The Affordable Care Act (ACA), formally known as the Patient Protection and Affordable Care Act and colloquially known as Obamacare, is a landmark
U.S. federal statute
The law of the United States comprises many levels of codified and uncodified forms of law, of which the most important is the nation's Constitution, which prescribes the foundation of the federal government of the United States, as well as va ...
enacted by the
111th United States Congress
The 111th United States Congress was a meeting of the legislative branch of the United States federal government from January 3, 2009, until January 3, 2011. It began during the last weeks of the George W. Bush administration, with th ...
and signed into law by President
Barack Obama
Barack Hussein Obama II ( ; born August 4, 1961) is an American politician who served as the 44th president of the United States from 2009 to 2017. A member of the Democratic Party, Obama was the first African-American president of the U ...
on March 23, 2010. Together with the
Health Care and Education Reconciliation Act of 2010
The Health Care and Education Reconciliation Act of 2010 (, ) is a law that was enacted by the 111th United States Congress, by means of the reconciliation process, in order to amend the Affordable Care Act (ACA) (). The law includes the St ...
amendment, it represents the
U.S. healthcare system
The United States far outspends any other nation on health care, measured both in ''per capita'' spending and as a percentage of GDP. Despite this, the country has significantly worse healthcare outcomes when compared to peer nations. The Uni ...
's most significant regulatory overhaul and expansion of coverage since the enactment of
Medicare and
Medicaid
Medicaid in the United States is a federal and state program that helps with healthcare costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and pers ...
in 1965.
The ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered.
The law also enacted a host of
delivery system reforms intended to constrain healthcare costs and improve quality. After it went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans.
The increased coverage was due, roughly equally, to an
expansion of Medicaid eligibility and to changes to
individual insurance markets. Both received new spending, funded through a combination of new taxes and cuts to Medicare provider rates and
Medicare Advantage
Medicare Advantage (Medicare Part C, MA) is a capitated program for providing Medicare benefits in the United States. Under Part C, Medicare pays a private-sector health insurer a fixed payment. The insurer then pays for the health care expenses ...
. Several
Congressional Budget Office
The Congressional Budget Office (CBO) is a federal agency within the legislative branch of the United States government that provides budget and economic information to Congress.
Inspired by California's Legislative Analyst's Office that manages ...
(CBO) reports said that overall these provisions reduced the
budget deficit
Within the budgetary process, deficit spending is the amount by which spending exceeds revenue over a particular period of time, also called simply deficit, or budget deficit; the opposite of budget surplus. The term may be applied to the budget ...
, that repealing ACA would increase the deficit,
and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution.
The act largely retained the existing structure of
Medicare,
Medicaid
Medicaid in the United States is a federal and state program that helps with healthcare costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and pers ...
, and the
employer market, but individual markets were radically overhauled.
Insurers were made to
accept all applicants without charging based on
preexisting condition
In the context of healthcare in the United States, a pre-existing condition is a medical condition that started before a person's health insurance went into effect. Before 2014, some insurance policies would not cover expenses due to pre-existin ...
s or demographic status (except age). To combat the resultant
adverse selection
In economics, insurance, and risk management, adverse selection is a market situation where buyers and sellers have different information. The result is that participants with key information might participate selectively in trades at the expe ...
, the act
mandated that individuals buy insurance (or pay a fine/tax) and that insurers cover a list of "
essential health benefits
In the United States, essential health benefits (EHBs) are a set of ten benefits, defined under the Affordable Care Act (ACA) of 2010, that must be covered by individually-purchased health insurance and plans in small-group markets both inside and ...
".
Before and after enactment the ACA faced strong political opposition, calls for repeal and
legal challenges. In ''
National Federation of Independent Business v. Sebelius
''National Federation of Independent Business v. Sebelius'', 567 U.S. 519 (2012), was a List of landmark court decisions in the United States, landmark United States Supreme Court decision in which the Court upheld Congress's power to enact most ...
'', the
Supreme Court
A supreme court is the highest court within the hierarchy of courts in most legal jurisdictions. Other descriptions for such courts include court of last resort, apex court, and high (or final) court of appeal. Broadly speaking, the decisions of ...
ruled that states could choose not to participate in the law's Medicaid expansion, but upheld the law as a whole.
The federal health insurance exchange,
HealthCare.gov
HealthCare.gov is a health insurance exchange website operated by the United States federal government under the Provisions of the Affordable Care Act, provisions of the Affordable Care Act or ACA, commonly referred to as “Obamacare”, which c ...
, faced major technical problems at the beginning of its rollout in 2013. Polls initially found that a
plurality of Americans opposed the act, although its individual provisions were generally more popular. By 2017, the law had majority support. President
Donald Trump
Donald John Trump (born June 14, 1946) is an American politician, media personality, and businessman who served as the 45th president of the United States from 2017 to 2021.
Trump graduated from the Wharton School of the University of Pe ...
rescinded the federal tax penalty for violating the
individual mandate
An individual mandate is a requirement by law for certain persons to purchase or otherwise obtain a good or service.
United States Militia act
The Militia Acts of 1792, based on the Constitution's militia clause (in addition to its affirmative ...
through the
Tax Cuts and Jobs Act of 2017
The Act to provide for reconciliation pursuant to titles II and V of the concurrent resolution on the budget for fiscal year 2018, , is a congressional revenue act of the United States originally introduced in Congress as the Tax Cuts and Jobs A ...
, starting in 2019.
This raised questions about whether the ACA was still constitutional. In June 2021, the Supreme Court upheld the ACA for the third time in ''
California v. Texas''.
Provisions


ACA amended the
Public Health Service Act of 1944 and inserted new provisions on affordable care into
Title 42 of the United States Code
Title 42 of the United States Code is the United States Code dealing with public health, social welfare, and civil rights.
Chapters
* —The Public Health Service
* —The Public Health Service, Supplemental Provisions
* —Sanitation a ...
.
The individual insurance market was radically overhauled, and many of the law's regulations applied specifically to this market,
while the structure of Medicare, Medicaid, and the
employer market were largely retained.
Some regulations applied to the employer market, and the law also made delivery system changes that affected most of the health care system.
Insurance regulations: individual policies
All new individual major medical health insurance policies sold to individuals and families faced new requirements. The requirements took effect on January 1, 2014. They include:
*
Guaranteed issue Guaranteed issue is a term used in health insurance to describe a situation where a policy is offered to any eligible applicant without regard to health status. Often this is the result of guaranteed issue statutes regarding how health insurance ma ...
prohibits insurers from denying coverage to individuals due to
preexisting condition
In the context of healthcare in the United States, a pre-existing condition is a medical condition that started before a person's health insurance went into effect. Before 2014, some insurance policies would not cover expenses due to pre-existin ...
s.
* States were required to ensure the availability of insurance for individual children who did not have coverage via their families.
* A partial
community rating
Community rating is a concept usually associated with health insurance, which requires health insurance providers to offer health insurance policies within a given territory at the same price to all persons without medical underwriting, regardless ...
allows premiums to vary only by age and location, regardless of preexisting conditions. Premiums for older applicants can be no more than three times those for the youngest.
*
Essential health benefits
In the United States, essential health benefits (EHBs) are a set of ten benefits, defined under the Affordable Care Act (ACA) of 2010, that must be covered by individually-purchased health insurance and plans in small-group markets both inside and ...
must be provided. The
National Academy of Medicine
The National Academy of Medicine (NAM), formerly called the Institute of Medicine (IoM) until 2015, is an American nonprofit, non-governmental organization. The National Academy of Medicine is a part of the National Academies of Sciences, En ...
defines the law's "essential health benefits" as "ambulatory patient services; emergency services; hospitalization; maternity and newborn care; mental health and substance use disorder services, including behavioral health treatment; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services and chronic disease management; and pediatric services, including oral and vision care"
and others rated Level A or B by the
U.S. Preventive Services Task Force
The United States Preventive Services Task Force (USPSTF) is "an independent panel of experts in primary care and prevention that systematically reviews the evidence of effectiveness and develops recommendations for clinical preventive services". ...
.
In determining essential benefits, the law required that standard benefits should offer at least that of a "typical employer plan".
States may require additional services.
* Preventive care and screenings for women. "
l Food and Drug Administration approved
contraceptive
Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unwanted pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth contr ...
methods, sterilization procedures, and patient education and counseling for all women with reproductive capacity". This mandate applies to all employers and educational institutions except for religious organizations.
These regulations were included on the recommendations of the
Institute of Medicine
The National Academy of Medicine (NAM), formerly called the Institute of Medicine (IoM) until 2015, is an American nonprofit, non-governmental organization. The National Academy of Medicine is a part of the National Academies of Sciences, E ...
.
* Annual and lifetime coverage caps on essential benefits were banned.
* Insurers are forbidden from dropping
policyholder
Insurance is a means of protection from financial loss in which, in exchange for a fee, a party agrees to compensate another party in the event of a certain loss, damage, or injury. It is a form of risk management, primarily used to hedge ...
s when they become ill.
* All policies must provide an annual maximum out-of-pocket (MOOP) payment cap for an individual's or family's medical expenses (excluding premiums). After the MOOP payment is reached, all remaining costs must be paid by the insurer.
* Preventive care, vaccinations and medical screenings cannot be subject to
co-payments,
co-insurance
In insurance, co-insurance or coinsurance is the splitting or spreading of risk among multiple parties.
In the United States
In the U.S. insurance market, co-insurance is the joint assumption of risk between the insurer and the insured. In title i ...
or
deductibles.
Specific examples of covered services include:
mammograms
Mammography (also called mastography) is the process of using low-energy X-rays (usually around 30 kVp) to examine the human breast for diagnosis and screening. The goal of mammography is the early detection of breast cancer, typically through d ...
and
colonoscopies
Colonoscopy () or coloscopy () is the endoscopic examination of the large bowel and the distal part of the small bowel with a CCD camera or a fiber optic camera on a flexible tube passed through the anus. It can provide a visual diagnosis (''e.g ...
, wellness visits,
gestational diabetes
Gestational diabetes is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy. Gestational diabetes generally results in few symptoms; however, it increases the risk of pre-eclampsia, depression, and of ...
screening,
HPV
Human papillomavirus infection (HPV infection) is caused by a DNA virus from the '' Papillomaviridae'' family. Many HPV infections cause no symptoms and 90% resolve spontaneously within two years. In some cases, an HPV infection persists and re ...
testing,
STI counseling,
HIV
The human immunodeficiency viruses (HIV) are two species of ''Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immune ...
screening and counseling, contraceptive methods, breastfeeding support/supplies and
domestic violence
Domestic violence (also known as domestic abuse or family violence) is violence or other abuse that occurs in a domestic setting, such as in a marriage or cohabitation. ''Domestic violence'' is often used as a synonym for ''intimate partner ...
screening and counseling.
* The law established four tiers of coverage: bronze, silver, gold and platinum. All categories offer essential health benefits. The categories vary in their division of premiums and out-of-pocket costs: bronze plans have the lowest monthly premiums and highest out-of-pocket costs, while platinum plans are the reverse.
The percentages of
health care costs
Health, according to the World Health Organization, is "a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity".World Health Organization. (2006)''Constitution of the World Health Organiza ...
that plans are expected to cover through premiums (as opposed to out-of-pocket costs) are, on average: 60% (bronze), 70% (silver), 80% (gold), and 90% (platinum).
* Insurers are required to implement an
appeal
In law, an appeal is the process in which cases are reviewed by a higher authority, where parties request a formal change to an official decision. Appeals function both as a process for error correction as well as a process of clarifying and ...
s process for coverage determination and claims on all new plans.
* Insurers must
spend at least 80–85% of premium dollars on health costs; rebates must be issued if this is violated.
Individual mandate
The
individual mandate
An individual mandate is a requirement by law for certain persons to purchase or otherwise obtain a good or service.
United States Militia act
The Militia Acts of 1792, based on the Constitution's militia clause (in addition to its affirmative ...
required everyone to have insurance or
pay a penalty. The mandate and limits on open enrollment
were designed to avoid the
insurance death spiral, minimize the
free rider problem
In the social sciences, the free-rider problem is a type of market failure that occurs when those who benefit from resources, public goods (such as public roads or public library), or services of a communal nature do not pay for them or under-p ...
and prevent the healthcare system from succumbing to
adverse selection
In economics, insurance, and risk management, adverse selection is a market situation where buyers and sellers have different information. The result is that participants with key information might participate selectively in trades at the expe ...
.
The mandate was intended to increase the size and diversity of the insured population, including more young and healthy participants to broaden the
risk pool A “Risk pool” is a form of risk management that is mostly practiced by insurance companies, which come together to form a pool to provide protection to insurance companies against catastrophic risks such as floods or earthquakes. The term is als ...
, spreading costs.
Among the groups who were not subject to the individual mandate are:
*
Illegal immigrants
Illegal immigration is the migration of people into a country in violation of the immigration laws of that country or the continued residence without the legal right to live in that country. Illegal immigration tends to be financially upwa ...
, estimated at 8million—or roughly a third of the 23 million projection—are ineligible for insurance
subsidies
A subsidy or government incentive is a form of financial aid or support extended to an economic sector (business, or individual) generally with the aim of promoting economic and social policy. Although commonly extended from the government, the ter ...
and Medicaid.
They remain eligible for emergency services.
* Medicaid-eligible citizens not enrolled in Medicaid.
* Citizens whose insurance coverage would cost more than 8% of household income.
* Citizens who live in
states that opt-out of Medicaid expansion and who qualify for neither existing Medicaid coverage nor subsidized coverage.
The
Tax Cuts and Jobs Act of 2017
The Act to provide for reconciliation pursuant to titles II and V of the concurrent resolution on the budget for fiscal year 2018, , is a congressional revenue act of the United States originally introduced in Congress as the Tax Cuts and Jobs A ...
,
reduced to 0 the fine/tax for violating the individual mandate, starting in 2019.
Exchanges
ACA mandated that health insurance exchanges be provided for each state. The exchanges are regulated, largely online marketplaces, administered by either federal or state governments, where individuals, families and small businesses can purchase private insurance plans.
Exchanges first offered insurance for 2014. Some exchanges also provide access to Medicaid.
States that set up their own exchanges have some discretion on standards and prices.
For example, states approve plans for sale, and thereby influence (through negotiations) prices. They can impose additional coverage requirements—such as abortion. Alternatively, states can make the federal government responsible for operating their exchanges.
Premium subsidies
Individuals whose household incomes are between 100% and 400% of the
federal poverty level
In the United States, poverty has both social and political implications. In 2020, there were 37.2 million people in poverty. Some of the many causes include income inequality, inflation, unemployment, debt traps and poor education.Western, B ...
(FPL) are eligible to receive
federal subsidies for premiums for policies purchased on an ACA exchange, provided they are not eligible for
Medicare,
Medicaid
Medicaid in the United States is a federal and state program that helps with healthcare costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and pers ...
, the
Children's Health Insurance Program
The Children's Health Insurance Program (CHIP) – formerly known as the State Children's Health Insurance Program (SCHIP) – is a program administered by the United States Department of Health and Human Services that provides matching funds to ...
, or other forms of public assistance health coverage, and do not have access to affordable coverage (no more than 9.86% of income for the employee's coverage) through their own or a family member's employer.
Households below the federal poverty level are not eligible to receive these subsidies. Lawful Residents and some other legally present immigrants whose household income is below 100% FPL and are not otherwise eligible for Medicaid are eligible for subsidies if they meet all other eligibility requirements.
Married people must file taxes jointly to receive subsidies. Enrollees must have U.S. citizenship or proof of legal residency to obtain a subsidy.
The subsidies for an ACA plan purchased on an exchange stop at 400% of the federal poverty level (FPL). According to the Kaiser Foundation, this results in a sharp "discontinuity of treatment" at 400% FPL, which is sometimes called the "subsidy cliff". After-subsidy premiums for the second lowest cost silver plan (SCLSP) just below the cliff are 9.86% of income in 2019.
Subsidies are provided as an advanceable,
refundable tax credit
A tax credit is a tax incentive which allows certain taxpayers to subtract the amount of the credit they have accrued from the total they owe the state. It may also be a credit granted in recognition of taxes already paid or a form of state "disc ...
.
The amount of subsidy is sufficient to reduce the premium for the second-lowest-cost silver plan (SCLSP) on an exchange cost a sliding-scale percentage of income. The percentage is based on the percent of federal poverty level (FPL) for the household, and varies slightly from year to year. In 2019, it ranged from 2.08% of income (100%-133% FPL) to 9.86% of income (300%-400% FPL).
The subsidy can be used for any plan available on the exchange, but not catastrophic plans. The subsidy may not exceed the premium for the purchased plan.
(In this section, the term "income" refers to modified
adjusted gross income
In the United States income tax system, adjusted gross income (AGI) is an individual's total gross income minus specific deductions. It is used to calculate taxable income, which is AGI minus allowances for personal exemptions and itemized deduc ...
.
)
Small businesses are eligible for a tax credit provided they enroll in the
SHOP
Shop or shopping refers to:
Business and commerce
* A casual word for a commercial establishment or for a place of business
* Machine shop, a workshop for machining
*"In the shop", referring to a car being at an automotive repair shop
*A wood s ...
Marketplace.
Cost-sharing reduction subsidies
As written, ACA mandated that insurers reduce copayments and deductibles for ACA exchange enrollees earning less than 250% of the FPL. Medicaid recipients were not eligible for the reductions.
So-called cost-sharing reduction (CSR) subsidies were to be paid to insurance companies to fund the reductions. During 2017, approximately $7 billion in CSR subsidies were to be paid, versus $34 billion for premium tax credits.
The latter was defined as
mandatory spending
The United States federal budget is divided into three categories: mandatory spending, discretionary spending, and interest on debt. Also known as entitlement spending, in US fiscal policy, mandatory spending is government spending on certain p ...
that does not require an annual Congressional appropriation. CSR payments were not explicitly defined as mandatory. This led to litigation and disruption later.
Risk management
ACA implemented multiple approaches to helping mitigate the disruptions to insurers that came with its many changes.
Risk corridors
The risk-corridor program was a temporary risk management device. It was intended to encourage reluctant insurers into ACA insurance market from 2014 to 2016. For those years the
Department of Health and Human Services
The United States Department of Health and Human Services (HHS) is a cabinet-level executive branch department of the U.S. federal government created to protect the health of all Americans and providing essential human services. Its motto is " ...
(DHHS) would cover some of the losses for insurers whose plans performed worse than they expected. Loss-making insurers would receive payments paid for in part by profit-making insurers. Similar risk corridors had been established for the
Medicare prescription drug benefit.
Many insurers initially offered exchange plans. However, the program did not pay for itself as planned, losing up to $8.3 billion for 2014 and 2015. Authorization had to be given so DHHS could pay insurers from "general government revenues". However, the
Consolidated Appropriations Act, 2014
The Consolidated Appropriations Act, 2014 (, nicknamed the Cromnibus) is an omnibus spending bill that packages several appropriation bills together in one larger bill. The 113th United States Congress failed to pass any of the twelve regular ...
(H.R. 3547) stated that no funds "could be used for risk-corridor payments". leaving the government in a potential breach of contract with insurers who offered qualified health plans.
Several insurers sued the government at the
United States Court of Federal Claims
The United States Court of Federal Claims (in case citations, Fed. Cl. or C.F.C.) is a United States federal court that hears monetary claims against the U.S. government. It was established by statute in 1982 as the United States Claims Court, ...
to recover the funds believed owed to them under the Risk Corridors program. While several were summarily closed, in the case of ''
Moda Health
Moda Health (formerly ODS Health) is a health insurance company based in Portland, Oregon. The company provides medical and dental insurance in Oregon, Alaska and Texas (and in Washington state before 2016). The Moda Center, a sports arena that is ...
v the United States'', Moda Health won a $214-million judgment in February 2017. Federal Claims judge
Thomas C. Wheeler
Thomas Craig Wheeler (born March 18, 1948) is a Senior status, Senior Federal tribunals in the United States#Article I tribunals, judge of the United States Court of Federal Claims, appointed to that court in 2005 by President George W. Bush.
Ea ...
stated, "the Government made a promise in the risk corridors program that it has yet to fulfill. Today, the court directs the Government to fulfill that promise. After all, to say to
oda 'The joke is on you. You shouldn't have trusted us,' is hardly worthy of our great government." Moda Health's case was appealed by the government to the
United States Court of Appeals for the Federal Circuit
The United States Court of Appeals for the Federal Circuit (in case citations, Fed. Cir. or C.A.F.C.) is a United States court of appeals that has special appellate jurisdiction over certain types of specialized cases in the Federal judiciary of ...
along with the appeals of the other insurers; here, the Federal Circuit reversed the Moda Health ruling and ruled across all the cases in favor of the government, that the appropriations riders ceded the government from paying out remain money due to the insurers. The Supreme Court reversed this ruling in the consolidated case, ''
Maine Community Health Options v. United States
''Maine Community Health Options v. United States'', 590 U.S. ___ (2020), was a United States Supreme Court case involving the expired Risk Corridors program of the Patient Protection and Affordable Care Act (ACA), through which the Department of ...
'', reaffirming as with Judge Wheeler that the government had a responsibility to pay those funds under the ACA and the use of riders to de-obligate its from those payments was illegal.
Reinsurance
The temporary reinsurance program is meant to stabilize premiums by reducing the incentive for insurers to raise premiums due to concerns about higher-risk enrollees. Reinsurance was based on retrospective costs rather than prospective risk evaluations. Reinsurance was available from 2014 through 2016.
Risk adjustment
Risk adjustment involves transferring funds from plans with lower-risk enrollees to plans with higher-risk enrollees. It was intended to encourage insurers to compete based on value and efficiency rather than by attracting healthier enrollees. Of the three risk management programs, only risk adjustment was permanent. Plans with low actuarial risk compensate plans with high actuarial risk.
Medicaid expansion
ACA revised and expanded
Medicaid
Medicaid in the United States is a federal and state program that helps with healthcare costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and pers ...
eligibility starting in 2014. All U.S. citizens and legal residents with income up to 133% of the
poverty line
The poverty threshold, poverty limit, poverty line or breadline is the minimum level of income deemed adequate in a particular country. The poverty line is usually calculated by estimating the total cost of one year's worth of necessities for t ...
, including adults without dependent children, would qualify for coverage in any state that participated in the Medicaid program. The federal government was to pay 100% of the increased cost in 2014, 2015 and 2016; 95% in 2017, 94% in 2018, 93% in 2019, and 90% in 2020 and all subsequent years. A 5% "income disregard" made the effective income eligibility limit for Medicaid 138% of the poverty level.
However, the
Supreme Court
A supreme court is the highest court within the hierarchy of courts in most legal jurisdictions. Other descriptions for such courts include court of last resort, apex court, and high (or final) court of appeal. Broadly speaking, the decisions of ...
ruled in ''
NFIB v. Sebelius'' that this provision of ACA was coercive, and that states could choose to continue at pre-ACA eligibility levels.
Medicare savings
Medicare reimbursements were reduced to insurers and drug companies for private
Medicare Advantage
Medicare Advantage (Medicare Part C, MA) is a capitated program for providing Medicare benefits in the United States. Under Part C, Medicare pays a private-sector health insurer a fixed payment. The insurer then pays for the health care expenses ...
policies that the
Government Accountability Office
The U.S. Government Accountability Office (GAO) is a legislative branch government agency that provides auditing, evaluative, and investigative services for the United States Congress. It is the supreme audit institution of the federal govern ...
and
Medicare Payment Advisory Commission
The Medicare Payment Advisory Commission (MedPAC) is an independent, non-partisan legislative branch agency headquartered in Washington, D.C. MedPAC was established by the Balanced Budget Act of 1997 (P.L. 105–33). The BBA formed MedPAC by merg ...
found to be excessively costly relative to standard Medicare;
and to hospitals that failed standards of efficiency and care.
Taxes
Medicare taxes
Income from self-employment and wages of single individuals in excess of $200,000 annually are subjected to an additional tax of 0.9%. The threshold amount is $250,000 for a married couple filing jointly (threshold applies to their total compensation), or $125,000 for a married person filing separately.
In ACA's companion legislation, the
Health Care and Education Reconciliation Act of 2010
The Health Care and Education Reconciliation Act of 2010 (, ) is a law that was enacted by the 111th United States Congress, by means of the reconciliation process, in order to amend the Affordable Care Act (ACA) (). The law includes the St ...
, an additional tax of 3.8% was applied to unearned income, specifically the lesser of net investment income and the amount by which adjusted gross income exceeds the above income limits.
Excise taxes
ACA included an excise tax of 40% ("
Cadillac tax
Informally, a Cadillac plan is any unusually expensive health insurance plan, usually arising in discussions of medical-cost control measures in the United States. The term derives from the Cadillac automobile, which has represented American luxury ...
") on total employer premium spending in excess of specified dollar amounts (initially $10,200 for single coverage and $27,500 for family coverage) indexed to inflation. This tax was originally scheduled to take effect in 2018, but was delayed until 2020 by the
Consolidated Appropriations Act, 2016
The Consolidated Appropriations Act, 2016 (, ), also known as the 2016 omnibus spending bill, is the United States appropriations legislation passed during the 114th Congress which provides spending permission to a number of federal agencies for ...
and again to 2022. Excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs. An excise tax of 2.3% on medical devices and a 10% excise tax on indoor tanning services were applied as well. The tax was repealed in late 2019.
SCHIP
The
State Children's Health Insurance Program
The Children's Health Insurance Program (CHIP) – formerly known as the State Children's Health Insurance Program (SCHIP) – is a program administered by the United States Department of Health and Human Services that provides matching funds to ...
(CHIP) enrollment process was simplified.
Dependents
Dependents were permitted to remain on their parents' insurance plan until their 26th birthday, including dependents who no longer lived with their parents, are not a dependent on a parent's tax return, are no longer a student, or are married.
Employer mandate
Businesses that employ fifty or more people but do not offer health insurance to their full-time employees are assessed additional tax if the government has subsidized a full-time employee's healthcare through tax deductions or other means. This is commonly known as the
employer mandate
A health insurance mandate is either an employer or individual mandate to obtain private health insurance instead of (or in addition to) a national health insurance plan.D. Andrew Austin, Thomas L. Hungerford (2010). Market Structure of the ...
.
This provision was included to encourage employers to continue providing insurance once the exchanges began operating.
Delivery system reforms
The act includes
delivery system reforms intended to constrain costs and improve quality. These include Medicare payment changes to discourage
hospital-acquired condition
A hospital-acquired condition (HAC) is an undesirable situation or condition that affects a patient and that arose during a stay in a hospital or medical facility. It is a designation used by Medicare/Medicaid in the US for determining MS-DRG re ...
s and
readmissions,
bundled payment Bundled payment is the reimbursement of health care providers (such as hospitals and physicians) "on the basis of expected costs for defined episodes of care." It has been described as "a middle ground" between fee-for-service reimbursement (in wh ...
initiatives, the
Center for Medicare and Medicaid Innovation The Center for Medicare and Medicaid Innovation (CMMI; also known as the CMS Innovation Center) is an organization of the United States government under the Centers for Medicare and Medicaid Services (CMS). It was created by the Patient Protection a ...
, the
Independent Payment Advisory Board
The Independent Payment Advisory Board, or IPAB, was to be a fifteen-member United States Government agency created in 2010 by sections 3403 and 10320 of the Patient Protection and Affordable Care Act which was to have the explicit task of achiev ...
, and
accountable care organization
An accountable care organization (ACO) is a healthcare organization that ties provider reimbursements to quality metrics and reductions in the cost of care. ACOs in the United States are formed from a group of coordinated health-care practitione ...
s.
Hospital quality
Health care cost/quality initiatives included incentives to
reduce hospital infections, adopt
electronic medical record
An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared throu ...
s, and to coordinate care and prioritize quality over quantity.
Bundled payments
Medicare switched from
fee-for-service to
bundled payment Bundled payment is the reimbursement of health care providers (such as hospitals and physicians) "on the basis of expected costs for defined episodes of care." It has been described as "a middle ground" between fee-for-service reimbursement (in wh ...
s. A single payment was to be paid to a hospital and a physician group for a defined episode of care (such as a
hip replacement
Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi (half) replacement. Such joint replacement o ...
) rather than separate payments to individual service providers.
Accountable care organizations
The
Medicare Shared Savings Program (MSSP) was established by section 3022 of the Affordable Care Act. It is the program by which an
accountable care organization
An accountable care organization (ACO) is a healthcare organization that ties provider reimbursements to quality metrics and reductions in the cost of care. ACOs in the United States are formed from a group of coordinated health-care practitione ...
interacts with the federal government, and by which accountable care organizations can be created. It is a
fee-for-service model.
The Act allowed the creation of accountable care organizations (ACOs), which are groups of doctors, hospitals and other providers that commit to give coordinated care to Medicare patients. ACOs were allowed to continue using
fee-for-service billing. They receive bonus payments from the government for minimizing costs while achieving quality benchmarks that emphasize prevention and mitigation of
chronic disease
A chronic condition is a health condition or disease that is persistent or otherwise long-lasting in its effects or a disease that comes with time. The term ''chronic'' is often applied when the course of the disease lasts for more than three mo ...
. Missing cost or quality benchmarks subjected them to penalties.
Unlike
health maintenance organization
In the United States, a health maintenance organization (HMO) is a medical insurance group that provides health services for a fixed annual fee. It is an organization that provides or arranges managed care for health insurance, self-funded healt ...
s, ACO patients are not required to obtain all care from the ACO. Also, unlike HMOs, ACOs must achieve quality-of-care goals.
Medicare drug benefit (Part D)
Medicare Part D participants received a 50% discount on brand name drugs purchased after exhausting their
initial coverage and before reaching the catastrophic-coverage threshold. By 2020, the "doughnut hole" would be completely filled.
State waivers
From 2017 onwards, states can apply for a "waiver for state innovation" which allows them to conduct experiments that meet certain criteria.
To obtain a waiver, a state must pass legislation setting up an alternative health system that provides insurance at least as comprehensive and as affordable as ACA, covers at least as many residents and does not increase the federal deficit.
These states can escape some of ACA's central requirements, including the individual and employer mandates and the provision of an insurance exchange.
The state would receive compensation equal to the aggregate amount of any federal subsidies and tax credits for which its residents and employers would have been eligible under ACA, if they cannot be paid under the state plan.
Other insurance provisions
The
Community Living Assistance Services and Supports Act
The Community Living Assistance Services and Supports Act (or CLASS Act) was a U.S. federal law, enacted as Title VIII of the Patient Protection and Affordable Care Act. The CLASS Act would have created a voluntary and public long-term care insura ...
(or CLASS Act) established a voluntary and public
long-term care insurance
Long-term care insurance (LTC or LTCI) is an insurance product, sold in the United States, United Kingdom and Canada that helps pay for the costs associated with long-term care. Long-term care insurance covers care generally not covered by health ...
option for employees,
The program was abolished as impractical without ever having taken effect.
Consumer Operated and Oriented Plans (CO-OP), member-governed non-profit insurers, could start providing health care coverage, based on a 5-year federal loan. As of 2017, only four of the original 23 co-ops were still in operation.
Nutrition labeling requirements
Nutrition labeling requirements officially took effect in 2010, but implementation was delayed, and they actually took effect on May 7, 2018.
Legislative history

ACA followed a long series of unsuccessful attempts by one party or the other to pass major insurance reforms. Innovations were limited to
health savings account
A health savings account (HSA) is a tax-advantaged medical savings account available to taxpayers in the United States who are enrolled in a high-deductible health plan (HDHP). The funds contributed to an account are not subject to federal inco ...
s (2003),
medical savings accounts (1996) or
flexible spending account
In the United States, a flexible spending account (FSA), also known as a flexible spending arrangement, is one of a number of tax-advantaged financial accounts, resulting in payroll tax savings. One significant disadvantage to using an FSA is th ...
s, which increased insurance options, but did not materially expand coverage. Health care was a major factor in multiple elections, but until 2009, neither party had the votes to overcome the other's opposition.
Individual mandate
The concept of an individual mandate goes back to at least 1989, when
The Heritage Foundation
The Heritage Foundation (abbreviated to Heritage) is an American conservative think tank based in Washington, D.C. that is primarily geared toward public policy. The foundation took a leading role in the conservative movement during the presiden ...
, a
conservative
Conservatism is a cultural, social, and political philosophy that seeks to promote and to preserve traditional institutions, practices, and values. The central tenets of conservatism may vary in relation to the culture and civilization i ...
think-tank, proposed an individual mandate as an alternative to
single-payer health care.
It was championed for a time by conservative economists and
Republican
Republican can refer to:
Political ideology
* An advocate of a republic, a type of government that is not a monarchy or dictatorship, and is usually associated with the rule of law.
** Republicanism, the ideology in support of republics or agains ...
senators as a market-based approach to healthcare reform on the basis of individual responsibility and avoidance of
free rider problem
In the social sciences, the free-rider problem is a type of market failure that occurs when those who benefit from resources, public goods (such as public roads or public library), or services of a communal nature do not pay for them or under-p ...
s. Specifically, because the 1986
Emergency Medical Treatment and Active Labor Act The Emergency Medical Treatment and Active Labor Act (EMTALA) is an act of the United States Congress, passed in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA). It requires hospital emergency departments that accept paym ...
(EMTALA) requires any hospital participating in Medicare (nearly all do) to provide emergency care to anyone who needs it, the government often indirectly bore the cost of those without the ability to pay.
President
Bill Clinton
William Jefferson Clinton ( né Blythe III; born August 19, 1946) is an American politician who served as the 42nd president of the United States from 1993 to 2001. He previously served as governor of Arkansas from 1979 to 1981 and agai ...
proposed a major healthcare reform bill in 1993
that ultimately failed. Clinton negotiated a compromise with the
105th Congress to instead enact the
State Children's Health Insurance Program (SCHIP) in 1997. The failed Clinton plan included a mandate for employers to provide health insurance to all employees through a regulated marketplace of
health maintenance organization
In the United States, a health maintenance organization (HMO) is a medical insurance group that provides health services for a fixed annual fee. It is an organization that provides or arranges managed care for health insurance, self-funded healt ...
s. Republican senators proposed an alternative that would have required individuals, but not employers, to buy insurance.

The 1993 Republican
Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'.
Advocates included prominent Republican senators such as
John Chafee
John Lester Hubbard Chafee ( ; October 22, 1922 – October 24, 1999) was an American politician and officer in the United States Marine Corps. A member of the Republican Party (United States), he served as the 66th Governor of Rhode Island, as ...
,
Orrin Hatch
Orrin Grant Hatch (March 22, 1934 – April 23, 2022) was an American attorney and politician who served as a United States senator from Utah from 1977 to 2019. Hatch's 42-year Senate tenure made him the longest-serving Republican U.S. senator ...
,
Chuck Grassley
Charles Ernest Grassley (born September 17, 1933) is an American politician serving as the president pro tempore emeritus of the United States Senate, and the Seniority in the United States Senate, senior United States Senate, United States sen ...
,
Bob Bennett and
Kit Bond
Christopher Samuel "Kit" Bond (born March 6, 1939) is an American attorney, politician and former United States Senator from Missouri and a member of the Republican Party. First elected to the U.S. Senate in 1986, he defeated Democrat Harriett W ...
. The 1994 Republican Consumer Choice Health Security Act, initially contained an individual mandate with a penalty provision; however, author
Don Nickles
Donald Lee Nickles (born December 6, 1948) is an American politician and lobbyist who was a Republican United States Senator from Oklahoma from 1981 to 2005. He was considered both a fiscal and social conservative. After retiring from the Senat ...
subsequently removed the mandate, stating, "government should not compel people to buy health insurance". At the time of these proposals, Republicans did not raise constitutional issues; Mark Pauly, who helped develop a proposal that included an individual mandate for
George H. W. Bush
George Herbert Walker BushSince around 2000, he has been usually called George H. W. Bush, Bush Senior, Bush 41 or Bush the Elder to distinguish him from his eldest son, George W. Bush, who served as the 43rd president from 2001 to 2009; pr ...
, remarked, "I don't remember that being raised at all. The way it was viewed by the Congressional Budget Office in 1994 was, effectively, as a tax."

In 2006,
an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an
insurance exchange. Republican Governor
Mitt Romney
Willard Mitt Romney (born March 12, 1947) is an American politician, businessman, and lawyer serving as the junior United States senator from Utah since January 2019, succeeding Orrin Hatch. He served as the 70th governor of Massachusetts f ...
vetoed the mandate, but after Democrats overrode his veto, he signed it into law.
Romney's implementation of the
'Health Connector' exchange and individual mandate in Massachusetts was at first lauded by Republicans. During
Romney's 2008 presidential campaign, Senator
Jim DeMint
James Warren DeMint (born September 2, 1951) is an American political advocate, businessman, author, and retired politician who served as a United States Senator from South Carolina and as president of the Heritage Foundation. DeMint is a member ...
praised Romney's ability to "take some good conservative ideas, like private health insurance, and apply them to the need to have everyone insured". Romney said of the individual mandate: "I'm proud of what we've done. If Massachusetts succeeds in implementing it, then that will be the model for the nation."
In 2007 Republican Senator
Bob Bennett and Democratic Senator
Ron Wyden
Ronald Lee Wyden (; born May 3, 1949) is an American politician and retired educator serving as the Seniority in the United States Senate, senior United States Senate, United States senator from Oregon, a seat he has held since 1996 United Stat ...
introduced the
Healthy Americans Act
The Healthy Americans Act (HAA), also known as the Wyden-Bennett Act, is a Senate bill that had proposed to improve health care in the United States, with changes that included the establishment of universal health care. It would transition a ...
, which featured an individual mandate and state-based,
regulated insurance markets called "State Health Help Agencies".
The bill attracted bipartisan support, but died in committee. Many of its
sponsors and co-sponsors remained in Congress during the 2008 healthcare debate.
By 2008 many Democrats were considering this approach as the basis for healthcare reform. Experts said the legislation that eventually emerged from Congress in 2009 and 2010 bore similarities to the 2007 bill
and that it took ideas from the Massachusetts reforms.
Academic foundation
A driving force behind Obama's healthcare reform was
Peter Orszag
Peter Richard Orszag (born December 16, 1968) is the CEO of Financial Advisory at Lazard. Before June 2019, he was the firm's Head of North American M&A and Global Co-Head of Healthcare.
Orszag previously served as a Vice Chairman of Corporate ...
, Director of the
Office of Management and Budget
The Office of Management and Budget (OMB) is the largest office within the Executive Office of the President of the United States (EOP). OMB's most prominent function is to produce the president's budget, but it also examines agency programs, pol ...
. Obama called Orszag his "healthcare czar" because of his knowledge of healthcare reform. Orszag had previously been director of the
Congressional Budget Office
The Congressional Budget Office (CBO) is a federal agency within the legislative branch of the United States government that provides budget and economic information to Congress.
Inspired by California's Legislative Analyst's Office that manages ...
, and under his leadership the agency had focused on using cost analysis to create an affordable and effective approach to health care reform. Orszag claimed that healthcare reform became Obama's top agenda item because he wanted it to be his legacy. According to an article by Ryan Lizza in ''The New Yorker'', the core of "the Obama budget is Orszag's belief
n..a government empowered with research on the most effective medical treatments". Obama bet "his presidency on Orszag's thesis of comparative effectiveness." Orszag's policies were influenced by an article in ''The Annals of Internal Medicine'' co-authored by Elliott S. Fisher, David Wennberg and others. The article presented strong evidence based on the co-authors' research that numerous procedures, therapies and tests were being delivered with scant evidence of their medical value. If those procedures and tests could be eliminated, this evidence suggested, medical costs might provide the savings to give healthcare to the uninsured population. After reading a ''The New Yorker'' article that used the "Dartmouth findings" to compare two counties in Texas with enormous variations in Medicare costs using hard data, Obama directed that his entire staff read it. More than anything else, the Dartmouth data intrigued Obama since it gave him an academic rationale for reshaping medicine.
The concept of comparing the effectiveness of healthcare options based on hard data ("comparative effectiveness" and "evidence-based medicine") was pioneered by John E. Wennberg, founder of
The Dartmouth Institute, co-founder of The Foundation for Informed Medical Decision Making and senior advisor to Health Dialog Inc., a venture that he and his researchers created to help insurers implement the Dartmouth findings.
Healthcare debate, 2008–10
Healthcare reform was a major topic during the
2008 Democratic presidential primaries. As the race narrowed, attention focused on the plans presented by the two leading candidates,
Hillary Clinton
Hillary Diane Rodham Clinton ( Rodham; born October 26, 1947) is an American politician, diplomat, and former lawyer who served as the 67th United States Secretary of State for President Barack Obama from 2009 to 2013, as a United States sen ...
and the eventual nominee,
Barack Obama
Barack Hussein Obama II ( ; born August 4, 1961) is an American politician who served as the 44th president of the United States from 2009 to 2017. A member of the Democratic Party, Obama was the first African-American president of the U ...
. Each candidate proposed a plan to cover the approximately 45 million Americans estimated to not have health insurance at some point each year. Clinton's proposal would have required all Americans to obtain coverage (in effect, an individual mandate), while Obama's proposal provided a
subsidy
A subsidy or government incentive is a form of financial aid or support extended to an economic sector (business, or individual) generally with the aim of promoting economic and social policy. Although commonly extended from the government, the ter ...
without a mandate.
During the
general election
A general election is a political voting election where generally all or most members of a given political body are chosen. These are usually held for a nation, state, or territory's primary legislative body, and are different from by-elections ( ...
, Obama said fixing healthcare would be one of his top four priorities as president.
Obama and his opponent, Senator
John McCain
John Sidney McCain III (August 29, 1936 – August 25, 2018) was an American politician and United States Navy officer who served as a United States senator from Arizona from 1987 until his death in 2018. He previously served two terms ...
, both proposed health insurance reforms, though their plans differed. McCain proposed tax credits for health insurance purchased in the individual market, which was estimated to reduce the number of uninsured people by about 2million by 2018. Obama proposed private and public group insurance, income-based subsidies, consumer protections, and expansions of Medicaid and SCHIP, which was estimated at the time to reduce the number of uninsured people by 33.9 million by 2018 at a higher cost.

Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform.
By July, a series of bills were approved by committees within the
House of Representatives
House of Representatives is the name of legislative bodies in many countries and sub-national entitles. In many countries, the House of Representatives is the lower house of a bicameral legislature, with the corresponding upper house often c ...
.
On the Senate side, from June to September, the
Senate Finance Committee
The United States Senate Committee on Finance (or, less formally, Senate Finance Committee) is a standing committee of the United States Senate. The Committee concerns itself with matters relating to taxation and other revenue measures generall ...
held a series of 31 meetings to develop a proposal. This group—in particular, Democrats
Max Baucus
Maxwell Sieben Baucus ( Enke; born December 11, 1941) is an American politician who served as a United States senator from Montana from 1978 to 2014. A member of the Democratic Party, he was a U.S. senator for over 35 years, making him the longe ...
,
Jeff Bingaman
Jesse Francis "Jeff" Bingaman Jr. (born October 3, 1943) is an American politician who served as a United States Senator from New Mexico from 1983 to 2013, for 5 terms. A member of the Democratic Party, he served as Chairman of Committee Outreac ...
and
Kent Conrad
Gaylord Kent Conrad (born March 12, 1948) is a former American politician who was a United States Senator from North Dakota. He is a member of the North Dakota Democratic-NPL Party, the North Dakota affiliate of the Democratic Party. First elec ...
, along with Republicans
Mike Enzi
Michael Bradley Enzi ( ; February 1, 1944 – July 26, 2021) was an American politician who served in the United States Senate from Wyoming as a member of the Republican Party from 1997 to 2021. Prior to his tenure in the United States Senate h ...
,
Chuck Grassley
Charles Ernest Grassley (born September 17, 1933) is an American politician serving as the president pro tempore emeritus of the United States Senate, and the Seniority in the United States Senate, senior United States Senate, United States sen ...
and
Olympia Snowe
Olympia Jean Snowe (; born February 21, 1947) is an American businesswoman and politician who was a United States Senator from Maine from 1995 to 2013. Snowe, a member of the Republican Party, became known for her ability to influence the outcom ...
—met for more than 60 hours, and the principles they discussed, in conjunction with the other committees, became the foundation of a Senate bill.
Congressional Democrats and health policy experts, such as
MIT
The Massachusetts Institute of Technology (MIT) is a private land-grant research university in Cambridge, Massachusetts. Established in 1861, MIT has played a key role in the development of modern technology and science, and is one of the m ...
economics professor
Jonathan Gruber and
David Cutler
David Matthew Cutler (born June 22, 1965) is the Otto Eckstein Professor of Applied Economics at Harvard University. He was given a five-year term appointment of Harvard College Professor, which recognizes excellence in undergraduate teaching. H ...
, argued that
guaranteed issue Guaranteed issue is a term used in health insurance to describe a situation where a policy is offered to any eligible applicant without regard to health status. Often this is the result of guaranteed issue statutes regarding how health insurance ma ...
would require both
community rating
Community rating is a concept usually associated with health insurance, which requires health insurance providers to offer health insurance policies within a given territory at the same price to all persons without medical underwriting, regardless ...
and an individual mandate to ensure that
adverse selection
In economics, insurance, and risk management, adverse selection is a market situation where buyers and sellers have different information. The result is that participants with key information might participate selectively in trades at the expe ...
and/or
"free riding" would not result in an
insurance "death spiral".
They chose this approach after concluding that
filibuster-proof support in the Senate was not present for more progressive plans such as
single-payer
Single-payer healthcare is a type of universal healthcare in which the costs of essential healthcare for all residents are covered by a single public system (hence "single-payer").
Single-payer systems may contract for healthcare services from ...
. By deliberately drawing on bipartisan ideas—the same basic outline was supported by former Senate Majority Leaders
Howard Baker
Howard Henry Baker Jr. (November 15, 1925 June 26, 2014) was an American politician and diplomat who served as a United States Senator from Tennessee from 1967 to 1985. During his tenure, he rose to the rank of Senate Minority Leader and then ...
,
Bob Dole
Robert Joseph Dole (July 22, 1923 – December 5, 2021) was an American politician and attorney who represented Kansas in the United States Senate from 1969 to 1996. He was the Republican Leader of the Senate during the final 11 years of his te ...
,
Tom Daschle and
George J. Mitchell
George John Mitchell Jr. (born August 20, 1933) is an American politician, diplomat, and lawyer. A leading member of the Democratic Party, he served as a United States senator from Maine from 1980 to 1995, and as Senate Majority Leader from 19 ...
—the bill's drafters hoped to garner the necessary votes.
However, following the incorporation of an individual mandate into the proposal, Republicans threatened to
filibuster
A filibuster is a political procedure in which one or more members of a legislative body prolong debate on proposed legislation so as to delay or entirely prevent decision. It is sometimes referred to as "talking a bill to death" or "talking out ...
any bill that contained it.
Senate Minority Leader
The positions of majority leader and minority leader are held by two United States senators and members of the party leadership of the United States Senate. They serve as the chief spokespersons for their respective political parties holding ...
Mitch McConnell
Addison Mitchell McConnell III (born February 20, 1942) is an American politician and retired attorney serving as the senior United States senator from Kentucky and the Senate minority leader since 2021. Currently in his seventh term, McConne ...
, who led the Republican response, concluded Republicans should not support the bill.
Republican senators, including those who had supported earlier proposals with a similar mandate, began to describe the mandate as "unconstitutional". Journalist
Ezra Klein
Ezra Klein (born May 10, 1984) is an American journalist, political analyst, ''New York Times'' columnist, and the host of ''The Ezra Klein Show'' podcast. He is a co-founder of '' Vox'' and formerly served as the website's editor-at-large. He h ...
wrote in ''
The New Yorker
''The New Yorker'' is an American weekly magazine featuring journalism, commentary, criticism, essays, fiction, satire, cartoons, and poetry. Founded as a weekly in 1925, the magazine is published 47 times annually, with five of these issues ...
'', "a policy that once enjoyed broad support within the Republican Party suddenly faced unified opposition."
The reform attracted attention from
lobbyists
In politics, lobbying, persuasion or interest representation is the act of lawfully attempting to influence the actions, policies, or decisions of government officials, most often legislators or members of regulatory agencies. Lobbying, whi ...
, including deals between lobby groups and the advocates to win the support of groups who had opposed past proposals.

During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals. The nascent
Tea Party movement
The Tea Party movement was an American fiscally conservative political movement within the Republican Party that began in 2009. Members of the movement called for lower taxes and for a reduction of the national debt and federal budget defic ...
organized protests and many
conservative
Conservatism is a cultural, social, and political philosophy that seeks to promote and to preserve traditional institutions, practices, and values. The central tenets of conservatism may vary in relation to the culture and civilization i ...
groups and individuals attended the meetings to oppose the proposed reforms.
Threats were made against members of Congress over the course of the debate.
In September 2009
Obama delivered another speech to a joint session of Congress supporting the negotiations.
On November 7, the House of Representatives passed the
Affordable Health Care for America Act
The Affordable Health Care for America Act (or HR 3962) was a bill that was crafted by the United States House of Representatives of the 111th United States Congress on October 29, 2009. The bill was sponsored by Representative Charles Rangel. ...
on a 220–215 vote and forwarded it to the Senate for passage.
Senate
The Senate began work on its own proposals while the House was still working. The
United States Constitution
The Constitution of the United States is the Supremacy Clause, supreme law of the United States, United States of America. It superseded the Articles of Confederation, the nation's first constitution, in 1789. Originally comprising seven ar ...
requires all revenue-related bills to originate in the House.
To formally comply with this requirement, the Senate repurposed H.R. 3590, a bill regarding housing tax changes for service members.
It had been passed by the House as a revenue-related modification to the
Internal Revenue Code
The Internal Revenue Code (IRC), formally the Internal Revenue Code of 1986, is the domestic portion of federal statutory tax law in the United States, published in various volumes of the United States Statutes at Large, and separately as Title 26 ...
. The bill became the Senate's vehicle for its healthcare reform proposal, discarding the bill's original content. The bill ultimately incorporated elements of proposals that were reported favorably by the Senate
Health
Health, according to the World Health Organization, is "a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity".World Health Organization. (2006)''Constitution of the World Health Organiza ...
and
Finance
Finance is the study and discipline of money, currency and capital assets. It is related to, but not synonymous with economics, the study of production, distribution, and consumption of money, assets, goods and services (the discipline of fina ...
committees. With the Republican Senate minority vowing to
filibuster
A filibuster is a political procedure in which one or more members of a legislative body prolong debate on proposed legislation so as to delay or entirely prevent decision. It is sometimes referred to as "talking a bill to death" or "talking out ...
, 60 votes would be necessary to pass the Senate. At the start of the
111th Congress, Democrats had 58 votes. The
Minnesota Senate election was ultimately won by Democrat
Al Franken
Alan Stuart Franken (born May 21, 1951) is an American comedian, politician, media personality, and author who served as a United States senator from Minnesota from 2009 to 2018. He gained fame as a writer and performer on the television comed ...
, making 59.
Arlen Specter
Arlen Specter (February 12, 1930 – October 14, 2012) was an American lawyer, author and politician who served as a United States Senator from Pennsylvania from 1981 to 2011. Specter was a Democrat from 1951 to 1965, then a Republican from ...
switched to the Democratic party in April 2009, giving them 60 seats, enough to end a filibuster.
Negotiations were undertaken attempting to satisfy moderate Democrats and to bring Republican senators aboard; particular attention was given to Republicans Bennett, Enzi, Grassley and Snowe.
After the Finance Committee vote on October 15, negotiations turned to moderate Democrats.
Senate Majority Leader
The positions of majority leader and minority leader are held by two United States senators and members of the party leadership of the United States Senate. They serve as the chief spokespersons for their respective political parties holding t ...
Harry Reid
Harry Mason Reid Jr. (; December 2, 1939 – December 28, 2021) was an American lawyer and politician who served as a United States senator from Nevada from 1987 to 2017. He led the Senate Democratic Caucus from 2005 to 2017 and was the Sena ...
focused on satisfying centrists. The holdouts came down to
Joe Lieberman
Joseph Isadore Lieberman (; born February 24, 1942) is an American politician, lobbyist, and attorney who served as a United States Senate, United States senator from Connecticut from 1989 to 2013. A former member of the Democratic Party (Uni ...
of Connecticut, an independent who caucused with Democrats, and conservative Nebraska Democrat
Ben Nelson
Earl Benjamin Nelson (born May 17, 1941) is an American attorney, businessman, and politician who served as the 37th governor of Nebraska from 1991 to 1999 and as a United States Senator from Nebraska from 2001 to 2013. He is a member of the De ...
. Lieberman's demand that the bill not include a
public option was met,
although supporters won various concessions, including allowing state-based public options such as Vermont's failed
Green Mountain Care
In 2011, the Vermont state government enacted a law functionally establishing the first state-level single-payer health care system in the United States. Green Mountain Care, established by the passage of H.202, creates a system in the state whe ...
.

The White House and Reid addressed Nelson's concerns during a 13-hour negotiation with two concessions: a compromise on
abortion
Abortion is the termination of a pregnancy by removal or expulsion of an embryo or fetus. An abortion that occurs without intervention is known as a miscarriage or "spontaneous abortion"; these occur in approximately 30% to 40% of pregn ...
, modifying the language of the bill "to give states the right to prohibit coverage of abortion within their own insurance exchanges", which would require consumers to pay for the procedure out of pocket if the state so decided; and an amendment to offer a higher rate of
Medicaid
Medicaid in the United States is a federal and state program that helps with healthcare costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and pers ...
reimbursement for Nebraska.
The latter half of the compromise was derisively termed the "Cornhusker Kickback" and was later removed.
On December 23, the Senate voted 60–39 to end debate on the bill: a
cloture vote to end the
filibuster
A filibuster is a political procedure in which one or more members of a legislative body prolong debate on proposed legislation so as to delay or entirely prevent decision. It is sometimes referred to as "talking a bill to death" or "talking out ...
. The bill then passed, also 60–39, on December 24, 2009, with all Democrats and two independents voting for it, and all Republicans against (except
Jim Bunning
James Paul David Bunning (October 23, 1931 – May 26, 2017) was an American professional baseball pitcher and politician who represented Kentucky in both chambers of the United States Congress. He was the sole Major League Baseball athlete to ha ...
, who did not vote).
The bill was endorsed by the
American Medical Association
The American Medical Association (AMA) is a professional association and lobbying group of physicians and medical students. Founded in 1847, it is headquartered in Chicago, Illinois. Membership was approximately 240,000 in 2016.
The AMA's state ...
and
AARP
AARP (formerly called the American Association of Retired Persons) is an interest group in the United States focusing on issues affecting those over the age of fifty. The organization said it had more than 38 million members in 2018. The magazin ...
.
On January 19, 2010,
Republican
Scott Brown Scott Brown may refer to:
Sportsmen
*Scott Brown (American football), American college football coach of Kentucky State
* Scott Brown (baseball) (born 1956), former Major League Baseball pitcher for the Cincinnati Reds
*Scott Brown (footballer, bor ...
was
elected to the Senate in a special election to replace the recently deceased
Ted Kennedy
Edward Moore Kennedy (February 22, 1932 – August 25, 2009) was an American lawyer and politician who served as a United States senator from Massachusetts for almost 47 years, from 1962 until his death in 2009. A member of the Democratic ...
, having campaigned on giving the Republican minority the 41st vote needed to sustain Republican filibusters.
Additionally, the symbolic importance of losing Kennedy's
traditionally Democratic Massachusetts seat made many Congressional Democrats concerned about the political cost of the bill.
House

With Democrats no longer able to get the 60 votes to break a filibuster in the Senate,
White House Chief of Staff Rahm Emanuel
Rahm Israel Emanuel (; born November 29, 1959) is an American politician and diplomat who is the current United States Ambassador to Japan. A member of the Democratic Party, he previously served two terms as the 55th Mayor of Chicago from 2011 ...
argued that Democrats should scale back to a less ambitious bill, but
House Speaker Nancy Pelosi
Nancy Patricia Pelosi (; ; born March 26, 1940) is an American politician who has served as Speaker of the United States House of Representatives since 2019 and previously from 2007 to 2011. She has represented in the United States House of ...
pushed back, dismissing more moderate reform as "Kiddie Care".
Obama remained insistent on comprehensive reform. The news that
Anthem
An anthem is a musical composition of celebration, usually used as a symbol for a distinct group, particularly the national anthems of countries. Originally, and in music theory and religious contexts, it also refers more particularly to short ...
in
California
California is a U.S. state, state in the Western United States, located along the West Coast of the United States, Pacific Coast. With nearly 39.2million residents across a total area of approximately , it is the List of states and territori ...
intended to raise premium rates for its patients by as much as 39% gave him new evidence of the need for reform.
On February 22, he laid out a "Senate-leaning" proposal to consolidate the bills. He held a meeting with both parties' leaders on February 25. The Democrats decided the House would pass the Senate's bill, to avoid another Senate vote.
House Democrats had expected to be able to negotiate changes
in a House–Senate conference before passing a final bill. Since any bill that emerged from conference that differed from the Senate bill would have to pass the Senate over another Republican filibuster, most House Democrats agreed to pass the Senate bill on condition that it be amended by a subsequent bill.
They drafted the
Health Care and Education Reconciliation Act
The Health Care and Education Reconciliation Act of 2010 (, ) is a law that was enacted by the 111th United States Congress, by means of the reconciliation process, in order to amend the Affordable Care Act (ACA) (). The law includes the ...
, which could be passed by the
reconciliation process
Budget reconciliation is a special parliamentary procedure of the United States Congress set up to expedite the passage of certain budgetary legislation in the United States Senate. The procedure overrides the filibuster rules in the Senate, w ...
.
Per the
Congressional Budget Act of 1974
The Congressional Budget and Impoundment Control Act of 1974 (, , ) is a United States federal law that governs the role of the Congress in the United States budget process.
The Congressional budget process
Titles I through IX of the law are also ...
, reconciliation cannot be subject to a
filibuster
A filibuster is a political procedure in which one or more members of a legislative body prolong debate on proposed legislation so as to delay or entirely prevent decision. It is sometimes referred to as "talking a bill to death" or "talking out ...
. But reconciliation is
limited to budget changes, which is why the procedure was not used to pass ACA in the first place; the bill had inherently non-budgetary regulations. Although the already-passed Senate bill could not have been passed by reconciliation, most of House Democrats' demands were budgetary: "these changes—higher subsidy levels, different kinds of taxes to pay for them, nixing the Nebraska Medicaid deal—mainly involve taxes and spending. In other words, they're exactly the kinds of policies that are well-suited for reconciliation."
The remaining obstacle was a pivotal group of
pro-life
Anti-abortion movements, also self-styled as pro-life or abolitionist movements, are involved in the abortion debate advocating against the practice of abortion and its legality. Many anti-abortion movements began as countermovements in respons ...
Democrats led by
Bart Stupak
Bartholomew Thomas Stupak (; born February 29, 1952) is an American politician and lobbyist. A member of the Democratic Party, Stupak served as the U.S. representative from from 1993 to 2011.
Stupak chose not to seek re-election in 2010. He dep ...
who were initially reluctant to support the bill. The group found the possibility of federal funding for abortion significant enough to warrant opposition. The Senate bill had not included language that satisfied their concerns, but they could not address abortion in the reconciliation bill as it would be non-budgetary. Instead, Obama issued
Executive Order 13535 Executive Order 13535 is an executive order announced by President Barack Obama on March 21, 2010, and signed on March 24, 2010. It reinforces a commitment to preservation of the Hyde Amendment's policy restricting federal funds for abortion within ...
, reaffirming the principles in the
Hyde Amendment
In U.S. politics, the Hyde Amendment is a legislative provision barring the use of federal funds to pay for abortion, except to save the life of the woman, or if the pregnancy arises from incest or rape. Before the Hyde Amendment took effect in ...
.
This won the support of Stupak and members of his group and assured the bill's passage.
The House passed the Senate bill with a 219–212 vote on March 21, 2010, with 34 Democrats and all 178 Republicans voting against it.
It passed the
second bill, by 220–211, the same day (with the Senate passing this bill via reconciliation by 56-43 a few days later). The day after the passage of ACA, March 22, Republicans introduced legislation to repeal it.
Obama signed ACA into law on March 23, 2010.
Post-enactment
Since passage, Republicans have voted to repeal all or parts of the Affordable Care Act more than sixty times.
The
Tax Cuts and Jobs Act of 2017
The Act to provide for reconciliation pursuant to titles II and V of the concurrent resolution on the budget for fiscal year 2018, , is a congressional revenue act of the United States originally introduced in Congress as the Tax Cuts and Jobs A ...
eliminated the fine for violating the individual mandate, starting in 2019. (The requirement itself is still in effect.)
In 2019 Congress repealed the so-called "Cadillac" tax on health insurance benefits, an excise tax on medical devices, and the Health Insurance Tax.
The
American Rescue Plan Act of 2021
The American Rescue Plan Act of 2021, also called the COVID-19 Stimulus Package or American Rescue Plan, is a economic stimulus bill passed by the 117th United States Congress and signed into law by President Joe Biden on March 11, 2021, to sp ...
, enacted during the
COVID-19 pandemic in the United States
The COVID-19 pandemic in the United States is a part of the COVID-19 pandemic, worldwide pandemic of COVID-19, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In the Uni ...
, expanded subsidies for marketplace health plans. A continuation of these subsidies was introduced as part of the
Inflation Reduction Act of 2022
The Inflation Reduction Act of 2022 (IRA) is a landmark United States federal law which aims to curb inflation by reducing the deficit, lowering prescription drug prices, and investing into domestic energy production while promoting clean en ...
.
Impact
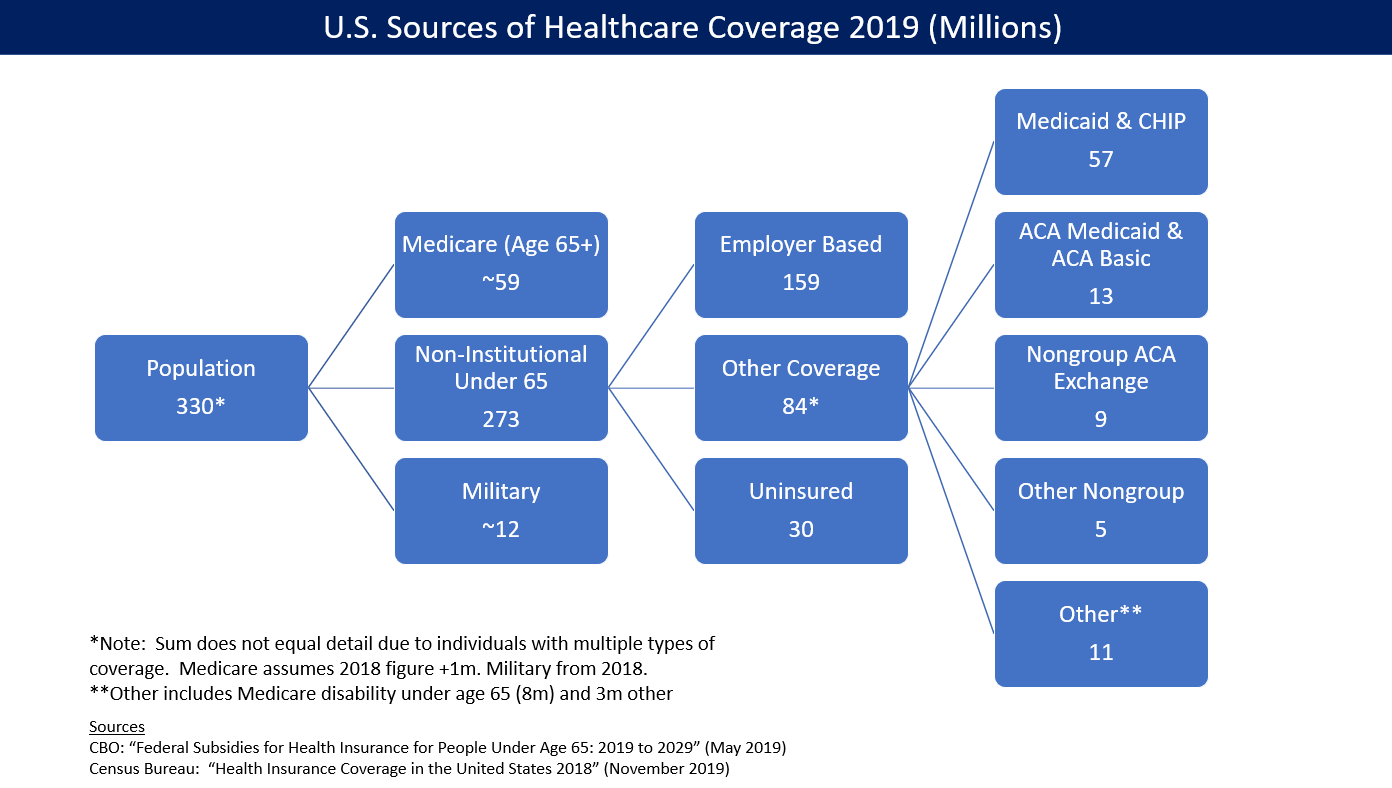
Coverage
The law caused a significant reduction in the number and percentage of people without health insurance. The CDC reported that the percentage of people without health insurance fell from 16.0% in 2010 to 8.9% from January to June 2016. The uninsured rate dropped in every congressional district in the U.S. from 2013 to 2015. The
Congressional Budget Office
The Congressional Budget Office (CBO) is a federal agency within the legislative branch of the United States government that provides budget and economic information to Congress.
Inspired by California's Legislative Analyst's Office that manages ...
reported in March 2016 that approximately 12 million people were covered by the exchanges (10 million of whom received subsidies) and 11 million added to Medicaid. Another million were covered by ACA's "Basic Health Program", for a total of 24 million.
CBO estimated that ACA would reduce the net number of uninsured by 22 million in 2016, using a slightly different computation for the above figures totaling ACA coverage of 26 million, less 4million for reductions in "employment-based coverage" and "non-group and other coverage".
The
U.S. Department of Health and Human Services (HHS) estimated that 20.0 million adults (aged 18–64) gained healthcare coverage via ACA as of February 2016;
similarly, the
Urban Institute
The Urban Institute is a Washington, D.C.–based think tank that carries out economic and social policy research to "open minds, shape decisions, and offer solutions". The institute receives funding from government contracts, foundations and pr ...
found in 2016 that 19.2 million non-elderly Americans gained health insurance coverage from 2010 to 2015. In 2016, CBO estimated the uninsured at approximately 27 million people, or around 10% of the population or 7–8% excluding unauthorized immigrants.
States that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while those that did not had a 14.1% uninsured rate, among adults aged 18–64.
As of December 2016 32 states (including Washington DC) had adopted the Medicaid extension.
A 2017 study found that the ACA reduced socioeconomic disparities in health care access.
The Affordable Care Act reduced the percent of Americans between 18 and 64 who were uninsured from 22.3 percent in 2010 to 12.4 percent in 2016. About 21 million more people have coverage ten years after the enactment of the ACA.
Ten years after its enactment studies showed that the ACA also had a positive effect on health and caused a reduction in mortality.
Taxes

Excise taxes
file:Lincoln Beer Stamp 1871.JPG, upright=1.2, 1871 U.S. Revenue stamp for 1/6 barrel of beer. Brewers would receive the stamp sheets, cut them into individual stamps, cancel them, and paste them over the Bunghole, bung of the beer barrel so when ...
from the Affordable Care Act raised $16.3 billion in
fiscal year
A fiscal year (or financial year, or sometimes budget year) is used in government accounting, which varies between countries, and for budget purposes. It is also used for financial reporting by businesses and other organizations. Laws in many ...
2015. $11.3 billion came from an excise tax placed directly on health insurers based on their market share. Annual excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs.
The
Individual mandate
An individual mandate is a requirement by law for certain persons to purchase or otherwise obtain a good or service.
United States Militia act
The Militia Acts of 1792, based on the Constitution's militia clause (in addition to its affirmative ...
tax was $695 per individual or $2,085 per family at a minimum, reaching as high as 2.5% of household income (whichever was higher). The tax was reduced to 0 at the end of 2018.
In fiscal year 2018, the individual and employer mandates yielded $4 billion each. Excise taxes on insurers and drug makers added $18 billion. Income tax surcharges produced 437 billion.
ACA reduced income inequality measured after taxes, due to the income tax surcharges and subsidies. CBO estimated that subsidies paid under the law in 2016 averaged $4,240 per person for 10 million individuals receiving them, roughly $42 billion. The tax subsidy for the employer market, was approximately $1,700 per person in 2016, or $266 billion total.
Insurance exchanges
As of August 2016, 15 states operated their own
health insurance marketplace
In the United States, health insurance marketplaces, also called health exchanges, are organizations in each state through which people can purchase health insurance. People can purchase health insurance that complies with the Patient Protection ...
. Other states either used the federal exchange, or operated in partnership with or supported by the federal government.
By 2019, 12 states and Washington DC operated their own exchanges.
Medicaid expansion in practice


As of December 2019, 37 states (including Washington DC) had adopted the Medicaid extension.
Those states that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while the others had a 14.1% uninsured rate, among adults aged 18 to 64.
Following the Supreme Court ruling in 2012, which held that states would not lose Medicaid funding if they did not expand Medicaid under ACA, several states rejected the option. Over half the national uninsured population lived in those states.
The
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services (CMS), is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer M ...
(CMS) estimated that the cost of expansion was $6,366 per person for 2015, about 49 percent above previous estimates. An estimated 9to 10 million people had gained Medicaid coverage, mostly low-income adults. The
Kaiser Family Foundation
KFF (Kaiser Family Foundation), also known as The Henry J. Kaiser Family Foundation, is an American non-profit organization, headquartered in San Francisco, California. It prefers KFF since its legal name can cause confusion as it is no longer a ...
estimated in October 2015 that 3.1 million additional people were not covered because of states that rejected the Medicaid expansion.
In many states income thresholds were significantly below 133% of the poverty line.
Many states did not make Medicaid available to childless adults at any income level.
Because subsidies on exchange insurance plans were not available to those below the poverty line, such individuals had no new options.
For example, in Kansas, where only non-disabled adults with children and with an income below 32% of the poverty line were eligible for Medicaid, those with incomes from 32% to 100% of the poverty level ($6,250 to $19,530 for a family of three) were ineligible for both Medicaid and federal subsidies to buy insurance. Absent children, non-disabled adults were not eligible for Medicaid there.
Studies of the impact of Medicaid expansion rejections calculated that up to 6.4 million people would have too much income for Medicaid but not qualify for exchange subsidies. Several states argued that they could not afford the 10% contribution in 2020.
Some studies suggested rejecting the expansion would cost more due to increased spending on uncompensated emergency care that otherwise would have been partially paid for by Medicaid coverage,
A 2016 study found that residents of Kentucky and Arkansas, which both expanded Medicaid, were more likely to receive health care services and less likely to incur emergency room costs or have trouble paying their medical bills. Residents of Texas, which did not accept the Medicaid expansion, did not see a similar improvement during the same period.
Kentucky opted for increased managed care, while Arkansas subsidized private insurance. Later Arkansas and Kentucky governors proposed reducing or modifying their programs. From 2013 to 2015, the uninsured rate dropped from 42% to 14% in Arkansas and from 40% to 9% in Kentucky, compared with 39% to 32% in Texas.
A 2016
DHHS study found that states that expanded Medicaid had lower premiums on exchange policies, because they had fewer low-income enrollees, whose health on average is worse than that of those with higher income.
In September 2019, the Census Bureau reported that states that expanded Medicaid under the ACA had considerably lower uninsured rates than states that did not. For example, for adults between 100% and 399% of poverty level, the uninsured rate in 2018 was 12.7% in expansion states and 21.2% in non-expansion states. Of the 14 states with uninsured rates of 10% or greater, 11 had not expanded Medicaid.
The drop in uninsured rates due to expanded Medicaid has broadened access to care among low-income adults, with post-ACA studies indicating an improvement in affordability, access to doctors, and usual sources of care.
A study using national data from the Health Reform Monitoring Survey determined that unmet need due to cost and inability to pay medical bills significantly decreased among low-income (up to 138% FPL) and moderate-income (139-199% FPL) adults, with unmet need due to cost decreasing by approximately 11 percentage points among low-income adults by the second enrollment period.
Importantly, issues with cost-related unmet medical needs, skipped medications, paying medical bills, and annual out-of-pocket spending have been significantly reduced among low-income adults in Medicaid expansion states compared to non-expansion states.
As well, expanded Medicaid has led to a 6.6% increase in physician visits by low-income adults, as well as increased usage of preventative care such as dental visits and cancer screenings among childless, low-income adults.
Improved health care coverage due to Medicaid expansion has been found in a variety of patient populations, such as adults with mental and substance use disorders, trauma patients, cancer patients, and people living with HIV.
Compared to 2011–13, in 2014 there was a 5.4 percentage point reduction in the uninsured rate of adults with mental disorders (from 21.3% to 15.9%) and a 5.1 percentage point reduction in the uninsured rate of adults with substance use disorders (from 25.9% to 20.8%); with increases in coverage occurring primarily through Medicaid.
Use of mental health treatment increased by 2.1 percentage points, from 43% to 45.1%.
Among trauma patients nationwide, the uninsured rate has decreased by approximately 50%.
Adult trauma patients in expansion states experienced a 13.7 percentage point reduction in uninsured rates compared to adult trauma patients in non-expansion states, and an accompanying 7.4 percentage point increase in discharge to rehabilitation. Following Medicaid expansion and dependent coverage expansion, young adults hospitalized for acute traumatic injury in Maryland experienced a 60% increase in rehabilitation, 25% reduction in mortality, and a 29.8% reduction in failure-to-rescue. Medicaid expansion's swift impact on cancer patients was demonstrated in a study using the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) program that evaluated more than 850,000 patients diagnosed with breast, lung, colorectal, prostate cancer, or thyroid cancer from 2010 to 2014. The study found that a cancer diagnosis in 2014 was associated with a 1.9 percentage-point absolute and 33.5% relative decrease in uninsured rates compared to a diagnosis made between 2010 and 2013.
Another study, using Surveillance, Epidemiology, and End Results (SEER) Program data from 2010 to 2014, found that Medicaid expansion was associated with a 6.4% net increase in early stage (in situ, local, or regional) diagnoses of all cancers combined.
Data from the Centers for Disease and Prevention's (CDC) Medical Monitoring Project demonstrated that between 2009 and 2012, approximately 18% of people living with HIV (PLWH) who were actively receiving HIV treatment were uninsured
and that at least 40% of HIV-infected adults receiving treatment were insured through Medicaid and/or Medicare, programs they qualified for only once their disease was advanced enough to be covered as a disability under Social Security.
Expanded Medicaid coverage of PLWH has been positively associated with health outcomes such as viral suppression, retention of care, hospitalization rates, and morbidity at the time of hospitalization.
An analysis of Behavioral Risk Factor Surveillance System (BRFSS) survey data found a 2.8% annual increase in viral suppression rates among all PLWH from 2010 to 2015 due to Medicaid expansion.
In Nebraska, PLWH newly covered by Medicaid expansion in 2013-14 were four times more likely to be virally suppressed than PLWH who were eligible but remained uninsured.
As an early adopter of Medicaid expansion, Massachusetts found a 65% rate of viral suppression among all PLWH and an 85% rate among those retained in healthcare in 2014, both substantially higher than the national average.
An analysis of hospital discharge data from 2012 to 2014 in four Medicaid expansion states and two non-expansion states revealed hospitalizations of uninsured PLWH fell from 13.7% to 5.5% in the four expansion states and rose from 14.5% to 15.7% in the two non-expansion states.
Importantly, uninsured PLWH were 40% more likely to die in the hospital than insured PLWH.
Other notable health outcomes associated with Medicaid expansion include improved glucose monitoring rates for patients with diabetes, better hypertension control, and reduced rates of major post-operative morbidity.
A July 2019 study by the National Bureau of Economic Research (NBER) indicated that states enacting Medicaid expansion exhibited statistically significant reductions in mortality rates. From that study, states that took Medicaid expansion "saved the lives of at least 19,200 adults aged 55 to 64 over the four-year period from 2014 to 2017."
[Broaddus, Matt, & Aron-Dine, Aviva. (November 6, 2019)]
''Medicaid Expansion Has Saved at Least 19,000 Lives, New Research Finds. State Decisions Not to Expand Have Led to 15,000 Premature Deaths''
Center on Budget and Policy Priorities. Archived at th
Wayback machine
on December 17, 2019. Further, 15,600 older adults died prematurely in the states that did not enact Medicaid expansion in those years according to the NBER research. "The lifesaving impacts of Medicaid expansion are large: an estimated 39 to 64 percent reduction in annual mortality rates for older adults gaining coverage."
Due to many states' failure to expand, many Democrats co-sponsored the proposed 2021 Cover Now Act that would allow county and municipal governments to fund Medicaid expansion.
Medicaid expansion by state
Insurance costs

National health care expenditures rose faster than national income both before (2009-2013: 3.73%) and after (2014-2018: 4.82%) ACA's major provisions took effect.
Premium prices rose considerably before and after. For example, a study published in 2016 found that the average requested 2017 premium increase among 40-year-old non-smokers was about 9percent, according to an analysis of 17 cities, although Blue Cross Blue Shield proposed increases of 40 percent in Alabama and 60 percent in Texas. However, some or all these costs were offset by tax credits. For example, the
Kaiser Family Foundation
KFF (Kaiser Family Foundation), also known as The Henry J. Kaiser Family Foundation, is an American non-profit organization, headquartered in San Francisco, California. It prefers KFF since its legal name can cause confusion as it is no longer a ...
reported that for the second-lowest cost "Silver plan", a 40-year old non-smoker making $30,000 per year would pay effectively the same amount in 2017 as they did in 2016 (about $208/month) after the tax credit, despite a large increase in the list price. This was consistent nationally. In other words, the subsidies increased along with the premium price, fully offsetting the increases for subsidy-eligible enrollees.
Premium cost increases in the employer market moderated after 2009. For example, healthcare premiums for those covered by employers rose by 69% from 2000 to 2005, but only 27% from 2010 to 2015,
with only a 3% increase from 2015 to 2016. From 2008 to 2010 (before passage of ACA) health insurance premiums rose by an average of 10% per year.
Several studies found that the
financial crisis
A financial crisis is any of a broad variety of situations in which some financial assets suddenly lose a large part of their nominal value. In the 19th and early 20th centuries, many financial crises were associated with banking panics, and man ...
and accompanying recession could not account for the entirety of the slowdown and that structural changes likely shared at least partial credit.
A 2013 study estimated that changes to the health system had been responsible for about a quarter of the recent reduction in inflation. Paul Krawzak claimed that even if cost controls succeed in reducing the amount spent on healthcare, such efforts on their own may be insufficient to outweigh the long-term burden placed by demographic changes, particularly
the growth of the population on Medicare.
In a 2016 review, Barack Obama claimed that from 2010 through 2014 mean annual growth in real per-enrollee Medicare spending was negative, down from a mean of 4.7% per year from 2000 through 2005 and 2.4% per year from 2006 to 2010; similarly, mean real per-enrollee growth in private insurance spending was 1.1% per year over the period, compared with a mean of 6.5% from 2000 through 2005 and 3.4% from 2005 to 2010.
Deductibles and co-payments
A contributing factor to premium cost moderation was that the insured faced higher
deductible
In an insurance policy, the deductible (in British English, the excess) is the amount paid
out of pocket by the policy holder before an insurance provider will pay any expenses. In general usage, the term ''deductible'' may be used to describe o ...
s,
copayment
A copayment or copay (called a gap in Australian English) is a fixed amount for a covered service, paid by a patient to the provider of service before receiving the service. It may be defined in an insurance policy and paid by an insured person ea ...
s and out-of-pocket maximums. In addition, many employees chose to combine a
health savings account
A health savings account (HSA) is a tax-advantaged medical savings account available to taxpayers in the United States who are enrolled in a high-deductible health plan (HDHP). The funds contributed to an account are not subject to federal inco ...
with higher deductible plans, making the net impact of ACA difficult to determine precisely.
For the group market (employer insurance), a 2016 survey found that:
* Deductibles grew 63% from 2011 to 2016, while premiums increased 19% and worker earnings grew by 11%.
* In 2016, 4 in 5 workers had an insurance deductible, which averaged $1,478. For firms with less than 200 employees, the deductible averaged $2,069.
* The percentage of workers with a deductible of at least $1,000 grew from 10% in 2006 to 51% in 2016. The 2016 figure dropped to 38% after taking employer contributions into account.
For the non-group market, of which two-thirds are covered by ACA exchanges, a survey of 2015 data found that:
* 49% had individual deductibles of at least $1,500 ($3,000 for family), up from 36% in 2014.
* Many exchange enrollees qualify for cost-sharing subsidies that reduce their net deductible.
* While about 75% of enrollees were "very satisfied" or "somewhat satisfied" with their choice of doctors and hospitals, only 50% had such satisfaction with their annual deductible.
* While 52% of those covered by ACA exchanges felt "well protected" by their insurance, in the group market 63% felt that way.
Health outcomes
According to a 2014 study, ACA likely prevented an estimated 50,000 preventable patient deaths from 2010 to 2013. Himmelstein and Woolhandler wrote in January 2017 that a rollback of ACA's Medicaid expansion alone would cause an estimated 43,956 deaths annually.
According to the Kaiser Foundation, expanding Medicaid in the remaining states would cover up to 4.5 million persons. A 2021 study found a significant decline in mortality rates in the states that opted in to the Medicaid expansion program compared with those states that did not do so. The study reported that states decisions' not to expand Medicaid resulted in approximately 15,600 excess deaths from 2014 through 2017.
Dependent Coverage Expansion (DCE) under the ACA has had a demonstrable effect on various health metrics of young adults, a group with a historically low level of insurance coverage and utilization of care.
Numerous studies have shown the target age group gained private health insurance relative to an older group after the policy was implemented, with an accompanying improvement in having a usual source of care, reduction in out-of-pocket costs of high-end medical expenditures, reduction in frequency of Emergency Department visits, 3.5% increase in hospitalizations and 9% increase in hospitalizations with a psychiatric diagnosis, 5.3% increase in utilizing specialty mental health care by those with a probable mental illness, 4% increase in reporting excellent mental health, and a 1.5-6.2% increase in reporting excellent physical health.
Studies have also found that DCE was associated with improvements in cancer prevention, detection, and treatment among young adult patients.
A study of 10,010 women aged 18–26 identified through the 2008-12 National Health Interview Survey found that the likelihood of HPV vaccination initiation and completion increased by 7.7 and 5.8 percentage points respectively when comparing before and after October 1, 2010.
Another study using National Cancer Database (NCDB) data from 2007 to 2012 found a 5.5 percentage point decrease in late-stage (stages III/IV) cervical cancer diagnosis for women aged 21–25 after DCE, and an overall decrease of 7.3 percentage points in late-stage diagnosis compared to those aged 26–34.
A study using SEER Program data from 2007 to 2012 found a 2.7 percentage point increase in diagnosis at stage I disease for patients aged 19–25 compared with those aged 26–34 for all cancers combined.
Studies focusing on cancer treatment after DCE found a 12.8 percentage point increase in the receipt of fertility-sparing treatment among cervical cancer patients aged 21–25 and an overall increase of 13.4 percentage points compared to those aged 26–34, as well as an increased likelihood that patients aged 19–25 with stage IIB-IIIC colorectal cancer receive timely adjuvant chemotherapy compared to those aged 27–34.
Two 2018 ''
JAMA
''The Journal of the American Medical Association'' (''JAMA'') is a peer-reviewed medical journal published 48 times a year by the American Medical Association. It publishes original research, reviews, and editorials covering all aspects of biom ...
'' studies found the Hospital Readmissions Reduction Program (HRRP) was associated with increased post-discharge mortality for patients hospitalized for heart failure and pneumonia. A 2019 ''JAMA'' study found that ACA decreased emergency department and hospital use by uninsured individuals. Several studies have indicated that increased 30-day, 90-day, and 1-year post-discharge mortality of heart failure patients can be attributed to "gaming the system" through inappropriate triage systems in emergency departments, use of observation stays when admissions are warranted, and delay of readmission beyond the 30th day post-discharge, strategies that can reduce readmission rates at the expense of quality of care and patient survival. The HRRP was also shown to disproportionately penalize safety-net hospitals that predominately serve low-income patients. A 2020 study by Treasury Department economists in the ''
Quarterly Journal of Economics
''The Quarterly Journal of Economics'' is a peer-reviewed academic journal published by the Oxford University Press for the Harvard University Department of Economics. Its current editors-in-chief are Robert J. Barro, Lawrence F. Katz, Nathan N ...
'' using a
randomized controlled trial
A randomized controlled trial (or randomized control trial; RCT) is a form of scientific experiment used to control factors not under direct experimental control. Examples of RCTs are clinical trials that compare the effects of drugs, surgical te ...
(the IRS sent letters to some taxpayers noting that they had paid a fine for not signing up for health insurance but not to other taxpayers) found that over two years, obtaining health insurance reduced mortality by 12 percent.
The study concluded that the letters, sent to 3.9 million people, may have saved 700 lives.
A 2020 ''JAMA'' study found that Medicare expansion under the ACA was associated with reduced incidence of advanced-stage breast cancer, indicating that Medicaid accessibility led to early detection of breast cancer and higher survival rates. Recent studies have also attributed to Medicaid expansion an increase in use of smoking cessation medications, cervical cancer screening, and colonoscopy, as well as an increase in the percentage of early-stage diagnosis of all cancers and the rate of cancer surgery for low-income patients.
These studies include a 2.1% increase in the probability of smoking cessation in Medicaid expansion states compared to non-expansion states, a 24% increase in smoking cessation medication use due to increased Medicaid-financed smoking cessation prescriptions, a 27.7% increase in the rate of colorectal cancer screening in Kentucky following Medicaid expansion with an accompanying improvement in colorectal cancer survival, and a 3.4% increase in cancer incidence following Medicaid expansion that was attributed to an increase in early-stage diagnoses.
Transition-of-care interventions and Alternative Payment Models under the ACA have also shown promise in improving health outcomes.
Post-discharge provider appointment and telephone follow-up interventions have been shown to reduce 30-day readmission rates among general medical-surgical inpatients.
Reductions in 60, 90, and 180 post-discharge day readmission rates due to transition-of-care interventions have also been demonstrated, and a reduction in 30-day mortality has been suggested.
Total joint arthroplasty bundles as part of the Bundled Payments for Care Improvement initiative have been shown to reduce discharge to inpatient rehabilitation facilities and post-acute care facilities, decrease hospital length of stay by 18% without sacrificing quality of care, and reduce the rate of total joint arthroplasty readmissions, half of which were due to surgical complications.
The Hospital Value-Based Purchasing Program in Medicaid has also shown the potential to improve health outcomes, with early studies reporting positive and significant effects on total patient experience score, 30-day readmission rates, incidences of pneumonia and pressure ulcers, and 30-day mortality rates for pneumonia.
The patient-centered medical home (PCMH) payment and care model, a team-based approach to population health management that risk-stratifies patients and provides focused care management and outreach to high-risk patients, has been shown to improve diabetes outcomes.
A widespread PCMH demonstration program focusing on diabetes, known as the Chronic Care Initiative in the Commonwealth of Pennsylvania, found statistically significant improvements in A1C testing, LDL-C testing, nephropathy screening and monitoring, and eye examinations, with an accompanying reduction in all-cause emergency department visits, ambulatory care-sensitive emergency department visits, ambulatory visits to specialists, and a higher rate of ambulatory visits to primary care providers.
The ACA overall has improved coverage and care of diabetes, with a significant portion of the 3.5 million uninsured US adults aged 18–64 with diabetes in 2009-10 likely gaining coverage and benefits such as closure of the Medicaid Part D coverage gap for insulin.
2.3 million of the approximately 4.6 million people aged 18–64 with undiagnosed diabetes in 2009-2010 may also have gained access to zero-cost preventative care due to section 2713 of the ACA, which prohibits cost sharing for United States Preventive Services Taskforce grade A or B recommended services, such as diabetes screenings.
Distributional impact

In March 2018, the CBO reported that ACA had reduced income inequality in 2014, saying the law led the lowest and second quintiles (the bottom 40%) to receive an average of an additional $690 and $560 respectively while causing households in the top 1% to pay an additional $21,000 due mostly to the net investment income tax and the additional Medicare tax. The law placed relatively little burden on households in the top quintile (top 20%) outside of the top 1%.
Federal deficit
CBO estimates of revenue and impact on deficit
The CBO reported in multiple studies that ACA would reduce the deficit, and repealing it would increase the deficit, primarily because of the elimination of Medicare reimbursement cuts.
The 2011 comprehensive CBO estimate projected a net deficit reduction of more than $200 billion during the 2012–2021 period:
it calculated the law would result in $604 billion in
total outlays offset by $813 billion in
total receipts, resulting in a $210 billion net deficit reduction.
The CBO separately predicted that while most of the spending provisions do not begin until 2014,
revenue would exceed spending in those subsequent years.
The CBO claimed the bill would "substantially reduce the growth of Medicare's payment rates for most services; impose an excise tax on insurance plans with relatively high premiums; and make various other changes to the federal tax code, Medicare, Medicaid, and other programs"
—ultimately extending the solvency of the
Medicare trust fund by eight years.
This estimate was made prior to the
Supreme Court's ruling that enabled states to
opt out of the Medicaid expansion, thereby forgoing the related federal funding. The
CBO and
JCT subsequently updated the budget projection, estimating the impact of the ruling would reduce the cost estimate of the insurance coverage provisions by $84 billion.
The CBO in June 2015 forecast that repeal of ACA would increase the deficit between $137 billion and $353 billion over the 2016–2025 period, depending on the impact of macroeconomic
feedback
Feedback occurs when outputs of a system are routed back as inputs as part of a chain of cause-and-effect that forms a circuit or loop. The system can then be said to ''feed back'' into itself. The notion of cause-and-effect has to be handled ...
effects. The CBO also forecast that repeal of ACA would likely cause an increase in GDP by an average of 0.7% in the period from 2021 to 2025, mainly by boosting the supply of labor.
Although the CBO generally does not provide cost estimates beyond the 10-year budget projection period because of the degree of uncertainty involved in the projection, it decided to do so in this case at the request of lawmakers, and estimated a second decade deficit reduction of $1.2 trillion.
CBO predicted deficit reduction around a broad range of one-half percent of GDP over the 2020s while cautioning that "a wide range of changes could occur".
In 2017 CBO estimated that repealing the individual mandate alone would reduce the 10-year deficit by $338 billion.
Opinions on CBO projections
The CBO cost estimates were criticized because they excluded the effects of potential legislation that would increase Medicare payments by more than $200 billion from 2010 to 2019. However, the so-called "
doc fix
The Medicare Sustainable Growth Rate (SGR) was a method used by the Centers for Medicare and Medicaid Services (CMS) in the United States to control spending by Medicare on physician services.
President Barack Obama signed a bill into law on Apr ...
" is a separate issue that would have existed with or without ACA. The
Center on Budget and Policy Priorities
The Center on Budget and Policy Priorities (CBPP) is a progressive American think tank that analyzes the impact of federal and state government budget policies. A 501(c)(3) nonprofit organization, the Center's stated mission is to "conduct resear ...
objected that Congress had a good record of implementing Medicare savings. According to their study, Congress followed through on the implementation of the vast majority of provisions enacted in the past 20 years to produce Medicare savings, although not the doc fix. The doc fix became obsolete in 2015 when the savings provision was eliminated, permanently removing that spending restraint.
Health economist
Health economics is a branch of economics concerned with issues related to efficiency, effectiveness, value and behavior in the production and consumption of health and healthcare. Health economics is important in determining how to impr ...
Uwe Reinhardt, wrote, "The rigid, artificial rules under which the Congressional Budget Office must score proposed legislation unfortunately cannot produce the best unbiased forecasts of the likely fiscal impact of any legislation."
Douglas Holtz-Eakin
Douglas James "Doug" Holtz-Eakin (born February 3, 1958) is an American economist. He was formerly an economics professor at Syracuse University, Director of the Congressional Budget Office, and chief economic policy adviser to Senator John McCain ...
alleged that the bill would increase the deficit by $562 billion because, he argued, it front-loaded revenue and back-loaded benefits.
Scheiber and Cohn rejected critical assessments of the law's deficit impact, arguing that predictions were biased towards underestimating deficit reduction. They noted, for example, it is easier to account for the cost of definite levels of subsidies to specified numbers of people than to account for savings from
preventive healthcare
Preventive healthcare, or prophylaxis, consists of measures taken for the purposes of disease prevention.Hugh R. Leavell and E. Gurney Clark as "the science and art of preventing disease, prolonging life, and promoting physical and mental hea ...
, and that the CBO had a track record of overestimating costs and underestimating savings of health legislation;
stating, "innovations in the delivery of medical care, like greater use of
electronic medical record
An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared throu ...
s and financial incentives for more coordination of care among doctors, would produce substantial savings while also slowing the relentless climb of medical expenses... But the CBO would not consider such savings in its calculations, because the innovations hadn't really been tried on such large scale or in concert with one another—and that meant there wasn't much hard data to prove the savings would materialize."
In 2010
David Walker said the CBO estimates were not likely to be accurate, because they were based on the assumption that the law would not change.
Employer mandate and part-time work
The employer mandate applies to employers of more than fifty where health insurance is provided only to the full-time workers.
Critics claimed it created a
perverse incentive
A perverse incentive is an incentive that has an unintended and undesirable result that is contrary to the intentions of its designers. The cobra effect is the most direct kind of perverse incentive, typically because the incentive unintentionall ...
to hire part-timers instead.
However, between March 2010 and 2014, the number of part-time jobs declined by 230,000 while the number of full-time jobs increased by two million.
In the public sector full-time jobs turned into part-time jobs much more than in the private sector.
A 2016 study found only limited evidence that ACA had increased part-time employment.
Several businesses and the state of Virginia added a 29-hour-a-week cap for their part-time employees, to reflect the 30-hour-or-more definition for full-time worker.
As of 2013, few companies had shifted their workforce towards more part-time hours (4% in a survey from the
Federal Reserve Bank of Minneapolis
Federal or foederal (archaic) may refer to:
Politics
General
*Federal monarchy, a federation of monarchies
*Federation, or ''Federal state'' (federal system), a type of government characterized by both a central (federal) government and states or ...
).
Trends in working hours
and the recovery from the
Great Recession
The Great Recession was a period of marked general decline, i.e. a recession, observed in national economies globally that occurred from late 2007 into 2009. The scale and timing of the recession varied from country to country (see map). At ...
correlate with the shift from part-time to full-time work. Other confounding impacts include that health insurance helps attract and retain employees, increases productivity and reduces absenteeism; and lowers corresponding training and administration costs from a smaller, more stable workforce.
Relatively few firms employ over 50 employees
and more than 90% of them already offered insurance.
Most policy analysts (both right and left) were critical of the employer mandate provision.
They argued that the perverse incentives regarding part-time hours, even if they did not change existing plans, were real and harmful;
that the raised
marginal cost
In economics, the marginal cost is the change in the total cost that arises when the quantity produced is incremented, the cost of producing additional quantity. In some contexts, it refers to an increment of one unit of output, and in others it r ...
of the 50th worker for businesses could limit companies' growth; that the costs of reporting and administration were not worth the costs of maintaining employer plans;
and noted that the employer mandate was not essential to maintain adequate risk pools.
The provision generated vocal opposition from business interests and some unions who were not granted exemptions.
Hospitals
From the start of 2010 to November 2014, 43 hospitals in
rural areas
In general, a rural area or a countryside is a geographic area that is located outside towns and cities. Typical rural areas have a low population density and small settlements. Agricultural areas and areas with forestry typically are describ ...
closed. Critics claimed the new law had caused these closures. Many rural hospitals were built using funds from the 1946
Hill–Burton Act
The Hospital Survey and Construction Act (), commonly known as the Hill–Burton Act, is a U.S. federal law passed in 1946, during the 79th United States Congress. It was sponsored by Senator Harold Burton of Ohio and Senator Lister Hill of Ala ...
. Some of these hospitals reopened as other medical facilities, but only a small number operated
emergency rooms (ER) or
urgent care An urgent care center (UCC), also known as an urgent treatment centre in the United Kingdom, is a type of walk-in clinic focused on the delivery of urgent ambulatory care in a dedicated medical facility outside of a traditional emergency department ...
centers.
Between January 2010 and 2015, a quarter of ER doctors said they had seen a major surge in patients, while nearly half had seen a smaller increase. Seven in ten ER doctors claimed they lacked the resources to deal with large increases in the number of patients. The biggest factor in the increased number of ER patients was insufficient primary care providers to handle the larger number of insured. Michael Lee, Jr. and Michael C. Monuteaux at Boston Children's Hospital analyzed national emergency department visits among children aged 0 to 17 from 2009 to 2016 using the American Community Survey (ACS) and Nationwide Emergency Department Sample (NEDS). They found no immediate change in pediatric emergency department visit rates the year after the ACA took full effect in 2014, but the rate of change from 2014 to 2016 was significantly higher than previous rate trends, almost 10%.
Several large insurers formed ACOs. Many hospitals merged and purchased physician practices, amounting to a significant consolidation of the provider industry. The increased market share gave them more leverage with insurers and reduced patient care options.
Economic consequences

CBO estimated in June 2015 that repealing ACA would:
* Decrease GDP in the short-term, as government spending (on subsidies) was only partially replaced by spending by recipients.
* Increase the supply of labor and aggregate compensation by about 0.8 and 0.9 percent over the 2021–2025 period. CBO cited ACA's expanded eligibility for Medicaid and subsidies and tax credits that rise with income as disincentives to work, so repealing ACA would remove those disincentives, encouraging workers to supply more labor, increasing the total number of hours worked by about 1.5% over the 2021–2025 period.
* Remove the higher tax rates on capital income, thereby encouraging investment, raising the capital stock and output in the long-run.
In 2015 the progressive
Center for Economic and Policy Research
The Center for Economic and Policy Research (CEPR) is a progressive American think tank that specializes in economic policy. Based in Washington, D.C. CEPR was co-founded by economists Dean Baker and Mark Weisbrot in 1999.
Considered a left-lea ...
found no evidence that companies were reducing worker hours to avoid ACA requirements for employees working more than 30 hours per week.
CBO estimated that ACA would slightly reduce the size of the labor force and number of hours worked, as some would no longer be tethered to employers for their insurance. Jonathan Cohn claimed that ACA's primary employment effect was to alleviate
job lock
The term job lock is used to describe the inability of an employee to freely leave a job because doing so will result in the loss of employee benefits (usually health or retirement related). In a broader sense, job lock may describe the situatio ...
and the reform's only significant employment impact was the retirement of those who were working only to stay insured.
Public opinion

Public views became increasingly negative in reaction to specific plans discussed during the legislative debate over 2009 and 2010. Approval varied by party, race and age. Some elements were more widely favored (preexisting conditions) or opposed (individual mandate).
In a 2010
poll
Poll, polled, or polling may refer to:
Figurative head counts
* Poll, a formal election
** Election verification exit poll, a survey taken to verify election counts
** Polling, voting to make decisions or determine opinions
** Polling places o ...
, 62% of respondents said they thought ACA would "increase the amount of money they personally spend on health care", 56% said the bill "gives the government too much involvement in health care", and 19% said they thought they and their families would be better off with the legislation. Other polls found that people were concerned the law would cost more than projected and would not do enough to control costs.
In a 2012 poll 44% supported the law, with 56% against. By 75% of Democrats, 27% of Independents and 14% of Republicans favored the law. 82% favored banning insurance companies from denying coverage to people with preexisting conditions, 61% favored allowing children to stay on their parents' insurance until age 26, 72% supported requiring companies with more than 50 employees to provide insurance for their employees, and 39% supported the individual mandate to own insurance or pay a penalty. By party affiliation, 19% of Republicans, 27% of Independents, and 59% of Democrats favored the mandate.
Other polls showed additional provisions receiving majority support, including the exchanges, pooling small businesses and the uninsured with other consumers and providing subsidies.
Some opponents believed the reform did not go far enough: a 2012 poll indicated that 71% of Republican opponents rejected it overall, while 29% believed it did not go far enough; independent opponents were divided 67% to 33%; and among the much smaller group of Democratic opponents, 49% rejected it overall and 51% wanted more.
In June 2013, a majority of the public (52–34%) indicated a desire for "Congress to implement or tinker with the law rather than repeal it". After the Supreme Court upheld the individual mandate, a 2012 poll held that "most Americans (56%) want to see critics of President Obama's health care law drop efforts to block it and move on to other national issues".
As of October 2013, approximately 40% were in favor while 51% were against. About 29% of
whites
White is a racialized classification of people and a skin color specifier, generally used for people of European origin, although the definition can vary depending on context, nationality, and point of view.
Description of populations as " ...
approved of the law, compared with 61% of
Hispanics
The term ''Hispanic'' ( es, hispano) refers to people, cultures, or countries related to Spain, the Spanish language, or Hispanidad.
The term commonly applies to countries with a cultural and historical link to Spain and to viceroyalties former ...
and 91% of
African American
African Americans (also referred to as Black Americans and Afro-Americans) are an ethnic group consisting of Americans with partial or total ancestry from sub-Saharan Africa. The term "African American" generally denotes descendants of ens ...
s. A solid majority of seniors opposed the idea and a solid majority of those under forty were in favor.
A 2014 poll reported that 26% of Americans support ACA. A later 2014 poll reported that 48.9% of respondents had an unfavorable view of ACA versus 38.3% who had a favorable view (of more than 5,500 individuals). Another held that 8% of respondents agreed the Affordable Care Act "is working well the way it is". In late 2014, a
Rasmussen
The surname Rasmussen () is a Danish and Norwegian surname, meaning '' Rasmus' son''. It is the ninth-most-common surname in Denmark, shared by about 1.9% of the population. poll reported Repeal: 30%, Leave as is: 13%, Improve: 52%.
In 2015, a poll reported that 47% of Americans approved the health care law. This was the first time a major poll indicated that more respondents approved than disapproved. A December 2016 poll reported that: a) 30% wanted to expand what the law does; b) 26% wanted to repeal the entire law; c) 19% wanted to move forward with implementing the law as it is; and d) 17% wanted to scale back what the law does, with the remainder undecided.
Separate polls from Fox News and NBC/''WSJ'', both taken during January 2017, indicated more people viewed the law favorably than did not for the first time. One of the reasons for the improving popularity of the law is that Democrats who had once opposed it (many still prefer "Medicare for all") shifted their positions because ACA was under threat of repeal. Another January 2017 poll reported that 35% of respondents believed "Obamacare" and the "Affordable Care Act" were different or did not know. (About 45% were unsure whether "repeal of Obamacare" also meant "repeal of the Affordable Care Act".) 39% did not know that "many people would lose coverage through Medicaid or subsidies for private health insurance if the A.C.A. were repealed and no replacement enacted," with Democrats far more likely (79%) to know that fact than Republicans (47%). A 2017 study found that personal experience with public health insurance programs led to greater support for the Affordable Care Act, most prominently among Republicans and low-information voters.
Political aspects
"Obamacare"
The term "Obamacare" was originally coined by opponents as a
pejorative
A pejorative or slur is a word or grammatical form expressing a negative or a disrespectful connotation, a low opinion, or a lack of respect toward someone or something. It is also used to express criticism, hostility, or disregard. Sometimes, a ...
. According to research by
Elspeth Reeve, the expression was used in early 2007, generally by writers describing the candidate's proposal for expanding coverage for the uninsured.
The term officially emerged in March 2007 when healthcare
lobbyist
In politics, lobbying, persuasion or interest representation is the act of lawfully attempting to influence the actions, policies, or decisions of government officials, most often legislators or members of regulatory agencies. Lobbying, which ...
Jeanne Schulte Scott wrote, "We will soon see a '
Giuliani Giuliani is an Italian family name, which can refer to:
* Carlo Giuliani, who died during the demonstrations against 2001 G8
* Carlo Giuliani (bishop), died 1663, bishop of Ston
* François Giuliani, (1938–2009) Algerian journalist and publicis ...
-care' and 'Obama-care' to go along with '
McCain-care', '
Edwards Edwards may refer to:
People
* Edwards (surname)
* Edwards family, a prominent family from Chile
* Edwards Barham (1937-2014), a former member of the Louisiana State Senate
* Edwards Pierrepont (1817–1892), an American attorney, jurist, and ora ...
-care', and a totally revamped and remodeled '
Hillary-care' from the 1990s".
In May 2007
Mitt Romney
Willard Mitt Romney (born March 12, 1947) is an American politician, businessman, and lawyer serving as the junior United States senator from Utah since January 2019, succeeding Orrin Hatch. He served as the 70th governor of Massachusetts f ...
introduced it to political discourse, saying, "How can we get those people insured without raising taxes and without having government take over healthcare?' And let me tell you, if we don't do it, the Democrats will. If the Democrats do it, it will be socialized medicine; it'll be government-managed care. It'll be what's known as Hillarycare or Barack Obamacare, or whatever you want to call it."
By mid-2012, Obamacare had become the
colloquial
Colloquialism (), also called colloquial language, everyday language or general parlance, is the linguistic style used for casual (informal) communication. It is the most common functional style of speech, the idiom normally employed in conver ...
term used both by supporters and opponents.
Obama endorsed the nickname, saying, "I have no problem with people saying Obama cares. I do care."
Common misconceptions
"Death panels"
On August 7, 2009,
Sarah Palin
Sarah Louise Palin (; Heath; born February 11, 1964) is an American politician, commentator, author, and reality television personality who served as the ninth governor of Alaska from 2006 until her resignation in 2009. She was the 2008 R ...
created the term "
death panel
"Death panel" is a political term that originated during the 2009 debate about federal health care legislation to cover the uninsured in the United States. Sarah Palin, former Republican Governor of Alaska and Vice Presidential Candidate in 20 ...
s" to describe groups who would decide whether sick patients were "worthy" of medical care.
"Death panel" referred to two claims about early drafts.
One was that under the law, seniors could be denied care due to their age and the other that the government would advise seniors to end their lives instead of receiving care. The ostensible basis of these claims was the provision for an
Independent Payment Advisory Board
The Independent Payment Advisory Board, or IPAB, was to be a fifteen-member United States Government agency created in 2010 by sections 3403 and 10320 of the Patient Protection and Affordable Care Act which was to have the explicit task of achiev ...
(IPAB).
IPAB was given the authority to recommend cost-saving changes to Medicare by facilitating the adoption of cost-effective treatments and cost-recovering measures when statutory expenditure levels were exceeded within any given three-year period. In fact, the Board was prohibited from recommending changes that would reduce payments before 2020, and was prohibited from recommending changes in premiums, benefits, eligibility and taxes, or other changes that would result in rationing.
The other related issue concerned
advance-care planning consultation:
a section of the House reform proposal would have reimbursed physicians for providing patient-requested consultations for Medicare recipients on end-of-life health planning (which is covered by many private plans), enabling patients to specify, on request, the kind of care they wished to receive. The provision was not included in ACA.
In 2010, the
Pew Research Center
The Pew Research Center is a nonpartisan American think tank (referring to itself as a "fact tank") based in Washington, D.C.
It provides information on social issues, public opinion, and demographic trends shaping the United States and the w ...
reported that 85% of Americans were familiar with the claim, and 30% believed it was true, backed by three contemporaneous polls. The allegation was named
PolitiFact
PolitiFact.com is an American nonprofit project operated by the Poynter Institute in St. Petersburg, Florida, with offices there and in Washington, D.C. It began in 2007 as a project of the ''Tampa Bay Times'' (then the ''St. Petersburg Times'' ...
's 2009 "Lie of the Year",
one of
FactCheck.org
FactCheck.org is a nonprofit website that aims to reduce the level of deception and confusion in Politics of the United States, U.S. politics by providing original research on misinformation and hoaxes. It is a project of the Annenberg Public Po ...
's "whoppers" and the most outrageous term by the
American Dialect Society
The American Dialect Society (ADS), founded in 1889, is a learned society "dedicated to the study of the English language in North America, and of other languages, or dialects of other languages, influencing it or influenced by it." The Society ...
.
AARP
AARP (formerly called the American Association of Retired Persons) is an interest group in the United States focusing on issues affecting those over the age of fifty. The organization said it had more than 38 million members in 2018. The magazin ...
described such rumors as "rife with gross—and even cruel—distortions".
Members of Congress
ACA requires members of Congress and their staffs to obtain health insurance either through an exchange or some other program approved by the law (such as Medicare), instead of using the insurance offered to federal employees (the
Federal Employees Health Benefits Program).
Illegal immigrants
ACA explicitly denies insurance subsidies to "unauthorized (illegal) aliens".
Exchange "death spiral"

Opponents claimed that combining immediate coverage with no provision for preexisting conditions would lead people to wait to get insured until they got sick. The individual mandate was designed to push people to get insured without waiting. This has been called a "death spiral". In the years after 2013, many insurers did leave specific marketplaces, claiming the risk pools were too small.
The
median
In statistics and probability theory, the median is the value separating the higher half from the lower half of a data sample, a population, or a probability distribution. For a data set, it may be thought of as "the middle" value. The basic fe ...
number of insurers per state was 4.0 in 2014, 5.0 in 2015, 4.0 in 2016 and 3.0 in 2017. Five states had one insurer in 2017, 13 had two, 11 had three; the remainder had four or more.
"If you like your plan"
At various times during and after ACA debate Obama said, "If you like your health care plan, you'll be able to keep your health care plan."
However, in fall 2013 millions of Americans with individual policies received notices that their insurance plans were terminated, and several million more risked seeing their current plans canceled.
PolitiFact cited various estimates that only about 2% of the total insured population (4million out of 262 million) received such notices. Obama's previous unambiguous assurance that consumers could keep their own plans became a focal point for critics, who challenged his truthfulness. Various bills were introduced in Congress to allow people to keep their plans. PolitiFact later scored Obama's claims as the 2013 "Lie of the Year".
Criticism and opposition
Opposition and efforts to repeal the legislation have drawn support from sources that include labor unions,
conservative
Conservatism is a cultural, social, and political philosophy that seeks to promote and to preserve traditional institutions, practices, and values. The central tenets of conservatism may vary in relation to the culture and civilization i ...
advocacy groups,
Republicans, small business organizations and the
Tea Party movement
The Tea Party movement was an American fiscally conservative political movement within the Republican Party that began in 2009. Members of the movement called for lower taxes and for a reduction of the national debt and federal budget defic ...
. These groups claimed the law would disrupt existing health plans, increase costs from new insurance standards, and increase the deficit. Some opposed the idea of
universal healthcare
Universal health care (also called universal health coverage, universal coverage, or universal care) is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized ar ...
, viewing insurance as similar to other unsubsidized goods. President
Donald Trump
Donald John Trump (born June 14, 1946) is an American politician, media personality, and businessman who served as the 45th president of the United States from 2017 to 2021.
Trump graduated from the Wharton School of the University of Pe ...
repeatedly promised to "repeal and replace" it.
unions that expressed concerns included the
AFL–CIO
The American Federation of Labor and Congress of Industrial Organizations (AFL–CIO) is the largest federation of unions in the United States. It is made up of 56 national and international unions, together representing more than 12 million ac ...
,
which called ACA "highly disruptive" to union health care plans, claiming it would drive up costs of union-sponsored plans; the
International Brotherhood of Teamsters
The International Brotherhood of Teamsters (IBT), also known as the Teamsters Union, is a labor union in the United States and Canada. Formed in 1903 by the merger of The Team Drivers International Union and The Teamsters National Union, the un ...
,
United Food and Commercial Workers International Union
The United Food and Commercial Workers International Union (UFCW) is a labor union representing approximately 1.3 million workers in the United States and Canada in industries including retail; meatpacking, food processing and manufacturing; hosp ...
, and
UNITE-HERE
UNITE HERE is a labor union in the United States and Canada with roughly 300,000 active members. The union's members work predominantly in the hotel, food service, laundry, warehouse, and casino gaming industries. The union was formed in 2004 by ...
, whose leaders sent a letter to Reid and Pelosi arguing, "PPACA will shatter not only our hard-earned health benefits, but destroy the foundation of the 40-hour work week that is the backbone of the American middle class."
In January 2014, Terry O'Sullivan, president of the
Laborers' International Union of North America
The Laborers' International Union of North America (LIUNA, stylized as LiUNA!), often shortened to just the Laborers' Union, is an American and Canadian labor union formed in 1903. As of 2017, they had about 500,000 members, about 80,000 of whom ...
(LIUNA) and D. Taylor, president of
Unite Here
UNITE HERE is a labor union in the United States and Canada with roughly 300,000 active members. The union's members work predominantly in the hotel, food service, laundry, warehouse, and casino gaming industries. The union was formed in 2004 by ...
sent a letter to Reid and Pelosi stating, "ACA, as implemented, undermines fair marketplace competition in the health care industry."
In October 2016,
Mark Dayton
Mark Brandt Dayton (born January 26, 1947) is an American politician who served as the 40th governor of Minnesota from 2011 to 2019. He was a United States Senator for Minnesota from 2001 to 2007, and the Minnesota State Auditor from 1991 to ...
, the governor of Minnesota and a member of the
Minnesota Democratic–Farmer–Labor Party
The Minnesota Democratic–Farmer–Labor Party (DFL) is the Minnesota affiliate of the U.S. Democratic Party. As of 2022, it controls four of Minnesota's eight U.S. House seats, both of its U.S. Senate seats, the Minnesota House of Represen ...
, said ACA had "many good features" but it was "no longer affordable for increasing numbers of people"; he called on the state legislature to provide emergency relief to policyholders. Dayton later said he regretted his remarks after they were seized on by Republicans seeking to repeal the law.
Legal challenges
''National Federation of Independent Business v. Sebelius''
Opponents challenged ACA's constitutionality in multiple lawsuits on multiple grounds. The Supreme Court ruled, 5–4, that the individual mandate was constitutional when viewed as a tax, although
not under the
Commerce Clause
The Commerce Clause describes an enumerated power listed in the United States Constitution ( Article I, Section 8, Clause 3). The clause states that the United States Congress shall have power "to regulate Commerce with foreign Nations, and amon ...
.
The Court further determined that states could not be forced to expand Medicaid. ACA withheld all Medicaid funding from states declining to participate in the expansion. The Court ruled that this was unconstitutionally coercive and that individual states had the right to opt out without losing preexisting Medicaid funding.
Contraception mandate
In March 2012, the
Roman Catholic Church
The Catholic Church, also known as the Roman Catholic Church, is the largest Christian church, with 1.3 billion baptized Catholics worldwide . It is among the world's oldest and largest international institutions, and has played a ...
, while supportive of ACA's objectives, voiced concern through the
United States Conference of Catholic Bishops
The United States Conference of Catholic Bishops (USCCB) is the episcopal conference of the Catholic Church in the United States. Founded in 1966 as the joint National Conference of Catholic Bishops (NCCB) and United States Catholic Conference (US ...
that aspects of the mandate covering contraception and sterilization and
HHS's narrow definition of a religious organization violated the
First Amendment
First or 1st is the ordinal form of the number one (#1).
First or 1st may also refer to:
*World record, specifically the first instance of a particular achievement
Arts and media Music
* 1$T, American rapper, singer-songwriter, DJ, and rec ...
right to
free exercise of religion
Freedom of religion or religious liberty is a principle that supports the freedom of an individual or community, in public or private, to manifest religion or belief in teaching, practice, worship, and observance. It also includes the freedom ...
and conscience. Various lawsuits addressed these concerns, including ''
Burwell v. Hobby Lobby Stores, Inc.
''Burwell v. Hobby Lobby Stores, Inc.'', 573 U.S. 682 (2014), is a List of landmark court decisions in the United States, landmark decision in United States corporate law by the Supreme Court of the United States, United States Supreme Court allow ...
'', which looked at private corporations and their duties under the ACA.
In ''
Little Sisters of the Poor Saints Peter and Paul Home v. Pennsylvania'', the Supreme Court ruled 7–2 on July 8, 2020, that employers with religious or moral objections to contraceptives can exclude such coverage from an employee's insurance plan. Writing for the majority, Justice
Clarence Thomas
Clarence Thomas (born June 23, 1948) is an American jurist who serves as an associate justice of the Supreme Court of the United States. He was nominated by President George H. W. Bush to succeed Thurgood Marshall and has served since 199 ...
said, "No language in the statute itself even hints that Congress intended that contraception should or must be covered. It was Congress, not the
dministration that declined to expressly require contraceptive coverage in the ACA itself." Justices Roberts, Alito, Gorsuch, and Kavanaugh joined Thomas's opinion. Justice
Elena Kagan
Elena Kagan ( ; born April 28, 1960) is an American lawyer who serves as an associate justice of the Supreme Court of the United States. She was nominated by President Barack Obama on May 10, 2010, and has served since August 7, 2010. Kagan ...
filed a concurring opinion in the judgment, in which
Stephen Breyer
Stephen Gerald Breyer ( ; born August 15, 1938) is a retired American lawyer and jurist who served as an associate justice of the U.S. Supreme Court from 1994 until his retirement in 2022. He was nominated by President Bill Clinton, and repl ...
joined. Justices Ginsburg and Sotomayor dissented, saying the court's ruling "leaves women workers to fend for themselves."
''King v Burwell''
On June 25, 2015, the U.S. Supreme Court ruled, 6–3, that federal subsidies for health insurance premiums could be used in the 34 states that did not set up their own insurance exchanges.
''House v. Price''
House Republicans sued the Obama administration in 2014, alleging that cost-sharing reduction subsidy payments to insurers were unlawful because Congress had not appropriated funds to pay for them. The argument classified the CSR subsidy as discretionary spending subject to annual appropriation. In May 2016, a federal judge ruled for the plaintiffs, but the Obama administration appealed. Later, President Trump ended the payments. This led to further litigation.
''United States House of Representatives v. Azar''
The House sued the administration, alleging that the money for CSRs to insurers had not been appropriated, as required for any federal government spending. The ACA subsidy that helps customers pay premiums was not part of the suit.
Without the CSRs, the government estimated that premiums would increase by 20% to 30% for silver plans. In 2017, the uncertainty about whether the payments would continue caused Blue Cross Blue Shield of North Carolina to try to raise premiums by 22.9% the next year, as opposed to an increase of 8.8% that it would have sought if the payments were assured.
U.S. District Judge
Rosemary M. Collyer
Rosemary Mayers Collyer (born November 19, 1945) is an inactive Senior United States district judge of the United States District Court for the District of Columbia,
and a Judge of the United States Foreign Intelligence Surveillance Court.
...
ruled that the cost-sharing program was unconstitutional for spending money that has not been specifically provided by an act of Congress, but concluded that Congress had in fact authorized that program to be created. The judge also found that Congress had provided authority to cover the spending for the tax credits to consumers who use them to help afford health coverage.
Collyer enjoined further cost-sharing payments, but stayed the order pending appeal to the
. The case ended in a settlement before the Circuit Court.
''California v. Texas''
Texas and 19 other states filed a civil suit in the
United States District Court for the Northern District of Texas in February 2018, arguing that with the passage of the
Tax Cuts and Jobs Act of 2017
The Act to provide for reconciliation pursuant to titles II and V of the concurrent resolution on the budget for fiscal year 2018, , is a congressional revenue act of the United States originally introduced in Congress as the Tax Cuts and Jobs A ...
, which eliminated the tax for not having health insurance, the individual mandate no longer had a constitutional basis and thus the entire ACA was no longer constitutional. The
Department of Justice
A justice ministry, ministry of justice, or department of justice is a ministry or other government agency in charge of the administration of justice. The ministry or department is often headed by a minister of justice (minister for justice in a ...
said it would no longer defend the ACA in court, but 17 states led by California stepped in to do so.
District Judge
Reed O'Connor of Texas ruled for the plaintiffs on December 14, 2018, writing that the "Individual Mandate can no longer be fairly read as an exercise of Congress's Tax Power and is still impermissible under the Interstate Commerce Clause—meaning the Individual Mandate is unconstitutional." He then further reasoned that the individual mandate is an essential part of the entire law, and thus was not severable, making the entire law unconstitutional. O'Connor's decision regarding severability turned on several passages from the Congressional debate that focused on the importance of the mandate. While he ruled the law unconstitutional, he did not overturn the law.
The intervening states appealed the decision to the
Fifth Circuit
The United States Court of Appeals for the Fifth Circuit (in case citations, 5th Cir.) is a United States federal court, federal court with appellate jurisdiction over the United States district court, district courts in the following United Stat ...
. These states argued that Congress's change in the tax was only reducing the amount of the tax, and that Congress had the power to write a stronger law to this end.
O'Connor stayed his decision pending the appeal. The Fifth Circuit heard the appeal on July 9, 2019; in the interim, the U.S. Department of Justice joined with Republican states to argue that the ACA was unconstitutional, while the Democratic states were joined by the Democrat-controlled U.S. House of Representatives. An additional question was addressed, as the Republican plaintiffs challenged the Democratic states'
standing
Standing, also referred to as orthostasis, is a position in which the body is held in an ''erect'' ("orthostatic") position and supported only by the feet. Although seemingly static, the body rocks slightly back and forth from the ankle in the s ...
to defend the ACA.
In December 2019, the Fifth Circuit agreed the individual mandate was unconstitutional, but did not agree that the entire law should be voided. Instead, it remanded the case to the District Court for reconsideration of that question. The Supreme Court accepted the case in March 2020, to be heard in the 2020–2021 term, with the ruling likely falling after the 2020 elections.
Democrats pointed out that the effect of invalidating the entire law would be to remove popular provisions such as the protection for preexisting conditions, and that the Republicans had still not offered any replacement plan—important issues in the 2020 elections.
On June 17, 2021, the Court rejected the challenge in a 7–2 decision, ruling that Texas and the other plaintiff states did not have standing to challenge the provision, leaving the full ACA intact.
Risk corridors
The Supreme Court ruled that promised risk corridor payments must be made even in the absence of specific appropriation of money by Congress.
Non-cooperation
Officials in Texas, Florida, Alabama, Wyoming, Arizona, Oklahoma and Missouri opposed those elements over which they had discretion.
For example, Missouri declined to expand Medicaid or
establish a health insurance marketplace engaging in active
non-cooperation, enacting a statute forbidding any state or local official to render any aid not specifically required by federal law.
Other Republicans discouraged efforts to advertise the law's benefits. Some conservative political groups launched ad campaigns to discourage enrollment.
Repeal efforts
ACA was the subject of many unsuccessful repeal efforts by
Republicans in the
111th,
112th, and
113th Congresses: Representatives
Steve King and
Michele Bachmann
Michele Marie Bachmann (; née Amble; born April 6, 1956) is an American politician who was the United States House of Representatives, U.S. representative for from 2007 until 2015. A member of the Republican Party (United States), Republican ...
introduced bills in the House to repeal the ACA the day after it was signed, as did Senator
Jim DeMint
James Warren DeMint (born September 2, 1951) is an American political advocate, businessman, author, and retired politician who served as a United States Senator from South Carolina and as president of the Heritage Foundation. DeMint is a member ...
in the Senate. In 2011, after Republicans gained control of the House, one of the first votes held was on a bill titled "Repealing the Job-Killing Health Care Law Act" (H.R. 2), which the House passed 245–189. All Republicans and three Democrats voted for repeal. In the Senate, the bill was offered as an amendment to an unrelated bill, but was voted down. President Obama said he would
veto
A veto is a legal power to unilaterally stop an official action. In the most typical case, a president or monarch vetoes a bill to stop it from becoming law. In many countries, veto powers are established in the country's constitution. Veto ...
the bill had it passed.
On February 3, 2015, the House of Representatives added its 67th repeal vote to the record (239 to 186). This attempt also failed.
2013 federal government shutdown
Strong partisan disagreement in Congress prevented adjustments to the Act's provisions.
But at least one change, a proposed repeal of a tax on medical devices, received bipartisan support. Some Congressional Republicans argued against improvements to the law on the grounds that they would weaken the arguments for repeal.
Republicans attempted to defund the ACA's implementation,
and in October 2013 House Republicans refused to fund the federal government unless it came with an implementation delay, after Obama unilaterally deferred the employer mandate by one year, which critics claimed he had no power to do. The House passed three versions of a bill funding the government while submitting various versions that would repeal or delay the ACA, with the last version delaying enforcement of the individual mandate. The Democratic Senate leadership said the Senate would pass only a bill without any restrictions on ACA. The
government shutdown
A government shutdown occurs when the Legislature, legislative branch does not pass key bills which fund or authorize the operations of the executive branch, resulting in the cessation of some or all operations of a government.
Government shutdo ...
lasted from October 1 to October 17.
2017 repeal effort
During a midnight congressional session starting January 11, the Senate of the
115th Congress of the United States voted to approve a "budget blueprint" that would allow
Republicans to repeal parts of the law "without threat of a
Democratic filibuster
A filibuster is a political procedure in which one or more members of a legislative body prolong debate on proposed legislation so as to delay or entirely prevent decision. It is sometimes referred to as "talking a bill to death" or "talking out ...
". The plan, which passed 51–48, was named by Senate Republicans the "Obamacare 'repeal resolution. Democrats opposing the resolution staged a protest during the vote.
House Republicans announced their replacement, the
American Health Care Act
The American Health Care Act of 2017 (often shortened to the AHCA or nicknamed Trumpcare) was a bill in the 115th United States Congress. The bill, which was passed by the United States House of Representatives but not by the United States S ...
, on March 6. On March 24, the AHCA failed amid a revolt among Republican representatives.
On May 4 the House voted to pass the AHCA by a margin of 217 to 213. The Senate Republican leadership announced that Senate Republicans would write their own version of the bill instead of voting on the House version.
Leader
Leadership, both as a research area and as a practical skill, encompasses the ability of an individual, group or organization to "lead", influence or guide other individuals, teams, or entire organizations. The word "leadership" often gets vi ...
McConnell named a group of 13 Republicans to draft the substitute version in private, raising bipartisan concerns about lack of transparency. On June 22, Republicans released the first discussion draft, which renamed it the "Better Care Reconciliation Act of 2017" (BCRA). On July 25, although no amendment proposal had garnered majority support, Republicans voted to advance the bill to the floor and begin formal consideration of amendments. Senators
Susan Collins
Susan Margaret Collins (born December 7, 1952) is an American politician serving as the senior United States senator from Maine. A member of the Republican Party, she has held her seat since 1997 and is Maine's longest-serving member of Co ...
and
Lisa Murkowski
Lisa Ann Murkowski ( ; born May 22, 1957) is an American attorney and politician serving as the senior United States senator for Alaska, having held that seat since 2002. Murkowski is the second-most senior Republican woman in the Senate, after S ...
were the only two dissenting Republicans, making the vote a 50–50 tie. Vice President
Mike Pence
Michael Richard Pence (born June 7, 1959) is an American politician who served as the 48th vice president of the United States from 2017 to 2021 under President Donald Trump. A member of the Republican Party, he previously served as the 50th ...
then cast the tie-breaking vote in the affirmative.
The revised BCRA failed, 43–57. A subsequent "Obamacare Repeal and Reconciliation Act" abandoned the "repeal and replace" approach in favor of a straight repeal, but that too failed, 45–55. Finally, the "Health Care Freedom Act", nicknamed "skinny repeal" because it would have made the least change to ACA, failed by 49–51, with Collins, Murkowski, and McCain joining all Democrats and independents in voting against it.
Actions to hinder implementation

Under both the ACA (current law) and the AHCA, the CBO reported that the health exchange marketplaces would remain stable.
But Republican politicians took a variety of steps to undermine it, creating uncertainty that adversely impacted enrollment and insurer participation while increasing premiums. Concern about the exchanges became another argument for reforms. Past and ongoing Republican attempts to weaken the law have included:
* Lawsuits such as ''
King v. Burwell
''King v. Burwell'', 576 U.S. 473 (2015), was a 6–3 decision by the Supreme Court of the United States interpreting provisions of the Patient Protection and Affordable Care Act (ACA). The Court's decision upheld, as consistent with the statute, ...
'' and ''
House v. Price
''United States House of Representatives v. Azar, et al.'' (previously ''v. Price, et al.''; originally ''v. Burwell, et al.'', also known as the ''House Republicans' lawsuit against President Obama'') was a lawsuit in which the United States Hou ...
''.
* President Trump ended the payment of
cost-sharing reduction subsidies to insurers on October 12, 2017. CBO estimated in September 2017 that discontinuing the payments would add an average of 15–20 percentage points to health insurance costs on the exchanges in 2018 while increasing the budget deficit nearly $200 billion over a decade.
In response, insurers sued the government for reimbursement. Various cases are under appeal as of 2019.
Several insurers and actuarial groups estimated this resulted in a 20 percentage point or more increase in premiums for the 2018 plan year. In other words, premium increases expected to be 10% or less in 2018 became 28–40% instead. The insurers would need to make up the $7 billion they had previously received in cost-sharing reductions (CSRs) by raising premiums. Since most premiums are subsidized, the federal government would cover most of the increases. CBO also estimated that initially up to one million fewer people would have health insurance coverage, although rising subsidies might eventually offset this. The 85% of enrollees who received subsidies would be unaffected. CBO expected the exchanges to remain stable (i.e., no "death spiral" before or after Trump's action) as the premiums would increase and prices would stabilize at the higher (non-CSR) level. Several insurance companies who sued the United States for failure to pay CSRs won cases in 2018 and 2019. The judiciary decided the insurance companies are entitled to unpaid CSRs.
* The 2015 appropriations bill had a rider that ended the payment of risk corridor funds. This was repeated in later years. This resulted in the bankruptcy of many co-ops. This action was attributed to Senator
Marco Rubio
Marco Antonio Rubio (born May 28, 1971) is an American politician and lawyer serving as the senior United States senator from Florida, a seat he has held since 2011. A member of the Republican Party, he served as Speaker of the Florida Hous ...
. The cutoff generated some 50 lawsuits. The Supreme Court granted
certiorari
In law, ''certiorari'' is a court process to seek judicial review of a decision of a lower court or government agency. ''Certiorari'' comes from the name of an English prerogative writ, issued by a superior court to direct that the record of ...
in 2019 in the case ''
Maine Community Health Options v. United States
''Maine Community Health Options v. United States'', 590 U.S. ___ (2020), was a United States Supreme Court case involving the expired Risk Corridors program of the Patient Protection and Affordable Care Act (ACA), through which the Department of ...
''.
* Trump weakened the individual mandate with his first executive order, which limited enforcement of the tax. For example, tax returns without indications of health insurance ("silent returns") will still be processed, overriding Obama's instructions to reject them.
* Trump reduced funding for advertising for exchange enrollment by up to 90%, with other reductions to support resources used to answer questions and help people sign-up for coverage. The CBO said the reductions would reduce ACA enrollment.
* Trump reduced the enrollment period for 2018 by half, to 45 days.
* Trump made public statements that the exchanges were unstable or in a
death spiral.
Socialism debate
Many economically conservative opponents called the ACA "
socialist
Socialism is a left-wing economic philosophy and movement encompassing a range of economic systems characterized by the dominance of social ownership of the means of production as opposed to private ownership. As a term, it describes the e ...
" or "
socialized medicine
Socialized medicine is a term used in the United States to describe and discuss systems of universal health care—medical and hospital care for all by means of government regulation of health care and subsidies derived from taxation. Because of ...
", pointing to the government redistribution of wealth via subsidies for low-income purchasers, expansion of the government-run Medicaid insurance, government requirements as to what products can be sold on the exchanges, and the individual mandate, which reduces freedom of consumer choice to be uninsured.
Other observers considered the law a relatively capitalist or "regulated free-market" means of paying for near-universal health care, because it creates new marketplaces with choices for consumers, largely relies on private employers and private health insurance companies, maintains private ownership of hospitals and doctor's offices, and was originally advocated for by economic conservatives as a capitalist alternative to
single-payer health care.
Some pointed out that the previous system also had socialist aspects. Even for-profit private health insurance companies socialize risk and redistribute wealth from people who have it (all premium payers) to those who need it (by paying for medically necessary healthcare).
The requirement to provide emergency care also forced redistribution from people who pay insurance premiums to those who choose to be uninsured, when they visit the emergency room.
Some Obamacare supporters accused conservatives of using the term "socialism" as a scare tactic for Obamacare as it was for Medicare and Medicaid,
and some embraced the label "socialism" as desirable, distinguishing
democratic socialism
Democratic socialism is a Left-wing politics, left-wing political philosophy that supports political democracy and some form of a socially owned economy, with a particular emphasis on economic democracy, workplace democracy, and workers' self- ...
as most desirable for education and health care, and
communism
Communism (from Latin la, communis, lit=common, universal, label=none) is a far-left sociopolitical, philosophical, and economic ideology and current within the socialist movement whose goal is the establishment of a communist society, a s ...
as undesirable.
Milos Forman opined that critics "falsely equate Western European-style socialism, and its government provision of social insurance and health care, with Marxist–Leninist totalitarianism".
Implementation
In 2010 small business tax credits took effect.
Then
Pre-Existing Condition Insurance Plan
The Pre-existing Condition Insurance Plan (PCIP) is a form of health insurance coverage offered to uninsured Americans who have been unable to obtain coverage because of a pre-existing condition. It will provide coverage to as many as 350,000 peopl ...
(PCIP) took effect to offer insurance to those who had been denied coverage by private insurance companies because of a preexisting condition.
By 2011, insurers had stopped marketing child-only policies in 17 states, as they sought to escape this requirement. In ''
National Federation of Independent Business v. Sebelius
''National Federation of Independent Business v. Sebelius'', 567 U.S. 519 (2012), was a List of landmark court decisions in the United States, landmark United States Supreme Court decision in which the Court upheld Congress's power to enact most ...
'' the Supreme Court allowed states to opt out of the Medicaid expansion.
In 2013, the
Internal Revenue Service
The Internal Revenue Service (IRS) is the revenue service for the United States federal government, which is responsible for collecting U.S. federal taxes and administering the Internal Revenue Code, the main body of the federal statutory ta ...
ruled that the cost of covering only the individual employee would be considered in determining whether the cost of coverage exceeded 9.5% of income. Family plans would not be considered even if the cost was above the 9.5% income threshold. On July2 Obama delayed the employer mandate until 2015.
The launch for both the state and federal exchanges was beset by management and technical failings.
HealthCare.gov
HealthCare.gov is a health insurance exchange website operated by the United States federal government under the Provisions of the Affordable Care Act, provisions of the Affordable Care Act or ACA, commonly referred to as “Obamacare”, which c ...
, the website that offers insurance through the exchanges operated by the federal government, crashed on opening and suffered many problems. Operations stabilized in 2014, although not all planned features were complete.
The
Government Accountability Office
The U.S. Government Accountability Office (GAO) is a legislative branch government agency that provides auditing, evaluative, and investigative services for the United States Congress. It is the supreme audit institution of the federal govern ...
released a non-partisan study in 2014 that concluded the administration had not provided "effective planning or oversight practices" in developing the exchanges.
In ''
Burwell v. Hobby Lobby
''Burwell v. Hobby Lobby Stores, Inc.'', 573 U.S. 682 (2014), is a landmark decision in United States corporate law by the United States Supreme Court allowing privately held for-profit corporations to be exempt from a regulation its owners relig ...
'' the Supreme Court exempted closely held corporations with religious convictions from the contraception rule.
At the beginning of the 2015, 11.7 million had signed up (ex-Medicaid). By the end of the year about 8.8 million consumers had stayed in the program. Congress repeatedly delayed the onset of the "
Cadillac tax
Informally, a Cadillac plan is any unusually expensive health insurance plan, usually arising in discussions of medical-cost control measures in the United States. The term derives from the Cadillac automobile, which has represented American luxury ...
" on expensive insurance plans first until 2020 and later until 2022 and repealed it in late 2019.
An estimated 9 to 10 million people had gained Medicaid coverage in 2016, mostly low-income adults. The five major national insurers expected to lose money on ACA policies in 2016, in part because the enrollees were lower income, older and sicker than expected.
More than 9.2 million people (3.0 million new customers and 6.2 million returning) enrolled on the national exchange in 2017, down some 400,000 from 2016. This decline was due primarily to the election of President Trump.
The eleven states that run their own exchanges signed up about 3million more.
The IRS announced that it would not require that tax returns indicate a person has health insurance, reducing the effectiveness of the individual mandate, in response to Trump's executive order. The CBO reported in March that the healthcare exchanges were expected to be stable.
In May the House voted to repeal ACA using the American Health Care Act. The individual mandate was repealed starting in 2019 via the Tax Cuts and Jobs Act.
The CBO estimated that the repeal would cause 13 million fewer people to have health insurance in 2027.
The 2017 Individual Market Stabilization Bill was proposed to fund cost cost-sharing reductions, provide more flexibility for state waivers, allow a new "Copper Plan" offering only catastrophic coverage, allow interstate insurance compacts, and redirect consumer fees to states for outreach. The bill failed.
By 2019, 35 states and the District of Columbia had either expanded coverage via traditional Medicaid or via an alternative program.
In popular culture
''
SNL'' presented a skit in October 2009 about the legislation's gridlock, with
Dwayne Johnson
Dwayne Douglas Johnson (born May 2, 1972), also known by his ring name The Rock, is an American actor and former professional wrestler. Widely regarded as one of the greatest professional wrestlers of all time, he was integral to the developm ...
playing an angry President Obama confronting three senators opposing the plan.
The show aired another skit in September 2013 with
Jay Pharoah
Jared Antonio Farrow (born October 14, 1987), better known by his stage name Jay Pharoah, is an American stand-up comedian, actor, and impressionist. Pharoah was a cast member on NBC's sketch comedy series ''Saturday Night Live'' from 2010 to 201 ...
as President Obama rolling out the plan to the public, and
Aaron Paul
Aaron Paul (born Aaron Paul Sturtevant; August 27, 1979) is an American actor best known for portraying Jesse Pinkman in the AMC series '' Breaking Bad'' (2008–2013), for which he won several awards, including the Critics' Choice Television ...
and other cast members playing ordinary Americans helping him in advocating for the legislation.
See also
*
Broccoli mandate
*
Comparison of the healthcare systems in Canada and the United States
*
Individual shared responsibility provision The individual shared responsibility provision, less formally known as the individual mandate, was the health insurance mandate imposed on individuals by the Affordable Care Act in the United States until tax year 2019. This individual mandate req ...
*
Massachusetts health care reform
The Massachusetts health care reform, commonly referred to as Romneycare, was a healthcare reform law passed in 2006 and signed into law by Governor Mitt Romney with the aim of providing health insurance to nearly all of the residents of the Co ...
(sometimes called "Romneycare")
*
Medicaid
Medicaid in the United States is a federal and state program that helps with healthcare costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and pers ...
*
Medicare Access and CHIP Reauthorization Act of 2015
Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), (, ) commonly called the Permanent Doc Fix, is a United States statute. Revising the Balanced Budget Act of 1997, the Bipartisan Act was the largest scale change to the American health c ...
(Reform to the American Health Care system signed into law by President Obama)
*
Single-payer health care
*
Universal health care
Universal health care (also called universal health coverage, universal coverage, or universal care) is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized ar ...
*
Universal health coverage by country
Government-guaranteed health care for all citizens of a country, sometimes called universal health care, is a broad concept that has been implemented in several ways. The common denominator for all such programs is some form of government action a ...
* U.S.
health care compared
Health, according to the World Health Organization, is "a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity".World Health Organization. (2006)''Constitution of the World Health Organiza ...
with eight other countries (tabular form)
References
Further reading
*
*
* Two volumes: This book contains an editorially enhanced version of the Patient Protection and Affordable Care Act that integrates in place changes made to it by the Reconciliation Act of 2010. ... A website, www.mediregs.com/cchhealthreform, has been created to expand access to key legislative materials.
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
Preliminary CBO documents
Patient Protection And Affordable Care Act, Incorporating The Manager's Amendment United States. Congressional Budget Office December 19, 2009. (Cost estimate)
** Effects Of The Patient Protection And Affordable Care Act On The Federal Budget And The Balance In The Hospital Insurance Trust Fund (December 23, 2009)
** Estimated Effect Of The Patient Protection And Affordable Care Act (Incorporating The Manager's Amendment) On The Hospital Insurance Trust Fund (December 23, 2009)
Base Analysis—H.R. 3590, Patient Protection and Affordable Care Act United States. Congressional Budget Office. November 18, 2009. (Cost estimate)
(The additional and/or related CBO reporting that follows can be accessed from the above link)
** Estimated Distribution Of Individual Mandate Penalties (November 20, 2009)
** Estimated Effects On Medicare Advantage Enrollment And Benefits Not Covered By Medicare (November 21, 2009)
** Estimated Effects On The Status Of The Hospital Insurance Trust Fund (November 21, 2009)
** Estimated Average Premiums Under Current Law (December 5, 2009)
** Additional Information About Employment-Based Coverage (December 7, 2009)
** Budgetary Treatment Of Proposals To Regulate Medical Loss Ratios (December 13, 2009)
CMS Estimates of the impact of P.L. 111-148
Estimated Financial Effects of the "Patient Protection and Affordable Care Act", as Amended April 22, 2010.
Estimated Effects of the "Patient Protection and Affordable Care Act", as Amended, on the Year of Exhaustion for the Part A Trust Fund, Part B Premiums, and Part A and Part B Coinsurance Amounts April 22, 2010.
CMS Estimates of the impact of H.R. 3590
Estimated Financial Effects of the "Patient Protection and Affordable Care Act of 2009", as Proposed by the Senate Majority Leader on November 18, 2009 December 10, 2009.
Estimated Effects of the "Patient Protection and Affordable Care Act" on the Year of Exhaustion for the Part A Trust Fund, Part B Premiums, and Part A and Part B Coinsurance Amounts December 10, 2009.
Senate Finance Committee meetings
Senate Finance Committee Hearings for the 111th Congress recorded by C-SPAN also available fro
Finance.Senate.Gov (accessed April 1, 2012).
External links
ACA text
Patient Protection and Affordable Care ActPDFdetails
as amended in the GPO GPO may refer to:
Government and politics
* General Post Office, Dublin
* General Post Office, in Britain
* Social Security Government Pension Offset, a provision reducing benefits
* Government Pharmaceutical Organization, a Thai state enterpris ...
br>Statute Compilations collection
Full text, summary, background, provisions and more
via Democratic Policy Committee (Senate.gov)
{{Authority control
Excises
Healthcare reform legislation in the United States
Internal Revenue Code
Internal Revenue Service
Obama administration controversies
Presidency of Barack Obama
United States federal health legislation
Omnibus legislation
Acts of the 111th United States Congress
March 2010 events in the United States

 ACA amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into
ACA amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into  ACA followed a long series of unsuccessful attempts by one party or the other to pass major insurance reforms. Innovations were limited to
ACA followed a long series of unsuccessful attempts by one party or the other to pass major insurance reforms. Innovations were limited to  The 1993 Republican Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'. Advocates included prominent Republican senators such as
The 1993 Republican Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'. Advocates included prominent Republican senators such as  In 2006, an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an insurance exchange. Republican Governor
In 2006, an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an insurance exchange. Republican Governor  Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform. By July, a series of bills were approved by committees within the
Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform. By July, a series of bills were approved by committees within the  During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals. The nascent
During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals. The nascent 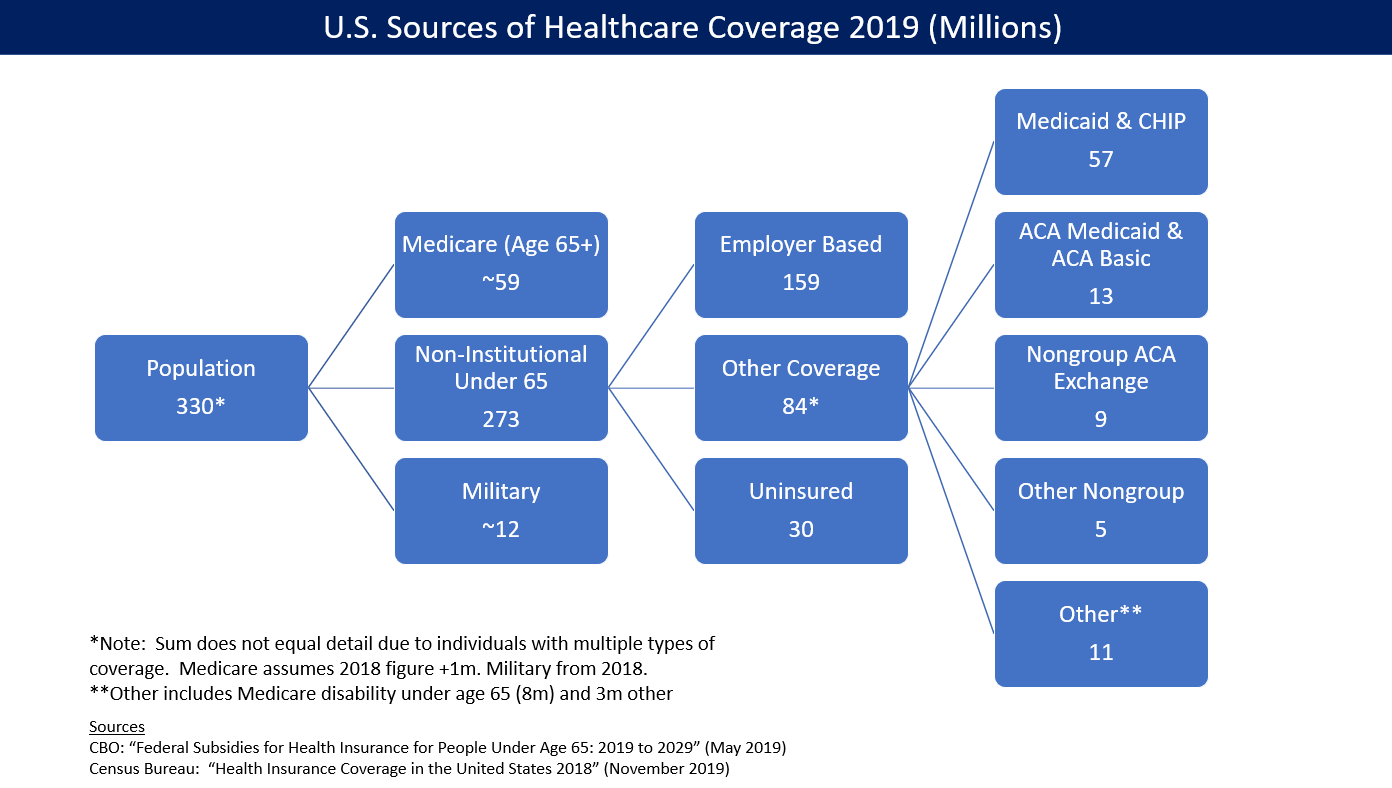

 As of December 2019, 37 states (including Washington DC) had adopted the Medicaid extension. Those states that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while the others had a 14.1% uninsured rate, among adults aged 18 to 64. Following the Supreme Court ruling in 2012, which held that states would not lose Medicaid funding if they did not expand Medicaid under ACA, several states rejected the option. Over half the national uninsured population lived in those states.
The
As of December 2019, 37 states (including Washington DC) had adopted the Medicaid extension. Those states that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while the others had a 14.1% uninsured rate, among adults aged 18 to 64. Following the Supreme Court ruling in 2012, which held that states would not lose Medicaid funding if they did not expand Medicaid under ACA, several states rejected the option. Over half the national uninsured population lived in those states.
The  National health care expenditures rose faster than national income both before (2009-2013: 3.73%) and after (2014-2018: 4.82%) ACA's major provisions took effect. Premium prices rose considerably before and after. For example, a study published in 2016 found that the average requested 2017 premium increase among 40-year-old non-smokers was about 9percent, according to an analysis of 17 cities, although Blue Cross Blue Shield proposed increases of 40 percent in Alabama and 60 percent in Texas. However, some or all these costs were offset by tax credits. For example, the
National health care expenditures rose faster than national income both before (2009-2013: 3.73%) and after (2014-2018: 4.82%) ACA's major provisions took effect. Premium prices rose considerably before and after. For example, a study published in 2016 found that the average requested 2017 premium increase among 40-year-old non-smokers was about 9percent, according to an analysis of 17 cities, although Blue Cross Blue Shield proposed increases of 40 percent in Alabama and 60 percent in Texas. However, some or all these costs were offset by tax credits. For example, the  In March 2018, the CBO reported that ACA had reduced income inequality in 2014, saying the law led the lowest and second quintiles (the bottom 40%) to receive an average of an additional $690 and $560 respectively while causing households in the top 1% to pay an additional $21,000 due mostly to the net investment income tax and the additional Medicare tax. The law placed relatively little burden on households in the top quintile (top 20%) outside of the top 1%.
In March 2018, the CBO reported that ACA had reduced income inequality in 2014, saying the law led the lowest and second quintiles (the bottom 40%) to receive an average of an additional $690 and $560 respectively while causing households in the top 1% to pay an additional $21,000 due mostly to the net investment income tax and the additional Medicare tax. The law placed relatively little burden on households in the top quintile (top 20%) outside of the top 1%.
 CBO estimated in June 2015 that repealing ACA would:
* Decrease GDP in the short-term, as government spending (on subsidies) was only partially replaced by spending by recipients.
* Increase the supply of labor and aggregate compensation by about 0.8 and 0.9 percent over the 2021–2025 period. CBO cited ACA's expanded eligibility for Medicaid and subsidies and tax credits that rise with income as disincentives to work, so repealing ACA would remove those disincentives, encouraging workers to supply more labor, increasing the total number of hours worked by about 1.5% over the 2021–2025 period.
* Remove the higher tax rates on capital income, thereby encouraging investment, raising the capital stock and output in the long-run.
In 2015 the progressive
CBO estimated in June 2015 that repealing ACA would:
* Decrease GDP in the short-term, as government spending (on subsidies) was only partially replaced by spending by recipients.
* Increase the supply of labor and aggregate compensation by about 0.8 and 0.9 percent over the 2021–2025 period. CBO cited ACA's expanded eligibility for Medicaid and subsidies and tax credits that rise with income as disincentives to work, so repealing ACA would remove those disincentives, encouraging workers to supply more labor, increasing the total number of hours worked by about 1.5% over the 2021–2025 period.
* Remove the higher tax rates on capital income, thereby encouraging investment, raising the capital stock and output in the long-run.
In 2015 the progressive  Public views became increasingly negative in reaction to specific plans discussed during the legislative debate over 2009 and 2010. Approval varied by party, race and age. Some elements were more widely favored (preexisting conditions) or opposed (individual mandate).
In a 2010
Public views became increasingly negative in reaction to specific plans discussed during the legislative debate over 2009 and 2010. Approval varied by party, race and age. Some elements were more widely favored (preexisting conditions) or opposed (individual mandate).
In a 2010  Opponents claimed that combining immediate coverage with no provision for preexisting conditions would lead people to wait to get insured until they got sick. The individual mandate was designed to push people to get insured without waiting. This has been called a "death spiral". In the years after 2013, many insurers did leave specific marketplaces, claiming the risk pools were too small.
The
Opponents claimed that combining immediate coverage with no provision for preexisting conditions would lead people to wait to get insured until they got sick. The individual mandate was designed to push people to get insured without waiting. This has been called a "death spiral". In the years after 2013, many insurers did leave specific marketplaces, claiming the risk pools were too small.
The  Under both the ACA (current law) and the AHCA, the CBO reported that the health exchange marketplaces would remain stable. But Republican politicians took a variety of steps to undermine it, creating uncertainty that adversely impacted enrollment and insurer participation while increasing premiums. Concern about the exchanges became another argument for reforms. Past and ongoing Republican attempts to weaken the law have included:
* Lawsuits such as ''
Under both the ACA (current law) and the AHCA, the CBO reported that the health exchange marketplaces would remain stable. But Republican politicians took a variety of steps to undermine it, creating uncertainty that adversely impacted enrollment and insurer participation while increasing premiums. Concern about the exchanges became another argument for reforms. Past and ongoing Republican attempts to weaken the law have included:
* Lawsuits such as ''