Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
In undamaged skin, the
epidermis
The epidermis is the outermost of the three layers that comprise the skin, the inner layers being the dermis and Subcutaneous tissue, hypodermis. The epidermis layer provides a barrier to infection from environmental pathogens and regulates the ...
(surface,
epithelia
Epithelium or epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. It is a thin, continuous, protective layer of compactly packed cells with a little intercellular ...
l layer) and
dermis (deeper,
connective layer) form a protective barrier against the external environment. When the barrier is broken, a regulated sequence of biochemical events is set into motion to repair the damage.
This process is divided into predictable phases: blood clotting (
hemostasis
In biology, hemostasis or haemostasis is a process to prevent and stop bleeding, meaning to keep blood within a damaged blood vessel (the opposite of hemostasis is hemorrhage). It is the first stage of wound healing. This involves coagulation, wh ...
),
inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
, tissue growth (
cell proliferation), and tissue remodeling (maturation and
cell differentiation
Cellular differentiation is the process in which a stem cell alters from one type to a differentiated one. Usually, the cell changes to a more specialized type. Differentiation happens multiple times during the development of a multicellula ...
). Blood clotting may be considered to be part of the inflammation stage instead of a separate stage.
The wound healing process is not only complex but fragile, and it is susceptible to interruption or failure leading to the formation of non-healing
chronic wound A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic.
Chronic wounds seem to be detained in on ...
s. Factors that contribute to non-healing chronic wounds are diabetes, venous or arterial disease, infection, and metabolic deficiencies of old age.
[Enoch, S. Price, P. (2004)]
''Cellular, molecular and biochemical differences in the pathophysiology of healing between acute wounds, chronic wounds and wounds in the elderly''
.
Wound care encourages and speeds wound healing via cleaning and protection from reinjury or infection. Depending on each patient's needs, it can range from the simplest
first aid
First aid is the first and immediate assistance given to any person with either a minor or serious illness or injury, with care provided to preserve life, prevent the condition from worsening, or to promote recovery. It includes initial in ...
to entire nursing specialties such as
wound, ostomy, and continence nursing Wound, ostomy, and continence nursing is a nursing specialty involved with the treatment of patients with acute and chronic wounds, patients with an ostomy (those who have had some kind of bowel or bladder diversion), and patients with incontinence ...
and
burn center
A burn center, burn unit, or burns unit is a hospital specializing in the treatment of burns. Burn centers are often used for the treatment and recovery of patients with more severe burns.
Overview
The severity of a burn, and therefore whethe ...
care.
Stages
* Hemostasis (blood clotting): Within the first few minutes of injury,
platelets
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby i ...
in the blood begin to stick to the injured site. They change into an amorphous shape, more suitable for clotting, and they release chemical signals to promote clotting. This results in the activation of
fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with pla ...
, which forms a mesh and acts as "glue" to bind platelets to each other. This makes a
clot
A thrombus (plural thrombi), colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of c ...
that serves to plug the break in the blood vessel, slowing/preventing further bleeding.
* Inflammation: During this phase, damaged and dead cells are cleared out, along with bacteria and other pathogens or debris. This happens through the process of
phagocytosis
Phagocytosis () is the process by which a cell uses its plasma membrane to engulf a large particle (≥ 0.5 μm), giving rise to an internal compartment called the phagosome. It is one type of endocytosis. A cell that performs phagocytosis i ...
, where white blood cells engulf debris and destroy it.
Platelet-derived growth factor
Platelet-derived growth factor (PDGF) is one among numerous growth factors that regulate cell growth and division. In particular, PDGF plays a significant role in blood vessel formation, the growth of blood vessels from already-existing blood ...
s are released into the wound that cause the migration and division of cells during the proliferative phase.
* Proliferation (growth of new tissue): In this phase,
angiogenesis,
collagen deposition,
granulation tissue
Granulation tissue is new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. Granulation tissue typically grows from the base of a wound and is able to fill wounds of almost any size ...
formation, epithelialization, and wound contraction occur.
In angiogenesis, vascular endothelial cells form new blood vessels.
In fibroplasia and granulation tissue formation,
fibroblast
A fibroblast is a type of biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework ( stroma) for animal tissues, and plays a critical role in wound healing. Fibroblasts are the most common cells of ...
s grow and form a new, provisional
extracellular matrix
In biology, the extracellular matrix (ECM), also called intercellular matrix, is a three-dimensional network consisting of extracellular macromolecules and minerals, such as collagen, enzymes, glycoproteins and hydroxyapatite that provide struc ...
(ECM) by excreting collagen and
fibronectin
Fibronectin is a high-molecular weight (~500-~600 kDa) glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. Fibronectin also binds to other extracellular matrix proteins such as collagen ...
.
Concurrently, re-epithelialization of the epidermis occurs, in which
epithelial cell
Epithelium or epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. It is a thin, continuous, protective layer of compactly packed cells with a little intercell ...
s proliferate and 'crawl' atop the wound bed, providing cover for the new tissue.
[Garg, H.G. (2000). ''Scarless Wound Healing''. New York Marcel Dekker, Inc. Electronic book.] In wound contraction,
myofibroblast
A myofibroblast is a cell phenotype that was first described as being in a state between a fibroblast and a smooth muscle cell.
Structure
Myofibroblasts are contractile web-like fusiform cells that are identifiable by their expression of α-sm ...
s decrease the size of the wound by gripping the wound edges and contracting using a mechanism that resembles that in smooth muscle cells. When the cells' roles are close to complete, unneeded cells undergo
apoptosis.
* Maturation (remodeling): During maturation and remodeling, collagen is realigned along tension lines, and cells that are no longer needed are removed by programmed cell death, or
apoptosis.

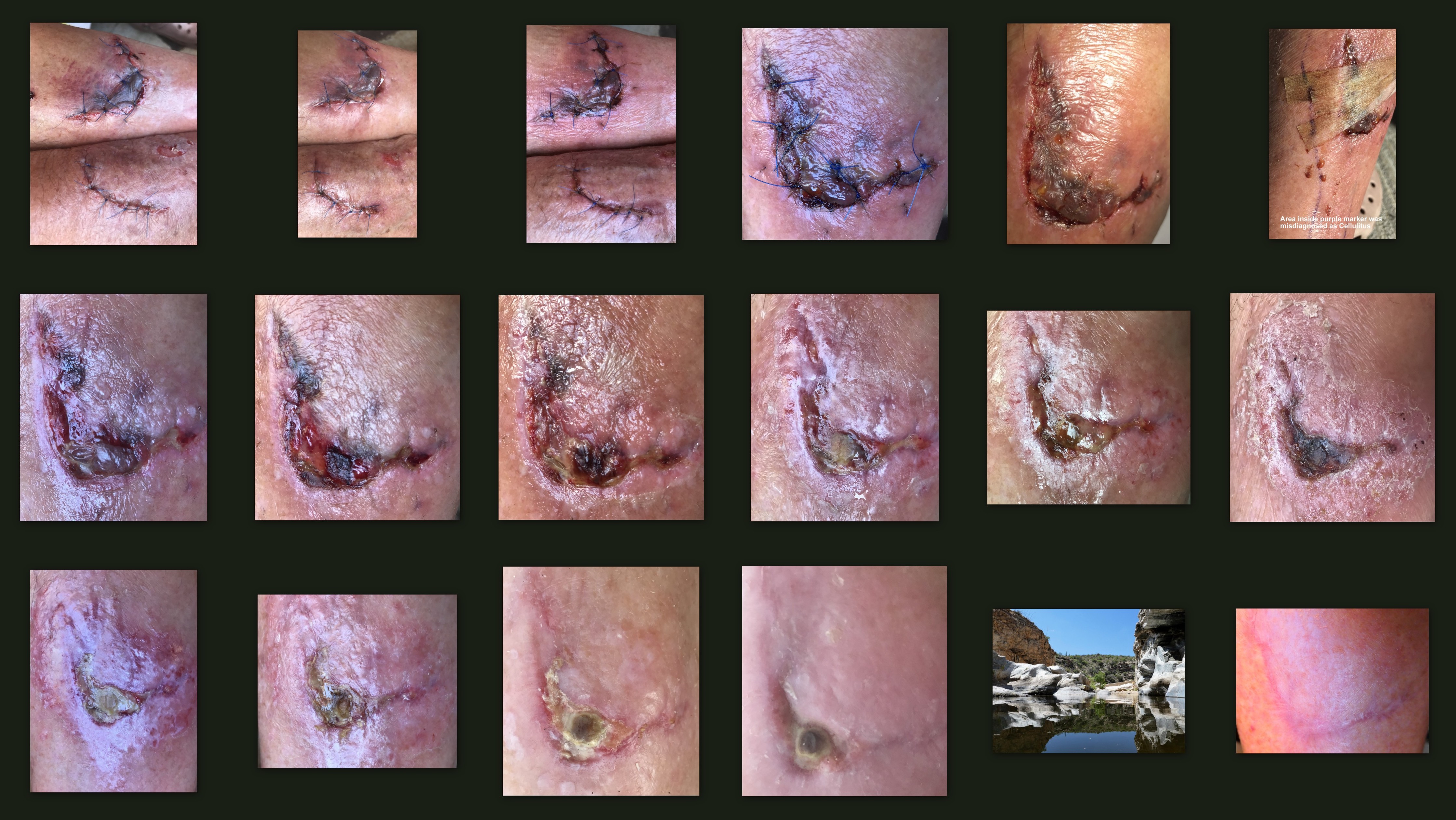
Timing and re-epithelialization
Timing is important to wound healing. Critically, the timing of wound re-epithelialization can decide the outcome of the healing.
If the epithelization of tissue over a denuded area is slow, a scar will form over many weeks, or months;
[ If the epithelization of a wounded area is fast, the healing will result in regeneration.]
Early vs cellular phase
Wound healing is classically divided into hemostasis
In biology, hemostasis or haemostasis is a process to prevent and stop bleeding, meaning to keep blood within a damaged blood vessel (the opposite of hemostasis is hemorrhage). It is the first stage of wound healing. This involves coagulation, wh ...
, inflammation, proliferation, and remodeling. Although a useful construct, this model employs considerable overlapping among individual phases. A complementary model has recently been describedregenerative medicine
Regenerative medicine deals with the "process of replacing, engineering or regenerating human or animal cells, tissues or organs to restore or establish normal function". This field holds the promise of engineering damaged tissues and organs by st ...
and tissue engineering
Tissue engineering is a biomedical engineering discipline that uses a combination of cells, engineering, materials methods, and suitable biochemical and physicochemical factors to restore, maintain, improve, or replace different types of biologi ...
(see Research and development section below). In this construct, the process of wound healing is divided into two major phases: the ''early phase'' and the ''cellular phase'':staging
Staging may refer to:
Computing
* Staging (cloud computing), a process used to assemble, test, and review a new solution before it is moved into production and the existing solution is decommissioned
* Staging (data), intermediately storing data b ...
for cellular attachment and subsequent cellular proliferation.
The cellular phase involves several types of cells working together to mount an inflammatory response, synthesize granulation tissue, and restore the epithelial layer.Epithelial
Epithelium or epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. It is a thin, continuous, protective layer of compactly packed cells with a little intercellu ...
-mesenchymal
Mesenchyme () is a type of loosely organized animal embryonic connective tissue of undifferentiated cells that give rise to most tissues, such as skin, blood or bone. The interactions between mesenchyme and epithelium help to form nearly every ...
interaction: re-epithelialization (phenotype
In genetics, the phenotype () is the set of observable characteristics or traits of an organism. The term covers the organism's morphology or physical form and structure, its developmental processes, its biochemical and physiological prop ...
change within hours, migration begins on day 1 or 2)
# Fibroblasts
A fibroblast is a type of biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework ( stroma) for animal tissues, and plays a critical role in wound healing. Fibroblasts are the most common cells ...
and myofibroblasts
A myofibroblast is a cell phenotype that was first described as being in a state between a fibroblast and a smooth muscle cell.
Structure
Myofibroblasts are contractile web-like fusiform cells that are identifiable by their expression of α-sm ...
: progressive alignment, collagen production, and matrix contraction (between day 4 and day 14)
# Endothelial cell
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the ves ...
s and angiogenesis (begins on day 4)
# Dermal matrix: elements of fabrication (begins on day 4, lasting 2 weeks) and alteration/remodeling (begins after week 2, lasting weeks to months—depending on wound size).
Inflammatory phase
Just before the inflammatory phase is initiated, the clotting cascade occurs in order to achieve hemostasis
In biology, hemostasis or haemostasis is a process to prevent and stop bleeding, meaning to keep blood within a damaged blood vessel (the opposite of hemostasis is hemorrhage). It is the first stage of wound healing. This involves coagulation, wh ...
, or the stopping of blood loss by way of a fibrin clot. Thereafter, various soluble factors (including chemokines and cytokines) are released to attract cells that phagocytise debris, bacteria, and damaged tissue, in addition to releasing signaling molecules that initiate the proliferative phase of wound healing.
Clotting cascade
When tissue is first wounded, blood comes in contact with collagen, triggering blood platelet
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby i ...
s to begin secreting inflammatory factors.[Rosenberg L., de la Torre J. (2006)]
Wound Healing, Growth Factors
. Emedicine.com. Accessed January 20, 2008. Platelets also express sticky glycoprotein
Glycoproteins are proteins which contain oligosaccharide chains covalently attached to amino acid side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as g ...
s on their cell membrane
The cell membrane (also known as the plasma membrane (PM) or cytoplasmic membrane, and historically referred to as the plasmalemma) is a biological membrane that separates and protects the interior of all cells from the outside environment (the ...
s that allow them to aggregate
Aggregate or aggregates may refer to:
Computing and mathematics
* collection of objects that are bound together by a root entity, otherwise known as an aggregate root. The aggregate root guarantees the consistency of changes being made within the ...
, forming a mass.Fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with pla ...
and fibronectin
Fibronectin is a high-molecular weight (~500-~600 kDa) glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. Fibronectin also binds to other extracellular matrix proteins such as collagen ...
cross-link together and form a plug that traps protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, respon ...
s and particles and prevents further blood loss.granulation tissue
Granulation tissue is new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. Granulation tissue typically grows from the base of a wound and is able to fill wounds of almost any size ...
and then later with collagen.
Platelets, the cells present in the highest numbers shortly after a wound occurs, release mediators into the blood, including cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in a ...
s and growth factor
A growth factor is a naturally occurring substance capable of stimulating cell proliferation, wound healing, and occasionally cellular differentiation. Usually it is a secreted protein or a steroid hormone. Growth factors are important for r ...
s.bradykinin
Bradykinin (BK) (Greek brady-, slow; -kinin, kīn(eîn) to move) is a peptide that promotes inflammation. It causes arterioles to dilate (enlarge) via the release of prostacyclin, nitric oxide, and endothelium-derived hyperpolarizing factor and m ...
, prostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are der ...
s, prostacyclin
Prostacyclin (also called prostaglandin I2 or PGI2) is a prostaglandin member of the eicosanoid family of lipid molecules. It inhibits platelet activation and is also an effective vasodilator.
When used as a drug, it is also known as epoprosten ...
s, thromboxane
Thromboxane is a member of the family of lipids known as eicosanoids. The two major thromboxanes are thromboxane A2 and thromboxane B2. The distinguishing feature of thromboxanes is a 6-membered ether-containing ring.
Thromboxane is named for ...
, and histamine
Histamine is an organic nitrogenous compound involved in local immune responses, as well as regulating physiological functions in the gut and acting as a neurotransmitter for the brain, spinal cord, and uterus. Since histamine was discovered in ...
,blood vessel
Blood vessels are the structures of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from ...
s to become dilated and porous
Porosity or void fraction is a measure of the void (i.e. "empty") spaces in a material, and is a fraction of the volume of voids over the total volume, between 0 and 1, or as a percentage between 0% and 100%. Strictly speaking, some tests measure ...
. In many ways, extravasated platelets in trauma perform a similar function to tissue macrophages and mast cell
A mast cell (also known as a mastocyte or a labrocyte) is a resident cell of connective tissue that contains many granules rich in histamine and heparin. Specifically, it is a type of granulocyte derived from the myeloid stem cell that is a pa ...
s exposed to microbial molecular signatures in infection: they become activated, and secrete molecular mediators – vasoactive amines, eicosanoid
Eicosanoids are signaling molecules made by the enzymatic or non-enzymatic oxidation of arachidonic acid or other polyunsaturated fatty acids (PUFAs) that are, similar to arachidonic acid, around 20 carbon units in length. Eicosanoids are a su ...
s, and cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in a ...
s – that initiate the inflammatory process.
Vasoconstriction and vasodilation
Immediately after a blood vessel
Blood vessels are the structures of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from ...
is breached, ruptured cell membrane
The cell membrane (also known as the plasma membrane (PM) or cytoplasmic membrane, and historically referred to as the plasmalemma) is a biological membrane that separates and protects the interior of all cells from the outside environment (the ...
s release inflammatory factors like thromboxane
Thromboxane is a member of the family of lipids known as eicosanoids. The two major thromboxanes are thromboxane A2 and thromboxane B2. The distinguishing feature of thromboxanes is a 6-membered ether-containing ring.
Thromboxane is named for ...
s and prostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are der ...
s that cause the vessel to spasm to prevent blood loss and to collect inflammatory cells and factors in the area.vasoconstriction
Vasoconstriction is the narrowing of the blood vessels resulting from contraction of the muscular wall of the vessels, in particular the large arteries and small arterioles. The process is the opposite of vasodilation, the widening of blood ve ...
lasts five to ten minutes and is followed by vasodilation
Vasodilation is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. The process is the opposite of vasoconstricti ...
, a widening of blood vessels, which peaks at about 20 minutes post-wounding.histamine
Histamine is an organic nitrogenous compound involved in local immune responses, as well as regulating physiological functions in the gut and acting as a neurotransmitter for the brain, spinal cord, and uterus. Since histamine was discovered in ...
.edema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area ma ...
tous because proteins from the bloodstream leak into the extravascular space, which increases its osmolar load and draws water into the area.porosity
Porosity or void fraction is a measure of the void (i.e. "empty") spaces in a material, and is a fraction of the volume of voids over the total volume, between 0 and 1, or as a percentage between 0% and 100%. Strictly speaking, some tests measure ...
of blood vessels also facilitates the entry of inflammatory cells like leukocyte
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mul ...
s into the wound site from the bloodstream
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, tha ...
.[Dealey C. (1999). ''The care of wounds: A guide for nurses''. Oxford; Malden, Mass. Blackwell Science. Electronic book.]
Polymorphonuclear neutrophils
Within an hour of wounding, polymorphonuclear neutrophil
Neutrophils (also known as neutrocytes or heterophils) are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying in ...
s (PMNs) arrive at the wound site and become the predominant cells in the wound for the first two days after the injury occurs, with especially high numbers on the second day.[de la Torre J., Sholar A. (2006)]
Wound healing: Chronic wounds
. Emedicine.com. Accessed January 20, 2008. They are attracted to the site by fibronectin, growth factors, and substances such as kinin A kinin is any of various structurally related polypeptides, such as bradykinin and kallidin. They are members of the autacoid family. Kinins are peptides that are cleaved from kininogens by the process of kallikreins. Kallikreins activate kinins ...
s. Neutrophils phagocytise debris and kill bacteria by releasing free radical
A daughter category of ''Ageing'', this category deals only with the biological aspects of ageing.
Ageing
Ailments of unknown cause
Biogerontology
Biological processes
Causes of death
Cellular processes
Gerontology
Life extension
Metabo ...
s in what is called a respiratory burst
Respiratory burst (or oxidative burst) is the rapid release of the reactive oxygen species (ROS), Superoxide, superoxide anion () and hydrogen peroxide (), from different Cell (biology), cell types.
This is usually utilised for mammalian immune sy ...
.protease
A protease (also called a peptidase, proteinase, or proteolytic enzyme) is an enzyme that catalyzes (increases reaction rate or "speeds up") proteolysis, breaking down proteins into smaller polypeptides or single amino acids, and spurring the form ...
s that break down damaged tissue. Functional neutrophils at the wound site only have life-spans of around two days, so they usually undergo apoptosis once they have completed their tasks and are engulfed and degraded by macrophages.helper T cell
The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of T cell that play an important role in the adaptive immune system. They aid the activity of other immune cells by releasing cytokines. They are consider ...
s, which secrete cytokines to cause more T cells to divide and to increase inflammation and enhance vasodilation and vessel permeability.
Macrophages
One of the roles of macrophages
Macrophages (abbreviated as M φ, MΦ or MP) ( el, large eaters, from Greek ''μακρός'' (') = large, ''φαγεῖν'' (') = to eat) are a type of white blood cell of the immune system that engulfs and digests pathogens, such as cancer ce ...
is to phagocytize other expended phagocyte
Phagocytes are cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or dying cells. Their name comes from the Greek ', "to eat" or "devour", and "-cyte", the suffix in biology denoting "cell", from the Greek ...
s,oxygen
Oxygen is the chemical element with the symbol O and atomic number 8. It is a member of the chalcogen group in the periodic table, a highly reactive nonmetal, and an oxidizing agent that readily forms oxides with most elements as we ...
content of their surroundings to produce factors that induce and speed angiogenesisextracellular matrix
In biology, the extracellular matrix (ECM), also called intercellular matrix, is a three-dimensional network consisting of extracellular macromolecules and minerals, such as collagen, enzymes, glycoproteins and hydroxyapatite that provide struc ...
.spleen
The spleen is an organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter. The word spleen comes . contains half the body's monocytes in reserve ready to be deployed to injured tissue.monocyte
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and conventional dendritic cells. As a part of the vertebrate innate immune system monocytes also i ...
s from the bloodstream enter the area through blood vessel walls.salamander
Salamanders are a group of amphibians typically characterized by their lizard-like appearance, with slender bodies, blunt snouts, short limbs projecting at right angles to the body, and the presence of a tail in both larvae and adults. All ten ...
resulted in failure of a typical regeneration response (limb regeneration), instead bringing on a repair (scarring) response.
Decline of inflammatory phase
As inflammation dies down, fewer inflammatory factors are secreted, existing ones are broken down, and numbers of neutrophils and macrophages are reduced at the wound site.biofilm
A biofilm comprises any syntrophic consortium of microorganisms in which cells stick to each other and often also to a surface. These adherent cells become embedded within a slimy extracellular matrix that is composed of extracellular ...
is present in the wound, these factors may cause a prolonged inflammatory phase and prevent the wound from properly commencing the proliferation phase of healing. This can lead to a chronic wound A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic.
Chronic wounds seem to be detained in on ...
.
Proliferative phase
About two or three days after the wound occurs, fibroblasts
A fibroblast is a type of biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework ( stroma) for animal tissues, and plays a critical role in wound healing. Fibroblasts are the most common cells ...
begin to enter the wound site, marking the onset of the proliferative phase even before the inflammatory phase has ended.[Falanga V. (2005). Wound Healing. American Academy of Dermatology (AAD).] As in the other phases of wound healing, steps in the proliferative phase do not occur in a series but rather partially overlap in time.
Angiogenesis
Also called neovascularization, the process of angiogenesis occurs concurrently with fibroblast proliferation when endothelial cells migrate to the area of the wound.[Kuwahara R.T. and Rasberry R. 2007.]
Chemical Peels
. Emedicine.com. Accessed September 15, 2007. Because the activity of fibroblasts and epithelial cells requires oxygen and nutrients, angiogenesis is imperative for other stages in wound healing, like epidermal and fibroblast migration. The tissue in which angiogenesis has occurred typically looks red (is erythema
Erythema (from the Greek , meaning red) is redness of the skin or mucous membranes, caused by hyperemia (increased blood flow) in superficial capillaries. It occurs with any skin injury, infection, or inflammation. Examples of erythema not asso ...
tous) due to the presence of capillaries
A capillary is a small blood vessel from 5 to 10 micrometres (μm) in diameter. Capillaries are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the smallest blood vessels in the body: ...
.Stem cell
In multicellular organisms, stem cells are undifferentiated or partially differentiated cells that can differentiate into various types of cells and proliferate indefinitely to produce more of the same stem cell. They are the earliest type of ...
s of endothelial cell
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the ves ...
s, originating from parts of uninjured blood vessels, develop pseudopod
A pseudopod or pseudopodium (plural: pseudopods or pseudopodia) is a temporary arm-like projection of a eukaryotic cell membrane that is emerged in the direction of movement. Filled with cytoplasm, pseudopodia primarily consist of actin filament ...
ia and push through the ECM
ECM may refer to:
Economics and commerce
* Engineering change management
* Equity capital markets
* Error correction model, an econometric model
* European Common Market
Mathematics
* Elliptic curve method
* European Congress of Mathematics
...
into the wound site to establish new blood vessels.Endothelial cell
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the ves ...
s are attracted to the wound area by fibronectin found on the fibrin scab and chemotactically by angiogenic factors released by other cells,[Romo T. and Pearson J.M. 2005.]
Wound Healing, Skin
. Emedicine.com. Accessed December 27, 2006. e.g. from macrophages and platelets when in a low-oxygen environment. Endothelial growth and proliferation is also directly stimulated by hypoxia, and presence of lactic acid
Lactic acid is an organic acid. It has a molecular formula . It is white in the solid state and it is miscible with water. When in the dissolved state, it forms a colorless solution. Production includes both artificial synthesis as well as natur ...
in the wound.transcription factor
In molecular biology, a transcription factor (TF) (or sequence-specific DNA-binding factor) is a protein that controls the rate of transcription of genetic information from DNA to messenger RNA, by binding to a specific DNA sequence. The fu ...
, hypoxia-inducible factor
Hypoxia-inducible factors (HIFs) are transcription factors that respond to decreases in available oxygen in the cellular environment, or hypoxia. They are only present in parahoxozoan animals.
Discovery
The HIF transcriptional complex w ...
(HIF) to transactivate In the context of gene regulation: transactivation is the increased rate of gene expression triggered either by biological processes or by artificial means, through the expression of an intermediate transactivator protein.
In the context of recep ...
a set of proliferative genes including vascular endothelial growth factor
Vascular endothelial growth factor (VEGF, ), originally known as vascular permeability factor (VPF), is a signal protein produced by many cells that stimulates the formation of blood vessels. To be specific, VEGF is a sub-family of growth factors, ...
(VEGF) and glucose transporter 1 (GLUT1).
To migrate, endothelial cells need collagenase
Collagenases are enzymes that break the peptide bonds in collagen. They assist in destroying extracellular structures in the pathogenesis of bacteria such as ''Clostridium''. They are considered a virulence factor, facilitating the spread of ...
s and plasminogen activator Plasminogen activators are serine proteases that catalyze the activation of plasmin via proteolytic cleavage of its zymogen form plasminogen. Plasmin is an important factor in fibrinolysis, the breakdown of fibrin polymers formed during blood clotti ...
to degrade the clot and part of the ECM.Zinc
Zinc is a chemical element with the symbol Zn and atomic number 30. Zinc is a slightly brittle metal at room temperature and has a shiny-greyish appearance when oxidation is removed. It is the first element in group 12 (IIB) of the periodic t ...
-dependent metalloproteinase
A metalloproteinase, or metalloprotease, is any protease enzyme whose catalytic mechanism involves a metal. An example is ADAM12 which plays a significant role in the fusion of muscle cells during embryo development, in a process known as myoge ...
s digest basement membrane
The basement membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between epithelial tissues including mesothelium and ...
and ECM to allow cell migration, proliferation and angiogenesis.
Fibroplasia and granulation tissue formation
Simultaneously with angiogenesis, fibroblast
A fibroblast is a type of biological cell that synthesizes the extracellular matrix and collagen, produces the structural framework ( stroma) for animal tissues, and plays a critical role in wound healing. Fibroblasts are the most common cells of ...
s begin accumulating in the wound site. Fibroblasts begin entering the wound site two to five days after wounding as the inflammatory phase is ending, and their numbers peak at one to two weeks post-wounding.ground substance Ground substance is an amorphous gel-like substance in the extracellular space that contains all components of the extracellular matrix (ECM) except for fibrous materials such as collagen and elastin. Ground substance is active in the development, ...
into the wound bed, and later collagen, which they can adhere to for migration.Granulation tissue
Granulation tissue is new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. Granulation tissue typically grows from the base of a wound and is able to fill wounds of almost any size ...
functions as rudimentary tissue, and begins to appear in the wound already during the inflammatory phase, two to five days post wounding, and continues growing until the wound bed is covered. Granulation tissue consists of new blood vessels, fibroblasts, inflammatory cells, endothelial cells, myofibroblasts, and the components of a new, provisional extracellular matrix
In biology, the extracellular matrix (ECM), also called intercellular matrix, is a three-dimensional network consisting of extracellular macromolecules and minerals, such as collagen, enzymes, glycoproteins and hydroxyapatite that provide struc ...
(ECM). The provisional ECM is different in composition from the ECM in normal tissue and its components originate from fibroblasts.glycosaminoglycan
Glycosaminoglycans (GAGs) or mucopolysaccharides are long, linear polysaccharides consisting of repeating disaccharide units (i.e. two-sugar units). The repeating two-sugar unit consists of a uronic sugar and an amino sugar, except in the case o ...
s, elastin, glycoprotein
Glycoproteins are proteins which contain oligosaccharide chains covalently attached to amino acid side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as g ...
s and proteoglycan
Proteoglycans are proteins that are heavily glycosylated. The basic proteoglycan unit consists of a "core protein" with one or more covalently attached glycosaminoglycan (GAG) chain(s). The point of attachment is a serine (Ser) residue to w ...
s.hyaluronan
Hyaluronic acid (; abbreviated HA; conjugate base hyaluronate), also called hyaluronan, is an anionic, nonsulfated glycosaminoglycan distributed widely throughout connective, epithelial, and neural tissues. It is unique among glycosaminogl ...
, which create a very hydrated matrix and facilitate cell migration.PDGF
Platelet-derived growth factor (PDGF) is one among numerous growth factors that regulate cell growth and division. In particular, PDGF plays a significant role in blood vessel formation, the growth of blood vessels from already-existing blood v ...
, TGF-β
Transforming growth factor beta (TGF-β) is a multifunctional cytokine belonging to the transforming growth factor superfamily that includes three different mammalian isoforms (TGF-β 1 to 3, HGNC symbols TGFB1, TGFB2, TGFB3) and many other ...
) and fibronectin encourage proliferation, migration to the wound bed, and production of ECM molecules by fibroblasts. Fibroblasts also secrete growth factors that attract epithelial cells to the wound site. Hypoxia also contributes to fibroblast proliferation and excretion of growth factors, though too little oxygen will inhibit their growth and deposition of ECM components, and can lead to excessive, fibrotic scar
A scar (or scar tissue) is an area of fibrous tissue that replaces normal skin after an injury. Scars result from the biological process of wound repair in the skin, as well as in other organs, and tissues of the body. Thus, scarring is a n ...
ring.
Collagen deposition
One of fibroblasts' most important duties is the production of collagen.traumatic injury
An injury is any physiological damage to living tissue caused by immediate physical stress. An injury can occur intentionally or unintentionally and may be caused by blunt trauma, penetrating trauma, burning, toxic exposure, asphyxiation, or ...
.Type III collagen
Type III Collagen is a homotrimer, or a protein composed of three identical peptide chains ( monomers), each called an alpha 1 chain of type III collagen. Formally, the monomers are called collagen type III, alpha-1 chain and in humans are encode ...
and fibronectin
Fibronectin is a high-molecular weight (~500-~600 kDa) glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. Fibronectin also binds to other extracellular matrix proteins such as collagen ...
generally begin to be produced in appreciable amounts at somewhere between approximately 10 hours[Fig. 9-1. The cellular, biochemical, and mechanical phases of wound healing. ] and 3 days,type I collagen
Type I collagen is the most abundant collagen of the human body. It forms large, eosinophilic fibers known as collagen fibers.
It is present in scar tissue, the end product when tissue heals by repair, as well as tendons, ligaments, the endom ...
.
Even as fibroblasts are producing new collagen, collagenases and other factors degrade it. Shortly after wounding, synthesis exceeds degradation so collagen levels in the wound rise, but later production and degradation become equal so there is no net collagen gain.
Epithelialization
The formation of granulation tissue into an open wound allows the reepithelialization phase to take place, as epithelial cells migrate across the new tissue to form a barrier between the wound and the environment.Basal
Basal or basilar is a term meaning ''base'', ''bottom'', or ''minimum''.
Science
* Basal (anatomy), an anatomical term of location for features associated with the base of an organism or structure
* Basal (medicine), a minimal level that is nec ...
keratinocyte
Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells.
Basal cells in the basal layer (''stratum basale'') of the skin are sometimes referred ...
s from the wound edges and dermal appendages such as hair follicle
The hair follicle is an organ found in mammalian skin. It resides in the dermal layer of the skin and is made up of 20 different cell types, each with distinct functions. The hair follicle regulates hair growth via a complex interaction betwe ...
s, sweat glands
Sweat glands, also known as sudoriferous or sudoriparous glands, , are small tubular structures of the skin that produce sweat. Sweat glands are a type of exocrine gland, which are glands that produce and secrete substances onto an epithelial sur ...
and sebacious (oil) glands are the main cells responsible for the epithelialization phase of wound healing.[ and nerves do not form. With the lack of hair follicles, nerves and sweat glands, the wound, and the resulting healing scar, provide a challenge to the body with regards to temperature control.]Keratinocyte
Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells.
Basal cells in the basal layer (''stratum basale'') of the skin are sometimes referred ...
s migrate without first proliferating.[Mulvaney M. and Harrington A. 1994.]
Chapter 7: Cutaneous trauma and its treatment
In, ''Textbook of Military Medicine: Military Dermatology''. Office of the Surgeon General, Department of the Army. Virtual Naval Hospital Project. Accessed through web archive on September 15, 2007. Thus the time of onset of migration is variable and may occur about one day after wounding.[Larjava H., Koivisto L., and Hakkinen L. 2002. Chapter 3: Keratinocyte Interactions with Fibronectin During Wound Healing. In, Heino, J. and Kahari, V.M. ''Cell Invasion''. Medical Intelligence Unit; 33. Georgetown, Tex., Austin, Tex Landes Bioscience, Inc. Electronic book.] Cells on the wound margins proliferate on the second and third day post-wounding in order to provide more cells for migration.basement membrane
The basement membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between epithelial tissues including mesothelium and ...
is not breached, epithelial cells are replaced within three days by division and upward migration of cells in the stratum basale
The ''stratum basale'' (basal layer, sometimes referred to as ''stratum germinativum'') is the deepest layer of the five layers of the epidermis, the external covering of skin in mammals.
The ''stratum basale'' is a single layer of columnar or ...
in the same fashion that occurs in uninjured skin.contact inhibition In cell biology, contact inhibition refers to two different but closely related phenomena: contact inhibition of locomotion (CIL) and contact inhibition of proliferation (CIP). CIL refers to the avoidance behavior exhibited by fibroblast-like cells ...
and by chemicals such as nitric oxide
Nitric oxide (nitrogen oxide or nitrogen monoxide) is a colorless gas with the formula . It is one of the principal oxides of nitrogen. Nitric oxide is a free radical: it has an unpaired electron, which is sometimes denoted by a dot in its ...
.desmosomes
A desmosome (; "binding body"), also known as a macula adherens (plural: maculae adherentes) (Latin for ''adhering spot''), is a cell structure specialized for cell-to-cell adhesion. A type of junctional complex, they are localized spot-like adh ...
and hemidesmosomes
Hemidesmosomes are very small stud-like structures found in keratinocytes of the epidermis of skin that attach to the extracellular matrix. They are similar in form to desmosomes when visualized by electron microscopy, however, desmosomes attach to ...
, which normally anchor the cells by intermediate filaments
Intermediate filaments (IFs) are cytoskeletal structural components found in the cells of vertebrates, and many invertebrates. Homologues of the IF protein have been noted in an invertebrate, the cephalochordate ''Branchiostoma''.
Intermed ...
in their cytoskeleton
The cytoskeleton is a complex, dynamic network of interlinking protein filaments present in the cytoplasm of all cells, including those of bacteria and archaea. In eukaryotes, it extends from the cell nucleus to the cell membrane and is comp ...
to other cells and to the ECM.Transmembrane
A transmembrane protein (TP) is a type of integral membrane protein that spans the entirety of the cell membrane. Many transmembrane proteins function as gateways to permit the transport of specific substances across the membrane. They frequentl ...
receptor protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, respon ...
s called integrin
Integrins are transmembrane receptors that facilitate cell-cell and cell-extracellular matrix (ECM) adhesion. Upon ligand binding, integrins activate signal transduction pathways that mediate cellular signals such as regulation of the cell cycle, ...
s, which are made of glycoprotein
Glycoproteins are proteins which contain oligosaccharide chains covalently attached to amino acid side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as g ...
s and normally anchor the cell to the basement membrane by its cytoskeleton
The cytoskeleton is a complex, dynamic network of interlinking protein filaments present in the cytoplasm of all cells, including those of bacteria and archaea. In eukaryotes, it extends from the cell nucleus to the cell membrane and is comp ...
, are released from the cell's intermediate filaments and relocate to actin
Actin is a protein family, family of Globular protein, globular multi-functional proteins that form microfilaments in the cytoskeleton, and the thin filaments in myofibril, muscle fibrils. It is found in essentially all Eukaryote, eukaryotic cel ...
filaments to serve as attachments to the ECM for pseudopod
A pseudopod or pseudopodium (plural: pseudopods or pseudopodia) is a temporary arm-like projection of a eukaryotic cell membrane that is emerged in the direction of movement. Filled with cytoplasm, pseudopodia primarily consist of actin filament ...
ia during migration.lamellipodia
The lamellipodium (plural lamellipodia) (from Latin ''lamella'', related to ', "thin sheet", and the Greek radical ''pod-'', "foot") is a cytoskeletal protein actin projection on the leading edge of the cell. It contains a quasi-two-dimension ...
and wide processes that look like ruffles.Actin
Actin is a protein family, family of Globular protein, globular multi-functional proteins that form microfilaments in the cytoskeleton, and the thin filaments in myofibril, muscle fibrils. It is found in essentially all Eukaryote, eukaryotic cel ...
filaments and pseudopod
A pseudopod or pseudopodium (plural: pseudopods or pseudopodia) is a temporary arm-like projection of a eukaryotic cell membrane that is emerged in the direction of movement. Filled with cytoplasm, pseudopodia primarily consist of actin filament ...
ia form.integrin
Integrins are transmembrane receptors that facilitate cell-cell and cell-extracellular matrix (ECM) adhesion. Upon ligand binding, integrins activate signal transduction pathways that mediate cellular signals such as regulation of the cell cycle, ...
s on the pseudopod attach to the ECM, and the actin filaments in the projection pull the cell along.filopodia
Filopodia (singular filopodium) are slender cytoplasmic projections that extend beyond the leading edge of lamellipodia in migrating cells. Within the lamellipodium, actin ribs are known as ''microspikes'', and when they extend beyond the lam ...
.basement membrane
The basement membrane is a thin, pliable sheet-like type of extracellular matrix that provides cell and tissue support and acts as a platform for complex signalling. The basement membrane sits between epithelial tissues including mesothelium and ...
form the stratum basale
The ''stratum basale'' (basal layer, sometimes referred to as ''stratum germinativum'') is the deepest layer of the five layers of the epidermis, the external covering of skin in mammals.
The ''stratum basale'' is a single layer of columnar or ...
. These basal cells continue to migrate across the wound bed, and epithelial cells above them slide along as well.Fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with pla ...
, collagen, and fibronectin in the ECM may further signal cells to divide and migrate. Like fibroblasts, migrating keratinocytes use the fibronectin cross-linked with fibrin that was deposited in inflammation as an attachment site to crawl across. As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue.
As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue.plasminogen activator Plasminogen activators are serine proteases that catalyze the activation of plasmin via proteolytic cleavage of its zymogen form plasminogen. Plasmin is an important factor in fibrinolysis, the breakdown of fibrin polymers formed during blood clotti ...
, which activates plasminogen
Plasmin is an important enzyme () present in blood that degrades many blood plasma proteins, including fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein (in the zymogen form of plasminogen) is encod ...
, turning it into plasmin
Plasmin is an important enzyme () present in blood that degrades many blood plasma proteins, including fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein (in the zymogen form of plasminogen) is encode ...
to dissolve the scab. Cells can only migrate over living tissue,matrix metalloproteinases
Matrix metalloproteinases (MMPs), also known as matrix metallopeptidases or matrixins, are metalloproteinases that are calcium-dependent zinc-containing endopeptidases; other family members are adamalysins, serralysins, and astacins. The MMPs b ...
(MMPs) to dissolve damaged parts of the ECM in their way, particularly at the front of the migrating sheet.contact inhibition In cell biology, contact inhibition refers to two different but closely related phenomena: contact inhibition of locomotion (CIL) and contact inhibition of proliferation (CIP). CIL refers to the avoidance behavior exhibited by fibroblast-like cells ...
causes them to stop migrating.desmosome
A desmosome (; "binding body"), also known as a macula adherens (plural: maculae adherentes) (Latin for ''adhering spot''), is a cell structure specialized for cell-to-cell adhesion. A type of junctional complex, they are localized spot-like adh ...
s and hemidesmosome
Hemidesmosomes are very small stud-like structures found in keratinocytes of the epidermis of skin that attach to the extracellular matrix. They are similar in form to desmosomes when visualized by electron microscopy, however, desmosomes attach to ...
s and become anchored once again to the basement membrane.Basal cells
The ''stratum basale'' (basal layer, sometimes referred to as ''stratum germinativum'') is the deepest layer of the five layers of the epidermis, the external covering of skin in mammals.
The ''stratum basale'' is a single layer of columnar or ...
begin to divide and differentiate in the same manner as they do in normal skin to reestablish the strata found in reepithelialized skin.
Contraction
Contraction is a key phase of wound healing with repair. If contraction continues for too long, it can lead to disfigurement and loss of function.myofibroblast
A myofibroblast is a cell phenotype that was first described as being in a state between a fibroblast and a smooth muscle cell.
Structure
Myofibroblasts are contractile web-like fusiform cells that are identifiable by their expression of α-sm ...
s.full thickness
Full may refer to:
* People with the surname Full, including:
** Mr. Full (given name unknown), acting Governor of German Cameroon, 1913 to 1914
* A property in the mathematical field of topology; see Full set
* A property of functors in the mathe ...
wounds, contraction peaks at 5 to 15 days post wounding.smooth muscle
Smooth muscle is an involuntary non- striated muscle, so-called because it has no sarcomeres and therefore no striations (''bands'' or ''stripes''). It is divided into two subgroups, single-unit and multiunit smooth muscle. Within single-unit ...
cells.desmosomes
A desmosome (; "binding body"), also known as a macula adherens (plural: maculae adherentes) (Latin for ''adhering spot''), is a cell structure specialized for cell-to-cell adhesion. A type of junctional complex, they are localized spot-like adh ...
. Also, at an adhesion called the fibronexus, actin in the myofibroblast is linked across the cell membrane to molecules in the extracellular matrix like fibronectin and collagen.
Maturation and remodeling
When the levels of collagen production and degradation equalize, the maturation phase of tissue repair is said to have begun.type III collagen
Type III Collagen is a homotrimer, or a protein composed of three identical peptide chains ( monomers), each called an alpha 1 chain of type III collagen. Formally, the monomers are called collagen type III, alpha-1 chain and in humans are encode ...
, which is prevalent during proliferation, is replaced by type I collagen.tension lines
Langer's lines, Langer lines of skin tension, or sometimes called cleavage lines, are Topological map, topological lines drawn on a map of the human body. They are parallel to the natural orientation of collagen fibers in the dermis, and generally ...
.[ to three weeks. The maturation phase can last for a year or longer, similarly depending on wound type.]tensile strength
Ultimate tensile strength (UTS), often shortened to tensile strength (TS), ultimate strength, or F_\text within equations, is the maximum stress that a material can withstand while being stretched or pulled before breaking. In brittle materials ...
of the wound increases.blood vessel
Blood vessels are the structures of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from ...
s that are no longer needed are removed by apoptosis.chronic wound A chronic wound is a wound that does not heal in an orderly set of stages and in a predictable amount of time the way most wounds do; wounds that do not heal within three months are often considered chronic.
Chronic wounds seem to be detained in on ...
Factors affecting wound healing
Many factors controlling the efficacy, speed, and manner of wound healing fall under two types: local and systemic factors.
Local factors
* Moisture; keeping a wound moist rather than dry makes wound healing more rapid and with less pain and less scarring
* Mechanical factors
* Oedema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area ma ...
* Ionizing radiation
* Faulty technique of wound closure
* Ischemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems ...
and necrosis
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated dig ...
* Foreign bodies. Sharp, small foreign bodies can penetrate the skin leaving little surface wound but causing internal injury and internal bleeding. For a glass foreign body, "frequently, an innocent skin wound disguises the extensive nature of the injuries beneath". First-degree nerve injury requires a few hours to a few weeks to recover. If a foreign body passes by a nerve and causes first-degree nerve injury during entry, then the sensation of the foreign body or pain due to internal wounding may be delayed by a few hours to a few weeks after entry. A sudden increase in pain during the first few weeks of wound healing could be a sign of a recovered nerve reporting internal injuries rather than a newly developed infection.
* Low oxygen tension
* Perfusion
Systemic factors
* Inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
* Diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
– Individuals with diabetes demonstrate reduced capability in the healing of acute wounds. Additionally, diabetic individuals are susceptible to developing chronic diabetic foot ulcers, a serious complication of diabetes which affects 15% of people with diabetes and accounts for 84% of all diabetes-related lower leg amputations. The impaired healing abilities of diabetics with diabetic foot ulcers and/or acute wounds involves multiple pathophysiological mechanisms.Nutrient
A nutrient is a substance used by an organism to survive, grow, and reproduce. The requirement for dietary nutrient intake applies to animals, plants, fungi, and protists. Nutrients can be incorporated into cells for metabolic purposes or excr ...
s – Malnutrition or nutritional deficiencies have a recognizable impact on wound healing post trauma or surgical intervention. Nutrients including proteins, carbohydrates, arginine, glutamine, polyunsaturated fatty acids, vitamin A, vitamin C, vitamin E, magnesium, copper, zinc and iron all play significant roles in wound healing.Metabolic disease
A metabolic disorder is a disorder that negatively alters the body's processing and distribution of macronutrients, such as proteins, fats, and carbohydrates. Metabolic disorders can happen when abnormal chemical reactions in the body alter the ...
s
* Immunosuppression
Immunosuppression is a reduction of the activation or efficacy of the immune system. Some portions of the immune system itself have immunosuppressive effects on other parts of the immune system, and immunosuppression may occur as an adverse react ...
* Connective tissue
Connective tissue is one of the four primary types of animal tissue, along with epithelial tissue, muscle tissue, and nervous tissue. It develops from the mesenchyme derived from the mesoderm the middle embryonic germ layer. Connective tissue ...
disorders
* Smoking – Smoking causes a delay in the speed of wound repair notably in the proliferative and inflammatory phases. It also increases the likelihood of certain complications such as wound rupture, wound and flap necrosis, decrease in wound tensile strength and infection.Passive smoking
Passive smoking is the inhalation of tobacco smoke, called secondhand smoke (SHS), or environmental tobacco smoke (ETS), by persons other than the intended "active" smoker. It occurs when tobacco smoke enters an environment, causing its inhala ...
also impairs a proper wound healing process.
* Age – Increased age (over 60 years) is a risk factor for impaired wound healing.unit of alcohol
Units of alcohol are used in the United Kingdom (UK) as a measure to quantify the actual alcoholic content within a given volume of an alcoholic beverage, in order to provide guidance on total alcohol consumption.
A number of other countries (in ...
causes a negative effect on re-epithelialization, wound closure, collagen production and angiogenesis.system of differential equations
In mathematics, a system of differential equations is a finite set of differential equations. Such a system can be either linear or non-linear. Also, such a system can be either a system of ordinary differential equations or a system of partial ...
solved through MATLAB
MATLAB (an abbreviation of "MATrix LABoratory") is a proprietary multi-paradigm programming language and numeric computing environment developed by MathWorks. MATLAB allows matrix manipulations, plotting of functions and data, implementa ...
. The models show that the "rate of the healing process" appears to be "highly influenced by the activity and size of the injury itself as well as the activity of the healing agent."
Research and development
Up until about 2000, the classic paradigm of wound healing, involving stem cells
In multicellular organisms, stem cells are undifferentiated or partially differentiated cells that can differentiate into various types of cells and proliferate indefinitely to produce more of the same stem cell. They are the earliest type of ...
restricted to organ-specific lineages, had never been seriously challenged. Since then, the notion of adult stem cells
Adult stem cells are undifferentiated cells, found throughout the body after development, that multiply by cell division to replenish dying cells and regenerate damaged tissues. Also known as somatic stem cells (from Greek σωματικóς ...
having cellular ''plasticity'' or the ability to differentiate into non-lineage cells has emerged as an alternative explanation.hematopoietic
Haematopoiesis (, from Greek , 'blood' and 'to make'; also hematopoiesis in American English; sometimes also h(a)emopoiesis) is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells ...
progenitor cells
In genealogy, the progenitor (rarer: primogenitor; german: Stammvater or ''Ahnherr'') is the – sometimes legendary – founder of a family, line of descent, clan or tribe, noble house, or ethnic group..
Ebenda''Ahnherr:''"Stammvater eine ...
(that give rise to mature cells in the blood) may have the ability ''de-differentiate'' back into hematopoietic stem cells and/or ''transdifferentiate'' into non-lineage cells, such as fibroblasts.
Stem cells and cellular plasticity
Multipotent adult stem cells have the capacity to be self-renewing and give rise to different cell types. Stem cells give rise to progenitor cells, which are cells that are not self-renewing, but can generate several types of cells. The extent of stem cell involvement in cutaneous (skin) wound healing is complex and not fully understood. Stem cell injection leads to wound healing primarily through stimulation of angiogenesis.
It is thought that the epidermis and dermis are reconstituted by mitotically active stem cells that reside at the apex of rete ridges
Rete pegs (also known as rete processes or rete ridges) are the epithelial extensions that project into the underlying connective tissue in both skin and mucous membranes.
In the epithelium of the mouth, the attached gingiva exhibit rete pegs, wh ...
(basal stem cells or BSC), the bulge of hair follicle
The hair follicle is an organ found in mammalian skin. It resides in the dermal layer of the skin and is made up of 20 different cell types, each with distinct functions. The hair follicle regulates hair growth via a complex interaction betwe ...
s (hair follicular stem cell or HFSC), and the papillary dermis (dermal stem cells).mesenchymal stem cells
Mesenchymal stem cells (MSCs) also known as mesenchymal stromal cells or medicinal signaling cells are multipotent stromal cells that can differentiate into a variety of cell types, including osteoblasts (bone cells), chondrocytes (cartilage cel ...
(MSC) and (2) hematopoietic stem cells
Hematopoietic stem cells (HSCs) are the stem cells that give rise to other blood cells. This process is called haematopoiesis. In vertebrates, the very first definitive HSCs arise from the ventral endothelial wall of the embryonic aorta within t ...
(HSC). Bone marrow also harbors a progenitor subpopulation (endothelial
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vesse ...
progenitor cells or EPC) that, in the same type of setting, are mobilized to aid in the reconstruction of blood vessels.leukocytes
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mul ...
(circulating fibrocyte
A fibrocyte is an inactive mesenchymal cell, that is, a cell showing minimal cytoplasm, limited amounts of rough endoplasmic reticulum and lacks biochemical evidence of protein synthesis.
The term ''fibrocyte'' contrasts with the term ''fibrobl ...
s) to the injured region, where they perform various functions related to wound healing.
Wound repair versus regeneration
An injury is an interruption of morphology and/or functionality of a given tissue. After injury, structural tissue heals with incomplete or complete regeneration.[ Tissue without an interruption to the morphology almost always completely regenerates. An example of complete regeneration without an interruption of the morphology is non-injured tissue, such as skin.][ Non-injured skin has a continued replacement and regeneration of cells which always results in complete regeneration.][
There is a subtle distinction between 'repair' and 'regeneration'.][ ''Repair'' means ''incomplete regeneration''.][
''True tissue regeneration'' or ''complete regeneration'',][ Though after injury mammals can completely regenerate spontaneously, they usually do not completely regenerate. An example of a tissue regenerating completely after an interruption of morphology is the ]endometrium
The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer: the basal layer contains stem cells which regenerate the functional layer. The functional lay ...
; the endometrium after the process of breakdown via the menstruation cycle heals with complete regeneration.extracellular matrix
In biology, the extracellular matrix (ECM), also called intercellular matrix, is a three-dimensional network consisting of extracellular macromolecules and minerals, such as collagen, enzymes, glycoproteins and hydroxyapatite that provide struc ...
(ECM) found in normal/un-injured dermis.myofibroblast
A myofibroblast is a cell phenotype that was first described as being in a state between a fibroblast and a smooth muscle cell.
Structure
Myofibroblasts are contractile web-like fusiform cells that are identifiable by their expression of α-sm ...
differentiation.
A new way of thinking derived from the notion that heparan sulfate
Heparan sulfate (HS) is a linear polysaccharide found in all animal tissues. It occurs as a proteoglycan (HSPG, i.e. Heparan Sulfate ProteoGlycan) in which two or three HS chains are attached in close proximity to cell surface or extracellular m ...
s are key player in tissue homeostasis: the process that makes the tissue replace dead cells by identical cells. In wound areas, tissue homeostasis is lost as the heparan sulfates are degraded preventing the replacement of dead cells by identical cells. Heparan sulfate analogue Heparan sulfate analogues are polymers engineered to mimic several properties of heparan sulfates. They can be constituted with a backbone of polysaccharides, such as poly glucose or glucuronatesPetit et al, Controlled sulfatation of natural anioni ...
s cannot be degraded by all known heparanases and glycanases and bind to the free heparin sulfate binding spots on the ECM, therefore preserving the normal tissue homeostasis and preventing scarring.[Van Neck et al, Heparan sulfate proteoglycan mimetics thrive tissue regeneration: an overview. In Intech book under the working title "Tissue Regeneration", is scheduled for on line publication on Nov 26, 2011"]
Repair or regeneration with regards to hypoxia-inducible factor 1-alpha (HIF-1a). In normal circumstances after injury HIF-1a is degraded by prolyl hydroxylases (PHDs). Scientists found that the simple up-regulation of HIF-1a via PHD inhibitors regenerates lost or damaged tissue in mammals that have a repair response; and the continued down-regulation of Hif-1a results in healing with a scarring response in mammals with a previous regenerative response to the loss of tissue. The act of regulating HIF-1a can either turn off, or turn on the key process of mammalian regeneration.[Zhang Y, Strehin I, Bedelbaeva K, Gourevitch D, Clark L, Leferovich J, Messersmith PB, Heber-Katz E. Drug-induced regeneration in adult mice. Sci Transl Med. 2015;290.]
Scarless wound healing
''Scarless wound healing'' is a concept based on the healing or repair of the skin (or other tissue/organs) after injury with the aim of healing with subjectively and relatively ''less'' scar
A scar (or scar tissue) is an area of fibrous tissue that replaces normal skin after an injury. Scars result from the biological process of wound repair in the skin, as well as in other organs, and tissues of the body. Thus, scarring is a n ...
tissue than normally expected. Scarless healing is sometimes mixed up with the concept of '' scar free healing,'' which is wound healing which results in absolutely no scar (''free'' of scarring). However they are different concepts.
A reverse to scarless wound healing is scarification
Scarification involves scratching, etching, burning/ branding, or superficially cutting designs, pictures, or words into the skin as a permanent body modification or body art. The body modification can take roughly 6–12 months to heal. In th ...
(wound healing to scar more). Historically, certain cultures consider scarification attractive;[Rush, J. (2005). Spiritual tattoo: a cultural history of tattooing, piercing, scarification, branding, and implants, Frog Ltd.] however, this is generally not the case in the modern western society, in which many patients are turning to plastic surgery
Plastic surgery is a surgical specialty involving the restoration, reconstruction or alteration of the human body. It can be divided into two main categories: reconstructive surgery and cosmetic surgery. Reconstructive surgery includes cranio ...
clinics with unrealistic expectations. Depending on scar
A scar (or scar tissue) is an area of fibrous tissue that replaces normal skin after an injury. Scars result from the biological process of wound repair in the skin, as well as in other organs, and tissues of the body. Thus, scarring is a n ...
type, treatment may be invasive (intralesional steroid injections, surgery) and/or conservative ( compression therapy, topical silicone gel, brachytherapy
Brachytherapy is a form of radiation therapy where a sealed radiation source is placed inside or next to the area requiring treatment. ''Brachy'' is Greek for short. Brachytherapy is commonly used as an effective treatment for cervical, prost ...
, photodynamic therapy
Photodynamic therapy (PDT) is a form of phototherapy involving light and a photosensitizing chemical substance, used in conjunction with molecular oxygen to elicit cell death ( phototoxicity).
PDT is popularly used in treating acne. It is used ...
).placebo effect
A placebo ( ) is a substance or treatment which is designed to have no therapeutic value. Common placebos include inert tablets (like sugar pills), inert injections (like saline), sham surgery, and other procedures.
In general, placebos can aff ...
, and the evidence base for the use of many current treatments is poor.tissue regeneration
In biology, regeneration is the process of renewal, restoration, and tissue growth that makes genomes, cells, organisms, and ecosystems resilient to natural fluctuations or events that cause disturbance or damage. Every species is capable of re ...
have expanded due to advances in cellular and molecular biology
Molecular biology is the branch of biology that seeks to understand the molecular basis of biological activity in and between cells, including biomolecular synthesis, modification, mechanisms, and interactions. The study of chemical and phys ...
.[Clark, R. (1996). The molecular and cellular biology of wound repair, Springer Us.] Currently, the principal goals in wound management are to achieve rapid wound closure with a functional tissue that has minimal aesthetic scarring.regeneration
Regeneration may refer to:
Science and technology
* Regeneration (biology), the ability to recreate lost or damaged cells, tissues, organs and limbs
* Regeneration (ecology), the ability of ecosystems to regenerate biomass, using photosynthesis
...
is limited to lower vertebrates, such as salamanders
Salamanders are a group of amphibians typically characterized by their lizard-like appearance, with slender bodies, blunt snouts, short limbs projecting at right angles to the body, and the presence of a tail in both larvae and adults. All te ...
, and invertebrates
Invertebrates are a paraphyletic group of animals that neither possess nor develop a vertebral column (commonly known as a ''backbone'' or ''spine''), derived from the notochord. This is a grouping including all animals apart from the chordate ...
.[ In print the antiquated concept of scarless healing was brought up the early 20th century and appeared in a paper published in the London Lancet. This process involved cutting in a surgical slant, instead of a right angle...; it was described in various Newspapers.]
Cancer
After inflammation, restoration of normal tissue integrity and function is preserved by feedback interactions between diverse cell types mediated by adhesion molecules and secreted cytokines. Disruption of normal feedback mechanisms in cancer threatens tissue integrity and enables a malignant tumor to escape the immune system. An example of the importance of the wound healing response within tumors is illustrated in work by Howard Chang and colleagues at Stanford University studying Breast cancers.
Oral collagen supplements
Preliminary results are promising for th
short and long-term use of oral collagen supplements for wound healing
and skin aging. Oral collagen supplements also increase skin elasticity, hydration, and dermal collagen density. Collagen supplementation is generally safe with no reported adverse events. Further studies are needed to elucidate medical use in skin barrier diseases such as atopic dermatitis and to determine optimal dosing regimens.
Wound Dressings
Modern wound dressing to aid in wound repair have undergone considerable research and development in recent years. Scientists aim to develop wound dressings which have the following characteristics:Antimicrobial
An antimicrobial is an agent that kills microorganisms or stops their growth. Antimicrobial medicines can be grouped according to the microorganisms they act primarily against. For example, antibiotics are used against bacteria, and antifungals ...
properties
* Maintain a humid environment
* Have high permeability to oxygen
* Easily removed from a wound site
* Non-anaphylactic
Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the follow ...
characteristics
Cotton gauze dressings have been the standard of care, despite their dry properties that can adhere to wound surfaces and cause discomfort upon removal. Recent research has set out to improve cotton gauze dressings to bring them closer in line to achieve modern wound dressing properties, by coating cotton gauze wound dressing with a chitosan
Chitosan is a linear polysaccharide composed of randomly distributed β-(1→4)-linked D-glucosamine (deacetylated unit) and ''N''-acetyl-D-glucosamine (acetylated unit). It is made by treating the chitin shells of shrimp and other crustacean ...
/ Ag/ ZnO nanocomposite
Nanocomposite is a multiphase solid material where one of the phases has one, two or three dimensions of less than 100 nanometers (nm) or structures having nano-scale repeat distances between the different phases that make up the material.
The i ...
. These updated dressing provide increase water absorbency and improved antibacterial efficacy.
Wound cleansing
Dirt or dust on the surface of the wound, bacteria, tissue that has died, and fluid from the wound may be cleaned. The evidence supporting the most effective technique is not clear and there is insufficient evidence to conclude whether cleaning wounds is beneficial for promoting healing or whether wound cleaning solutions (polyhexamethylene biguanide, aqueous oxygen peroxide, etc.) are better than sterile water or saline solutions to help venous leg ulcers heal.
Simulating wound healing from a growth perspective
Considerable effort has been devoted to understanding the physical relationships governing wound healing and subsequent scarring, with mathematical models and simulations developed to elucidate these relationships. The growth of tissue around the wound site is a result of the migration of cells and collagen deposition by these cells. The alignment of collagen describes the degree of scarring; basket-weave orientation of collagen is characteristic of normal skin, whereas aligned collagen fibers lead to significant scarring. It has been shown that the growth of tissue and extent of scar formation can be controlled by modulating the stress at a wound site.
The growth of tissue can be simulated using the aforementioned relationships from a biochemical and biomechanical point of view. The biologically active chemicals that play an important role in wound healing are modeled with Fickian diffusion to generate concentration profiles. The balance equation for open systems when modeling wound healing incorporates mass growth due to cell migration and proliferation. Here the following equation is used:
Dtρ0 = Div (R) + R0,
where ''ρ'' represents mass density, ''R'' represents a mass flux (from cell migration), and ''R0'' represents a mass source (from cell proliferation, division, or enlargement). Relationships like these can be incorporated into an agent-based model
An agent-based model (ABM) is a computational model for simulating the actions and interactions of autonomous agents (both individual or collective entities such as organizations or groups) in order to understand the behavior of a system and what ...
s, where the sensitivity to single parameters such as initial collagen alignment, cytokine properties, and cell proliferation rates can be tested.
Wound closure intentions
Successful wound healing is dependent on various cell types, molecular mediators and structural elements.
Primary intention
Primary intention is the healing of a clean wound without tissue loss.laceration
A wound is a rapid onset of injury that involves lacerated or punctured skin (an ''open'' wound), or a contusion (a ''closed'' wound) from blunt force trauma or compression. In pathology, a ''wound'' is an acute injury that damages the epider ...
s, well reduced bone fracture
A bone fracture (abbreviated FRX or Fx, Fx, or #) is a medical condition in which there is a partial or complete break in the continuity of any bone in the body. In more severe cases, the bone may be broken into several fragments, known as a '' ...
s, healing after flap surgery
Flap surgery is a technique in plastic and reconstructive surgery where any type of tissue is lifted from a donor site and moved to a recipient site with an intact blood supply. This is distinct from a graft, which does not have an intact blo ...
.
* Early removal of dressings from clean or clean-contaminated wounds does affect primary healing of wounds.
Secondary intention
* Secondary intention is implemented when primary intention is not possible because of significant tissue damage or loss, usually due to the wound having been created by major trauma.gingivoplasty
Gingivoplasty is the process by which the gingiva are reshaped to correct deformities. Gingivoplasty is similar to gingivectomy but with a different objective. This is a procedure performed to eliminate periodontal pockets along with the reshaping ...
, tooth extraction
A dental extraction (also referred to as tooth extraction, exodontia, exodontics, or informally, tooth pulling) is the removal of teeth from the dental alveolus (socket) in the alveolar bone. Extractions are performed for a wide variety of reaso ...
sockets, poorly reduced fractures, burns, severe lacerations, pressure ulcers.
* There is insufficient evidence that the choice of dressings or topical agents affects the secondary healing of wounds.
* There is lack of evidence for the effectiveness of negative pressure wound therapy in wound healing by secondary intention.
Tertiary intention
(Delayed primary closure):
* The wound is initially cleaned, debrided and observed, typically 4 or 5 days before closure.
* The wound is purposely left open.
* Examples: healing of wounds by use of tissue grafts.
If the wound edges are not reapproximated immediately, delayed primary wound healing transpires. This type of healing may be desired in the case of contaminated wounds. By the fourth day, phagocytosis of contaminated tissues is well underway, and the processes of epithelization, collagen deposition, and maturation are occurring. Foreign materials are walled off by macrophages that may metamorphose into epithelioid cells, which are encircled by mononuclear leukocytes, forming granulomas. Usually the wound is closed surgically at this juncture, and if the "cleansing" of the wound is incomplete, chronic inflammation can ensue, resulting in prominent scarring.
Overview of involved growth factors
Following are the main growth factors
A growth factor is a naturally occurring substance capable of stimulating cell proliferation, wound healing, and occasionally cellular differentiation. Usually it is a secreted protein or a steroid hormone. Growth factors are important for re ...
involved in wound healing:
Complications of wound healing
The major complications are many:
# Deficient scar formation: Results in wound dehiscence
Wound dehiscence is a surgical complication in which a wound ruptures along a surgical incision. Risk factors include age, collagen disorder such as Ehlers–Danlos syndrome, diabetes, obesity, poor knotting or grabbing of stitches, and trauma ...
or rupture of the wound due to inadequate formation of granulation tissue.
# Excessive scar formation: Hypertrophic scar
A hypertrophic scar is a cutaneous condition characterized by deposits of excessive amounts of collagen which gives rise to a raised scar, but not to the degree observed with keloids. Like keloids, they form most often at the sites of pimples, bo ...
, keloid
Keloid, also known as keloid disorder and keloidal scar,
is the formation of a type of scar which, depending on its maturity, is composed mainly of either type III (early) or type I (late) collagen. It is a result of an overgrowth of granulation ...
, desmoid
Aggressive fibromatosis or desmoid tumor is a rare condition. Desmoid tumors arise from cells called fibroblasts, which are found throughout the body and provide structural support, protection to the vital organs, and play a critical role in wou ...
.
# Exuberant granulation (proud flesh
Granulation tissue is new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. Granulation tissue typically grows from the base of a wound and is able to fill wounds of almost any size ...
).
# Deficient contraction (in skin grafts) or excessive contraction (in burns).
# Others: Dystrophic calcification
Dystrophic calcification (DC) is the calcification occurring in degenerated or necrotic tissue, as in hyalinized scars, degenerated foci in leiomyomas, and caseous nodules. This occurs as a reaction to tissue damage, including as a consequence o ...
, pigmentary changes, painful scars, incisional hernia
An incisional hernia is a type of hernia caused by an incompletely-healed surgical wound. Since median incisions in the abdomen are frequent for abdominal exploratory surgery, ventral incisional hernias are often also classified as ventral her ...
Other complications can include infection and Marjolin's ulcer
Marjolin's ulcer refers to an aggressive ulcerating squamous cell carcinoma presenting in an area of previously traumatized, chronically inflamed, or scarred skin.Freedberg, et al. (2003). ''Fitzpatrick's Dermatology in General Medicine''. (6th e ...
.
Biologics, skin substitutes, biomembranes and scaffolds
Advancements in the clinical understanding of wounds and their pathophysiology have commanded significant biomedical innovations in the treatment of acute, chronic, and other types of wounds. Many biologics, skin substitutes, biomembranes and scaffolds have been developed to facilitate wound healing through various mechanisms. This includes a number of products under the trade names such as ''Epicel'', ''Laserskin'', ''Transcyte, Dermagraft, AlloDerm/Strattice, Biobrane, Integra, Apligraf, OrCel, GraftJacket and PermaDerm.''[Vyas KS, Vasconez HC]
Wound Healing: Biologics, Skin Substitutes, Biomembranes and Scaffolds
. Healthcare. 2014; 2(3):356-400.
See also
* Collective cell migration Collective cell migration describes the movements of group of cells and the emergence of collective behavior from cell-environment interactions and cell-cell communication. Collective cell migration is an essential process in the lives of multicellu ...
* Dressing (medical)
A dressing is a sterile pad or compress applied to a wound to promote healing and protect the wound from further harm. A dressing is designed to be in direct contact with the wound, as distinguished from a bandage, which is most often used to hol ...
* History of wound care
* Regeneration in humans
Regeneration in humans is the regrowth of lost tissues or organs in response to injury. This is in contrast to wound healing, or partial regeneration, which involves closing up the injury site with some gradation of scar tissue. Some tissues such a ...
* Wound bed preparation
Wound bed preparation (WBP) is a systematic approach to wound management by identifying and removing barriers to healing. The concept was originally developed in plastic surgery. During the year 2000, the concept was applied to systematizing the t ...
* Wound licking
Wound licking is an instinctive response in humans and many other animals to cover an injury with saliva. Dogs, cats, small rodents, horses, and primates all lick wounds. Saliva contains tissue factor which promotes the blood clotting mechani ...
* Scar free healing
Notes and references
External links
{{Authority control
Healing
Skin physiology
Physiology
Trauma surgery
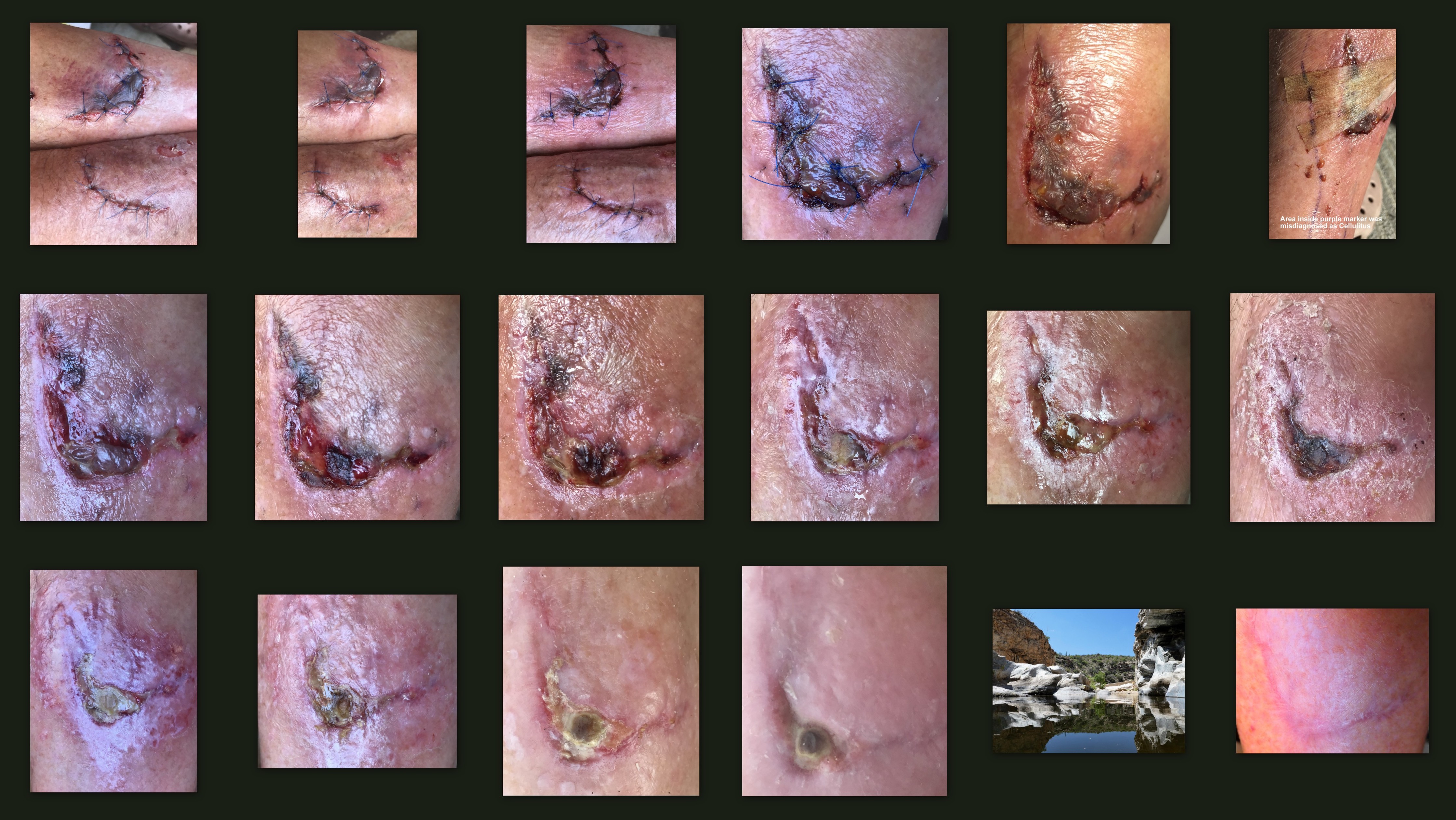 The wound healing process is not only complex but fragile, and it is susceptible to interruption or failure leading to the formation of non-healing
The wound healing process is not only complex but fragile, and it is susceptible to interruption or failure leading to the formation of non-healing 
 As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue. Epithelial cells have the ability to phagocytize debris such as dead tissue and bacterial matter that would otherwise obstruct their path. Because they must dissolve any scab that forms, keratinocyte migration is best enhanced by a moist environment, since a dry one leads to formation of a bigger, tougher scab. To make their way along the tissue, keratinocytes must dissolve the clot, debris, and parts of the ECM in order to get through. They secrete
As keratinocytes migrate, they move over granulation tissue but stay underneath the scab, thereby separating the scab from the underlying tissue. Epithelial cells have the ability to phagocytize debris such as dead tissue and bacterial matter that would otherwise obstruct their path. Because they must dissolve any scab that forms, keratinocyte migration is best enhanced by a moist environment, since a dry one leads to formation of a bigger, tougher scab. To make their way along the tissue, keratinocytes must dissolve the clot, debris, and parts of the ECM in order to get through. They secrete