seizures, but not absence seizures. The intr ...
, and
glibenclamide
Glibenclamide, also known as glyburide, is an antidiabetic medication used to treat type 2 diabetes. It is recommended that it be taken together with diet and exercise. It may be used with other antidiabetic medication. It is not recommended f ...
, has been reported.
Substances known to be potentially dangerous include ''
Aconitum
''Aconitum'' (), also known as aconite, monkshood, wolf's-bane, leopard's bane, mousebane, women's bane, devil's helmet, queen of poisons, or blue rocket, is a genus of over 250 species of flowering plants belonging to the family Ranunculaceae. ...
'',
secretions from the
Asiatic toad
The Asiatic toad or Chusan Island toad (''Bufo gargarizans'') is a species of toad endemic to East Asia. The species was previously classified as ''Bufo bufo gargarizans'', a subspecies of the common toad.
Distribution and habitat
It is comm ...
,
powdered centipede,
the Chinese beetle (''
Mylabris phalerata''),
certain fungi,
''
Aristolochia
''Aristolochia'' () is a large plant genus with over 500 species that is the type genus of the family Aristolochiaceae. Its members are commonly known as birthwort, pipevine or Dutchman's pipe and are widespread and occur in the most diverse clima ...
'',
arsenic sulfide (
realgar
Realgar ( ), also known as "ruby sulphur" or "ruby of arsenic", is an arsenic sulfide mineral with the chemical formula ╬▒-. It is a soft, sectile mineral occurring in monoclinic crystals, or in granular, compact, or powdery form, often in asso ...
),
mercury sulfide,
and
cinnabar
Cinnabar (), or cinnabarite (), from the grc, ╬║╬╣╬Į╬Į╬¼╬▓╬▒Žü╬╣ (), is the bright scarlet to brick-red form of Mercury sulfide, mercury(II) sulfide (HgS). It is the most common source ore for refining mercury (element), elemental mercury and ...
.
Asbestos ore (
Actinolite
Actinolite is an amphibole silicate mineral with the chemical formula .
Etymology
The name ''actinolite'' is derived from the Greek word ''aktis'' (), meaning "beam" or "ray", because of the mineral's fibrous nature.
Mineralogy
Actinolite is ...
, Yang Qi Shi, ķś│ĶĄĘń¤│) is used to treat impotence in TCM.
[''Encyclopedic Reference of Traditional Chinese Medicine'', Xinrong Yang, p. 8]
Due to
galena
Galena, also called lead glance, is the natural mineral form of lead(II) sulfide (PbS). It is the most important ore of lead and an important source of silver.
Galena is one of the most abundant and widely distributed sulfide minerals. It cryst ...
's (
litharge
Litharge (from Greek lithargyros, lithos (stone) + argyros (silver) ''╬╗╬╣╬Ė╬¼Žü╬│ŽģŽü╬┐Žé'') is one of the natural mineral forms of lead(II) oxide, PbO. Litharge is a secondary mineral which forms from the oxidation of galena ores. It forms as coa ...
,
lead(II) oxide
Lead(II) oxide, also called lead monoxide, is the inorganic compound with the molecular formula Pb O. PbO occurs in two polymorphs: litharge having a tetragonal crystal structure, and massicot having an orthorhombic crystal structure. Modern ap ...
) high lead content, it is known to be toxic.
Lead, mercury, arsenic, copper, cadmium, and thallium have been detected in TCM products sold in the U.S. and China.
To avoid its toxic adverse effects ''
Xanthium sibiricum'' must be processed.
Hepatotoxicity
Hepatotoxicity (from ''hepatic toxicity'') implies chemical-driven liver damage. Drug-induced liver injury is a cause of acute and chronic liver disease caused specifically by medications and the most common reason for a drug to be withdrawn fro ...
has been reported with products containing ''
Reynoutria multiflora
''Reynoutria multiflora'' ( syn. ''Fallopia multiflora'' and ''Polygonum multiflorum'') is a species of flowering plant in the buckwheat family Polygonaceae native to central and southern China. It is known by the English common names tuber flee ...
'' (
synonym
A synonym is a word, morpheme, or phrase that means exactly or nearly the same as another word, morpheme, or phrase in a given language. For example, in the English language, the words ''begin'', ''start'', ''commence'', and ''initiate'' are all ...
''Polygonum multiflorum''),
glycyrrhizin
Glycyrrhizin (or glycyrrhizic acid or glycyrrhizinic acid) is the chief sweet-tasting constituent of ''Glycyrrhiza glabra'' ( liquorice) root. Structurally, it is a saponin used as an emulsifier and gel-forming agent in foodstuffs and cosmet ...
, ''
Senecio
''Senecio'' is a genus of flowering plants in the daisy family (Asteraceae) that includes ragworts and groundsels.
Variously circumscribed taxonomically, the genus ''Senecio'' is one of the largest genera of flowering plants.
Description
Mor ...
'' and ''
Symphytum
''Symphytum'' is a genus of flowering plants in the borage family, Boraginaceae, known by the common name comfrey (pronounced ). There are 59 recognized species.WFO (2022): Symphytum L. Published on the Internet; http://www.worldfloraonline.org/ ...
''.
The herbs indicated as being hepatotoxic included ''
Dictamnus dasycarpus
''Dictamnus dasycarpus'' or chinese dittany is a species of flowering plant in the family Rutaceae, native from southeast Siberia to China and Korea. It was first described by Nikolai Turczaninow in 1842. It has also been treated as only a variet ...
'', ''
Astragalus membranaceous
''Astragalus mongholicus'', synonyms including ''Astragalus propinquus'' and ''Astragalus membranaceus'', commonly known as Mongolian milkvetch in English; 'ąźčāąĮčćąĖčĆ' in Mongolian; ''hu├Īng q├Ł'' (), ''b─øi q├Ł'' () or ''hu├Īng hu─ü hu├Īng ...
'', and ''
Paeonia lactiflora
''Paeonia lactiflora'' (Chinese peony, Chinese herbaceous peony, or common garden peony) is a species of herbaceous perennial flowering plant in the family Paeoniaceae, native to central and eastern Asia from eastern Tibet across northern Chi ...
''.
Contrary to popular belief, ''
Ganoderma lucidum'' mushroom extract, as an adjuvant for cancer immunotherapy, appears to have the potential for toxicity.
A 2013 review suggested that although the
antimalarial
Antimalarial medications or simply antimalarials are a type of antiparasitic chemical agent, often naturally derived, that can be used to treat or to prevent malaria, in the latter case, most often aiming at two susceptible target groups, young ...
herb ''
Artemisia annua
''Artemisia annua'', also known as sweet wormwood, sweet annie, sweet sagewort, annual mugwort or annual wormwood (), is a common type of wormwood native to temperate Asia, but naturalized in many countries including scattered parts of North Am ...
'' may not cause hepatotoxicity, haematotoxicity, or hyperlipidemia, it should be used cautiously during pregnancy due to a potential risk of embryotoxicity at a high dose.
However, many adverse reactions are due to misuse or abuse of Chinese medicine.
For example, the misuse of the dietary supplement ''
Ephedra Ephedra may refer to:
* Ephedra (medicine), a medicinal preparation from the plant ''Ephedra sinica''
* ''Ephedra'' (plant), genus of gymnosperm shrubs
See also
* Ephedrine
Ephedrine is a central nervous system (CNS) stimulant that is of ...
'' (containing ephedrine) can lead to adverse events including gastrointestinal problems as well as sudden death from
cardiomyopathy
Cardiomyopathy is a group of diseases that affect the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. A ...
.
Products adulterated with pharmaceuticals for weight loss or erectile dysfunction are one of the main concerns.
Chinese herbal medicine has been a major cause of
acute liver failure
Acute liver failure is the appearance of severe complications rapidly after the first signs (such as jaundice) of liver disease, and indicates that the liver has sustained severe damage (loss of function of 80ŌĆō90% of liver cells). The complicati ...
in China.
The harvesting of
Guano
Guano (Spanish from qu, wanu) is the accumulated excrement of seabirds or bats. As a manure, guano is a highly effective fertilizer due to the high content of nitrogen, phosphate, and potassium, all key nutrients essential for plant growth. G ...
from bat caves (''Ye Ming Sha'') brings workers into close contact with these animals, increasing the risk of
zoonosis
A zoonosis (; plural zoonoses) or zoonotic disease is an infectious disease of humans caused by a pathogen (an infectious agent, such as a bacterium, virus, parasite or prion) that has jumped from a non-human (usually a vertebrate) to a human. ...
. The Chinese virologist
Shi Zhengli
Shi Zhengli (; born 26 May 1964) is a Chinese virologist who researches SARS-like coronaviruses of bat origin. Shi directs the Center for Emerging Infectious Diseases at the Wuhan Institute of Virology (WIV). In 2017, Shi and her colleague Cui ...
has identified dozens of SARS-like
coronavirus
Coronaviruses are a group of related RNA viruses that cause diseases in mammals and birds. In humans and birds, they cause respiratory tract infections that can range from mild to lethal. Mild illnesses in humans include some cases of the com ...
es in samples of bat droppings.
Acupuncture and moxibustion


Acupuncture is the insertion of needles into superficial structures of the body (skin, subcutaneous tissue, muscles) ŌĆō usually at acupuncture points (acupoints) ŌĆō and their subsequent manipulation; this aims at influencing the flow of
qi.
According to TCM it relieves
pain
Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, ...
and treats (and prevents) various diseases.
The US FDA classifies single-use acupuncture needles as Class II medical devices, under CFR 21.
Acupuncture is often accompanied by moxibustion ŌĆō the Chinese characters for acupuncture () literally meaning "acupuncture-moxibustion" ŌĆō which involves burning
mugwort
Mugwort is a common name for several species of aromatic flowering plants in the genus ''Artemisia.'' In Europe, mugwort most often refers to the species '' Artemisia vulgaris'', or common mugwort. In East Asia the species '' Artemisia argyi'' i ...
on or near the skin at an acupuncture point.
According to the
American Cancer Society
The American Cancer Society (ACS) is a nationwide voluntary health organization dedicated to eliminating cancer. Established in 1913, the society is organized into six geographical regions of both medical and lay volunteers operating in more than ...
, "available scientific evidence does not support claims that moxibustion is effective in preventing or treating cancer or any other disease".
In
electroacupuncture
Electroacupuncture is a form of acupuncture where a small electric current is passed between pairs of acupuncture needles.
According to some acupuncturists, this practice augments the use of regular acupuncture, can restore health and well-bei ...
, an electric current is applied to the needles once they are inserted, to further stimulate the respective acupuncture points.
A recent historian of Chinese medicine remarked that it is "nicely ironic that the specialty of acupuncture -- arguably the most questionable part of their medical heritage for most Chinese at the start of the twentieth century -- has become the most marketable aspect of Chinese medicine." She found that acupuncture as we know it today has hardly been in existence for sixty years. Moreover, the fine,
filiform
Filiform, thread or filament like, can refer to:
* Filiform, a common term used in botany to describe a thread-like shape
*Filiform, or filiform catheter
In medicine, a catheter (/╦łk├”╬Ė╔Öt╔Ör/) is a thin tubing (material), tube made from m ...
needle we think of as the acupuncture needle today was not widely used a century ago. Present day acupuncture was developed in the 1930s and put into wide practice only as late as the 1960s.
Efficacy
A 2013 editorial in the American journal ''
Anesthesia and Analgesia'' stated that acupuncture studies produced inconsistent results, (i.e. acupuncture relieved pain in some conditions but had no effect in other very similar conditions) which suggests the presence of
false positive results. These may be caused by factors like biased study design, poor blinding, and the classification of electrified needles (a type of
TENS
Transcutaneous electrical nerve stimulation (TENS or TNS) is the use of electric current produced by a device to stimulate the nerves for therapeutic purposes. TENS, by definition, covers the complete range of transcutaneously applied currents ...
) as a form of acupuncture. The inability to find consistent results despite more than 3,000 studies, the editorial continued, suggests that the treatment seems to be a
placebo effect
A placebo ( ) is a substance or treatment which is designed to have no therapeutic value. Common placebos include inert tablets (like sugar pills), inert injections (like Saline (medicine), saline), sham surgery, and other procedures.
In general ...
and the existing equivocal positive results are the type of
noise
Noise is unwanted sound considered unpleasant, loud or disruptive to hearing. From a physics standpoint, there is no distinction between noise and desired sound, as both are vibrations through a medium, such as air or water. The difference arise ...
one expects to see after a large number of studies are performed on an inert therapy. The editorial concluded that the best controlled studies showed a clear pattern, in which the outcome does not rely upon needle location or even needle insertion, and since "these variables are those that define acupuncture, the only sensible conclusion is that acupuncture does not work."
According to the US NIH National Cancer Institute, a review of 17,922 patients reported that real acupuncture relieved muscle and joint pain, caused by aromatase inhibitors, much better than sham acupuncture.
Regarding cancer patients, The review hypothesized that acupuncture may cause physical responses in nerve cells, the pituitary gland, and the brain ŌĆō releasing proteins, hormones, and chemicals that are proposed to affect blood pressure, body temperature, immune activity, and endorphin release.
A 2012 meta-analysis concluded that the mechanisms of acupuncture "are clinically relevant, but that an important part of these total effects is not due to issues considered to be crucial by most acupuncturists, such as the correct location of points and depth of needling ...
ut is... associated with more potent placebo or context effects".
Commenting on this meta-analysis, both
Edzard Ernst
Edzard Ernst (born 30 January 1948) is a retired British-German academic physician and researcher specializing in the study of complementary and alternative medicine. He was Professor of Complementary Medicine at the University of Exeter, alleged ...
and David Colquhoun said the results were of negligible clinical significance.
[ Reply to: ]
A 2011 overview of
Cochrane reviews found evidence that suggests acupuncture is effective for some but not all kinds of pain.
A 2010 systematic review found that there is evidence "that acupuncture provides a short-term clinically relevant effect when compared with a waiting list control or when acupuncture is added to another intervention" in the treatment of chronic low back pain.
Two review articles discussing the effectiveness of acupuncture, from 2008 and 2009, have concluded that there is not enough evidence to conclude that it is effective beyond the placebo effect.
Acupuncture is generally safe when administered using Clean Needle Technique (CNT).
Although serious
adverse effects
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. The term complica ...
are rare, acupuncture is not without risk.
Severe adverse effects, including very rarely death (5 case reports), have been reported.
Tui na

Tui na () is a form of massage, based on the assumptions of TCM, from which
shiatsu
''Shiatsu'' ( ; ) is a form of Japanese bodywork based on concepts in traditional Chinese medicine such as qi meridians. Having been popularized in the twentieth century by Tokujiro Namikoshi (1905ŌĆō2000), ''shiatsu'' derives from the older ...
is thought to have evolved.
Techniques employed may include thumb presses, rubbing, percussion, and assisted stretching.
Qigong
Q├¼g┼Źng () is a TCM system of exercise and meditation that combines regulated breathing, slow movement, and focused awareness, purportedly to cultivate and balance qi.
One branch of qigong is qigong massage, in which the practitioner combines massage techniques with awareness of the acupuncture channels and points.
Qi is air, breath, energy, or primordial life source that is neither matter or spirit. While Gong is a skillful movement, work, or exercise of the qi.
Forms
* ''Nei gong'': introspective and meditative
* ''Wai gong'': external energy and motion
* ''Dong gong'': dynamic or active
* ''Jing gong'': tranquil or passive
Other therapies
Cupping

Cupping () is a type of Chinese massage, consisting of placing several glass "cups" (open spheres) on the body. A match is lit and placed inside the cup and then removed before placing the cup against the skin. As the air in the cup is heated, it expands, and after placing in the skin, cools, creating lower pressure inside the cup that allows the cup to stick to the skin via
suction.
When combined with massage oil, the cups can be slid around the back, offering "reverse-pressure massage".
Gua sha

Gua sha () is abrading the skin with pieces of smooth jade, bone, animal tusks or horns or smooth stones; until red spots then bruising cover the area to which it is done. It is believed that this treatment is for almost any ailment. The red spots and bruising take three to ten days to heal, there is often some soreness in the area that has been treated.
Die-da
Di─ō-d├Ī () or Dit Da, is a traditional Chinese
bone-setting
Traditional bone-setting is a type of a folk medicine in which practitioners engaged in joint manipulation. Before the advent of chiropractors, osteopaths and physical therapists, bone-setters were the main providers of this type of treatment. T ...
technique, usually practiced by martial artists who know aspects of Chinese medicine that apply to the treatment of
trauma
Trauma most often refers to:
* Major trauma, in physical medicine, severe physical injury caused by an external source
* Psychological trauma, a type of damage to the psyche that occurs as a result of a severely distressing event
*Traumatic i ...
and injuries such as bone fractures, sprains, and bruises. Some of these specialists may also use or recommend other disciplines of Chinese medical therapies if serious injury is involved. Such practice of bone-setting () is not common in the West.
Chinese food therapy
The concepts ''yin'' and ''yang'' are associated with different classes of foods, and tradition considers it important to consume them in a balanced fashion.
Regulations
Many governments have enacted laws to regulate TCM practice.
Australia
From 1 July 2012 Chinese medicine practitioners must be registered under the national registration and accreditation scheme with the Chinese Medicine Board of Australia and meet the Board's Registration Standards, to practice in Australia.
Canada
TCM is regulated in five provinces in Canada: Alberta, British Columbia,
Ontario,
Quebec, and Newfoundland & Labrador.
China (mainland)
The People's Republic of China has supported TCM since its founding in 1949
The
National Administration of Traditional Chinese Medicine
National Administration of Traditional Chinese Medicine () is a state administration of the People's Republic of China under the jurisdiction of the National Health Commission (formerly the National Health and Family Planning Commission), respons ...
was created in 1949, which then absorbed existing TCM management in 1986 with major changes in 1998.
China's National People's Congress Standing Committee passed the country's first law on TCM in 2016, which came into effect on 1 July 2017. The new law standardized TCM certifications by requiring TCM practitioners to (i) pass exams administered by provincial-level TCM authorities, and (ii) obtain recommendations from two certified practitioners. TCM products and services can be advertised only with approval from the local TCM authority.
Hong Kong
During
British rule
The British Raj (; from Hindi ''r─üj'': kingdom, realm, state, or empire) was the rule of the British Crown on the Indian subcontinent;
*
* it is also called Crown rule in India,
*
*
*
*
or Direct rule in India,
* Quote: "Mill, who was hims ...
, Chinese medicine practitioners in Hong Kong were not recognized as "medical doctors", which means they could not issue prescription drugs, give injections, etc. However, TCM practitioners could register and operate TCM as "herbalists". The Chinese Medicine Council of Hong Kong was established in 1999. It regulates the compounds and professional standards for TCM practitioners. All TCM practitioners in Hong Kong are required to register with the council. The eligibility for registration includes a recognised 5-year university degree of TCM, a 30-week minimum supervised clinical internship, and passing the licensing exam.
[The Chinese Medicine Council of Hong Kong](_blank)
Hong Kong Registered the Chinese Medicine Practitioner licensure requirements
Macau
The
Portuguese Macau
Portuguese Macau (officially the Province of Macau until 1976, and then the Autonomous Region of Macau from 1976 to 1999) was a Portuguese Empire, Portuguese colony that existed from the first official Portuguese settlement in 1557 to the ...
government seldom interfered in the affairs of Chinese society, including with regard to regulations on the practice of TCM. There were a few TCM pharmacies in Macau during the colonial period. In 1994, the Portuguese Macau government published Decree-Law no. 53/94/M that officially started to regulate the TCM market. After the sovereign handover, the Macau S.A.R. government also published regulations on the practice of TCM. In 2000,
Macau University of Science and Technology
The Macau University of Science and Technology (M.U.S.T., ; pt, Universidade de Ciência e Tecnologia de Macau) is a private university founded in 2000 at Taipa, Macau, China.
M.U.S.T. is acknowledged by Macau Education and Youth Developmen ...
and
Nanjing University of Traditional Chinese Medicine
The Nanjing University of Chinese Medicine (a.k.a. NJUCM, ), is located in Nanjing, capital of China's Jiangsu province. It is jointly constructed by the People's Government of Jiangsu Province and the State Administration of Traditional Chinese ...
established the Macau College of Traditional Chinese Medicine to offer a degree course in Chinese medicine.
In Macau, the legitimacy of Chinese medicine is not built upon "miracle making". Instead, it is achieved through a celebration of cultural tradition rejuvenated with discourses of nationalism and modernity, and through the mutual constructions of medical references between doctors and patients.
In 2022, a new law regulating TCM, Law no. 11/2021, came into effect. The same law also repealed Decree-Law no. 53/94/M.
Indonesia

All traditional medicines, including TCM, are regulated by Indonesian Minister of Health Regulation of 2013 on traditional medicine. Traditional medicine license (''Surat Izin Pengobatan Tradisional'' ŌĆō SIPT) is granted to the practitioners whose methods are recognized as safe and may benefit health.
The TCM clinics are registered but there is no explicit regulation for it. The only TCM method which is accepted by medical logic and is empirically proofed is acupuncture.
[Cheta Nilawaty dan Rini Kustiati. 13 August 2012. TEMPO]
Belum Ada Aturan Soal Klinik Pengobatan Cina
. The acupuncturists can get SIPT and participate in health care facilities.
Japan

Malaysia
The Traditional and Complementary Medicine Bill was passed by parliament in 2012 establishing the Traditional and Complementary Medicine Council to register and regulate traditional and complementary medicine practitioners, including TCM practitioners as well as other traditional and complementary medicine practitioners such as those in traditional Malay medicine and traditional Indian medicine.
Netherlands

There are no specific regulations in the Netherlands on TCM;
TCM is neither prohibited nor recognised by the
government of the Netherlands
The politics of the Netherlands take place within the framework of a parliamentary representative democracy, a constitutional monarchy, and a decentralised unitary state.''Civil service systems in Western Europe'' edited by A. J. G. M. Bekke, ...
.
that are used in TCM are classified as foods and
food supplement
A dietary supplement is a manufactured product intended to supplement one's diet by taking a pill, capsule, tablet, powder, or liquid. A supplement can provide nutrients either extracted from food sources or that are synthetic in order ...
s, and these Chinese herbs can be imported into the Netherlands as well as marketed as such without any type registration or notification to the government.
Despite its status, some private
health insurance
Health insurance or medical insurance (also known as medical aid in South Africa) is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among ma ...
companies reimburse a certain amount of annual costs for
acupuncture
Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine (TCM) in which thin needles are inserted into the body. Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientifi ...
treatments, this depends on one's insurance policy, as not all insurance policies cover it, and if the acupuncture practitioner is or is not a member of one of the professional organisations that are recognised by private health insurance companies.
The recognized professional organizations include the Nederlandse Vereniging voor Acupunctuur (NVA), Nederlandse Artsen Acupunctuur Vereniging (NAAV), ZHONG, (Nederlandse Vereniging voor Traditionele Chinese Geneeskunde), Nederlandse Beroepsvereniging Chinese Geneeswijzen Yi (NBCG Yi), and Wetenschappelijke Artsen Vereniging voor Acupunctuur in Nederland (WAVAN).
New Zealand
Although there are no regulatory standards for the practice of TCM in New Zealand, in the year 1990, acupuncture was included in the Governmental
Accident Compensation Corporation
The Accident Compensation Corporation (ACC) ( mi, Te Kaporeihana ─Ćwhina Hunga Whara) is the New Zealand Crown entity responsible for administering the country's no-fault accidental injury compensation scheme, commonly referred to as the ACC sch ...
(ACC) Act. This inclusion granted qualified and professionally registered acupuncturists to provide subsidised care and treatment to citizens, residents, and temporary visitors for work or sports related injuries that occurred within and upon the land of New Zealand. The two bodies for the regulation of acupuncture and attainment of ACC treatment provider status in New Zealand are Acupuncture NZ and The New Zealand Acupuncture Standards Authority.
Singapore
The TCM Practitioners Act was passed by Parliament in 2000 and the TCM Practitioners Board was established in 2001 as a statutory board under the Ministry of Health, to register and regulate TCM practitioners. The requirements for registration include possession of a diploma or degree from a TCM educational institution/university on a gazetted list, either structured TCM clinical training at an approved local TCM educational institution or foreign TCM registration together with supervised TCM clinical attachment/practice at an approved local TCM clinic, and upon meeting these requirements, passing the Singapore TCM Physicians Registration Examination (STRE) conducted by the TCM Practitioners Board.
United States
As of July 2012, only six states lack legislation to regulate the professional practice of TCM:
Alabama
(We dare defend our rights)
, anthem = "Alabama (state song), Alabama"
, image_map = Alabama in United States.svg
, seat = Montgomery, Alabama, Montgomery
, LargestCity = Huntsville, Alabama, Huntsville
, LargestCounty = Baldwin County, Al ...
,
Kansas
Kansas () is a state in the Midwestern United States. Its capital is Topeka, and its largest city is Wichita. Kansas is a landlocked state bordered by Nebraska to the north; Missouri to the east; Oklahoma to the south; and Colorado to the ...
,
North Dakota
North Dakota () is a U.S. state in the Upper Midwest, named after the Native Americans in the United States, indigenous Dakota people, Dakota Sioux. North Dakota is bordered by the Canadian provinces of Saskatchewan and Manitoba to the north a ...
,
South Dakota
South Dakota (; Sioux language, Sioux: , ) is a U.S. state in the West North Central states, North Central region of the United States. It is also part of the Great Plains. South Dakota is named after the Lakota people, Lakota and Dakota peo ...
,
Oklahoma
Oklahoma (; Choctaw language, Choctaw: ; chr, ßÄŻßĦßÄ│ßÄ░ßÄ╣, ''Okalahoma'' ) is a U.S. state, state in the South Central United States, South Central region of the United States, bordered by Texas on the south and west, Kansas on the nor ...
, and
Wyoming
Wyoming () is a U.S. state, state in the Mountain states, Mountain West subregion of the Western United States. It is bordered by Montana to the north and northwest, South Dakota and Nebraska to the east, Idaho to the west, Utah to the south ...
. In 1976, California established an Acupuncture Board and became the first state licensing professional acupuncturists.
[ California Acupuncture Board.]
See also
*
Compendium of Materia Medica
The ''Bencao gangmu'', known in English as the ''Compendium of Materia Medica'' or ''Great Pharmacopoeia'', is an encyclopedic gathering of medicine, natural history, and Chinese herbology compiled and edited by Li Shizhen and published in the ...
*
Huangdi Neijing
''Huangdi Neijing'' (), literally the ''Inner Canon of the Yellow Emperor'' or ''Esoteric Scripture of the Yellow Emperor'', is an ancient Chinese medical text or group of texts that has been treated as a fundamental doctrinal source for Chines ...
* ''
American Journal of Chinese Medicine''
*
The body in traditional Chinese medicine
The model of the body in traditional Chinese medicine (TCM) has the following elements:
* the Fundamental Substances;
* Qi, Blood, Jing (Essence), Shen (Mind) that nourish and protect the Zang-Fu organs;
* and the meridians (''jing-luo'') whic ...
*
Capsicum plaster
*
Chinese classic herbal formula
*
Chinese herbology
Chinese herbology () is the theory of traditional Chinese herbal therapy, which accounts for the majority of treatments in traditional Chinese medicine (TCM). A ''Nature'' editorial described TCM as "fraught with pseudoscience", and said that t ...
*
Chinese Ophthalmology Chinese ophthalmology () is part of the Traditional Chinese medicine (TCM). Here diseases of the eyes are treated with Chinese herbs, acupuncture/moxibustion, tuina, Chinese dietary therapy as well as qigong and taijiquan.
Inscriptions on oracle ...
*
Chinese patent medicine
Chinese patent medicine () are herbal medicines in Traditional Chinese medicine, modernized into a ready-to-use form such as tablets, oral solutions or dry suspensions, as opposed to herbs that require cooking (hot water extraction).
Description ...
*
Guizhentang Pharmaceutical company
*
Hallucinogenic plants in Chinese herbals For over two millennia, texts in Chinese herbology and traditional Chinese medicine have recorded medicinal plants that are also hallucinogens and psychedelics. Some are familiar psychoactive plants in Western herbal medicine (e.g., , i.e. ''Hyosc ...
*
HIV/AIDS and traditional Chinese medicine
* ''
Journal of Traditional Chinese Medicine
''The Journal of Traditional Chinese Medicine'' was the first English-language journal on the subject of traditional Chinese medicine, including acupuncture, herbal medicine, homeopathy, massotherapy, mind-body therapies, palliative care and other ...
''
*
Hua Tuo
Hua Tuo ( 140ŌĆō208), courtesy name Yuanhua, was a Chinese physician who lived during the late Eastern Han dynasty. The historical texts '' Records of the Three Kingdoms'' and '' Book of the Later Han'' record Hua Tuo as the first person in Ch ...
*
Li Shizhen
Li Shizhen (July 3, 1518 ŌĆō 1593), courtesy name Dongbi, was a Chinese acupuncturist, herbalist, naturalist, pharmacologist, physician, and writer of the Ming dynasty. He is the author of a 27-year work, found in the ''Compendium of M ...
*
List of branches of alternative medicine
This is a list of articles covering alternative medicine topics.
A
* Activated charcoal cleanse
* Acupressure
* Acupuncture
* Affirmative prayer
* Alexander technique
* Alternative cancer treatments
* Animal-Assisted Therapy
* Anthroposo ...
*
List of topics characterized as pseudoscience
This is a list of topics that have, either currently or in the past, been characterized as pseudoscience by academics or researchers. Detailed discussion of these topics may be found on their main pages. These characterizations were made in the ...
*
List of traditional Chinese medicines
In Traditional Chinese Medicine, there are roughly 13,000 medicinals used in China and over 100,000 medicinal prescriptions recorded in the ancient literature.Certain progress of clinical research on Chinese integrative medicine, Keji Chen, Bei Yu ...
*
Medicinal mushrooms
Medicinal fungi are fungi that contain metabolites or can be induced to produce metabolites through biotechnology to develop prescription drugs. Compounds successfully developed into drugs or under research include antibiotics, anti-cancer drugs, ...
*
Pharmacognosy
*
Public health in the People's Republic of China
*
Qingdai
*
Qiu Li Gao Qiu Li Gao or Autumn Pear Syrup or Sydney Paste is a pear syrup or paste used as a traditional medicine in East Asia, in particular in Chinese food therapy.
History
The preparation was known as early as the Qing Dynasty, when it was mentioned in ...
*
Snake farm
A snake farm is a facility that houses and breeds a wide variety of snakes, often for the purpose of research and the collection of venom for the creation of antivenom. Many snake farms are primarily tourist attractions. Notable snake farms exist ...
*
Sun Simiao
Sun Simiao (; died 682) was a Chinese physician and writer of the Sui and Tang dynasty. He was titled as China's King of Medicine (, Yaowang) for his significant contributions to Chinese medicine and tremendous care to his patients.
Books
Sun ...
*
Tao Hongjing
Tao Hongjing (456ŌĆō536), courtesy name Tongming, was a Chinese alchemist, astronomer, calligrapher, military general, musician, physician, and pharmacologist, and writer during the Northern and Southern dynasties (420ŌĆō589). A polymathic indiv ...
*
Traditional Korean medicine
Traditional Korean medicine (known in North Korea as Koryo medicine) refers to the forms of traditional medicine practiced in Korea.
History
Korean medicine traditions originated in ancient and prehistoric times and can be traced back as far a ...
*
Traditional Mongolian medicine
*
Traditional Vietnamese medicine
Traditional Vietnamese medicine (Y hß╗Źc Cß╗Ģ truyß╗ün Viß╗ćt Nam), also known as Southern Herbology (Thuß╗æc Nam) is a traditional medicine practiced by Vietnamese people. It is influenced by traditional Chinese medicine. The other traditional ...
*
Traditional Tibetan medicine
Traditional Tibetan medicine (), also known as Sowa-Rigpa medicine, is a centuries-old traditional medical system that employs a complex approach to diagnosis, incorporating techniques such as pulse analysis and urinalysis, and utilizes behavior ...
*
Traditional Indian medicine
*
Turtle farming
Turtle farming is the practice of raising turtles and tortoises of various species commercially. Raised animals are sold for use as gourmet food, traditional medicine ingredients, or as pets. Some farms also sell young animals to other farms, e ...
*
Zhang Jiegu
Zhang Yuansu Õ╝Āõ║ōń┤Ā (a.k.a. Zhang Jiegu; ca. 1151ŌĆō1234) was one of the most historically influential Traditional Chinese medicine physicians in the period of transition from China's northern Jin dynasty to the Mongolian Yuan dynasty
...
Notes
References
Citations
Sources
*
*
*
*
*
*
* Review of Liu Lihong ''Classical Chinese Medicine'' (below). Also free online at ''China File'
Chinese Medicine in Covid Wards.
*
*
*
*
*
*
*
*
*
*
Further reading
*
* Shows early use of Chinese medicine not always perceived as "Chinese."
*
*
*
*
* McGrew, Roderick. ''Encyclopedia of Medical History'' (1985), brief history on pp. 56ŌĆō59
*
*
*
*
*
*
*
*
External links
Medicinal Plant Images DatabaseĆöSchool of Chinese Medicine, Hong Kong Baptist University
Chinese Medicine Specimen DatabaseĆöSchool of Chinese Medicine, Hong Kong Baptist University
''Literary Review Compilation on Traditional Chinese Medicine'' PDF, 133 pages; compiled by the Association Qu├®b├®coise des Th├®rapeutes Naturels (AQTN)
{{Authority control
Alternative medicine
Pharmacy in China
Pseudoscience
 Scholars in the history of medicine in China distinguish its doctrines and practice from those of present-day TCM. As Ian Johnson notes, the term "Traditional Chinese Medicine" was coined by "party propagandists" and first appeared in English in 1955.
Scholars in the history of medicine in China distinguish its doctrines and practice from those of present-day TCM. As Ian Johnson notes, the term "Traditional Chinese Medicine" was coined by "party propagandists" and first appeared in English in 1955.  The meridians (, ) are believed to be channels running from the z├Āng-fŪö in the interior (, ) of the body to the limbs and joints ("the surface" , transporting qi and xu─Ģ." [The jingluo transport qi and blood through the whole body, connecting the zang-fu with limbs and joints, connecting interior with surface, up with down, inside with outside ...] as seen at TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being (, lit. "the Twelve Vessels") and () respectively." [(3.) The Twelve Vessels ... (4.) The Extraordinary Eight Vessels ...] as seen at There's also a number of less customary channels branching from the "regular" meridians.
The meridians (, ) are believed to be channels running from the z├Āng-fŪö in the interior (, ) of the body to the limbs and joints ("the surface" , transporting qi and xu─Ģ." [The jingluo transport qi and blood through the whole body, connecting the zang-fu with limbs and joints, connecting interior with surface, up with down, inside with outside ...] as seen at TCM identifies 12 "regular" and 8 "extraordinary" meridians; the Chinese terms being (, lit. "the Twelve Vessels") and () respectively." [(3.) The Twelve Vessels ... (4.) The Extraordinary Eight Vessels ...] as seen at There's also a number of less customary channels branching from the "regular" meridians.

 The term "herbal medicine" is somewhat misleading in that, while plant elements are by far the most commonly used substances in TCM, other, non-botanic substances are used as well: animal, human, and mineral products are also used. Thus, the term "medicinal" (instead of herb) may be used, although there is no scientific evidence that any of these compounds have medicinal effects.
The term "herbal medicine" is somewhat misleading in that, while plant elements are by far the most commonly used substances in TCM, other, non-botanic substances are used as well: animal, human, and mineral products are also used. Thus, the term "medicinal" (instead of herb) may be used, although there is no scientific evidence that any of these compounds have medicinal effects.
 Traditional Chinese medicine also includes some human parts: the classic Materia medica (
Traditional Chinese medicine also includes some human parts: the classic Materia medica (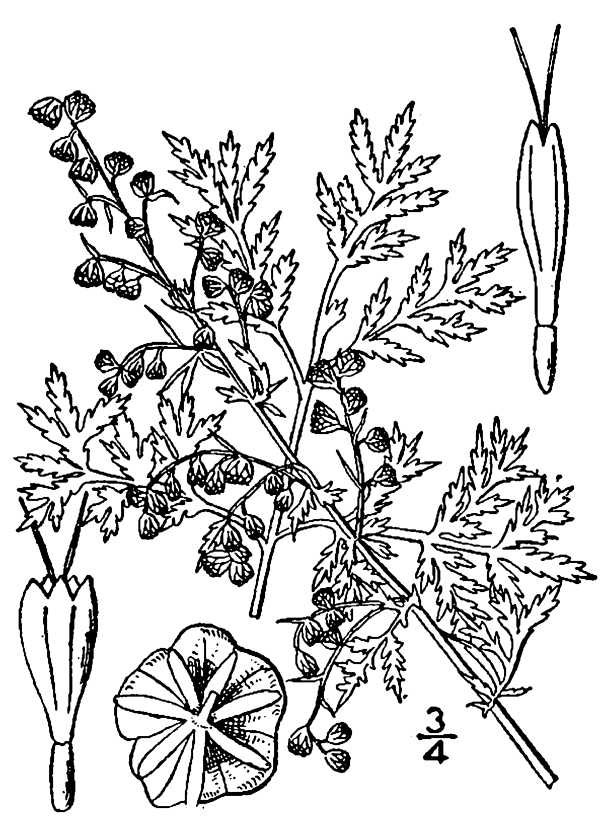 With an eye to the enormous Chinese market, pharmaceutical companies have explored creating new drugs from traditional remedies. The journal ''Nature'' commented that "claims made on behalf of an uncharted body of knowledge should be treated with the customary skepticism that is the bedrock of both science and medicine."
There had been success in the 1970s, however, with the development of the antimalarial drug
With an eye to the enormous Chinese market, pharmaceutical companies have explored creating new drugs from traditional remedies. The journal ''Nature'' commented that "claims made on behalf of an uncharted body of knowledge should be treated with the customary skepticism that is the bedrock of both science and medicine."
There had been success in the 1970s, however, with the development of the antimalarial drug  From the earliest records regarding the use of compounds to today, the toxicity of certain substances has been described in all Chinese materiae medicae. Since TCM has become more popular in the Western world, there are increasing concerns about the potential toxicity of many traditional Chinese plants, animal parts and minerals. Traditional Chinese herbal remedies are conveniently available from grocery stores in most Chinese neighborhoods; some of these items may contain toxic ingredients, are imported into the U.S. illegally, and are associated with claims of therapeutic benefit without evidence. For most compounds, efficacy and toxicity testing are based on traditional knowledge rather than laboratory analysis. The toxicity in some cases could be confirmed by modern research (i.e., in scorpion); in some cases it could not (i.e., in '' Curculigo''). Traditional herbal medicines can contain extremely toxic chemicals and heavy metals, and naturally occurring toxins, which can cause illness, exacerbate pre-existing poor health or result in death. Botanical misidentification of plants can cause toxic reactions in humans. The description of some plants used in TCM has changed, leading to unintended poisoning by using the wrong plants. A concern is also contaminated herbal medicines with microorganisms and fungal toxins, including
From the earliest records regarding the use of compounds to today, the toxicity of certain substances has been described in all Chinese materiae medicae. Since TCM has become more popular in the Western world, there are increasing concerns about the potential toxicity of many traditional Chinese plants, animal parts and minerals. Traditional Chinese herbal remedies are conveniently available from grocery stores in most Chinese neighborhoods; some of these items may contain toxic ingredients, are imported into the U.S. illegally, and are associated with claims of therapeutic benefit without evidence. For most compounds, efficacy and toxicity testing are based on traditional knowledge rather than laboratory analysis. The toxicity in some cases could be confirmed by modern research (i.e., in scorpion); in some cases it could not (i.e., in '' Curculigo''). Traditional herbal medicines can contain extremely toxic chemicals and heavy metals, and naturally occurring toxins, which can cause illness, exacerbate pre-existing poor health or result in death. Botanical misidentification of plants can cause toxic reactions in humans. The description of some plants used in TCM has changed, leading to unintended poisoning by using the wrong plants. A concern is also contaminated herbal medicines with microorganisms and fungal toxins, including 
 Acupuncture is the insertion of needles into superficial structures of the body (skin, subcutaneous tissue, muscles) ŌĆō usually at acupuncture points (acupoints) ŌĆō and their subsequent manipulation; this aims at influencing the flow of qi. According to TCM it relieves
Acupuncture is the insertion of needles into superficial structures of the body (skin, subcutaneous tissue, muscles) ŌĆō usually at acupuncture points (acupoints) ŌĆō and their subsequent manipulation; this aims at influencing the flow of qi. According to TCM it relieves  Tui na () is a form of massage, based on the assumptions of TCM, from which
Tui na () is a form of massage, based on the assumptions of TCM, from which  Gua sha () is abrading the skin with pieces of smooth jade, bone, animal tusks or horns or smooth stones; until red spots then bruising cover the area to which it is done. It is believed that this treatment is for almost any ailment. The red spots and bruising take three to ten days to heal, there is often some soreness in the area that has been treated.
Gua sha () is abrading the skin with pieces of smooth jade, bone, animal tusks or horns or smooth stones; until red spots then bruising cover the area to which it is done. It is believed that this treatment is for almost any ailment. The red spots and bruising take three to ten days to heal, there is often some soreness in the area that has been treated.
 All traditional medicines, including TCM, are regulated by Indonesian Minister of Health Regulation of 2013 on traditional medicine. Traditional medicine license (''Surat Izin Pengobatan Tradisional'' ŌĆō SIPT) is granted to the practitioners whose methods are recognized as safe and may benefit health. The TCM clinics are registered but there is no explicit regulation for it. The only TCM method which is accepted by medical logic and is empirically proofed is acupuncture.Cheta Nilawaty dan Rini Kustiati. 13 August 2012. TEMPO
All traditional medicines, including TCM, are regulated by Indonesian Minister of Health Regulation of 2013 on traditional medicine. Traditional medicine license (''Surat Izin Pengobatan Tradisional'' ŌĆō SIPT) is granted to the practitioners whose methods are recognized as safe and may benefit health. The TCM clinics are registered but there is no explicit regulation for it. The only TCM method which is accepted by medical logic and is empirically proofed is acupuncture.Cheta Nilawaty dan Rini Kustiati. 13 August 2012. TEMPO
 There are no specific regulations in the Netherlands on TCM; TCM is neither prohibited nor recognised by the
There are no specific regulations in the Netherlands on TCM; TCM is neither prohibited nor recognised by the