Myocardial Infarction on:
[Wikipedia]
[Google]
[Amazon]
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause
 If impaired blood flow to the heart lasts long enough, it triggers a process called the ischemic cascade; the heart cells in the territory of the blocked coronary artery die ( infarction), chiefly through
If impaired blood flow to the heart lasts long enough, it triggers a process called the ischemic cascade; the heart cells in the territory of the blocked coronary artery die ( infarction), chiefly through

 Electrocardiograms (ECGs) are a series of leads placed on a person's chest that measure electrical activity associated with contraction of the heart muscle. The taking of an ECG is an important part of the workup of an AMI, and ECGs are often not just taken once but may be repeated over minutes to hours, or in response to changes in signs or symptoms.
ECG readouts product a waveform with different labelled features. In addition to a rise in biomarkers, a rise in the ST segment, changes in the shape or flipping of T waves, new Q waves, or a new left bundle branch block can be used to diagnose an AMI. In addition, ST elevation can be used to diagnose an ST segment myocardial infarction (STEMI). A rise must be new in V2 and V3 ≥2 mm (0,2 mV) for males or ≥1.5 mm (0.15 mV) for females or ≥1 mm (0.1 mV) in two other adjacent chest or limb leads. ST elevation is associated with infarction, and may be preceded by changes indicating ischemia, such as ST depression or inversion of the T waves. Abnormalities can help differentiate the location of an infarct, based on the leads that are affected by changes. Early STEMIs may be preceded by peaked T waves. Other ECG abnormalities relating to complications of acute myocardial infarctions may also be evident, such as atrial or ventricular fibrillation.
Electrocardiograms (ECGs) are a series of leads placed on a person's chest that measure electrical activity associated with contraction of the heart muscle. The taking of an ECG is an important part of the workup of an AMI, and ECGs are often not just taken once but may be repeated over minutes to hours, or in response to changes in signs or symptoms.
ECG readouts product a waveform with different labelled features. In addition to a rise in biomarkers, a rise in the ST segment, changes in the shape or flipping of T waves, new Q waves, or a new left bundle branch block can be used to diagnose an AMI. In addition, ST elevation can be used to diagnose an ST segment myocardial infarction (STEMI). A rise must be new in V2 and V3 ≥2 mm (0,2 mV) for males or ≥1.5 mm (0.15 mV) for females or ≥1 mm (0.1 mV) in two other adjacent chest or limb leads. ST elevation is associated with infarction, and may be preceded by changes indicating ischemia, such as ST depression or inversion of the T waves. Abnormalities can help differentiate the location of an infarct, based on the leads that are affected by changes. Early STEMIs may be preceded by peaked T waves. Other ECG abnormalities relating to complications of acute myocardial infarctions may also be evident, such as atrial or ventricular fibrillation.

File:UOTW 36 - Ultrasound of the Week 1.webm, Poor movement of the heart due to an MI as seen on ultrasound
File:UOTW 36 - Ultrasound of the Week 2.webm, Pulmonary edema due to an MI as seen on ultrasound

.
. Board of Industrial Insurance Appeals. Retrieved November 22, 2006. In addition, in some jurisdictions, heart attacks had by persons in particular occupations such as police officers may be classified as line-of-duty injuries by statute or policy. In some countries or states, a person having had an MI may be prevented from participating in activity that puts other people's lives at risk, for example driving a car or flying an airplane.
American Heart Association's Heart Attack web site
— Information and resources for preventing, recognizing, and treating a heart attack. * TIMI Score fo
UA/NSTEMI
an
STEMI
HEART Score for Major Cardiac Events
* {{Authority control Aging-associated diseases Causes of death Ischemic heart diseases Medical emergencies Articles containing video clips Wikipedia medicine articles ready to translate Acute pain Wikipedia emergency medicine articles ready to translate
heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, a ...
, an irregular heartbeat
Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults ...
, cardiogenic shock or cardiac arrest.
Most MIs occur due to coronary artery disease. Risk factors include high blood pressure
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. Long-term high bl ...
, smoking
Smoking is a practice in which a substance is burned and the resulting smoke is typically breathed in to be tasted and absorbed into the bloodstream. Most commonly, the substance used is the dried leaves of the tobacco plant, which have bee ...
, diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
, lack of exercise
Sedentary lifestyle is a lifestyle type, in which one is physically inactive and does little or no physical movement and or exercise. A person living a sedentary lifestyle is often sitting or lying down while engaged in an activity like soci ...
, obesity, high blood cholesterol
Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood. It is a form of hyperlipidemia (high levels of lipids in the blood), hyperlipoproteinemia (high levels of lipoproteins in the blood), ...
, poor diet and excessive alcohol intake
Alcohol abuse encompasses a spectrum of unhealthy alcohol drinking behaviors, ranging from binge drinking to alcohol dependence, in extreme cases resulting in health problems for individuals and large scale social problems such as alcohol-relat ...
. The complete blockage of a coronary artery caused by a rupture of an atherosclerotic plaque is usually the underlying mechanism of an MI. MIs are less commonly caused by coronary artery spasms, which may be due to cocaine, significant emotional stress (commonly known as Takotsubo syndrome
Takotsubo cardiomyopathy or Takotsubo syndrome (TTS), also known as stress cardiomyopathy, is a type of non-ischemic cardiomyopathy in which there is a sudden temporary weakening of the muscular portion of the heart. It usually appears after a ...
or ''broken heart syndrome'') and extreme cold, among others. A number of tests are useful to help with diagnosis, including electrocardiograms (ECGs), blood tests and coronary angiography. An ECG, which is a recording of the heart's electrical activity, may confirm an ST elevation MI ( STEMI), if ST elevation is present. Commonly used blood tests include troponin and less often creatine kinase MB.
Treatment of an MI is time-critical. Aspirin is an appropriate immediate treatment for a suspected MI. Nitroglycerin
Nitroglycerin (NG), (alternative spelling of nitroglycerine) also known as trinitroglycerin (TNG), nitro, glyceryl trinitrate (GTN), or 1,2,3-trinitroxypropane, is a dense, colorless, oily, explosive liquid most commonly produced by nitrating g ...
or opioids may be used to help with chest pain; however, they do not improve overall outcomes. Supplemental oxygen is recommended in those with low oxygen levels or shortness of breath. In a STEMI, treatments attempt to restore blood flow to the heart and include percutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(PCI), where the arteries are pushed open and may be stented, or thrombolysis, where the blockage is removed using medications. People who have a non-ST elevation myocardial infarction ( NSTEMI) are often managed with the blood thinner heparin
Heparin, also known as unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. Since heparins depend on the activity of antithrombin, they are considered anticoagulants. Specifically it is also used in the treatm ...
, with the additional use of PCI in those at high risk. In people with blockages of multiple coronary arteries and diabetes, coronary artery bypass surgery (CABG) may be recommended rather than angioplasty. After an MI, lifestyle modifications, along with long-term treatment with aspirin, beta blockers and statins, are typically recommended.
Worldwide, about 15.9 million myocardial infarctions occurred in 2015. More than 3 million people had an ST elevation MI, and more than 4 million had an NSTEMI. STEMIs occur about twice as often in men as women. About one million people have an MI each year in the United States. In the developed world, the risk of death in those who have had an STEMI is about 10%. Rates of MI for a given age have decreased globally between 1990 and 2010. In 2011, an MI was one of the top five most expensive conditions during inpatient hospitalizations in the US, with a cost of about $11.5 billion for 612,000 hospital stays.
Terminology
Myocardial infarction (MI) refers to tissue death ( infarction) of the heart muscle (myocardium
Cardiac muscle (also called heart muscle, myocardium, cardiomyocytes and cardiac myocytes) is one of three types of vertebrate muscle tissues, with the other two being skeletal muscle and smooth muscle. It is an involuntary, striated muscle that ...
) caused by ischaemia, the lack of oxygen delivery to myocardial tissue. It is a type of acute coronary syndrome, which describes a sudden or short-term change in symptoms related to blood flow to the heart. Unlike the other type of acute coronary syndrome, unstable angina, a myocardial infarction occurs when there is cell death, which can be estimated by measuring by a blood test for biomarkers (the cardiac protein troponin). When there is evidence of an MI, it may be classified as an ST elevation myocardial infarction (STEMI) or Non-ST elevation myocardial infarction (NSTEMI) based on the results of an ECG.
The phrase "heart attack" is often used non-specifically to refer to myocardial infarction. An MI is different from—but can cause— cardiac arrest, where the heart is not contracting at all or so poorly that all vital organs cease to function, thus might lead to death. It is also distinct from heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, a ...
, in which the pumping action of the heart is impaired. However, an MI may lead to heart failure.
Signs and symptoms
Chest pain that may or may not radiate to other parts of the body is the most typical and significant symptom of myocardial infarction. It might be accompanied by other symptoms such as sweating.Pain
Chest pain is one of the most common symptoms of acute myocardial infarction and is often described as a sensation of tightness, pressure, or squeezing. Pain radiates most often to the left arm, but may also radiate to the lower jaw, neck, right arm, back, and upper abdomen. The pain most suggestive of an acute MI, with the highest likelihood ratio, is pain radiating to the right arm and shoulder. Similarly, chest pain similar to a previous heart attack is also suggestive. The pain associated with MI is usually diffuse, does not change with position, and lasts for more than 20 minutes. It might be described as pressure, tightness, knifelike, tearing, burning sensation (all these are also manifested during other diseases). It could be felt as an unexplained anxiety, and pain might be absent altogether.Levine's sign
Levine's sign is a clenched fist held over the chest to describe ischemic chest pain.
It is named for Samuel A. Levine (1891–1966), an influential American cardiologist, who first observed that many patients with chest pain made this same sign ...
, in which a person localizes the chest pain by clenching one or both fists over their sternum, has classically been thought to be predictive of cardiac chest pain, although a prospective observational study showed it had a poor positive predictive value
The positive and negative predictive values (PPV and NPV respectively) are the proportions of positive and negative results in statistics and diagnostic tests that are true positive and true negative results, respectively. The PPV and NPV descr ...
.
Typically, chest pain because of ischemia, be it unstable angina or myocardial infarction, lessens with the use of nitroglycerin
Nitroglycerin (NG), (alternative spelling of nitroglycerine) also known as trinitroglycerin (TNG), nitro, glyceryl trinitrate (GTN), or 1,2,3-trinitroxypropane, is a dense, colorless, oily, explosive liquid most commonly produced by nitrating g ...
, but nitroglycerin may also relieve chest pain arising from non-cardiac causes.
Other
Chest pain may be accompanied bysweating
Perspiration, also known as sweating, is the production of fluids secreted by the sweat glands in the skin of mammals.
Two types of sweat glands can be found in humans: eccrine glands and apocrine glands. The eccrine sweat glands are distr ...
, nausea or vomiting, and fainting, and these symptoms may also occur without any pain at all. In women, the most common symptoms of myocardial infarction include shortness of breath, weakness, and fatigue
Fatigue describes a state of tiredness that does not resolve with rest or sleep. In general usage, fatigue is synonymous with extreme tiredness or exhaustion that normally follows prolonged physical or mental activity. When it does not resolve ...
. Women are more likely to have unusual or unexplained tiredness and nausea or vomiting as symptoms. Women having heart attacks are more likely to have palpitations, back pain, labored breath, vomiting, and left arm pain than men, although the studies showing these differences had high variability. Women are less likely to report chest pain during a heart attack and more likely to report nausea, jaw pain, neck pain, cough, and fatigue, although these findings are inconsistent across studies. Women with heart attacks also had more indigestion, dizziness, loss of appetite, and loss of consciousness. Shortness of breath is a common, and sometimes the only symptom, occurring when damage to the heart limits the output of the left ventricle, with breathlessness arising either from low oxygen in the blood, or pulmonary edema. Other less common symptoms include weakness, light-headedness, palpitations, and abnormalities in heart rate or blood pressure. These symptoms are likely induced by a massive surge of catecholamines from the sympathetic nervous system
The sympathetic nervous system (SNS) is one of the three divisions of the autonomic nervous system, the others being the parasympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of th ...
, which occurs in response to pain and, where present, low blood pressure. Loss of consciousness due to inadequate blood flow to the brain
The brain is an organ that serves as the center of the nervous system in all vertebrate and most invertebrate animals. It consists of nervous tissue and is typically located in the head ( cephalization), usually near organs for special ...
and cardiogenic shock, and sudden death
Sudden Death or Sudden death may refer to:
Medical
* Cardiac arrest, also known as sudden cardiac death, natural death from cardiac causes
* Sudden cardiac death of athletes
* Sudden infant death syndrome
* Sudden unexpected death in epilepsy
* ...
, frequently due to the development of ventricular fibrillation, can occur in myocardial infarctions. Cardiac arrest, and atypical symptoms such as palpitations
Palpitations are perceived abnormalities of the heartbeat characterized by awareness of cardiac muscle contractions in the chest, which is further characterized by the hard, fast and/or irregular beatings of the heart.
Symptoms include a rapi ...
, occur more frequently in women, the elderly, those with diabetes, in people who have just had surgery, and in critically ill patients.
Absence
"Silent" myocardial infarctions can happen without any symptoms at all. These cases can be discovered later on electrocardiograms, using blood enzyme tests, or at autopsy after a person has died. Such silent myocardial infarctions represent between 22 and 64% of all infarctions, and are more common in theelderly
Old age refers to ages nearing or surpassing the life expectancy of human beings, and is thus the end of the human life cycle. Terms and euphemisms for people at this age include old people, the elderly (worldwide usage), OAPs (British usage ...
, in those with diabetes mellitus
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
and after heart transplantation. In people with diabetes, differences in pain threshold, autonomic neuropathy, and psychological
Psychology is the scientific study of mind and behavior. Psychology includes the study of conscious and unconscious phenomena, including feelings and thoughts. It is an academic discipline of immense scope, crossing the boundaries between t ...
factors have been cited as possible explanations for the lack of symptoms. In heart transplantation, the donor
A donor in general is a person, organization or government which donates something voluntarily. The term is usually used to represent a form of pure altruism, but is sometimes used when the payment for a service is recognized by all parties as rep ...
heart is not fully innervated by the nervous system of the recipient.
Risk factors
The most prominent risk factors for myocardial infarction are older age, activelysmoking
Smoking is a practice in which a substance is burned and the resulting smoke is typically breathed in to be tasted and absorbed into the bloodstream. Most commonly, the substance used is the dried leaves of the tobacco plant, which have bee ...
, high blood pressure
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. Long-term high bl ...
, diabetes mellitus
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
, and total cholesterol and high-density lipoprotein
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins. Lipoproteins are complex particles composed of multiple proteins which transport all fat molecules ( lipids) around the body within the water outside cells. They are ...
levels. Many risk factors of myocardial infarction are shared with coronary artery disease, the primary cause of myocardial infarction, with other risk factors including male sex, low levels of physical activity, a past family history, obesity, and alcohol use. Risk factors for myocardial disease are often included in risk factor stratification scores, such as the Framingham Risk Score. At any given age, men are more at risk than women for the development of cardiovascular disease. High levels of blood cholesterol is a known risk factor, particularly high low-density lipoprotein, low high-density lipoprotein
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins. Lipoproteins are complex particles composed of multiple proteins which transport all fat molecules ( lipids) around the body within the water outside cells. They are ...
, and high triglycerides.
Many risk factors for myocardial infarction are potentially modifiable, with the most important being tobacco smoking (including secondhand smoke). Smoking appears to be the cause of about 36% and obesity the cause of 20% of coronary artery disease. Lack of physical activity has been linked to 7–12% of cases. Less common causes include stress-related causes such as job stress
Occupational stress is psychological stress related to one's job. Occupational stress refers to a chronic condition. Occupational stress can be managed by understanding what the stressful conditions at work are and taking steps to remediate thos ...
, which accounts for about 3% of cases, and chronic high stress levels.
Diet
There is varying evidence about the importance ofsaturated fat
A saturated fat is a type of fat in which the fatty acid chains have all single bonds. A fat known as a glyceride is made of two kinds of smaller molecules: a short glycerol backbone and fatty acids that each contain a long linear or branched c ...
in the development of myocardial infarctions. Eating polyunsaturated fat instead of saturated fat
A saturated fat is a type of fat in which the fatty acid chains have all single bonds. A fat known as a glyceride is made of two kinds of smaller molecules: a short glycerol backbone and fatty acids that each contain a long linear or branched c ...
s has been shown in studies to be associated with a decreased risk of myocardial infarction, while other studies find little evidence that reducing dietary saturated fat or increasing polyunsaturated fat
Polyunsaturated fats are fats in which the constituent hydrocarbon chain possesses two or more carbon–carbon double bonds. Polyunsaturated fat can be found mostly in nuts, seeds, fish, seed oils, and oysters. "Unsaturated" refers to the fact tha ...
intake affects heart attack risk. Dietary cholesterol does not appear to have a significant effect on blood cholesterol and thus recommendations about its consumption may not be needed. Trans fats do appear to increase risk. Acute and prolonged intake of high quantities of alcoholic drinks (3–4 or more daily) increases the risk of a heart attack.
Genetics
Family history ofischemic heart disease
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic pla ...
or MI, particularly if one has a male first-degree relative (father, brother) who had a myocardial infarction before age 55 years, or a female first-degree relative (mother, sister) less than age 65 increases a person's risk of MI.
Genome-wide association studies have found 27 genetic variants that are associated with an increased risk of myocardial infarction. The strongest association of MI has been found with chromosome 9 on the short arm ''p'' at locus 21, which contains genes CDKN2A and 2B, although the single nucleotide polymorphisms
In genetics, a single-nucleotide polymorphism (SNP ; plural SNPs ) is a germline substitution of a single nucleotide at a specific position in the genome. Although certain definitions require the substitution to be present in a sufficiently larg ...
that are implicated are within a non-coding region. The majority of these variants are in regions that have not been previously implicated in coronary artery disease. The following genes have an association with MI: PCSK9, SORT1, MIA3, WDR12, MRAS, PHACTR1, LPA, TCF21, MTHFDSL, ZC3HC1, CDKN2A, 2B, ABO, PDGF0, APOA5, MNF1ASM283, COL4A1, HHIPC1, SMAD3, ADAMTS7, RAS1, SMG6, SNF8, LDLR
The low-density lipoprotein receptor (LDL-R) is a mosaic protein of 839 amino acids (after removal of 21-amino acid signal peptide) that mediates the endocytosis of cholesterol-rich low-density lipoprotein (LDL). It is a cell-surface receptor th ...
, SLC5A3, MRPS6, KCNE2.
Other
The risk of having a myocardial infarction increases with older age, low physical activity, and lowsocioeconomic status
Socioeconomic status (SES) is an economic and sociological combined total measure of a person's work experience and of an individual's or family's economic access to resources and social position in relation to others. When analyzing a family's ...
. Heart attacks appear to occur more commonly in the morning hours, especially between 6AM and noon. Evidence suggests that heart attacks are at least three times more likely to occur in the morning than in the late evening. Shift work is also associated with a higher risk of MI. And one analysis has found an increase in heart attacks immediately following the start of daylight saving time
Daylight saving time (DST), also referred to as daylight savings time or simply daylight time (United States, Canada, and Australia), and summer time (United Kingdom, European Union, and others), is the practice of advancing clocks (typical ...
.
Women who use combined oral contraceptive pills have a modestly increased risk of myocardial infarction, especially in the presence of other risk factors. The use of non-steroidal anti inflammatory drugs
Non-steroidal anti-inflammatory drugs (NSAID) are members of a Indication (medicine), therapeutic drug class which Analgesic, reduces pain, Anti-inflammatory, decreases inflammation, Antipyretic, decreases fever, and Antithrombotic, prevents blo ...
(NSAIDs), even for as short as a week, increases risk.
Endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, f ...
in women under the age of 40 is an identified risk factor.
Air pollution is also an important modifiable risk. Short-term exposure to air pollution such as carbon monoxide
Carbon monoxide ( chemical formula CO) is a colorless, poisonous, odorless, tasteless, flammable gas that is slightly less dense than air. Carbon monoxide consists of one carbon atom and one oxygen atom connected by a triple bond. It is the si ...
, nitrogen dioxide, and sulfur dioxide
Sulfur dioxide (IUPAC-recommended spelling) or sulphur dioxide (traditional Commonwealth English) is the chemical compound with the formula . It is a toxic gas responsible for the odor of burnt matches. It is released naturally by volcanic activ ...
(but not ozone) have been associated with MI and other acute cardiovascular events. For sudden cardiac deaths, every increment of 30 units in Pollutant Standards Index correlated with an 8% increased risk of out-of-hospital cardiac arrest on the day of exposure. Extremes of temperature are also associated.
A number of acute and chronic infections including '' Chlamydophila pneumoniae'', influenza
Influenza, commonly known as "the flu", is an infectious disease caused by influenza viruses. Symptoms range from mild to severe and often include fever, runny nose, sore throat, muscle pain, headache, coughing, and fatigue. These symptoms ...
, '' Helicobacter pylori'', and '' Porphyromonas gingivalis'' among others have been linked to atherosclerosis and myocardial infarction. As of 2013, there is no evidence of benefit from antibiotics or vaccination, however, calling the association into question. Myocardial infarction can also occur as a late consequence of Kawasaki disease.
Calcium deposits in the coronary arteries can be detected with CT scan
A computed tomography scan (CT scan; formerly called computed axial tomography scan or CAT scan) is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers ...
s. Calcium seen in coronary arteries can provide predictive information beyond that of classical risk factors. High blood levels of the amino acid homocysteine is associated with premature atherosclerosis; whether elevated homocysteine in the normal range is causal is controversial.
In people without evident coronary artery disease, possible causes for the myocardial infarction are coronary spasm or coronary artery dissection.
Mechanism
Atherosclerosis
The most common cause of a myocardial infarction is the rupture of an atherosclerotic plaque on an artery supplying heart muscle. Plaques can become unstable, rupture, and additionally promote the formation of a blood clot that blocks the artery; this can occur in minutes. Blockage of an artery can lead to tissue death in tissue being supplied by that artery. Atherosclerotic plaques are often present for decades before they result in symptoms. The gradual buildup of cholesterol and fibrous tissue in plaques in the wall of the coronary arteries or other arteries, typically over decades, is termedatherosclerosis
Atherosclerosis is a pattern of the disease arteriosclerosis in which the wall of the artery develops abnormalities, called lesions. These lesions may lead to narrowing due to the buildup of atheromatous plaque. At onset there are usually ...
. Atherosclerosis is characterized by progressive inflammation of the walls of the arteries. Inflammatory cells, particularly macrophage
Macrophages (abbreviated as M φ, MΦ or MP) ( el, large eaters, from Greek ''μακρός'' (') = large, ''φαγεῖν'' (') = to eat) are a type of white blood cell of the immune system that engulfs and digests pathogens, such as cancer ce ...
s, move into affected arterial walls. Over time, they become laden with cholesterol products, particularly LDL, and become foam cells. A cholesterol core forms as foam cells die. In response to growth factors secreted by macrophages, smooth muscle
Smooth muscle is an involuntary non-striated muscle, so-called because it has no sarcomeres and therefore no striations (''bands'' or ''stripes''). It is divided into two subgroups, single-unit and multiunit smooth muscle. Within single-unit mus ...
and other cells move into the plaque and act to stabilize it. A stable plaque may have a thick fibrous cap with calcification. If there is ongoing inflammation, the cap may be thin or ulcerate. Exposed to the pressure associated with blood flow, plaques, especially those with a thin lining, may rupture and trigger the formation of a blood clot (thrombus). The cholesterol crystals have been associated with plaque rupture through mechanical injury and inflammation.
Other causes
Atherosclerotic disease is not the only cause of myocardial infarction, but it may exacerbate or contribute to other causes. A myocardial infarction may result from a heart with a limited blood supply subject to increased oxygen demands, such as in fever, a fast heart rate, hyperthyroidism, too few red blood cells in the bloodstream, or low blood pressure. Damage or failure of procedures such aspercutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
or coronary artery bypass grafts may cause a myocardial infarction. Spasm of coronary arteries, such as Prinzmetal's angina may cause blockage.
Tissue death
 If impaired blood flow to the heart lasts long enough, it triggers a process called the ischemic cascade; the heart cells in the territory of the blocked coronary artery die ( infarction), chiefly through
If impaired blood flow to the heart lasts long enough, it triggers a process called the ischemic cascade; the heart cells in the territory of the blocked coronary artery die ( infarction), chiefly through necrosis
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated dige ...
, and do not grow back. A collagen scar forms in their place. When an artery is blocked, cells lack oxygen, needed to produce ATP
ATP may refer to:
Companies and organizations
* Association of Tennis Professionals, men's professional tennis governing body
* American Technical Publishers, employee-owned publishing company
* ', a Danish pension
* Armenia Tree Project, non ...
in mitochondria
A mitochondrion (; ) is an organelle found in the Cell (biology), cells of most Eukaryotes, such as animals, plants and Fungus, fungi. Mitochondria have a double lipid bilayer, membrane structure and use aerobic respiration to generate adenosi ...
. ATP is required for the maintenance of electrolyte balance, particularly through the Na/K ATPase. This leads to an ischemic cascade of intracellular changes, necrosis and apoptosis of affected cells.
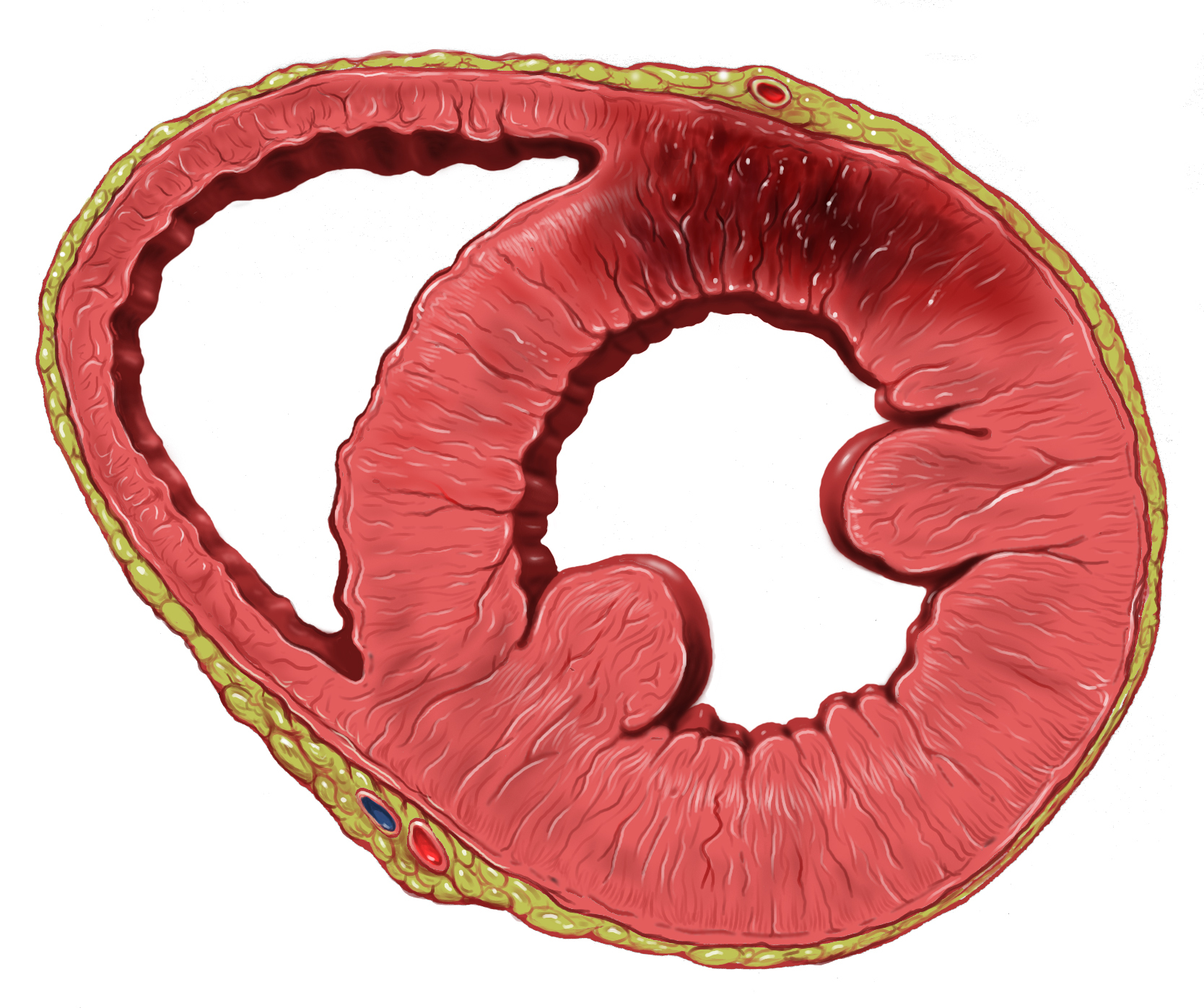
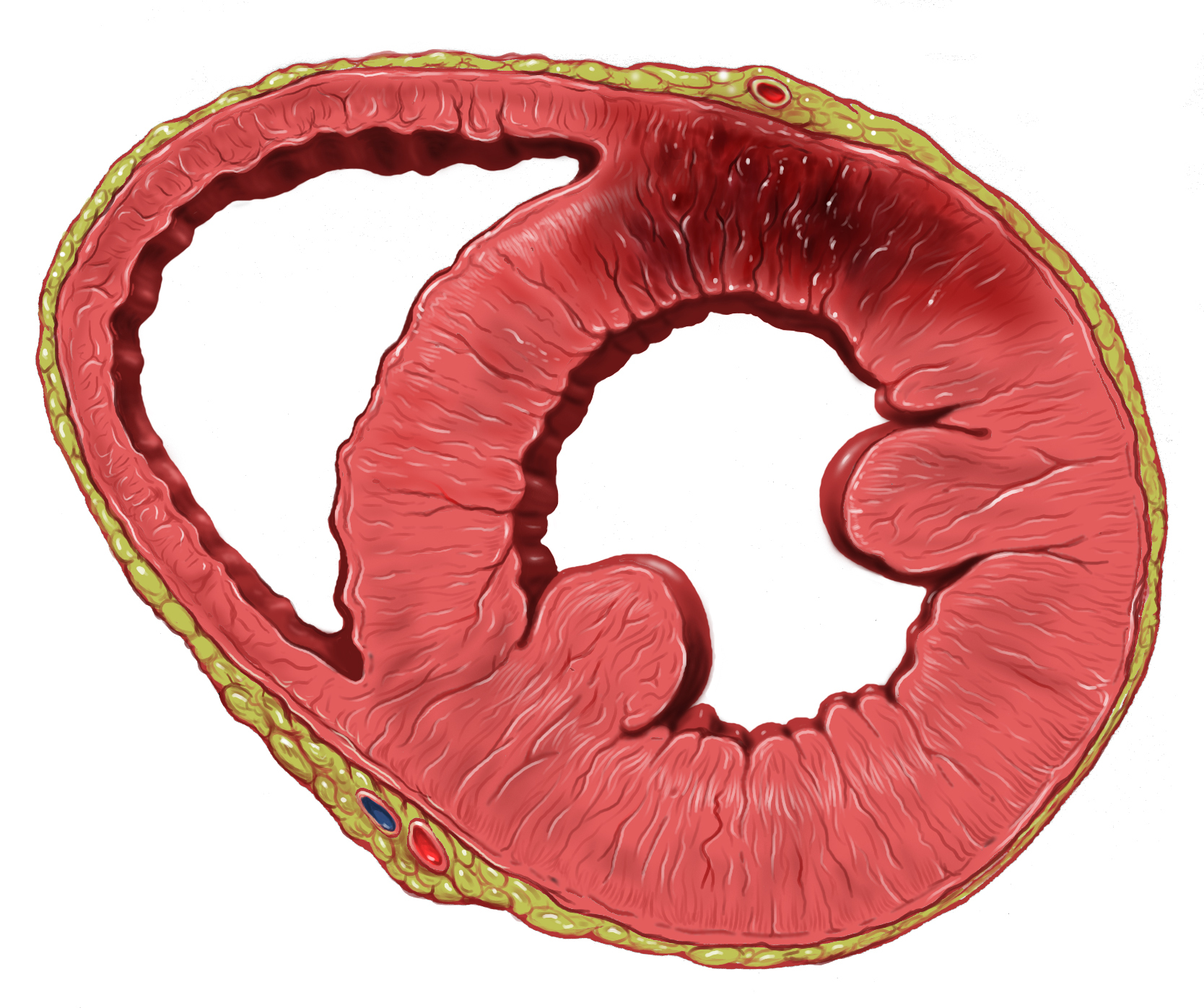
Cells in the area with the worst blood supply, just below the inner surface of the heart ( endocardium), are most susceptible to damage. Ischemia first affects this region, the ''subendocardial'' region, and tissue begins to die within 15–30 minutes of loss of blood supply. The dead tissue is surrounded by a zone of potentially reversible ischemia that progresses to become a full-thickness ''transmural'' infarct. The initial "wave" of infarction can take place over 3–4 hours. These changes are seen on gross pathology and cannot be predicted by the presence or absence of Q waves on an ECG. The position, size and extent of an infarct depends on the affected artery, totality of the blockage, duration of the blockage, the presence of collateral blood vessels, oxygen demand, and success of interventional procedures.
Tissue death and myocardial scarring alter the normal conduction pathways of the heart, and weaken affected areas. The size and location puts a person at risk of abnormal heart rhythms (arrhythmias) or heart block, aneurysm of the heart ventricles, inflammation of the heart wall following infarction, and rupture of the heart wall that can have catastrophic consequences.
Injury to the myocardium also occurs during re-perfusion. This might manifest as ventricular arrhythmia. The re-perfusion injury is a consequence of the calcium and sodium uptake from the cardiac cells and the release of oxygen radicals during reperfusion. No-reflow phenomenon—when blood is still unable to be distributed to the affected myocardium despite clearing the occlusion—also contributes to myocardial injury. Topical endothelial swelling is one of many factors contributing to this phenomenon.
Diagnosis

Criteria
A myocardial infarction, according to current consensus, is defined by elevated cardiac biomarkers with a rising or falling trend and at least one of the following: * Symptoms relating to ischemia * Changes on an electrocardiogram (ECG), such as ST segment changes, new left bundle branch block, or pathologic Q waves * Changes in the motion of the heart wall on imaging * Demonstration of a thrombus on angiogram or at autopsy.Types
A myocardial infarction is usually clinically classified as an ST-elevation MI (STEMI) or a non-ST elevation MI (NSTEMI). These are based on ST elevation, a portion of a heartbeat graphically recorded on an ECG. STEMIs make up about 25–40% of myocardial infarctions. A more explicit classification system, based on international consensus in 2012, also exists. This classifies myocardial infarctions into five types: # Spontaneous MI related to plaque erosion and/or rupture fissuring, or dissection # MI related to ischemia, such as from increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anemia, arrhythmias, high blood pressure, or low blood pressure # Sudden unexpected cardiac death, including cardiac arrest, where symptoms may suggest MI, an ECG may be taken with suggestive changes, or a blood clot is found in a coronary artery by angiography and/or at autopsy, but where blood samples could not be obtained, or at a time before the appearance of cardiac biomarkers in the blood # Associated with coronary angioplasty or stents #* Associated withpercutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(PCI)
#* Associated with stent thrombosis as documented by angiography or at autopsy
# Associated with CABG
Coronary artery bypass surgery, also known as coronary artery bypass graft (CABG, pronounced "cabbage") is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve Angina pe ...
# Associated with spontaneous coronary artery dissection in young, fit women
Cardiac biomarkers
There are many differentbiomarker
In biomedical contexts, a biomarker, or biological marker, is a measurable indicator of some biological state or condition. Biomarkers are often measured and evaluated using blood, urine, or soft tissues to examine normal biological processes, p ...
s used to determine the presence of cardiac muscle damage. Troponins, measured through a blood test, are considered to be the best, and are preferred because they have greater sensitivity and specificity for measuring injury to the heart muscle than other tests. A rise in troponin occurs within 2–3 hours of injury to the heart muscle, and peaks within 1–2 days. The level of the troponin, as well as a change over time, are useful in measuring and diagnosing or excluding myocardial infarctions, and the diagnostic accuracy of troponin testing is improving over time. One high-sensitivity cardiac troponin can rule out a heart attack as long as the ECG is normal.
Other tests, such as CK-MB or myoglobin
Myoglobin (symbol Mb or MB) is an iron- and oxygen-binding protein found in the cardiac and skeletal muscle tissue of vertebrates in general and in almost all mammals. Myoglobin is distantly related to hemoglobin. Compared to hemoglobin, myoglobi ...
, are discouraged. CK-MB is not as specific as troponins for acute myocardial injury, and may be elevated with past cardiac surgery, inflammation or electrical cardioversion; it rises within 4–8 hours and returns to normal within 2–3 days. Copeptin may be useful to rule out MI rapidly when used along with troponin.
Electrocardiogram
 Electrocardiograms (ECGs) are a series of leads placed on a person's chest that measure electrical activity associated with contraction of the heart muscle. The taking of an ECG is an important part of the workup of an AMI, and ECGs are often not just taken once but may be repeated over minutes to hours, or in response to changes in signs or symptoms.
ECG readouts product a waveform with different labelled features. In addition to a rise in biomarkers, a rise in the ST segment, changes in the shape or flipping of T waves, new Q waves, or a new left bundle branch block can be used to diagnose an AMI. In addition, ST elevation can be used to diagnose an ST segment myocardial infarction (STEMI). A rise must be new in V2 and V3 ≥2 mm (0,2 mV) for males or ≥1.5 mm (0.15 mV) for females or ≥1 mm (0.1 mV) in two other adjacent chest or limb leads. ST elevation is associated with infarction, and may be preceded by changes indicating ischemia, such as ST depression or inversion of the T waves. Abnormalities can help differentiate the location of an infarct, based on the leads that are affected by changes. Early STEMIs may be preceded by peaked T waves. Other ECG abnormalities relating to complications of acute myocardial infarctions may also be evident, such as atrial or ventricular fibrillation.
Electrocardiograms (ECGs) are a series of leads placed on a person's chest that measure electrical activity associated with contraction of the heart muscle. The taking of an ECG is an important part of the workup of an AMI, and ECGs are often not just taken once but may be repeated over minutes to hours, or in response to changes in signs or symptoms.
ECG readouts product a waveform with different labelled features. In addition to a rise in biomarkers, a rise in the ST segment, changes in the shape or flipping of T waves, new Q waves, or a new left bundle branch block can be used to diagnose an AMI. In addition, ST elevation can be used to diagnose an ST segment myocardial infarction (STEMI). A rise must be new in V2 and V3 ≥2 mm (0,2 mV) for males or ≥1.5 mm (0.15 mV) for females or ≥1 mm (0.1 mV) in two other adjacent chest or limb leads. ST elevation is associated with infarction, and may be preceded by changes indicating ischemia, such as ST depression or inversion of the T waves. Abnormalities can help differentiate the location of an infarct, based on the leads that are affected by changes. Early STEMIs may be preceded by peaked T waves. Other ECG abnormalities relating to complications of acute myocardial infarctions may also be evident, such as atrial or ventricular fibrillation.

Imaging
Noninvasive imaging plays an important role in the diagnosis and characterisation of myocardial infarction. Tests such as chest X-rays can be used to explore and exclude alternate causes of a person's symptoms.Echocardiography
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart.
It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Echocardiography has become routinely used in t ...
may assist in modifying clinical suspicion of ongoing myocardial infarction in patients that can't be ruled out or ruled in following initial ECG and Troponin testing. Myocardial perfusion imaging has no role in the acute diagnostic algorithm, however it can confirm a clinical suspicion of Chronic Coronary Syndrome when the patient's history, physical examination (including cardiac examination) ECG, and cardiac biomarkers suggest coronary artery disease.
Echocardiography
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart.
It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Echocardiography has become routinely used in t ...
, an ultrasound scan of the heart, is able to visualize the heart, its size, shape, and any abnormal motion of the heart walls as they beat that may indicate a myocardial infarction. The flow of blood can be imaged, and contrast dyes may be given to improve image. Other scans using radioactive contrast include SPECT CT-scans
A computed tomography scan (CT scan; formerly called computed axial tomography scan or CAT scan) is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers ...
using thallium, sestamibi
Technetium (99mTc) sestamibi (INN) (commonly sestamibi; USP: technetium Tc 99m sestamibi; trade name Cardiolite) is a pharmaceutical agent used in nuclear medicine imaging. The drug is a coordination complex consisting of the radioisotope techn ...
(MIBI scan
Technetium (99mTc) sestamibi (INN) (commonly sestamibi; USP: technetium Tc 99m sestamibi; trade name Cardiolite) is a pharmaceutical agent used in nuclear medicine imaging. The drug is a coordination complex consisting of the radioisotope techn ...
s) or tetrofosmin
Technetium (99mTc) tetrofosmin is a drug used in nuclear medicine cardiac imaging. It is sold under the brand name Myoview (GE Healthcare). The radioisotope, technetium-99m, is chelated by two 1,2-''bis''i-(2-ethoxyethyl)phosphinothane ligands whi ...
; or a PET scan using Fludeoxyglucose or rubidium-82. These nuclear medicine scans can visualize the perfusion of heart muscle. SPECT may also be used to determine viability of tissue, and whether areas of ischemia are inducible.
Medical societies and professional guidelines recommend that the physician confirm a person is at high risk for Chronic Coronary Syndrome before conducting diagnostic non-invasive imaging tests to make a diagnosis, as such tests are unlikely to change management and result in increased costs. Patients who have a normal ECG and who are able to exercise, for example, most likely do not merit routine imaging.
Differential diagnosis
There are many causes of chest pain, which can originate from the heart,lung
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either sid ...
s, gastrointestinal tract
The gastrointestinal tract (GI tract, digestive tract, alimentary canal) is the tract or passageway of the digestive system that leads from the mouth to the anus. The GI tract contains all the major organ (biology), organs of the digestive syste ...
, aorta, and other muscles, bones and nerves surrounding the chest. In addition to myocardial infarction, other causes include angina, insufficient blood supply (ischemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems wi ...
) to the heart muscles without evidence of cell death, gastroesophageal reflux disease; pulmonary embolism, tumors of the lungs, pneumonia, rib fracture, costochondritis, heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, a ...
and other musculoskeletal injuries. Rarer severe differential diagnoses include aortic dissection, esophageal rupture, tension pneumothorax, and pericardial effusion causing cardiac tamponade. The chest pain in an MI may mimic heartburn. Causes of sudden-onset breathlessness generally involve the lungs or heart – including pulmonary edema, pneumonia, allergic reactions and asthma, and pulmonary embolus, acute respiratory distress syndrome and metabolic acidosis
Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys ...
. There are many different causes of fatigue, and myocardial infarction is not a common cause.
Prevention
There is a large crossover between the lifestyle and activity recommendations to prevent a myocardial infarction, and those that may be adopted as secondary prevention after an initial myocardial infarction, because of shared risk factors and an aim to reduce atherosclerosis affecting heart vessels. Theinfluenza vaccine
Influenza vaccines, also known as flu shots, are vaccines that protect against infection by influenza viruses. New versions of the vaccines are developed twice a year, as the influenza virus rapidly changes. While their effectiveness varies fr ...
also appear to protect against myocardial infarction with a benefit of 15 to 45%.
Primary prevention
Lifestyle
Physical activity can reduce the risk of cardiovascular disease, and people at risk are advised to engage in 150 minutes of moderate or 75 minutes of vigorous-intensity aerobic exercise a week. Keeping a healthy weight, drinking alcohol within the recommended limits, and quitting smoking reduce the risk of cardiovascular disease. Substitutingunsaturated fat
An unsaturated fat is a fat or fatty acid in which there is at least one double bond within the fatty acid chain. A fatty acid chain is monounsaturated if it contains one double bond, and polyunsaturated if it contains more than one double b ...
s such as olive oil
Olive oil is a liquid fat obtained from olives (the fruit of ''Olea europaea''; family Oleaceae), a traditional tree crop of the Mediterranean Basin, produced by pressing whole olives and extracting the oil. It is commonly used in cooking: f ...
and rapeseed oil
Close-up of canola blooms
Canola flower
Rapeseed oil is one of the oldest known vegetable oils. There are both edible and industrial forms produced from rapeseed, the seed of several cultivars of the plant family Brassicaceae. Historically, i ...
instead of saturated fats may reduce the risk of myocardial infarction, although there is not universal agreement. Dietary modifications are recommended by some national authorities, with recommendations including increasing the intake of wholegrain starch, reducing sugar intake (particularly of refined sugar), consuming five portions of fruit and vegetables daily, consuming two or more portions of fish per week, and consuming 4–5 portions of unsalted nuts
Nut often refers to:
* Nut (fruit), fruit composed of a hard shell and a seed, or a collective noun for dry and edible fruits or seeds
* Nut (hardware), fastener used with a bolt
Nut or Nuts may also refer to:
Arts, entertainment, and media Com ...
, seeds, or legume
A legume () is a plant in the family Fabaceae (or Leguminosae), or the fruit or seed of such a plant. When used as a dry grain, the seed is also called a pulse. Legumes are grown agriculturally, primarily for human consumption, for livestock f ...
s per week. The dietary pattern with the greatest support is the Mediterranean diet. Vitamins and mineral supplements are of no proven benefit, and neither are plant stanols or sterols
Sterol is an organic compound with formula , whose molecule is derived from that of gonane by replacement of a hydrogen atom in position 3 by a hydroxyl group. It is therefore an alcohol of gonane. More generally, any compounds that contain the gon ...
.
Public health measures may also act at a population level to reduce the risk of myocardial infarction, for example by reducing unhealthy diets (excessive salt, saturated fat, and trans fat) including food labeling and marketing requirements as well as requirements for catering and restaurants, and stimulating physical activity. This may be part of regional cardiovascular disease prevention programs or through the health impact assessment of regional and local plans and policies.
Most guidelines recommend combining different preventive strategies. A 2015 Cochrane Review found some evidence that such an approach might help with blood pressure, body mass index and waist circumference. However, there was insufficient evidence to show an effect on mortality or actual cardio-vascular events.
Medication
Statins, drugs that act to lower blood cholesterol, decrease the incidence and mortality rates of myocardial infarctions. They are often recommended in those at an elevated risk of cardiovascular diseases. Aspirin has been studied extensively in people considered at increased risk of myocardial infarction. Based on numerous studies in different groups (e.g. people with or without diabetes), there does not appear to be a benefit strong enough to outweigh the risk of excessive bleeding. Nevertheless, many clinical practice guidelines continue to recommend aspirin for primary prevention, and some researchers feel that those with very high cardiovascular risk but low risk of bleeding should continue to receive aspirin.Secondary prevention
There is a large crossover between the lifestyle and activity recommendations to prevent a myocardial infarction, and those that may be adopted as secondary prevention after an initial myocardial infarct. Recommendations include stopping smoking, a gradual return to exercise, eating a healthy diet, low insaturated fat
A saturated fat is a type of fat in which the fatty acid chains have all single bonds. A fat known as a glyceride is made of two kinds of smaller molecules: a short glycerol backbone and fatty acids that each contain a long linear or branched c ...
and low in cholesterol, drinking alcohol within recommended limits, exercising, and trying to achieve a healthy weight. Exercise is both safe and effective even if people have had stents or heart failure, and is recommended to start gradually after 1–2 weeks. Counselling should be provided relating to medications used, and for warning signs of depression. Previous studies suggested a benefit from omega-3 fatty acid supplementation but this has not been confirmed.
Medications
Following a heart attack, nitrates, when taken for two days, and ACE-inhibitors decrease the risk of death. Other medications include: Aspirin is continued indefinitely, as well as another antiplatelet agent such as clopidogrel or ticagrelor ("dual antiplatelet therapy" or DAPT) for up to twelve months. If someone has another medical condition that requires anticoagulation (e.g. with warfarin) this may need to be adjusted based on risk of further cardiac events as well as bleeding risk. In those who have had a stent, more than 12 months of clopidogrel plus aspirin does not affect the risk of death.Beta blocker
Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms, and to protect the heart from a second heart attack after a first heart attack ( secondary prevention). They are ...
therapy such as metoprolol or carvedilol is recommended to be started within 24 hours, provided there is no acute heart failure or heart block. The dose should be increased to the highest tolerated. Contrary to what was long believed, the use of beta blockers does not appear to affect the risk of death, possibly because other treatments for MI have improved. When beta blocker medication is given within the first 24–72 hours of a STEMI no lives are saved. However, 1 in 200 people were prevented from a repeat heart attack, and another 1 in 200 from having an abnormal heart rhythm. Additionally, for 1 in 91 the medication causes a temporary decrease in the heart's ability to pump blood.
ACE inhibitor therapy should be started within 24 hours, and continued indefinitely at the highest tolerated dose. This is provided there is no evidence of worsening kidney failure, high potassium, low blood pressure, or known narrowing of the renal arteries
The renal arteries are paired arteries that supply the kidneys with blood. Each is directed across the crus of the diaphragm, so as to form nearly a right angle.
The renal arteries carry a large portion of total blood flow to the kidneys. Up t ...
. Those who cannot tolerate ACE inhibitors may be treated with an angiotensin II receptor antagonist.
Statin therapy has been shown to reduce mortality and subsequent cardiac events and should be commenced to lower LDL cholesterol. Other medications, such as ezetimibe, may also be added with this goal in mind.
Aldosterone antagonists ( spironolactone or eplerenone) may be used if there is evidence of left ventricular dysfunction after an MI, ideally after beginning treatment with an ACE inhibitor.
Other
A defibrillator, an electric device connected to the heart and surgically inserted under the skin, may be recommended. This is particularly if there are any ongoing signs of heart failure, with a lowleft ventricular ejection fraction
An ejection fraction (EF) is the volumetric fraction (or portion of the total) of fluid (usually blood) ejected from a chamber (usually the heart) with each contraction (or heartbeat). It can refer to the cardiac atrium, ventricle, gall bladder, o ...
and a New York Heart Association grade II or III after 40 days of the infarction. Defibrillators detect potentially fatal arrhythmia and deliver an electrical shock to the person to depolarize a critical mass of the heart muscle.
Management
A myocardial infarction requires immediate medical attention. Treatment aims to preserve as much heart muscle as possible, and to prevent further complications. Treatment depends on whether the myocardial infarction is a STEMI or NSTEMI. Treatment in general aims to unblock blood vessels, reduce blood clot enlargement, reduce ischemia, and modify risk factors with the aim of preventing future MIs. In addition, the main treatment for myocardial infarctions with ECG evidence of ST elevation (STEMI) include thrombolysis orpercutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
, although PCI is also ideally conducted within 1–3 days for NSTEMI. In addition to clinical judgement, risk stratification may be used to guide treatment, such as with the TIMI
The Thrombolysis In Myocardial Infarction, or TIMI Study Group, is an Academic Research Organization (ARO) affiliated with Brigham and Women's Hospital and Harvard Medical School dedicated to advancing the knowledge and care of patients with c ...
and GRACE scoring systems.
Pain
The pain associated with myocardial infarction is often treated withnitroglycerin
Nitroglycerin (NG), (alternative spelling of nitroglycerine) also known as trinitroglycerin (TNG), nitro, glyceryl trinitrate (GTN), or 1,2,3-trinitroxypropane, is a dense, colorless, oily, explosive liquid most commonly produced by nitrating g ...
, a vasodilator
Vasodilation is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. The process is the opposite of vasoconstriction, ...
, or opioid medications such as morphine. Nitroglycerin (given under the tongue or injected into a vein) may improve blood supply to the heart. It is an important part of therapy for its pain relief effects, though there is no proven benefit to mortality
Mortality is the state of being mortal, or susceptible to death; the opposite of immortality.
Mortality may also refer to:
* Fish mortality, a parameter used in fisheries population dynamics to account for the loss of fish in a fish stock throug ...
. Morphine or other opioid medications may also be used, and are effective for the pain associated with STEMI. There is poor evidence that morphine shows any benefit to overall outcomes, and there is some evidence of potential harm.
Antithrombotics
Aspirin, an antiplatelet drug, is given as aloading dose
In pharmacokinetics, a loading dose is an initial higher dose of a drug that may be given at the beginning of a course of treatment before dropping down to a lower maintenance dose.
A loading dose is most useful for drugs that are eliminated from ...
to reduce the clot size and reduce further clotting in the affected artery. It is known to decrease mortality associated with acute myocardial infarction by at least 50%. P2Y12 inhibitors
P2Y12 is a chemoreceptor for adenosine diphosphate (ADP) that belongs to the Gi class of a group of G protein-coupled (GPCR) purinergic receptors. This P2Y receptor family has several receptor subtypes with different pharmacological select ...
such as clopidogrel, prasugrel and ticagrelor are given concurrently, also as a loading dose
In pharmacokinetics, a loading dose is an initial higher dose of a drug that may be given at the beginning of a course of treatment before dropping down to a lower maintenance dose.
A loading dose is most useful for drugs that are eliminated from ...
, with the dose depending on whether further surgical management or fibrinolysis is planned. Prasugrel and ticagrelor are recommended in European and American guidelines, as they are active more quickly and consistently than clopidogrel. P2Y12 inhibitors are recommended in both NSTEMI and STEMI, including in PCI, with evidence also to suggest improved mortality. Heparin
Heparin, also known as unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. Since heparins depend on the activity of antithrombin, they are considered anticoagulants. Specifically it is also used in the treatm ...
s, particularly in the unfractionated form, act at several points in the clotting cascade, help to prevent the enlargement of a clot, and are also given in myocardial infarction, owing to evidence suggesting improved mortality rates. In very high-risk scenarios, inhibitors of the platelet glycoprotein αIIbβ3a receptor such as eptifibatide or tirofiban may be used.
There is varying evidence on the mortality benefits in NSTEMI. A 2014 review of P2Y12 inhibitors such as clopidogrel found they do not change the risk of death when given to people with a suspected NSTEMI prior to PCI, nor do heparins change the risk of death. They do decrease the risk of having a further myocardial infarction.
Angiogram
Primarypercutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(PCI) is the treatment of choice for STEMI if it can be performed in a timely manner, ideally within 90–120 minutes of contact with a medical provider. Some recommend it is also done in NSTEMI within 1–3 days, particularly when considered high-risk. A 2017 review, however, did not find a difference between early versus later PCI in NSTEMI.
PCI involves small probes, inserted through peripheral blood vessels such as the femoral artery or radial artery into the blood vessels of the heart. The probes are then used to identify and clear blockages using small balloons, which are dragged through the blocked segment, dragging away the clot, or the insertion of stents. Coronary artery bypass grafting is only considered when the affected area of heart muscle is large, and PCI is unsuitable, for example with difficult cardiac anatomy. After PCI, people are generally placed on aspirin indefinitely and on dual antiplatelet therapy (generally aspirin and clopidogrel) for at least a year.
Fibrinolysis
If PCI cannot be performed within 90 to 120 minutes in STEMI then fibrinolysis, preferably within 30 minutes of arrival to hospital, is recommended. If a person has had symptoms for 12 to 24 hours evidence for effectiveness of thrombolysis is less and if they have had symptoms for more than 24 hours it is not recommended. Thrombolysis involves the administration of medication that activates the enzymes that normally dissolve blood clots. These medications include tissue plasminogen activator, reteplase, streptokinase, and tenecteplase. Thrombolysis is not recommended in a number of situations, particularly when associated with a high risk of bleeding or the potential for problematic bleeding, such as active bleeding, paststroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
s or bleeds into the brain, or severe hypertension
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. Long-term high bl ...
. Situations in which thrombolysis may be considered, but with caution, include recent surgery, use of anticoagulants, pregnancy, and proclivity to bleeding. Major risks of thrombolysis are major bleeding and intracranial bleeding. Pre-hospital thrombolysis reduces time to thrombolytic treatment, based on studies conducted in higher income countries, however it is unclear whether this has an impact on mortality rates.
Other
In the past, high flow oxygen was recommended for everyone with a possible myocardial infarction. More recently, no evidence was found for routine use in those with normal oxygen levels and there is potential harm from the intervention. Therefore, oxygen is currently only recommended if oxygen levels are found to be low or if someone is in respiratory distress. If despite thrombolysis there is significant cardiogenic shock, continued severe chest pain, or less than a 50% improvement in ST elevation on the ECG recording after 90 minutes, then rescue PCI is indicated emergently. Those who have had cardiac arrest may benefit from targeted temperature management with evaluation for implementation of hypothermia protocols. Furthermore, those with cardiac arrest, and ST elevation at any time, should usually have angiography. Aldosterone antagonists appear to be useful in people who have had an STEMI and do not have heart failure.Rehabilitation and exercise
Cardiac rehabilitation benefits many who have experienced myocardial infarction, even if there has been substantial heart damage and resultant left ventricular failure. It should start soon after discharge from the hospital. The program may include lifestyle advice, exercise, social support, as well as recommendations about driving, flying, sports participation, stress management, and sexual intercourse. Returning to sexual activity after myocardial infarction is a major concern for most patients, and is an important area to be discussed in the provision of holistic care. In the short-term, exercise-based cardiovascular rehabilitation programs may reduce the risk of a myocardial infarction, reduces a large number of hospitalizations from all causes, reduces hospital costs, improveshealth-related quality of life
In general, quality of life (QoL or QOL) is the perceived quality of an individual's daily life, that is, an assessment of their well-being or lack thereof. This includes all emotional, social and physical aspects of the individual's life. In heal ...
, and has a small effect on all-cause mortality. Longer-term studies indicate that exercise-based cardiovascular rehabilitation programs may reduce cardiovascular mortality and myocardial infarction.
Prognosis
The prognosis after myocardial infarction varies greatly depending on the extent and location of the affected heart muscle, and the development and management of complications. Prognosis is worse with older age and social isolation. Anterior infarcts, persistent ventricular tachycardia or fibrillation, development of heart blocks, and left ventricular impairment are all associated with poorer prognosis. Without treatment, about a quarter of those affected by MI die within minutes and about forty percent within the first month. Morbidity and mortality from myocardial infarction has however improved over the years due to earlier and better treatment: in those who have a STEMI in the United States, between 5 and 6 percent die before leaving the hospital and 7 to 18 percent die within a year. It is unusual for babies to experience a myocardial infarction, but when they do, about half die. In the short-term, neonatal survivors seem to have a normal quality of life.Complications
Complications may occur immediately following the myocardial infarction or may take time to develop. Disturbances of heart rhythms, including atrial fibrillation, ventricular tachycardia and fibrillation and heart block can arise as a result of ischemia, cardiac scarring, and infarct location.Stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
is also a risk, either as a result of clots transmitted from the heart during PCI, as a result of bleeding following anticoagulation, or as a result of disturbances in the heart's ability to pump effectively as a result of the infarction. Regurgitation of blood through the mitral valve is possible, particularly if the infarction causes dysfunction of the papillary muscle. Cardiogenic shock as a result of the heart being unable to adequately pump blood may develop, dependent on infarct size, and is most likely to occur within the days following an acute myocardial infarction. Cardiogenic shock is the largest cause of in-hospital mortality. Rupture of the ventricular dividing wall or left ventricular wall may occur within the initial weeks. Dressler's syndrome, a reaction following larger infarcts and a cause of pericarditis
Pericarditis is inflammation of the pericardium, the fibrous sac surrounding the heart. Symptoms typically include sudden onset of sharp chest pain, which may also be felt in the shoulders, neck, or back. The pain is typically less severe when sit ...
is also possible.
Heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, a ...
may develop as a long-term consequence, with an impaired ability of heart muscle to pump, scarring, and an increase in the size of the existing muscle. Aneurysm of the left ventricle myocardium develops in about 10% of MI and is itself a risk factor for heart failure, ventricular arrhythmia, and the development of clots.
Risk factors for complications and death include age, hemodynamic parameters (such as heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, a ...
, cardiac arrest on admission, systolic
Systole ( ) is the part of the cardiac cycle during which some chambers of the heart contract after refilling with blood. The term originates, via New Latin, from Ancient Greek (''sustolē''), from (''sustéllein'' 'to contract'; from ''sun ...
blood pressure, or Killip class of two or greater), ST-segment deviation, diabetes, serum creatinine, peripheral vascular disease, and elevation of cardiac markers.
Epidemiology
Myocardial infarction is a common presentation of coronary artery disease. The World Health Organization estimated in 2004, that 12.2% of worldwide deaths were from ischemic heart disease; with it being the leading cause of death in high- or middle-income countries and second only to lower respiratory infections in lower-income countries. Worldwide, more than 3 million people have STEMIs and 4 million have NSTEMIs a year. STEMIs occur about twice as often in men as women. Rates of death from ischemic heart disease (IHD) have slowed or declined in most high-income countries, although cardiovascular disease still accounted for one in three of all deaths in the US in 2008. For example, rates of death from cardiovascular disease have decreased almost a third between 2001 and 2011 in the United States. In contrast, IHD is becoming a more common cause of death in the developing world. For example, inIndia
India, officially the Republic of India ( Hindi: ), is a country in South Asia. It is the seventh-largest country by area, the second-most populous country, and the most populous democracy in the world. Bounded by the Indian Ocean on the ...
, IHD had become the leading cause of death by 2004, accounting for 1.46 million deaths (14% of total deaths) and deaths due to IHD were expected to double during 1985–2015. Globally, disability adjusted life year
The disability-adjusted life year (DALY) is a measure of overall disease burden, expressed as the number of years lost due to ill-health, disability or early death. It was developed in the 1990s as a way of comparing the overall health and life ex ...
s (DALYs) lost to ischemic heart disease are predicted to account for 5.5% of total DALYs in 2030, making it the second-most-important cause of disability (after unipolar depressive disorder), as well as the leading cause of death by this date.
Social determinants of health
Social determinants such asneighborhood
A neighbourhood (British English, Irish English, Australian English and Canadian English) or neighborhood (American English; see spelling differences) is a geographically localised community within a larger city, town, suburb or rural area, ...
disadvantage, immigration
Immigration is the international movement of people to a destination country of which they are not natives or where they do not possess citizenship in order to settle as permanent residents or naturalized citizens. Commuters, tourists, a ...
status, lack of social support
Social support is the perception and actuality that one is cared for, has assistance available from other people, and most popularly, that one is part of a supportive social network. These supportive resources can be emotional (e.g., nurturance), ...
, social isolation, access to health services
Health care or healthcare is the improvement of health via the preventive healthcare, prevention, diagnosis, therapy, treatment, wiktionary:amelioration, amelioration or cure of disease, illness, injury, and other disability, physical and menta ...
play an important role in myocardial infarction risk and survival. Studies have shown that low socioeconomic status
Socioeconomic status (SES) is an economic and sociological combined total measure of a person's work experience and of an individual's or family's economic access to resources and social position in relation to others. When analyzing a family's ...
is associated with an increased risk of poorer survival. There are well-documented disparities in myocardial infarction survival by socioeconomic status
Socioeconomic status (SES) is an economic and sociological combined total measure of a person's work experience and of an individual's or family's economic access to resources and social position in relation to others. When analyzing a family's ...
, race, education, and census-tract-level poverty
Poverty is the state of having few material possessions or little income. Poverty can have diverse social, economic, and political causes and effects. When evaluating poverty in ...
.
Race: In the U.S. African Americans have a greater burden of myocardial infarction and other cardiovascular events. On a population level, there is a higher overall prevalence of risk factors that are unrecognized and therefore not treated, which places these individuals at a greater likelihood of experiencing adverse outcomes and therefore potentially higher morbidity and mortality
Mortality is the state of being mortal, or susceptible to death; the opposite of immortality.
Mortality may also refer to:
* Fish mortality, a parameter used in fisheries population dynamics to account for the loss of fish in a fish stock throug ...
.
Socioeconomic status: Among individuals who live in the low- socioeconomic (SES) areas, which is close to 25% of the US population, myocardial infarctions (MIs) occurred twice as often compared with people who lived in higher SES areas.
Immigration status: In 2018 many lawfully present immigrant
Immigration is the international movement of people to a destination country of which they are not natives or where they do not possess citizenship in order to settle as permanent residents or naturalized citizens. Commuters, tourists, and ...
s who are eligible for coverage remain uninsured because immigrant families face a range of enrollment barriers, including fear, confusion about eligibility policies, difficulty navigating the enrollment process, and language
Language is a structured system of communication. The structure of a language is its grammar and the free components are its vocabulary. Languages are the primary means by which humans communicate, and may be conveyed through a variety of ...
and literacy challenges. Uninsured undocumented immigrants are ineligible for coverage options due to their immigration status.
Health care access: Lack of health insurance
Health insurance or medical insurance (also known as medical aid in South Africa) is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among ...
and financial concerns about accessing care were associated with delays in seeking emergency care for acute myocardial infarction which can have significant, adverse consequences on patient outcomes.
Education: Researchers found that compared to people with graduate degrees, those with lower educational attainment appeared to have a higher risk of heart attack, dying from a cardiovascular event, and overall death.
Society and culture
Depictions of heart attacks in popular media often include collapsing or loss of consciousness which are not common symptoms; these depictions contribute to widespread misunderstanding about the symptoms of myocardial infarctions, which in turn contributes to people not getting care when they should.Legal implications
Atcommon law
In law, common law (also known as judicial precedent, judge-made law, or case law) is the body of law created by judges and similar quasi-judicial tribunals by virtue of being stated in written opinions."The common law is not a brooding omniprese ...
, in general, a myocardial infarction is a disease
A disease is a particular abnormal condition that negatively affects the structure or function of all or part of an organism, and that is not immediately due to any external injury. Diseases are often known to be medical conditions that a ...
, but may sometimes be an injury
An injury is any physiological damage to living tissue caused by immediate physical stress. An injury can occur intentionally or unintentionally and may be caused by blunt trauma, penetrating trauma, burning, toxic exposure, asphyxiation, o ...
. This can create coverage issues in the administration of no-fault insurance schemes such as workers' compensation. In general, a heart attack is not covered;Workers' Compensation FAQ.
Prairie View A&M University
Prairie View A&M University (PVAMU or PV) is a public historically black land-grant university in Prairie View, Texas. Founded in 1876, it is one of Texas's two land-grant universities and the second oldest public institution of higher learnin ...
. Retrieved November 22, 2006. however, it may be a work-related injury if it results, for example, from unusual emotional stress or unusual exertion.SIGNIFICANT DECISIONS Subject Index. Board of Industrial Insurance Appeals. Retrieved November 22, 2006. In addition, in some jurisdictions, heart attacks had by persons in particular occupations such as police officers may be classified as line-of-duty injuries by statute or policy. In some countries or states, a person having had an MI may be prevented from participating in activity that puts other people's lives at risk, for example driving a car or flying an airplane.
References
Sources
* * * * * * *Further reading
* *External links
*American Heart Association's Heart Attack web site
— Information and resources for preventing, recognizing, and treating a heart attack. * TIMI Score fo
UA/NSTEMI
an
STEMI
HEART Score for Major Cardiac Events
* {{Authority control Aging-associated diseases Causes of death Ischemic heart diseases Medical emergencies Articles containing video clips Wikipedia medicine articles ready to translate Acute pain Wikipedia emergency medicine articles ready to translate