2012 outbreak of Salmonella on:
[Wikipedia]
[Google]
[Amazon]
The 2012 outbreak of Salmonella took place in 15 places worldwide with over 2,300 strains identified.
In general, the
Estes Hatchery
located in Springfield, Missouri. This outbreak resulted in one casualty. One month later (March 2012), 46 people in the United States were infected with ''Salmonella'' Hadar through contact with live poultry. There were no deaths, and the infected humans were located in 11 different states. The specific hatchery name is withheld, but it was concluded by the CDC that this strain of ''Salmonella'' originated in one unnamed hatchery in Idaho. In the same month, one of three strains of ''Salmonella'' – Infantis, Newport, or Lille – were contracted by 195 people from contact with live poultry (whether for purposes of agriculture or pet keeping). Of those infected, two died from infection. This particular outbreak, though stemming from only the Mt. Healthy Hatchery in Ohio, expanded across 27 states.
 East Coast tomatoes tend to have higher rates of ''Salmonella'' infection than West Coast tomatoes. This seems to be due to the
East Coast tomatoes tend to have higher rates of ''Salmonella'' infection than West Coast tomatoes. This seems to be due to the
 The various outbreaks of ''Salmonella'' serotypes in the U.S. and abroad began at different points either in late 2011 or early 2012; however, all cases were concluded at the end of 2012. Those who were infected either persisted through the symptoms or expired from ''Salmonella''s destruction to their immune system. If there was a specific point of origin for an outbreak, a recall of the product helped to decrease more possible exposure. None of the people infected showed symptoms or maintained symptoms into 2013. This biotic disturbance had a major impact on society. It increased awareness about the ease in which bacteria spread among organisms. It helped to prompt researchers to look into ways to prevent crops from becoming contaminated in the field. Most importantly, this disturbance has been occurring with increasing frequency, which seems counter-intuitive because salmonellosis is an easily preventable disease; if simple food safety steps were taken, unnecessary hospitalizations and deaths could have been eliminated in 2012.
In order to prevent serious outbreaks similar to the one in 2012 in the future, some precautions must be taken. When handling food, one must be careful not to cross-contaminate raw poultry products or other meats with other foods. Anyone handling food should also be sure to wash their hands frequently. All persons should wash their hands after using the restroom as bacteria can survive for long periods of time outside of the body and the bacteria will be spread from the unwashed hands to possible food items or anything that may enter the mouth area. When cooking, one should take care to heat foods to at least 167 °F for a minimum of ten minutes to ensure that the entire product is evenly cooked. This is because heat and ultraviolet radiation are good neutralizers of ''Salmonella'' bacterium.
Recent outbreaks have occurred, and although not all infections can be eliminated, most can be hindered either through coating crops with ''Salmonella''-fighting bacteria or through human precautions.
The various outbreaks of ''Salmonella'' serotypes in the U.S. and abroad began at different points either in late 2011 or early 2012; however, all cases were concluded at the end of 2012. Those who were infected either persisted through the symptoms or expired from ''Salmonella''s destruction to their immune system. If there was a specific point of origin for an outbreak, a recall of the product helped to decrease more possible exposure. None of the people infected showed symptoms or maintained symptoms into 2013. This biotic disturbance had a major impact on society. It increased awareness about the ease in which bacteria spread among organisms. It helped to prompt researchers to look into ways to prevent crops from becoming contaminated in the field. Most importantly, this disturbance has been occurring with increasing frequency, which seems counter-intuitive because salmonellosis is an easily preventable disease; if simple food safety steps were taken, unnecessary hospitalizations and deaths could have been eliminated in 2012.
In order to prevent serious outbreaks similar to the one in 2012 in the future, some precautions must be taken. When handling food, one must be careful not to cross-contaminate raw poultry products or other meats with other foods. Anyone handling food should also be sure to wash their hands frequently. All persons should wash their hands after using the restroom as bacteria can survive for long periods of time outside of the body and the bacteria will be spread from the unwashed hands to possible food items or anything that may enter the mouth area. When cooking, one should take care to heat foods to at least 167 °F for a minimum of ten minutes to ensure that the entire product is evenly cooked. This is because heat and ultraviolet radiation are good neutralizers of ''Salmonella'' bacterium.
Recent outbreaks have occurred, and although not all infections can be eliminated, most can be hindered either through coating crops with ''Salmonella''-fighting bacteria or through human precautions.
United States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territori ...
alone experiences 1 million cases of salmonellosis
Salmonellosis, more commonly known as food poisoning is a symptomatic infection caused by bacteria of the ''Salmonella'' type. It is also a food-borne disease and are defined as diseases, usually either infectious or toxic in nature, caused
by a ...
per year. In Europe, although there are around 100,000 incidents of salmonellosis reported annually, there has been a steady decrease in cases over the past four years. The exact number of those infected is impossible to know as not all cases are reported. Of these reported cases, some can be classified as foodborne disease
Foodborne illness (also foodborne disease and food poisoning) is any illness resulting from the spoilage of contaminated food by pathogenic bacteria, viruses, or parasites that contaminate food,
as well as prions (the agents of mad cow disease) ...
outbreak
In epidemiology, an outbreak is a sudden increase in occurrences of a disease when cases are in excess of normal expectancy for the location or season. It may affect a small and localized group or impact upon thousands of people across an entire ...
s by the Centers for Disease Control and Prevention
The Centers for Disease Control and Prevention (CDC) is the national public health agency of the United States. It is a United States federal agency, under the Department of Health and Human Services, and is headquartered in Atlanta, Georgi ...
(CDC) if "two or more people get the same illness from the same contaminated food or drink" or zoonotic
A zoonosis (; plural zoonoses) or zoonotic disease is an infectious disease of humans caused by a pathogen (an infectious agent, such as a bacterium, virus, parasite or prion) that has jumped from a non-human (usually a vertebrate) to a human. ...
outbreaks if "two or more people get the same illness from the same pet or other animal". In 2012, the various strains or serotypes
A serotype or serovar is a distinct variation within a species of bacteria or virus or among immune cells of different individuals. These microorganisms, viruses, or cells are classified together based on their surface antigens, allowing the epi ...
of the '' Salmonella'' bacteria, related to the outbreaks in the United States, infected over 1800 people and killed seven. In Europe, the European Centre for Disease Prevention and Control (ECDC) reported 91,034 cases of ''Salmonella'' infection with 65,317 cases related to the 2012 outbreaks. Of those 65,317 cases, there were 61 deaths.
''Salmonella'' bacteria can be found in almost any product or animal that has been exposed to fecal matter. These exposures can occur from crops grown from waste-based fertilizers or from food items handled by infected humans. Salmonellosis is an intestinal disease, meaning that the bacteria must be ingested and processed through the intestines in order for infection to occur. Thus, salmonellosis is commonly spread to humans through ingestion of contaminated food items. It can also be spread through contact with reptiles and birds, usually after the person handles the animal or its environment (without hand-washing immediately) and then touches their mouth or food items. Those infected usually develop symptoms anywhere from 12 to 72 hours after first contact with ''Salmonella'' bacteria, and most do not require serious medical attention. This salmonellosis displays itself in humans with fever, abdominal pain, nausea, and, most commonly, diarrhea for a period of up to 7 days. Those requiring hospitalization usually are dehydrated or have extreme diarrhea, which can turn deadly, especially if the salmonella bacteria reaches the bloodstream. The elderly, young children, and those with weakened immune systems are most at risk for developing salmonellosis and having severe reactions. The most common serotypes of ''Salmonella'' in the United States and Europe are Enteritidis and Typhimurium.
Origins of outbreak
The 2012 outbreak did not have one start and end date due to the multivariate origination sites and stages of investigation. Each outbreak followed its own pattern of contamination, spread, infection, and containment throughout the course of 2012. Worldwide, there were 15 different foodborne and zoonotic origins of the ''Salmonella'' outbreaks. Eighteen of the over 2,300 strains of ''Salmonella'' were found in infected humans and contaminated products in Europe and the U.S. As with all diseases, there were certain places and serotypes that contributed more to the magnitude of the 2012 outbreak. As such, the origins listed below had the greatest frequency of occurrence and overall impact on society.Hedgehogs
''S''. Typhimurium has traditionally been an uncommon serotype of ''Salmonella''; however, beginning in January 2012 through the end of 2012, the number of cases steadily rose, with 18 human cases in the United States alone (spread among eight states). The infection caused one death and four hospitalizations. These infections stem from contact with pet hedgehogs or with the animals' surroundings. No one pet provider was linked to the infected hedgehogs.Feeder rodents
One epidemic of ''Salmonella enterica'' I 4,5,12:i:- in the United States in February 2012 affected 46 people across 22 states. The outbreak seemed to be linked to the handling of live or frozen feeder mice and rats for reptile and amphibian pets. A similar outbreak occurred in the United States and United Kingdom in 2009 and 2010 from the same two breeders implicated in this 2012 occurrence. Also, more than a third of those infected were young children, highlighting their propensity for infection.Live poultry
The outbreaks in 2012 that occurred due to contact with live poultry were of five different serotypes of ''Salmonella'' bacteria originating in three distinct locations. The first infections were reported in February 2012. Spanning 23 states, there were 93 humans infected with the Montevideo serotype of ''Salmonella''. All were infected with this strain from contact with baby ducklings or chicks from thEstes Hatchery
located in Springfield, Missouri. This outbreak resulted in one casualty. One month later (March 2012), 46 people in the United States were infected with ''Salmonella'' Hadar through contact with live poultry. There were no deaths, and the infected humans were located in 11 different states. The specific hatchery name is withheld, but it was concluded by the CDC that this strain of ''Salmonella'' originated in one unnamed hatchery in Idaho. In the same month, one of three strains of ''Salmonella'' – Infantis, Newport, or Lille – were contracted by 195 people from contact with live poultry (whether for purposes of agriculture or pet keeping). Of those infected, two died from infection. This particular outbreak, though stemming from only the Mt. Healthy Hatchery in Ohio, expanded across 27 states.
Small turtles
First investigated at the end of March 2012, there were a total of 84 cases of infected humans across 15 states of the United States by November 2012. These people's salmonellosis (either from ''Salmonella'' Sandiego or ''Salmonella'' Newport) stemmed from contact with small turtles or their habitats. Some of these turtles were purchased from street merchants. No one source of the ''Salmonella'' contaminations was identified, and no human deaths occurred. Due to past outbreaks, there is a law in place making it illegal to sell or own a turtle with a shell length less than four inches, as these seem to generally be the sources of most ''Salmonella'' bacteria in small turtles.Raw scraped ground tuna product
First reported in April 2012, an outbreak of salmonellosis caused by rarer serotypes, ''Salmonella'' Bareilly and ''Salmonella'' Nchanga, was reported in 28 states, mostly in the Eastern U.S., having caused no deaths, but 425 cases of illness and 55 hospitalizations. This outbreak was linked to the consumption of raw scraped ground tuna product. The source was frozen raw yellowfin tuna product aka Nakaochi Scrape manufactured by Moon Marine USA Corporation. This product was voluntarily recalled after theCDC
The Centers for Disease Control and Prevention (CDC) is the national public health agency of the United States. It is a United States federal agency, under the Department of Health and Human Services, and is headquartered in Atlanta, Georgi ...
discovered strains of ''Salmonella'' in the packages. The company eventually recalled another type of canned tuna for fear it may have been contaminated, too. This outbreak was significant in that it was the first salmonellosis case in the United States connected to raw, scraped tuna products, as well as being the first time ''S''. Nchanga was discovered in food products in the United States.
Smoked salmon
In July 2012, an outbreak of salmonellosis occurred in the Netherlands and the United States. According to theNational Institute for Public Health and the Environment
The National Institute for Public Health and the Environment ( nl, Rijksinstituut voor Volksgezondheid en Milieu or simply RIVM) is a Dutch research institute that is an independent agency of the Ministry of Health, Welfare and Sport.
RIVM perfo ...
, by the end of 2012, 1060 people in the Netherlands and 100 in the United States contracted salmonellosis from smoked salmon infected with ''Salmonella'' Thompson. On November 2, the RIVM
The National Institute for Public Health and the Environment ( nl, Rijksinstituut voor Volksgezondheid en Milieu or simply RIVM) is a Dutch research institute that is an independent agency of the Ministry of Health, Welfare and Sport.
RIVM perfo ...
confirmed that there were 4 deaths and over 1060 cases linked to ''S''. Thompson in the Netherlands. The infections were linked to smoked salmon from the manufacturer Foppen, where the contamination had occurred. A recall involving a quarter million customers was undertaken in the United States. The CDC did not classify this as an outbreak because there were not a verified number of people infected from only this source in the U.S.
Presence in agriculture
Contamination through defecation
Because animals are the main transporters of ''Salmonella'', crops can become infected. This generally occurs because of the use of manure-based fertilizers on farms. Some animals do not appear sick (especially infected poultry); however, they carry the ''Salmonella'' in their intestines and when they defecate, the bacteria spreads to the soil. Sometimes, the sick animals manifest the illness in ways similar to humans with similar consequences. They may have diarrhea, fever, and then die if they are not treated. After their death, the other animals raised with them can become infected through contact with their feces. Therefore, if this infected manure is used as a fertilizer for crops, then the crops will contain trace amounts of infectious ''Salmonella'' bacteria that can spread to humans after the crops are harvested. Poultry can become infected by living close together in hatcheries, where multiple animals are defecating. Some poultry are hatched to be sold domestically, while others are hatched for production to be consumed later. If live poultry are infected and sold domestically, they can infect other animals who may be around them in a domestic situation e.g. other pets. Because poultry do not show symptoms, infections are usually not obvious until humans or other animals in contact with the poultry become ill.Tomatoes
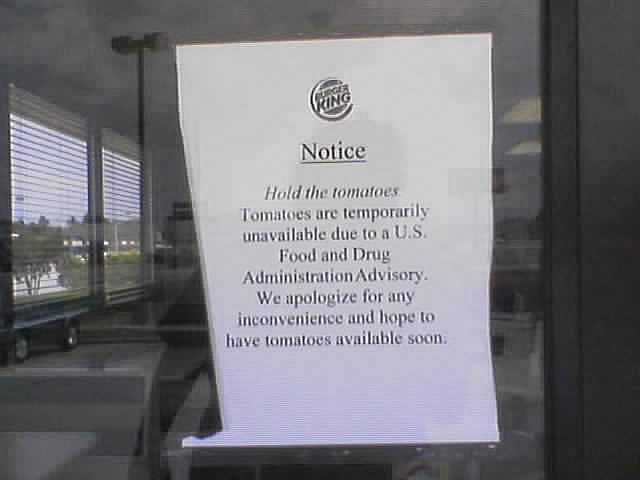
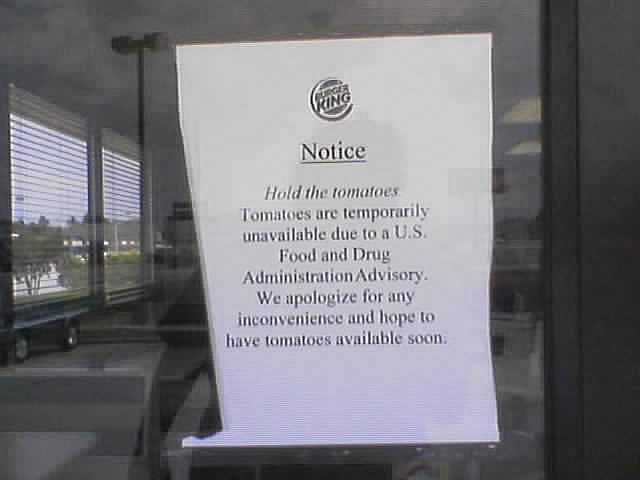 East Coast tomatoes tend to have higher rates of ''Salmonella'' infection than West Coast tomatoes. This seems to be due to the
East Coast tomatoes tend to have higher rates of ''Salmonella'' infection than West Coast tomatoes. This seems to be due to the microbiome
A microbiome () is the community of microorganisms that can usually be found living together in any given habitat. It was defined more precisely in 1988 by Whipps ''et al.'' as "a characteristic microbial community occupying a reasonably wel ...
of the East Coast of the United States, where there are far less soil bacteria that destroy ''Salmonella'' versus the microbiome of the West Coast where these bacteria are abundant. Because of the anti-salmonella bacteria limiting its spread, fewer people on the West Coast report cases of salmonellosis. Additionally, street-sold natural tomatoes have been consistently tied to outbreaks of ''Salmonella''. Street-sold (unregulated) items are independently produced and sold to consumers. This does not include fresh produce markets. These strong links to salmonellosis is in due in part do the lack of Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a List of United States federal agencies, federal agency of the United States Department of Health and Human Services, Department of Health and Human Services. The FDA is respon ...
(FDA) oversight on unregistered vendors. Another cause of ''Salmonella'' bacteria growth may be due to contact with contaminated irrigation water. The tomatoes (or any plant) are much more likely to become infected if the soil in which the roots are located are contaminated or if the actual blossom is contaminated. These two entry points lead to the most likely scenarios in which a healthy tomato plant may become infected with some serotype of ''Salmonella''.
End of 2012 outbreak and future prevention
 The various outbreaks of ''Salmonella'' serotypes in the U.S. and abroad began at different points either in late 2011 or early 2012; however, all cases were concluded at the end of 2012. Those who were infected either persisted through the symptoms or expired from ''Salmonella''s destruction to their immune system. If there was a specific point of origin for an outbreak, a recall of the product helped to decrease more possible exposure. None of the people infected showed symptoms or maintained symptoms into 2013. This biotic disturbance had a major impact on society. It increased awareness about the ease in which bacteria spread among organisms. It helped to prompt researchers to look into ways to prevent crops from becoming contaminated in the field. Most importantly, this disturbance has been occurring with increasing frequency, which seems counter-intuitive because salmonellosis is an easily preventable disease; if simple food safety steps were taken, unnecessary hospitalizations and deaths could have been eliminated in 2012.
In order to prevent serious outbreaks similar to the one in 2012 in the future, some precautions must be taken. When handling food, one must be careful not to cross-contaminate raw poultry products or other meats with other foods. Anyone handling food should also be sure to wash their hands frequently. All persons should wash their hands after using the restroom as bacteria can survive for long periods of time outside of the body and the bacteria will be spread from the unwashed hands to possible food items or anything that may enter the mouth area. When cooking, one should take care to heat foods to at least 167 °F for a minimum of ten minutes to ensure that the entire product is evenly cooked. This is because heat and ultraviolet radiation are good neutralizers of ''Salmonella'' bacterium.
Recent outbreaks have occurred, and although not all infections can be eliminated, most can be hindered either through coating crops with ''Salmonella''-fighting bacteria or through human precautions.
The various outbreaks of ''Salmonella'' serotypes in the U.S. and abroad began at different points either in late 2011 or early 2012; however, all cases were concluded at the end of 2012. Those who were infected either persisted through the symptoms or expired from ''Salmonella''s destruction to their immune system. If there was a specific point of origin for an outbreak, a recall of the product helped to decrease more possible exposure. None of the people infected showed symptoms or maintained symptoms into 2013. This biotic disturbance had a major impact on society. It increased awareness about the ease in which bacteria spread among organisms. It helped to prompt researchers to look into ways to prevent crops from becoming contaminated in the field. Most importantly, this disturbance has been occurring with increasing frequency, which seems counter-intuitive because salmonellosis is an easily preventable disease; if simple food safety steps were taken, unnecessary hospitalizations and deaths could have been eliminated in 2012.
In order to prevent serious outbreaks similar to the one in 2012 in the future, some precautions must be taken. When handling food, one must be careful not to cross-contaminate raw poultry products or other meats with other foods. Anyone handling food should also be sure to wash their hands frequently. All persons should wash their hands after using the restroom as bacteria can survive for long periods of time outside of the body and the bacteria will be spread from the unwashed hands to possible food items or anything that may enter the mouth area. When cooking, one should take care to heat foods to at least 167 °F for a minimum of ten minutes to ensure that the entire product is evenly cooked. This is because heat and ultraviolet radiation are good neutralizers of ''Salmonella'' bacterium.
Recent outbreaks have occurred, and although not all infections can be eliminated, most can be hindered either through coating crops with ''Salmonella''-fighting bacteria or through human precautions.
References
{{reflist, 30em Disease outbreaks in the Netherlands Disease outbreaks in the United States 2012 in the Netherlands Salmonella Salmonellosis Food safety scandals Food recalls 2012 disease outbreaks 2012 disasters in the Netherlands