Insulinoma on:
[Wikipedia]
[Google]
[Amazon]
An insulinoma is a
 The definitive management is the surgical removal of the insulinoma. This may involve removing part of the pancreas, as well (
The definitive management is the surgical removal of the insulinoma. This may involve removing part of the pancreas, as well (
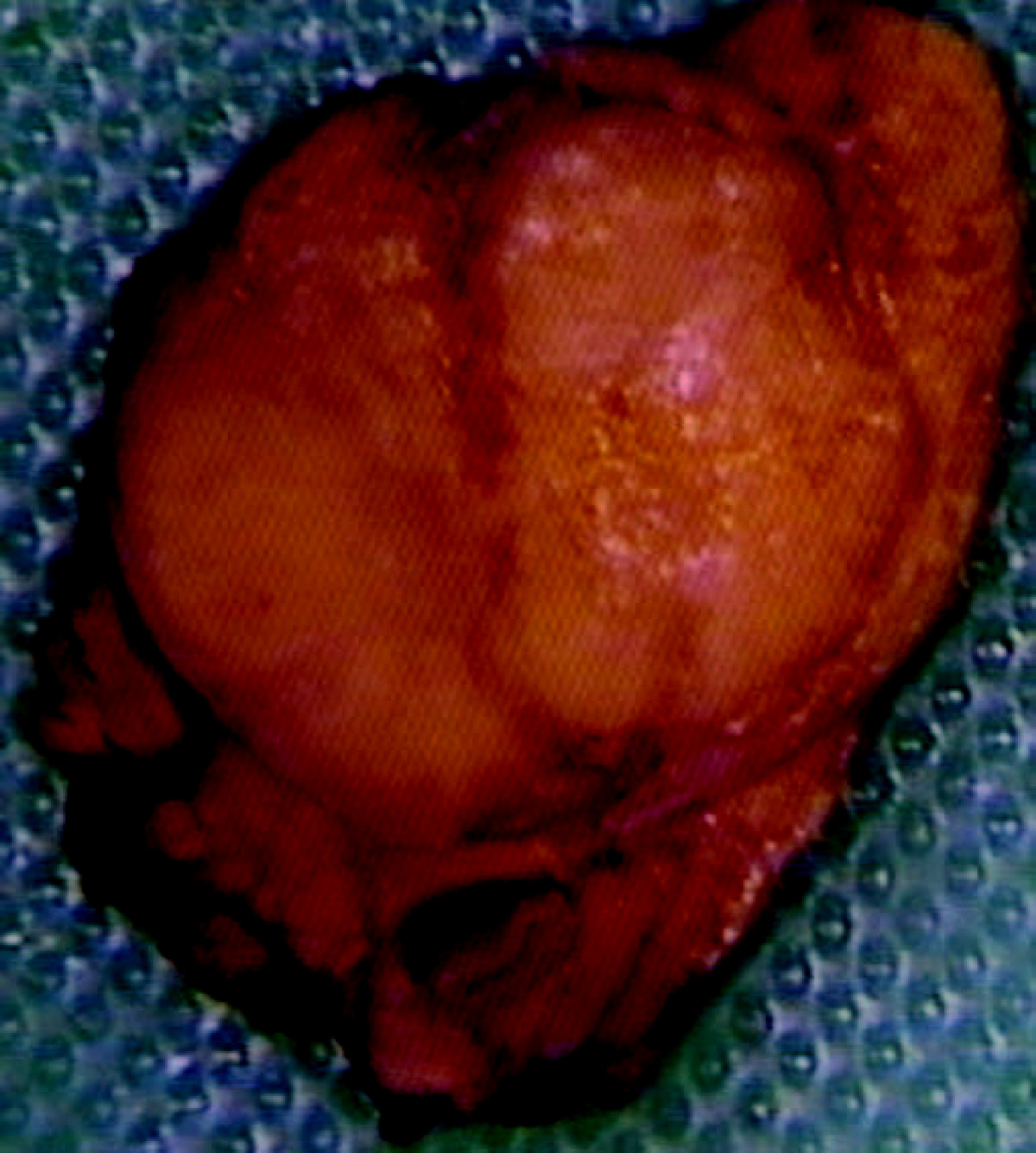
Image:Pancreatic insulinoma (1).JPG, Pancreatic insulinoma
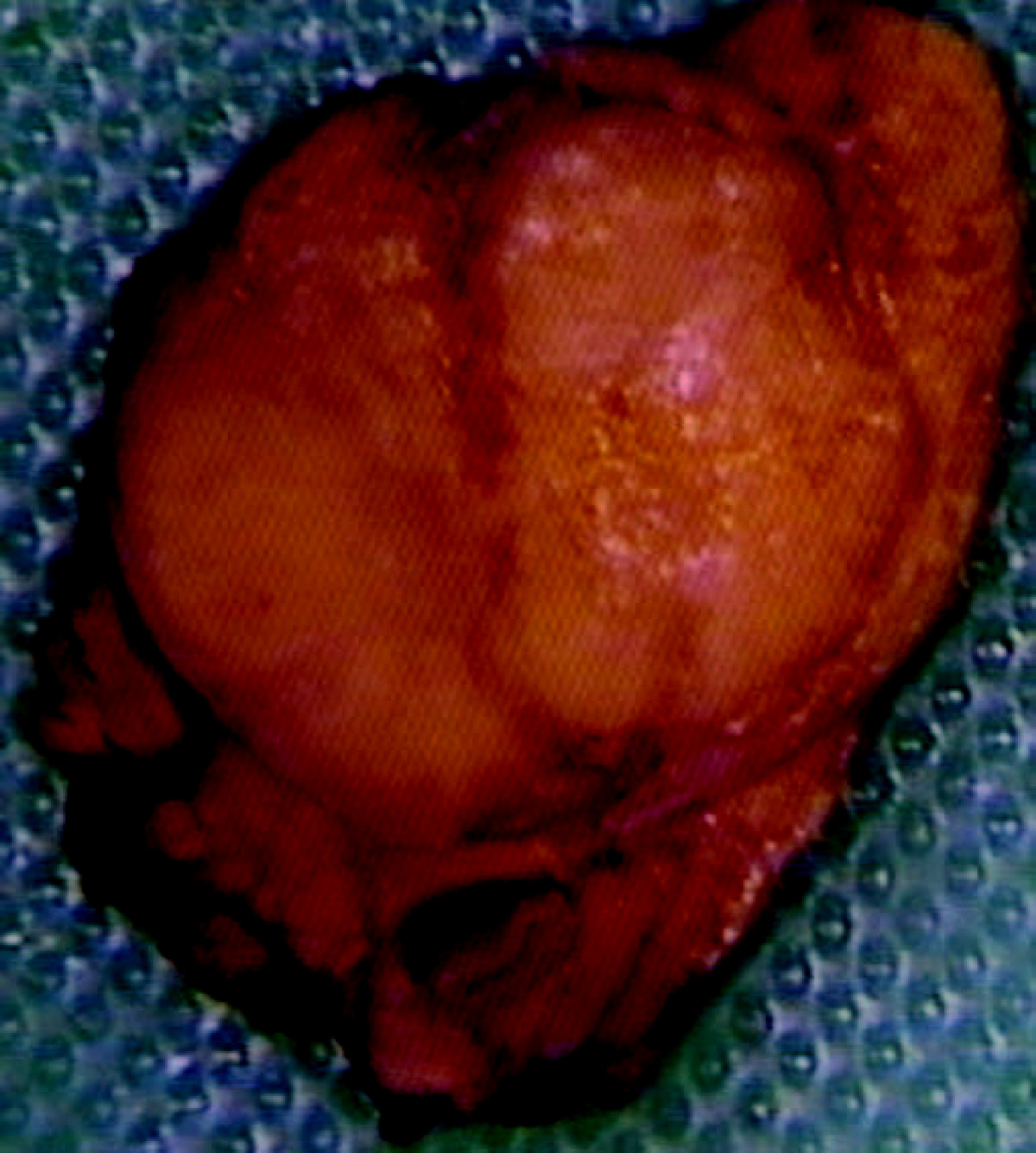
Image:Pancreatic insulinoma (2).JPG, Pancreatic insulinoma
Image:Pancreatic insulinoma (3) Chromogranin A.JPG, Chromogranin A
Image:Pancreatic insulinoma (4) Insulin immuostain.JPG, Insulin immuostain
tumour
A neoplasm () is a type of abnormal and excessive growth of tissue. The process that occurs to form or produce a neoplasm is called neoplasia. The growth of a neoplasm is uncoordinated with that of the normal surrounding tissue, and persists ...
of the pancreas
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e. it has both an end ...
that is derived from beta cell
Beta cells (β-cells) are a type of cell found in pancreatic islets that synthesize and secrete insulin and amylin. Beta cells make up 50–70% of the cells in human islets. In patients with Type 1 diabetes, beta-cell mass and function are di ...
s and secretes insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism o ...
. It is a rare form of a neuroendocrine tumour
Neuroendocrine tumors (NETs) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They most commonly occur in the intestine, where they are often called carcinoid tumors, but they are also found in the pancreas, lung ...
. Most insulinomas are benign
Malignancy () is the tendency of a medical condition to become progressively worse.
Malignancy is most familiar as a characterization of cancer. A ''malignant'' tumor contrasts with a non-cancerous ''benign'' tumor in that a malignancy is not s ...
in that they grow exclusively at their origin within the pancreas, but a minority metastasize
Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, then, ...
. Insulinomas are one of the functional pancreatic neuroendocrine tumour (PNET) group ("functional" because it increases production of insulin). In the Medical Subject Headings
Medical Subject Headings (MeSH) is a comprehensive controlled vocabulary for the purpose of indexing journal articles and books in the life sciences. It serves as a thesaurus that facilitates searching. Created and updated by the United States N ...
classification, insulinoma is the only subtype of "islet cell adenoma".
Beta cells secrete insulin in response to increases in blood glucose
Glycaemia, also known as blood sugar level, blood sugar concentration, or blood glucose level is the measure of glucose concentrated in the blood of humans or other animals. Approximately 4 grams of glucose, a simple sugar, is present in the blo ...
. The resulting increase in insulin acts to lower blood glucose back to normal levels, at which point further secretion of insulin is stopped. In contrast, the secretion of insulin by insulinomas is not properly regulated by glucose, and the tumours continue to secrete insulin causing glucose levels to fall further than normal.
As a result, patients present symptoms of low blood glucose (hypoglycemia
Hypoglycemia, also called low blood sugar, is a fall in blood sugar to levels below normal, typically below 70 mg/dL (3.9 mmol/L). Whipple's triad is used to properly identify hypoglycemic episodes. It is defined as blood glucose belo ...
), which are improved by eating. The diagnosis of an insulinoma is usually made biochemically with low blood glucose, elevated insulin, proinsulin
Proinsulin is the prohormone precursor to insulin made in the beta cells of the islets of Langerhans, specialized regions of the pancreas. In humans, proinsulin is encoded by the ''INS'' gene. The islets of Langerhans only secrete between 1% and ...
, and C-peptide levels, and confirmed by localizing the tumour with medical imaging
Medical imaging is the technique and process of imaging the interior of a body for clinical analysis and medical intervention, as well as visual representation of the function of some organs or tissues (physiology). Medical imaging seeks to rev ...
or angiography
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. Modern angiography is perfor ...
. The definitive treatment is surgery.
Signs and symptoms
Patients with insulinomas usually developneuroglycopenic
Neuroglycopenia is a shortage of glucose (glycopenia) in the brain, usually due to hypoglycemia. Glycopenia affects the function of neurons, and alters brain function and behavior. Prolonged or recurrent neuroglycopenia can result in loss of consc ...
symptoms. These include recurrent headache, lethargy
Lethargy is a state of tiredness, sleepiness, weariness, fatigue, sluggishness or lack of energy. It can be accompanied by depression, decreased motivation, or apathy. Lethargy can be a normal response to inadequate sleep, overexertion, overwo ...
, diplopia
Diplopia is the simultaneous perception of two images of a single object that may be displaced horizontally or vertically in relation to each other. Also called double vision, it is a loss of visual focus under regular conditions, and is often v ...
, and blurred vision, particularly with exercise or fasting. Severe hypoglycemia may result in seizure
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with l ...
s, coma
A coma is a deep state of prolonged unconsciousness in which a person cannot be awakened, fails to respond normally to painful stimuli, light, or sound, lacks a normal wake-sleep cycle and does not initiate voluntary actions. Coma patients exhi ...
, and permanent neurological damage. Symptoms resulting from the catecholaminergic
Catecholaminergic means "related to catecholamines". The catecholamine neurotransmitters include dopamine, epinephrine (adrenaline), and norepinephrine (noradrenaline).
A catecholaminergic agent (or drug) is a chemical which functions to direc ...
response to hypoglycemia (i.e. tremulousness, palpitations, tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ( ...
, sweating, hunger, anxiety, nausea) are not as common. Sudden weight gain is sometimes seen.
Diagnosis
The diagnosis of insulinoma is suspected in a patient with symptomatic fasting hypoglycemia. The conditions ofWhipple’s triad
Whipple's triad is a collection of three signs (called Whipple's criteria) that suggests that a patient's symptoms result from hypoglycaemia that may indicate insulinoma. The essential conditions are symptoms of hypoglycaemia, low blood plasma ...
need to be met for the diagnosis of "true hypoglycemia" to be made:
# symptoms and signs of hypoglycemia,
# concomitant plasma glucose level of 45 mg/dL (2.5 mmol/L) or less, and
# reversibility of symptoms with administration of glucose.
Blood tests
These blood tests are needed to diagnose insulinoma: *glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using ...
* insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism o ...
* C-peptide
The connecting peptide, or C-peptide, is a short 31-amino-acid polypeptide that connects insulin's A-chain to its B-chain in the proinsulin molecule. In the context of diabetes or hypoglycemia, a measurement of C-peptide blood serum levels can ...
If available, a proinsulin
Proinsulin is the prohormone precursor to insulin made in the beta cells of the islets of Langerhans, specialized regions of the pancreas. In humans, proinsulin is encoded by the ''INS'' gene. The islets of Langerhans only secrete between 1% and ...
level might be useful, as well. Other blood tests may help rule out other conditions which can cause hypoglycemia.
Suppression tests
Normally, endogenous insulin production is suppressed in the setting of hypoglycemia. A 72-hour fast, usually supervised in a hospital setting, can be done to see if insulin levels fail to suppress, which is a strong indicator of the presence of an insulin-secreting tumour. During the test, the patient may have calorie-free and caffeine-free liquids. Capillary blood glucose is measured every 4 hours using a reflectance meter, until values < 60 mg/dL (3.3 mmol/L) are obtained. Then, the frequency of blood glucose measurement is increased to every hour until values are < 49 mg/dL (2.7 mmol/L). At that point, or when the patient has symptoms of hypoglycemia, a blood test is drawn for serum glucose, insulin, proinsulin, and C-peptide levels. The fast is then stopped at that point, and the hypoglycemia is treated with intravenous dextrose or carbohydrate-containing food or drink.Diagnostic imaging
The insulinoma might be localized by noninvasive means, usingultrasound
Ultrasound is sound waves with frequency, frequencies higher than the upper audible limit of human hearing range, hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hea ...
, CT scan, or MRI
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves ...
techniques. An indium-111 pentetreotide scan is more sensitive than ultrasound, CT, or MRI for detection of somatostatin receptor positive tumours, but not a good diagnostic tool for insulinomas. An endoscopic ultrasound
Endoscopic ultrasound (EUS) or echo-endoscopy is a medical procedure in which endoscopy (insertion of a probe into a hollow organ) is combined with ultrasound to obtain images of the internal organs in the chest, abdomen and colon. It can be used ...
has a sensitivity of 40-93% (depending on the location of the tumour) for detecting insulinomas.
Sometimes, angiography
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. Modern angiography is perfor ...
with percutaneous transhepatic pancreatic vein
In human anatomy, the pancreatic veins consist of several small blood vessels which drain the body and tail of the pancreas
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in t ...
catheterization to sample the blood for insulin levels is required. Calcium
Calcium is a chemical element with the symbol Ca and atomic number 20. As an alkaline earth metal, calcium is a reactive metal that forms a dark oxide-nitride layer when exposed to air. Its physical and chemical properties are most similar to ...
can be injected into selected arteries to stimulate insulin release from various parts of the pancreas, which can be measured by sampling blood from their respective veins. The use of calcium stimulation improves the specificity of this test.During surgery to remove an insulinoma, an intraoperative ultrasound can sometimes localize the tumour, which helps guide the surgeon in the operation and has a higher sensitivity than noninvasive imaging tests.
Treatment
 The definitive management is the surgical removal of the insulinoma. This may involve removing part of the pancreas, as well (
The definitive management is the surgical removal of the insulinoma. This may involve removing part of the pancreas, as well (Whipple procedure
A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chro ...
and distal pancreatectomy
In medicine, a pancreatectomy is the surgery, surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy (Whipple procedure), distal pancreatectomy, segmental pancreatectomy, and tot ...
).
Medications such as diazoxide
Diazoxide, sold under the brand name Proglycem and others, is a medication used to treat low blood sugar due to a number of specific causes. This includes islet cell tumors that cannot be removed and leucine sensitivity. It can also be used in ...
and somatostatin can be used to block the release of insulin for patients who are not surgical candidates or who otherwise have inoperable tumours.
Streptozotocin
Streptozotocin or streptozocin ( INN, USP) (STZ) is a naturally occurring alkylating antineoplastic agent that is particularly toxic to the insulin-producing beta cells of the pancreas in mammals. It is used in medicine for treating certain can ...
is used in islet cell carcinoma
An islet is a very small, often unnamed island. Most definitions are not precise, but some suggest that an islet has little or no vegetation and cannot support human habitation. It may be made of rock, sand and/or hard coral; may be permanent ...
s which produce excessive insulin. Combination chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs (chemotherapeutic agents or alkylating agents) as part of a standardized chemotherapy regimen. Chemotherap ...
is used, either doxorubicin
Doxorubicin, sold under the brand name Adriamycin among others, is a chemotherapy medication used to treat cancer. This includes breast cancer, bladder cancer, Kaposi's sarcoma, lymphoma, and acute lymphocytic leukemia. It is often used toge ...
and streptozotocin, or fluorouracil
Fluorouracil (5-FU), sold under the brand name Adrucil among others, is a cytotoxic chemotherapy medication used to treat cancer. By intravenous injection it is used for treatment of colorectal cancer, oesophageal cancer, stomach cancer, pan ...
and streptozocin in patients where doxorubicin is contraindicated.
In metastasizing tumours with intrahepatic growth, hepatic arterial occlusion or embolization
Embolization refers to the passage and lodging of an embolus within the bloodstream. It may be of natural origin ( pathological), in which sense it is also called embolism, for example a pulmonary embolism; or it may be artificially indu ...
can be used.
Prognosis
Most patients with benign insulinomas can be cured with surgery. Persistent or recurrent hypoglycemia after surgery tends to occur in patients with multiple tumours. About 2% of patients developdiabetes mellitus
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level ( hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ap ...
after their surgery.
Incidence
Insulinomas are rareneuroendocrine tumour
Neuroendocrine tumors (NETs) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They most commonly occur in the intestine, where they are often called carcinoid tumors, but they are also found in the pancreas, lung ...
s with an incidence estimated at one to four new cases per million persons per year. Insulinoma is one of the most common types of tumours arising from the islets of Langerhans
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine (hormone-producing) cells, discovered in 1869 by German pathological anatomist Paul Langerhans. The pancreatic islets constitute 1–2% of ...
cells (pancreatic endocrine tumours). Estimates of malignancy (metastases) range from 5 to 30%. Over 99% of insulinomas originate in the pancreas, with rare cases from ectopic pancreatic tissue. About 5% of cases are associated with tumours of the parathyroid glands and the pituitary (multiple endocrine neoplasia type 1
Multiple endocrine neoplasia type 1 (MEN-1) is one of a group of disorders, the multiple endocrine neoplasias, that affect the endocrine system through development of neoplastic lesions in pituitary, parathyroid gland and pancreas.
It was first d ...
) and are more likely to be multiple and malignant. Most insulinomas are small, less than 2 cm.
History
Hypoglycemia was first recognized in the 19th century. In the 1920s, after the discovery of insulin and its use in the treatment of diabetics, hyperinsulinism was suspected to be a cause of hypoglycemia in nondiabetics. A pioneering description of hyperinsulinism as a cause of hypoglycemia was published bySeale Harris
Seale Harris (March 13, 1870 – March 17, 1957) was an American physician and researcher born in Cedartown, Georgia. He was nicknamed "the Benjamin Franklin of Medicine" by contemporaries for his leadership and writing on a wide range of medical a ...
in 1924. The first report of a surgical cure of hypoglycemia by removing an islet cell tumour was in 1929.
An insulinoma removed from a woman in Munich provided insulin mRNA that was used in the first human gene cloning experiment. In 1979, Axel Ulrich cloned this gene into ''E. coli''. Most therapeutic insulin used today derives from this woman's tumour.
Additional images
See also
* Causes of hypoglycemia * Metastatic InsulinomaReferences
Further reading
* * *External links
{{Endocrine gland neoplasia Endocrine neoplasia Rare cancers Amyloidosis