Ovarian cancer is a
cancerous
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bl ...
tumor
A neoplasm () is a type of abnormal and excessive growth of tissue. The process that occurs to form or produce a neoplasm is called neoplasia. The growth of a neoplasm is uncoordinated with that of the normal surrounding tissue, and persists ...
of an
ovary.
It may originate from the ovary itself or more commonly from communicating nearby structures such as
fallopian tubes or the
inner lining of the abdomen.
The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or
spread
Spread may refer to:
Places
* Spread, West Virginia
Arts, entertainment, and media
* ''Spread'' (film), a 2009 film.
* ''$pread'', a quarterly magazine by and for sex workers
* "Spread", a song by OutKast from their 2003 album ''Speakerboxxx/T ...
to other parts of the body. When this process begins, there may be no or only vague symptoms.
[ Symptoms become more noticeable as the cancer progresses.][ These symptoms may include ]bloating
Abdominal bloating (or simply bloating) is a short-term disease that affects the gastrointestinal tract. Bloating is generally characterized by an excess buildup of gas, air or fluids in the stomach. A person may have feelings of tightness, pres ...
, vaginal bleeding, pelvic pain, abdominal swelling, constipation
Constipation is a bowel dysfunction that makes bowel movements infrequent or hard to pass. The stool is often hard and dry. Other symptoms may include abdominal pain, bloating, and feeling as if one has not completely passed the bowel movement ...
, and loss of appetite
Anorexia is a medical term for a loss of appetite. While the term in non-scientific publications is often used interchangeably with anorexia nervosa, many possible causes exist for a loss of appetite, some of which may be harmless, while others i ...
, among others.[ Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, ]lungs
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side ...
, and liver
The liver is a major organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the synthesis of proteins and biochemicals necessary for digestion and growth. In humans, it ...
.
The risk of ovarian cancer increases with age. Most cases of ovarian cancer develop after menopause.ovulate
Ovulation is the release of eggs from the ovaries. In women, this event occurs when the ovarian follicles rupture and release the secondary oocyte ovarian cells. After ovulation, during the luteal phase, the egg will be available to be fertilized ...
d more over their lifetime.[ Other risk factors include hormone therapy after ]menopause
Menopause, also known as the climacteric, is the time in women's lives when menstrual periods stop permanently, and they are no longer able to bear children. Menopause usually occurs between the age of 47 and 54. Medical professionals often ...
, fertility medication, and obesity
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's ...
.hormonal birth control
Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones, although in India one selective estrogen receptor modulator is marketed as a contraceptive. The origina ...
, tubal ligation
Tubal ligation (commonly known as having one's "tubes tied") is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus the ...
, pregnancy, and breast feeding
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that brea ...
.[ About 10% of cases are related to inherited genetic risk; women with mutations in the genes '']BRCA1
Breast cancer type 1 susceptibility protein is a protein that in humans is encoded by the ''BRCA1'' () gene. Orthologs are common in other vertebrate species, whereas invertebrate genomes may encode a more distantly related gene. ''BRCA1'' is a ...
'' or '' BRCA2'' have about a 50% chance of developing the disease.[ Some family cancer syndromes such as hereditary nonpolyposis colon cancer and Peutz-Jeghers syndrome also increase the risk of developing ovarian cancer.][ There are five main subtypes of ovarian carcinoma, of which high-grade serous carcinoma (HGSC) is the most common.][ Less common types of ovarian cancer include germ cell tumors and sex cord stromal tumors.][ A diagnosis of ovarian cancer is confirmed through a ]biopsy
A biopsy is a medical test commonly performed by a surgeon, interventional radiologist, or an interventional cardiologist. The process involves extraction of sample cells or tissues for examination to determine the presence or extent of a dise ...
of tissue, usually removed during surgery.[
Screening is not recommended in women who are at average risk, as evidence does not support a reduction in death and the high rate of false positive tests may lead to unneeded surgery, which is accompanied by its own risks.][ If caught and treated in an early stage, ovarian cancer is often curable.][ Treatment usually includes some combination of surgery, ]radiation therapy
Radiation therapy or radiotherapy, often abbreviated RT, RTx, or XRT, is a therapy using ionizing radiation, generally provided as part of cancer treatment to control or kill malignant cells and normally delivered by a linear accelerator. Radi ...
, and chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs ( chemotherapeutic agents or alkylating agents) as part of a standardized chemotherapy regimen. Chemothe ...
.five-year survival rate
The five-year survival rate is a type of survival rate for estimating the prognosis of a particular disease, normally calculated from the point of diagnosis. Lead time bias from earlier diagnosis can affect interpretation of the five-year surviva ...
in the United States is 49%.[
In 2020, new cases occurred in approximately 313,000 women. In 2019 it resulted in 13,445 deaths in the United States.][Zhou Z, Wang X, Ren X, Zhou L, Wang N, Kang H. Disease Burden and Attributable Risk Factors of Ovarian Cancer From 1990 to 2017: Findings From the Global Burden of Disease Study 2017. Front Public Health. 2021 Sep 17;9:619581. doi: 10.3389/fpubh.2021.619581. PMID 34604147; PMCID: PMC8484795.] Ovarian cancer is the second-most common gynecologic cancer in the United States. It causes more deaths than any other cancer of the female reproductive system. Among women it ranks fifth in cancer-related deaths. The typical age of diagnosis is 63.
Signs and symptoms
Early symptoms
 Early signs and symptoms of ovarian cancer may be absent or subtle. In most cases, symptoms exist for several months before being recognized and diagnosed.
Early signs and symptoms of ovarian cancer may be absent or subtle. In most cases, symptoms exist for several months before being recognized and diagnosed.irritable bowel syndrome
Irritable bowel syndrome (IBS) is a "disorder of gut-brain interaction" characterized by a group of symptoms that commonly include abdominal pain and or abdominal bloating and changes in the consistency of bowel movements. These symptoms may ...
.[ Ovarian borderline tumors, also known as low malignant potential (LMP) ovarian tumors, do not cause an increase in CA125 levels and are not identifiable with an ultrasound. The typical symptoms of an LMP tumor can include ]abdominal distension
Abdominal distension occurs when substances, such as air (gas) or fluid, accumulate in the abdomen causing its expansion. It is typically a symptom of an underlying disease or dysfunction in the body, rather than an illness in its own right. Pe ...
or pelvic pain. Particularly large masses tend to be benign or borderline.bloating
Abdominal bloating (or simply bloating) is a short-term disease that affects the gastrointestinal tract. Bloating is generally characterized by an excess buildup of gas, air or fluids in the stomach. A person may have feelings of tightness, pres ...
, abdominal or pelvic pain or discomfort, back pain, irregular menstruation
Irregular menstruation is a menstrual disorder whose manifestations include irregular cycle lengths as well as metrorrhagia (vaginal bleeding between expected periods). The possible causes of irregular menstruation may vary. The common factors of ...
or postmenopausal vaginal bleeding, pain or bleeding after or during sexual intercourse, loss of appetite
Anorexia is a medical term for a loss of appetite. While the term in non-scientific publications is often used interchangeably with anorexia nervosa, many possible causes exist for a loss of appetite, some of which may be harmless, while others i ...
, fatigue, diarrhea
Diarrhea, also spelled diarrhoea, is the condition of having at least three loose, liquid, or watery bowel movements each day. It often lasts for a few days and can result in dehydration due to fluid loss. Signs of dehydration often begin w ...
, indigestion, heartburn
Heartburn, also known as pyrosis, cardialgia or acid indigestion, is a burning sensation in the central chest or upper central abdomen. Heartburn is usually due to regurgitation of gastric acid (gastric reflux) into the esophagus. It is the m ...
, constipation
Constipation is a bowel dysfunction that makes bowel movements infrequent or hard to pass. The stool is often hard and dry. Other symptoms may include abdominal pain, bloating, and feeling as if one has not completely passed the bowel movement ...
, nausea
Nausea is a diffuse sensation of unease and discomfort, sometimes perceived as an urge to vomit. While not painful, it can be a debilitating symptom if prolonged and has been described as placing discomfort on the chest, abdomen, or back of the ...
, feeling full, and possibly urinary symptoms (including frequent urination and urgent urination).[
]
Later symptoms
 Later symptoms of ovarian cancer are due to the growing mass causing pain by pressing on other abdominopelvic organs or from metastases.
Later symptoms of ovarian cancer are due to the growing mass causing pain by pressing on other abdominopelvic organs or from metastases.ovarian torsion
Ovarian torsion (OT) or adnexal torsion is an abnormal condition where an ovary twists on its attachment to other structures, such that blood flow is decreased. Symptoms typically include pelvic pain on one side. While classically the pain is sud ...
develops. If these symptoms start to occur more often or more severely than usual, especially after no significant history of such symptoms, ovarian cancer is considered.teratoma
A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the ovary, testicle, or coccyx.
Symptoms
Symptoms may be minimal if the tumor is small. A testicular ter ...
s can cause growing teratoma syndrome or peritoneal gliomatosis.abnormal vaginal bleeding
Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reprod ...
after menopause in most cases. Other common symptoms include hirsutism
Hirsutism is excessive body hair on parts of the body where hair is normally absent or minimal. The word is from early 17th century: from Latin ''hirsutus'' meaning "hairy". It usually refers to a "male" pattern of hair growth in a female that ...
, abdominal pain, virilization
Virilization or masculinization is the biological development of adult male characteristics in young males or females. Most of the changes of virilization are produced by androgens.
Virilization is most commonly used in three medical and biology ...
, and an adnexal mass
In anatomy, adnexa (plural) refers to the appendage
An appendage (or outgrowth) is an external body part, or natural prolongation, that protrudes from an organism's body.
In arthropods, an appendage refers to any of the homologous body parts ...
.
Children
In adolescents or children with ovarian tumors, symptoms can include severe abdominal pain, irritation of the peritoneum
The peritoneum is the serous membrane forming the lining of the abdominal cavity or coelom in amniotes and some invertebrates, such as annelids. It covers most of the intra-abdominal (or coelomic) organs, and is composed of a layer of meso ...
, or bleeding
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vag ...
.amenorrhea
Amenorrhea is the absence of a menstrual period in a woman of reproductive age. Physiological states of amenorrhoea are seen, most commonly, during pregnancy and lactation (breastfeeding). Outside the reproductive years, there is absence of menses ...
. As the cancer becomes more advanced, it can cause an accumulation of fluid in the abdomen and lead to distension. If the malignancy has not been diagnosed by the time it causes ascites, it is typically diagnosed shortly thereafter.pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
.
Risk factors
There are many known risk factors that may increase a women's risk of developing ovarian cancer. The risk of developing ovarian cancer is related to the amount of time a woman spends ovulating.[
The risk of developing ovarian cancer is less for women who have fewer menstrual cycles, no menstrual cycles, ]breast feeding
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that brea ...
, take oral contraceptives, have multiple pregnancies, and have a pregnancy at an early age. The risk of developing ovarian cancer is reduced in women who have had tubal ligation
Tubal ligation (commonly known as having one's "tubes tied") is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus the ...
(colloquially known as having one's "tubes tied"), both ovaries removed, or hysterectomy (an operation in which the uterus is removed).
Hormones
The use of fertility medication may contribute to ovarian borderline tumor formation, but the link between the two is disputed and difficult to study.[ Fertility drugs may be associated with a higher risk of borderline tumors.][ The risk factor may instead be infertility itself, not the treatment.][
Hormonal conditions such as ]polycystic ovary syndrome
Polycystic ovary syndrome, or PCOS, is the most common endocrine disorder in women of reproductive age. The syndrome is named after the characteristic cysts which may form on the ovaries, though it is important to note that this is a sign and no ...
and endometriosis are associated with ovarian cancer, but the link is not completely confirmed.[ as is pain with menstruation. Endometriosis is associated with clear-cell and endometrioid subtypes, low-grade serous tumors, stage I and II tumors, grade 1 tumors, and lower mortality.][
]
Genetics
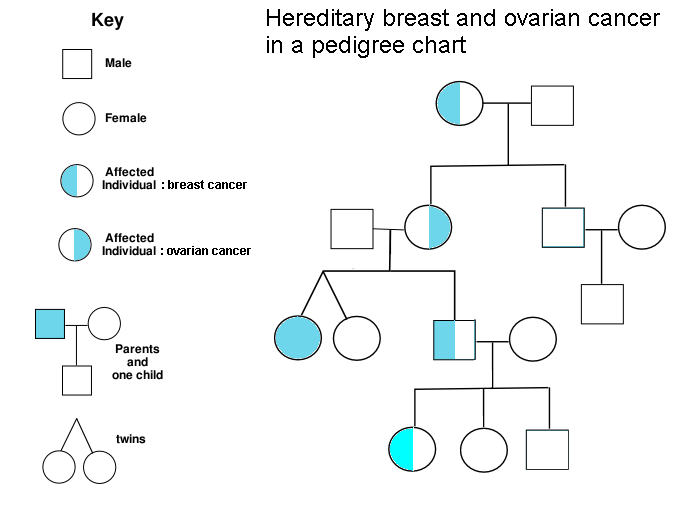 A family history of ovarian cancer is a risk factor for ovarian cancer. Women with hereditary nonpolyposis colon cancer (Lynch syndrome), and those with BRCA-1 and BRCA-2 genetic abnormalities are at increased risk.
The major genetic risk factor for ovarian cancer is a mutation in ''BRCA1'' or ''BRCA2'' genes, or in
A family history of ovarian cancer is a risk factor for ovarian cancer. Women with hereditary nonpolyposis colon cancer (Lynch syndrome), and those with BRCA-1 and BRCA-2 genetic abnormalities are at increased risk.
The major genetic risk factor for ovarian cancer is a mutation in ''BRCA1'' or ''BRCA2'' genes, or in DNA mismatch repair
DNA mismatch repair (MMR) is a system for recognizing and repairing erroneous insertion, deletion, and mis-incorporation of bases that can arise during DNA replication and recombination, as well as repairing some forms of DNA damage.
Mismatch ...
genes, which is present in 10% of ovarian cancer cases. Only one allele
An allele (, ; ; modern formation from Greek ἄλλος ''állos'', "other") is a variation of the same sequence of nucleotides at the same place on a long DNA molecule, as described in leading textbooks on genetics and evolution.
::"The chro ...
needs to be mutated to place a person at high risk. The gene can be inherited through either the maternal or paternal line, but has variable penetrance
Penetrance in genetics is the proportion of individuals carrying a particular variant (or allele) of a gene (the genotype) that also express an associated trait (the phenotype). In medical genetics, the penetrance of a disease-causing mutation is t ...
.[ Though mutations in these genes are usually associated with increased risk of breast cancer, they also carry a substantial lifetime risk of ovarian cancer, a risk that peaks in a person's 40s and 50s. The lowest risk cited is 30% and the highest 60%.][ Mutations in BRCA1 have a lifetime risk of developing ovarian cancer of 15–45%.][
In the United States, five of 100 women with a ]first-degree relative
A first-degree relative (FDR) is a person's parent (father or mother), full sibling (brother or sister) or child. It constitutes a category of family members that largely overlaps with the term nuclear family, but without spouses.
If the persons ...
with ovarian cancer will eventually get ovarian cancer themselves, placing those with affected family members at triple the risk of women with unaffected family members. Seven of 100 women with two or more relatives with ovarian cancer will eventually get ovarian cancer.[ BRCA mutations are associated with high-grade serous nonmucinous epithelial ovarian cancer.] A strong family history of endometrial cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known as
A strong family history of endometrial cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known as hereditary nonpolyposis colorectal cancer
Hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome is an autosomal dominant genetic condition that is associated with a high risk of colon cancer as well as other cancers including endometrial cancer (second most common), ovary, ...
(also known as Lynch syndrome), which confers a higher risk for developing a number of cancers, including ovarian cancer. Lynch syndrome is caused by mutations in mismatch repair genes, including ''MSH2
DNA mismatch repair protein Msh2 also known as MutS homolog 2 or MSH2 is a protein that in humans is encoded by the ''MSH2'' gene, which is located on chromosome 2. MSH2 is a tumor suppressor gene and more specifically a caretaker gene that codes ...
, MLH1, MLH6, PMS1
PMS1 protein homolog 1 is a protein that in humans is encoded by the ''PMS1'' gene.
Function
The protein encoded by this gene was identified by its homology to a yeast protein involved in DNA mismatch repair. A role for this protein in mismatch ...
'', and '' PMS2''.[ The risk of ovarian cancer for an individual with Lynch syndrome is between 10 and 12 percent.][ Women of Icelandic descent, European Jewish descent/ Ashkenazi Jewish descent, and Hungarian descent are at higher risk for epithelial ovarian cancer.][ Estrogen receptor beta gene ( ESR2) seems to be a key to pathogenesis and response to therapy. Other genes that have been associated with ovarian cancer are '' BRIP1'', '']MSH6
MSH6 or mutS homolog 6 is a gene that codes for DNA mismatch repair protein Msh6 in the budding yeast ''Saccharomyces cerevisiae''. It is the homologue of the human "G/T binding protein," (GTBP) also called p160 or hMSH6 (human MSH6). The MSH6 prot ...
'', ''RAD51C
RAD51 homolog C (S. cerevisiae), also known as RAD51C, is a protein which in humans is encoded by the ''RAD51C'' gene.
Function
The RAD51C protein is one of five paralogs of RAD51, including RAD51B ( RAD51L1), RAD51C (RAD51L2), RAD51D ( RAD51 ...
'' and ''RAD51D
DNA repair protein RAD51 homolog 4 is a protein that in humans is encoded by the ''RAD51L3'' gene.
Function
The protein encoded by this gene is a member of the RAD51 protein family. RAD51 family members are highly similar to bacterial RecA and ...
''.CHEK2
CHEK2 (Checkpoint kinase 2) is a tumor suppressor gene that encodes the protein CHK2, a serine-threonine kinase. CHK2 is involved in DNA repair, cell cycle arrest or apoptosis in response to DNA damage. Mutations to the CHEK2 gene have been linked ...
'', ''PALB2
Partner and localizer of BRCA2, also known as PALB2 or FANCN, is a protein which in humans is encoded by the ''PALB2'' gene.
Function
This gene encodes a protein that functions in genome maintenance ( double strand break repair). This prote ...
'' and ''RAD50
DNA repair protein RAD50, also known as RAD50, is a protein that in humans is encoded by the ''RAD50'' gene.
Function
The protein encoded by this gene is highly similar to ''Saccharomyces cerevisiae'' Rad50, a protein involved in DNA double- ...
'' have also been associated with ovarian cancer.Peutz–Jeghers syndrome
Peutz–Jeghers syndrome (often abbreviated PJS) is an autosomal dominant genetic disorder characterized by the development of benign hamartomatous polyps in the gastrointestinal tract and hyperpigmented macules on the lips and oral mucosa (melanos ...
, a rare genetic disorder, also predisposes women to sex cord tumour with annular tubules
Sex cord tumour with annular tubules (SCTAT) is a rare ovarian tumour in the sex cord group of gonadal tumours.
Pathology
These tumours may be seen in the context of Peutz–Jeghers syndrome or be sporadic. Large tumours are more likely to be s ...
.[ ]Ollier disease
Ollier disease is a rare sporadic nonhereditary skeletal disorder in which typically benign cartilaginous tumors (enchondromas) develop near the growth plate cartilage. This is caused by cartilage rests that grow and reside within the metaphysis o ...
and Maffucci syndrome
Maffucci syndrome is a very rare disorder in which multiple benign tumors of cartilage develop within the bones (such tumors are known as enchondromas). The tumors most commonly appear in the bones of the hands, feet, and limbs, causing bone deform ...
are associated with granulosa cell tumor
Granulosa cell tumours are tumours that arise from granulosa cells. They are estrogen secreting tumours and present as large, complex, ovarian masses. These tumours are part of the sex cord-gonadal stromal tumour or non-epithelial group of tumours ...
s in children and may also be associated with Sertoli-Leydig tumors. Benign fibromas are associated with nevoid basal cell carcinoma syndrome
Nevoid basal-cell carcinoma syndrome (NBCCS) is an inherited medical condition involving defects within multiple body systems such as the skin, nervous system, eyes, endocrine system, and bones. People with this syndrome are particularly prone to ...
.[
]
Diet
Alcohol consumption does not appear to be related to ovarian cancer.whole grain
A whole grain is a grain of any cereal and pseudocereal that contains the endosperm, germ, and bran, in contrast to refined grains, which retain only the endosperm.
As part of a general healthy diet, consumption of whole grains is associated w ...
s, and a diet that avoids or limits red and processed meat
Processed meat is considered to be any meat which has been modified in order to either improve its taste or to extend its shelf life. Methods of meat processing include salting, curing, fermentation, smoking, and/or the addition of chemical pre ...
s and processed sugar. High consumption of total, saturated and trans-fats increases ovarian cancer risk. A 2021 umbrella review found that coffee, egg, and fat intake significantly increases the risk of ovarian cancer. There is mixed evidence from studies on ovarian cancer risk and consumption of dairy product
Dairy products or milk products, also known as lacticinia, are food products made from (or containing) milk. The most common dairy animals are cow, water buffalo, nanny goat, and ewe. Dairy products include common grocery store food items in th ...
s.
Environmental factors
Industrialized nations, with the exception of Japan, have high rates of epithelial ovarian cancer, which may be due to diet in those countries. White women are at a 30–40% higher risk for ovarian cancer when compared to Black women and Hispanic women, likely due to socioeconomic factors; white women tend to have fewer children and different rates of gynecologic surgeries that affect risk for ovarian cancer.[
Tentative evidence suggests that ]talc
Talc, or talcum, is a Clay minerals, clay mineral, composed of hydrated magnesium silicate with the chemical formula Mg3Si4O10(OH)2. Talc in powdered form, often combined with corn starch, is used as baby powder. This mineral is used as a thi ...
, pesticides
Pesticides are substances that are meant to control pests. This includes herbicide, insecticide, nematicide, molluscicide, piscicide, avicide, rodenticide, bactericide, insect repellent, animal repellent, microbicide, fungicide, and lampric ...
, and herbicides
Herbicides (, ), also commonly known as weedkillers, are substances used to control undesired plants, also known as weeds.EPA. February 201Pesticides Industry. Sales and Usage 2006 and 2007: Market Estimates. Summary in press releasMain page fo ...
increase the risk of ovarian cancer. The American Cancer Society notes that as of now, no study has been able to accurately link any single chemical in the environment, or in the human diet, directly to mutations that cause ovarian cancer.
Other
Other factors that have been investigated, such as smoking
Smoking is a practice in which a substance is burned and the resulting smoke is typically breathed in to be tasted and absorbed into the bloodstream. Most commonly, the substance used is the dried leaves of the tobacco plant, which have bee ...
, low levels of vitamin D
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and many other biological effects. In humans, the most important compounds in this group are vitamin D3 (c ...
in the blood, presence of inclusion ovarian cysts
An ovarian cyst is a fluid-filled sac within the ovary. Often they cause no symptoms. Occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes ...
, and infection with human papilloma virus
Human papillomavirus infection (HPV infection) is caused by a DNA virus from the ''Papillomaviridae'' family. Many HPV infections cause no symptoms and 90% resolve spontaneously within two years. In some cases, an HPV infection persists and res ...
(the cause of some cases of cervical cancer
Cervical cancer is a cancer arising from the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Early on, typically no symptoms are seen. Later symptoms may include abnormal ...
), have been disproven as risk factors for ovarian cancer.talc
Talc, or talcum, is a Clay minerals, clay mineral, composed of hydrated magnesium silicate with the chemical formula Mg3Si4O10(OH)2. Talc in powdered form, often combined with corn starch, is used as baby powder. This mineral is used as a thi ...
is controversial, because it can act as an irritant if it travels through the reproductive tract to the ovaries.talc
Talc, or talcum, is a Clay minerals, clay mineral, composed of hydrated magnesium silicate with the chemical formula Mg3Si4O10(OH)2. Talc in powdered form, often combined with corn starch, is used as baby powder. This mineral is used as a thi ...
elsewhere on the body is unrelated to ovarian cancer.[ ]Sitting
Sitting is a basic action and resting position in which the body weight is supported primarily by the bony ischial tuberosities with the buttocks in contact with the ground or a horizontal surface such as a chair seat, instead of by the lower l ...
regularly for prolonged periods is associated with higher mortality from epithelial ovarian cancer. The risk is not negated by regular exercise, though it is lowered.[
]Smoking
Smoking is a practice in which a substance is burned and the resulting smoke is typically breathed in to be tasted and absorbed into the bloodstream. Most commonly, the substance used is the dried leaves of the tobacco plant, which have bee ...
tobacco is associated with a higher risk of mucinous ovarian cancer; after smoking cessation
Smoking cessation, usually called quitting smoking or stopping smoking, is the process of discontinuing tobacco smoking. Tobacco smoke contains nicotine, which is addictive and can cause dependence. As a result, nicotine withdrawal often make ...
, the risk eventually returns to normal. Higher levels of C-reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin-6 ...
are associated with a higher risk of developing ovarian cancer.
Protective factors
Suppression of ovulation, which would otherwise cause damage to the ovarian epithelium
The ovary is an organ in the female reproductive system that produces an ovum. When released, this travels down the fallopian tube into the uterus, where it may become fertilized by a sperm. There is an ovary () found on each side of the body. T ...
and, consequently, inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
, is generally protective. This effect can be achieved by having children, taking combined oral contraceptive
The combined oral contraceptive pill (COCP), often referred to as the birth control pill or colloquially as "the pill", is a type of birth control that is designed to be taken orally by women. The pill contains two important hormones: progesti ...
s, and breast feeding
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that brea ...
, all of which are protective factors.[ A longer period of breastfeeding correlates with a larger decrease in the risk of ovarian cancer.][ Each birth decreases risk of ovarian cancer more, and this effect is seen with up to five births. Combined oral contraceptives reduce the risk of ovarian cancer by up to 50%, and the protective effect of combined oral contraceptives can last 25–30 years after they are discontinued.][ Regular use of ]aspirin
Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and/or inflammation, and as an antithrombotic. Specific inflammatory conditions which aspirin is used to treat inc ...
or acetaminophen
Paracetamol, also known as acetaminophen, is a medication used to treat fever and mild to moderate pain. Common brand names include Tylenol and Panadol.
At a standard dose, paracetamol only slightly decreases body temperature; it is inferior ...
(paracetamol) may be associated with a lower risk of ovarian cancer; other NSAIDs do not seem to have a similar protective effect.Tubal ligation
Tubal ligation (commonly known as having one's "tubes tied") is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus th ...
is protective because carcinogen
A carcinogen is any substance, radionuclide, or radiation that promotes carcinogenesis (the formation of cancer). This may be due to the ability to damage the genome or to the disruption of cellular metabolic processes. Several radioactive substan ...
s are unable to reach the ovary and fimbriae via the vagina, uterus, and Fallopian tubes.Hysterectomy
Hysterectomy is the surgical removal of the uterus. It may also involve removal of the cervix, ovaries (oophorectomy), Fallopian tubes (salpingectomy), and other surrounding structures.
Usually performed by a gynecologist, a hysterectomy may b ...
reduces the risk, and removal of both Fallopian tubes and ovaries (bilateral salpingo-oophorectomy
In medicine, salpingo-oophorectomy is the removal of an ovary and its Fallopian tube. This procedure is most frequently associated with prophylactic surgery in response to the discovery of a BRCA mutation, particularly those of the normally tumo ...
) dramatically reduces the risk of not only ovarian cancer but breast cancer as well.carotene
The term carotene (also carotin, from the Latin ''carota'', "carrot") is used for many related unsaturated hydrocarbon substances having the formula C40Hx, which are synthesized by plants but in general cannot be made by animals (with the exc ...
, fiber
Fiber or fibre (from la, fibra, links=no) is a natural or artificial substance that is significantly longer than it is wide. Fibers are often used in the manufacture of other materials. The strongest engineering materials often incorporate ...
, and vitamin
A vitamin is an organic molecule (or a set of molecules closely related chemically, i.e. vitamers) that is an Nutrient#Essential nutrients, essential micronutrient that an organism needs in small quantities for the proper functioning of its ...
s with low amounts of fat—specifically, a diet with non-starchy vegetables (e.g. broccoli
Broccoli (''Brassica oleracea'' var. ''italica'') is an edible green plant in the cabbage family (family Brassicaceae, genus ''Brassica'') whose large flowering head, stalk and small associated leaves are eaten as a vegetable. Broccoli is cl ...
and onion
An onion (''Allium cepa'' L., from Latin ''cepa'' meaning "onion"), also known as the bulb onion or common onion, is a vegetable that is the most widely cultivated species of the genus ''Allium''. The shallot is a botanical variety of the onion ...
s) may be protective.flavanoid
Flavonoids (or bioflavonoids; from the Latin word ''flavus'', meaning yellow, their color in nature) are a class of polyphenolic secondary metabolites found in plants, and thus commonly consumed in the diets of humans.
Chemically, flavonoids ...
s and green tea
Green tea is a type of tea that is made from '' Camellia sinensis'' leaves and buds that have not undergone the same withering and oxidation process which is used to make oolong teas and black teas. Green tea originated in China, and since the ...
intake can significantly reduce ovarian cancer risk.
Pathophysiology
Ovarian cancer forms when errors in normal ovarian cell growth
Cell growth refers to an increase in the total mass of a cell, including both cytoplasmic, nuclear and organelle volume. Cell growth occurs when the overall rate of cellular biosynthesis (production of biomolecules or anabolism) is greater than ...
occur. Usually, when cells grow old or get damaged, they die
Die, as a verb, refers to death, the cessation of life.
Die may also refer to:
Games
* Die, singular of dice, small throwable objects used for producing random numbers
Manufacturing
* Die (integrated circuit), a rectangular piece of a semicondu ...
, and new cells take their place. Cancer starts when new cells form unneeded, and old or damaged cells do not die as they should. The buildup of extra cells often forms a mass of tissue called an ovarian tumor
Ovarian tumors, or ovarian neoplasms, are tumors arising from the ovary. They can be benign or malignant (ovarian cancer). They consist of mainly solid tissue, while ovarian cysts contain fluid.
Histopathologic classification
Ovarian tumors are ...
or growth. These abnormal cancer cells have many genetic abnormalities
A genetic disorder is a health problem caused by one or more abnormalities in the genome. It can be caused by a mutation in a single gene (monogenic) or multiple genes (polygenic) or by a chromosomal abnormality. Although polygenic disorders ...
that cause them to grow excessively.corpus luteum
The corpus luteum (Latin for "yellow body"; plural corpora lutea) is a temporary endocrine structure in female ovaries involved in the production of relatively high levels of progesterone, and moderate levels of estradiol, and inhibin A. It is t ...
. This structure needs to be repaired by dividing cells in the ovary.[ Continuous ovulation for a long time means more repair of the ovary by dividing cells, which can acquire mutations in each division.][
Overall, the most common gene mutations in ovarian cancer occur in '' NF1, BRCA1, BRCA2, ''and '' CDK12''. Type I ovarian cancers, which tend to be less aggressive, tend to have ]microsatellite instability
Microsatellite instability (MSI) is the condition of genetic hypermutability (predisposition to mutation) that results from impaired DNA mismatch repair (MMR). The presence of MSI represents phenotypic evidence that MMR is not functioning normal ...
in several genes, including both oncogenes (most notably '' BRAF'' and ''KRAS
''KRAS'' (Kirsten rat sarcoma virus) is a gene that provides instructions for making a protein called K-Ras, a part of the RAS/MAPK pathway. The protein relays signals from outside the cell to the cell's nucleus. These signals instruct the cell ...
'') and tumor suppressors (most notably '' PTEN'').p53
p53, also known as Tumor protein P53, cellular tumor antigen p53 (UniProt name), or transformation-related protein 53 (TRP53) is a regulatory protein that is often mutated in human cancers. The p53 proteins (originally thought to be, and often s ...
, BRCA1'', and ''BRCA2''.[ Low-grade cancers tend to have mutations in KRAS, whereas cancers of any grade that develop from low malignant potential tumors tend to have mutations in p53.][ Type I cancers tend to develop from precursor lesions, whereas Type II cancers can develop from a ]serous tubal intraepithelial carcinoma
In physiology, serous fluid or serosal fluid (originating from the Medieval Latin word ''serosus'', from Latin ''serum'') is any of various body fluids resembling serum, that are typically pale yellow or transparent and of a benign nature. The fl ...
.[ The most common mutations in BRCA1 and BRCA2 are the frameshift mutations that originated in a small founder effect, founding population of Ashkenazi Jews.][
Almost 100% of rare mucinous carcinomas have mutations in ''KRAS'' and amplifications of ''ERBB2'' (also known as ''Her2/neu'').][ Overall, 20% of ovarian cancers have mutations in ''Her2/neu''.][
Serous carcinomas may develop from ]serous tubal intraepithelial carcinoma
In physiology, serous fluid or serosal fluid (originating from the Medieval Latin word ''serosus'', from Latin ''serum'') is any of various body fluids resembling serum, that are typically pale yellow or transparent and of a benign nature. The fl ...
, rather than developing spontaneously from ovarian tissue. Other carcinomas develop from cortical inclusion cysts, which are groups of epithelial ovarian cells inside the stroma (animal tissue), stroma.[
]
Diagnosis
Examination

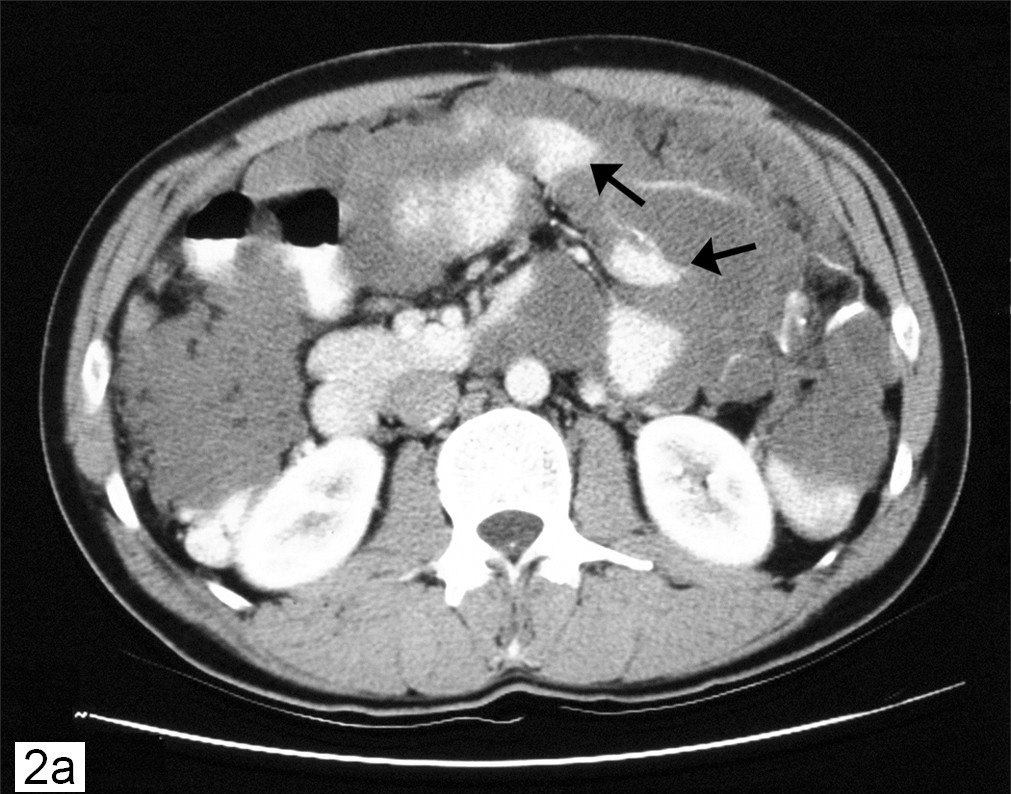
 Diagnosis of ovarian cancer starts with a physical examination (including a pelvic examination), a blood test (for CA-125 and sometimes other markers), and transvaginal ultrasound.
Diagnosis of ovarian cancer starts with a physical examination (including a pelvic examination), a blood test (for CA-125 and sometimes other markers), and transvaginal ultrasound.[ Sometimes a rectovaginal examination is used to help plan a surgery.][ The diagnosis must be confirmed with surgery to inspect the abdominal cavity, take biopsies (tissue samples for histopathology, microscopic analysis), and look for cancer cells in the abdominal fluid. This helps to determine if an ovarian mass is benign or malignant.][
Ovarian cancer's early stages (I/II) are difficult to diagnose because most symptoms are nonspecific and thus of little use in diagnosis; as a result, it is rarely diagnosed until it spreads and advances to later stages (III/IV). Additionally, symptoms of ovarian cancer may appear similar to ]irritable bowel syndrome
Irritable bowel syndrome (IBS) is a "disorder of gut-brain interaction" characterized by a group of symptoms that commonly include abdominal pain and or abdominal bloating and changes in the consistency of bowel movements. These symptoms may ...
. In women in whom pregnancy is a possibility, BHCG level can be measured during the diagnosis process. Serum alpha-fetoprotein, neuron-specific enolase, and lactate dehydrogenase can be measured in young girls and adolescents with suspected ovarian tumor
Ovarian tumors, or ovarian neoplasms, are tumors arising from the ovary. They can be benign or malignant (ovarian cancer). They consist of mainly solid tissue, while ovarian cysts contain fluid.
Histopathologic classification
Ovarian tumors are ...
s as younger women with ovarian cancer are more likely to have malignant germ cell tumors.ovarian torsion
Ovarian torsion (OT) or adnexal torsion is an abnormal condition where an ovary twists on its attachment to other structures, such that blood flow is decreased. Symptoms typically include pelvic pain on one side. While classically the pain is sud ...
, dermoid cyst, cystadenoma (serous or mucinous), Diverticular abscess, diverticular or appendiceal abscess, nerve sheath tumor, pelvic kidney, Ureteral diverticulum, ureteral or bladder diverticulum, benign cystic mesothelioma of the peritoneum, peritoneal tuberculosis, or paraovarian cyst. Ovaries that can be felt are also a sign of ovarian cancer in postmenopausal women. Other parts of a physical examination for suspected ovarian cancer can include a breast examination and a digital rectal exam. Palpation of the Supraclavicular lymph nodes, supraclavicular, Axillary lymph nodes, axillary, and Inguinal lymph node, inguinal lymph nodes may reveal lymphadenopathy, which can be indicative of metastasis. Another indicator may be the presence of a pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
, which can be noted on auscultation.[ when an ovarian cancer is present, these tests often show thrombocytosis, a high number of platelets (20–25% of patients) and hyponatremia, low blood sodium levels due to chemical signals secreted by the tumor.][ A positive test for inhibin A and inhibin B can indicate a granulosa cell tumor.]ovarian cysts
An ovarian cyst is a fluid-filled sac within the ovary. Often they cause no symptoms. Occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes ...
, systemic lupus erythematosus, liver disease, inflammatory bowel disease, pelvic inflammatory disease, and leiomyoma.pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
. Another test for metastatic disease, though it is infrequently used, is a barium enema, which can show if the rectosigmoid colon is involved in the disease. Positron emission tomography, bone scans, and paracentesis are of limited use; in fact, paracentesis can cause metastases to form at the needle insertion site and may not provide useful results.salpingo-oophorectomy
In medicine, salpingo-oophorectomy is the removal of an ovary and its Fallopian tube. This procedure is most frequently associated with prophylactic surgery in response to the discovery of a BRCA mutation, particularly those of the normally tumo ...
, removal of a single affected ovary and Fallopian tube. Fluid from the abdominal cavity can also be analyzed for cancerous Cell (biology), cells. If cancer is found, this procedure can also be used to determine the extent of its spread (which is a form of tumor staging).[
Pafolacianine is Indication (medicine), indicated for use in adults with ovarian cancer to help identify cancerous lesions during surgery.][ ]
Risk scoring
A widely recognized method of estimating the risk of malignant ovarian cancer is the risk of malignancy index (RMI), calculated based on an initial Medical diagnosis#Other diagnostic procedure methods, workup.[
Two methods can be used to determine the ultrasound score and menopausal score, with the resultant scores being referred to as RMI 1 and RMI 2, respectively, depending on what method is used.
Another method for quantifying risk of ovarian cancer is the Risk of Ovarian Cancer Algorithm (ROCA), which observes levels over time and determines if they are increasing rapidly enough to warrant transvaginal ultrasound.]
Pathology
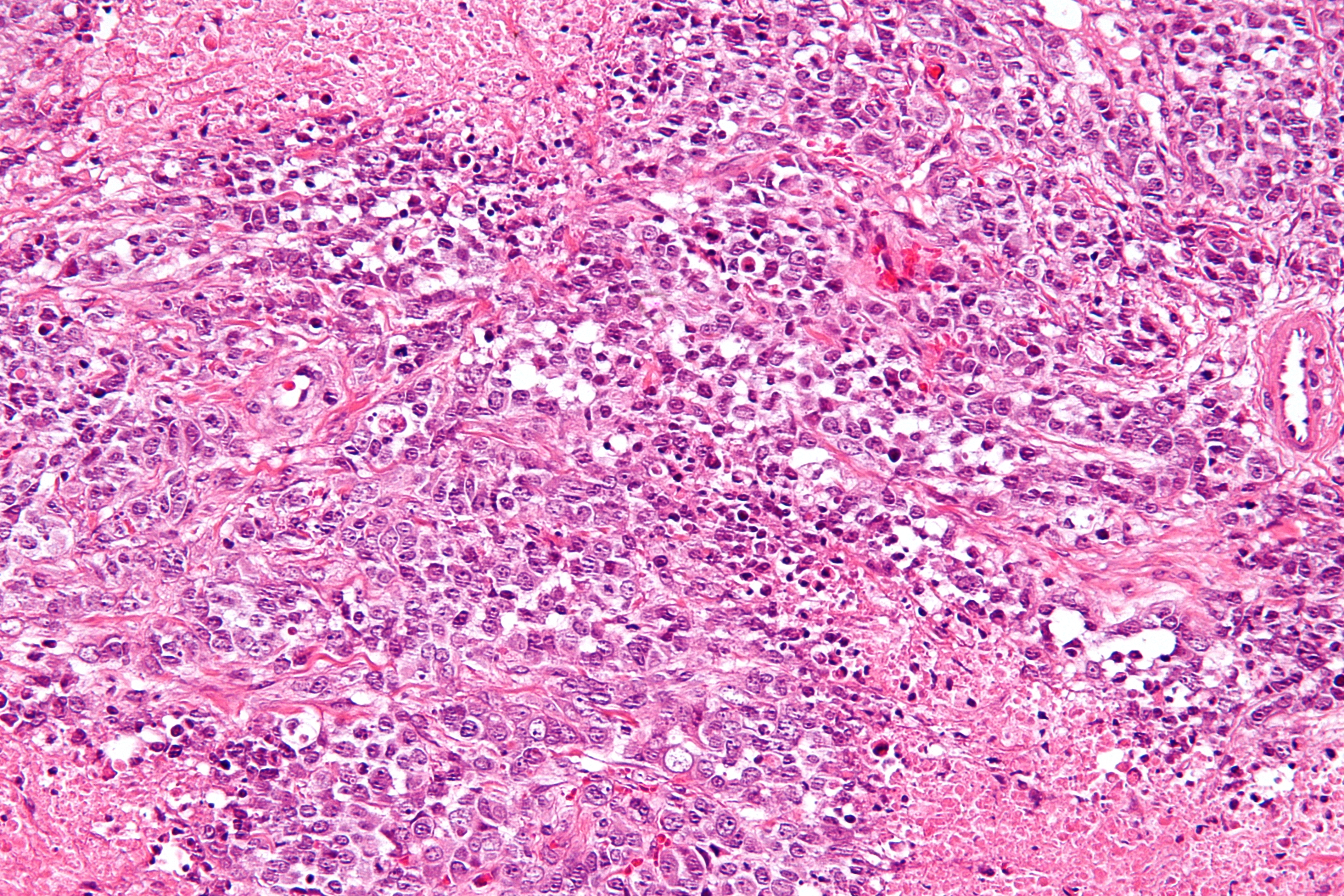
 Ovarian cancers are classified according to the microscopic appearance of their structures (histology or histopathology). Histology dictates many aspects of clinical treatment, management, and prognosis. The gross pathology of ovarian cancers is very similar regardless of histologic type: ovarian tumors have solid and cystic masses.
Ovarian cancers are classified according to the microscopic appearance of their structures (histology or histopathology). Histology dictates many aspects of clinical treatment, management, and prognosis. The gross pathology of ovarian cancers is very similar regardless of histologic type: ovarian tumors have solid and cystic masses.[
]
Epithelial carcinoma
 Epithelial ovarian cancer typically presents at an advanced stage and is derived from the malignant transformation of the epithelium of the ovarian surface, peritoneum, or fallopian tube.
Epithelial ovarian cancer typically presents at an advanced stage and is derived from the malignant transformation of the epithelium of the ovarian surface, peritoneum, or fallopian tube.
= Serous carcinoma
=
 Serous ovarian cancer is the most common type of epithelial ovarian cancer and it accounts for about two-thirds of cases of epithelial ovarian cancer.
Serous ovarian cancer is the most common type of epithelial ovarian cancer and it accounts for about two-thirds of cases of epithelial ovarian cancer.
= Small-cell carcinoma
=
 Small-cell carcinoma, Small-cell ovarian carcinoma is rare and aggressive, with two main subtypes: hypercalcemic and pulmonary.
Small-cell carcinoma, Small-cell ovarian carcinoma is rare and aggressive, with two main subtypes: hypercalcemic and pulmonary.
Primary peritoneal carcinoma
Primary peritoneal carcinomas develop from the peritoneum
The peritoneum is the serous membrane forming the lining of the abdominal cavity or coelom in amniotes and some invertebrates, such as annelids. It covers most of the intra-abdominal (or coelomic) organs, and is composed of a layer of meso ...
, a membrane that covers the abdominal cavity that has the same embryonic origin as the ovary. They are often discussed and classified with ovarian cancers when they affect the ovary.
= Clear-cell carcinoma
=
 Clear cell ovarian carcinoma is a rare subtype of epithelial ovarian cancer. Those diagnosed with clear cell ovarian carcinoma are typically younger at the age of diagnosis and diagnosed at earlier stages than other subtypes of epithelial ovarian cancer.
Clear cell ovarian carcinoma is a rare subtype of epithelial ovarian cancer. Those diagnosed with clear cell ovarian carcinoma are typically younger at the age of diagnosis and diagnosed at earlier stages than other subtypes of epithelial ovarian cancer.
= Clear-cell adenocarcinoma
=
 Clear-cell adenocarcinomas are histopathologically similar to other clear cell carcinomas, with clear cells and hobnail cells. They represent approximately 5–10% of epithelial ovarian cancers and are associated with endometriosis in the pelvic cavity. They are typically early-stage and therefore curable by surgery, but advanced clear-cell adenocarcinomas (approximately 20%) have a poor prognosis and are often resistant to platinum chemotherapy.
Clear-cell adenocarcinomas are histopathologically similar to other clear cell carcinomas, with clear cells and hobnail cells. They represent approximately 5–10% of epithelial ovarian cancers and are associated with endometriosis in the pelvic cavity. They are typically early-stage and therefore curable by surgery, but advanced clear-cell adenocarcinomas (approximately 20%) have a poor prognosis and are often resistant to platinum chemotherapy.
= Endometrioid
=
Endometrioid adenocarcinomas make up approximately 13-15% of all ovarian cancers.
Malignant mixed müllerian tumor (carcinosarcoma)
Mixed müllerian tumors make up less than 1% of ovarian cancer. They have epithelial and mesenchymal cells visible and tend to have a poor prognosis.
= Mucinous
=
Mucinous tumors include mucinous adenocarcinoma and mucinous cystadenocarcinoma.
Mucinous adenocarcinoma
Mucinous adenocarcinomas make up 5–10% of epithelial ovarian cancers. Histologically, they are similar to intestinal or cervical adenocarcinomas and are often actually metastases of appendiceal cancer, appendiceal or colon cancers. Advanced mucinous adenocarcinomas have a poor prognosis, generally worse than serous tumors, and are often resistant to platinum chemotherapy, though they are rare.
Pseudomyxoma peritonei
 ''Pseudomyxoma peritonei'' refers to a collection of encapsulated mucous or gelatinous material in the abdominopelvic cavity, which is very rarely caused by a primary mucinous ovarian tumor. More commonly, it is associated with ovarian metastases of intestinal cancer.
''Pseudomyxoma peritonei'' refers to a collection of encapsulated mucous or gelatinous material in the abdominopelvic cavity, which is very rarely caused by a primary mucinous ovarian tumor. More commonly, it is associated with ovarian metastases of intestinal cancer.
= Undifferentiated epithelial
=
Undifferentiated cancers - those where the cell type cannot be determined - make up about 10% of epithelial ovarian cancers and have a comparatively poor prognosis.
Malignant Brenner tumor
 Malignant Brenner tumors are rare. Histologically, they have dense fibrous stroma with areas of transitional epithelium and some squamous differentiation. To be classified as a malignant Brenner tumor, it must have Brenner tumor foci and transitional cell carcinoma. The transitional cell carcinoma component is typically poorly differentiated and resembles urinary tract cancer.
Malignant Brenner tumors are rare. Histologically, they have dense fibrous stroma with areas of transitional epithelium and some squamous differentiation. To be classified as a malignant Brenner tumor, it must have Brenner tumor foci and transitional cell carcinoma. The transitional cell carcinoma component is typically poorly differentiated and resembles urinary tract cancer.
Transitional cell carcinoma
Transitional cell carcinomas represent less than 5% of ovarian cancers. Histologically, they appear similar to bladder carcinoma. The prognosis is intermediate - better than most epithelial cancers but worse than malignant Brenner tumors.
Sex cord-stromal tumor
Sex cord-stromal tumour, Sex cord-stromal tumor, including estrogen-producing granulosa cell tumor
Granulosa cell tumours are tumours that arise from granulosa cells. They are estrogen secreting tumours and present as large, complex, ovarian masses. These tumours are part of the sex cord-gonadal stromal tumour or non-epithelial group of tumours ...
, the benign thecoma, and virilizing Sertoli-Leydig cell tumor or arrhenoblastoma, accounts for 7% of ovarian cancers. They occur most frequently in women between 50 and 69 years of age but can occur in women of any age, including young girls. They are not typically aggressive and are usually unilateral;[ they are therefore usually treated with surgery alone. Sex cord-stromal tumors are the main hormone-producing ovarian tumors.]ovarian torsion
Ovarian torsion (OT) or adnexal torsion is an abnormal condition where an ovary twists on its attachment to other structures, such that blood flow is decreased. Symptoms typically include pelvic pain on one side. While classically the pain is sud ...
, hemorrhage from or rupture of the tumor, an abdominal mass, and hormonal disruption. In children, precocious puberty#Isosexual and heterosexual, isosexual precocious pseudopuberty may occur with granulosa cell tumors since they produce estrogen. These tumors cause abnormalities in menstruation (menometrorrhagia, excessive bleeding, oligomenorrhea, infrequent menstruation, or amenorrhea, no menstruation) or postmenopausal bleeding. Because these tumors produce estrogen, they can cause or occur at the same time as endometrial cancer or breast cancer. Other sex-cord/stromal tumors present with distinct symptoms. Sertoli-Leydig cell tumors cause virilization
Virilization or masculinization is the biological development of adult male characteristics in young males or females. Most of the changes of virilization are produced by androgens.
Virilization is most commonly used in three medical and biology ...
and hirsutism, excessive hair growth due to the production of testosterone and androstenedione, which can also cause Cushing's syndrome in rare cases. Also, sex-cord stromal tumors occur that do not cause a hormonal imbalance, including benign fibromas, which cause ascites and hydrothorax.[ With germ cell tumors, sex cord-stromal tumors are the most common ovarian cancer diagnosed in women under 20.][
]
= Granulosa cell tumor
=
Granulosa cell tumors are the most common sex-cord stromal tumors, making up 70% of cases, and are divided into two histologic subtypes: adult granulosa cell tumors, which develop in women over 50, and juvenile granulosa tumors, which develop before puberty or before the age of 30. Both develop in the ovarian follicle from a population of cells that surrounds germinal cells.
Adult granulosa cell tumor
Adult granulosa cell tumors are characterized by later onset (30+ years, 50 on average). These tumors produce high levels of estrogen, which causes its characteristic symptoms: menometrorrhagia; endometrial hyperplasia; Breast pain, tender, Breast enlargement, enlarged breasts; Vaginal bleeding, postmenopausal bleeding; and Amenorrhoea, secondary amenorrhea. The mass of the tumor can cause other symptoms, including abdominal pain and distension, or symptoms similar to an ectopic pregnancy if the tumor bleeds and ruptures.
Juvenile granulosa cell tumor
= Sertoli-Leydig cell tumor
=
Sertoli-Leydig tumors are most common in women before the age of 30, and particularly common before puberty.
= Sclerosing stromal tumors
=
Sclerosing stromal tumors typically occur in girls before puberty or women before the age of 30.
Germ cell tumor
Germ cell tumors of the ovary develop from the ovarian germ cells.teratoma
A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the ovary, testicle, or coccyx.
Symptoms
Symptoms may be minimal if the tumor is small. A testicular ter ...
s and most teratomas are benign. Malignant teratomas tend to occur in older women, when one of the germ layers in the tumor develops into a squamous cell carcinoma.[ Germ-cell tumors tend to occur in young women (20s–30s) and girls, making up 70% of the ovarian cancer seen in that age group.][ Most germ-cell cancers have a better prognosis than other subtypes and are more sensitive to chemotherapy. They are more likely to be stage I at diagnosis.][
Germ-cell tumors are typically discovered when they become large, palpable masses. However, like sex cord tumors, they can cause ovarian torsion or hemorrhage and, in children, isosexual precocious puberty. They frequently metastasize to nearby lymph nodes, especially para-aortic and pelvic lymph nodes.][ The most common symptom of germ cell tumors is Abdominal pain, subacute abdominal pain caused by the tumor bleeding, Necrosis, necrotizing, or stretching the ovarian capsule. If the tumor ruptures, causes significant bleeding, or torses the ovary, it can cause Acute abdomen, acute abdominal pain, which occurs in less than 10% of those with germ-cell tumors. They can also secrete hormones which change the menstrual cycle. In 25% of germ-cell tumors, the cancer is discovered during a Well-woman examination, routine examination and does not cause symptoms.]
= Dysgerminoma
=
 Dysgerminoma accounts for 35% of ovarian cancer in young women and is the most likely germ cell tumor to metastasize to the lymph nodes; nodal metastases occur in 25–30% of cases.
Dysgerminoma accounts for 35% of ovarian cancer in young women and is the most likely germ cell tumor to metastasize to the lymph nodes; nodal metastases occur in 25–30% of cases. They are composed of cells that cannot Cellular differentiation, differentiate further and develop directly from germ cells or from gonadoblastomas. Dysgerminomas contain syncytiotrophoblasts in approximately 5% of cases, and can therefore cause elevated hCG levels. On gross appearance, dysgerminomas are typically pink to tan-colored, have multiple lobes, and are solid. Microscopically, they appear identical to seminomas and very close to Embryonic germ cell, embryonic primordial germ cells, having large, polyhedral, rounded clear cells. The nuclei are uniform and round or square with prominent Nucleolus, nucleoli and the cytoplasm has high levels of glycogen. Inflammation is another prominent histologic feature of dysgerminomas.
They are composed of cells that cannot Cellular differentiation, differentiate further and develop directly from germ cells or from gonadoblastomas. Dysgerminomas contain syncytiotrophoblasts in approximately 5% of cases, and can therefore cause elevated hCG levels. On gross appearance, dysgerminomas are typically pink to tan-colored, have multiple lobes, and are solid. Microscopically, they appear identical to seminomas and very close to Embryonic germ cell, embryonic primordial germ cells, having large, polyhedral, rounded clear cells. The nuclei are uniform and round or square with prominent Nucleolus, nucleoli and the cytoplasm has high levels of glycogen. Inflammation is another prominent histologic feature of dysgerminomas.
= Choriocarcinoma
=
Choriocarcinoma can occur as a primary ovarian tumor developing from a germ cell, though it is usually a gestational disease that metastasizes to the ovary. Primary ovarian choriocarcinoma has a poor prognosis and can occur without a pregnancy. They produce high levels of hCG and can cause Precocious puberty, early puberty in children or menometrorrhagia (irregular, heavy menstruation) after menarche.
= Immature (solid) teratoma
=
 Immature, or solid, teratomas are the most common type of ovarian germ cell tumor, making up 40–50% of cases. Teratomas are characterized by the presence of disorganized tissues arising from all three embryonic germ layers: ectoderm, mesoderm, and endoderm; immature teratomas also have undifferentiated stem cells that make them more malignant than mature teratomas (dermoid cysts). The different tissues are visible on gross pathology and often include bone, cartilage, hair, mucus, or Sebaceous gland, sebum, but these tissues are not visible from the outside, which appears to be a solid mass with lobes and cysts. Histologically, they have large amounts of neuroectoderm organized into sheets and tubules along with Neuroglia, glia; the amount of neural tissue determines the histologic grade. Immature teratomas usually only affect one ovary (10% co-occur with dermoid cysts) and usually metastasize throughout the peritoneum. They can also cause mature teratoma implants to grow throughout the abdomen in a disease called growing teratoma syndrome; these are usually benign but will continue to grow during chemotherapy, and often necessitate further surgery. Unlike mature teratomas, immature teratomas form many Adhesion (medicine), adhesions, making them less likely to cause ovarian torsion. There is no specific marker for immature teratomas, but carcinoembryonic antigen (CEA), CA-125, CA19-9, or AFP can sometimes indicate an immature teratoma.
Immature, or solid, teratomas are the most common type of ovarian germ cell tumor, making up 40–50% of cases. Teratomas are characterized by the presence of disorganized tissues arising from all three embryonic germ layers: ectoderm, mesoderm, and endoderm; immature teratomas also have undifferentiated stem cells that make them more malignant than mature teratomas (dermoid cysts). The different tissues are visible on gross pathology and often include bone, cartilage, hair, mucus, or Sebaceous gland, sebum, but these tissues are not visible from the outside, which appears to be a solid mass with lobes and cysts. Histologically, they have large amounts of neuroectoderm organized into sheets and tubules along with Neuroglia, glia; the amount of neural tissue determines the histologic grade. Immature teratomas usually only affect one ovary (10% co-occur with dermoid cysts) and usually metastasize throughout the peritoneum. They can also cause mature teratoma implants to grow throughout the abdomen in a disease called growing teratoma syndrome; these are usually benign but will continue to grow during chemotherapy, and often necessitate further surgery. Unlike mature teratomas, immature teratomas form many Adhesion (medicine), adhesions, making them less likely to cause ovarian torsion. There is no specific marker for immature teratomas, but carcinoembryonic antigen (CEA), CA-125, CA19-9, or AFP can sometimes indicate an immature teratoma.
= Mature teratoma (dermoid cyst)
=
Mature teratomas, or dermoid cysts, are rare tumors consisting of mostly benign tissue that develop after menopause. The tumors consist of disorganized tissue with nodules of malignant tissue, which can be of various types. The most common malignancy is Squamous-cell carcinoma, squamous cell carcinoma, but adenocarcinoma, basal-cell carcinoma, Carcinoid, carcinoid tumor, neuroectodermal tumor, Melanoma, malignant melanoma, sarcoma, Sebaceous carcinoma, sebaceous tumor, and struma ovarii can also be part of the dermoid cyst. They are treated with surgery and adjuvant platinum chemotherapy or radiation.
= Yolk sac tumor/endodermal sinus tumor
=
Yolk sac tumors, formerly called endodermal sinus tumors, make up approximately 10–20% of ovarian germ cell malignancies, and have the worst prognosis of all ovarian germ cell tumors. They occur both before menarche (in one-third of cases) and after menarche (the remaining two-thirds of cases). Half of the people with yolk sac tumors are diagnosed in stage I. Typically, they are unilateral until metastasis, which occurs within the peritoneal cavity and via the bloodstream to the lungs. Yolk sac tumors grow quickly and recur easily, and are not easily treatable once they have recurred. Stage I yolk sac tumors are highly treatable, with a 5-year disease-free survival rate of 93%, but stage II-IV tumors are less treatable, with survival rates of 64–91%.
= Embryonal carcinoma
=
Embryonal carcinomas, a rare tumor type usually found in mixed tumors, develop directly from germ cells but are not terminally differentiated; in rare cases, they may develop in dysgenetic gonads. They can develop further into a variety of other neoplasms, including choriocarcinoma, yolk sac tumor, and teratoma. They occur in younger people, with an average age at diagnosis of 14, and secrete both alpha-fetoprotein (in 75% of cases) and hCG.
= Polyembryoma
=
Polyembryomas, the most immature form of teratoma and very rare ovarian tumors, are histologically characterized by having several embryo-like bodies with structures resembling a germ disk, yolk sac, and amniotic sac. Syncytiotrophoblast, Syncytiotrophoblast giant cells also occur in polyembryomas.
Squamous cell carcinoma
Primary ovarian squamous cell carcinomas are rare and have a poor prognosis when advanced. More typically, ovarian squamous cell carcinomas are cervical metastases, areas of differentiation in an endometrioid tumor, or derived from a mature teratoma.
Mixed tumors
Mixed tumors contain elements of more than one of the above classes of tumor histology. To be classed as a mixed tumor, the minor type must make up more than 10% of the tumor.
Secondary ovarian cancer
Ovarian cancer can also be a secondary cancer, the result of metastasis from a primary cancer elsewhere in the body.[ About 5-30% of ovarian cancers are due to metastases, while the rest are primary cancers.][ ] Common primary cancers are breast cancer, colon cancer, appendiceal cancer, and stomach cancer (primary gastric cancers that metastasize to the ovary are called Krukenberg tumors).[ Krukenberg tumors have signet ring cells and mucinous cells.]
Borderline tumors
Ovarian borderline tumors, sometimes called low malignant potential (LMP) ovarian tumors, have some benign and some malignant features.[ Implants of LMP tumors are often non-invasive.]
Staging
Ovarian cancer is staged using the International Federation of Gynecology and Obstetrics, FIGO staging system and uses information obtained after surgery, which can include a total Hysterectomy, abdominal hysterectomy via Laparotomy, midline laparotomy, Salpingoophorectomy, removal of (usually) both ovaries and Fallopian tubes, Omentectomy, (usually) the omentum, pelvic washing, pelvic (peritoneal) washings, assessment of Retroperitoneal lymph node dissection, retroperitoneal lymph nodes (including the Pelvic lymph nodes, pelvic and Paraaortic lymph node, para-aortic lymph nodes), appendectomy in suspected mucinous tumors, and pelvic/peritoneal biopsies for cytopathology.[ Around 30% of ovarian cancers that appear confined to the ovary have metastasized microscopically, which is why even stage-I cancers must be staged completely.][ 22% of cancers presumed to be stage I are observed to have lymphatic metastases.][
]
FIGO
 File:Diagram showing stage 1 ovarian cancer CRUK 193.svg, Stage 1 ovarian cancer
File:Diagram showing stage 2A to 2C ovarian cancer CRUK 214.svg, Stage 2 ovarian cancer
File:Diagram showing stage 3A to 3C ovarian cancer CRUK 225.svg, Stage 3 ovarian cancer
File:Diagram showing stage 4 ovarian cancer CRUK 233.svg, Stage 4 ovarian cancer
File:Diagram showing stage 1 ovarian cancer CRUK 193.svg, Stage 1 ovarian cancer
File:Diagram showing stage 2A to 2C ovarian cancer CRUK 214.svg, Stage 2 ovarian cancer
File:Diagram showing stage 3A to 3C ovarian cancer CRUK 225.svg, Stage 3 ovarian cancer
File:Diagram showing stage 4 ovarian cancer CRUK 233.svg, Stage 4 ovarian cancer
AJCC/TNM
The AJCC/TNM staging system indicates where the tumor has developed, spread to lymph nodes, and metastasis.
Grading
Grade 1 tumors have well differentiated cells (look very similar to the normal tissue) and are the ones with the best prognosis. Grade 2 tumors are also called moderately well-differentiated and they are made up of cells that resemble the normal tissue. Grade 3 tumors have the worst prognosis and their cells are abnormal, referred to as poorly differentiated.
Metastasis in ovarian cancer is very common in the abdomen and occurs via exfoliation, where cancer cells burst through the ovarian capsule and are able to move freely throughout the peritoneal cavity. Ovarian cancer metastases usually grow on the surface of organs rather than the inside; they are also common on the omentum and the peritoneal lining. Cancer cells can also travel through the lymphatic system and metastasize to lymph nodes connected to the ovaries via blood vessels; i.e. the lymph nodes along the Suspensory ligament of ovary, infundibulopelvic ligament, the Broad ligament of the uterus, broad ligament, and the Round ligament of uterus, round ligament. The most commonly affected groups include the paraaortic lymph node, paraaortic, hypogastric lymph node, hypogastric, external iliac lymph nodes, external iliac, obturator lymph nodes, obturator, and inguinal lymph nodes. Usually, ovarian cancer does not metastasize to the liver, lung, brain, or kidneys unless it is a recurrent disease; this differentiates ovarian cancer from many other forms of cancer.
Prevention
Women with strong genetic risk for ovarian cancer may consider the surgical removal of their ovaries as a preventive measure. This is often done after completion of childbearing years. This reduces the chances of developing both breast cancer (by around 50%) and ovarian cancer (by about 96%) in women at high risk. Women with ''BRCA'' gene mutations usually also have their Fallopian tubes removed at the same time (salpingo-oophorectomy), since they also have an increased risk of Fallopian tube cancer. However, these statistics may overestimate the risk reduction because of how they have been studied.[
Women with a significant family history for ovarian cancer are often referred to a genetic counselor to see if testing for BRCA mutations would be beneficial.][ The use of oral contraceptives, the absence of 'periods' during the menstrual cycle, and tubal ligation reduce the risk.]talc
Talc, or talcum, is a Clay minerals, clay mineral, composed of hydrated magnesium silicate with the chemical formula Mg3Si4O10(OH)2. Talc in powdered form, often combined with corn starch, is used as baby powder. This mineral is used as a thi ...
have not been identified as increasing the risk for developing ovarian cancer.[
]
Screening
There is no simple and reliable way to test for ovarian cancer in women who do not have any signs or symptoms. Screening is not recommended in women who are at average risk, as evidence does not support a reduction in death and the high rate of false positive tests may lead to unneeded surgery, which is accompanied by its own risks.[ Women with high risk of ovarian cancer that are currently identified based on family history and genetic testing may benefit from screening.][
Ovarian cancer is usually only palpable in advanced stages.][ Screening is not recommended using CA-125 measurements, HE4 levels, ultrasound, or adnexal palpation in women who are at average risk. This high risk group has benefited with earlier detection.][
Screening with transvaginal ultrasound, pelvic examination, and CA-125 levels can be used instead of preventive surgery in women who have BRCA1 or BRCA2 mutations. This strategy has shown some success.][
Screening for CA125, a chemical released by ovarian tumours, with follow-up using ultrasound, was shown to be ineffective in reducing mortality in a large-scale UK study.
There have been some screening trials that have used age, family history of ovarian cancer, and mutation status to identify target populations for screening.]
Management
Once it is determined that ovarian, fallopian tube or primary peritoneal cancer is present, treatment is scheduled by a gynecologic oncologist (a physician trained to treat cancers of a woman's reproductive system). Gynecologic oncologists can perform surgery on and give chemotherapy to women with ovarian cancer. A treatment plan is developed.chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs ( chemotherapeutic agents or alkylating agents) as part of a standardized chemotherapy regimen. Chemothe ...
, and sometimes radiotherapy, regardless of the subtype of ovarian cancer.
Surgery
Surgery has been the standard of care for decades and may be necessary for obtaining a specimen for medical diagnosis, diagnosis. The surgery depends upon the extent of nearby invasion of other tissues by the cancer when it is diagnosed. This extent of the cancer is described by assigning it a stage, the presumed type, and the grade of cancer. The gynecological surgeon may remove one (unilateral oophorectomy) or both ovaries (bilateral oophorectomy). The Fallopian tubes (salpingectomy), uterus (hysterectomy), and the Greater omentum, omentum (omentectomy) may also be removed. Typically, all of these organs are removed.[ but a recent study has shown a longer overall survival in recurrent ovarian cancer when surgery combined with chemotherapy was performed compared to treatment with chemotherapy alone. Computed tomography (abdominal CT) is often used to assess if primary debulking surgery is possible, but low certainty evidence also suggests fluorodeoxyglucose‐18 (FDG) PET/CT and MRI may be useful as an addition for assessing macroscopic incomplete debulking. More complete debulking is associated with better outcomes: women with no macroscopic evidence of disease after debulking have a median survival of 39 months, as opposed to 17 months with less complete surgery.][ By removing metastases, many cells that are resistant to chemotherapy are removed, and any clumps of cells that have died are also removed. This allows chemotherapy to better reach the remaining cancer cells, which are more likely to be fast-growing and therefore chemosensitive.][ This is particularly important in germ cell tumors because they frequently metastasize to nearby lymph nodes.][
If ovarian cancer recurs, secondary surgery is sometimes a treatment option. This depends on how easily the tumor can be removed, how much fluid has accumulated in the abdomen, and overall health.][ Effectivenes of this surgery depends on surgical technique, completeness of cytoreduction, and extent of disease. It also can be helpful in people who had their first surgery done by a generalist and in epithelial ovarian cancer.]menopause
Menopause, also known as the climacteric, is the time in women's lives when menstrual periods stop permanently, and they are no longer able to bear children. Menopause usually occurs between the age of 47 and 54. Medical professionals often ...
, which can cause osteoporosis. After surgery, hormone replacement therapy can be considered, especially in younger women. This therapy can consist of a combination of estrogen and progesterone, or estrogen alone. Estrogen alone is safe after hysterectomy; when the uterus is still present, unopposed estrogen dramatically raises the risk of endometrial cancer.[ Estrogen therapy after surgery does not change survival rates.]
Chemotherapy
Chemotherapy has been a general standard of care for ovarian cancer for decades, although with variable protocols. Chemotherapy is used after surgery to treat any residual disease, if appropriate. In some cases, there may be reason to perform chemotherapy first, followed by surgery. This is called "neoadjuvant chemotherapy", and is common when a tumor cannot be completely removed or optimally debulked via surgery. Though it has not been shown to increase survival, it can reduce the risk of complications after surgery. If a unilateral salpingo-oophorectomy or other surgery is performed, additional chemotherapy, called "adjuvant chemotherapy", can be given.[ Germ-cell tumors and malignant sex-cord/stromal tumors are treated with chemotherapy, though dysgerminomas and sex-cord tumors are not typically very responsive.][
]
Platinum-sensitive or platinum-resistant
If ovarian cancer recurs, it is considered partially platinum-sensitive or platinum-resistant, based on the time since the last recurrence treated with platins: partially platinum-sensitive cancers recurred 6–12 months after last treatment, and platinum-resistant cancers have an interval of less than 6 months. Second-line chemotherapy can be given after the cancer becomes symptomatic because no difference in survival is seen between treating asymptomatic (elevated CA-125) and symptomatic recurrences.
For platinum-sensitive tumors, platins are the drugs of choice for second-line chemotherapy, in combination with other cytotoxic agents. Regimens include carboplatin combined with doxorubicin#Liposomal formulations, pegylated liposomal doxorubicin, gemcitabine, or paclitaxel.
Radiation therapy
Dysgerminomas are most effectively treated with radiation,[ though this can cause infertility and is being phased out in favor of chemotherapy.][ Radiation therapy does not improve survival in people with well-differentiated tumors.]
Hormonal therapy
Despite the fact that 60% of ovarian tumors have estrogen receptors, ovarian cancer is only rarely responsive to hormonal treatments. A Cochrane review found a lack of evidence about the effects of tamoxifen in people with relapsed ovarian cancer. Estrogen alone does not have an effect on the cancer, and tamoxifen and letrozole are rarely effective.[ "Some women with borderline malignancy ovarian cancer and stromal ovarian cancer may receive hormonal therapy."][
]
Immunotherapy
Immunotherapy is a topic of current research in ovarian cancer. In some cases, the antibody drug bevacizumab, though still a topic of active research, is used to treat advanced cancer along with chemotherapy.
Follow-up
Specific follow-up depends on, for example, the type and stage of ovarian cancer, the treatment, and the presence of any symptoms. Usually, a check-up appointment is made about every 2 to 3 months initially, followed by twice per year for up to 5 years. For epithelial ovarian cancers, the most common test upon follow-up is CA-125 level. However, treatment based only on elevated CA-125 levels and not any symptoms can increase side effects without any prolongation of life, so the implication of the outcome of a CA-125 test can be discussed before taking it.[Follow-up care]
from American Cancer Society. Last Medical Review: 03/21/2013. Last Revised: 02/06/2014 The recommendation as of 2014 is recurrent cancer may be present if the CA-125 level is twice normal.[ Treating a recurrence detected by CA-125 does not improve survival.][ Inhibin can also be useful for monitoring the progress of sex-cord tumors, along with mullerian inhibiting substance. AFP can also be used to monitor Sertoli-Leydig tumors.][ In dysgerminomas, lactate dehydrogenase and its two isozymes (LDH-1 and LDH-2) are used to test for recurrence.][, which cites
* ] Imaging without these indications is discouraged because it is unlikely to detect a recurrence, improve survival, and because it has its own costs and side effects.[ If a tumor is easily imaged, imaging may be used to monitor the progress of treatment.
]
Palliative care
Palliative care focuses on relieving symptoms and increasing or maintaining quality of life. This type of treatment's purpose is not to cure the cancer but to make the woman more comfortable while living with cancer that can not be cured. It has been recommended as part of the treatment plan for any person with advanced ovarian cancer or patients with significant symptoms. In platinum-refractory and platinum-resistant cases, other palliative chemotherapy is the main treatment.[
Palliative care can entail treatment of symptoms and complications of the cancer, including pain, nausea, constipation, ascites, bowel obstruction, edema, ]pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
, and mucositis. Especially if the cancer advances and becomes incurable, treatment of symptoms becomes one of the main goals of therapy. Palliative care can also entail helping with decision-making such as if or when hospice care is appropriate, and the preferred place for the patient at end of life care.
Psychosocial care
Ovarian cancer has a significant effect on quality of life, psychological health and well-being. Interventions are available to help with the needs and social support. Many ovarian cancer survivors report a good quality of life and optimism. Others reported a "spiritual change" that helped them find Meaning of life, meaning during their experience. Others have described their loss of faith after their diagnosis with ovarian cancer. Those who have gone through treatment sometimes experience social isolation but benefit from having relationships with other survivors. Frustration and Guilt (emotion), guilt have been described by some who have expressed their inability to care for their family.menopause
Menopause, also known as the climacteric, is the time in women's lives when menstrual periods stop permanently, and they are no longer able to bear children. Menopause usually occurs between the age of 47 and 54. Medical professionals often ...
that can result in Dyspareunia, painful intercourse, vaginal dryness, loss of Hypoactive sexual desire disorder, sexual desire and being tired. Though prognosis is better for younger survivors, the impact on sexuality can still be substantial.
Prognosis
 Ovarian cancer usually has a relatively poor prognosis. It is disproportionately deadly because it lacks any clear early detection or screening test, meaning most cases are not diagnosed until they have reached advanced stages.
Ovarian cancer usually has a relatively poor prognosis. It is disproportionately deadly because it lacks any clear early detection or screening test, meaning most cases are not diagnosed until they have reached advanced stages.[
Ovarian cancer metastasizes early in its development, often before it has been diagnosed. High-grade tumors metastasize more readily than low-grade tumors. Typically, tumor cells begin to metastasize by growing in the peritoneal cavity.][ More than 60% of women presenting with ovarian cancer have stage-III or stage-IV cancer, when it has already spread beyond the ovaries. Ovarian cancers shed cells into the naturally occurring fluid within the abdominal cavity. These cells can then implant on other abdominal (peritoneal) structures, including the uterus, urinary bladder, bowel, mesentery, lining of the bowel wall, and Greater omentum, omentum, forming new tumor growths before cancer is even suspected.
The five-year survival rate for all stages of ovarian cancer is 46%; the one-year survival rate is 72% and the ten-year survival rate is 35%. For cases where a diagnosis is made early in the disease, when the cancer is still confined to the primary site, the five-year survival rate is 92.7%.][Survival rates based on SEER incidence and NCHS mortality statistics, as cited by the National Cancer Institute i]
SEER Stat Fact Sheets — Cancer of the Ovary
About 70% of women with advanced disease respond to initial treatment, most of whom attain complete remission, but half of these women experience a recurrence 1–4 years after treatment.[ Brain metastasis is more common in stage III/IV cancer but can still occur in cancers staged at I/II. People with brain metastases survive a median of 8.2 months, though surgery, chemotherapy, and Whole brain radiotherapy, whole brain radiation therapy can improve survival.][ Around two-thirds of dysgerminomas are diagnosed at stage I.][ Low malignant potential tumors usually only have a bad prognosis when there are invasive tumor implants found in the peritoneal cavity.][
Complications of ovarian cancer can include spread of the cancer to other organs, progressive function loss of various organs, ascites, and intestinal obstructions, which can be fatal. Intestinal obstructions in multiple sites are the most common proximate cause of death.][ Intestinal obstruction in ovarian cancer can either be a true obstruction, where tumor blocks the intestinal lumen, or a pseudo-obstruction, when tumor prevents normal peristalsis. Continuous accumulation of ascites can be treated by placing a drain that can be self-drained.][
]
Prognostic factors
There are a number of prognostic factors in ovarian cancer. Positive prognostic factors – those indicating better chances of survival – include no residual disease after surgery (stage III/IV), complete macroscopic resection (stage IV), BRCA2 mutations, young age (under 45 years), nonserous type, low histologic grade, early stage, co-occurrence with endometrial cancer, and low CA-125 levels. There is conflicting evidence for BRCA1 as a prognostic factor. Conversely, negative prognostic factors – those that indicate a worse chance of survival – include rupture of the ovarian capsule during surgery, older age (over 45 years), mucinous type, stage IV, high histologic grade, clear cell type, upper abdominal involvement, high CA-125 levels, the presence of tumor cells in the blood, and elevated Cyclooxygenase 2, cyclooxygenase-2.
Survival rates
Overall five-year survival rates for all types of ovarian cancer are presented below by stage and histologic grade:[
The survival rates given below are for the different types of ovarian cancer, according to American Cancer Society.]
Recurrence rates
Ovarian cancer frequently recurs after treatment. Overall, in a 5-year period, 20% of stage I and II cancers recur. Most recurrences are in the abdomen.[ When a dysgerminoma recurs, it is most likely to recur within a year of diagnosis, and other malignant germ cell tumors recur within 2 years 90% of the time. Germ cell tumors other than dysgerminomas have a poor prognosis when they relapse, with a 10% long-term survival rate.][ Low malignant potential tumors rarely relapse, even when fertility-sparing surgery is the treatment of choice. 15% of LMP tumors relapse after unilateral surgery in the previously unaffected ovary, and they are typically easily treated with surgery. More advanced tumors may take up to 20 years to relapse, if they relapse at all, and are only treated with surgery unless the tumor has changed its histological characteristics or grown very quickly. In these cases, and when there is significant ascites, chemotherapy may also be used. Relapse is usually indicated by rising CA-125 levels and then progresses to symptomatic relapse within 2–6 months.][ Recurrent sex cord-stromal tumors are typically unresponsive to treatment but not aggressive.][
It is the most deadly gynecologic cancer.]
Epidemiology
 Globally, in 2018, the incidence of ovarian cancer was 6.6 per 100,000 and mortality was 3.9.
Globally, in 2018, the incidence of ovarian cancer was 6.6 per 100,000 and mortality was 3.9.
United States
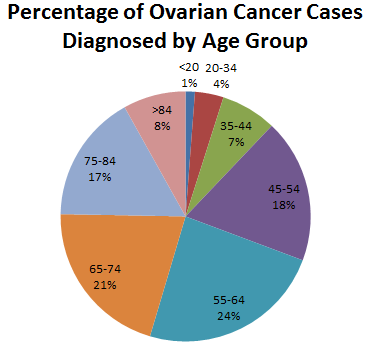 In 2022, in the United States, an estimated 19,880 new cases were diagnosed and 12,810 women died of ovarian cancer. The 5-year relative survival rate is 49.7%.
In 2022, in the United States, an estimated 19,880 new cases were diagnosed and 12,810 women died of ovarian cancer. The 5-year relative survival rate is 49.7%.
United Kingdom
It is the 5th-most common cancer in UK women (around 7,100 were diagnosed in 2011) and the 5th-most common cause of cancer death in women (around 4,300 died in 2012).
Ethnicity
Black women have twice the risk for sex cord-stromal tumors compared to non-Black women.
Older women
In the US, the incidence rate in women over 50 is approximately 33 per 100,000. The rate of ovarian cancer between 1993 and 2008 decreased in women of the 40–49 age cohort and in the 50–64 age cohort.
In pregnancy
Malignant germ cell tumors are the type of ovarian cancer most likely to occur during pregnancy. They are typically diagnosed when an adnexal mass is found on examination (in 1–2% of all pregnancies), a tumor is seen on ultrasound, or the parent's level of alpha-fetoprotein is elevated. Dermoid cysts and dysgerminomas are the most common germ cell tumors during pregnancy. Germ cell tumors diagnosed during pregnancy are unlikely to have metastasized and can be treated by surgery and, in some cases, chemotherapy, which carries the risk of birth defects. Yolk sac tumors and immature teratomas grow particularly quickly and are usually treated with chemotherapy even during pregnancy; however, dysgerminomas that have been optimally debulked may be treated after childbirth.
Other animals
Ovarian tumors have been reported in equine mares. Reported tumor types include teratoma,granulosa cell tumor
Granulosa cell tumours are tumours that arise from granulosa cells. They are estrogen secreting tumours and present as large, complex, ovarian masses. These tumours are part of the sex cord-gonadal stromal tumour or non-epithelial group of tumours ...
.
Research
Screening
Screening by hysteroscopy to obtain cell samples obtained for histological examination is being developed. This is similar to the current pap smear that is used to detect cervical cancer.[ subscription required] The UK Collaborative Trial of Ovarian Cancer Screening is testing a screening technique that combines CA-125 blood tests with transvaginal ultrasound.[ Other studies suggest that this screening procedure may be effective.][ The ROCA method combined with transvaginal ultrasonography is being researched in high-risk women to determine if it is a viable screening method. It is also being investigated in normal-risk women as it has shown promise in the wider population.][ Studies are also in progress to determine if screening helps detect cancer earlier in people with BRCA mutations.]
Prognosis research
Research into various prognostic factors for ovarian cancer is also going on. Recent research shows that thrombocytosis predicts lower survival and higher stage cancer.[ Ongoing research is also investigating the benefits of surgery for recurrent ovarian cancer.]
Immunotherapy
While an active area of research, as of 2018 there is no good evidence that immunotherapy is effective for ovarian cancer.[ and has been cited as having at least a 15% response rate.][ It is being investigated particularly in mucinous ovarian cancers.]
Pharmacology
mTOR inhibitors were a highly investigated potential treatment in the 2000s and 2010s, but the side effects of these drugs (particularly hyperglycemia and hyperlipidemia) were not well tolerated and the survival benefit not confirmed. PI3 kinase inhibitors have been of interest, but they tend to be highly toxic and cause diarrhea
Diarrhea, also spelled diarrhoea, is the condition of having at least three loose, liquid, or watery bowel movements each day. It often lasts for a few days and can result in dehydration due to fluid loss. Signs of dehydration often begin w ...
. Another investigated drug is selumetinib, a MAPK inhibitor. It improved survival, but did not correlate with any mutations found in tumors.[
Bevacizumab can also be combined with platinum chemotherapy, a combination that has had positive preliminary results in PFS, but equivocal results regarding overall survival. One disadvantage to these treatments is the side effect profile, which includes hypertension, high blood pressure and proteinuria. The drug can also exacerbate bowel disease, leading to fistulae or bowel perforation. Vintafolide, which consists of an antifolate conjugated with vinblastine, is also in clinical trials; it may prove beneficial because folate receptors are overexpressed in many ovarian cancers.][ Another potential immunotherapy is trastuzumab, which is active against tumors positive for Her2/neu mutations.][ Other angiogenesis inhibitors are also being investigated as potential ovarian cancer treatments. Combretastatin and pazopanib are being researched in combination for recurrent ovarian cancer. Trebananib and tasquinimod are other angiogenesis inhibitors being investigated. The monoclonal antibody farletuzumab is being researched as an adjuvant to traditional chemotherapy. Another type of immunotherapy involves vaccines, including TroVax.][ Cisplatin and paclitaxel are both being researched as intraperitoneal chemotherapy agents. A specific chemotherapy regimen for rare clear-cell cancers is also under investigation: irinotecan combined with cisplatin.][ Rucaparib is another PARP inhibitor being researched in BRCA-positive and BRCA-negative recurrent advanced ovarian cancer. Niraparib is a PARP inhibitor being tested in BRCA-positive recurrent ovarian cancer.]
Hormones and radiation
Hormone therapies are a topic of current research in ovarian cancer, particularly, the value of certain medications used to treat breast cancer. These include tamoxifen, letrozole, and anastrozole. Preliminary studies have showed a benefit for tamoxifen in a small number of people with advanced ovarian cancer. Letrozole may help to slow or stop growth of estrogen receptor positive ovarian cancer. Anastrozole is being investigated in postmenopausal people with estrogen receptor-positive cancer.
Inflammation
There are some indications that pelvic inflammatory disease may be associated with ovarian cancer, especially in non-western countries. It may be due to the inflammatory process present with pelvic inflammatory disease.
Clinical trials
Clinical trials are monitored and funded by US governmental organizations to test treatment options to see if they are safe and effective. These include NIH Clinical Research Trials and You (National Institutes of Health), Learn About Clinical Trials (National Cancer Institute), Search for Clinical Trials (National Cancer Institute), ClinicalTrials.gov (National Institutes of Health).[ Clinical trials are also conducted in Canada.]
References
Further reading
*
*
External links
*
What is Ovarian Cancer Infographic, information on ovarian cancer
- Mount Sinai Hospital, New York
{{DEFAULTSORT:Ovarian Cancer
Gynaecological cancer
Gynaecology
Oncology
Ovarian cancer,
Wikipedia medicine articles ready to translate
 Early signs and symptoms of ovarian cancer may be absent or subtle. In most cases, symptoms exist for several months before being recognized and diagnosed. Symptoms can often be misdiagnosed as
Early signs and symptoms of ovarian cancer may be absent or subtle. In most cases, symptoms exist for several months before being recognized and diagnosed. Symptoms can often be misdiagnosed as  Later symptoms of ovarian cancer are due to the growing mass causing pain by pressing on other abdominopelvic organs or from metastases. Because of the anatomic location of the ovaries deep in the pelvis, most masses are large and advanced at the time of diagnosis. The growing mass may cause pain if
Later symptoms of ovarian cancer are due to the growing mass causing pain by pressing on other abdominopelvic organs or from metastases. Because of the anatomic location of the ovaries deep in the pelvis, most masses are large and advanced at the time of diagnosis. The growing mass may cause pain if 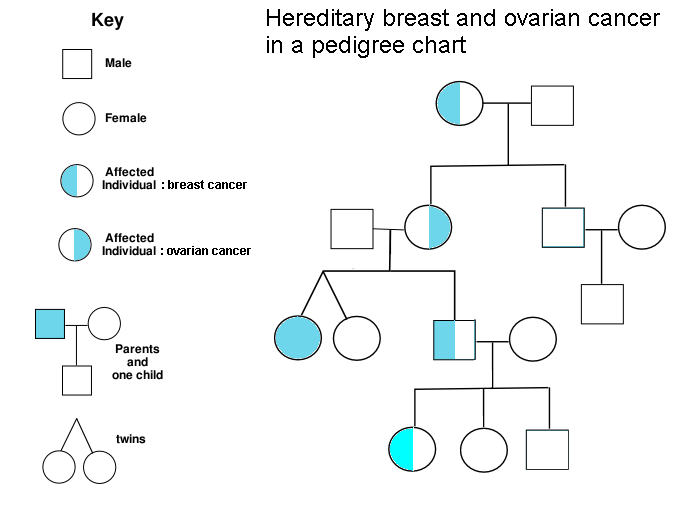 A family history of ovarian cancer is a risk factor for ovarian cancer. Women with hereditary nonpolyposis colon cancer (Lynch syndrome), and those with BRCA-1 and BRCA-2 genetic abnormalities are at increased risk.
The major genetic risk factor for ovarian cancer is a mutation in ''BRCA1'' or ''BRCA2'' genes, or in
A family history of ovarian cancer is a risk factor for ovarian cancer. Women with hereditary nonpolyposis colon cancer (Lynch syndrome), and those with BRCA-1 and BRCA-2 genetic abnormalities are at increased risk.
The major genetic risk factor for ovarian cancer is a mutation in ''BRCA1'' or ''BRCA2'' genes, or in  A strong family history of endometrial cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known as
A strong family history of endometrial cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known as 
 Diagnosis of ovarian cancer starts with a physical examination (including a pelvic examination), a blood test (for CA-125 and sometimes other markers), and transvaginal ultrasound. Sometimes a rectovaginal examination is used to help plan a surgery. The diagnosis must be confirmed with surgery to inspect the abdominal cavity, take biopsies (tissue samples for histopathology, microscopic analysis), and look for cancer cells in the abdominal fluid. This helps to determine if an ovarian mass is benign or malignant.
Ovarian cancer's early stages (I/II) are difficult to diagnose because most symptoms are nonspecific and thus of little use in diagnosis; as a result, it is rarely diagnosed until it spreads and advances to later stages (III/IV). Additionally, symptoms of ovarian cancer may appear similar to
Diagnosis of ovarian cancer starts with a physical examination (including a pelvic examination), a blood test (for CA-125 and sometimes other markers), and transvaginal ultrasound. Sometimes a rectovaginal examination is used to help plan a surgery. The diagnosis must be confirmed with surgery to inspect the abdominal cavity, take biopsies (tissue samples for histopathology, microscopic analysis), and look for cancer cells in the abdominal fluid. This helps to determine if an ovarian mass is benign or malignant.
Ovarian cancer's early stages (I/II) are difficult to diagnose because most symptoms are nonspecific and thus of little use in diagnosis; as a result, it is rarely diagnosed until it spreads and advances to later stages (III/IV). Additionally, symptoms of ovarian cancer may appear similar to  Ovarian cancers are classified according to the microscopic appearance of their structures (histology or histopathology). Histology dictates many aspects of clinical treatment, management, and prognosis. The gross pathology of ovarian cancers is very similar regardless of histologic type: ovarian tumors have solid and cystic masses. According to Surveillance Epidemiology and End Results, SEER, the types of ovarian cancers in women age 20 and over are:
Ovarian cancers are histologically and genetically divided into type I or type II. Type I cancers are of low histological grade and include endometrioid, mucinous, and clear-cell carcinomas. Type II cancers are of higher histological grade and include serous carcinoma and carcinosarcoma.
Ovarian cancers are classified according to the microscopic appearance of their structures (histology or histopathology). Histology dictates many aspects of clinical treatment, management, and prognosis. The gross pathology of ovarian cancers is very similar regardless of histologic type: ovarian tumors have solid and cystic masses. According to Surveillance Epidemiology and End Results, SEER, the types of ovarian cancers in women age 20 and over are:
Ovarian cancers are histologically and genetically divided into type I or type II. Type I cancers are of low histological grade and include endometrioid, mucinous, and clear-cell carcinomas. Type II cancers are of higher histological grade and include serous carcinoma and carcinosarcoma.
 Serous ovarian cancer is the most common type of epithelial ovarian cancer and it accounts for about two-thirds of cases of epithelial ovarian cancer. Low-grade serous carcinoma is less aggressive than high-grade serous carcinomas, though it does not typically respond well to chemotherapy or hormonal treatments. Serous carcinomas are thought to begin in the Fallopian tube. High grade serous carcinoma accounts for 75% of all epithelial ovarian cancer. About 15-20% of high grade serous carcinoma have germline BRCA1 and BRCA2 mutations. Histologically, the growth pattern of high grade serous carcinoma is heterogenous and has some papillary or solid growth patterns. The tumor cells are atypical with large, irregular nuclei. It has a high proliferation rate. 50% of the time, serous carcinomas are bilateral, and in 85% of cases, they have spread beyond the ovary at the time of diagnosis.
Serous Tubal Intraepithelial Carcinoma (STIC) is now recognized to be the precursor lesion of most so-called ovarian high-grade serous carcinomas.
STIC is characterised by
#Abnormal p53 staining
#Ki67 proliferation index in excess of 10%
#Positive WT1 (to exclude metastases)
Serous ovarian cancer is the most common type of epithelial ovarian cancer and it accounts for about two-thirds of cases of epithelial ovarian cancer. Low-grade serous carcinoma is less aggressive than high-grade serous carcinomas, though it does not typically respond well to chemotherapy or hormonal treatments. Serous carcinomas are thought to begin in the Fallopian tube. High grade serous carcinoma accounts for 75% of all epithelial ovarian cancer. About 15-20% of high grade serous carcinoma have germline BRCA1 and BRCA2 mutations. Histologically, the growth pattern of high grade serous carcinoma is heterogenous and has some papillary or solid growth patterns. The tumor cells are atypical with large, irregular nuclei. It has a high proliferation rate. 50% of the time, serous carcinomas are bilateral, and in 85% of cases, they have spread beyond the ovary at the time of diagnosis.
Serous Tubal Intraepithelial Carcinoma (STIC) is now recognized to be the precursor lesion of most so-called ovarian high-grade serous carcinomas.
STIC is characterised by
#Abnormal p53 staining
#Ki67 proliferation index in excess of 10%
#Positive WT1 (to exclude metastases)
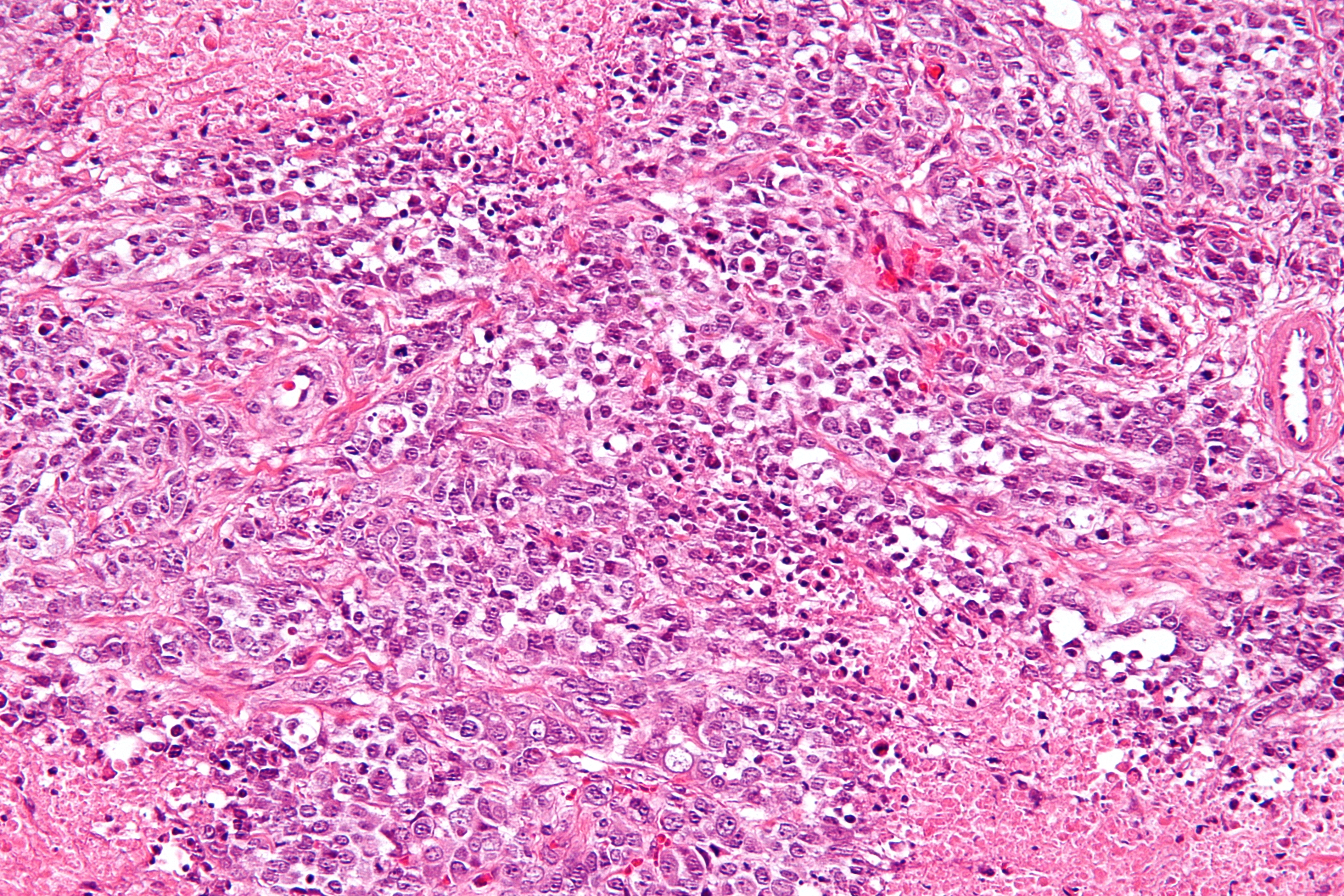 Small-cell carcinoma, Small-cell ovarian carcinoma is rare and aggressive, with two main subtypes: hypercalcemic and pulmonary. This rare malignancy most commonly affects young women under the age of 40 years old with a range between 14 months to 58 years. The mean age of diagnosis of 24 years. Approximately two-thirds of patients will present with paraneoplastic hypercalcemia meaning they have high blood calcium levels for an unknown reason. The tumor secretes Parathyroid hormone related protein which acts similarly to PTH and binds PTH receptors in the bone and kidney causing hypercalcemia. Recent research has found an inactivating germline and somatic mutation of ''SMARCA4'' gene. The hypercalcemic subtype is very aggressive and has a overall survival rate of 16% with a recurrence rate of 65% in patients who receive treatment. Patients who have spread of the disease to other parts of the body tend to die 2 years after the diagnosis. Extra-ovarian spread is involved in 50% of cases and lymph node spread is present in 55% of cases. The most common initial presentation is a rapidly growing unilateral pelvic mass with a mean size of 15 cm. Histologically, it is characterized by many sheets of small, round, tightly packed cells with clusters, nests, and cords. Immunohistochemistry is typically positive for vimentin, cytokeratin, CD10, p53, and WT-1.
Small cell ovarian carcinoma of the pulmonary subtype presents differently from the hypercalcemic subtype. Typically, pulmonary small cell ovarian cancer usually affects both ovaries of older women and looks like Small-cell carcinoma, oat-cell carcinoma of the lung. The average age of disease onset is 59 years old and approximately 45% of cases are bilateral for the pulmonary subtype. Additionally, several hormones can be elevated in the pulmonary subtype including serotonin, somatostatin, insulin, gastrin, and calcitonin.
Small-cell carcinoma, Small-cell ovarian carcinoma is rare and aggressive, with two main subtypes: hypercalcemic and pulmonary. This rare malignancy most commonly affects young women under the age of 40 years old with a range between 14 months to 58 years. The mean age of diagnosis of 24 years. Approximately two-thirds of patients will present with paraneoplastic hypercalcemia meaning they have high blood calcium levels for an unknown reason. The tumor secretes Parathyroid hormone related protein which acts similarly to PTH and binds PTH receptors in the bone and kidney causing hypercalcemia. Recent research has found an inactivating germline and somatic mutation of ''SMARCA4'' gene. The hypercalcemic subtype is very aggressive and has a overall survival rate of 16% with a recurrence rate of 65% in patients who receive treatment. Patients who have spread of the disease to other parts of the body tend to die 2 years after the diagnosis. Extra-ovarian spread is involved in 50% of cases and lymph node spread is present in 55% of cases. The most common initial presentation is a rapidly growing unilateral pelvic mass with a mean size of 15 cm. Histologically, it is characterized by many sheets of small, round, tightly packed cells with clusters, nests, and cords. Immunohistochemistry is typically positive for vimentin, cytokeratin, CD10, p53, and WT-1.
Small cell ovarian carcinoma of the pulmonary subtype presents differently from the hypercalcemic subtype. Typically, pulmonary small cell ovarian cancer usually affects both ovaries of older women and looks like Small-cell carcinoma, oat-cell carcinoma of the lung. The average age of disease onset is 59 years old and approximately 45% of cases are bilateral for the pulmonary subtype. Additionally, several hormones can be elevated in the pulmonary subtype including serotonin, somatostatin, insulin, gastrin, and calcitonin.
 Clear cell ovarian carcinoma is a rare subtype of epithelial ovarian cancer. Those diagnosed with clear cell ovarian carcinoma are typically younger at the age of diagnosis and diagnosed at earlier stages than other subtypes of epithelial ovarian cancer. The highest incidence of clear cell carcinoma of the ovary have been observed among young Asian women, especially those of Korean, Taiwanese, and Japanese background. Endometriosis has been linked to being the main risk factor for the development of clear cell carcinoma of the ovary and has been found to be present in 50% of women diagnosed with clear cell carcinoma of the ovary. The development of clots in the legs such as deep vein thromboembolism or in the lungs with pulmonary embolism is reported to be 40% higher in patients with clear cell carcinoma than other epithelial ovarian cancer subtypes. Mutations in molecular pathways such as ARID1A, PIK3, and PIK3CA have been found to be linked to clear cell carcinoma. They typically present as a large, unilateral mass, with a mean size between 13–15 cm. 90% of cases are unilateral. Clear-cell ovarian carcinomas do not typically respond well to chemotherapy due to intrinsic chemoresistance therefore treatment is typically with aggressive cytoreductive surgery and platinum-based chemotherapy.
Clear cell ovarian carcinoma is a rare subtype of epithelial ovarian cancer. Those diagnosed with clear cell ovarian carcinoma are typically younger at the age of diagnosis and diagnosed at earlier stages than other subtypes of epithelial ovarian cancer. The highest incidence of clear cell carcinoma of the ovary have been observed among young Asian women, especially those of Korean, Taiwanese, and Japanese background. Endometriosis has been linked to being the main risk factor for the development of clear cell carcinoma of the ovary and has been found to be present in 50% of women diagnosed with clear cell carcinoma of the ovary. The development of clots in the legs such as deep vein thromboembolism or in the lungs with pulmonary embolism is reported to be 40% higher in patients with clear cell carcinoma than other epithelial ovarian cancer subtypes. Mutations in molecular pathways such as ARID1A, PIK3, and PIK3CA have been found to be linked to clear cell carcinoma. They typically present as a large, unilateral mass, with a mean size between 13–15 cm. 90% of cases are unilateral. Clear-cell ovarian carcinomas do not typically respond well to chemotherapy due to intrinsic chemoresistance therefore treatment is typically with aggressive cytoreductive surgery and platinum-based chemotherapy.
 Clear-cell adenocarcinomas are histopathologically similar to other clear cell carcinomas, with clear cells and hobnail cells. They represent approximately 5–10% of epithelial ovarian cancers and are associated with endometriosis in the pelvic cavity. They are typically early-stage and therefore curable by surgery, but advanced clear-cell adenocarcinomas (approximately 20%) have a poor prognosis and are often resistant to platinum chemotherapy.
Clear-cell adenocarcinomas are histopathologically similar to other clear cell carcinomas, with clear cells and hobnail cells. They represent approximately 5–10% of epithelial ovarian cancers and are associated with endometriosis in the pelvic cavity. They are typically early-stage and therefore curable by surgery, but advanced clear-cell adenocarcinomas (approximately 20%) have a poor prognosis and are often resistant to platinum chemotherapy.
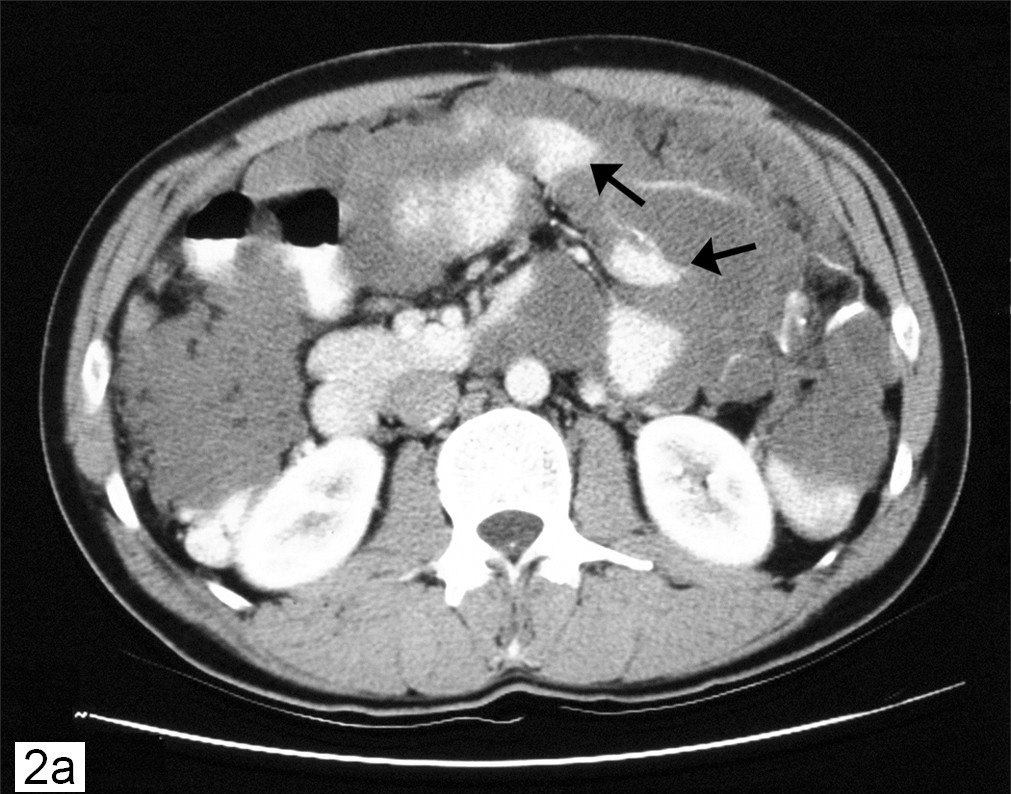 ''Pseudomyxoma peritonei'' refers to a collection of encapsulated mucous or gelatinous material in the abdominopelvic cavity, which is very rarely caused by a primary mucinous ovarian tumor. More commonly, it is associated with ovarian metastases of intestinal cancer.
''Pseudomyxoma peritonei'' refers to a collection of encapsulated mucous or gelatinous material in the abdominopelvic cavity, which is very rarely caused by a primary mucinous ovarian tumor. More commonly, it is associated with ovarian metastases of intestinal cancer.
 Malignant Brenner tumors are rare. Histologically, they have dense fibrous stroma with areas of transitional epithelium and some squamous differentiation. To be classified as a malignant Brenner tumor, it must have Brenner tumor foci and transitional cell carcinoma. The transitional cell carcinoma component is typically poorly differentiated and resembles urinary tract cancer.
Malignant Brenner tumors are rare. Histologically, they have dense fibrous stroma with areas of transitional epithelium and some squamous differentiation. To be classified as a malignant Brenner tumor, it must have Brenner tumor foci and transitional cell carcinoma. The transitional cell carcinoma component is typically poorly differentiated and resembles urinary tract cancer.
 Dysgerminoma accounts for 35% of ovarian cancer in young women and is the most likely germ cell tumor to metastasize to the lymph nodes; nodal metastases occur in 25–30% of cases. These tumors may have mutations in CD117, the ''KIT'' gene, a mutation known for its role in gastrointestinal stromal tumor. Swyer syndrome, People with an XY karyotype and ovaries (gonadal dysgenesis) or an X,0 karyotype and ovaries (Turner syndrome) who develop a unilateral dysgerminoma are at risk for a gonadoblastoma in the other ovary, and in this case, both ovaries are usually removed when a unilateral dysgerminoma is discovered to avoid the risk of another malignant tumor. Gonadoblastomas in people with Swyer or Turner syndrome become malignant in approximately 40% of cases. However, in general, dysgerminomas are bilateral 10–20% of the time.
Dysgerminoma accounts for 35% of ovarian cancer in young women and is the most likely germ cell tumor to metastasize to the lymph nodes; nodal metastases occur in 25–30% of cases. These tumors may have mutations in CD117, the ''KIT'' gene, a mutation known for its role in gastrointestinal stromal tumor. Swyer syndrome, People with an XY karyotype and ovaries (gonadal dysgenesis) or an X,0 karyotype and ovaries (Turner syndrome) who develop a unilateral dysgerminoma are at risk for a gonadoblastoma in the other ovary, and in this case, both ovaries are usually removed when a unilateral dysgerminoma is discovered to avoid the risk of another malignant tumor. Gonadoblastomas in people with Swyer or Turner syndrome become malignant in approximately 40% of cases. However, in general, dysgerminomas are bilateral 10–20% of the time.
 They are composed of cells that cannot Cellular differentiation, differentiate further and develop directly from germ cells or from gonadoblastomas. Dysgerminomas contain syncytiotrophoblasts in approximately 5% of cases, and can therefore cause elevated hCG levels. On gross appearance, dysgerminomas are typically pink to tan-colored, have multiple lobes, and are solid. Microscopically, they appear identical to seminomas and very close to Embryonic germ cell, embryonic primordial germ cells, having large, polyhedral, rounded clear cells. The nuclei are uniform and round or square with prominent Nucleolus, nucleoli and the cytoplasm has high levels of glycogen. Inflammation is another prominent histologic feature of dysgerminomas.
They are composed of cells that cannot Cellular differentiation, differentiate further and develop directly from germ cells or from gonadoblastomas. Dysgerminomas contain syncytiotrophoblasts in approximately 5% of cases, and can therefore cause elevated hCG levels. On gross appearance, dysgerminomas are typically pink to tan-colored, have multiple lobes, and are solid. Microscopically, they appear identical to seminomas and very close to Embryonic germ cell, embryonic primordial germ cells, having large, polyhedral, rounded clear cells. The nuclei are uniform and round or square with prominent Nucleolus, nucleoli and the cytoplasm has high levels of glycogen. Inflammation is another prominent histologic feature of dysgerminomas.
 Immature, or solid, teratomas are the most common type of ovarian germ cell tumor, making up 40–50% of cases. Teratomas are characterized by the presence of disorganized tissues arising from all three embryonic germ layers: ectoderm, mesoderm, and endoderm; immature teratomas also have undifferentiated stem cells that make them more malignant than mature teratomas (dermoid cysts). The different tissues are visible on gross pathology and often include bone, cartilage, hair, mucus, or Sebaceous gland, sebum, but these tissues are not visible from the outside, which appears to be a solid mass with lobes and cysts. Histologically, they have large amounts of neuroectoderm organized into sheets and tubules along with Neuroglia, glia; the amount of neural tissue determines the histologic grade. Immature teratomas usually only affect one ovary (10% co-occur with dermoid cysts) and usually metastasize throughout the peritoneum. They can also cause mature teratoma implants to grow throughout the abdomen in a disease called growing teratoma syndrome; these are usually benign but will continue to grow during chemotherapy, and often necessitate further surgery. Unlike mature teratomas, immature teratomas form many Adhesion (medicine), adhesions, making them less likely to cause ovarian torsion. There is no specific marker for immature teratomas, but carcinoembryonic antigen (CEA), CA-125, CA19-9, or AFP can sometimes indicate an immature teratoma.
Stage I teratomas make up the majority (75%) of cases and have the best prognosis, with 98% of patients surviving 5 years; if a Stage I tumor is also grade 1, it can be treated with unilateral surgery only. Stage II though IV tumors make up the remaining quarter of cases and have a worse prognosis, with 73–88% of patients surviving 5 years.
Immature, or solid, teratomas are the most common type of ovarian germ cell tumor, making up 40–50% of cases. Teratomas are characterized by the presence of disorganized tissues arising from all three embryonic germ layers: ectoderm, mesoderm, and endoderm; immature teratomas also have undifferentiated stem cells that make them more malignant than mature teratomas (dermoid cysts). The different tissues are visible on gross pathology and often include bone, cartilage, hair, mucus, or Sebaceous gland, sebum, but these tissues are not visible from the outside, which appears to be a solid mass with lobes and cysts. Histologically, they have large amounts of neuroectoderm organized into sheets and tubules along with Neuroglia, glia; the amount of neural tissue determines the histologic grade. Immature teratomas usually only affect one ovary (10% co-occur with dermoid cysts) and usually metastasize throughout the peritoneum. They can also cause mature teratoma implants to grow throughout the abdomen in a disease called growing teratoma syndrome; these are usually benign but will continue to grow during chemotherapy, and often necessitate further surgery. Unlike mature teratomas, immature teratomas form many Adhesion (medicine), adhesions, making them less likely to cause ovarian torsion. There is no specific marker for immature teratomas, but carcinoembryonic antigen (CEA), CA-125, CA19-9, or AFP can sometimes indicate an immature teratoma.
Stage I teratomas make up the majority (75%) of cases and have the best prognosis, with 98% of patients surviving 5 years; if a Stage I tumor is also grade 1, it can be treated with unilateral surgery only. Stage II though IV tumors make up the remaining quarter of cases and have a worse prognosis, with 73–88% of patients surviving 5 years.
 Ovarian cancer usually has a relatively poor prognosis. It is disproportionately deadly because it lacks any clear early detection or screening test, meaning most cases are not diagnosed until they have reached advanced stages.
Ovarian cancer metastasizes early in its development, often before it has been diagnosed. High-grade tumors metastasize more readily than low-grade tumors. Typically, tumor cells begin to metastasize by growing in the peritoneal cavity. More than 60% of women presenting with ovarian cancer have stage-III or stage-IV cancer, when it has already spread beyond the ovaries. Ovarian cancers shed cells into the naturally occurring fluid within the abdominal cavity. These cells can then implant on other abdominal (peritoneal) structures, including the uterus, urinary bladder, bowel, mesentery, lining of the bowel wall, and Greater omentum, omentum, forming new tumor growths before cancer is even suspected.
The five-year survival rate for all stages of ovarian cancer is 46%; the one-year survival rate is 72% and the ten-year survival rate is 35%. For cases where a diagnosis is made early in the disease, when the cancer is still confined to the primary site, the five-year survival rate is 92.7%.Survival rates based on SEER incidence and NCHS mortality statistics, as cited by the National Cancer Institute i
Ovarian cancer usually has a relatively poor prognosis. It is disproportionately deadly because it lacks any clear early detection or screening test, meaning most cases are not diagnosed until they have reached advanced stages.
Ovarian cancer metastasizes early in its development, often before it has been diagnosed. High-grade tumors metastasize more readily than low-grade tumors. Typically, tumor cells begin to metastasize by growing in the peritoneal cavity. More than 60% of women presenting with ovarian cancer have stage-III or stage-IV cancer, when it has already spread beyond the ovaries. Ovarian cancers shed cells into the naturally occurring fluid within the abdominal cavity. These cells can then implant on other abdominal (peritoneal) structures, including the uterus, urinary bladder, bowel, mesentery, lining of the bowel wall, and Greater omentum, omentum, forming new tumor growths before cancer is even suspected.
The five-year survival rate for all stages of ovarian cancer is 46%; the one-year survival rate is 72% and the ten-year survival rate is 35%. For cases where a diagnosis is made early in the disease, when the cancer is still confined to the primary site, the five-year survival rate is 92.7%.Survival rates based on SEER incidence and NCHS mortality statistics, as cited by the National Cancer Institute i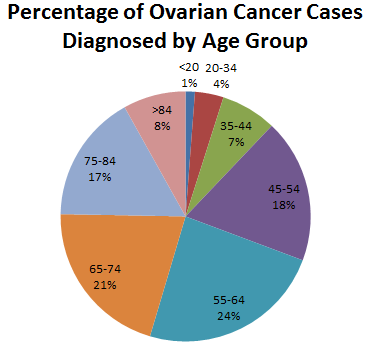 In 2022, in the United States, an estimated 19,880 new cases were diagnosed and 12,810 women died of ovarian cancer. The 5-year relative survival rate is 49.7%. Around 57% cases have metastasized at the time of diagnosis.
In 2014, over 220,000 diagnoses of epithelial ovarian cancer were made yearly. The overall lifetime risk in the US is around 1.6% In the US, ovarian cancer affects 1.3–1.4% and is the cause of death of about 1% of women. In the United States, it is also the fifth-most common cancer in women but the fourth-most common cause of cancer death. This decrease made it the ninth-most common cancer in women.
The risks from developing specific types of ovarian cancer varies. Germ cell tumors and sex cord-stromal tumors are less common than epithelial tumors. The number of new cases a year in the US is 0.4 per 100,000 women and 0.2 per 100,000 women, respectively. In young people, sex-cord stromal tumors and germ cell tumors total 1% of overall ovarian cancer. Ovarian cancer represents approximately 4% of cancers diagnosed in women.
In 2022, in the United States, an estimated 19,880 new cases were diagnosed and 12,810 women died of ovarian cancer. The 5-year relative survival rate is 49.7%. Around 57% cases have metastasized at the time of diagnosis.
In 2014, over 220,000 diagnoses of epithelial ovarian cancer were made yearly. The overall lifetime risk in the US is around 1.6% In the US, ovarian cancer affects 1.3–1.4% and is the cause of death of about 1% of women. In the United States, it is also the fifth-most common cancer in women but the fourth-most common cause of cancer death. This decrease made it the ninth-most common cancer in women.
The risks from developing specific types of ovarian cancer varies. Germ cell tumors and sex cord-stromal tumors are less common than epithelial tumors. The number of new cases a year in the US is 0.4 per 100,000 women and 0.2 per 100,000 women, respectively. In young people, sex-cord stromal tumors and germ cell tumors total 1% of overall ovarian cancer. Ovarian cancer represents approximately 4% of cancers diagnosed in women.