|
Length Of Stay
Length of stay (LOS) is the duration of a single episode of hospitalization. patient, Inpatient days are calculated by subtracting day of admission from day of :wikt:discharge, discharge. Analysis A common statistic associated with length of stay is the average length of stay (ALOS), a mean calculated by dividing the sum of inpatient days by the number of patients admissions with the same diagnosis-related group classification. A variation in the calculation of ALOS can be to consider only length of stay during the period under analysis. Length of stay is typically highly skewness, skewed, so statistical approaches taking that into account are recommended. While the mean length of stay is useful from the point of view of costs, it may be a poor statistic in terms of representing a typical length of stay; the median may be preferred. It is useful to be able to predict an individual's expected length of stay or to model length of stay to determine factors that affect it. Various ana ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hospital
A hospital is a health care institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care. Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, seniors' (geriatric) hospitals, and hospitals for dealing with specific medical needs such as psychiatric treatment (see psychiatric hospital) and certain disease categories. Specialized hospitals can help reduce health care costs compared to general hospitals. Hospitals are classified as general, specialty, or government depending on the sources of income received. A teachi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Patient
A patient is any recipient of health care services that are performed by healthcare professionals. The patient is most often ill or injured and in need of treatment by a physician, nurse, optometrist, dentist, veterinarian, or other health care provider. Etymology The word patient originally meant 'one who suffers'. This English noun comes from the Latin word ', the present participle of the deponent verb, ', meaning 'I am suffering,' and akin to the Greek verb (', to suffer) and its cognate noun (). This language has been construed as meaning that the role of patients is to passively accept and tolerate the suffering and treatments prescribed by the healthcare providers, without engaging in shared decision-making about their care. Outpatients and inpatients An outpatient (or out-patient) is a patient who attends an outpatient clinic with no plan to stay beyond the duration of the visit. Even if the patient will not be formally admitted with a note as an outpatient, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Diagnosis-related Group
Diagnosis-related group (DRG) is a system to classify hospital cases into one of originally 467 groups, with the last group (coded as 470 through v24, 999 thereafter) being "Ungroupable". This system of classification was developed as a collaborative project by Robert B Fetter, PhD, of the Yale School of Management, and John D. Thompson, MPH, of the Yale School of Public Health.Fetter RB, Shin Y, Freeman JL, Averill RF, Thompson JD (1980) Case mix definition by diagnosis related groups. Medical Care 18(2):1–53 The system is also referred to as "the DRGs", and its intent was to identify the "products" that a hospital provides. One example of a "product" is an appendectomy. The system was developed in anticipation of convincing Congress to use it for reimbursement, to replace "cost based" reimbursement that had been used up to that point. DRGs are assigned by a "grouper" program based on ICD (International Classification of Diseases) diagnoses, procedures, age, sex, discharge ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Skewness
In probability theory and statistics, skewness is a measure of the asymmetry of the probability distribution of a real-valued random variable about its mean. The skewness value can be positive, zero, negative, or undefined. For a unimodal distribution, negative skew commonly indicates that the ''tail'' is on the left side of the distribution, and positive skew indicates that the tail is on the right. In cases where one tail is long but the other tail is fat, skewness does not obey a simple rule. For example, a zero value means that the tails on both sides of the mean balance out overall; this is the case for a symmetric distribution, but can also be true for an asymmetric distribution where one tail is long and thin, and the other is short but fat. Introduction Consider the two distributions in the figure just below. Within each graph, the values on the right side of the distribution taper differently from the values on the left side. These tapering sides are called ''tail ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Median
In statistics and probability theory, the median is the value separating the higher half from the lower half of a data sample, a population, or a probability distribution. For a data set, it may be thought of as "the middle" value. The basic feature of the median in describing data compared to the mean (often simply described as the "average") is that it is not skewed by a small proportion of extremely large or small values, and therefore provides a better representation of a "typical" value. Median income, for example, may be a better way to suggest what a "typical" income is, because income distribution can be very skewed. The median is of central importance in robust statistics, as it is the most resistant statistic, having a breakdown point of 50%: so long as no more than half the data are contaminated, the median is not an arbitrarily large or small result. Finite data set of numbers The median of a finite list of numbers is the "middle" number, when those numbers are list ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
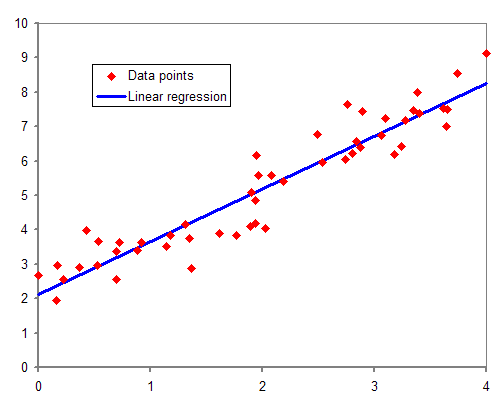
Regression Model
In statistical modeling, regression analysis is a set of statistical processes for estimating the relationships between a dependent variable (often called the 'outcome' or 'response' variable, or a 'label' in machine learning parlance) and one or more independent variables (often called 'predictors', 'covariates', 'explanatory variables' or 'features'). The most common form of regression analysis is linear regression, in which one finds the line (or a more complex linear combination) that most closely fits the data according to a specific mathematical criterion. For example, the method of ordinary least squares computes the unique line (or hyperplane) that minimizes the sum of squared differences between the true data and that line (or hyperplane). For specific mathematical reasons (see linear regression), this allows the researcher to estimate the conditional expectation (or population average value) of the dependent variable when the independent variables take on a given set of ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Markov Chain
A Markov chain or Markov process is a stochastic model describing a sequence of possible events in which the probability of each event depends only on the state attained in the previous event. Informally, this may be thought of as, "What happens next depends only on the state of affairs ''now''." A countably infinite sequence, in which the chain moves state at discrete time steps, gives a discrete-time Markov chain (DTMC). A continuous-time process is called a continuous-time Markov chain (CTMC). It is named after the Russian mathematician Andrey Markov. Markov chains have many applications as statistical models of real-world processes, such as studying cruise control systems in motor vehicles, queues or lines of customers arriving at an airport, currency exchange rates and animal population dynamics. Markov processes are the basis for general stochastic simulation methods known as Markov chain Monte Carlo, which are used for simulating sampling from complex probability dist ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Negative Binomial
In probability theory and statistics, the negative binomial distribution is a discrete probability distribution that models the number of failures in a sequence of independent and identically distributed Bernoulli trials before a specified (non-random) number of successes (denoted r) occurs. For example, we can define rolling a 6 on a die as a success, and rolling any other number as a failure, and ask how many failure rolls will occur before we see the third success (r=3). In such a case, the probability distribution of the number of failures that appear will be a negative binomial distribution. An alternative formulation is to model the number of total trials (instead of the number of failures). In fact, for a specified (non-random) number of successes (r), the number of failures (n - r) are random because the total trials (n) are random. For example, we could use the negative binomial distribution to model the number of days n (random) a certain machine works (specified by r) ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Prospective Payment System
A prospective payment system (PPS) is a term used to refer to several payment methodologies for which means of determining insurance reimbursement is based on a predetermined payment regardless of the intensity of the actual service provided. It includes a system for paying hospitals based on predetermined prices, from Medicare. Payments are typically based on codes provided on the insurance claim such as these: * Diagnosis-related groups for hospital inpatient claims * Ambulatory Payment Classification for hospital outpatient claims * Current Procedural Terminology for other outpatient claims The PPS was established by the Centers for Medicare and Medicaid Services (CMS), as a result of the Social Security Amendments Act of 1983, specifically to address expensive hospital care. Regardless of services provided, payment was of an established fee. The idea was to encourage hospitals to lower their prices for expensive hospital care. In 2000, CMS changed the reimbursement system ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medicare (United States)
Medicare is a government national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the SSA, including people with end stage renal disease and amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease). In 2018, according to the 2019 Medicare Trustees Report, Medicare provided health insurance for over 59.9 million individuals—more than 52 million people aged 65 and older and about 8 million younger people. According to annual Medicare Trustees reports and research by the government's MedPAC group, Medicare covers about half of healthcare expenses of those enrolled. Enrollees almost always cover most of the remaining costs by taking additional private insurance and/or by joining a public Part C or P ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Inpatient Care
Inpatient care is the care of patients whose condition requires admission to a hospital. Progress in modern medicine and the advent of comprehensive out-patient clinics ensure that patients are only admitted to a hospital when they are extremely ill or have severe physical trauma. Progress Patients enter inpatient care mainly from previous ambulatory care such as referral from a family doctor, or through emergency medicine departments. The patient formally becomes an "inpatient" at the writing of an admission note. Likewise, it is formally ended by writing a discharge note. Planning for patient discharge Health care professionals involved in rehabilitation are often involved in discharge planning for patients. When considering patient discharge, there are a number of factors to take into consideration: the patient's current state, their place of residence and the type of support available. When considering the patient's current state, although the patient may be eligible for dis ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |