|
Total Complement Activity
Total complement activity (TCA) refers to a series of tests that determine the functioning of the complement system in an individual. Tests A variety of tests can be used to measure TCA, but the most commonly used on is the CH50 test. Other tests include the liposome immunoassay (LIA), single tube titration method, and the plate-hemolysis method. CH50 Procedure The test is based on the capacity of an individual's serum to lyse sheep erythrocytes coated with anti-sheep antibodies (preferably rabbit IgG). The individual's serum is diluted until the minimum concentration is reached that 50% of the sheep red blood cells are lysed, and that concentration is recorded as the CH50. The CH50 is testing the classical complement pathway in an individual thus requiring functioning C1-C9 factors. CH50 Interpretation If an individual has deficient or malfunctioning complement factors, then at a baseline they have decreased capacity to lyse the erythrocytes. Therefore, any dilution t ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Complement System
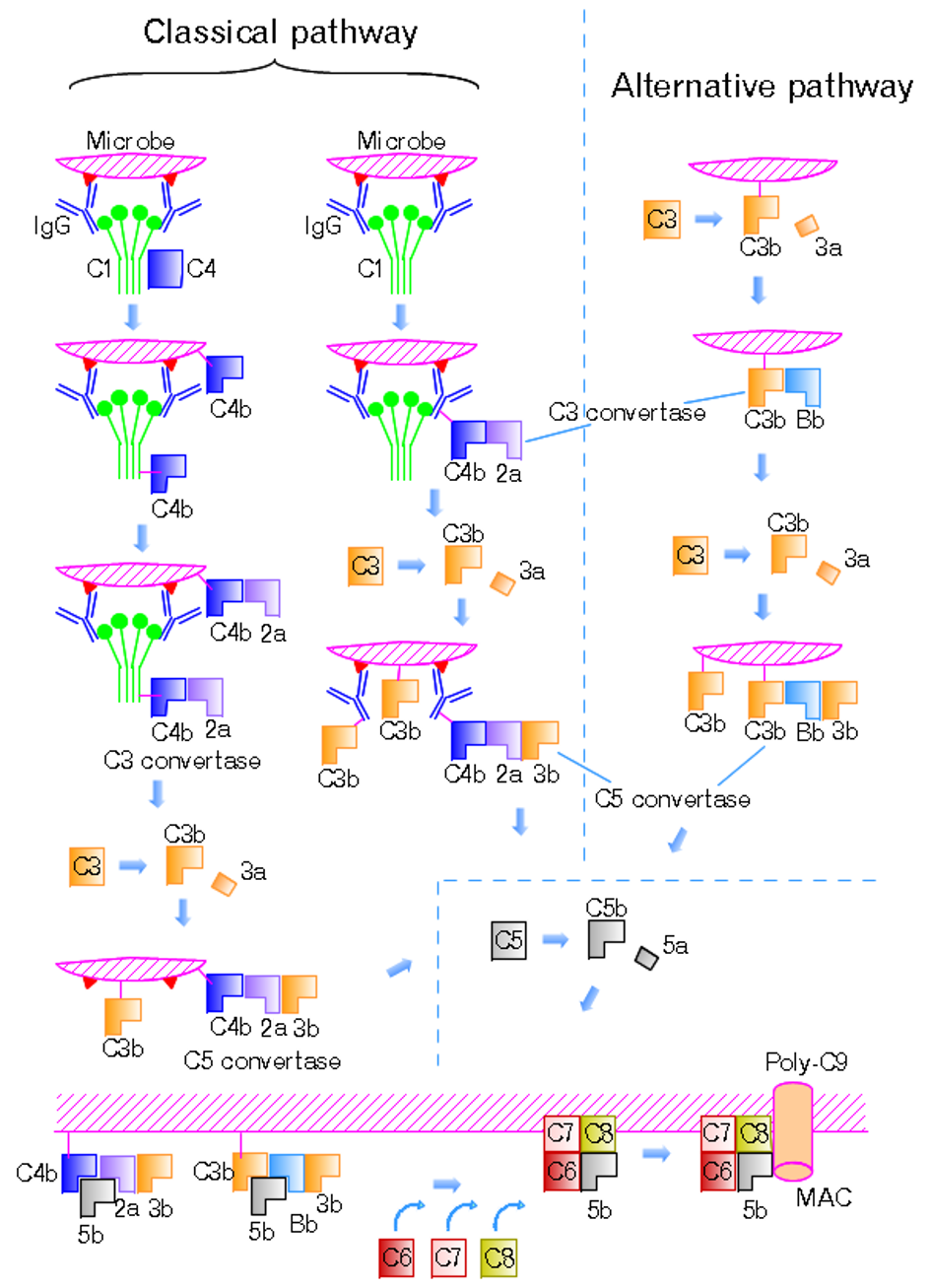
The complement system, also known as complement cascade, is a part of the immune system that enhances (complements) the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism, promote inflammation, and attack the pathogen's cell membrane. It is part of the innate immune system, which is not adaptable and does not change during an individual's lifetime. The complement system can, however, be recruited and brought into action by antibodies generated by the adaptive immune system. The complement system consists of a number of small proteins that are synthesized by the liver, and circulate in the blood as inactive precursors. When stimulated by one of several triggers, proteases in the system cleave specific proteins to release cytokines and initiate an amplifying cascade of further cleavages. The end result of this ''complement activation'' or ''complement fixation'' cascade is stimulation of phagocytes to clear foreign and damaged material ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Immunoglobulin G
Immunoglobulin G (Ig G) is a type of antibody. Representing approximately 75% of serum antibodies in humans, IgG is the most common type of antibody found in blood circulation. IgG molecules are created and released by plasma B cells. Each IgG antibody has two paratopes. Function Antibodies are major components of humoral immunity. IgG is the main type of antibody found in blood and extracellular fluid, allowing it to control infection of body tissues. By binding many kinds of pathogens such as viruses, bacteria, and fungi, IgG protects the body from infection. It does this through several mechanisms: * IgG-mediated binding of pathogens causes their immobilization and binding together via agglutination; IgG coating of pathogen surfaces (known as opsonization) allows their recognition and ingestion by phagocytic immune cells leading to the elimination of the pathogen itself; * IgG activates all the classical pathway of the complement system, a cascade of immune protein pr ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Classical Complement Pathway
The classical complement pathway is one of three pathways which activate the complement system, which is part of the immune system. The classical complement pathway is initiated by antigen-antibody complexes with the antibody isotypes IgG and IgM. Following activation, a series of proteins are recruited to generate C3 convertase (C4b2b, historically referred C4b2a), which cleaves the C3 protein. The C3b component of the cleaved C3 binds to C3 convertase (C4b2b) to generate C5 convertase (C4b2b3b), which cleaves the C5 protein. The cleaved products attract phagocytes to the site of infection and tags target cells for elimination by phagocytosis. In addition, the C5 convertase initiates the terminal phase of the complement system, leading to the assembly of the membrane attack complex ( MAC). The membrane attack complex creates a pore on the target cell's membrane, inducing cell lysis and death. The classical complement pathway can also be activated by apoptotic cells, necrotic ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage causes tissue repair and subsequent formation of scar tissue, which over time can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen may become spontaneously infected. More serious complications include hepatic encephalopathy, bleeding from dilated veins ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hepatitis
Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is ''acute'' if it resolves within six months, and '' chronic'' if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer. Hepatitis is most commonly caused by the virus ''hepatovirus A'', '' B'', '' C'', '' D'', and '' E''. Other viruses can also cause liver inflammation, including cytomegalovirus, Epstein–Barr virus, and yellow fever virus. Other common causes of hepatitis include heavy alcohol use, certain medications, toxins, other infections, autoimmune diseases, and non-alcoholic steatohepatitis (NASH). Hepa ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Systemic Lupus Erythematosus
Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms. The cause of SLE is not clear. It is thought to involve a mixture of genetics combined with environmental factors. Among identical twins, if one is affected there is a 24% chance the other one will also develop the disease. Female sex hormones, sunlight, smoking, vitamin D deficiency, and certain infections are also believed to increase a person's risk. The mechanism involves an immune response by autoantibodies against a person's own tissues. T ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hereditary Angioedema
Hereditary angioedema (HAE) is a disorder that results in recurrent attacks of severe swelling. The swelling most commonly affects the arms, legs, face, intestinal tract, and airway. If the intestinal tract is affected, abdominal pain and vomiting may occur. Swelling of the airway can result in its obstruction and trouble breathing. Without preventive treatment, attacks typically occur every two weeks and last for a few days. There are three main types of HAE. Types I and II are caused by a mutation in the '' SERPING1'' gene, which makes the C1 inhibitor protein, while type III is often due to a mutation in the '' F12'' (factor XII) gene. The result is increased levels of bradykinin, which promotes swelling. The condition may be inherited in an autosomal dominant manner or occur as a new mutation. Triggers for an attack may include minor trauma or stress, but attacks often occur without any obvious preceding event. Diagnosis of types I and II is based on measurement of C4 and C ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bleeding, prolonged cough, unexplained weight loss, and a change in bowel movements. While these symptoms may indicate cancer, they can also have other causes. Over 100 types of cancers affect humans. Tobacco use is the cause of about 22% of cancer deaths. Another 10% are due to obesity, poor diet, lack of physical activity or excessive drinking of alcohol. Other factors include certain infections, exposure to ionizing radiation, and environmental pollutants. In the developing world, 15% of cancers are due to infections such as ''Helicobacter pylori'', hepatitis B, hepatitis C, human papillomavirus infection, Epstein–Barr virus and human immunodeficiency virus (HIV). These factors act, at least partly, by changing the genes of ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Ulcerative Colitis
Ulcerative colitis (UC) is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and anemia may also occur. Often, symptoms come on slowly and can range from mild to severe. Symptoms typically occur intermittently with periods of no symptoms between flares. Complications may include abnormal dilation of the colon (megacolon), inflammation of the eye, joints, or liver, and colon cancer. The cause of UC is unknown. Theories involve immune system dysfunction, genetics, changes in the normal gut bacteria, and environmental factors. Rates tend to be higher in the developed world with some proposing this to be the result of less exposure to intestinal infections, or to a Western diet and lifestyle. The removal of the appendix at an early age may be protective. Diagnosis is typically by colonoscopy with tissue biopsies. It is ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Terminal Complement Pathway Deficiency
Terminal complement pathway deficiency is a genetic condition affecting the complement membrane attack complex (MAC). It involves deficiencies of C5, C6, C7, and C8. (While C9 is part of the MAC, and deficiencies have been identified, it is not required for cell lysis.) People with this condition are prone to meningococcal ''Neisseria meningitidis'', often referred to as meningococcus, is a Gram-negative bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia, a life-threatening sepsis. The bacterium is referred to as a ... infection. Vaccination may be recommended. Cause Diagnosis Suspect terminal complement pathway deficiency with patients who have more than one episode of Neisseria infection. Initial complement tests often include C3 and C4, but not C5 through C9. Instead, the CH50 result may play a role in diagnosis: if the CH50 level is low but C3 and C4 are normal, then analysis of the individual terminal components ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Complement System
The complement system, also known as complement cascade, is a part of the immune system that enhances (complements) the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism, promote inflammation, and attack the pathogen's cell membrane. It is part of the innate immune system, which is not adaptable and does not change during an individual's lifetime. The complement system can, however, be recruited and brought into action by antibodies generated by the adaptive immune system. The complement system consists of a number of small proteins that are synthesized by the liver, and circulate in the blood as inactive precursors. When stimulated by one of several triggers, proteases in the system cleave specific proteins to release cytokines and initiate an amplifying cascade of further cleavages. The end result of this ''complement activation'' or ''complement fixation'' cascade is stimulation of phagocytes to clear foreign and damaged material ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |





.png)