haemothorax on:
[Wikipedia]
[Google]
[Amazon]
A hemothorax (derived from hemo-
 When a hemothorax occurs, blood enters the pleural cavity. The blood loss from the circulation has several effects. Firstly, as blood builds up within the pleural cavity, it begins to interfere with the normal movement of the lungs, preventing one or both lungs from fully expanding and thereby interfering with the normal transfer of oxygen and carbon dioxide to and from the blood. Secondly, blood that has been lost into the pleural cavity can no longer be circulated. Hemothoraces can lead to significant blood loss – each half of the thorax can hold more than 1500 milliliters of blood, representing more than 25% of an average adult's total blood volume. The body may struggle to cope with this blood loss, and tries to compensate by maintaining blood pressure by forcing the heart to pump harder and faster, and by squeezing or constricting small blood vessels in the arms and legs. These compensatory mechanisms can be recognised by a rapid resting heart rate and cool fingers and toes.
If the blood within the pleural cavity is not removed, it will eventually
When a hemothorax occurs, blood enters the pleural cavity. The blood loss from the circulation has several effects. Firstly, as blood builds up within the pleural cavity, it begins to interfere with the normal movement of the lungs, preventing one or both lungs from fully expanding and thereby interfering with the normal transfer of oxygen and carbon dioxide to and from the blood. Secondly, blood that has been lost into the pleural cavity can no longer be circulated. Hemothoraces can lead to significant blood loss – each half of the thorax can hold more than 1500 milliliters of blood, representing more than 25% of an average adult's total blood volume. The body may struggle to cope with this blood loss, and tries to compensate by maintaining blood pressure by forcing the heart to pump harder and faster, and by squeezing or constricting small blood vessels in the arms and legs. These compensatory mechanisms can be recognised by a rapid resting heart rate and cool fingers and toes.
If the blood within the pleural cavity is not removed, it will eventually
File:UOTW 38 - Ultrasound of the Week 4.jpg, Ultrasound scan of the chest showing a left-sided hemothorax
File:CT scan showing hemothorax caused by warfarin use.png, CT scan of the chest showing a hemothorax caused by warfarin use
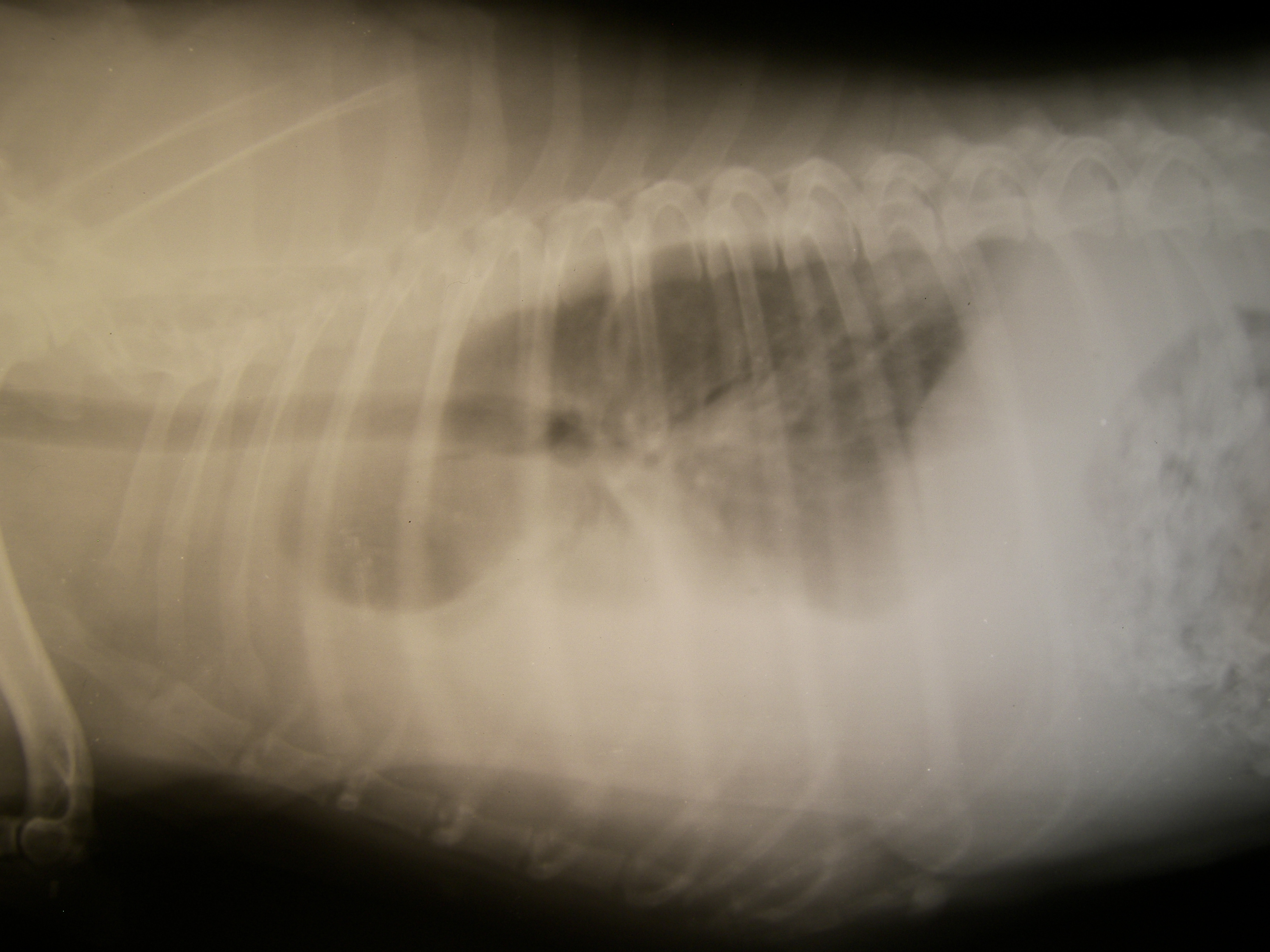
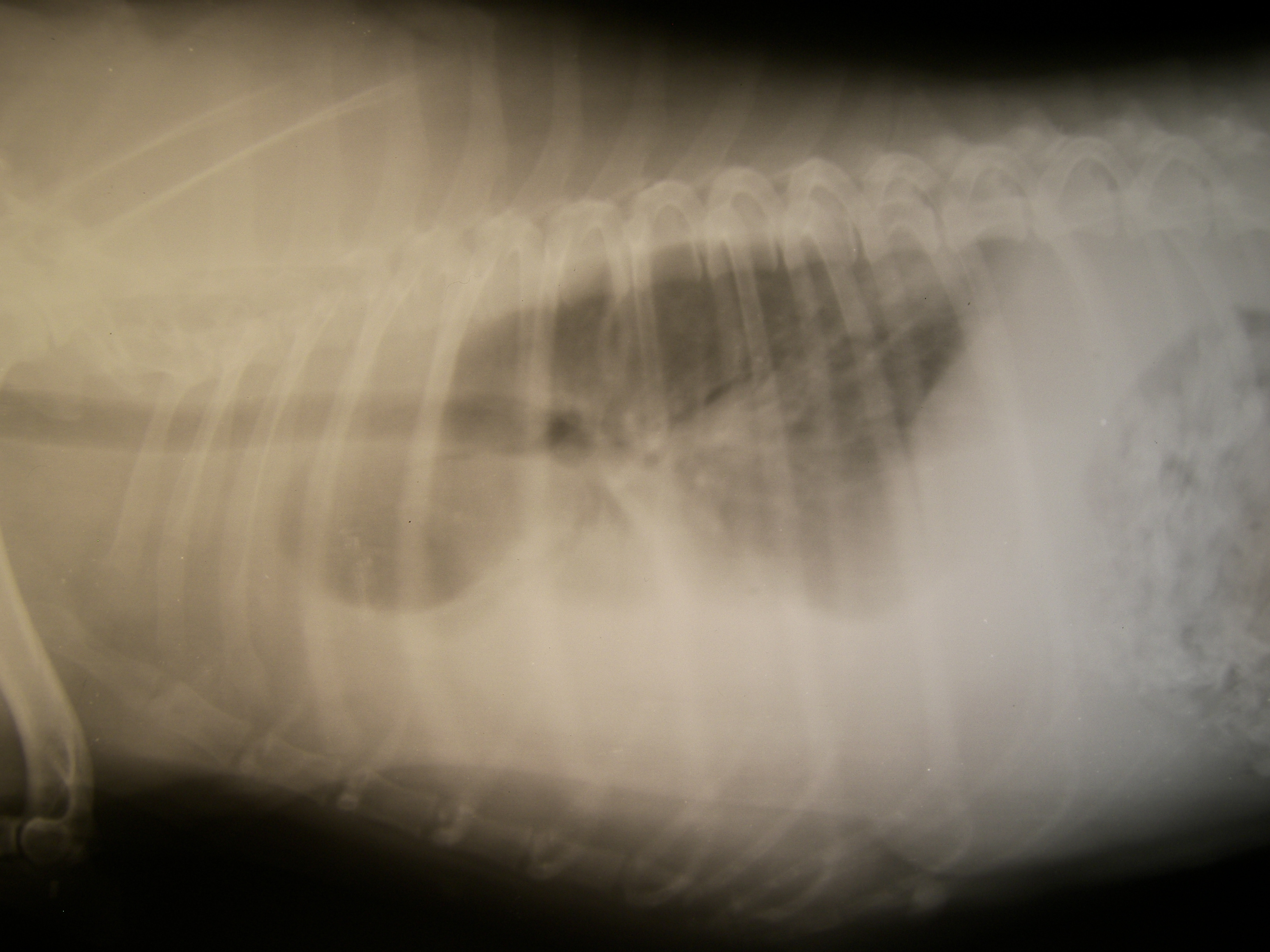
File:Chest MRI showing hemothorax in a 16 day old infant (cropped).png, Chest MRI showing a hemothorax in a 16-day-old infant
 Although imaging techniques can demonstrate that fluid is present within the pleural space, it may be unclear what this fluid represents. To establish the nature of the fluid, a sample can be removed by inserting a needle into the pleural cavity in a procedure known as a
Although imaging techniques can demonstrate that fluid is present within the pleural space, it may be unclear what this fluid represents. To establish the nature of the fluid, a sample can be removed by inserting a needle into the pleural cavity in a procedure known as a
 Blood in the cavity can be removed by inserting a drain (
Blood in the cavity can be removed by inserting a drain (

 In horses, hemothorax is uncommon and usually traumatic. It may occur along with pneumothorax. It is mainly diagnosed by ultrasound. Treatment involves supportive care, correction of the underlying cause, and occasionally drainage. The prognosis is variable.
Hemothorax is usually caused by trauma to the thorax. It can result from any injury that involves the pleural, intercostal, intervertebral,
In horses, hemothorax is uncommon and usually traumatic. It may occur along with pneumothorax. It is mainly diagnosed by ultrasound. Treatment involves supportive care, correction of the underlying cause, and occasionally drainage. The prognosis is variable.
Hemothorax is usually caused by trauma to the thorax. It can result from any injury that involves the pleural, intercostal, intervertebral,
lood
Lodewyk de Jager (born 17 December 1992) is a South African professional rugby union player for the South Africa national team and in the English Premiership. He usually plays as a lock.
Career
De Jager played at youth level for the and al ...
+ thorax
The thorax or chest is a part of the anatomy of humans, mammals, and other tetrapod animals located between the neck and the abdomen. In insects, crustaceans, and the extinct trilobites, the thorax is one of the three main divisions of the c ...
hest plural ''hemothoraces'') is an accumulation of blood within the pleural cavity
The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication b ...
. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal b ...
invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fa ...
, in response to a collapsed lung
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is ...
, or rarely in association with other conditions.
Hemothoraces are usually diagnosed using a chest X-ray
A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in me ...
, but they can be identified using other forms of imaging including ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies ...
, a CT scan, or an MRI
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves ...
. They can be differentiated from other forms of fluid within the pleural cavity by analysing a sample of the fluid, and are defined as having a hematocrit
The hematocrit () (Ht or HCT), also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is norm ...
of greater than 50% that of the person's blood. Hemothoraces may be treated by draining the blood using a chest tube
A chest tube (also chest drain, thoracic catheter, tube thoracostomy or intercostal drain) is a surgical drain that is inserted through the chest wall and into the pleural space or the mediastinum in order to remove clinically undesired substance ...
. Surgery may be required if the bleeding continues. If treated, the prognosis is usually good. Complications of a hemothorax include infection within the pleural cavity and the formation of scar tissue.
Background
The lungs are surrounded by two layers of tissue called thepulmonary pleurae
The pulmonary pleurae (''sing.'' pleura) are the two opposing layers of serous membrane overlying the lungs and the inside of the surrounding chest walls.
The inner pleura, called the visceral pleura, covers the surface of each lung and dips be ...
. In most healthy people, these two layers are tightly apposed, separated only by a small amount of pleural fluid
The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication be ...
. In certain disease states, the space between these two layers, called the pleural cavity
The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication b ...
, swells with fluid. This accumulation of fluid in the pleural cavity is called pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
. Pleural effusions are given specific names depending on the nature of the fluid: hydrothorax
Hydrothorax is a type of pleural effusion in which transudate accumulates in the pleural cavity. This condition is most likely to develop secondary to congestive heart failure, following an increase in hydrostatic pressure within the lungs. More ...
for serous fluid
In physiology, serous fluid or serosal fluid (originating from the Medieval Latin word ''serosus'', from Latin ''serum'') is any of various body fluids resembling serum, that are typically pale yellow or transparent and of a benign nature. The fl ...
, pyothorax
Pleural empyema is a collection of pus in the pleural cavity caused by microorganisms, usually bacteria. Often it happens in the context of a pneumonia, injury, or chest surgery. It is one of the various kinds of pleural effusion. There are three ...
for pus, hemothorax for blood, and urinothorax
Urinothorax (''pl''. urinothoraces) is defined as urine in the fluid-filled cavity that surrounds the lungs. It is usually caused by obstructive uropathy. It is mainly diagnosed by analyzing the pleural fluid. Treatment involves treating the un ...
for urine.
Signs and symptoms
Signs and symptoms include anxiety, rapid breathing, restlessness, shock, and pale, cool, clammy skin. When the affected area is percussed, a dull feeling may be observed. Neck veins may be flat and breathing sounds reduced. It can also cause a collapsed lung (atelectasis
Atelectasis is the collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct ...
). Massive hemothorax, often defined as over 1.5 liters of blood initially when an intercostal drain is placed, or a bleeding rate greater than .2 liters/hr, can result in shock with two causes: massive bleeding resulting from hypovolemic shock, and venous pressure from the retained blood, impairing blood flow.
Causes
Hemothoraces are classified in three broad categories according to the cause and in order of frequency: traumatic, iatrogenic, or nontraumatic. All three categories have the potential to affect major arteries and result in death by blood loss.Traumatic
Hemothorax is most often caused by blunt or penetrating trauma to the chest. In blunt traumatic cases, hemothorax typically occurs when rib fracture damages the intercostal vessels or the intraparenchymal pulmonary vessel, while in penetrating trauma, hemothorax occurs due to injuries directly affecting blood vessels in the thoracic wall, lung parenchyma, or the heart. If large blood vessels such as the aorta are damaged, the blood loss can be massive. Minor chest trauma can cause hemothorax when the blood's ability to clot is diminished as result either ofanticoagulant
Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where t ...
medications or when there are bleeding disorders such as hemophilia
Haemophilia, or hemophilia (), is a mostly inherited genetic disorder that impairs the body's ability to make blood clots, a process needed to stop bleeding. This results in people bleeding for a longer time after an injury, easy bruising ...
.
Iatrogenic
Iatrogenic
Iatrogenesis is the causation of a disease, a harmful complication, or other ill effect by any medical activity, including diagnosis, intervention, error, or negligence. "Iatrogenic", ''Merriam-Webster.com'', Merriam-Webster, Inc., accessed 27 ...
hemothorax can occur as a complication of heart and lung surgery, for example the rupture of lung arteries caused by the placement of catheters, thoracotomy, thoracostomy, or thoracentesis
Thoracentesis , also known as thoracocentesis (from Greek ''thōrax'' 'chest, thorax'—GEN ''thōrakos''—and ''kentēsis'' 'pricking, puncture'), pleural tap, needle thoracostomy, or needle decompression (often used term), is an invasive med ...
. The most common iatrogenic causes include subclavian venous catheterizations and chest tube placements, with an occurrence rate of around 1%. Sometimes, a Swan-Ganz catheter causes rupture of the pulmonary artery, causing a massive hemothorax. It can also be caused by other procedures like pleural
The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication b ...
, lung
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of ...
, or transbronchial biopsies, CPR
Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation in an effort to manually preserve intact brain function until further measures are taken to restore spont ...
, Nuss procedure
The Nuss procedure is a minimally-invasive procedure, invented in 1987 by Dr. Donald Nuss for treating pectus excavatum. He developed it at Children's Hospital of The King's Daughters, in Norfolk, Virginia. The operation typically takes approxi ...
, or endoscopic treatment of esophageal varices
Esophageal varices are extremely dilated sub-mucosal veins in the lower third of the esophagus. They are most often a consequence of portal hypertension, commonly due to cirrhosis. People with esophageal varices have a strong tendency to develop s ...
. Iatrogenic hemothorax is more common in people who have chronic kidney disease in the intensive care unit.
Nontraumatic
Less frequently, hemothoraces may occur spontaneously. Nontraumatic hemothoraces most frequently occur as a complication of some forms of cancer if the tumour invades the pleural space. Cancers responsible for hemothoraces includeangiosarcoma
Angiosarcoma is a rare and aggressive cancer that starts in the endothelial cells that line the walls of blood vessels or lymphatic vessels. Since they are made from vascular lining, they can appear anywhere and at any age, but older people are ...
s, schwannoma
A schwannoma (or neurilemmoma) is a usually benign nerve sheath tumor composed of Schwann cells, which normally produce the insulating myelin sheath covering peripheral nerves.
Schwannomas are homogeneous tumors, consisting only of Schwann cells ...
s, mesothelioma
Mesothelioma is a type of cancer that develops from the thin layer of tissue that covers many of the internal organs (known as the mesothelium). The most common area affected is the lining of the lungs and chest wall. Less commonly the lining ...
, thymoma
A thymoma is a tumor originating from the epithelial cells of the thymus that is considered a rare malignancy. Thymomas are frequently associated with neuromuscular disorders such as myasthenia gravis; thymoma is found in 20% of patients with ...
s, germ cell tumours, and lung cancer
Lung cancer, also known as lung carcinoma (since about 98–99% of all lung cancers are carcinomas), is a malignant lung tumor characterized by uncontrolled cell growth in tissues of the lung. Lung carcinomas derive from transformed, mali ...
. Significant hemothoraces can occur with spontaneous rupture of small vessels when the blood's ability to clot is diminished as result of anticoagulant
Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where t ...
medications. In cases caused by anticoagulant therapy, the hemothorax becomes noticeable 4–7 days after anticoagulant therapy is started. In cases of hemothorax complicating pulmonary embolism treatment, the hemothorax is usually on the side of the original embolism. Those with an abnormal accumulation of air within the pleural space (a pneumothorax) can bleed into the cavity, which occurs in about 5% of cases of spontaneous pneumothorax, especially when lung bullae
A focal lung pneumatosis, is an enclosed pocket of air or gas in the lung and includes blebs, bullae, pulmonary cysts, and lung cavities. Blebs and bullae can be classified by their wall thickness.
* A bleb has a wall thickness of less than 1 mm ...
rupture. The resulting combination of air and blood within the pleural space is known as a hemopneumothorax. Bone growth in exostosis
An exostosis, also known as bone spur, is the formation of new bone on the surface of a bone. Exostoses can cause chronic pain ranging from mild to debilitatingly severe, depending on the shape, size, and location of the lesion. It is most commonl ...
can create sharp edges, which can result in hemothorax by damaging adjacent arteries. It can occur postpartum
The postpartum (or postnatal) period begins after childbirth and is typically considered to end within 6 weeks as the mother's body, including hormone levels and uterus size, returns to a non-pregnant state. The terms puerperium, puerperal pe ...
due to the change in thoracic pressure during labor.
Vascular
Vascular causes of hemothorax include rupture of the descending aorta, in which case it initially involves the left pleural and mediastinal area due to the close vicinity of the pleural cavity. Rarely, a rupture of the thoracic aorta can result in a hemothorax, but the bleeding usually occurs in the pericardial space. Spontaneous tearing of blood vessels is more likely to occur in those with disorders that weaken blood vessels such as some forms of Ehlers-Danlos syndrome, disorders that lead to malformed blood vessels as seen in Rendu-Osler-Weber syndrome, or in bleeding disorders such as hemophilia and Glanzmann thrombasthenia. Other rare causes of hemothorax includeneurofibromatosis type 1
Neurofibromatosis (NF) is a group of three conditions in which tumors grow in the nervous system. The three types are neurofibromatosis type I (NF1), neurofibromatosis type II (NF2), and schwannomatosis. In NF1 symptoms include light brown spo ...
and extramedullary hematopoiesis.
Catamenial
Rarely, hemothoraces can arise due toextrapelvic endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fall ...
, a condition in which tissue similar to the lining that normally covers the inside of the uterus
The uterus (from Latin ''uterus'', plural ''uteri'') or womb () is the organ in the reproductive system of most female mammals, including humans that accommodates the embryonic and fetal development of one or more embryos until birth. The ...
forms in unusual locations outside the pelvis. Endometriotic tissue that implants on the pleural surface can bleed in response to the hormonal changes of the menstrual cycle, causing what is known as a catamenial hemothorax as part of thoracic endometriosis along with catamenial pneumothorax
Catamenial pneumothorax is a spontaneous pneumothorax that recurs during menstruation, within 72 hours before or after the onset of a cycle. It usually involves the right side of the chest and right lung, and is associated with thoracic endometrio ...
, catamenial hemoptysis
Hemoptysis is the coughing up of blood or blood-stained mucus from the bronchi, larynx, trachea, or lungs. In other words, it is the airway bleeding. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia, a ...
, and lung nodule
A lung nodule or pulmonary nodule is a relatively small focal density in the lung. A solitary pulmonary nodule (SPN) or coin lesion, is a mass in the lung smaller than three centimeters in diameter. A pulmonary micronodule has a diameter of less ...
s of endometriosis.
Catamenial hemothorax represents 14% of cases of thoracic endometriosis syndrome while catamenial pneumothorax is seen in 73%, catamenial hemoptysis in 7%, and pulmonary nodules in 6%.
Mechanism
 When a hemothorax occurs, blood enters the pleural cavity. The blood loss from the circulation has several effects. Firstly, as blood builds up within the pleural cavity, it begins to interfere with the normal movement of the lungs, preventing one or both lungs from fully expanding and thereby interfering with the normal transfer of oxygen and carbon dioxide to and from the blood. Secondly, blood that has been lost into the pleural cavity can no longer be circulated. Hemothoraces can lead to significant blood loss – each half of the thorax can hold more than 1500 milliliters of blood, representing more than 25% of an average adult's total blood volume. The body may struggle to cope with this blood loss, and tries to compensate by maintaining blood pressure by forcing the heart to pump harder and faster, and by squeezing or constricting small blood vessels in the arms and legs. These compensatory mechanisms can be recognised by a rapid resting heart rate and cool fingers and toes.
If the blood within the pleural cavity is not removed, it will eventually
When a hemothorax occurs, blood enters the pleural cavity. The blood loss from the circulation has several effects. Firstly, as blood builds up within the pleural cavity, it begins to interfere with the normal movement of the lungs, preventing one or both lungs from fully expanding and thereby interfering with the normal transfer of oxygen and carbon dioxide to and from the blood. Secondly, blood that has been lost into the pleural cavity can no longer be circulated. Hemothoraces can lead to significant blood loss – each half of the thorax can hold more than 1500 milliliters of blood, representing more than 25% of an average adult's total blood volume. The body may struggle to cope with this blood loss, and tries to compensate by maintaining blood pressure by forcing the heart to pump harder and faster, and by squeezing or constricting small blood vessels in the arms and legs. These compensatory mechanisms can be recognised by a rapid resting heart rate and cool fingers and toes.
If the blood within the pleural cavity is not removed, it will eventually clot
A thrombus (plural thrombi), colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cr ...
. This clot tends to stick the parietal and visceral pleura together and has the potential to lead to scarring within the pleura, which if extensive leads to the condition known as a fibrothorax
Fibrothorax is a medical condition characterised by severe scarring (fibrosis) and fusion of the layers of the pleural space surrounding the lungs resulting in decreased movement of the lung and ribcage. The main symptom of fibrothorax is shortn ...
. Following the initial loss of blood, a small hemothorax may irritate the pleura, causing additional fluid to seep out, leading to a bloodstained pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per k ...
. Furthermore, as enzymes in the pleural fluid
The pleural cavity, pleural space, or interpleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication be ...
begin to break down the clot, the protein concentration of the pleural fluid increases. As a result, the osmotic pressure
Osmotic pressure is the minimum pressure which needs to be applied to a solution to prevent the inward flow of its pure solvent across a semipermeable membrane.
It is also defined as the measure of the tendency of a solution to take in a pure ...
of the pleural cavity increases, causing fluid to leak into the pleural cavity from the surrounding tissues.
Diagnosis
Hemothoraces are most commonly detected using achest X-ray
A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in me ...
, although ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies ...
is sometimes used in an emergency setting. It can be suspected in any person with any form of chest trauma. However, plain X-rays may miss smaller hemothoraces while other imaging modalities such as computed tomography (CT), or magnetic resonance imaging may be more sensitive. In cases where the nature of an effusion is in doubt, a sample of fluid can be aspirated and analysed in a procedure called thoracentesis
Thoracentesis , also known as thoracocentesis (from Greek ''thōrax'' 'chest, thorax'—GEN ''thōrakos''—and ''kentēsis'' 'pricking, puncture'), pleural tap, needle thoracostomy, or needle decompression (often used term), is an invasive med ...
. Physical examination is used initially. Auscultation has been reported to have an accuracy of nearly 100% in diagnosing hemopneumothorax.
Chest X-ray
A chest X-ray is the most common technique used to diagnosis a hemothorax. X-rays should ideally be taken in an upright position (an erect chest X-ray), but may be performed with the person lying on their back (supine) if an erect chest X-ray is not feasible. On an erect chest X-ray, a hemothorax is suggested by blunting of thecostophrenic angle
The costodiaphragmatic recess, also called the costophrenic recess or phrenicocostal sinus, costodiaphragmatic-recess Retrieved May 2011
Imaging
In anatomy, the costophrenic angles are the places where the diaphragm (''-phrenic'') meets the ribs ...
or partial or complete opacification of the affected half of the thorax. On a supine film the blood tends to layer in the pleural space, but can be appreciated as a haziness of one half of the thorax relative to the other. A small hemothorax may be missed on a chest X-ray as several hundred milliliters of blood can be hidden by the diaphragm
Diaphragm may refer to:
Anatomy
* Thoracic diaphragm, a thin sheet of muscle between the thorax and the abdomen
* Pelvic diaphragm or pelvic floor, a pelvic structure
* Urogenital diaphragm or triangular ligament, a pelvic structure
Other
* Diap ...
and abdominal viscera on an erect film. Supine X-rays are even less sensitive and as much as one liter of blood can be missed on a supine film.
Other methods
Ultrasonography may be used to detect hemothorax and other pleural effusions. This technique is of particular use in the critical care and trauma settings as it provides rapid, reliable results at the bedside. Ultrasound is more sensitive than chest x-ray in detecting hemothorax. Ultrasound can cause issues in people who are morbidlyobese
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's we ...
or have subcutaneous emphysema. When CT is unavailable in the current setting or the person cannot be moved to the scan, ultrasound is used.
Computed tomography (CT or CAT) scans may be useful for diagnosing retained hemothorax as this form of imaging can detect much smaller amounts of fluid than a plain chest X-ray. However, CT is less used as a primary means of diagnosis within the trauma setting, as these scans require a critically ill person to be transported to a scanner, are slower, and require the subject to remain supine.
Magnetic resonance imaging (MRI) can be used to differentiate between a hemothorax and other forms of pleural effusion, and can suggest how long the hemothorax has been present for. Fresh blood can be seen as a fluid with low T1 but high T2 signals, while blood that has been present for more than a few hours displays both low T1 and T2 signals. MRI is used infrequently in the trauma setting due to the prolonged time required to perform an MRI, and the deterioration in image quality that occurs with motion.
Thoracentesis
 Although imaging techniques can demonstrate that fluid is present within the pleural space, it may be unclear what this fluid represents. To establish the nature of the fluid, a sample can be removed by inserting a needle into the pleural cavity in a procedure known as a
Although imaging techniques can demonstrate that fluid is present within the pleural space, it may be unclear what this fluid represents. To establish the nature of the fluid, a sample can be removed by inserting a needle into the pleural cavity in a procedure known as a thoracentesis
Thoracentesis , also known as thoracocentesis (from Greek ''thōrax'' 'chest, thorax'—GEN ''thōrakos''—and ''kentēsis'' 'pricking, puncture'), pleural tap, needle thoracostomy, or needle decompression (often used term), is an invasive med ...
or pleural tap. In this context, the most important assessment of the pleural fluid is the percentage by volume that is taken up by red blood cells (the hematocrit
The hematocrit () (Ht or HCT), also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is norm ...
) A hemothorax is defined as having a hematocrit of at least 50% of that found in the affected person's blood, although the hematocrit of a chronic hemothorax may be between 25 and 50% if additional fluid has been secreted by the pleura. Pleural fluid can dilute hemothoraces in as low as 3–4 days. The red blood cells in the effusion spontaneously break down. Distinguishing the pleural fluid from blood by colour is impossible when the hematocrit value is over 5%. For these reasons, even if there is a hematocrit value under 50%, further investigations can be done in order to figure out if there is a source of bleeding. Hematocrit can be roughly calculated by dividing the red blood cell count of the pleural fluid by 100,000. Thoracentesis is the test most commonly used to diagnose a hemothorax in animals. Hemothorax can itself be a rare complication of thoracentesis if the intercostal artery is punctured.
Treatment
The treatment of a hemothorax depends largely on the extent of bleeding. While small hemothoraces may require little in the way of treatment, larger hemothoraces may require fluid resuscitation to replace the blood that has been lost, drainage of the blood within the pleural space using a procedure known as a tubethoracostomy
A thoracostomy is a small incision of the chest wall, with maintenance of the opening for drainage. It is most commonly used for the treatment of a pneumothorax. This is performed by physicians, paramedics, and nurses usually via needle thoracosto ...
, and potentially surgery in the form of a thoracotomy
A thoracotomy is a surgical procedure to gain access into the pleural space of the chest. It is performed by surgeons (emergency physicians or paramedics under certain circumstances) to gain access to the thoracic organs, most commonly the hea ...
or video-assisted thoracoscopic surgery
Video-assisted thoracoscopic surgery (VATS) is a type of minimally invasive thoracic surgery performed using a small video camera mounted to a fiberoptic thoracoscope (either 5 mm or 10 mm caliber), with or without angulated visualiza ...
(VATS) to prevent further bleeding. Occasionally, transcatheter arterial embolization may be used to stop ongoing arterial bleeding. Additional treatment options include antibiotics to reduce the risk of infection and fibrinolytic therapy
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive p ...
to break down clotted blood within the pleural space.
Thoracostomy
 Blood in the cavity can be removed by inserting a drain (
Blood in the cavity can be removed by inserting a drain (chest tube
A chest tube (also chest drain, thoracic catheter, tube thoracostomy or intercostal drain) is a surgical drain that is inserted through the chest wall and into the pleural space or the mediastinum in order to remove clinically undesired substance ...
) in a procedure called a tube thoracostomy. This procedure is indicated for most causes of hemothorax, but should be avoided in aortic rupture which should be managed with immediate surgery. The thoracostomy tube is usually placed between the ribs in the sixth or seventh intercostal space
The intercostal space (ICS) is the anatomic space between two ribs (Lat. costa). Since there are 12 ribs on each side, there are 11 intercostal spaces, each numbered for the rib superior to it.
Structures in intercostal space
* several kind ...
at the mid-axillary line
The axillary lines are the anterior axillary line, midaxillary line and the posterior axillary line.
The anterior axillary line
is a coronal line on the anterior torso marked by the anterior axillary fold. It's the imaginary line that runs dow ...
. It is important to avoid a chest tube becoming obstructed by clotted blood as obstruction prevents adequate drainage of the pleural space. Clotting occurs as the clotting cascade
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism ...
is activated when the blood leaves the blood vessels and comes into contact with the pleural surface, injured lung or chest wall, or the thoracostomy tube. Inadequate drainage may lead to a retained hemothorax, increasing the risk of infection within the pleural space (empyema
An empyema () is a collection or gathering of pus within a naturally existing anatomical cavity. For example, pleural empyema is empyema of the pleural cavity. It must be differentiated from an abscess, which is a collection of pus in a newly fo ...
) or the formation of scar tissue (fibrothorax). Thoracostomy tubes with a diameter of 24–36 F (large-bore tubes) should be used, as these reduce the risk of blood clots obstructing the tube. Manual manipulation of chest tubes (referred to as milking, stripping, or tapping) is commonly performed to maintain an open tube, but no conclusive evidence has demonstrated that this improves drainage. If a chest tube does become obstructed, the tube can be cleared using open or closed techniques. Tubes should be removed as soon as drainage has stopped, as prolonged tube placement increases the risk of empyema.


Surgery
About 10–20% of traumatic hemothoraces require surgical management. Larger hemothoraces, or those that continue to bleed following drainage, may require surgery. This surgery may take the form of a traditional open-chest procedure (a thoracotomy), but may be performed using video-associated thoracoscopic surgery (VATS). While there is no universally accepted cutoff for the volume of blood loss required before surgery is indicated, generally accepted indications include more than 1500 mL of blood drained from a thoracostomy, bleeding rate of over 500mL/hr in the first hour followed by over 200 mL, hemodynamic instability, or the need for repeat blood transfusions. VATS is less invasive and cheaper than an open thoracotomy, and can reduce the length of hospital stay, but a thoracotomy may be preferred whenhypovolemic shock
Hypovolemic shock is a form of shock caused by severe hypovolemia (insufficient blood volume or extracellular fluid in the body). It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a ...
is present, in order to watch bleeding. The procedure should ideally be performed within 72 hours of the injury as delay may increase the risk of complications. In clotted hemothorax, VATS is the generally preferred procedure to remove the clot, and is indicated if the hemothorax fills 1/3 or more of a hemithorax. The ideal time to remove a clot using VATS is at 48–96 hours, but can be attempted up to nine days after the injury.
Other
Thoracentesis is no longer used in the ''treatment'' of hemothorax, although it may still be used to treat small hemothoraces. In catamenial hemothorax, the bleeding is typically self-limiting and mild. Most people with the condition are stable and can be treated with hormonal therapies. They are only partially effective. Surgical removal of the endometrial tissue may be necessary in recurrent cases. However, the disease frequently recurs. Resuscitation with intravenous fluids or withblood products
A blood product is any therapeutic substance prepared from human blood. This includes whole blood; blood components; and plasma derivatives. Whole blood is not commonly used in transfusion medicine. Blood components include: red blood cell conce ...
may be required. In fulminant cases, transfusions may be administered before admission to the hospital. Clotting abnormalities, such as those caused by anticoagulant medications, should be reversed. Prophylactic antibiotics are given for 24 hours in the case of trauma. Blood clots may be retained within the pleural cavity despite chest tube drainage. They are a risk factor for complications like fibrothorax and empyema. Such retained clots should be removed, preferably with video-assisted thoracoscopic surgery
Video-assisted thoracoscopic surgery (VATS) is a type of minimally invasive thoracic surgery performed using a small video camera mounted to a fiberoptic thoracoscope (either 5 mm or 10 mm caliber), with or without angulated visualiza ...
(VATS). If VATS is unavailable, an alternative is fibrinolytic therapy
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive p ...
such as streptokinase
Streptokinase (SK) is a thrombolytic medication activating plasminogen by nonenzymatic mechanism. As a medication it is used to break down clots in some cases of myocardial infarction (heart attack), pulmonary embolism, and arterial thromboembol ...
or urokinase
Urokinase, also known as urokinase-type plasminogen activator (uPA), is a serine protease present in humans and other animals. The human urokinase protein was discovered, but not named, by McFarlane and Pilling in 1947. Urokinase was originally ...
given directly into the pleural space seven to ten days after the injury. The issues with fibrinolytic therapy include having a high cost and lengthened hospital stay. Residual clot that does not dissipate in response to fibrinolytics may require surgical removal in the form of decortication.
Prognosis
The prognosis following a hemothorax depends on its size, the treatment given, and the underlying cause. While small hemothoraces may cause little in the way of problems, in severe cases an untreated hemothorax may be rapidly fatal due to uncontrolled blood loss. If left untreated, the accumulation of blood may put pressure on themediastinum
The mediastinum (from ) is the central compartment of the thoracic cavity. Surrounded by loose connective tissue, it is an undelineated region that contains a group of structures within the thorax, namely the heart and its vessels, the esopha ...
and the trachea, limiting the heart's ability to fill. However, if treated, the prognosis following a traumatic hemothorax is usually favourable and dependent on other non-thoracic injuries that have been sustained at the same time, the age of the person, and the need for mechanical ventilation
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move a ...
. Hemothoraces caused by benign conditions such as endometriosis have a good prognosis, while those caused by neurofibromatosis type 1 has a 36% rate of death, and those caused by aortic rupture are often fatal. Penetrating trauma is significantly less common, and has a much higher death rate, with up to 90% dying before arriving at the hospital. Gunshot wound
A gunshot wound (GSW) is a penetrating injury caused by a projectile (e.g. a bullet) from a gun (typically firearm or air gun). Damages may include bleeding, bone fractures, organ damage, wound infection, loss of the ability to move pa ...
s are associated with a higher death rates compared to stab wound
A stab wound is a specific form of penetrating trauma to the skin that results from a knife or a similar pointed object. While stab wounds are typically known to be caused by knives, they can also occur from a variety of implements, including brok ...
s. In cases of penetrating trauma involving the heart, less than 1% survive.
Complications
Complications can occur following a hemothorax, and are more likely to occur if the blood has not been adequately drained from the pleural cavity. Blood that remains within the pleural space can become infected, and is known as anempyema
An empyema () is a collection or gathering of pus within a naturally existing anatomical cavity. For example, pleural empyema is empyema of the pleural cavity. It must be differentiated from an abscess, which is a collection of pus in a newly fo ...
. It occurs in 3–4% of traumatic cases, and 27-33% of retained hemothoraces. It is more likely in people who develop shock, had a contaminated pleural space during the injury, persistent bronchopleural fistula A bronchopleural fistula (BPF) is a fistula between the pleural space and the lung. It can develop following pneumonectomy, lung ablation, post-traumatically, or with certain types of infection. It may also develop when large airways are in communic ...
e, and lung contusions. The likelihood of it can be reduced by keeping thoracostomy tubes sterile and by keeping the pleural surfaces close together to prevent fluid or blood from accumulating between the surfaces. The retained blood can irritate the pleura, causing scar tissue (adhesions
Adhesions are fibrous bands that form between tissues and organs, often as a result of injury during surgery. They may be thought of as internal scar tissue that connects tissues not normally connected.
Pathophysiology
Adhesions form as a natural ...
) to form. If extensive, this scar tissue can encase the lung, restricting movement of the chest wall, and is then referred to as a fibrothorax
Fibrothorax is a medical condition characterised by severe scarring (fibrosis) and fusion of the layers of the pleural space surrounding the lungs resulting in decreased movement of the lung and ribcage. The main symptom of fibrothorax is shortn ...
. Less than 1 percent of cases go on to develop a fibrothorax. Cases with hemopneumothorax or infection more often develop fibrothorax. After the chest tube is removed, over 10% of cases develop pleural effusions that are mostly self-limited and leave no lasting complications. In such cases, thoracentesis is performed to eliminate the possibility of an infection being present. Other potential complications include atelectasis
Atelectasis is the collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct ...
, lung infection, pneumothorax, sepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is follo ...
, respiratory distress
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing disc ...
, hypotension
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure (the top number) and the di ...
, tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ( ...
, pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severit ...
, adhesions, and impaired lung function.
Epidemiology
Trauma to the thorax results in approximately 16,000 to 30,000 deaths every year. There are about 300,000 cases of hemothorax in the U.S every year.Polytrauma Polytrauma and multiple trauma are medical terms describing the condition of a person who has been subjected to multiple traumatic injuries, such as a serious head injury in addition to a serious burn. The term is defined via an Injury Severity Sc ...
(injury to multiple body systems) involves chest injuries in 60% of cases and commonly leads to hemothorax. In a case study, 37% of people hospitalized for blunt chest trauma had traumatic hemothorax. Hemothorax commonly occurs with a displaced rib fracture.
Other animals
Horses
 In horses, hemothorax is uncommon and usually traumatic. It may occur along with pneumothorax. It is mainly diagnosed by ultrasound. Treatment involves supportive care, correction of the underlying cause, and occasionally drainage. The prognosis is variable.
Hemothorax is usually caused by trauma to the thorax. It can result from any injury that involves the pleural, intercostal, intervertebral,
In horses, hemothorax is uncommon and usually traumatic. It may occur along with pneumothorax. It is mainly diagnosed by ultrasound. Treatment involves supportive care, correction of the underlying cause, and occasionally drainage. The prognosis is variable.
Hemothorax is usually caused by trauma to the thorax. It can result from any injury that involves the pleural, intercostal, intervertebral, cardiac
The heart is a muscular organ in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as carbon dioxide to t ...
, or thoracic wall muscle. It can rarely be caused by diaphragmatic rupture that results in abdominal herniation. Hemothorax can be caused be cancers involving the thoracic, pulmonary, and mediastinal wall. The most common cancer resulting in hemothorax is a hemangiosarcoma
Hemangiosarcoma is a rapidly growing, highly invasive variety of cancer that occurs almost exclusively in dogs, and only rarely in cats, horses, mice, or humans (vinyl chloride toxicity). It is a sarcoma arising from the lining of blood vessels; ...
.
Clinical signs and symptoms may be variable and cause-dependant. They may include rapid breathing, pain, and shallow breathing in cases with a rib fracture. In the case of extensive bleeding, signs of hypovolemia may occur, and rapid death may result within hours. In less acute cases with slower bleeding, anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
and hypoproteinemia may gradually develop.
Ultrasound can detect blood in the pleural cavity. Blood in the thorax is shown by a uniform area without flocculation
Flocculation, in the field of chemistry, is a process by which colloidal particles come out of suspension to sediment under the form of floc or flake, either spontaneously or due to the addition of a clarifying agent. The action differs from ...
. Pleural effusions without blood are usually hypoechoic. Echogenicity
Echogenicity (misspelled sometimes as echogenecity) or echogeneity is the ability to bounce an echo, e.g. return the signal in ultrasound examinations. In other words, echogenicity is higher when the surface bouncing the sound echo reflects incre ...
is indicated by cellular debris and/or fibrin. Bloody pleural effusions are shows by a swirling, hyperechoic pattern. When a stethoscope is used (auscultation
Auscultation (based on the Latin verb ''auscultare'' "to listen") is listening to the internal sounds of the body, usually using a stethoscope. Auscultation is performed for the purposes of examining the circulatory and respiratory systems (he ...
), the heartbeat sounds are faint. When percussion is performed, it produces a dull area. However, especially in traumatic cases, percussion may be painful. Although nonspecific, physical examinations may show reduced lung sounds and muffled, widespread heart sounds. Similar signs and symptoms may occur when other fluids are in the pleural cavity.
Treatment includes correction of the underlying cause. Drainage is not always required, but can be performed in case of infection or fluid levels resulting in respiratory compromise. However, drainage in contraindicated in cases caused by clotting disorders. Additionally, broad spectrum antibiotics can be given in the case of open trauma or pulmonary rupture. Supportive care may be required. It may include intranasal oxygen, painkillers, blood transfusions, and fluids. In order to avoid fluid overload, fluids are given slowly.
The prognosis significantly depends on the underlying cause of the hemothorax. In cases caused by uncomplicated thoracic trauma, the prognosis may be good, but the prognosis is worse in cases that are complicated by pleuritis
Pleurisy, also known as pleuritis, is inflammation of the membranes that surround the lungs and line the chest cavity (pleurae). This can result in a sharp chest pain while breathing. Occasionally the pain may be a constant dull ache. Other sym ...
. Cases caused by cancer or clotting disorders have a poor prognosis, as do cases with massive bleeding due to injury to the heart or very large blood vessels.
References
External links
{{Trauma , state=autocollapse Chest trauma Disorders of fascia Medical emergencies Diseases of pleura