local anesthetic nerve block on:
[Wikipedia]
[Google]
[Amazon]
 Local anesthetic nerve block (local anesthetic regional nerve blockade, or often simply nerve block) is a short-term nerve block involving the injection of
Local anesthetic nerve block (local anesthetic regional nerve blockade, or often simply nerve block) is a short-term nerve block involving the injection of


 Local anesthetic nerve block (local anesthetic regional nerve blockade, or often simply nerve block) is a short-term nerve block involving the injection of
Local anesthetic nerve block (local anesthetic regional nerve blockade, or often simply nerve block) is a short-term nerve block involving the injection of local anesthetic
A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general a ...
as close to the nerve
A nerve is an enclosed, cable-like bundle of nerve fibers (called axons) in the peripheral nervous system.
A nerve transmits electrical impulses. It is the basic unit of the peripheral nervous system. A nerve provides a common pathway for the ...
as possible for pain relief
Pain management is an aspect of medicine and health care involving relief of pain (pain relief, analgesia, pain control) in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professional ...
. The local anesthetic bathes the nerve and numbs the area of the body that is supplied by that nerve. The goal of the nerve block is to prevent pain by blocking the transmission of pain signals from the affected area. Nerve blocks have a number of uses including treating headache disorders and providing anesthesia during surgery. The pain relief
Pain management is an aspect of medicine and health care involving relief of pain (pain relief, analgesia, pain control) in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professional ...
provided by the block is present during the surgery and continues to last after the procedure. This can lead to a reduction in the amount of opiates
An opiate, in classical pharmacology, is a substance derived from opium. In more modern usage, the term ''opioid'' is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain (including antagonist ...
needed for pain control. The advantages of nerve blocks over general anesthesia
General anaesthesia (UK) or general anesthesia (US) is a medically induced loss of consciousness that renders the patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general ...
include faster recovery, monitored anesthesia care vs. intubation
Intubation (sometimes entubation) is a medical procedure involving the insertion of a tube into the body. Patients are generally anesthetized beforehand. Examples include tracheal intubation, and the balloon tamponade with a Sengstaken-Blake ...
with an airway tube, and much less postoperative pain.
Mechanism of action
Local anesthetics act on thevoltage-gated sodium channels
Sodium channels are integral membrane proteins that form ion channels, conducting sodium ions (Na+) through a cell's membrane. They belong to the superfamily of cation channels and can be classified according to the trigger that opens the chan ...
that conduct electrical impulses and mediate fast depolarization
In biology, depolarization or hypopolarization is a change within a cell, during which the cell undergoes a shift in electric charge distribution, resulting in less negative charge inside the cell compared to the outside. Depolarization is ess ...
along nerves. Local anesthetics also act on potassium channel
Potassium channels are the most widely distributed type of ion channel found in virtually all organisms. They form potassium-selective pores that span cell membranes. Potassium channels are found in most cell types and control a wide variety of c ...
s, but they block sodium channels more.
Lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lid ...
preferentially binds to the inactivated state of voltage-gated sodium channels, but has also been found to bind potassium channels, G protein-coupled receptor
G protein-coupled receptors (GPCRs), also known as seven-(pass)-transmembrane domain receptors, 7TM receptors, heptahelical receptors, serpentine receptors, and G protein-linked receptors (GPLR), form a large group of evolutionarily-related p ...
s, NMDA receptor
The ''N''-methyl-D-aspartate receptor (also known as the NMDA receptor or NMDAR), is a glutamate receptor and ion channel found in neurons. The NMDA receptor is one of three types of ionotropic glutamate receptors, the other two being AMPA and ...
s, and calcium channel
A calcium channel is an ion channel which shows selective permeability to calcium ions. It is sometimes synonymous with voltage-gated calcium channel, although there are also ligand-gated calcium channels.
Comparison tables
The following tables e ...
s ''in vitro
''In vitro'' (meaning in glass, or ''in the glass'') studies are performed with microorganisms, cells, or biological molecules outside their normal biological context. Colloquially called " test-tube experiments", these studies in biology a ...
''. The duration of the block is mostly influenced by the amount of time the anesthetic is near the nerve. Lipid solubility, blood flow in the tissue, and presence of vasoconstrictors with the anesthetic all play a role in this. A higher lipid solubility makes the anesthetic more potent and have a longer duration of action; however, it also increases the toxicity of the drug.
Complications
The most common complications of nerve blocks include bleeding, infection, and block failure. Local anesthetic toxicity, the most dangerous complication, is often first detected by symptoms of numbness and tingling around the mouth, metallic taste, or ringing in the ears. Additionally, it may lead to seizures, arrhythmias, and may progress to cardiac arrest. This reaction may stem from an allergy, excessive dose, or intravascular injection. Other complications include nerve injury which has an extremely low rate of 0.029-0.2%. Some research even suggests that ultrasound lowers the risk to 0.0037%. The use of ultrasound and nerve stimulation has greatly improved practitioners’ ability to safely administer nerve blocks. Nerve injury most often occurs fromischaemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems ...
, compression, direct neurotoxicity, needle laceration, and inflammation.
Common local anesthetics and adjuvants
Local anesthetics are broken down into two categories: ester-linked and amide-linked. The esters includebenzocaine
Benzocaine, sold under the brand name Orajel amongst others, is an ester local anesthetic commonly used as a topical pain reliever or in cough drops. It is the active ingredient in many over-the-counter anesthetic ointments such as products ...
, procaine, tetracaine, and chloroprocaine. The amides include lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lid ...
, mepivacaine, prilocaine, bupivacaine, ropivacaine, and levobupivacaine. Chloroprocaine is a short-acting drug (45–90 minutes), lidocaine and mepivacaine are intermediate duration (90–180 minutes), and bupivacaine, levobupivacaine, and ropivacaine are long-acting (4–18 hours). Drugs commonly used for peripheral nerve blocks include lidocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lid ...
, ropivacaine, bupivacaine, and mepivacaine. These drugs are often combined with adjuvants, drugs that boost the effect of each other, with the end goal of increasing the duration of the analgesia
Pain management is an aspect of medicine and health care involving relief of pain (pain relief, analgesia, pain control) in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professional ...
or shortening time of onset. Adjuvants may include epinephrine
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions (e.g., respiration). It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and ...
, clonidine
Clonidine, sold under the brand name Catapres among others, is an α2-adrenergic agonist medication used to treat high blood pressure, ADHD, drug withdrawal ( alcohol, opioids, or nicotine), menopausal flushing, diarrhea, spasticity, and c ...
, and dexmedetomidine. Vasoconstriction
Vasoconstriction is the narrowing of the blood vessels resulting from contraction of the muscular wall of the vessels, in particular the large arteries and small arterioles. The process is the opposite of vasodilation, the widening of blood vess ...
caused by local anesthetic may be further enhanced synergistically with the addition of epinephrine, the most widely used additive. Epinephrine increases the length of analgesic duration and decreases blood flow by acting as an agonist at the α1-adrenoceptor. Dexmedetomidine is not as widely used as epinephrine. Studies in humans indicate improved onset time and increased duration of analgesia.
Duration of nerve block
The duration of the nerve block depends on the type of local anesthetics used and the amount injected around the target nerve. There are short acting (45–90 minutes), intermediate duration (90–180 minutes), and long acting anesthetics (4–18 hours). Block duration can be prolonged with use of a vasoconstrictor such as epinephrine, which decreases the diffusion of the anesthetic away from the nerve. There are various types of nerve blocks currently performed. Therapeutic blocks may be used for acute pain patients, diagnostic blocks are used to find pain sources, prognostic blocks are used to determine subsequent pain management options, preemptive blocks minimize postoperative pain, and some blocks can be used in place of surgery. Certain surgeries may benefit from placing a catheter that stays in place for 2–3 days postoperatively. Catheters are indicated for some surgeries where the expected postoperative pain lasts longer than 15–20 hours. Pain medication can be injected through the catheter to prevent a spike in pain when the initial block wears off. Nerve blocks may also reduce the risk of developing persistent postoperative pain several months after surgery. Local anesthetic nerve blocks are sterile procedures that can be performed with the help of anatomical landmarks,ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies ...
, fluoroscopy
Fluoroscopy () is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a physician to see the internal structure and function ...
(a live X-ray), or CT. Use of any one of these imaging modalities enables the physician to view the placement of the needle. Electrical stimulation can also provide feedback on the proximity of the needle to the target nerve.
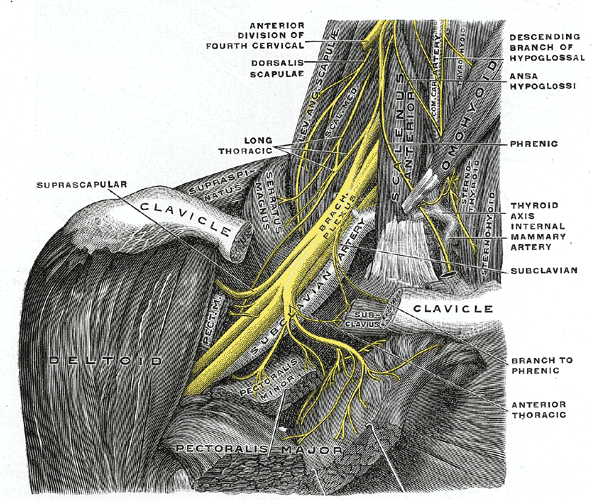
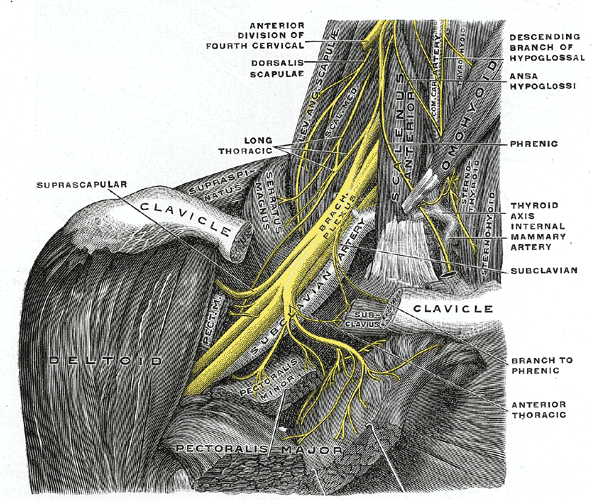
Upper extremity nerve blocks
The brachial plexus is a bundle of nerves innervating the shoulder and arm and can be blocked at different levels depending on the type of upper extremity surgery being performed. Interscalene brachial plexus blocks can be done before shoulder, arm, and elbow surgery. The interscalene block is done at the neck where the brachial plexus emerges between the anterior and middle scalene muscles. Lidocaine is injected first to numb the skin and then a blunt needle is used to protect the nerves from damage as the physician places the needle very close to the nerves. The needle goes in about 3–4 cm and a single shot of local anesthetic is injected or a catheter is placed. The most common local anesthetics used at the site of the nerves are bupivicaine, mepivicaine, and chloroprocaine. There is a very high chance that thephrenic nerve
The phrenic nerve is a mixed motor/sensory nerve which originates from the C3-C5 spinal nerves in the neck. The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. ...
, which innervates the diaphragm
Diaphragm may refer to:
Anatomy
* Thoracic diaphragm, a thin sheet of muscle between the thorax and the abdomen
* Pelvic diaphragm or pelvic floor, a pelvic structure
* Urogenital diaphragm or triangular ligament, a pelvic structure
Other
* Diap ...
, will be blocked so this block should only be done on patients who have use of their accessory respiratory muscles. The block may not affect the C8 and T1 roots which supply part of the hand, so it is usually not done for hand surgeries.
The supraclavicular and infraclavicular blocks can be performed for surgeries on the humerus
The humerus (; ) is a long bone in the arm that runs from the shoulder to the elbow. It connects the scapula and the two bones of the lower arm, the radius and ulna, and consists of three sections. The humeral upper extremity consists of a r ...
, elbow, and hand. These blocks are indicated for the same surgeries but they provide different views of the nerves, so it depends on the individual patient's anatomy to determine which block should be performed. A pneumothorax
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve i ...
is a risk with these blocks, so the pleura
The pulmonary pleurae (''sing.'' pleura) are the two opposing layers of serous membrane overlying the lungs and the inside of the surrounding chest walls.
The inner pleura, called the visceral pleura, covers the surface of each lung and dips b ...
should be checked with ultrasound to make sure the lung was not punctured during the block.
The axillary block is indicated for elbow, forearm, and hand surgery. It anesthetizes the median, ulnar, and radial nerves. This block is useful because it has less risk than the interscalene (spinal cord or vertebral artery puncture) or supraclavicular (pneumothorax) brachial plexus blocks.
Lower extremity nerve blocks
Fascia iliaca block is indicated for pain relief for hip fractures in adults and femoral fractures in children. It works by affecting the femoral, obturator and the lateral cutaneous nerves.3-in-1 nerve block
3-in-One Oil is a general-purpose lubricating oil sold for household and do-it-yourself use. It was originally formulated in 1894 for use on bicycles, and remains a popular lubricant for their chains. Its name, given by inventor George W. Cole o ...
is indicated for pain relief for hip fractures.
The femoral nerve block
A femoral nerve block is a nerve block that uses local anesthetic to achieve analgesia in the leg. The block works by affecting the femoral nerve.
A femoral nerve block (FNB) results in anesthesia of the skin and muscles of the anterior thigh an ...
is indicated for femur, anterior thigh, and knee surgery. It is performed slightly inferior to the inguinal ligament, and the nerve is under the fascia iliaca.
The sciatic nerve block is done for surgeries at or below the knee. The nerve is located in the gluteus maximus muscle. The popliteal block is done for ankle, achilles tendon, and foot surgery. It is done above the knee on the posterior leg where the sciatic nerve starts splitting into the common peroneal and tibial nerves.
The saphenous nerve block is often done in combination with the popliteal block for surgeries below the knee. The saphenous nerve is numbed at the medial part of the lower thigh under the sartorius muscle.
The lumbar plexus block is an advanced technique indicated for hip, anterior thigh, and knee surgery. The lumbar plexus is composed of nerves originating from L1 to L4 spinal roots such as the iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, femoral, and obturator nerves. Since the plexus is located deep, there is an increased risk of local anesthetic toxicity, so less toxic anesthetics like chloroprocaine or mepivacaine mixed with ropivacaine are often recommended. A curvilinear ultrasound probe can be used but it is often difficult to see the plexus, so a nerve stimulator is used to locate it.
Paravertebral nerve block
The paravertebral block is versatile and can be used for various surgeries depending on the vertebral level it is done. A block at the neck in the cervical region is useful for thyroid gland and carotid artery surgery. At the chest and abdomen in the thoracic region, blocks are used for breast, thoracic, and abdominal surgery. One of the first instances on using continuous paravertebral blockade in the body was by the thoracic team led by Sabanathan in Bradford. A block at the hip in the lumbar region is indicated for hip, knee, and anterior thigh surgeries. The paravertebral block provides unilateral analgesia, but bilateral blocks can be performed for abdominal surgeries. Since it is a unilateral block, it may be chosen over epidurals for patients who can't tolerate the hypotension that follows bilateral sympathectomy. The paravertebral space is located a couple centimeters lateral to the spinous process and is bounded posteriorly by the superior costotransverse ligament and anteriorly by the parietal pleura. Complications include pneumothorax, vascular puncture, hypotension, and pleural puncture.References
{{Reflist Regional anesthesia