Hemolytic Plaque Technique on:
[Wikipedia]
[Google]
[Amazon]

 Hemolysis or haemolysis (), also known by several other names, is the rupturing (
Hemolysis or haemolysis (), also known by several other names, is the rupturing (
 '' In vitro'' hemolysis can be caused by improper technique during collection of blood specimens, by the effects of mechanical processing of blood, or by bacterial action in cultured blood specimens.
'' In vitro'' hemolysis can be caused by improper technique during collection of blood specimens, by the effects of mechanical processing of blood, or by bacterial action in cultured blood specimens.
 Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various
Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various
 Material was copied from this source, which is available under a Creative Commons License. It may also lead to increased levels of the heme breakdown product stercobilin in the stool.
Splenectomy of those with hemolytic disorders appears to increase risk of developing
Material was copied from this source, which is available under a Creative Commons License. It may also lead to increased levels of the heme breakdown product stercobilin in the stool.
Splenectomy of those with hemolytic disorders appears to increase risk of developing
Effects of Hemolysis on Clinical Specimens
Hematology

 Hemolysis or haemolysis (), also known by several other names, is the rupturing (
Hemolysis or haemolysis (), also known by several other names, is the rupturing (lysis
Lysis ( ) is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ''lysate''. In molecular bio ...
) of red blood cells (erythrocytes) and the release of their contents ( cytoplasm) into surrounding fluid (e.g. blood plasma). Hemolysis may occur in vivo or in vitro.
One cause of hemolysis is the action of hemolysins, toxins that are produced by certain pathogenic bacteria
Pathogenic bacteria are bacteria that can cause disease. This article focuses on the bacteria that are pathogenic to humans. Most species of bacteria are harmless and are often Probiotic, beneficial but others can cause infectious diseases. The n ...
or fungi. Another cause is intense physical exercise. Hemolysins damage the red blood cell's cytoplasmic membrane, causing lysis and eventually cell death.
Etymology
From hemo- + -lysis, from , "blood") + , "loosening").Inside the body
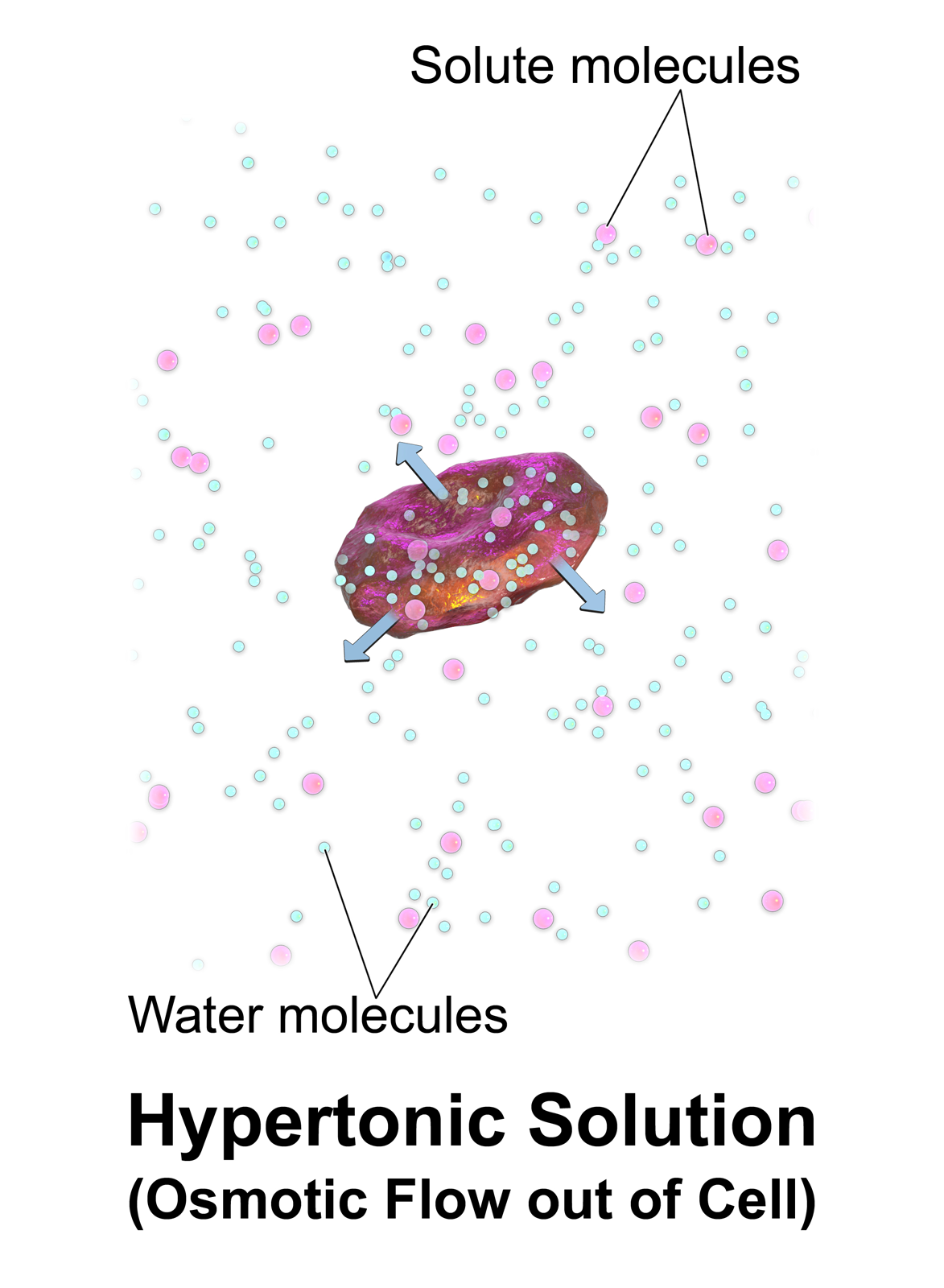
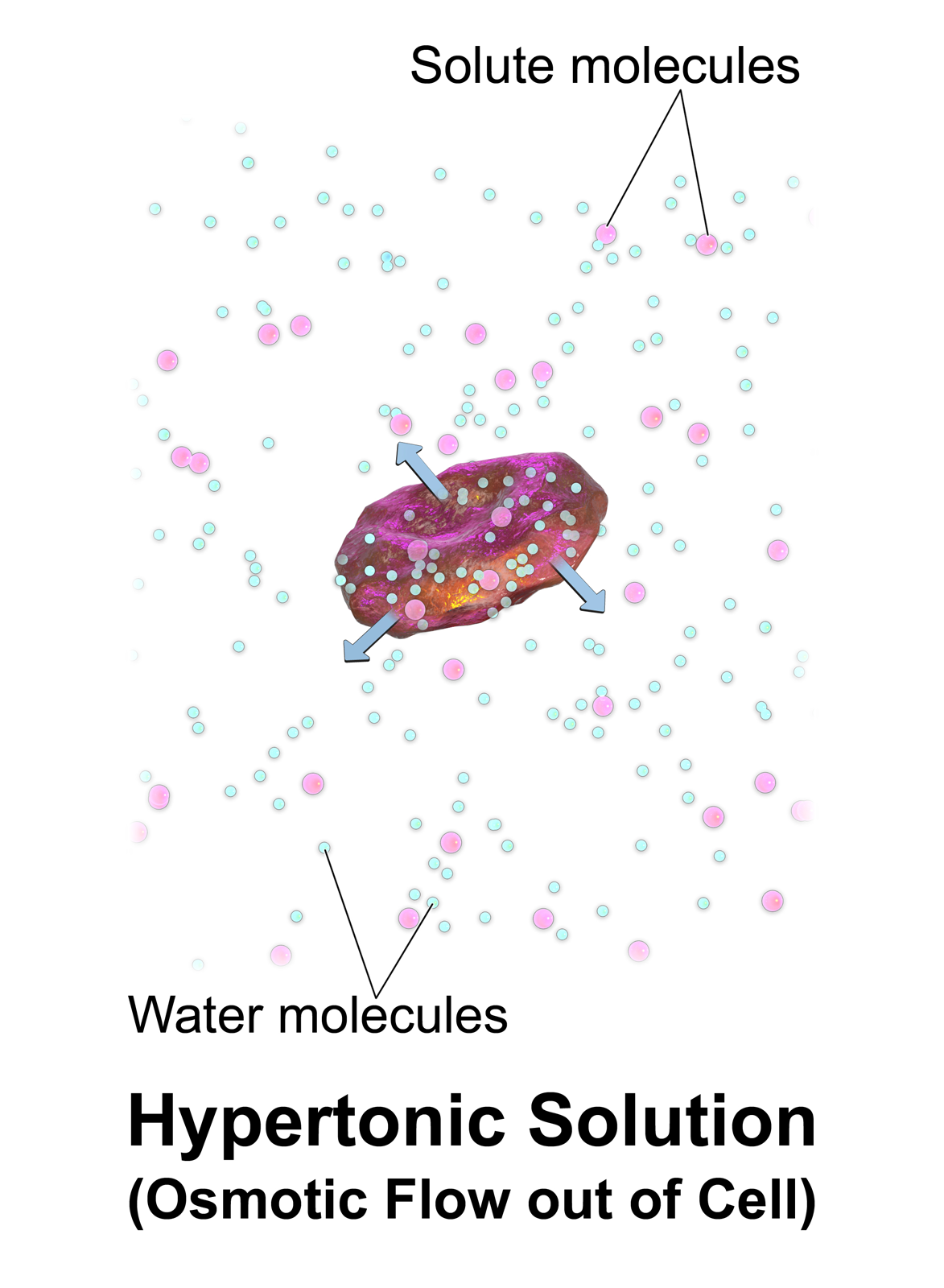
Hemolysis inside the body can be caused by a large number of medical conditions, including some parasites (''e.g.'', '' Plasmodium''), some autoimmune disorders (''e.g.'', autoimmune haemolytic anaemia, drug-induced hemolytic anemia, atypical hemolytic uremic syndrome (aHUS)), some genetic disorders (''e.g.'', Sickle-cell disease or G6PD deficiency), or blood with too low a solute concentration ( hypotonic to cells). Hemolysis can lead to hemoglobinemia due to hemoglobin released into the blood plasma, which plays a significant role in the pathogenesis of sepsis and can lead to increased risk of infection due to its inhibitory effects on theinnate immune system
The innate, or nonspecific, immune system is one of the two main immunity strategies (the other being the adaptive immune system) in vertebrates. The innate immune system is an older evolutionary defense strategy, relatively speaking, and is the ...
.
Parasitic hemolysis
Because the feeding process of the '' Plasmodium'' parasites damages red blood cells, malaria is sometimes called "parasitic hemolysis" in medical literature.HELLP, pre-eclampsia, or eclampsia
:See HELLP syndrome,Pre-eclampsia
Pre-eclampsia is a disorder of pregnancy characterized by the onset of high blood pressure and often a significant amount of protein in the urine. When it arises, the condition begins after 20 weeks of pregnancy. In severe cases of the disease ...
, and Eclampsia
Hemolytic disease of the newborn
Hemolytic disease of the newborn is an autoimmune disease resulting from the mother's antibodies crossing the placenta to the fetus. This most often occurs when the mother has previously been exposed to blood antigens present on the fetus but foreign to her, through either a blood transfusion or a previous pregnancy.Hemolytic anemia
Because ''in vivo'' hemolysis destroys red blood cells, in uncontrolled, chronic or severe cases it can lead to hemolytic anemia.Hemolytic crisis
A hemolytic crisis, or hyperhemolytic crisis, is characterized by an accelerated rate of red blood cell destruction leading to anemia,jaundice
Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme meta ...
, and reticulocytosis
Reticulocytosis is a condition where there is an increase in reticulocytes, immature red blood cells.
It is commonly seen in anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry ...
. Hemolytic crises are a major concern with sickle-cell disease and G6PD deficiency.
Toxic agent ingestion or poisoning
'' Paxillus involutus'' ingestion can cause hemolysis.Space hemolysis
Spaceflight can cause hemolysis.Intrinsic causes
Hemolysis may result from intrinsic defects in the red blood cell itself: * Defects of red blood cell membrane production (as in hereditary spherocytosis and hereditary elliptocytosis) * Defects in hemoglobin production (as inthalassemia
Thalassemias are inherited blood disorders characterized by decreased hemoglobin production. Symptoms depend on the type and can vary from none to severe. Often there is mild to severe anemia (low red blood cells or hemoglobin). Anemia can result ...
, sickle-cell disease and congenital dyserythropoietic anemia
Congenital dyserythropoietic anemia (CDA) is a rare blood disorder, similar to the thalassemias. CDA is one of many types of anemia, characterized by ineffective erythropoiesis, and resulting from a decrease in the number of red blood cells (RBCs) ...
)
* Defective red cell metabolism (as in glucose-6-phosphate dehydrogenase deficiency and pyruvate kinase deficiency)
* Paroxysmal nocturnal hemoglobinuria (PNH), sometimes referred to as Marchiafava-Micheli syndrome, is a rare, acquired, potentially life-threatening disease of the blood characterized by complement-induced intravascular hemolytic anemia.
Extrinsic causes
Extrinsic hemolysis is caused by the red blood cell's environment: * Immune-mediated causes could include transient factors as in '' Mycoplasma pneumoniae'' infection ( cold agglutinin disease) or permanent factors as inautoimmune disease
An autoimmune disease is a condition arising from an abnormal immune response to a functioning body part. At least 80 types of autoimmune diseases have been identified, with some evidence suggesting that there may be more than 100 types. Nearly a ...
s like autoimmune hemolytic anemia (itself more common in diseases such as systemic lupus erythematosus
Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Comm ...
, rheumatoid arthritis, Hodgkin's lymphoma, and chronic lymphocytic leukemia
Chronic lymphocytic leukemia (CLL) is a type of cancer in which the bone marrow makes too many lymphocytes (a type of white blood cell). Early on, there are typically no symptoms. Later, non-painful lymph node swelling, feeling tired, fever, nigh ...
).
* Spur cell hemolytic anemia Spur cell hemolytic anemia, Chronic liver disease impairs the liver's ability to esterify cholesterol, causing free cholesterol to bind to the red cell membrane, increasing its surface area without increasing its volume. This condition also creates ...
* Any of the causes of hypersplenism
Splenomegaly is an enlargement of the spleen. The spleen usually lies in the left upper quadrant (LUQ) of the human abdomen. Splenomegaly is one of the four cardinal signs of ''hypersplenism'' which include: some reduction in number of circulati ...
(increased activity of the spleen), such as portal hypertension
Portal hypertension is abnormally increased portal venous pressure – blood pressure in the portal vein and its branches, that drain from most of the intestine to the liver. Portal hypertension is defined as a hepatic venous pressure gradient gr ...
.
* Acquired hemolytic anemia is also encountered in burns and as a result of certain infections (e.g. malaria).
* Lead poisoning
Lead poisoning, also known as plumbism and saturnism, is a type of metal poisoning caused by lead in the body. The brain is the most sensitive. Symptoms may include abdominal pain, constipation, headaches, irritability, memory problems, inferti ...
or poisoning by arsine or stibine
Stibine (IUPAC name: stibane) is a chemical compound with the formula SbH3. A pnictogen hydride, this colourless, highly toxic gas is the principal covalent hydride of antimony, and a heavy analogue of ammonia. The molecule is pyramidal with H–S ...
causes non-immune hemolytic anemia.
* Runners
Running is a method of terrestrial locomotion allowing humans and other animals to move rapidly on foot. Running is a type of gait characterized by an aerial phase in which all feet are above the ground (though there are exceptions). This is ...
can develop hemolytic anemia due to " footstrike hemolysis", the destruction of red blood cells in feet at foot impact.
* Low-grade hemolytic anemia occurs in 70% of prosthetic heart valve recipients, and severe hemolytic anemia occurs in 3%.
Intravascular hemolysis
Intravascular hemolysis describes hemolysis that happens mainly inside the vasculature. As a result, the contents of the red blood cell are released into the general circulation, leading to hemoglobinemia and increasing the risk of ensuinghyperbilirubinemia
Bilirubin (BR) (Latin for "red bile") is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from the ...
.
Intravascular hemolysis may occur when red blood cells are targeted by autoantibodies
An autoantibody is an antibody (a type of protein) produced by the immune system that is directed against one or more of the individual's own proteins. Many autoimmune diseases (notably lupus erythematosus) are associated with such antibodies.
Pr ...
, leading to complement fixation, or by damage by parasites such as '' Babesia''. Additionally, thrombotic microangiopathy (TMA) can result in hemolysis of red blood cells. TMA is frequently observed in aHUS patients where clots form in the small vessels of the kidney resulting in damaged red blood cells as they attempt to pass through the restricted vessels.
Extravascular hemolysis
Extravascular hemolysis refers to hemolysis taking place in the liver, spleen,bone marrow
Bone marrow is a semi-solid tissue found within the spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It is composed of hematopoietic ce ...
, and lymph nodes. In this case little hemoglobin escapes into blood plasma. The macrophages of the reticuloendothelial system in these organs engulf and destroy structurally-defective red blood cells, or those with antibodies attached, and release unconjugated bilirubin into the blood plasma circulation. Typically, the spleen destroys mildly abnormal red blood cells or those coated with IgG-type antibodies, while severely abnormal red blood cells or those coated with IgM-type antibodies are destroyed in the circulation or in the liver.
If extravascular hemolysis is extensive, hemosiderin can be deposited in the spleen, bone marrow, kidney, liver, and other organs, resulting in hemosiderosis.
Outside the body
 '' In vitro'' hemolysis can be caused by improper technique during collection of blood specimens, by the effects of mechanical processing of blood, or by bacterial action in cultured blood specimens.
'' In vitro'' hemolysis can be caused by improper technique during collection of blood specimens, by the effects of mechanical processing of blood, or by bacterial action in cultured blood specimens.
From specimen collection
Most causes of ''in vitro'' hemolysis are related to specimen collection. Difficult collections, unsecure line connections, contamination, and incorrect needle size, as well as improper tube mixing and incorrectly filled tubes are all frequent causes of hemolysis. Excessive suction can cause the red blood cells to be smashed on their way through the hypodermic needle owing to turbulence and physical forces. Such hemolysis is more likely to occur when a patient's veins are difficult to find or when they collapse when blood is removed by a syringe or a modern vacuum tube. Experience and proper technique are key for any phlebotomist, nurse or doctor to prevent hemolysis. ''In vitro'' hemolysis during specimen collection can cause inaccurate laboratory test results by contaminating the surrounding plasma with the contents of hemolyzed red blood cells. For example, the concentration of potassium inside red blood cells is much higher than in the plasma and so an elevated potassium level is usually found in biochemistry tests of hemolyzed blood. After the blood collection process, ''in vitro'' hemolysis can still occur in a sample due to external factors, such as prolonged storage, incorrect storage conditions and excessive physical forces by dropping or vigorously mixing the tube.From mechanical blood processing during surgery
In some surgical procedures (especially some heart operations) where substantial blood loss is expected, machinery is used for intraoperative blood salvage. A centrifuge process takes blood from the patient, washes the red blood cells with normal saline, and returns them to the patient's blood circulation. Hemolysis may occur if the centrifuge rotates too quickly (generally greater than 500 rpm)—essentially this is hemolysis occurring outside of the body. Increased hemolysis occurs with massive amounts of sudden blood loss, because the process of returning a patient's cells must be done at a correspondingly higher speed to prevent hypotension, pH imbalance, and a number of other hemodynamic and blood level factors. Modeling of fluid flows to predict the likelihood of red cell membrane rupture in response to stress is an active area of research.From bacteria culture
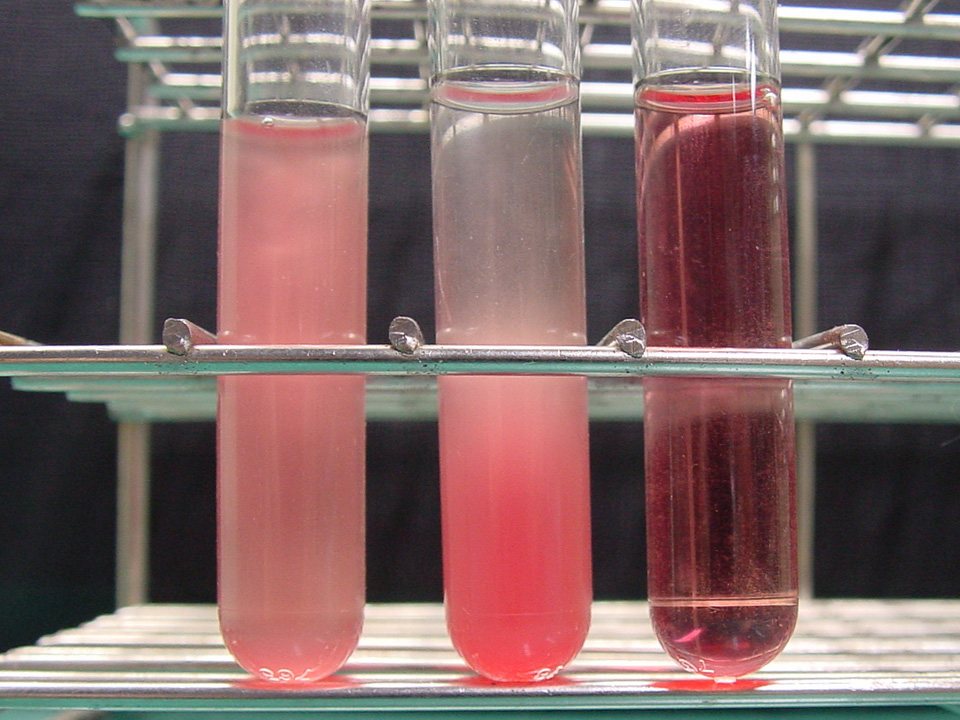
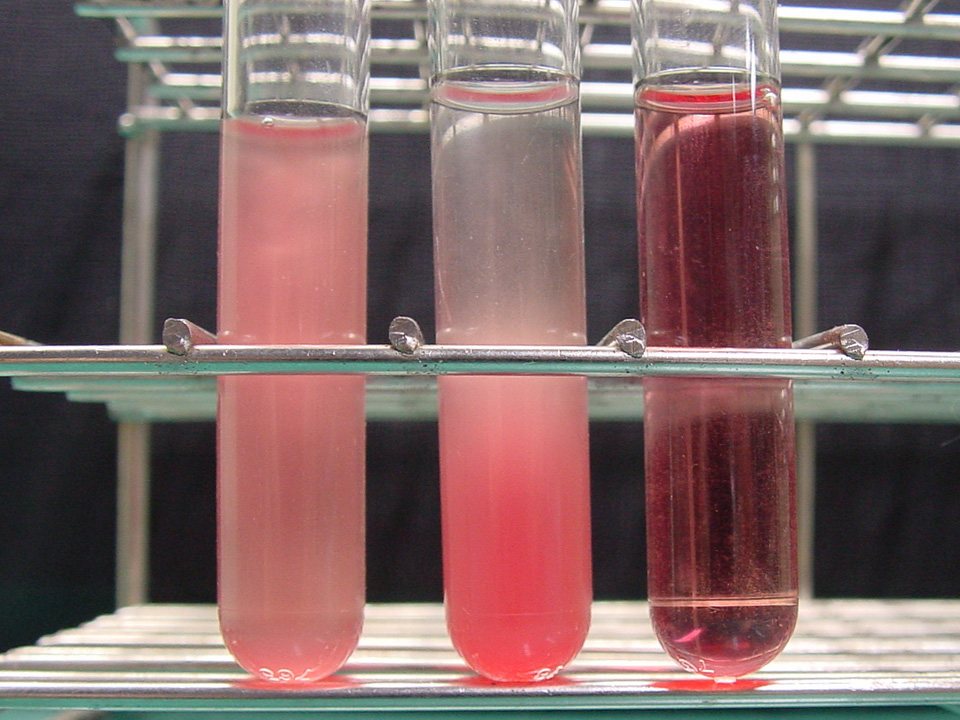
 Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various
Visualizing the physical appearance of hemolysis in cultured blood samples may be used as a tool to determine the species of various Gram-positive bacteria
In bacteriology, gram-positive bacteria are bacteria that give a positive result in the Gram stain test, which is traditionally used to quickly classify bacteria into two broad categories according to their type of cell wall.
Gram-positive bact ...
infections (''e.g.'', '' Streptococcus'').
Nomenclature
Hemolysis is sometimes called hematolysis, erythrolysis, or erythrocytolysis. The words ''hemolysis'' () and ''hematolysis'' () both use combining forms conveying the idea of "lysis
Lysis ( ) is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ''lysate''. In molecular bio ...
of blood" ('' hemo-'' or '' hemato-'' + '' -lysis''). The words ''erythrolysis'' () and ''erythrocytolysis'' () both use combining forms conveying the idea of "lysis
Lysis ( ) is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ''lysate''. In molecular bio ...
of erythrocytes" ('' erythro-'' ± '' cyto-'' + '' -lysis'').
Red blood cells (erythrocytes) have a short lifespan (approximately 120 days), and old ( senescent) cells are constantly removed and replaced with new ones via erythropoiesis. This breakdown/replacement process is called erythrocyte turnover. In this sense, erythrolysis or hemolysis is a normal process that happens continually. However, these terms are usually used to indicate that the lysis is pathological.
Complications
Pulmonary hypertension has been gaining recognition as a complication of chronic hereditary and acquired hemolysis. Free hemoglobin released during hemolysis inactivates thevasodilator
Vasodilation is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. The process is the opposite of vasoconstriction, ...
nitric oxide (NO). Hemolysis also releases arginase that depletes L-arginine, the substrate needed for NO synthesis. This reduces NO-dependent vasodilation and induces platelet activation, thrombin generation, procoagulant factors and tissue factor
Tissue factor, also called platelet tissue factor, factor III, or CD142, is a protein encoded by the ''F3'' gene, present in subendothelial tissue and leukocytes. Its role in the clotting process is the initiation of thrombin formation from the ...
activation, contributing to the formation of thrombosis. This can lead to esophageal spasm and dysphagia, abdominal pain, erectile dysfunction
Erectile dysfunction (ED), also called impotence, is the type of sexual dysfunction in which the penis fails to become or stay erect during sexual activity. It is the most common sexual problem in men.Cunningham GR, Rosen RC. Overview of male ...
, systemic hypertension, decreased organ perfusion, promotion of inflammation and coagulation, and thrombosis.
Chronic hemolysis may also lead to endothelial dysfunction, heightened endothelin-1-mediated responses and vasculopathy. The release of heme leads to the production of bilirubin
Bilirubin (BR) (Latin for "red bile") is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from the ...
and depletion of plasma proteins, such as albumin, haptoglobin, and hemopexin, which may lead to jaundice
Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme meta ...
. pulmonary thrombosis
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathin ...
.
Complications may also arise from the increased workload for the kidney as it secretes erythropoietin
Erythropoietin (; EPO), also known as erythropoetin, haematopoietin, or haemopoietin, is a glycoprotein cytokine secreted mainly by the kidneys in response to cellular hypoxia; it stimulates red blood cell production (erythropoiesis) in the bo ...
to stimulate the bone marrow
Bone marrow is a semi-solid tissue found within the spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It is composed of hematopoietic ce ...
to produce more reticulocytes (red blood cell precursors) to compensate for the loss of red blood cells due to hemolysis.
See also
* Hemolysin * Glucose-6-phosphate dehydrogenase deficiencyReferences
External links
{{Medical resources , ICD10 = , ICD9 = , ICDO = , OMIM = , DiseasesDB = , MedlinePlus = , eMedicineSubj = , eMedicineTopic = , MeshID = D006461 , GeneReviewsNBK = , GeneReviewsName = , NORD = , GARDNum = , GARDName = , Orphanet = , AO = , RP = , WO = , OrthoInfo = , NCI = , Scholia = , SNOMED CT =Effects of Hemolysis on Clinical Specimens
Hematology