calcium homeostasis on:
[Wikipedia]
[Google]
[Amazon]
 Calcium metabolism is the movement and regulation of
Calcium metabolism is the movement and regulation of
 The active absorption of calcium from the gut is regulated by the
The active absorption of calcium from the gut is regulated by the
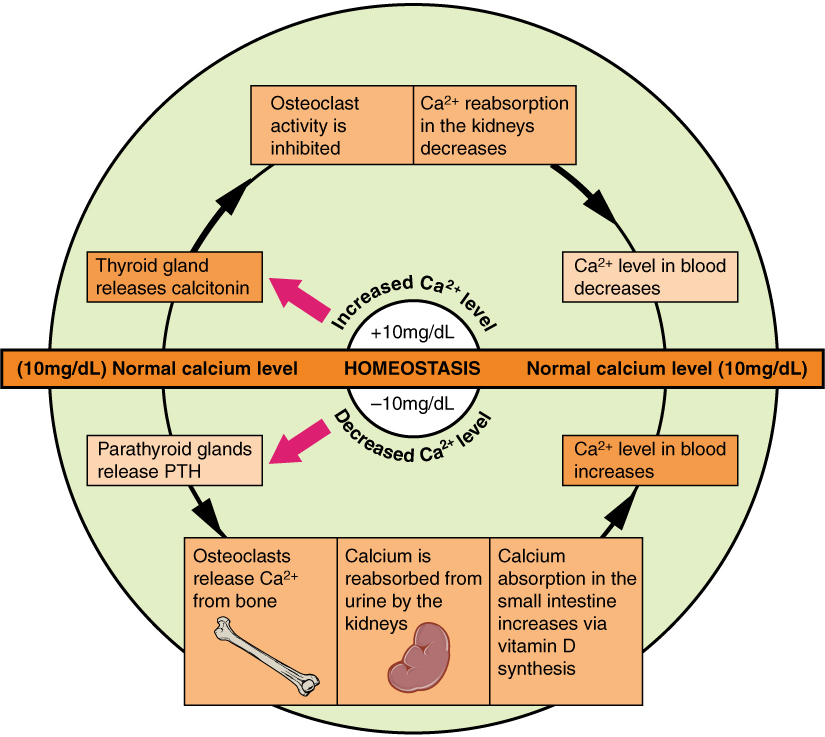
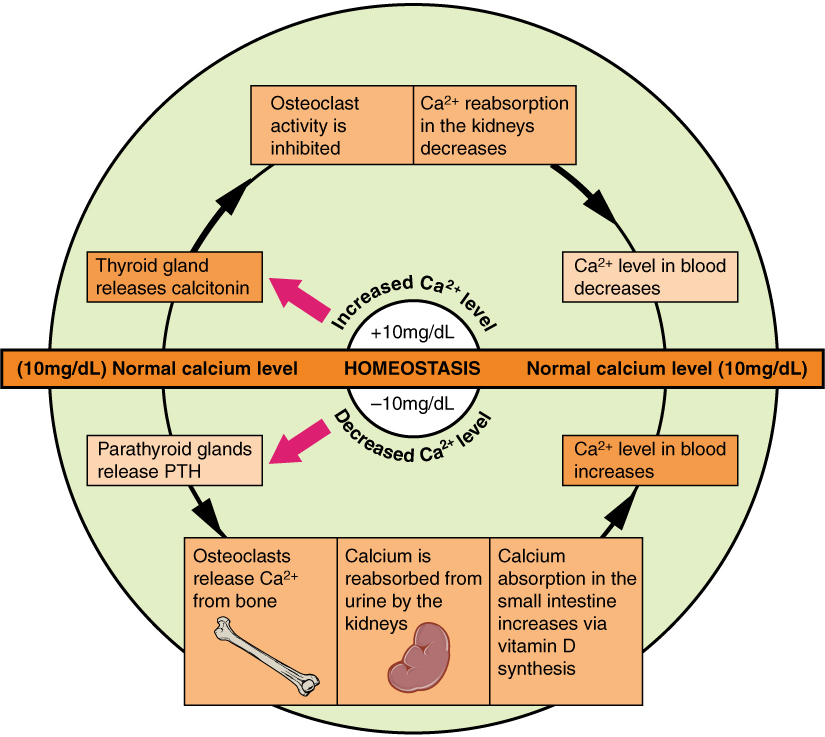
 The plasma ionized calcium concentration is regulated within narrow limits (1.3–1.5 mmol/L). This is achieved by both the parafollicular cells of the thyroid gland, and the parathyroid glands constantly sensing (i.e. measuring) the concentration of calcium ions in the blood flowing through them.
The plasma ionized calcium concentration is regulated within narrow limits (1.3–1.5 mmol/L). This is achieved by both the parafollicular cells of the thyroid gland, and the parathyroid glands constantly sensing (i.e. measuring) the concentration of calcium ions in the blood flowing through them.

Calcium
at Lab Tests Online * {{DEFAULTSORT:Calcium Metabolism Physiology Calcium Human homeostasis Endocrine system
 Calcium metabolism is the movement and regulation of
Calcium metabolism is the movement and regulation of calcium
Calcium is a chemical element; it has symbol Ca and atomic number 20. As an alkaline earth metal, calcium is a reactive metal that forms a dark oxide-nitride layer when exposed to air. Its physical and chemical properties are most similar to it ...
ions (Ca2+) ''in'' (via the gut) and ''out'' (via the gut and kidney
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organ (anatomy), organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and rig ...
s) of the body, and ''between'' body compartments: the blood plasma
Blood plasma is a light Amber (color), amber-colored liquid component of blood in which blood cells are absent, but which contains Blood protein, proteins and other constituents of whole blood in Suspension (chemistry), suspension. It makes up ...
, the extracellular
This glossary of biology terms is a list of definitions of fundamental terms and concepts used in biology, the study of life and of living organisms. It is intended as introductory material for novices; for more specific and technical definitions ...
and intracellular
This glossary of biology terms is a list of definitions of fundamental terms and concepts used in biology, the study of life and of living organisms. It is intended as introductory material for novices; for more specific and technical definitions ...
fluids, and bone
A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, ...
. Bone acts as a calcium storage center for deposits and withdrawals as needed by the blood via continual bone remodeling
300 px, Bone tissue is removed by osteoclasts, and then new bone tissue is formed by osteoblasts. Both processes utilize cytokine ( Insulin-like_growth_factor.html" ;"title="TGF-β, Insulin-like growth factor">IGF) signalling.
In osteology, bone ...
.
An important aspect of calcium metabolism
Metabolism (, from ''metabolē'', "change") is the set of life-sustaining chemical reactions in organisms. The three main functions of metabolism are: the conversion of the energy in food to energy available to run cellular processes; the co ...
is plasma calcium homeostasis
In biology, homeostasis (British English, British also homoeostasis; ) is the state of steady internal physics, physical and chemistry, chemical conditions maintained by organism, living systems. This is the condition of optimal functioning fo ...
, the regulation of calcium ions in the blood plasma
Blood plasma is a light Amber (color), amber-colored liquid component of blood in which blood cells are absent, but which contains Blood protein, proteins and other constituents of whole blood in Suspension (chemistry), suspension. It makes up ...
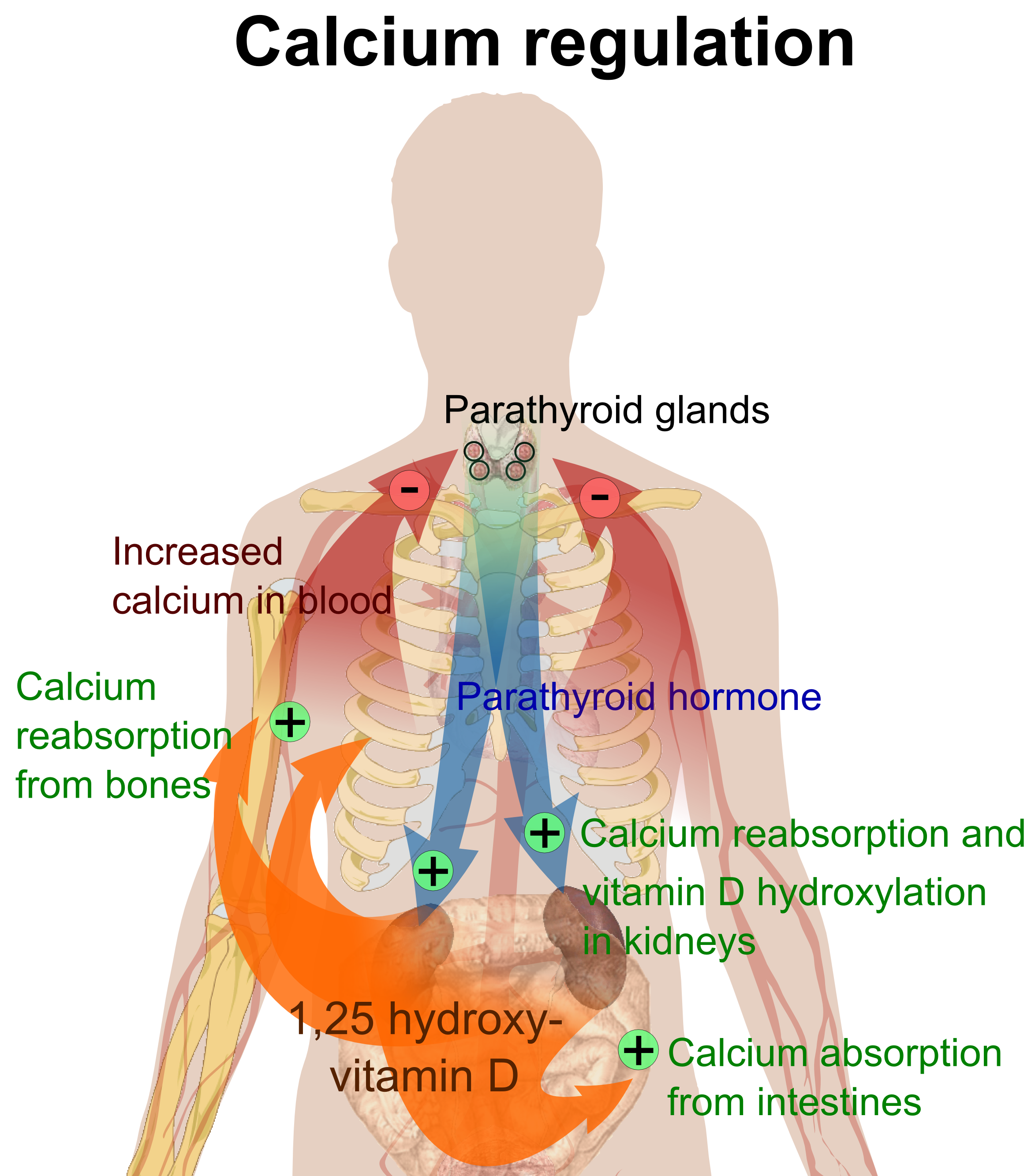
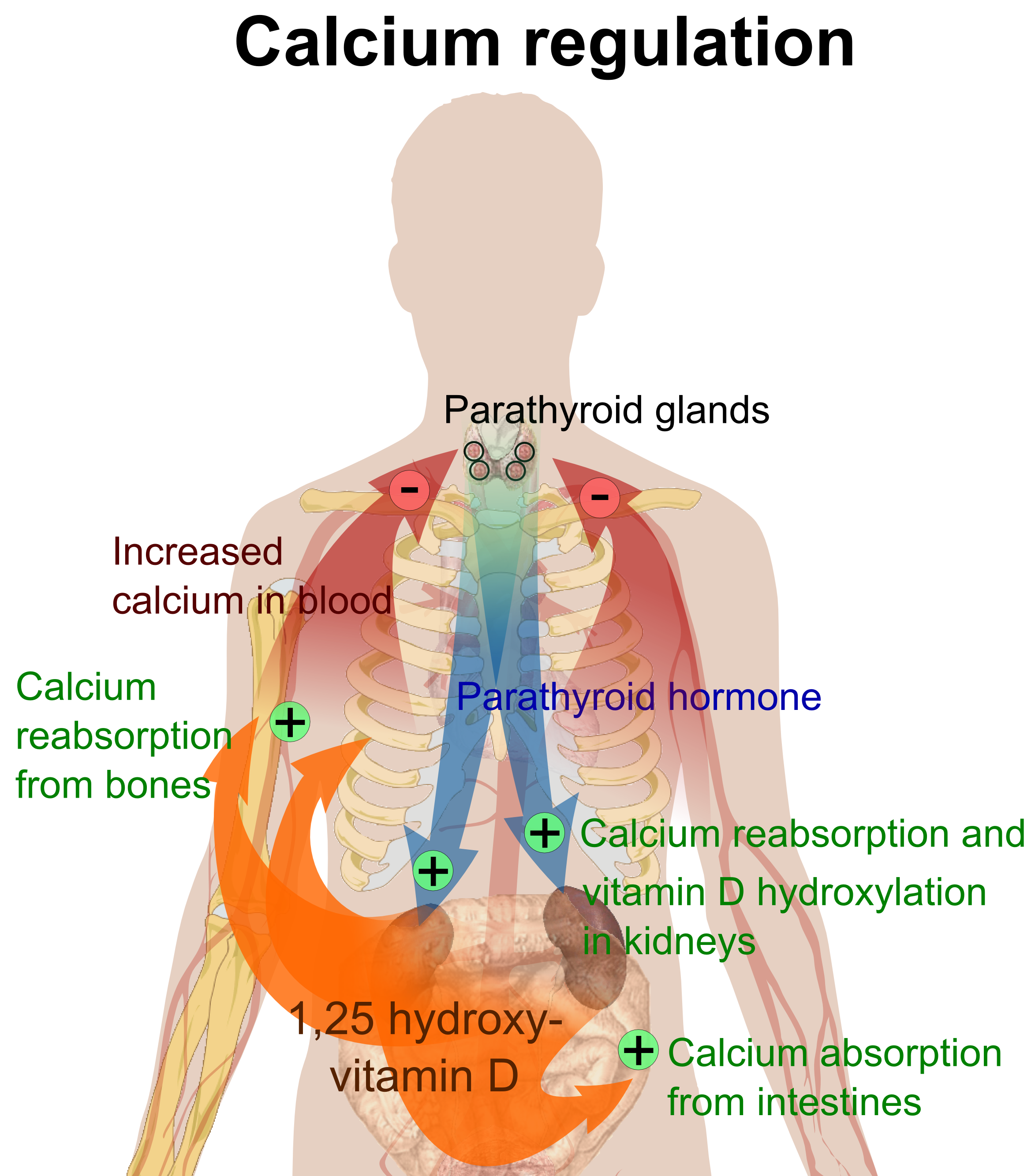
within narrow limits. The level of the calcium in plasma is regulated by the hormones parathyroid hormone (PTH) and calcitonin
Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the ...
. PTH is released by the chief cells of the parathyroid glands when the plasma calcium level falls below the normal range in order to raise it; calcitonin is released by the parafollicular cells of the thyroid gland
The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans, it is a butterfly-shaped gland located in the neck below the Adam's apple. It consists of two connected lobes. The lower two thirds of the lobes are connected by ...
when the plasma level of calcium is above the normal range in order to lower it.
Body compartment content
Calcium is the most abundant mineral in thehuman body
The human body is the entire structure of a Human, human being. It is composed of many different types of Cell (biology), cells that together create Tissue (biology), tissues and subsequently Organ (biology), organs and then Organ system, org ...
. The average adult body contains in total approximately 1 kg, 99% in the skeleton in the form of calcium phosphate salts. The extracellular fluid (ECF) contains approximately 22 mmol, of which about 9 mmol is in the plasma. Approximately 10 mmol of calcium is exchanged between bone and the ECF over a period of twenty-four hours.
Blood concentration
The concentration of calcium ions inside cells (in theintracellular fluid
The human body and even its individual body fluids may be conceptually divided into various fluid compartments, which, although not literally fascial compartment, anatomic compartments, do represent a real division in terms of how portions of the ...
) is more than 7,000 times lower than in the blood plasma (i.e. at <0.0002 mmol/L, compared with 1.4 mmol/L in the plasma)
Normal plasma levels
The plasma ''total calcium'' concentration is in the range of 2.2–2.6 mmol/L (9–10.5 mg/dL), and the normal ''ionized calcium'' is 1.3–1.5 mmol/L (4.5–5.6 mg/dL). The amount of total calcium in the blood varies with the level of plasma albumin, the most abundant protein in plasma, and therefore the main carrier of protein-bound calcium in the blood. The biologic effect of calcium is, however, determined by the amount of ''ionized calcium'', rather than the total calcium. It is therefore the plasmaionized
Ionization or ionisation is the process by which an atom or a molecule acquires a negative or positive charge by gaining or losing electrons, often in conjunction with other chemical changes. The resulting electrically charged atom or molecule i ...
calcium level which is tightly regulated to remain within very narrow limits by homeostatic negative feedback
Negative feedback (or balancing feedback) occurs when some function (Mathematics), function of the output of a system, process, or mechanism is feedback, fed back in a manner that tends to reduce the fluctuations in the output, whether caused ...
systems.
Between 35 and 50% of the calcium in plasma is protein-bound, and 5–10% is in the form of complexes with organic acids and phosphates. The remainder (50–60%) is ionized. The ionized calcium can be determined directly by colorimetry, or it can be read off from nomogram
A nomogram (), also called a nomograph, alignment chart, or abac, is a graphical Analog computer, calculating device, a two-dimensional diagram designed to allow the approximate graphical computation of a Function (mathematics), mathematical fu ...
s, though the usefulness of the latter is limited when the pH and protein content of the plasma deviate widely from the normal.
Function
Calcium has several main functions in the body.Bound to serum proteins
It readily binds to proteins, particularly those with amino acids whose side chains terminate in carboxyl (-COOH) groups (e.g. glutamate residues). When such binding occurs the electrical charges on the protein chain change, causing the protein's tertiary structure (i.e. 3-dimensional form) to change. Good examples of this are several of the clotting factors in the blood plasma, which are functionless in the absence of calcium ions, but become fully functional on the addition of the correct concentration of calcium salts.Voltage gated sodium channels
The voltage gated sodium ion channels in the cell membranes of nerves and muscle are particularly sensitive to the calcium ion concentration in the plasma. Relatively small decreases in the plasma ionized calcium levels (hypocalcemia
Hypocalcemia is a medical condition characterized by low calcium levels in the blood serum. The normal range of blood calcium is typically between 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), while levels less than 2.1 ...
) cause these channels to leak sodium into the nerve cells or axons, making them hyper-excitable ( positive bathmotropic effect), thus causing spontaneous muscle spasms ( tetany) and paraesthesia
Paresthesia is a sensation of the skin that may feel like numbness (''hypoesthesia''), tingling, pricking, chilling, or burning. It can be temporary or chronic and has many possible underlying causes. Paresthesia is usually painless and can oc ...
(the sensation of "pins and needles") of the extremities and round the mouth. When the plasma ionized calcium rises above normal (hypercalcemia
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range for total calcium is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L def ...
) more calcium is bound to these sodium channels having a negative bathmotropic effect on them, causing lethargy, muscle weakness, anorexia, constipation and labile emotions.
Intracellular signalling
Because the intracellular calcium ion concentration is extremely low (see above) the entry of minute quantities of calcium ions from the endoplasmic reticulum or from the extracellular fluids, cause rapid, very marked, and readily reversible changes in the relative concentration of these ions in thecytosol
The cytosol, also known as cytoplasmic matrix or groundplasm, is one of the liquids found inside cells ( intracellular fluid (ICF)). It is separated into compartments by membranes. For example, the mitochondrial matrix separates the mitochondri ...
. This can therefore serve as a very effective intracellular signal (or "second messenger
Second messengers are intracellular signaling molecules released by the cell in response to exposure to extracellular signaling molecules—the first messengers. (Intercellular signals, a non-local form of cell signaling, encompassing both first m ...
") in a variety of circumstances, including muscle contraction
Muscle contraction is the activation of Tension (physics), tension-generating sites within muscle cells. In physiology, muscle contraction does not necessarily mean muscle shortening because muscle tension can be produced without changes in musc ...
, the release of hormones (e.g. insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the insulin (''INS)'' gene. It is the main Anabolism, anabolic hormone of the body. It regulates the metabol ...
from the beta cells in the pancreatic islets
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine (hormone-producing) cells, discovered in 1869 by German pathological anatomist Paul Langerhans. The pancreatic islets constitute 1–2% o ...
) or neurotransmitters (e.g. acetylcholine
Acetylcholine (ACh) is an organic compound that functions in the brain and body of many types of animals (including humans) as a neurotransmitter. Its name is derived from its chemical structure: it is an ester of acetic acid and choline. Par ...
from pre-synaptic terminals of nerves) and other functions.
Bone
Calcium acts structurally as supporting material in bones as calcium hydroxyapatite (Ca10(PO4)6(OH)2).Muscle
Inskeletal
A skeleton is the structural frame that supports the body of most animals. There are several types of skeletons, including the exoskeleton, which is a rigid outer shell that holds up an organism's shape; the endoskeleton, a rigid internal fram ...
and heart muscle, calcium ions, released from the sarcoplasmic reticulum (the endoplasmic reticulum
The endoplasmic reticulum (ER) is a part of a transportation system of the eukaryote, eukaryotic cell, and has many other important functions such as protein folding. The word endoplasmic means "within the cytoplasm", and reticulum is Latin for ...
of striated muscles), bind to the troponin C
Troponin C is a protein which is part of the troponin complex. It contains four calcium-binding EF hands, although different isoforms may have fewer than four functional calcium-binding subdomains. It is a component of thin filaments, along ...
protein present on the actin
Actin is a family of globular multi-functional proteins that form microfilaments in the cytoskeleton, and the thin filaments in muscle fibrils. It is found in essentially all eukaryotic cells, where it may be present at a concentration of ...
-containing thin filaments of the myofibril
A myofibril (also known as a muscle fibril or sarcostyle) is a basic rod-like organelle of a muscle cell. Skeletal muscles are composed of long, tubular cells known as Skeletal muscle#Skeletal muscle cells, muscle fibers, and these cells contain ...
s. The troponin's 3D structure changes as a result, causing the tropomyosin
Tropomyosin is a two-stranded alpha-helical, coiled coil protein found in many animal and fungal cells. In animals, it is an important component of the muscular system which works in conjunction with troponin to regulate muscle contraction. It ...
to which it is attached to be rolled away from the myosin
Myosins () are a Protein family, family of motor proteins (though most often protein complexes) best known for their roles in muscle contraction and in a wide range of other motility processes in eukaryotes. They are adenosine triphosphate, ATP- ...
-binding sites on the actin molecules that form the back-bone of the thin filaments. Myosin
Myosins () are a Protein family, family of motor proteins (though most often protein complexes) best known for their roles in muscle contraction and in a wide range of other motility processes in eukaryotes. They are adenosine triphosphate, ATP- ...
can then bind to the exposed myosin-binding sites on the thin filament, to undergo a repeating series of conformational changes called the cross-bridge cycle, for which ATP provides the energy. During the cycle, each myosin protein ‘paddles’ along the thin actin filament, repeatedly binding to myosin-binding sites along the actin filament, ratcheting and letting go. In effect, the thick filament moves or slides along the thin filament, resulting in muscle contraction
Muscle contraction is the activation of Tension (physics), tension-generating sites within muscle cells. In physiology, muscle contraction does not necessarily mean muscle shortening because muscle tension can be produced without changes in musc ...
. This process is known as the sliding filament model
Sliding may refer to:
* Sliding (dance), also floating or gliding, a group of footwork-oriented dance techniques
* Slide (baseball), an attempt by a baseball runner to avoid getting tagged out
* Sliding (motion)
See also
* Slide (disambiguation)
...
of muscle contraction.
Sources
Not all the calcium in the diet can be readily absorbed from the gut. The calcium that is most readily absorbed is found in dairy products (72%), vegetables (7%), grains (5%), legumes (4%), fruit (3%), protein (3%). The calcium contained in vegetable matter is often complexed with phytates, oxalates,citrate
Citric acid is an organic compound with the formula . It is a colorless weak organic acid. It occurs naturally in citrus fruits. In biochemistry
Biochemistry, or biological chemistry, is the study of chemical processes within and relati ...
and other organic acids, such as the long-chained fatty acids (e.g. palmitic acid
Palmitic acid (hexadecanoic acid in IUPAC nomenclature) is a fatty acid with a 16-carbon chain. It is the most common saturated fatty acid found in animals, plants and microorganisms.Gunstone, F. D., John L. Harwood, and Albert J. Dijkstra. The ...
), with which calcium binds to form insoluble calcium soaps.
Bone storage
Calcium flow to and from thebone
A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, ...
may be positive, negative, or neutral. When it is neutral, about 5–10 mmol is turned over a day. Bone serves as an important storage point for calcium, as it contains 99% of the total body calcium. Calcium release from bone is regulated by parathyroid hormone in conjunction with calcitriol
Calcitriol is a hormone and the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the exp ...
manufactured in the kidney under the influence of PTH. Calcitonin
Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the ...
(a hormone secreted by the thyroid gland when plasma ionized calcium levels are high or rising; not to be confused with "calcitriol" which is manufactured in the kidney) stimulates incorporation of calcium into bone.
Intestinal absorption
The normal adult diet contains about 25 mmol of calcium per day. Only about 5 mmol of this is absorbed into the body per day (see below).Barrett KE, Barman SM, Boitano S, Brooks H, "Chapter 23. Hormonal Control of Calcium & Phosphate Metabolism & the Physiology of Bone" (Chapter). Barrett KE, Barman SM, Boitano S, Brooks H: Ganong's Review of Medical Physiology, 23e: http://www.accessmedicine.com/content.aspx?aID=5244785 . Calcium is absorbed across the intestinal epithelial cell'sbrush border
A brush border (striated border or brush border membrane) is the microvillus-covered surface of simple cuboidal and simple columnar epithelium found in different parts of the body. Microvilli are approximately 100 nanometers in diameter and th ...
membrane. The TRPV6 channel was proposed to be the major player in intestinal Ca2+ uptake. However, ''Trpv6'' KO mice did not display significant reduction of serum calcium levels and showed only slightly reduced or even unchanged intestinal Ca2+ absorption, indicating that other absorption pathways must exist. Recently, TRPM7 was linked to intestinal calcium uptake. The authors could show that intestinal deletion of TRPM7 results in strongly reduced calcium levels in serum and bones, and intensively increased levels of calcitriol
Calcitriol is a hormone and the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the exp ...
and PTH, indicating that TRPM7 is essential for the intestinal bulk uptake of calcium. After the cellular uptake, calcium is immediately bound to calbindin
Calbindins are three different calcium-binding proteins: calbindin 1, calbindin, calretinin and S100G. They were originally described as vitamin D-dependent calcium-binding proteins in the intestine and kidney of chicks and mammals. They are now ...
, a vitamin D-dependent calcium-binding protein
Calbindins are three different calcium-binding proteins: calbindin, calretinin and S100G. They were originally described as vitamin D-dependent calcium-binding proteins in the intestine and kidney of chicks and mammals. They are now classified ...
. Calbindin transfers the calcium directly into the epithelial cell's endoplasmic reticulum
The endoplasmic reticulum (ER) is a part of a transportation system of the eukaryote, eukaryotic cell, and has many other important functions such as protein folding. The word endoplasmic means "within the cytoplasm", and reticulum is Latin for ...
, through which the calcium is transferred to the basal membrane on the opposite side of the cell, without entering its cytosol
The cytosol, also known as cytoplasmic matrix or groundplasm, is one of the liquids found inside cells ( intracellular fluid (ICF)). It is separated into compartments by membranes. For example, the mitochondrial matrix separates the mitochondri ...
or intracellular fluid. From there calcium pumps ( PMCA1) actively transport calcium into the body. Active transport of calcium occurs primarily in the duodenum
The duodenum is the first section of the small intestine in most vertebrates, including mammals, reptiles, and birds. In mammals, it may be the principal site for iron absorption.
The duodenum precedes the jejunum and ileum and is the shortest p ...
portion of the intestine when calcium intake is low; and through passive paracellular transport
Paracellular transport refers to the transfer of substances across an epithelium by passing through the intercellular space ''between'' the cells. It is in contrast to transcellular transport, where the substances travel ''through'' the cell, pas ...
in the jejunum
The jejunum is the second part of the small intestine in humans and most higher vertebrates, including mammals, reptiles, and birds. Its lining is specialized for the absorption by enterocytes of small nutrient molecules which have been pr ...
and ileum
The ileum () is the final section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In fish, the divisions of the small intestine are not as clear and the terms posterior intestine or distal intestine may ...
parts when calcium intake is high, independently of Vitamin D level.
calcitriol
Calcitriol is a hormone and the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the exp ...
(or 1,25 dihydroxycholecalciferol, or 1,25 dihydroxyvitamin D3) concentration in the blood. Calcitriol is a cholesterol derivative. Under the influence of ultraviolet light on the skin, cholesterol is converted to previtamin D3 which spontaneously isomerizes to vitamin D3 (or cholecalciferol). It is then converted from cholecalciferol to calcifediol in the liver. Under the influence of parathyroid hormone, the kidneys
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and right in the retro ...
convert calcifediol into the active hormone calcitriol, which acts on the epithelial cells (enterocyte
Enterocytes, or intestinal absorptive cells, are simple columnar epithelial cells which line the inner surface of the small and large intestines. A glycocalyx surface coat contains digestive enzymes. Microvilli on the apical surface increase ...
s) lining the small intestine to increase the rate of absorption of calcium from the intestinal contents. In short the cycle is following:
: 7-Dehydrocholesterol Previtamin D3 Vitamin D3 Calcifediol Calcitriol
Calcitriol is a hormone and the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the exp ...
Low PTH levels in the blood (which occur under physiological conditions when the plasma ionized calcium levels are high) inhibit the conversion of cholecalciferol into calcitriol, which in turn inhibits calcium absorption from the gut. The opposite happens when the plasma ionized calcium levels are low: parathyroid hormone is secreted into the blood and the kidneys convert more calcifediol into the active calcitriol, increasing calcium absorption from the gut.Stryer L. ''Biochemistry'' (Fourth Edition). Chapter 27 "Vitamin D is derived from cholesterol by the ring-splitting action of light". New York, W.H. Freeman and Company.
Reabsorption
Intestine
Since about 15 mmol of calcium is excreted into the intestine via the bile per day, the total amount of calcium that reaches the duodenum and jejunum each day is about 40 mmol (25 mmol from the diet plus 15 mmol from the bile), of which, on average, 20 mmol is absorbed (back) into the blood. The net result is that about 5 mmol more calcium is absorbed from the gut than is excreted into it via the bile. If there is no active bone building (as in childhood), or increased need for calcium during pregnancy and lactation, the 5 mmol calcium that is absorbed from the gut makes up for urinary losses that are only partially regulated.Barrett KE, Barman SM, Boitano S, Brooks H, "Chapter 23. Hormonal Control of Calcium & Phosphate Metabolism & the Physiology of Bone" (Chapter). Barrett KE, Barman SM, Boitano S, Brooks H: Ganong's Review of Medical Physiology, 23e: http://www.accessmedicine.com/content.aspx?aID=5244785 .Kidneys
Thekidney
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organ (anatomy), organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and rig ...
s filter 250 mmol of calcium ions a day in pro-urine (or glomerular filtrate), and resorbs 245 mmol, leading to a net average loss in the urine of about 5 mmol/d. The quantity of calcium ions excreted in the urine per day is partially under the influence of the plasma parathyroid hormone (PTH) level - high levels of PTH decreasing the rate of calcium ion excretion, and low levels increasing it.The main determinant of the amount of calcium excreted into the urine per day is the plasma ionized calcium concentration. The plasma parathyroid hormone (PTH) concentration only increases or decreases the amount of calcium excreted at any ''given plasma ionized calcium concentration''. Thus, in primary hyperparathyroidism
Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands ( primary hyperparathyroidism) or as response to external stimuli ( secondary hyperparathyroi ...
the quantity of calcium excreted in the urine per day is ''increased'' despite the high levels of PTH in the blood. This is because hyperparathyroidism results in hypercalcemia
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range for total calcium is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L def ...
, which increases the urinary calcium concentration ( hypercalcuria) despite the modestly increased rate of calcium re-absorption from the renal tubules caused by PTH's effect on those tubules. Kidney stones
Kidney stone disease (known as nephrolithiasis, renal calculus disease, or urolithiasis) is a crystallopathy and occurs when there are too many minerals in the urine and not enough liquid or hydration. This imbalance causes tiny pieces of cr ...
are therefore often a first indication of hyperparathyroidism, especially since the hypercalcuria is accompanied by an increase in urinary phosphate excretion (a direct result of the high plasma PTH levels). Together the calcium and phosphate tend to precipitate out as water-insoluble salts, which readily form solid “stones”. However, parathyroid hormone has a greater effect on the quantity of phosphate ions (HPO42−) excreted in the urine. Phosphates form insoluble salts in combination with calcium ions. High concentrations of HPO42− in the plasma, therefore, lower the ionized calcium level in the extra-cellular fluids. Thus, the excretion of more phosphate than calcium ions in the urine raises the plasma ionized calcium level, even though the total calcium concentration might be lowered.
The kidney influences the plasma ionized calcium concentration in yet another manner. It processes vitamin D
Vitamin D is a group of structurally related, fat-soluble compounds responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, along with numerous other biological functions. In humans, the most important compo ...
3 into calcitriol
Calcitriol is a hormone and the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the exp ...
, the active form that is most effective in promoting the intestinal absorption of calcium. This conversion of vitamin D3 into calcitriol, is also promoted by high plasma parathyroid hormone levels.Stryer L. ''Biochemistry'' (Fourth Edition). Chapter 27 "Vitamin D is derived from cholesterol by the ring-splitting action of light". New York, W.H. Freeman and Company.
Excretion
Intestine
Most excretion of excess calcium is via the bile and feces, because the plasma calcitriol levels (which ultimately depend on the plasma calcium levels) regulate how much of the biliary calcium is reabsorbed from the intestinal contents.Kidneys
Urinary excretion of calcium is normally about 5 mmol (200 mg) /day. This is less in comparison to what is excreted via the feces (15 mmol/day).Regulation
 The plasma ionized calcium concentration is regulated within narrow limits (1.3–1.5 mmol/L). This is achieved by both the parafollicular cells of the thyroid gland, and the parathyroid glands constantly sensing (i.e. measuring) the concentration of calcium ions in the blood flowing through them.
The plasma ionized calcium concentration is regulated within narrow limits (1.3–1.5 mmol/L). This is achieved by both the parafollicular cells of the thyroid gland, and the parathyroid glands constantly sensing (i.e. measuring) the concentration of calcium ions in the blood flowing through them.
High plasma level
When the concentration of calcium rises, the parafollicular cells of the thyroid gland increase their secretion ofcalcitonin
Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the ...
, a polypeptide hormone, into the blood. At the same time, the parathyroid glands reduce the secretion of parathyroid hormone (PTH), also a polypeptide hormone, into the blood. The resulting high levels of calcitonin in the blood stimulate osteoblast
Osteoblasts (from the Greek combining forms for " bone", ὀστέο-, ''osteo-'' and βλαστάνω, ''blastanō'' "germinate") are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts fu ...
s in bone to remove calcium from blood plasma and deposit it as bone.
The reduced levels of PTH inhibit removal of calcium from the skeleton. The low levels of PTH have several other effects: there is increased loss of calcium in the urine, but more importantly, the loss of phosphate ions through urine is inhibited. Phosphate ions will therefore be retained in the plasma where they form insoluble salts with calcium ions, thereby removing them from the ionized calcium pool in the blood. The low levels of PTH also inhibit the formation of calcitriol
Calcitriol is a hormone and the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the exp ...
(not to be confused with calcitonin
Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the ...
) from cholecalciferol (vitamin D3) by the kidneys.
The reduction in the blood calcitriol concentration acts (comparatively slowly) on the epithelial cells (enterocytes
Enterocytes, or intestinal absorptive cells, are simple columnar epithelial cells which line the inner surface of the small and large intestines. A glycocalyx surface coat contains digestive enzymes. Microvilli on the apical surface increase i ...
) of the duodenum, inhibiting their ability to absorb calcium from the intestinal contents.Guyton A (1976). ‘’Medical Physiology’’. p.1062; New York, Saunders and Co. The low calcitriol levels also act on bone causing the osteoclast
An osteoclast () is a type of bone cell that breaks down bone tissue. This function is critical in the maintenance, repair, and bone remodeling, remodeling of bones of the vertebrate, vertebral skeleton. The osteoclast disassembles and digests th ...
s to release fewer calcium ions into the blood plasma.

Low plasma level
When the plasma ionized calcium level is low or falls the opposite happens. Calcitonin secretion is inhibited and PTH secretion is stimulated, resulting in calcium being removed from bone to rapidly correct the plasma calcium level. The high plasma PTH levels inhibit calcium loss via the urine while stimulating the excretion of phosphate ions via that route. They also stimulate the kidneys to manufacture calcitriol (a steroid hormone), which enhances the ability of the cells lining the gut to absorb calcium from the intestinal contents into the blood, by stimulating the production ofcalbindin
Calbindins are three different calcium-binding proteins: calbindin 1, calbindin, calretinin and S100G. They were originally described as vitamin D-dependent calcium-binding proteins in the intestine and kidney of chicks and mammals. They are now ...
in these cells. The PTH stimulated production of calcitriol also causes calcium to be released from bone into the blood, by the release of RANKL
Receptor activator of nuclear factor kappa- ligand (RANKL), also known as tumor necrosis factor ligand superfamily member 11 (TNFSF11), TNF-related activation-induced cytokine (TRANCE), osteoprotegerin ligand (OPGL), and osteoclast differentiat ...
(a cytokine
Cytokines () are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling.
Cytokines are produced by a broad range of cells, including immune cells like macrophages, B cell, B lymphocytes, T cell, T lymphocytes ...
, or local hormone) from the osteoblast
Osteoblasts (from the Greek combining forms for " bone", ὀστέο-, ''osteo-'' and βλαστάνω, ''blastanō'' "germinate") are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts fu ...
s which increases the bone resorptive activity by the osteoclasts. These are, however, relatively slow processes
Thus fast short term regulation of the plasma ionized calcium level primarily involves rapid movements of calcium into or out of the skeleton. Long term regulation is achieved by regulating the amount of calcium absorbed from the gut or lost via the feces.
Disorders
Hypocalcemia
Hypocalcemia is a medical condition characterized by low calcium levels in the blood serum. The normal range of blood calcium is typically between 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), while levels less than 2.1 ...
(low blood calcium) and hypercalcemia
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range for total calcium is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L def ...
(high blood calcium) are both serious medical disorders. Osteoporosis
Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to more porous bone, and consequent increase in Bone fracture, fracture risk.
It is the most common reason f ...
, osteomalacia
Osteomalacia is a disease characterized by the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D, or because of resorption of calcium. The impairment of b ...
and rickets
Rickets, scientific nomenclature: rachitis (from Greek , meaning 'in or of the spine'), is a condition that results in weak or soft bones in children and may have either dietary deficiency or genetic causes. Symptoms include bowed legs, stun ...
are bone disorders linked to calcium metabolism disorders and effects of vitamin D
Vitamin D is a group of structurally related, fat-soluble compounds responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, along with numerous other biological functions. In humans, the most important compo ...
. Renal osteodystrophy is a consequence of chronic kidney failure
Chronic kidney disease (CKD) is a type of long-term kidney disease, defined by the sustained presence of abnormal kidney function and/or abnormal kidney structure. To meet criteria for CKD, the abnormalities must be present for at least three mo ...
related to the calcium metabolism.
A diet adequately rich in calcium may reduce calcium loss from bone with advancing (post- menopausal) age. A low dietary calcium intake may be a risk factor in the development of osteoporosis
Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to more porous bone, and consequent increase in Bone fracture, fracture risk.
It is the most common reason f ...
in later life; and a diet with sustained adequate amounts of calcium may reduce the risk of osteoporosis.
Research
The role that calcium might have in reducing the rates of colorectal cancer has been the subject of many studies. However, given its modest efficacy, there is no current medical recommendation to use calcium for cancer reduction.See also
* European Calcium SocietyFootnotes
References
External links
Calcium
at Lab Tests Online * {{DEFAULTSORT:Calcium Metabolism Physiology Calcium Human homeostasis Endocrine system