Prenatal testing is a tool that can be used to detect some
birth defects
A birth defect is an abnormal condition that is present at birth, regardless of its cause. Birth defects may result in disabilities that may be physical, intellectual, or developmental. The disabilities can range from mild to severe. Birth de ...
at various stages prior to birth. Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of
prenatal care
Prenatal care, also known as antenatal care, is a type of preventive healthcare for pregnant individuals. It is provided in the form of medical checkups and healthy lifestyle recommendations for the pregnant person. Antenatal care also consists of ...
that focus on detecting problems with the pregnancy as early as possible. These may be
anatomic and
physiologic problems with the health of the
zygote
A zygote (; , ) is a eukaryote, eukaryotic cell (biology), cell formed by a fertilization event between two gametes.
The zygote's genome is a combination of the DNA in each gamete, and contains all of the genetic information of a new individ ...
,
embryo
An embryo ( ) is the initial stage of development for a multicellular organism. In organisms that reproduce sexually, embryonic development is the part of the life cycle that begins just after fertilization of the female egg cell by the male sp ...
, or
fetus
A fetus or foetus (; : fetuses, foetuses, rarely feti or foeti) is the unborn offspring of a viviparous animal that develops from an embryo. Following the embryonic development, embryonic stage, the fetal stage of development takes place. Pren ...
, either before
gestation
Gestation is the period of development during the carrying of an embryo, and later fetus, inside viviparous animals (the embryo develops within the parent). It is typical for mammals, but also occurs for some non-mammals. Mammals during pregn ...
even starts (as in
preimplantation genetic diagnosis) or as early in gestation as practicable. Screening can detect problems such as
neural tube defects,
chromosome
A chromosome is a package of DNA containing part or all of the genetic material of an organism. In most chromosomes, the very long thin DNA fibers are coated with nucleosome-forming packaging proteins; in eukaryotic cells, the most import ...
abnormalities, and gene
mutation
In biology, a mutation is an alteration in the nucleic acid sequence of the genome of an organism, virus, or extrachromosomal DNA. Viral genomes contain either DNA or RNA. Mutations result from errors during DNA or viral replication, ...
s that would lead to
genetic disorder
A genetic disorder is a health problem caused by one or more abnormalities in the genome. It can be caused by a mutation in a single gene (monogenic) or multiple genes (polygenic) or by a chromosome abnormality. Although polygenic disorders ...
s and birth defects such as
spina bifida
Spina bifida (SB; ; Latin for 'split spine') is a birth defect in which there is incomplete closing of the vertebral column, spine and the meninges, membranes around the spinal cord during embryonic development, early development in pregnancy. T ...
,
cleft palate
A cleft lip contains an opening in the upper lip that may extend into the nose. The opening may be on one side, both sides, or in the middle. A cleft palate occurs when the palate (the roof of the mouth) contains an opening into the nose. The ...
,
Down syndrome,
trisomy 18,
Tay–Sachs disease
Tay–Sachs disease is an Genetic disorder, inherited fatal lysosomal storage disease that results in the destruction of nerve cells in the brain and spinal cord. The most common form is infantile Tay–Sachs disease, which becomes apparent arou ...
,
sickle cell anemia
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the oxygen-carrying ...
,
thalassemia
Thalassemias are a group of Genetic disorder, inherited blood disorders that manifest as the production of reduced hemoglobin. Symptoms depend on the type of thalassemia and can vary from none to severe, including death. Often there is mild to ...
,
cystic fibrosis
Cystic fibrosis (CF) is a genetic disorder inherited in an autosomal recessive manner that impairs the normal clearance of Sputum, mucus from the lungs, which facilitates the colonization and infection of the lungs by bacteria, notably ''Staphy ...
,
muscular dystrophy
Muscular dystrophies (MD) are a genetically and clinically heterogeneous group of rare neuromuscular diseases that cause progressive weakness and breakdown of skeletal muscles over time. The disorders differ as to which muscles are primarily affe ...
, and
fragile X syndrome
Fragile X syndrome (FXS) is a genetic neurodevelopmental disorder. The average IQ in males with FXS is under 55, while affected females tend to be in the borderline to normal range, typically around 70–85. Physical features may include a lo ...
. Some tests are designed to discover problems which primarily affect the health of the mother, such as
PAPP-A to detect
pre-eclampsia
Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the new onset of hypertension, high blood pressure and often a significant amount of proteinuria, protein in the urine or by the new onset of high blood pressure a ...
or
glucose tolerance tests to diagnose
gestational diabetes. Screening can also detect anatomical defects such as
hydrocephalus
Hydrocephalus is a condition in which cerebrospinal fluid (CSF) builds up within the brain, which can cause pressure to increase in the skull. Symptoms may vary according to age. Headaches and double vision are common. Elderly adults with n ...
,
anencephaly,
heart defects, and
amniotic band syndrome.
Prenatal
screening focuses on finding problems among a large population with affordable and noninvasive methods. Prenatal diagnosis focuses on pursuing additional detailed information once a particular problem has been found, and can sometimes be more invasive. The most common screening procedures are routine
ultrasounds, blood tests, and blood pressure measurement. Common diagnosis procedures include
amniocentesis
Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is ...
and
chorionic villus sampling. In some cases, the tests are administered to determine if the fetus will be aborted, though physicians and patients also find it useful to diagnose high-risk pregnancies early so that delivery can be scheduled in a
tertiary care hospital where the baby can receive appropriate care.
Prenatal testing in recent years has been moving towards non-invasive methods to determine the fetal risk for genetic disorders. The rapid advancement of modern high-performance molecular technologies along with the discovery of
cell-free fetal DNA
Cell-free fetal DNA (cffDNA) is fetal DNA that circulates freely in the maternal blood. Maternal blood is sampled by venipuncture. Analysis of cffDNA is a method of non-invasive prenatal diagnosis frequently ordered for pregnant women of advance ...
(cffDNA) in maternal plasma has led to new methods for the determination of fetal chromosomal
aneuploidies. This type of testing is referred to as
non-invasive prenatal testing (NIPT) or as non-invasive prenatal screening. Invasive procedures remain important, though, especially for their diagnostic value in confirming positive non-invasive findings and detecting genetic disorders. Birth defects have an occurrence between 1 and 6%.
Purpose
There are three purposes of prenatal diagnosis: (1) to enable timely medical or surgical treatment of a condition before or after birth, (2) to give the parents the chance to abort a fetus with the diagnosed condition, and (3) to give parents the chance to prepare psychologically, socially, financially, and medically for a baby with a health problem or disability, or for the likelihood of a stillbirth. Prior information about problems in pregnancy means that healthcare staff as well as parents can better prepare themselves for the delivery of a child with a health problem. For example, Down syndrome is associated with cardiac defects that may need intervention immediately upon birth.
Prenatal screening
Maternal serum screening
First-trimester maternal serum screening can check levels of free β-
hCG,
PAPP-A, intact or beta hCG, or h-hCG in the woman's
serum, and combine these with the measurement of
nuchal translucency (NT). Some institutions also look for the presence of a fetal nasalbone on the ultrasound.
Second-trimester maternal serum screening (
AFP screening, triple screen, quad screen, or penta screen) can check levels of
alpha fetoprotein, β-
hCG,
inhibin-A,
estriol, and h-hCG (hyperglycosolated hCG) in the woman's
serum.
The
triple test measures
serum levels of
AFP,
estriol, and
beta-hCG, with a 70%
sensitivity and 5%
false-positive rate. It is complemented in some regions of the United States, as the ''Quad test'' (adding inhibin A to the panel, resulting in an 81% sensitivity and 5% false-positive rate for detecting
Down syndrome when taken at 15–18 weeks of
gestational age).
The biomarkers
PAPP-A and β-
hCG seem to be altered for pregnancies resulting from ICSI, causing a higher false-positive rate. Correction factors have been developed and
should be used when screening for Down's syndrome in singleton pregnancies after ICSI,
but in twin pregnancies such correction factors have not been fully elucidated.
In
vanishing twin pregnancies with a second gestational sac with a dead fetus, first-trimester screening should be based solely on the maternal age and the nuchal translucency scan as biomarkers are altered in these cases.
Advances in prenatal screening
Measurement of
fetal proteins in maternal serum is a part of standard prenatal screening for
fetal aneuploidy and
neural tube defects
Neural tube defects (NTDs) are a group of birth defects in which an opening in the spine or cranium remains from early in human development. In the third week of pregnancy called gastrulation, specialized cells on the dorsal side of the embry ...
. Computational predictive model shows that extensive and diverse feto-maternal protein trafficking occurs during pregnancy and can be readily detected non-invasively in maternal
whole blood. This computational approach circumvented a major limitation, the abundance of maternal proteins interfering with the detection of fetal proteins, to fetal proteomic analysis of maternal blood. Entering fetal gene transcripts previously identified in maternal whole blood into a computational predictive model helped develop a comprehensive proteomic network of the term neonate. It also shows that the fetal proteins detected in pregnant woman's blood originate from a diverse group of tissues and organs from the developing fetus. Development proteomic networks dominate the functional characterization of the predicted proteins, illustrating the potential clinical application of this technology as a way to monitor normal and abnormal fetal development.
The difference in
methylation
Methylation, in the chemistry, chemical sciences, is the addition of a methyl group on a substrate (chemistry), substrate, or the substitution of an atom (or group) by a methyl group. Methylation is a form of alkylation, with a methyl group replac ...
of specific DNA sequences between mother and fetus can be used to identify fetal-specific DNA in the blood circulation of the mother. In a study published in the March 6, 2011, online issue of ''
Nature
Nature is an inherent character or constitution, particularly of the Ecosphere (planetary), ecosphere or the universe as a whole. In this general sense nature refers to the Scientific law, laws, elements and phenomenon, phenomena of the physic ...
'', using this non-invasive technique a group of investigators from Greece and UK achieved correct diagnosis of 14
trisomy 21
A trisomy is a type of polysomy in which there are three instances of a particular chromosome, instead of the normal two. A trisomy is a type of aneuploidy (an abnormal number of chromosomes).
Description and causes
Most organisms that repro ...
(
Down syndrome) and 26 normal cases. Using
massive parallel sequencing
Massive parallel sequencing or massively parallel sequencing is any of several high-throughput approaches to DNA sequencing using the concept of massively parallel processing; it is also called next-generation sequencing (NGS) or second-generation ...
, a study testing for trisomy 21 only, successfully detected 209 of 212 cases (98.6%) with 3 false-positives in 1,471 pregnancies (0.2%).
With commercially available non-invasive (blood) testing for Down syndrome having become available to patients in the United States and already available in China, in October 2011, the International Society for Prenatal Diagnosis created some guidance. Based on its
sensitivity and specificity
In medicine and statistics, sensitivity and specificity mathematically describe the accuracy of a test that reports the presence or absence of a medical condition. If individuals who have the condition are considered "positive" and those who do ...
, it constitutes an advanced screening test and that positive results require confirmation by an invasive test, and that while effective in the diagnosis of Down syndrome, it cannot assess half the abnormalities detected by invasive testing. The test is not recommended for general use until results from broader studies have been reported, but may be useful in high-risk patients in conjunction with genetic counseling.
A study in 2012 found that the maternal plasma cell-free DNA test was also able to detect trisomy 18 (Edwards syndrome) in 100% of the cases (59/59) at a false-positive rate of 0.28%, and trisomy 13 (Patau syndrome) in 91.7% of the cases (11/12) at a false-positive rate of 0.97%. The test interpreted 99.1% of samples (1,971/1,988); among the 17 samples without an interpretation, three were trisomy 18. The study stated that if z-score cutoffs for trisomy 18 and 13 were raised slightly, the overall false-positive rates for the three aneuploidies could be as low as 0.1% (2/1,688) at an overall detection rate of 98.9% (280/283) for common aneuploidies (this includes all three trisomies: Down, Edwards and Patau).
Prenatal genetic testing
The goal of prenatal genetic testing is to identify pregnancies at high risk of abnormalities, allowing for early intervention, termination or appropriate management and preparation measures. Prenatal genetic testing can be subdivided into two categories: screening and diagnostic testing. Screening informs an individual of the potential for certain abnormalities occurring, whereas, diagnostic testing is used to confirm/diagnose that specific abnormalities exist within the fetus. Prenatal screens are typically less invasive than prenatal diagnostic tests. Screening comes with much lower risks, however, the results are not as definitive as diagnostic tests. Providers often recommend following up with a diagnostic test upon receipt of a positive result from a specific screen.
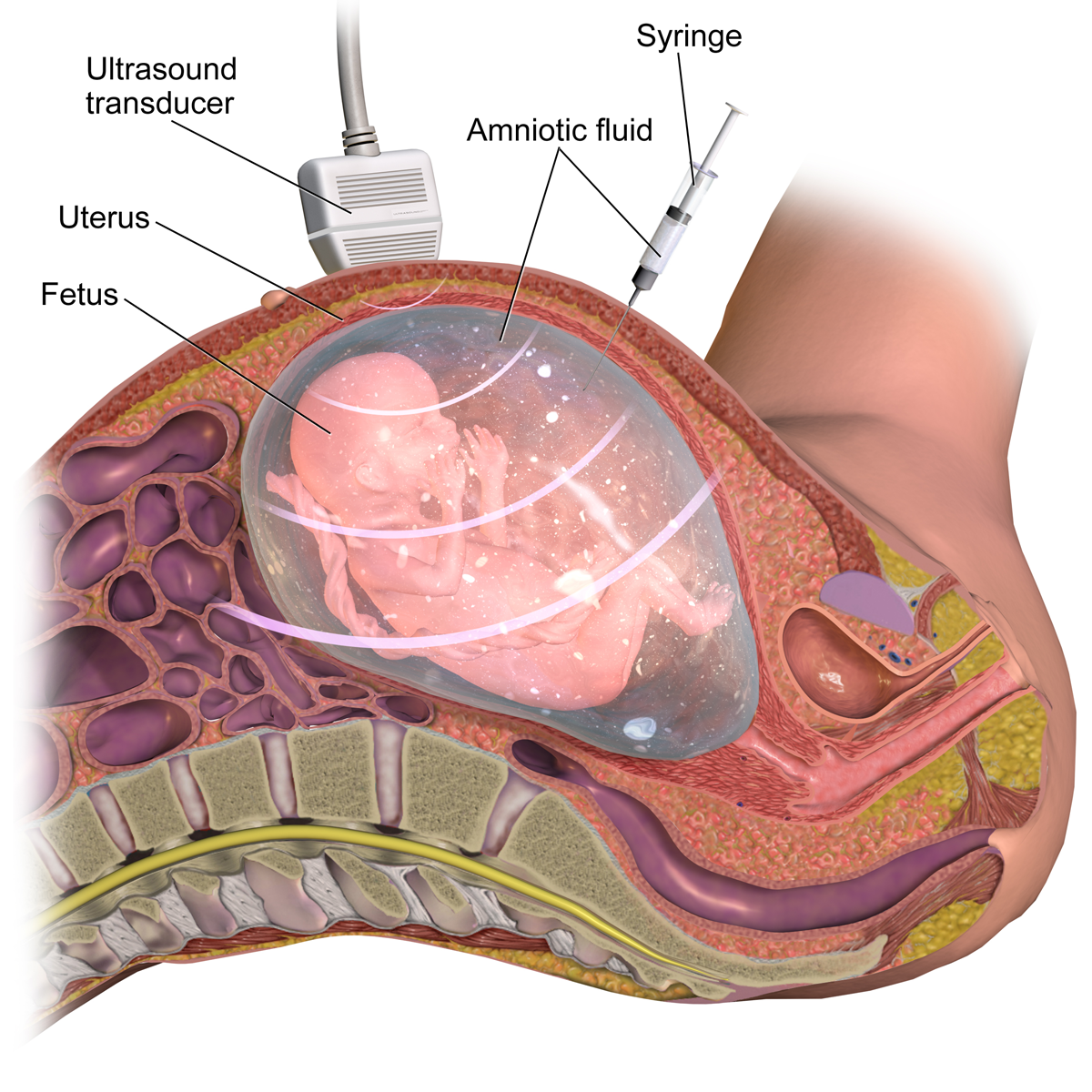
Medically invasive techniques are those in which a tool is used to access something inside the body. There are varying degrees of invasiveness, depending on what specimen is required to complete the test. The typical blood draw administered by a healthcare professional is one of the most common invasive medical practices. Since it causes minimal discomfort and there is very low risk associated with the sample collection, a blood draw is considered less invasive. Chorionic villus sampling (CVS) and Amniocentesis are the most invasive prenatal tests because there is greater associated risk and the sample is more difficult to access. These procedures are done via needle insertion into the abdomen to collect a sample within the uterus, meaning exceptional care/precision is required.
Prenatal genetic testing can identify various chromosomal abnormalities, autosomal conditions, various birth defects, and some fetal blood disorders.
Chromosomal abnormalities are when the chromosomes differ in either structure or number when compared to a typical reference genome. This includes chromosomal deletions, duplications, inversions, and translocations. Some examples of chromosomal abnormalities include:
*
Down syndrome (trisomy 21)
*
Edwards syndrome (trisomy 18)
*
Patau syndrome
Patau syndrome is a syndrome caused by a chromosomal abnormality, in which some or all of the cells of the body contain extra genetic material from chromosome 13. The extra genetic material disrupts normal development, causing multiple and co ...
(trisomy 13)
*
Turner syndrome
Turner syndrome (TS), commonly known as 45,X, or 45,X0,Also written as 45,XO. is a chromosomal disorder in which cells of females have only one X chromosome instead of two, or are partially missing an X chromosome (sex chromosome monosomy) lea ...
(monosomy X)
*
Klinefelter syndrome
Klinefelter syndrome (KS), also known as 47,XXY, is a chromosome anomaly where a male has an extra X chromosome. These complications commonly include infertility and small, poorly functioning testicles (if present). These symptoms are often n ...
(XXY)
*
Trisomy X
Trisomy X, also known as triple X syndrome and characterized by the karyotype 47,XXX, is a chromosome disorder in which a female has an extra copy of the X chromosome. It is relatively common and occurs in 1 in 1,000 females, but is rarely diagn ...
(XXX)
*
Jacobs syndrome (XYY)
*
Pallister–Killian syndrome
*
Wolf–Hirschhorn syndrome
Wolf–Hirschhorn syndrome (WHS) is a chromosomal deletion syndrome resulting from a partial deletion on the short arm of chromosome 4 el(4)(p16.3) Features include a distinct craniofacial phenotype and intellectual disability.
Signs and sympt ...
*
Cri-du-chat syndrome
*
WAGR syndrome
*
DiGeorge syndrome
DiGeorge syndrome, also known as 22q11.2 deletion syndrome, is a syndrome caused by a microdeletion on the long arm of chromosome 22. While the symptoms can vary, they often include congenital heart problems, specific facial features, frequent ...
*
Fragile X syndrome
Fragile X syndrome (FXS) is a genetic neurodevelopmental disorder. The average IQ in males with FXS is under 55, while affected females tend to be in the borderline to normal range, typically around 70–85. Physical features may include a lo ...
– Prader-Willi/Angelman syndrome
Autosomal recessive
In genetics, dominance is the phenomenon of one variant (allele) of a gene on a chromosome masking or overriding the Phenotype, effect of a different variant of the same gene on Homologous chromosome, the other copy of the chromosome. The firs ...
conditions occur when both parents pass on a mutation within an autosomal (non-sex) chromosome. Some examples of autosomal recessive conditions are:
*
Cystic fibrosis
Cystic fibrosis (CF) is a genetic disorder inherited in an autosomal recessive manner that impairs the normal clearance of Sputum, mucus from the lungs, which facilitates the colonization and infection of the lungs by bacteria, notably ''Staphy ...
*
Sickle cell anemia
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the oxygen-carrying ...
*
Tay–Sachs disease
Tay–Sachs disease is an Genetic disorder, inherited fatal lysosomal storage disease that results in the destruction of nerve cells in the brain and spinal cord. The most common form is infantile Tay–Sachs disease, which becomes apparent arou ...
*
Spinal muscular atrophy
*
Autosomal recessive polycystic kidney disease
*
Phenylketonuria
Phenylketonuria (PKU) is an inborn error of metabolism that results in decreased metabolism of the amino acid phenylalanine. Untreated PKU can lead to intellectual disability, seizures, behavioral problems, and mental disorders. It may also r ...
Neural tube defects are a type of birth defect that occurs when the neural tube of a fetus does not form/close properly, potentially effecting other systems throughout the body. Some examples of neural tube defects are:
*
Spina bifida
Spina bifida (SB; ; Latin for 'split spine') is a birth defect in which there is incomplete closing of the vertebral column, spine and the meninges, membranes around the spinal cord during embryonic development, early development in pregnancy. T ...
*
Anencephaly
*
Encephalocele
Encephalocele is a neural tube defect characterized by sac-like protrusions of the brain and the Biological membrane, membranes that cover it through openings in the human skull, skull. These defects are caused by failure of the neural tube to cl ...
*
Tethered spinal cord syndrome
Abdominal wall defects are a type of birth defect that occur when the abdominal wall of a fetus does not form properly, potentially effecting other organs throughout the body. Some examples of abdominal wall defects are:
*
Gastroschisis
Gastroschisis is a birth defect in which the baby's intestines extend outside of the abdomen through a hole next to the belly button. The size of the hole is variable, and other organs including the stomach and liver may also occur outside the b ...
*
Omphalocele
An omphalocele or omphalocoele, also known as an exomphalos, is a rare abdominal wall defect. Beginning at the 6th week of development, rapid elongation of the gut and increased liver size reduces intra abdominal space, which pushes intestinal lo ...
*
Bladder exstrophy
Bladder exstrophy is a congenital anomaly that exists along the spectrum of the exstrophy-epispadias complex, and most notably involves protrusion of the urinary bladder through a defect in the abdominal wall. Its presentation is variable, ofte ...
*
Cloacal exstrophy
A cloaca ( ), : cloacae ( or ), or vent, is the rear orifice that serves as the only opening for the digestive (rectum), reproductive, and urinary tracts (if present) of many vertebrate animals. All amphibians, reptiles, birds, cartilaginou ...
*
Ectopia cordis
*
Pentalogy of Cantrell
* Body-stalk anomaly
Blood disorders can occur from a negative interaction between the maternal blood and the fetal blood. An example of a fetal blood disorder is
Hemolytic disease of the fetus.
Ultrasound imaging and serum markers as indications for genetic testing
Ultrasound imaging provides the opportunity to conduct a nuchal translucency (NT) scan screening for chromosomal abnormalities such as
Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), and
Patau syndrome
Patau syndrome is a syndrome caused by a chromosomal abnormality, in which some or all of the cells of the body contain extra genetic material from chromosome 13. The extra genetic material disrupts normal development, causing multiple and co ...
(trisomy 13). Using the information from the NT scan the mother can be offered an invasive diagnostic test for fetal chromosomal abnormalities. Serum markers are used in a similar fashion to identify gestations that should be recommended for further testing. When the NT scan or serum markers arouse suspicion for chromosomal abnormalities the following genetic tests may be conducted on fetal or placental tissue samples: Interphase-
fluorescence in situ hybridization (FISH),
quantitative PCR
A real-time polymerase chain reaction (real-time PCR, or qPCR when used quantitatively) is a laboratory technique of molecular biology based on the polymerase chain reaction (PCR). It monitors the amplification of a targeted DNA molecule duri ...
and
direct preparation of chromosomes from chorionic villi.
Screens
Carrier screening
Carrier screening is a general DNA test that uses a blood or cheek swab sample to determine if the parents carry certain genetic conditions. This test can be done anytime, whether the individual(s) are considering starting a family or have already become pregnant. Various types of carrier screens are available that test for progressively more genetic abnormalities. The single gene/condition screen will test for a specific condition, whereas, the expanded carrier screen will test for hundreds of different abnormalities that can be inherited by a fetus. There are also three gene/condition and ethnic specific carrier tests. In the case of a positive test result, further testing is often recommended, as the carrier test only determines if the parent(s) is a carrier, not if the gene has definitively been passed to the fetus.
Placental acellular DNA (pa-DNA)
Placental acellular (fetal cell-free) DNA testing (pa-DNA) allows for the detection of apoptotic placental cells and placental DNA circulating in maternal blood for the noninvasive diagnosis of fetal aneuploidy.
A meta-analysis that investigated the success rate of using placental acellular DNA from maternal blood to screen for aneuploidies found that this technique detected trisomy 13 in 99% of the cases, trisomy 18 in 98% of the cases and trisomy 21 in 99% of the cases.
Failed tests using placental acellular DNA are more likely to occur in fetuses with trisomy 13 and trisomy 18 but not with trisomy 21. Previous studies found elevated levels of acellular placental DNA for trisomy 13 and 21 from maternal serum when compared to women with euploid pregnancies.
However, an elevation of acellular DNA for trisomy 18 was not observed.
Circulating placental nucleated cells comprise only three to six percent of maternal blood plasma DNA, reducing the detection rate of fetal developmental abnormalities.
Two alternative approaches have been developed for the detection of fetal aneuploidy. The first involves the measuring of the
allelic ratio of
single nucleotide polymorphism
In genetics and bioinformatics, a single-nucleotide polymorphism (SNP ; plural SNPs ) is a germline substitution of a single nucleotide at a specific position in the genome. Although certain definitions require the substitution to be present in ...
s (SNPs) in the
mRNA
In molecular biology, messenger ribonucleic acid (mRNA) is a single-stranded molecule of RNA that corresponds to the genetic sequence of a gene, and is read by a ribosome in the process of Protein biosynthesis, synthesizing a protein.
mRNA is ...
coding region in the
placenta
The placenta (: placentas or placentae) is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas, and waste exchange between ...
. The next approach is analyzing both maternal and placental DNA and looking for differences in the
DNA methylation
DNA methylation is a biological process by which methyl groups are added to the DNA molecule. Methylation can change the activity of a DNA segment without changing the sequence. When located in a gene promoter (genetics), promoter, DNA methylati ...
patterns.
First/Second/Third trimester Screen
The first, second, combined, and third trimester screens typically consist of an ultrasound (abdominal and/or transvaginal) and maternal blood/serum testing. The ultrasound is used to visually assess the growth, development, and activity of the fetus through imaging observations and measurements. The ultrasound portion of the first trimester screen can include a nuchal translucency screen and a fetal nasal bone determination screen. The available blood tests from the first trimester screen can test for plasma protein A and human chorionic gonadotropin. The second trimester screen looks at specific blood markers, to include the estriol, inhibin and human chorionic gonadotropin hormones and often consists of Alpha-fetoprotein (AFP) screening. Any abnormal results from these screening tests can indicate the possibility of abnormal conditions such as Trisomy 18, Trisomy 21 (Down syndrome), and spina bifida.
Alpha-fetoprotein (AFP)/multiple marker test
The AFP test is often done in the second trimester using the serum from the maternal blood draw. This test looks at a specific protein that is formed in the liver of the fetus and released into the fluid contents of the womb, which is then absorbed into the mother's blood stream. Multiple determinations stem from the results of AFP testing. Genetically, it can expose chromosomal and neural defects.
Diagnostic tests
Chorionic Villus Sampling (CVS)
CVS is an invasive diagnostic test that can be done during the first trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal abnormalities. A tissue cell sample of the placenta is obtained abdominally via needle or via vaginal insertion of a catheter/syringe into the cervix in combination with ultrasound to guide the procedure. Positive results from CVS require blood testing for confirmation.
Amniocentesis
Amniocentesis is an invasive diagnostic test that can be done during the second trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal and/or neural tube abnormalities. The procedure is typically done via needle, in combination with ultrasound for guidance, to obtain a sample of the amniotic fluid surrounding the fetus.
Cordocentesis/Percutaneous umbilical blood sampling (PUBS)
PUBS is an invasive diagnostic test that can be done during the second trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal and/or blood abnormalities. The demand for cordocentesis tests is diminishing because it has been replaced with CVS and Amniocentesis, which carry less risk. The procedure is typically done via needle into the mother's abdomen, in combination with ultrasound for guidance, to obtain a blood sample from the umbilical cord of the fetus.
Prenatal genetic testing analysis techniques
Digital PCR
Recently, it has been proposed that digital
PCR analysis can be conducted on fetal cell-free DNA for detection of fetal aneuploidy. Research has shown that digital PCR can be used to differentiate between normal and aneuploid DNA.
A variation of the PCR technique called
multiplex ligation-dependent probe amplification
Multiplex ligation-dependent probe amplification (MLPA) is a variation of the multiplex polymerase chain reaction that permits amplification of multiple targets with only a single primer (molecular biology), primer pair. It detects copy number cha ...
(MLPA), targeting DNA, has been successively applied for diagnosing fetal aneuploidy as a chromosome- or gene-specific assay.
Shotgun sequencing
Fetal cell-free DNA has been directly sequenced using
shotgun sequencing technology. In one study, DNA was obtained from the blood plasma of eighteen pregnant women. This was followed by mapping the chromosome using the quantification of fragments. This was done using advanced methods in
DNA sequencing
DNA sequencing is the process of determining the nucleic acid sequence – the order of nucleotides in DNA. It includes any method or technology that is used to determine the order of the four bases: adenine, thymine, cytosine, and guanine. The ...
resulting in the parallel sequencing of the fetal DNA. The amount of sequence tags mapped to each chromosome was counted. If there was a surplus or deficiency in any of the chromosomes, this meant that there was a fetal aneuploid. Using this method of shotgun sequencing, the successful identification of trisomy 21 (Down syndrome), trisomy 18 (Edward syndrome), and trisomy 13 (Patau syndrome) was possible. This method of noninvasive diagnosis is now starting to be heavily used and researched further.
Other techniques
Microarray analysis, karyotyping, and different genome sequencing techniques are also used to detect abnormalities. Fetal components in samples from maternal blood plasma can be analyzed by genome-wide techniques not only by total DNA, but also by
methylated DNA immunoprecipitation (with tiling array),
microRNA
Micro ribonucleic acid (microRNA, miRNA, μRNA) are small, single-stranded, non-coding RNA molecules containing 21–23 nucleotides. Found in plants, animals, and even some viruses, miRNAs are involved in RNA silencing and post-transcr ...
(such as with Megaplex) and total RNA (
RNA-sequencing).
By invasiveness
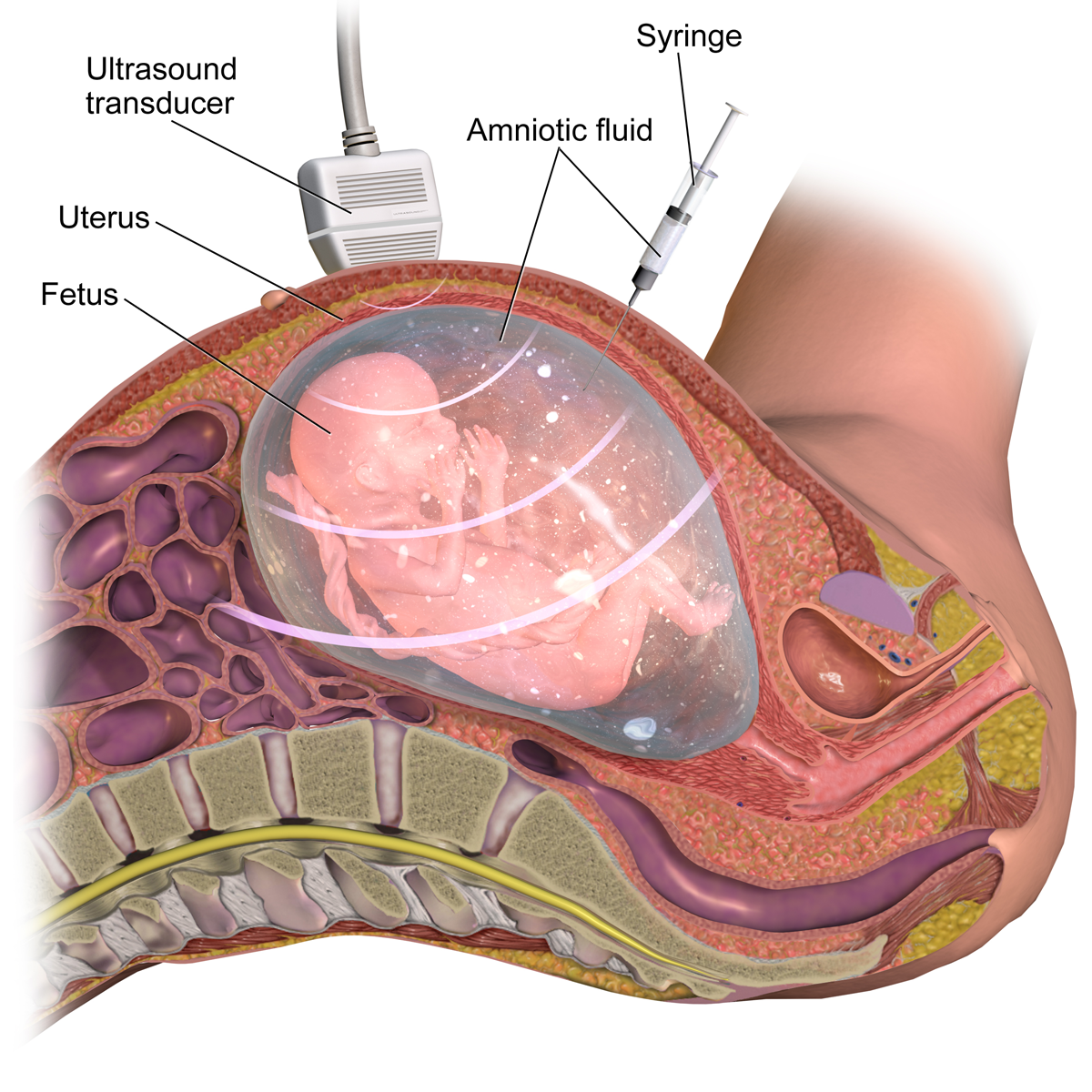
Diagnostic prenatal testing can be performed by
invasive or
non-invasive methods. An invasive method involves probes or needles being inserted into the
uterus
The uterus (from Latin ''uterus'', : uteri or uteruses) or womb () is the hollow organ, organ in the reproductive system of most female mammals, including humans, that accommodates the embryonic development, embryonic and prenatal development, f ...
, e.g.
amniocentesis
Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is ...
, which can be done from about 14 weeks gestation, and usually up to about 20 weeks, and
chorionic villus sampling, which can be done earlier (between 9.5 and 12.5 weeks gestation) but which may be slightly more risky to the fetus. One study comparing transabdominal chorionic villus sampling with second trimester amniocentesis found no significant difference in the total pregnancy loss between the two procedures.
[Amniocentesis and chorionic villus sampling for prenatal diagnosis (Review)](_blank)
By Alfirevic Z, Mujezinovic F, Sundberg K at The Cochrane Collaboration, 2009 However,
transcervical chorionic villus sampling carries a significantly higher risk, compared with a second-trimester amniocentesis, of total pregnancy loss (
relative risk
The relative risk (RR) or risk ratio is the ratio of the probability of an outcome in an exposed group to the probability of an outcome in an unexposed group. Together with risk difference and odds ratio, relative risk measures the association bet ...
1.40; 95%
confidence interval 1.09 to 1.81) and spontaneous miscarriage (9.4% risk; relative risk 1.50; 95% confidence interval 1.07 to 2.11).

Non-invasive techniques include examinations of the woman's womb through
ultrasonography
Medical ultrasound includes diagnostic techniques (mainly imaging) using ultrasound, as well as therapeutic applications of ultrasound. In diagnosis, it is used to create an image of internal body structures such as tendons, muscles, joints, ...
and maternal serum screens (i.e.
Alpha-fetoprotein
Alpha-fetoprotein (AFP, α-fetoprotein; also sometimes called alpha-1-fetoprotein, alpha-fetoglobulin, or alpha fetal protein) is a protein that in humans is encoded by the ''AFP'' gene. The ''AFP'' gene is located on the ''q'' arm of chromosome ...
). Blood tests for select trisomies (Down syndrome in the United States, Down and Edwards syndromes in China) based on detecting
cell-free placental DNA present in maternal blood, also known as non-invasive prenatal testing (NIPT), have become available.
If an elevated risk of chromosomal or genetic abnormality is indicated by a non-invasive screening test, a more invasive technique may be employed to gather more information.
In the case of neural tube defects, a detailed ultrasound can non-invasively provide a definitive diagnosis.
One of the major advantages of the non-invasive prenatal testing is that the chance of a false positive result is very low. This accuracy is very important for the pregnant woman, as due to a high sensitivity and specificity of the testing, especially for Down syndrome, the invasive testing could be avoided, which includes the risk of a miscarriage.
Testing guidelines and qualifying risk factors for invasive testing
The American College of Obstetricians and Gynecologists (
ACOG) guidelines currently recommend that anyone who is pregnant, regardless of age, should discuss and be offered non-invasive prenatal genetic screening and diagnostic testing options. Non-invasive prenatal genetic screening is typically performed at the end of the 1st trimester (11–14 weeks) or during the beginning of the second trimester (15–20 weeks). This involves the pregnant woman receiving a blood draw with a needle and a syringe and an ultrasound of the fetus. Screening tests can then include serum analyte screening or
cell-free fetal DNA
Cell-free fetal DNA (cffDNA) is fetal DNA that circulates freely in the maternal blood. Maternal blood is sampled by venipuncture. Analysis of cffDNA is a method of non-invasive prenatal diagnosis frequently ordered for pregnant women of advance ...
, and
nuchal translucency ultrasound T respectively. It is important to note that screening tests are not diagnostic, and concerning screening results should be followed up with invasive diagnostic testing for a confirmed diagnosis. Invasive diagnostic prenatal genetic testing can involve chronic villus sampling (CVS) or
amniocentesis
Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is ...
.
The ACOG recommends genetic screening before pregnancy to all pregnant women planning to have a family. After comprehensive counseling and discussion that acknowledges residual risks, it is important to respect the patients' right of choosing whether or not to pursue any component of genetic testing.
The following are some reasons why a woman might consider her risk of birth defects already to be high enough to warrant skipping screening and going straight for invasive testing:
* Increased risk of fetal aneuploidy based on personal obstetric history or family history affected by aneuploidy
* Increased risk for a known genetic or biochemical disease of the fetus
* Maternal transmissible infectious disease such as rubella or toxoplasma
* Parental request in the context of acute parental anxiety or under exceptional circumstances
Patient acceptance
Research was conducted to determine how women felt about noninvasive diagnosis of fetal aneuploid using maternal blood. This study was conducted using surveys. It was reported that eighty-two percent of pregnant women and seventy-nine percent of female medical students view this type of diagnosis in a positive light, agreeing that it is important for prenatal care. Overall, women responded optimistically that this form of diagnosis will be available in the future.
By pregnancy stage
Pre-conception
Prior to conception, couples may elect to have genetic testing done to determine the odds of conceiving a child with a known genetic anomaly. The most common in the Caucasian population are:
*
Cystic fibrosis
Cystic fibrosis (CF) is a genetic disorder inherited in an autosomal recessive manner that impairs the normal clearance of Sputum, mucus from the lungs, which facilitates the colonization and infection of the lungs by bacteria, notably ''Staphy ...
*
Fragile X syndrome
Fragile X syndrome (FXS) is a genetic neurodevelopmental disorder. The average IQ in males with FXS is under 55, while affected females tend to be in the borderline to normal range, typically around 70–85. Physical features may include a lo ...
* Blood disorders such as
sickle cell disease
Sickle cell disease (SCD), also simply called sickle cell, is a group of inherited Hemoglobinopathy, haemoglobin-related blood disorders. The most common type is known as sickle cell anemia. Sickle cell anemia results in an abnormality in the ...
*
Tay-Sachs disease
*
Spinal muscular atrophy
Hundreds of additional conditions are known and more discovered on a regular basis. However the economic justification for population-wide testing of all known conditions is not well supported, particularly once the cost of possible false positive results and concomitant follow-up testing are taken into account. There are also ethical concerns related to this or any type of
genetic testing
Genetic testing, also known as DNA testing, is used to identify changes in DNA sequence or chromosome structure. Genetic testing can also include measuring the results of genetic changes, such as RNA analysis as an output of gene expression, or ...
.
One or both partners may be aware of other family members with these diseases. Testing prior to conception may alleviate concern, prepare the couple for the potential short- or long-term consequences of having a child with the disease, direct the couple toward adoption or foster parenting, or prompt for
preimplantation genetic testing during
''in vitro'' fertilization. If a genetic disorder is found, professional
genetic counseling is usually recommended owing to the host of ethical considerations related to subsequent decisions for the partners and potential impact on their extended families. Most, but not all, of these diseases follow
Mendelian inheritance
Mendelian inheritance (also known as Mendelism) is a type of biological inheritance following the principles originally proposed by Gregor Mendel in 1865 and 1866, re-discovered in 1900 by Hugo de Vries and Carl Correns, and later popularize ...
patterns.
Fragile X syndrome
Fragile X syndrome (FXS) is a genetic neurodevelopmental disorder. The average IQ in males with FXS is under 55, while affected females tend to be in the borderline to normal range, typically around 70–85. Physical features may include a lo ...
is related to expansion of certain repeated DNA segments and may change generation-to-generation.
First trimester
At early presentation of pregnancy at around 6 weeks, early dating ultrasound scan may be offered to help confirm the
gestational age of the embryo and check for a single or twin pregnancy, but such a scan is unable to detect common abnormalities. Details of prenatal screening and testing options may be provided.
Around weeks 11–13,
nuchal translucency scan (NT) may be offered which can be combined with blood tests for PAPP-A and beta-hCG, two serum markers that correlate with chromosomal abnormalities, in what is called the First Trimester Combined Test. The results of the blood test are then combined with the NT ultrasound measurements, maternal age, and gestational age of the fetus to yield a risk score for Down syndrome, trisomy 18, and trisomy 13. First Trimester Combined Test has a sensitivity (i.e. detection rate for abnormalities) of 82–87% and a false-positive rate of around 5%.
Cell-free fetal DNA
Cell-free fetal DNA (cffDNA) is fetal DNA that circulates freely in the maternal blood. Maternal blood is sampled by venipuncture. Analysis of cffDNA is a method of non-invasive prenatal diagnosis frequently ordered for pregnant women of advance ...
is also available during the first trimester of pregnancy.
Second trimester
The
anomaly scan is performed between 18 and 22 weeks of
gestational age. The
International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) recommends that this ultrasound is performed as a matter of routine
prenatal care
Prenatal care, also known as antenatal care, is a type of preventive healthcare for pregnant individuals. It is provided in the form of medical checkups and healthy lifestyle recommendations for the pregnant person. Antenatal care also consists of ...
, to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, and to assess for
congenital malformations and
multiple pregnancies (i.e. twins). The scan can detect
anencephaly, open
spina bifida
Spina bifida (SB; ; Latin for 'split spine') is a birth defect in which there is incomplete closing of the vertebral column, spine and the meninges, membranes around the spinal cord during embryonic development, early development in pregnancy. T ...
,
cleft lip
A cleft lip contains an opening in the upper lip that may extend into the nose. The opening may be on one side, both sides, or in the middle. A cleft palate occurs when the palate (the roof of the mouth) contains an opening into the nasal cavi ...
,
diaphragmatic hernia
Diaphragmatic hernia is a defect or hole in the diaphragm that allows the abdominal contents to move into the chest cavity. Treatment is usually surgical.
Types
* Congenital diaphragmatic hernia
** Morgagni's hernia
** Bochdalek hernia
* Hi ...
,
gastroschisis
Gastroschisis is a birth defect in which the baby's intestines extend outside of the abdomen through a hole next to the belly button. The size of the hole is variable, and other organs including the stomach and liver may also occur outside the b ...
,
omphalocele
An omphalocele or omphalocoele, also known as an exomphalos, is a rare abdominal wall defect. Beginning at the 6th week of development, rapid elongation of the gut and increased liver size reduces intra abdominal space, which pushes intestinal lo ...
,
congenital heart defect
A congenital heart defect (CHD), also known as a congenital heart anomaly, congenital cardiovascular malformation, and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital h ...
,
bilateral renal agenesis,
osteochondrodysplasia,
Edwards syndrome, and
Patau syndrome
Patau syndrome is a syndrome caused by a chromosomal abnormality, in which some or all of the cells of the body contain extra genetic material from chromosome 13. The extra genetic material disrupts normal development, causing multiple and co ...
.
A second-trimester
Quad blood test may be taken (the
Triple test is widely considered obsolete but in some states, such as Missouri, where
Medicaid
Medicaid is a government program in the United States that provides health insurance for adults and children with limited income and resources. The program is partially funded and primarily managed by U.S. state, state governments, which also h ...
only covers the Triple test, that's what the patient typically gets). With ''integrated screening'', both a First Trimester Combined Test and a Triple/Quad test is performed, and a report is only produced after both tests have been analyzed. However patients may not wish to wait between these two sets of tests. With ''sequential screening'', a first report is produced after the first trimester sample has been submitted, and a final report after the second sample. With ''contingent screening'', patients at very high or very low risks will get reports after the first-trimester sample has been submitted. Only patients with ''moderate risk'' (risk score between 1:50 and 1:2000) will be asked to submit a second-trimester sample, after which they will receive a report combining information from both serum samples and the
NT measurement. The First Trimester Combined Test and the Triple/Quad test together have a sensitivity of 88–95% with a 5% false-positive rate for Down syndrome, though they can also be analyzed in such a way as to offer a 90% sensitivity with a 2% false-positive rate. Finally, patients who do not receive an NT ultrasound in the 1st trimester may still receive a Serum Integrated test involving measuring PAPP-A serum levels in the 1st trimester and then doing a Quad test in the 2nd trimester. This offers an 85–88% sensitivity and 5% false-positive rate for Down syndrome. Also, a patient may skip the 1st-trimester screening entirely and receive only a 2nd-trimester Quad test, with an 81% sensitivity for Down syndrome and 5% false-positive rate.
Third trimester
Third-trimester prenatal testing generally focuses on maternal wellbeing and reducing fetal morbidity/mortality.
Group B streptococcal infection (also called Group B strep) may be offered, which is a major cause of neonatal morbidity and mortality. Group B strep is an infection that may be passed to an infant during birth. Vaginal screening for GBS is performed between 34 and 37 weeks of gestational age, so that mothers that are positive for the bacterium can receive treatment before delivery. During the third trimester, some institutions may require evaluations of hemoglobin/hematocrit, syphilis serology, and HIV screening. Also, before delivery, an assessment of fetal position and estimated fetal weight is documented.
Legislation
In Europe
Prenatal diagnosis (DPN) is permitted throughout Europe, with the exception of Ireland. Eight (8) countries have no legislation on this matter. However, there are differences between states. For instance, in
Poland
Poland, officially the Republic of Poland, is a country in Central Europe. It extends from the Baltic Sea in the north to the Sudetes and Carpathian Mountains in the south, bordered by Lithuania and Russia to the northeast, Belarus and Ukrai ...
, the deadline for DPN is 22 weeks. In
Malta
Malta, officially the Republic of Malta, is an island country in Southern Europe located in the Mediterranean Sea, between Sicily and North Africa. It consists of an archipelago south of Italy, east of Tunisia, and north of Libya. The two ...
, the Parliamentary Social Affairs Committee specified in its 2005 report that DPN should only be allowed for conditions for which therapeutic options exist. Nevertheless, all countries prohibit DPN for non-medical purposes (such as sex selection), for example.
In France
Article L2131-1 of the Public Health Code, stemming from the July 2011 bioethics law, states that "prenatal diagnosis refers to medical practices, including obstetric and fetal ultrasound, aimed at detecting, in utero, a particularly severe condition in the embryo or fetus." The law requires that pregnant women receive clear information about these techniques to "assess the risk that the embryo or fetus may have a condition that could alter the course or management of the pregnancy.
Ethical and practical issues
Non-genetic prenatal testing
Parents need to make informed decisions about screening, diagnosis, and any actions to be taken as a result. Many screening tests are inaccurate, so one worrisome test result frequently leads to additional, more invasive tests. If prenatal testing confirms a serious disability, many parents are forced to decide whether to continue the pregnancy or seek an abortion. The "option" of screening becomes an unexpected requirement to decide.
In some genetic conditions, for instance
cystic fibrosis
Cystic fibrosis (CF) is a genetic disorder inherited in an autosomal recessive manner that impairs the normal clearance of Sputum, mucus from the lungs, which facilitates the colonization and infection of the lungs by bacteria, notably ''Staphy ...
, an abnormality can only be detected if DNA is obtained from the fetus. Usually an invasive method is needed to do this.
Ultrasound of a fetus, which is considered a screening test, can sometimes miss subtle abnormalities. For example, studies show that a detailed 2nd-trimester ultrasound, also called a level 2 ultrasound, can detect about 97% of neural tube defects such as
spina bifida
Spina bifida (SB; ; Latin for 'split spine') is a birth defect in which there is incomplete closing of the vertebral column, spine and the meninges, membranes around the spinal cord during embryonic development, early development in pregnancy. T ...
. Ultrasound results may also show "soft signs," such as an
Echogenic intracardiac focus or a
Choroid plexus cyst, which are usually normal, but can be associated with an increased risk for
chromosome
A chromosome is a package of DNA containing part or all of the genetic material of an organism. In most chromosomes, the very long thin DNA fibers are coated with nucleosome-forming packaging proteins; in eukaryotic cells, the most import ...
abnormalities.
Other screening tests, such as the Quad test, can also have false positives and false negatives. Even when the Quad results are positive (or, to be more precise, when the Quad test yields a score that shows at least a 1 in 270 risk of abnormality), usually the pregnancy is normal, but additional diagnostic tests are offered. In fact, consider that Down syndrome affects about 1:400 pregnancies; if you screened 4000 pregnancies with a Quad test, there would probably be 10 Down syndrome pregnancies of which the Quad test, with its 80% sensitivity, would call 8 of them high-risk. The quad test would also tell 5% (~200) of the 3990 normal women that they are high-risk. Therefore, about 208 women would be told they are high-risk, but when they undergo an invasive test, only 8 (or 4% of the high risk pool) will be confirmed as positive and 200 (96%) will be told that their pregnancies are normal. Since amniocentesis has approximately a 0.5% chance of miscarriage, one of those 200 normal pregnancies might result in a miscarriage because of the invasive procedure. Meanwhile, of the 3792 women told they are low-risk by the Quad test, 2 of them will go on to deliver a baby with Down syndrome. The Quad test is therefore said to have a 4%
positive predictive value (PPV) because only 4% of women who are told they are "high-risk" by the screening test actually have an affected fetus. The other 96% of the women who are told they are "high-risk" find out that their pregnancy is normal.
By comparison, in the same 4000 women, a screening test that has a 99% sensitivity and a 0.5% false positive rate would detect all 10 positives while telling 20 normal women that they are positive. Therefore, 30 women would undergo a confirmatory invasive procedure and 10 of them (33%) would be confirmed as positive and 20 would be told that they have a normal pregnancy. Of the 3970 women told by the screen that they are negative, none of the women would have an affected pregnancy. Therefore, such a screen would have a 33% positive predictive value.
The real-world false-positive rate for the Quad test (as well as 1st Trimester Combined, Integrated, etc.) is greater than 5%. 5% was the rate quoted in the large clinical studies that were done by the best researchers and physicians, where all the ultrasounds were done by well-trained sonographers and the gestational age of the fetus was calculated as closely as possible. In the real world, where calculating gestational age may be a less precise art, the formulas that generate a patient's risk score are not as accurate and the false-positive rate can be higher, even 10%.
Because of the low accuracy of conventional screening tests, 5–10% of women, often those who are older, will opt for an invasive test even if they received a low-risk score from the screening. A patient who received a 1:330 risk score, while technically low-risk (since the cutoff for high-risk is commonly quoted as 1:270), might be more likely to still opt for a confirmatory invasive test. On the other hand, a patient who receives a 1:1000 risk score is more likely to feel assuaged that her pregnancy is normal.
Both
false positives
A false positive is an error in binary classification in which a test result incorrectly indicates the presence of a condition (such as a disease when the disease is not present), while a false negative is the opposite error, where the test res ...
and
false negatives will have a large impact on a couple when they are told the result, or when the child is born.
Diagnostic
Diagnosis (: diagnoses) is the identification of the nature and cause of a certain phenomenon. Diagnosis is used in a lot of different academic discipline, disciplines, with variations in the use of logic, analytics, and experience, to determine " ...
tests, such as amniocentesis, are considered to be very accurate for the defects they check for, though even these tests are not perfect, with a reported 0.2% error rate (often due to rare abnormalities such as mosaic Down syndrome where only some of the fetal/placental cells carry the genetic abnormality).
A higher
maternal serum AFP level indicates a greater risk for anencephaly and open spina bifida. This screening is 80% and 90% sensitive for spina bifida and anencephaly, respectively.
Amniotic fluid
acetylcholinesterase
Acetylcholinesterase (HUGO Gene Nomenclature Committee, HGNC symbol ACHE; EC 3.1.1.7; systematic name acetylcholine acetylhydrolase), also known as AChE, AChase or acetylhydrolase, is the primary cholinesterase in the body. It is an enzyme th ...
and
AFP level are more
sensitive and
specific than AFP in predicting neural tube defects.
Many maternal-fetal specialists do not bother to even do an AFP test on their patients because they do a detail ultrasound on all of them in the 2nd trimester, which has a 97% detection rate for neural tube defects such as anencephaly and open spina bifida. Performing tests to determine possible birth defects is mandatory in all U.S. states. Failure to detect issues early can have dangerous consequences on both the mother and the baby.
OBGYNs may be held culpable. In one case a man who was born with spina bifida was awarded $2 million in settlement, apart from medical expenses, due to the OBGYN's negligence in conducting AFP tests.
No prenatal test can detect ''all'' forms of birth defects and abnormalities.
Prenatal genetic testing
Another important issue is the uncertainty of prenatal genetic testing. Uncertainty on genetic testing results from several reasons: the genetic test is associated with a disease but the prognosis and/or probability is unknown, the genetic test provides information different than the familiar disease they tested for, found genetic variants have unknown significance, and finally, results may not be associated with found fetal abnormalities. Richardson and Ormond thoroughly addressed the issue of uncertainty of genetic testing and explained its implication for bioethics. First, the principle of beneficence is assumed in prenatal testing by decreasing the risk of miscarriage, however, uncertain information derived from genetic testing may harm the parents by provoking anxiety and leading to the termination of a fetus that is probably healthy. Second, the principle of autonomy is undermined given a lack of comprehension resulting from new technologies and changing knowledge in the field of genetics. And third, the principle of justice raised issues regarding equal access to emerging prenatal tests.
Availability of treatments
If a genetic disease is detected, there is often no treatment that can help the fetus until it is born. However, in the US, there are prenatal surgeries for
spina bifida
Spina bifida (SB; ; Latin for 'split spine') is a birth defect in which there is incomplete closing of the vertebral column, spine and the meninges, membranes around the spinal cord during embryonic development, early development in pregnancy. T ...
fetus. Early diagnosis gives the parents time to research and discuss post-natal treatment and care, or in some cases, abortion.
Genetic counselors are usually called upon to help families make informed decisions regarding results of prenatal diagnosis.
Patient education
Researchers have studied how disclosing amniocentesis or
chorionic villous sampling (CVS) results on a fixed date versus a variable date (i.e. "when available") affects maternal anxiety. Systematic review of the relevant articles found no conclusive evidence to support issuing amniocentesis results as soon as they become available (in comparison to issuing results on a pre-defined fixed date). The researchers concluded that further studies evaluating the effect of different strategies for disclosing CVS results on maternal anxiety are needed.
Concerns from disability rights activists and scholars
Since its introduction in 2011 to 2025, there has been a global expansion of
non-invasive prenatal testing (NIPT). Initially, only women at-high risk for
chromosomal abnormalities underwent NIPT, however in recent years it has become routine during pregnancy. NIPT is especially accurate at detecting trisomy 21, also known as
Down's Syndrome, which is the most common form of chromosomal disorder in live births. In England, Whales, and Scotland abortion due to disability is legal under the
Abortion Act of 1967. In the US, it is estimated that NIPT has potentially led to a 30% decrease of people living with Down's Syndrome. Disability rights activists and scholars have suggested a more critical view of prenatal testing not as a test itself but rather for its implications for people with disabilities. They argue that access to prenatal testing could result in pressure to abort fetuses that might be born with disabilities, and that these pressures rely on eugenics interests and
ableist stereotypes. This selective abortion relies on the ideas that people with disabilities cannot live desirable lives, that they will not be able to flourish and that they are burdens to their families. Activists argue that inevitably societal perceptions about disabilities will influence the decision to terminate a pregnancy. For this reason, Marsha Saxton suggests that families should question whether or not they are relying on real, factual information about people with disabilities or on stereotypes if they decide to abort a fetus with a disability.
Societal pressures
Amniocentesis has become the standard of care for prenatal care visits for women who are "at risk" or over a certain age. The wide use of amniocentesis has been defined as consumeristic. and some argue that this can be in conflict with the right to privacy, Most obstetricians (depending on the country) offer patients the AFP
triple test, HIV test, and ultrasounds routinely. However, almost all women meet with a
genetic counselor before deciding whether to have prenatal diagnosis. It is the role of the genetic counselor to accurately inform women of the risks and benefits of prenatal diagnosis. Genetic counselors are trained to be non-directive and to support the patient's decision. Some doctors do advise women to have certain prenatal tests and the patient's partner may also influence the woman's decision.
Legal
In August 2023, the Iranian government banned import and manufacture of tests kits required for first screening trimester tests, it will plague the population according to society of medicine in genetic . Iranian
state welfare organization had a genetics condition program since 1997.
See also
*
Amniocentesis
Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is ...
*
Amniotic stem cell bank
*
Amniotic stem cells
*
Chorionic villi
Chorionic villi are Wiktionary:villus, villi that sprout from the chorion to provide maximal contact area with maternal blood.
They are an essential element in pregnancy from a histology, histomorphologic perspective, and are, by definition, a pr ...
*
Genetic counseling
*
Newborn screening
Newborn screening (NBS) is a public health program of screening (medicine), screening in infants shortly after birth for conditions that are treatable, but not clinically evident in the newborn period. The goal is to identify infants at risk for ...
Notes and references
External links
Our Bodies Ourselves chapter on Prenatal Testing and Disability RightsPrenatal Tests and Why Are They Important?– March Of Dimes
{{DEFAULTSORT:Prenatal Diagnosis
Obstetrical procedures
Midwifery
 Diagnostic prenatal testing can be performed by invasive or non-invasive methods. An invasive method involves probes or needles being inserted into the
Diagnostic prenatal testing can be performed by invasive or non-invasive methods. An invasive method involves probes or needles being inserted into the  Non-invasive techniques include examinations of the woman's womb through
Non-invasive techniques include examinations of the woman's womb through