|
OPQRST
__NOTOC__OPQRST is a mnemonic initialism used by medical professionals to accurately discern reasons for a patient's symptoms and history in the event of an acute illness. It is specifically adapted to elicit symptoms of a possible heart attack. Each letter stands for an important line of questioning for the patient assessment. This is usually taken along with vital signs and the SAMPLE history and would usually be recorded by the person delivering the aid, such as in the "Subjective" portion of a SOAP note, for later reference. "PQRST" (onset "O") is sometimes used in conjunction. The term "OPQRST-AAA" adds "aggravating/alleviating factors", "associated symptoms", and "attributions/adaptations". Use The parts of the mnemonic are: ;Onset of the event :What the patient was doing when it started (active, inactive, stressed, etc.), whether the patient believes that activity prompted the pain, and whether the onset was sudden, gradual or part of an ongoing chronic problem. ; ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medical Mnemonics
This is a list of mnemonics used in medicine and medical science, categorized and alphabetized. A mnemonic is any technique that assists the human memory with information retention or retrieval by making abstract or impersonal information more accessible and meaningful, and therefore easier to remember; many of them are acronyms or initialisms which reduce a lengthy set of terms to a single, easy-to-remember word or phrase. Mnemonics with wikipages # ABC — airway, breathing, and circulation # AEIOU-TIPS — causes of altered mental status # APGAR — a backronym for appearance, pulse, grimace, activity, respiration (used to assess newborn babies) # ASHICE — age, sex, history, injuries/illness, condition, ETA/extra information # FAST — face, arms, speech, time (stroke symptoms) # Hs and Ts — causes of cardiac arrest # IS PATH WARM? — suicide risk factors # OPQRST — onset, provocation, quality, region, severity, time (symptom checklist often used by first responder ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Sample History
SAMPLE history is a mnemonic acronym to remember key questions for a person's medical assessment. The SAMPLE history is sometimes used in conjunction with vital signs and OPQRST. The questions are most commonly used in the field of emergency medicine by first responders during the secondary assessment. It is used for alert people, but often much of this information can also be obtained from the family or friend of an unresponsive person. In the case of severe trauma, this portion of the assessment is less important. A derivative of SAMPLE history is AMPLE history which places a greater emphasis on a person's medical history. Meaning The parts of the mnemonic are: *S – Signs/Symptoms (Symptoms are important but they are subjective.) *A – Allergies *M – Medications *P – Past Pertinent medical history *L – Last Oral Intake (Sometimes also Last Menstrual Cycle.) *E – Events Leading Up To Present Illness / Injury See also * OPQRST * DCAP-BTLS *ABC (medicine) ABC and ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
SAMPLE History
SAMPLE history is a mnemonic acronym to remember key questions for a person's medical assessment. The SAMPLE history is sometimes used in conjunction with vital signs and OPQRST. The questions are most commonly used in the field of emergency medicine by first responders during the secondary assessment. It is used for alert people, but often much of this information can also be obtained from the family or friend of an unresponsive person. In the case of severe trauma, this portion of the assessment is less important. A derivative of SAMPLE history is AMPLE history which places a greater emphasis on a person's medical history. Meaning The parts of the mnemonic are: *S – Signs/Symptoms (Symptoms are important but they are subjective.) *A – Allergies *M – Medications *P – Past Pertinent medical history *L – Last Oral Intake (Sometimes also Last Menstrual Cycle.) *E – Events Leading Up To Present Illness / Injury See also * OPQRST * DCAP-BTLS *ABC (medicine) ABC and ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
History Of The Present Illness
Following the chief complaint in medical history taking, a history of the present illness (abbreviated HPI) (termed history of presenting complaint (HPC) in the UK) refers to a detailed interview prompted by the chief complaint or presenting symptom (for example, pain). Questions to include Different sources include different questions to be asked while conducting an HPI. Several acronyms have been developed to categorize the appropriate questions to include. The Centers for Medicare and Medicaid Services has published criteria for what constitutes a reimbursable HPI. A "brief HPI" constitutes one to three of these elements. An "extended HPI" includes four or more of these elements. Also usable is SOCRATES. For chronic pain, the Stanford Five Stanford Five in pain management is an augmented set of medical history obtained by the clinician during the medical interview for patients with pain. Unlike the OPQRST of pain history designed to elicit aspects of the pain experience ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
SOAP Note
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. Documenting patient encounters in the medical record is an integral part of practice workflow starting with appointment scheduling, patient check-in and exam, documentation of notes, check-out, rescheduling, and medical billing. Additionally, it serves as a general cognitive framework for physicians to follow as they assess their patients. The SOAP note originated from the ''problem-oriented medical record'' (POMR), developed nearly 50 years ago by Lawrence Weed, MD. It was initially developed for physicians to allow them to approach complex patients with multiple problems in a highly organized way. Today, it is widely adopted as a communication tool between inter-disciplinary healthcare providers as a way to document a patient's progress. SOAP n ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Myocardial Infarction
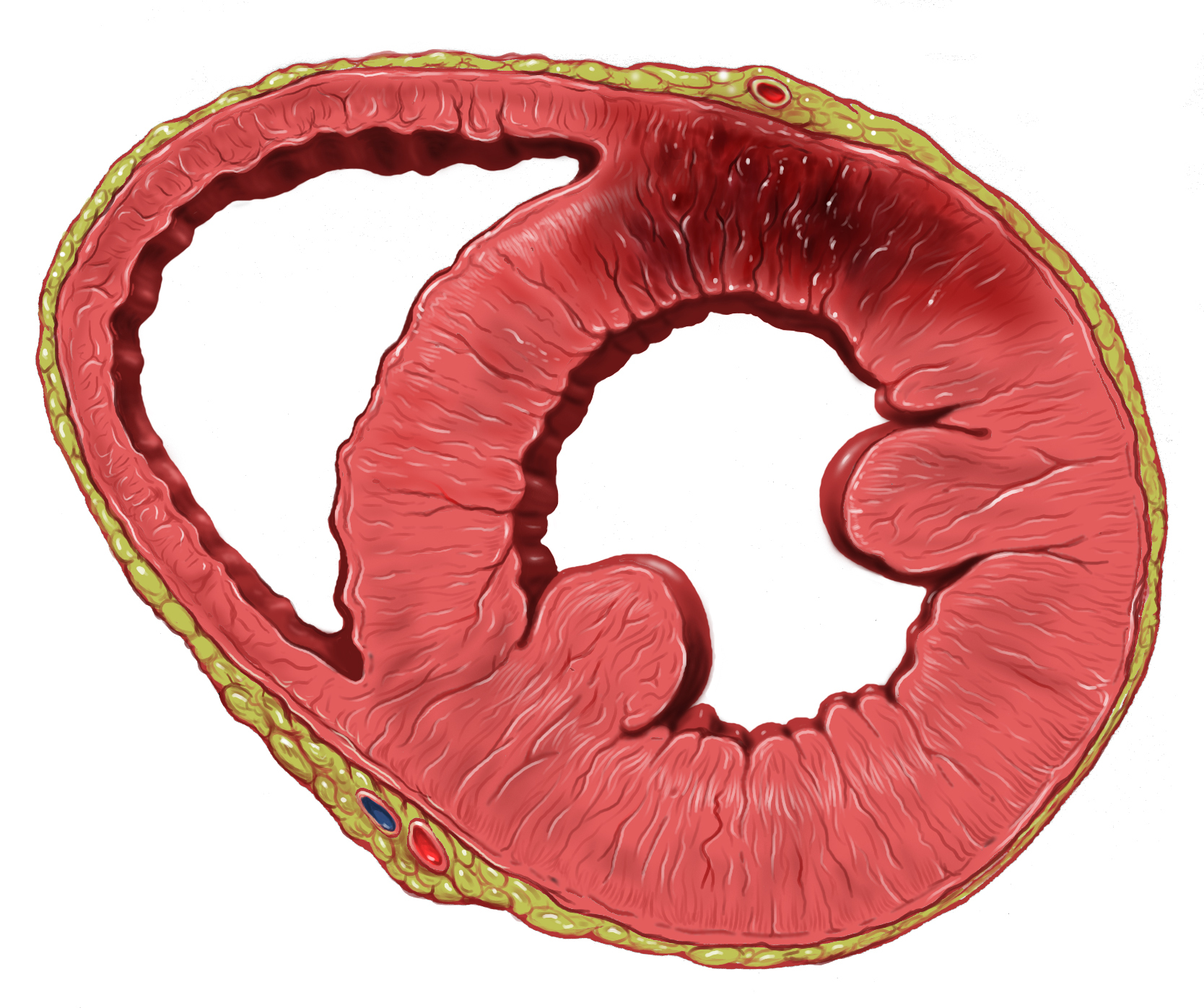
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest. Most MIs occur due to coronary artery disease. Risk factors include high blood pressure, smoking, diabetes, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Health Assessment
A health assessment is a plan of care that identifies the specific needs of a person and how those needs will be addressed by the healthcare system or skilled nursing facility. Health assessment is the evaluation of the health status by performing a physical exam after taking a health history. It is done to detect diseases early in people that may look and feel well. Evidence does not support routine health assessments in otherwise healthy people. Health assessment is the evaluation of the health status of an individual along the health continuum. The purpose of the assessment is to establish where on the health continuum the individual is because this guides how to approach and treat the individual. The health care approaches range from preventive, to treatment, to palliative care in relation to the individual's status on the health continuum. It is not the treatment or treatment plan. The plan related to findings is a care plan which is preceded by the specialty such as medic ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Vital Signs
Vital signs (also known as vitals) are a group of the four to six most crucial medical signs that indicate the status of the body's vital (life-sustaining) functions. These measurements are taken to help assess the general physical health of a person, give clues to possible diseases, and show progress toward recovery. The normal ranges for a person's vital signs vary with age, weight, gender, and overall health. There are four primary vital signs: body temperature, blood pressure, pulse (heart rate), and breathing rate (respiratory rate), often notated as BT, BP, HR, and RR. However, depending on the clinical setting, the vital signs may include other measurements called the "fifth vital sign" or "sixth vital sign". Vital signs are recorded using the LOINC internationally accepted standard coding system. Early warning scores have been proposed that combine the individual values of vital signs into a single score. This was done in recognition that deteriorating vital signs ofte ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Acute (medical)
In medicine, describing a disease as acute denotes that it is of short duration and, as a corollary of that, of recent onset. The quantification of how much time constitutes "short" and "recent" varies by disease and by context, but the core denotation of "acute" is always qualitatively in contrast with " chronic", which denotes long-lasting disease (for example, in acute leukaemia and chronic leukaemia). In addition, "acute" also often connotes two other meanings: sudden onset and severity, such as in acute myocardial infarction (AMI), where suddenness and severity are both established aspects of the meaning. It thus often connotes that the condition is fulminant (as in the AMI example), but not always (as in acute rhinitis, which is usually synonymous with the common cold). The one thing that acute MI and acute rhinitis have in common is that they are not chronic. They can happen again (as in recurrent pneumonia, that is, multiple acute pneumonia episodes), but they are not t ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Initialism
An acronym is a word or name formed from the initial components of a longer name or phrase. Acronyms are usually formed from the initial letters of words, as in ''NATO'' (''North Atlantic Treaty Organization''), but sometimes use syllables, as in ''Benelux'' (short for ''Belgium, the Netherlands, and Luxembourg''). They can also be a mixture, as in ''radar'' (''Radio Detection And Ranging''). Acronyms can be pronounced as words, like ''NASA'' and ''UNESCO''; as individual letters, like ''FBI'', ''TNT'', and ''ATM''; or as both letters and words, like '' JPEG'' (pronounced ') and ''IUPAC''. Some are not universally pronounced one way or the other and it depends on the speaker's preference or the context in which it is being used, such as '' SQL'' (either "sequel" or "ess-cue-el"). The broader sense of ''acronym''—the meaning of which includes terms pronounced as letters—is sometimes criticized, but it is the term's original meaning and is in common use. Dictionary and st ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Palpation
Palpation is the process of using one's hands to check the body, especially while perceiving/diagnosing a disease or illness. Usually performed by a health care practitioner, it is the process of feeling an object in or on the body to determine its size, shape, firmness, or location (for example, a veterinarian can feel the stomach of a pregnant animal to ensure good health and successful delivery). Palpation is an important part of the physical examination; the sense of touch is just as important in this examination as the sense of sight is. Physicians develop great skill in palpating problems below the surface of the body, becoming able to detect things that untrained persons would not. Mastery of anatomy and much practice are required to achieve a high level of skill. The concept of being able to detect or notice subtle tactile signs and to recognize their significance or implications is called appreciating them (just as in general vocabulary one can speak of appreciating ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Myocardial Infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest. Most MIs occur due to coronary artery disease. Risk factors include high blood pressure, smoking, diabetes, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
.png)

