Gestational Diabetes on:
[Wikipedia]
[Google]
[Amazon]
Gestational diabetes is a condition in which a woman without
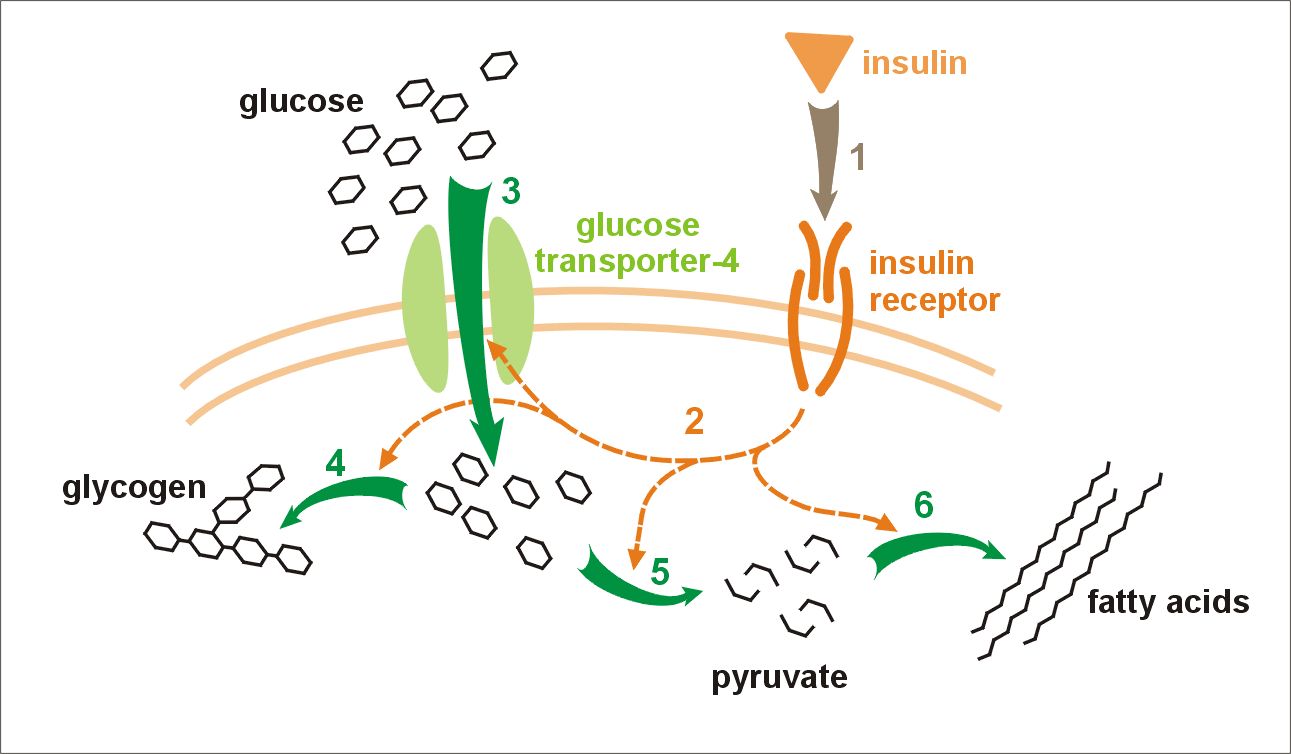 The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor. The interference probably occurs at the level of the
The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor. The interference probably occurs at the level of the
 Treatment of GDM with diet and insulin reduces health problems mother and child. Treatment of GDM is also accompanied by more inductions of labour.
A repeat OGTT should be carried out 6 weeks after delivery, to confirm the diabetes has disappeared. Afterwards, regular screening for type 2 diabetes is advised.
Lifestyle interventions include exercise, diet advice, behavioural interventions, relaxation, self-monitoring glucose, and combined interventions. Women with gestational diabetes who receive lifestyle interventions seem to have less postpartum depression, and were more likely to reach their weight loss targets after giving birth, than women who had no intervention. Their babies are also less likely to be large for their gestational age, and have less percentage of fat when they are born. More research is needed to find out which lifestyle interventions are best. Some women with GDM use
Treatment of GDM with diet and insulin reduces health problems mother and child. Treatment of GDM is also accompanied by more inductions of labour.
A repeat OGTT should be carried out 6 weeks after delivery, to confirm the diabetes has disappeared. Afterwards, regular screening for type 2 diabetes is advised.
Lifestyle interventions include exercise, diet advice, behavioural interventions, relaxation, self-monitoring glucose, and combined interventions. Women with gestational diabetes who receive lifestyle interventions seem to have less postpartum depression, and were more likely to reach their weight loss targets after giving birth, than women who had no intervention. Their babies are also less likely to be large for their gestational age, and have less percentage of fat when they are born. More research is needed to find out which lifestyle interventions are best. Some women with GDM use
IDF Diabetes Atlas
International Diabetes Federation
* National Institute of Child Health and Human Development �
Am I at Risk for Gestational Diabetes?
* National Institute of Child Health and Human Development �
Managing Gestational Diabetes: A Patient's Guide to a Healthy Pregnancy
* Gestational Diabetes Resource Guide �
American Diabetes Association
* Diabetes.co.uk
{{DEFAULTSORT:Gestational Diabetes Diabetes Health issues in pregnancy Women's health Wikipedia medicine articles ready to translate
diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level ( hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
develops high blood sugar
Hyperglycemia is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even ...
levels during pregnancy
Pregnancy is the time during which one or more offspring develops (gestation, gestates) inside a woman, woman's uterus (womb). A multiple birth, multiple pregnancy involves more than one offspring, such as with twins.
Pregnancy usually occur ...
. Gestational diabetes generally results in few symptoms; however, it increases the risk of pre-eclampsia, depression, and of needing a Caesarean section. Babies born to mothers with poorly treated gestational diabetes are at increased risk of macrosomia
Large for gestational age (LGA) is a term used to describe infants that are born with an abnormally high weight, specifically in the 90th percentile or above, compared to other babies of the same developmental age. Macrosomia is a similar term tha ...
, of having hypoglycemia after birth, and of jaundice. If untreated, diabetes can also result in stillbirth. Long term, children are at higher risk of being overweight and of developing type 2 diabetes.
Gestational diabetes can occur during pregnancy because of insulin resistance or reduced production of insulin. Risk factors include being overweight, previously having gestational diabetes, a family history of type 2 diabetes, and having polycystic ovarian syndrome
Polycystic ovary syndrome, or PCOS, is the most common endocrine disorder in women of reproductive age. The syndrome is named after the characteristic cysts which may form on the ovaries, though it is important to note that this is a sign and no ...
. Diagnosis is by blood tests. For those at normal risk, screening is recommended between 24 and 28 weeks' gestation. For those at high risk, testing may occur at the first prenatal visit
Prenatal care, also known as antenatal care, is a type of preventive healthcare. It is provided in the form of medical checkups, consisting of recommendations on managing a healthy lifestyle and the provision of medical information such as materna ...
.
Maintenance of healthy weight and exercising before pregnancy assist in prevention. Gestational diabetes is treated with a diabetic diet
A diabetic diet is a diet that is used by people with diabetes mellitus or high blood sugar to minimize symptoms and dangerous complications of long-term elevations in blood sugar ( i.e.: cardiovascular disease, kidney disease, obesity).
Among ...
, exercise, medication (such as metformin
Metformin, sold under the brand name Glucophage, among others, is the main first-line medication for the treatment of type 2 diabetes, particularly in people who are overweight. It is also used in the treatment of polycystic ovary syndrome. ...
), and sometimes insulin injections. Most women manage blood sugar with diet and exercise. Blood sugar testing among those who are affected is often recommended four times a day. Breastfeeding
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that br ...
is recommended as soon as possible after birth.
Gestational diabetes affects 3–9% of pregnancies, depending on the population studied. It is especially common during the third trimester
Pregnancy is the time during which one or more offspring develops ( gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.
Pregnancy usually occurs by sexual intercourse, but can ...
. It affects 1% of those under the age of 20 and 13% of those over the age of 44. A number of ethnic groups including Asians, American Indians, Indigenous Australians
Indigenous Australians or Australian First Nations are people with familial heritage from, and membership in, the ethnic groups that lived in Australia before British colonisation. They consist of two distinct groups: the Aboriginal peoples ...
, and Pacific Islander
Pacific Islanders, Pasifika, Pasefika, or rarely Pacificers are the peoples of the Pacific Islands. As an ethnic/racial term, it is used to describe the original peoples—inhabitants and diasporas—of any of the three major subregions of O ...
s are at higher risk. In 90% of cases, gestational diabetes resolves after the baby is born. Women, however, are at an increased risk of developing type 2 diabetes.
Classification
Gestational diabetes is formally defined as "any degree of glucose intolerance with onset or first recognition during pregnancy". And the rest of the issue B1–B167. This definition acknowledges the possibility that a woman may have previously undiagnosed diabetes mellitus, or may have developed diabetes coincidentally with pregnancy. Whether symptoms subside after pregnancy is also irrelevant to the diagnosis. A woman is diagnosed with gestational diabetes when glucose intolerance continues beyond 24 to 28 weeks of gestation. The White classification, named after Priscilla White, who pioneered research on the effect of diabetes types on perinatal outcome, is widely used to assess maternal and fetal risk. It distinguishes between gestational diabetes (type A) and pregestational diabetes (diabetes that existed prior to pregnancy). These two groups are further subdivided according to their associated risks and management. The two subtypes of gestational diabetes under this classification system are: * Type A1: abnormal oral glucose tolerance test (OGTT), but normal blood glucose levels during fasting and two hours after meals; diet modification is sufficient to control glucose levels * Type A2: abnormal OGTT compounded by abnormal glucose levels during fasting and/or after meals; additional therapy with insulin or other medications is required Diabetes which existed prior to pregnancy is also split up into several subtypes under this system: * Type B: onset at age 20 or older and duration of less than 10 years. * Type C: onset at age 10–19 or duration of 10–19 years. * Type D: onset before age 10 or duration greater than 20 years. * Type E: overt diabetes mellitus with calcified pelvic vessels. * Type F:diabetic nephropathy
Diabetic nephropathy, also known as diabetic kidney disease, is the chronic loss of kidney function occurring in those with diabetes mellitus. Diabetic nephropathy is the leading causes of chronic kidney disease (CKD) and end-stage renal disease ...
.
* Type R: proliferative retinopathy
Retinopathy is any damage to the retina of the eyes, which may cause vision impairment. Retinopathy often refers to retinal vascular disease, or damage to the retina caused by abnormal blood flow. Age-related macular degeneration is technically inc ...
.
* Type RF: retinopathy
Retinopathy is any damage to the retina of the eyes, which may cause vision impairment. Retinopathy often refers to retinal vascular disease, or damage to the retina caused by abnormal blood flow. Age-related macular degeneration is technically inc ...
and nephropathy.
* Type H: ischemic heart disease.
* Type T: prior kidney transplant.
An early age of onset or long-standing disease comes with greater risks, hence the first three subtypes.
Two other sets of criteria are available for diagnosis of gestational diabetes, both based on blood-sugar levels.
Criteria for diagnosis of gestational diabetes, using the 100 gram Glucose Tolerance Test
The glucose tolerance test (GTT, not to be confused with GGT test) is a medical test in which glucose is given and blood samples taken afterward to determine how quickly it is cleared from the blood. The test is usually used to test for diabetes, ...
, according to Carpenter and Coustan:
* Fasting 95 mg/dl
* 1 hour 180 mg/dl
* 2 hours 155 mg/dl
* 3 hours 140 mg/dl
Criteria for diagnosis of gestational diabetes according to National Diabetes Data Group:
* Fasting 105 mg/dl
* 1 hour 190 mg/dl
* 2 hours 165 mg/dl
* 3 hours 145 mg/dl
Risk factors
Classical risk factors for developing gestational diabetes are: * Polycystic ovary syndrome * A previous diagnosis of gestational diabetes orprediabetes
Prediabetes is a component of the metabolic syndrome and is characterized by elevated blood sugar levels that fall below the threshold to diagnose diabetes mellitus. It usually does not cause symptoms but people with prediabetes often have obesit ...
, impaired glucose tolerance
Prediabetes is a component of the metabolic syndrome and is characterized by elevated blood sugar levels that fall below the threshold to diagnose diabetes mellitus. It usually does not cause symptoms but people with prediabetes often have obesit ...
, or impaired fasting glycaemia
* A family history
Genealogy () is the study of families, family history, and the tracing of their lineages. Genealogists use oral interviews, historical records, genetic analysis, and other records to obtain information about a family and to demonstrate kin ...
revealing a first-degree relative with type 2 diabetes
* Maternal age – a woman's risk factor increases as she gets older (especially for women over 35 years of age).
* Paternal age – one study found that a father's age over 55 years was associated with GD
* Ethnicity (those with higher risk factors include African-Americans
African Americans (also referred to as Black Americans and Afro-Americans) are an ethnic group consisting of Americans with partial or total ancestry from sub-Saharan Africa. The term "African American" generally denotes descendants of enslav ...
, Afro-Caribbeans
Afro-Caribbean people or African Caribbean are Caribbean people who trace their full or partial ancestry to Sub-Saharan Africa. The majority of the modern African-Caribbeans descend from Africans taken as slaves to colonial Caribbean via the tr ...
, Native Americans, Hispanics, Pacific Islanders
Pacific Islanders, Pasifika, Pasefika, or rarely Pacificers are the peoples of the Pacific Islands. As an ethnic/ racial term, it is used to describe the original peoples—inhabitants and diasporas—of any of the three major subregions of Oce ...
, and people originating from South Asia
South Asia is the southern subregion of Asia, which is defined in both geographical
Geography (from Greek: , ''geographia''. Combination of Greek words ‘Geo’ (The Earth) and ‘Graphien’ (to describe), literally "earth descr ...
)
* Being overweight, obese
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's we ...
or severely obese increases the risk by a factor 2.1, 3.6 and 8.6, respectively.
* A previous pregnancy which resulted in a child with a macrosomia
Large for gestational age (LGA) is a term used to describe infants that are born with an abnormally high weight, specifically in the 90th percentile or above, compared to other babies of the same developmental age. Macrosomia is a similar term tha ...
(high birth weight: >90th centile or >4000 g (8 lbs 12.8 oz))
* Previous poor obstetric history
* Other genetic risk factors: There are at least 10 genes where certain polymorphism are associated with an increased risk of gestational diabetes, most notably TCF7L2
Transcription factor 7-like 2 (T-cell specific, HMG-box), also known as TCF7L2 or TCF4, is a protein acting as a transcription factor that, in humans, is encoded by the ''TCF7L2'' gene. The TCF7L2 gene is located on chromosome 10q25.2–q25.3, con ...
.
In addition to this, statistics show a double risk of GDM in smokers. Some studies have looked at more controversial potential risk factors, such as short stature
Short stature refers to a height of a human which is below typical. Whether a person is considered short depends on the context. Because of the lack of preciseness, there is often disagreement about the degree of shortness that should be called ' ...
.
About 40–60% of women with GDM have no demonstrable risk factor; for this reason many advocate to screen all women. Typically, women with GDM exhibit no symptoms (another reason for universal screening), but some women may demonstrate increased thirst
Thirst is the craving for potable fluids, resulting in the basic instinct of animals to drink. It is an essential mechanism involved in fluid balance. It arises from a lack of fluids or an increase in the concentration of certain osmolites, suc ...
, increased urination
Urination, also known as micturition, is the release of urine from the urinary bladder through the urethra to the outside of the body. It is the urinary system's form of excretion. It is also known medically as micturition, voiding, uresis, ...
, fatigue, nausea and vomiting, bladder infection, yeast infection
Candidiasis is a fungal infection due to any type of '' Candida'' (a type of yeast). When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth ...
s and blurred vision.
Pathophysiology
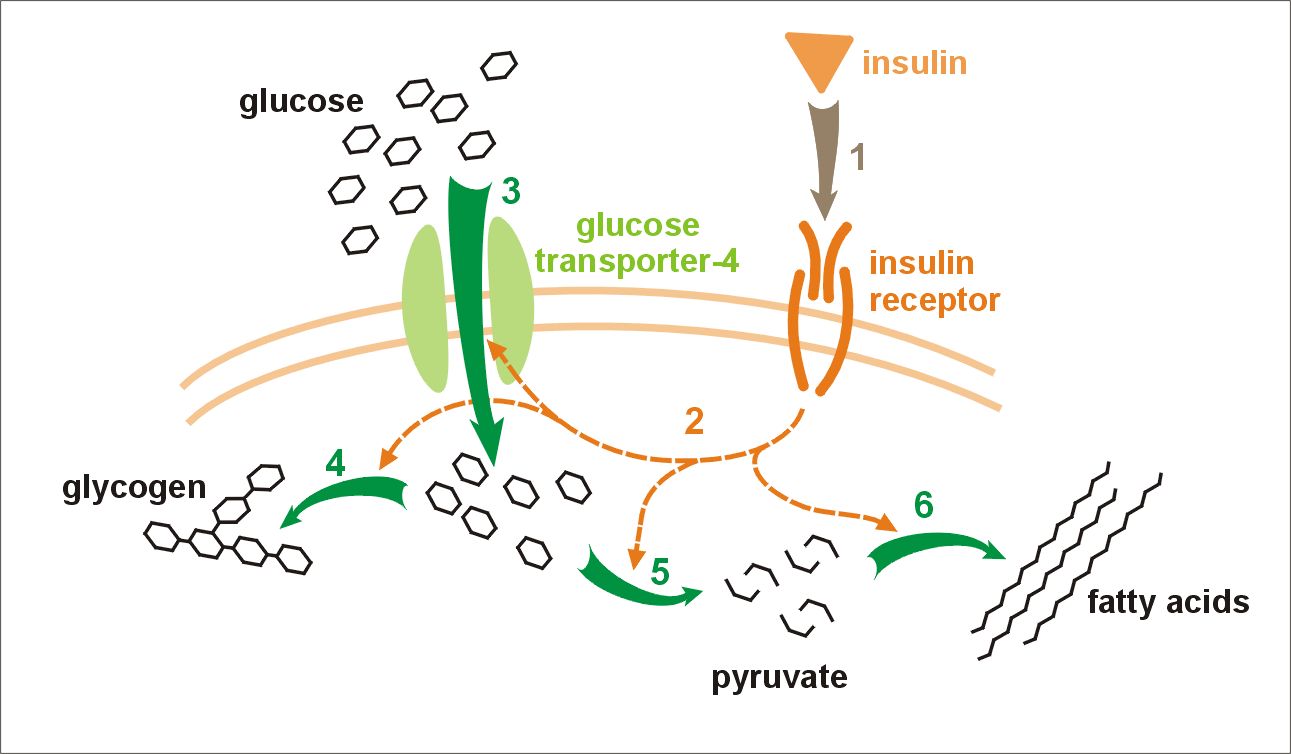 The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor. The interference probably occurs at the level of the
The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GDM is increased insulin resistance. Pregnancy hormones and other factors are thought to interfere with the action of insulin as it binds to the insulin receptor. The interference probably occurs at the level of the cell signaling
In biology, cell signaling (cell signalling in British English) or cell communication is the ability of a cell to receive, process, and transmit signals with its environment and with itself. Cell signaling is a fundamental property of all cellula ...
pathway beyond the insulin receptor. Since insulin promotes the entry of glucose into most cells, insulin resistance prevents glucose from entering the cells properly. As a result, glucose remains in the bloodstream, where glucose levels rise. More insulin is needed to overcome this resistance; about 1.5–2.5 times more insulin is produced than in a normal pregnancy.
Insulin resistance is a normal phenomenon emerging in the second trimester of pregnancy, which in cases of GDM progresses thereafter to levels seen in a non-pregnant woman with type 2 diabetes. It is thought to secure glucose supply to the growing fetus. Women with GDM have an insulin resistance that they cannot compensate for with increased production in the β-cells of the pancreas. Placental hormones, and, to a lesser extent, increased fat
In nutrition, biology, and chemistry, fat usually means any ester of fatty acids, or a mixture of such compounds, most commonly those that occur in living beings or in food.
The term often refers specifically to triglycerides (triple est ...
deposits during pregnancy, seem to mediate insulin resistance during pregnancy. Cortisol and progesterone are the main culprits, but human placental lactogen, prolactin
Prolactin (PRL), also known as lactotropin, is a protein best known for its role in enabling mammals to produce milk. It is influential in over 300 separate processes in various vertebrates, including humans. Prolactin is secreted from the pit ...
and estradiol
Estradiol (E2), also spelled oestradiol, is an estrogen steroid hormone and the major female sex hormone. It is involved in the regulation of the estrous and menstrual female reproductive cycles. Estradiol is responsible for the development o ...
contribute, too. Multivariate stepwise regression analysis reveals that, in combination with other placental hormones, leptin, tumor necrosis factor alpha, and resistin are involved in the decrease in insulin sensitivity occurring during pregnancy, with tumor necrosis factor alpha named as the strongest independent predictor of insulin sensitivity in pregnancy. An inverse correlation with the changes in insulin sensitivity from the time before conception through late gestation accounts for about half of the variance in the decrease in insulin sensitivity during gestation: in other words, low levels or alteration of TNF alpha factors corresponds with a greater chance of, or predisposition to, insulin resistance or sensitivity.
It is unclear why some women are unable to balance insulin needs and develop GDM; however, a number of explanations have been given, similar to those in type 2 diabetes: autoimmunity
In immunology, autoimmunity is the system of immune responses of an organism against its own healthy cells, tissues and other normal body constituents. Any disease resulting from this type of immune response is termed an "autoimmune disease". ...
, single gene mutations, obesity, along with other mechanisms.
Though the clinical presentation of gestational diabetes is well characterized, the biochemical mechanism behind the disease is not well known. One proposed biochemical mechanism involves insulin-producing β-cell adaptation controlled by the HGF/c-MET signaling pathway. β-cell adaption refers to the change that pancreatic islet cells undergo during pregnancy in response to maternal hormones in order to compensate for the increased physiological needs of mother and baby. These changes in the β-cells cause increased insulin secretion as a result of increased β-cell proliferation.
HGF/c-MET
c-Met, also called tyrosine-protein kinase Met or hepatocyte growth factor receptor (HGFR), is a protein that in humans is encoded by the ''MET'' gene. The protein possesses tyrosine kinase activity. The primary single chain precursor protein i ...
has also been implicated in β-cell regeneration, which suggests that HGF/c-MET may help increase β-cell mass in order to compensate for insulin needs during pregnancy. Recent studies support that loss of HGF/c-MET signaling results in aberrant β-cell adaptation.
c-MET is a receptor tyrosine kinase
Receptor tyrosine kinases (RTKs) are the high- affinity cell surface receptors for many polypeptide growth factors, cytokines, and hormones. Of the 90 unique tyrosine kinase genes identified in the human genome, 58 encode receptor tyrosine kin ...
(RTK) that is activated by its ligand, hepatocyte growth factor (HGF), and is involved in the activation of several cellular processes. When HGF binds c-MET, the receptor homodimerizes and self-phosphorylates to form an SH2 recognition domain. The downstream pathways activated include common signaling molecules such as RAS and MAPK, which affect cell motility, and cell cycle progression.
Studies have shown that HGF is an important signaling molecule in stress related situations where more insulin is needed. Pregnancy causes increased insulin resistance and so a higher insulin demand. The β-cells must compensate for this by either increasing insulin production or proliferating. If neither of the processes occur, then markers for gestational diabetes are observed. It has been observed that pregnancy increases HGF levels, showing a correlation that suggests a connection between the signaling pathway and increased insulin needs. In fact, when no signaling is present, gestational diabetes is more likely to occur.
The exact mechanism of HGF/c-MET regulated β-cell adaptation is not yet known but there are several hypotheses about how the signaling molecules contribute to insulin levels during pregnancy. c-MET may interact with FoxM1, a molecule important in the cell cycle, as FOXM1 levels decrease when c-MET is not present. Additionally, c-MET may interact with p27 as the protein levels increase with c-MET is not present. Another hypothesis says that c-MET may control β-cell apoptosis because a lack of c-MET causes increases cell death but the signaling mechanisms have not been elucidated.
Although the mechanism of HGF/c-MET control of gestational diabetes is not yet well understood, there is a strong correlation between the signaling pathway and the inability to produce an adequate amount of insulin during pregnancy and thus it may be the target for future diabetic therapies.
Because glucose travels across the placenta (through diffusion facilitated by GLUT1
Glucose transporter 1 (or GLUT1), also known as solute carrier family 2, facilitated glucose transporter member 1 (SLC2A1), is a uniporter protein that in humans is encoded by the ''SLC2A1'' gene. GLUT1 facilitates the transport of glucose across ...
carrier), which is located in the syncytiotrophoblast on both the microvillus and basal membranes, these membranes may be the rate-limiting step in placental glucose transport. There is a two- to three-fold increase in the expression of syncytiotrophoblast glucose transporters with advancing gestation. Finally, the role of GLUT3/GLUT4 transport remains speculative. If the untreated gestational diabetes fetus is exposed to consistently higher glucose levels, this leads to increased fetal levels of insulin (insulin itself cannot cross the placenta). The growth-stimulating effects of insulin can lead to excessive growth and a large body (macrosomia
Large for gestational age (LGA) is a term used to describe infants that are born with an abnormally high weight, specifically in the 90th percentile or above, compared to other babies of the same developmental age. Macrosomia is a similar term tha ...
). After birth, the high glucose environment disappears, leaving these newborns with ongoing high insulin production and susceptibility to low blood glucose levels ( hypoglycemia).
Screening
A number of screening and diagnostic tests have been used to look for high levels ofglucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, u ...
in plasma or serum in defined circumstances. One method is a stepwise approach where a suspicious result on a screening test is followed by diagnostic test. Alternatively, a more involved diagnostic test can be used directly at the first prenatal visit for a woman with a high-risk pregnancy. (for example in those with polycystic ovarian syndrome
Polycystic ovary syndrome, or PCOS, is the most common endocrine disorder in women of reproductive age. The syndrome is named after the characteristic cysts which may form on the ovaries, though it is important to note that this is a sign and no ...
or acanthosis nigricans
Acanthosis nigricans is a medical sign characterised by brown-to-black, poorly defined, velvety hyperpigmentation of the skin. It is usually found in body folds, such as the posterior and lateral folds of the neck, the armpits, groin, navel, foreh ...
).
Non-challenge blood glucose tests involve measuring glucose levels in blood samples without challenging the subject with glucose solutions. A blood glucose level is determined when fasting, two hours after a meal, or simply at any random time. In contrast, challenge tests involve drinking a glucose solution and measuring glucose concentration thereafter in the blood; in diabetes, they tend to remain high. The glucose solution has a very sweet taste which some women find unpleasant; sometimes, therefore, artificial flavours are added. Some women may experience nausea during the test, and more so with higher glucose levels.
There is currently not enough research to show which way is best at diagnosing gestational diabetes. Routine screening of women with a glucose challenge test may find more women with gestational diabetes than only screening women with risk factors. It is not clear how these screening tests affect the rest of the pregnancy. Future research should include how the method of screening impacts the mother and baby.
Pathways
Opinions differ about optimal screening and diagnostic measures, in part due to differences in population risks, cost-effectiveness considerations, and lack of an evidence base to support large national screening programs. The most elaborate regimen entails a random blood glucose test during a booking visit, a screening glucose challenge test around 24–28 weeks' gestation, followed by an OGTT if the tests are outside normal limits. If there is a high suspicion, a woman may be tested earlier. In theUnited States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territori ...
, most obstetricians prefer universal screening with a screening glucose challenge test. In the United Kingdom
The United Kingdom of Great Britain and Northern Ireland, commonly known as the United Kingdom (UK) or Britain, is a country in Europe, off the north-western coast of the European mainland, continental mainland. It comprises England, Scotlan ...
, obstetric units often rely on risk factors and a random blood glucose test. The American Diabetes Association and the Society of Obstetricians and Gynaecologists of Canada
The Society of Obstetricians and Gynaecologists of Canada (SOGC) is a national medical society in Canada, representing over 4,000 obstetricians/gynaecologists, family physicians, nurses, midwives, and allied health professionals in the field of s ...
recommend routine screening unless the woman is low risk (this means the woman must be younger than 25 years and have a body mass index less than 27, with no personal, ethnic or family risk factors) The Canadian Diabetes Association and the American College of Obstetricians and Gynecologists
The American College of Obstetricians and Gynecologists (ACOG) is a professional association of physicians specializing in obstetrics and gynecology in the United States. Several Latin American countries are also represented within Districts of ...
recommend universal screening.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2003 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. ''Can J Diabetes'' 2003; 27 (Suppl 2): 1–140. The U.S. Preventive Services Task Force found there is insufficient evidence to recommend for or against routine screening, and a 2017 a Cochrane review found that there is not evidence to determine which screening method is best for women and their babies.
Some pregnant women and careproviders choose to forgo routine screening due to the absence of risk factors, however this is not advised due to the large proportion of women who develop gestational diabetes despite having no risk factors present and the dangers to the mother and baby if gestational diabetes remains untreated.
Non-challenge blood glucose tests
When a plasma glucose level is found to be higher than 126 mg/dL (7.0 mmol/L) after fasting, or over 200 mg/dL (11.1 mmol/L) on any occasion, and if this is confirmed on a subsequent day, the diagnosis of GDM is made, and no further testing is required. These tests are typically performed at the first antenatal visit. They are simple to administer and inexpensive, but have a lower test performance compared to the other tests, with moderate sensitivity, low specificity and highfalse positive
A false positive is an error in binary classification in which a test result incorrectly indicates the presence of a condition (such as a disease when the disease is not present), while a false negative is the opposite error, where the test resul ...
rates.
Screening glucose challenge test
The screening glucose challenge test (sometimes called the O'Sullivan test) is performed between 24 and 28 weeks, and can be seen as a simplified version of the oral glucose tolerance test (OGTT). No previous fasting is required for this screening test, in contrast to the OGTT. The O'Sullivan test involves drinking a solution containing 50 grams of glucose, and measuring blood levels one hour later. If the cut-off point is set at 140 mg/dL (7.8 mmol/L), 80% of women with GDM will be detected. If this threshold for further testing is lowered to 130 mg/dL, 90% of GDM cases will be detected, but there will also be more women who will be subjected to a consequent OGTT unnecessarily.Oral glucose tolerance test
A standardizedoral glucose tolerance test
The glucose tolerance test (GTT, not to be confused with GGT test) is a medical test in which glucose is given and blood samples taken afterward to determine how quickly it is cleared from the blood. The test is usually used to test for diabetes, ...
(OGTT) should be done in the morning after an overnight fast of between 8 and 14 hours. During the three previous days the subject must have an unrestricted diet (containing at least 150 g carbohydrate
In organic chemistry, a carbohydrate () is a biomolecule consisting of carbon (C), hydrogen (H) and oxygen (O) atoms, usually with a hydrogen–oxygen atom ratio of 2:1 (as in water) and thus with the empirical formula (where ''m'' may or m ...
per day) and unlimited physical activity. The subject should remain seated during the test and should not smoke throughout the test.
The test involves drinking a solution containing a certain amount of glucose, usually 75 g or 100 g, and drawing blood to measure glucose levels at the start and on set time intervals thereafter.
The diagnostic criteria from the National Diabetes Data Group (NDDG) have been used most often, but some centers rely on the Carpenter and Coustan criteria, which set the cutoff for normal at lower values. Compared with the NDDG criteria, the Carpenter and Coustan criteria lead to a diagnosis of gestational diabetes in 54 percent more pregnant women, with an increased cost and no compelling evidence of improved perinatal outcomes.
The following are the values which the American Diabetes Association considers to be abnormal during the 100 g of glucose OGTT:
* Fasting blood glucose level ≥95 mg/dL (5.33 mmol/L)
* 1 hour blood glucose level ≥180 mg/dL (10 mmol/L)
* 2 hour blood glucose level ≥155 mg/dL (8.6 mmol/L)
* 3 hour blood glucose level ≥140 mg/dL (7.8 mmol/L)
An alternative test uses a 75 g glucose load and measures the blood glucose levels before and after one and two hours, using the same reference values. This test will identify fewer women who are at risk, and there is only a weak concordance (agreement rate) between this test and a three-hour 100 g test.
The glucose values used to detect gestational diabetes were first determined by O'Sullivan and Mahan (1964) in a retrospective cohort study
A retrospective cohort study, also called a historic cohort study, is a longitudinal cohort study used in medical and psychological research. A cohort of individuals that share a common exposure factor is compared with another group of equival ...
(using a 100 grams of glucose OGTT) designed to detect risk of developing type 2 diabetes in the future. The values were set using whole blood and required two values reaching or exceeding the value to be positive. Subsequent information led to alterations in O'Sullivan's criteria. When methods for blood glucose determination changed from the use of whole blood to venous plasma samples, the criteria for GDM were also changed.
Urinary glucose testing
Women with GDM may have high glucose levels in their urine ( glucosuria). Although dipstick testing is widely practiced, it performs poorly, and discontinuing routine dipstick testing has not been shown to cause underdiagnosis where universal screening is performed. Increasedglomerular filtration rate
Renal functions include maintaining an acid–base balance; regulating fluid balance; regulating sodium, potassium, and other electrolytes; clearing toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pre ...
s during pregnancy contribute to some 50% of women having glucose in their urine on dipstick tests at some point during their pregnancy. The sensitivity of glucosuria for GDM in the first two trimesters is only around 10% and the positive predictive value is around 20%.
Prevention
Vitamin D supplementation during pregnancy may help to prevent gestational diabetes. A 2015 review found that when done during pregnancy moderate physical exercise is effective for the prevention of gestational diabetes. A 2014 review however did not find a significant effect. It is uncertain if additional dietary advice interventions help to reduce the risk of gestational diabetes. However, data from theNurses' Health Study
The Nurses Health Study is a series of prospective studies that examine epidemiology and the long-term effects of nutrition, hormones, environment, and nurses' work-life on health and disease development. The studies have been among the largest in ...
shows that adherence to a healthy plant-based diet
A plant-based diet is a diet consisting mostly or entirely of plant-based foods. Plant-based diets encompass a wide range of dietary patterns that contain low amounts of animal products and high amounts of plant products such as vegetables, fru ...
is associated with lower risk for GDM.
Diet and physical activity interventions designed to prevent excessive gestational weight gain reduce the rates of gestational diabetes. However, the impact of these interventions varies with the body-mass index of the person as well as with the region in which the studies were performed.
Moderate-quality evidence suggest that there is a reduced risk of gestational diabetes mellitus and caesarean section with combined diet and exercise interventions during pregnancy as well as reductions in gestational weight gain, compared with standard care.
It has been suggested that for women who have had gestational diabetes, diet, exercise, education, and lifestyle changes between pregnancies may lower their chances of having gestational diabetes again in future pregnancies. However, there is no research to show whether interventions between pregnancies lower the number of women who develop gestational diabetes again.
Management
 Treatment of GDM with diet and insulin reduces health problems mother and child. Treatment of GDM is also accompanied by more inductions of labour.
A repeat OGTT should be carried out 6 weeks after delivery, to confirm the diabetes has disappeared. Afterwards, regular screening for type 2 diabetes is advised.
Lifestyle interventions include exercise, diet advice, behavioural interventions, relaxation, self-monitoring glucose, and combined interventions. Women with gestational diabetes who receive lifestyle interventions seem to have less postpartum depression, and were more likely to reach their weight loss targets after giving birth, than women who had no intervention. Their babies are also less likely to be large for their gestational age, and have less percentage of fat when they are born. More research is needed to find out which lifestyle interventions are best. Some women with GDM use
Treatment of GDM with diet and insulin reduces health problems mother and child. Treatment of GDM is also accompanied by more inductions of labour.
A repeat OGTT should be carried out 6 weeks after delivery, to confirm the diabetes has disappeared. Afterwards, regular screening for type 2 diabetes is advised.
Lifestyle interventions include exercise, diet advice, behavioural interventions, relaxation, self-monitoring glucose, and combined interventions. Women with gestational diabetes who receive lifestyle interventions seem to have less postpartum depression, and were more likely to reach their weight loss targets after giving birth, than women who had no intervention. Their babies are also less likely to be large for their gestational age, and have less percentage of fat when they are born. More research is needed to find out which lifestyle interventions are best. Some women with GDM use probiotics
Probiotics are live microorganisms promoted with claims that they provide health benefits when consumed, generally by improving or restoring the gut microbiota. Probiotics are considered generally safe to consume, but may cause bacteria- host i ...
but it is very uncertain if there are any benefits in terms of blood glucose levels, high blood pressure disorders or induction of labour.
If a diabetic diet
A diabetic diet is a diet that is used by people with diabetes mellitus or high blood sugar to minimize symptoms and dangerous complications of long-term elevations in blood sugar ( i.e.: cardiovascular disease, kidney disease, obesity).
Among ...
or G.I. Diet, exercise, and oral medication are inadequate to control glucose levels, insulin therapy may become necessary.
The development of macrosomia can be evaluated during pregnancy by using sonography
Medical ultrasound includes diagnostic techniques (mainly imaging techniques) using ultrasound, as well as therapeutic applications of ultrasound. In diagnosis, it is used to create an image of internal body structures such as tendons, musc ...
. Women who use insulin, with a history of stillbirth, or with hypertension are managed like women with overt diabetes.
Lifestyle
Counselling before pregnancy (for example, about preventive folic acid supplements) and multidisciplinary management are important for good pregnancy outcomes. Most women can manage their GDM with dietary changes and exercise. Self monitoring of blood glucose levels can guide therapy. Some women will needantidiabetic drugs
Drugs used in diabetes treat diabetes mellitus by altering the glucose level in the blood. With the exceptions of insulin, most GLP receptor agonists ( liraglutide, exenatide, and others), and pramlintide, all are administered orally and are ...
, most commonly insulin therapy.
Any diet needs to provide sufficient calories for pregnancy, typically 2,000–2,500 kcal with the exclusion of simple carbohydrates. The main goal of dietary modifications is to avoid peaks in blood sugar levels. This can be done by spreading carbohydrate intake over meals and snacks throughout the day, and using slow-release carbohydrate sources—known as the G.I. Diet. Since insulin resistance is highest in mornings, breakfast carbohydrates need to be restricted more.
The Mediterranean diet
The Mediterranean diet is a diet inspired by the eating habits of people who live near the Mediterranean Sea. When initially formulated in the 1960s, it drew on the cuisines of Greece, Italy, France and Spain. In decades since, it has also incor ...
may be associated with reduced incidence of gestational diabetes. However, there is not enough evidence to indicate if one type of dietary advice is better than another.
Regular moderately intense physical exercise is advised, although there is no consensus on the specific structure of exercise programs for GDM. Pregnant women who exercise have lower blood sugar levels when fasting and after meals compared to those who do not exercise. It is not clear which form of exercise is best when pregnant.
Self monitoring can be accomplished using a handheld capillary glucose dosage system. Compliance with these glucometer systems can be low. There is not a lot of research into what target blood sugar levels should be for women with gestational diabetes and targets recommended to women vary around the world. Target ranges advised by the Australasian Diabetes in Pregnancy Society are as follows:
* fasting capillary blood glucose levels <5.5 mmol/L
* 1 hour postprandial capillary blood glucose levels <8.0 mmol/L
* 2 hour postprandial blood glucose levels <6.7 mmol/L
Regular blood samples can be used to determine HbA1c
Glycated hemoglobin, also known as HbA1c, glycohemoglobin, hemoglobin A1c, A1C, is a form of hemoglobin (Hb) that is chemically linked to a sugar. Most monosaccharides, including glucose, galactose and fructose, spontaneously (i.e. non-enzymati ...
levels, which give an idea of glucose control over a longer time period.
Research suggests a possible benefit of breastfeeding
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that br ...
to reduce the risk of diabetes and related risks for both mother and child.
Medication
If monitoring reveals failing control of glucose levels with these measures, or if there is evidence of complications like excessive fetal growth, treatment with insulin might be necessary. This is most commonly fast-acting insulin given just before eating to blunt glucose rises after meals. Care needs to be taken to avoid low blood sugar levels due to excessive insulin. Insulin therapy can be normal or very tight; more injections can result in better control but requires more effort, and there is no consensus that it has large benefits. A 2016Cochrane review
Cochrane (previously known as the Cochrane Collaboration) is a British international charitable organisation formed to organise medical research findings to facilitate evidence-based choices about health interventions involving health profes ...
concluded that quality evidence is not yet available to determine the best blood sugar range for improving health for pregnant women with GDM and their babies.
There is some evidence that certain medications by mouth might be safe in pregnancy, or at least, are less dangerous to the developing fetus than poorly controlled diabetes. When comparing which diabetes tablets (medication by mouth) work best and are safest, there is not enough quality research to support one medication over another. The medication metformin
Metformin, sold under the brand name Glucophage, among others, is the main first-line medication for the treatment of type 2 diabetes, particularly in people who are overweight. It is also used in the treatment of polycystic ovary syndrome. ...
is better than glyburide. If blood glucose cannot be adequately controlled with a single agent, the combination of metformin and insulin may be better than insulin alone. Another review found good short term safety for both the mother and baby with metformin but unclear long term safety.
People may prefer metformin by mouth to insulin injections. Treatment of polycystic ovarian syndrome with metformin during pregnancy has been noted to decrease GDM levels.
Almost half of the women did not reach sufficient control with metformin alone and needed supplemental therapy with insulin; compared to those treated with insulin alone, they required less insulin, and they gained less weight. With no long-term studies into children of women treated with the drug, there remains a possibility of long-term complications from metformin therapy. Babies born to women treated with metformin have been found to develop less visceral fat, making them less prone to insulin resistance in later life.
Prognosis
Gestational diabetes generally resolves once the baby is born. Based on different studies, the chances of developing GDM in a second pregnancy, if a woman had GDM in her first pregnancy, are between 30 and 84%, depending on ethnic background. A second pregnancy within one year of the previous pregnancy has a large likelihood of GDM recurrence. Women diagnosed with gestational diabetes have an increased risk of developing diabetes mellitus in the future. The risk is highest in women who needed insulin treatment, had antibodies associated with diabetes (such as antibodies againstglutamate decarboxylase
Glutamate decarboxylase or glutamic acid decarboxylase (GAD) is an enzyme that catalyzes the decarboxylation of glutamate to gamma-aminobutyric acid (GABA) and carbon dioxide (). GAD uses pyridoxal-phosphate (PLP) as a cofactor. The reaction p ...
, islet cell antibodies and/or insulinoma antigen-2), women with more than two previous pregnancies, and women who were obese (in order of importance). Women requiring insulin to manage gestational diabetes have a 50% risk of developing diabetes within the next five years. Depending on the population studied, the diagnostic criteria and the length of follow-up, the risk can vary enormously. The risk appears to be highest in the first 5 years, reaching a plateau thereafter. One of the longest studies followed a group of women from Boston, Massachusetts; half of them developed diabetes after 6 years, and more than 70% had diabetes after 28 years. In a retrospective study in Navajo women, the risk of diabetes after GDM was estimated to be 50 to 70% after 11 years. Another study found a risk of diabetes after GDM of more than 25% after 15 years. In populations with a low risk for type 2 diabetes, in lean subjects and in women with auto-antibodies
An autoantibody is an antibody (a type of protein) produced by the immune system that is directed against one or more of the individual's own proteins. Many autoimmune diseases (notably lupus erythematosus) are associated with such antibodies.
Pr ...
, there is a higher rate of women developing type 1 diabetes (LADA).
Children of women with GDM have an increased risk for childhood and adult obesity and an increased risk of glucose intolerance and type 2 diabetes later in life. This risk relates to increased maternal glucose values. It is currently unclear how much genetic susceptibility and environmental factors contribute to this risk, and whether treatment of GDM can influence this outcome.
Relative benefits and harms of different oral anti-diabetic medications are not yet well understood as of 2017.
There are scarce statistical data on the risk of other conditions in women with GDM; in the Jerusalem Perinatal study, 410 out of 37,962 women were reported to have GDM, and there was a tendency towards more breast and pancreatic cancer, but more research is needed to confirm this finding.
Research is being conducted to develop a web-based clinical decision support system for GDM prediction using machine learning techniques. Results so far demonstrated great potential in clinical practicality for automatic GDM prognosis.
Complications
GDM poses a risk to mother and child. This risk is largely related to uncontrolled blood glucose levels and its consequences. The risk increases with higher blood glucose levels. Treatment resulting in better control of these levels can reduce some of the risks of GDM considerably. The two main risks GDM imposes on the baby are growth abnormalities and chemical imbalances after birth, which may require admission to a neonatal intensive care unit. Infants born to mothers with GDM are at risk of being both large for gestational age (macrosomic) in unmanaged GDM, andsmall for gestational age
Small for gestational age (SGA) newborns are those who are smaller in size than normal for the gestational age, most commonly defined as a weight below the 10th percentile for the gestational age.
Causes
Being small for gestational age is broadly ...
and Intrauterine growth retardation in managed GDM. Macrosomia in turn increases the risk of instrumental deliveries (e.g. forceps
Forceps (plural forceps or considered a plural noun without a singular, often a pair of forceps; the Latin plural ''forcipes'' is no longer recorded in most dictionaries) are a handheld, hinged instrument used for grasping and holding objects. Fo ...
, ventouse and caesarean section) or problems during vaginal delivery (such as shoulder dystocia
Shoulder dystocia is when, after vaginal delivery of the head, the baby's anterior shoulder gets caught above the mother's pubic bone. Signs include retraction of the baby's head back into the vagina, known as "turtle sign". Complications for th ...
). Macrosomia may affect 12% of normal women compared to 20% of women with GDM. However, the evidence for each of these complications is not equally strong; in the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study for example, there was an increased risk for babies to be large but not small for gestational age in women with uncontrolled GDM. In a recent birth cohot study of 5150 deliveries, a research group active at the University of Helsinki and Helsinki University Hospital, Finland demonstrated that the mother's GDM is an independent factor that increases the risk of fetal hypoxia, during labour. The study was published in the ''Acta Diabetologica'' in June 2021. Another finding was that GDM increased the susceptibility of the fetus to intrapartum hypoxia, regardless of the size of the fetus. The risk of hypoxia and the resulting risk of poor condition in newborn infants was nearly 7-fold in the fetuses of mothers with GDM compared to the fetuses of non-diabetic mothers. Furthermore, according to the findings, the risk of needing to perform resuscitation on the newborn after birth was 10-fold.
Another finding was that gestational diabetes increased the susceptibility of the fetus to intrapartal hypoxia, regardless of the size of the fetus.
"The risk of hypoxia and the resulting risk of poor condition in newborn infants was nearly seven-fold in the fetuses of mothers with gestational diabetes compared to the fetuses of non-diabetic mothers," says researcher Mikko Tarvonen. According to the findings, the risk of needing to perform resuscitation on the newborn was ten-fold.Research into complications for GDM is difficult because of the many confounding factors (such as obesity). Labelling a woman as having GDM may in itself increase the risk of having an unnecessary caesarean section.
Neonates born from women with consistently high blood sugar levels are also at an increased risk of low blood glucose ( hypoglycemia), jaundice, high red blood cell
Red blood cells (RBCs), also referred to as red cells, red blood corpuscles (in humans or other animals not having nucleus in red blood cells), haematids, erythroid cells or erythrocytes (from Greek ''erythros'' for "red" and ''kytos'' for "holl ...
mass ( polycythemia) and low blood calcium (hypocalcemia
Hypocalcemia is a medical condition characterized by low calcium levels in the blood serum. The normal range of blood calcium is typically between 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L) while levels less than 2.1 mm ...
) and magnesium (hypomagnesemia
Magnesium deficiency is an electrolyte disturbance in which there is a low level of magnesium in the body. It can result in multiple symptoms. Symptoms include tremor, poor coordination, muscle spasms, loss of appetite, personality changes, an ...
). Untreated GDM also interferes with maturation, causing dysmature babies prone to respiratory distress syndrome due to incomplete lung maturation and impaired surfactant synthesis.
Unlike pre-gestational diabetes, gestational diabetes has not been clearly shown to be an independent risk factor for birth defects. Birth defects usually originate sometime during the first trimester
Pregnancy is the time during which one or more offspring develops ( gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.
Pregnancy usually occurs by sexual intercourse, but ...
(before the 13th week) of pregnancy, whereas GDM gradually develops and is least pronounced during the first and early second trimester. Studies have shown that the offspring of women with GDM are at a higher risk for congenital malformations. A large case-control study found that gestational diabetes was linked with a limited group of birth defects, and that this association was generally limited to women with a higher body mass index (≥ 25 kg/m2). It is difficult to make sure that this is not partially due to the inclusion of women with pre-existent type 2 diabetes who were not diagnosed before pregnancy.
Because of conflicting studies, it is unclear at the moment whether women with GDM have a higher risk of preeclampsia. In the HAPO study, the risk of preeclampsia was between 13% and 37% higher, although not all possible confounding factors were corrected.
Epidemiology
Gestational diabetes affects 3–10% of pregnancies, depending on the population studied.References
External links
IDF Diabetes Atlas
International Diabetes Federation
* National Institute of Child Health and Human Development �
Am I at Risk for Gestational Diabetes?
* National Institute of Child Health and Human Development �
Managing Gestational Diabetes: A Patient's Guide to a Healthy Pregnancy
* Gestational Diabetes Resource Guide �
American Diabetes Association
* Diabetes.co.uk
{{DEFAULTSORT:Gestational Diabetes Diabetes Health issues in pregnancy Women's health Wikipedia medicine articles ready to translate