History And Naming Of Human Leukocyte Antigens on:
[Wikipedia]
[Google]
[Amazon]

 Late in 1973 a pair of researchers in Australia, Rolf Zinkernagel and Peter Doherty made a revelatory discovery that altered the thinking of immunologists forever. The pair was doing research on viral infections in mice and noticed that T-cells that prevented viral infections in some mice wouldn't always prevent the same infection in other mice. After looking at the MHCs present in the mice, they realized that cytotoxic T-cells could only identify virus infections in cells with the right Class I compatibility gene. Traditional thinking was that the immune system identified infections directly but this discovery turned that theory on its head. Compatibility genes were essential in immune system mediated viral clearing. The pair coined the term "MHC Restriction" to describe this relationship between T-cells, specific MHC proteins, and viral detection. In 1975, in an article in the journal ''Lancet'', they introduced the idea of "altered self", meaning that viruses alter the MHC proteins and this alteration is detected by T-cells. For their work they won the 1996 Nobel Prize. It took the work of many others to determine how T-cells made this identification.
Late in 1973 a pair of researchers in Australia, Rolf Zinkernagel and Peter Doherty made a revelatory discovery that altered the thinking of immunologists forever. The pair was doing research on viral infections in mice and noticed that T-cells that prevented viral infections in some mice wouldn't always prevent the same infection in other mice. After looking at the MHCs present in the mice, they realized that cytotoxic T-cells could only identify virus infections in cells with the right Class I compatibility gene. Traditional thinking was that the immune system identified infections directly but this discovery turned that theory on its head. Compatibility genes were essential in immune system mediated viral clearing. The pair coined the term "MHC Restriction" to describe this relationship between T-cells, specific MHC proteins, and viral detection. In 1975, in an article in the journal ''Lancet'', they introduced the idea of "altered self", meaning that viruses alter the MHC proteins and this alteration is detected by T-cells. For their work they won the 1996 Nobel Prize. It took the work of many others to determine how T-cells made this identification.
 In the early 1960s, some physicians began more aggressive attempts at
In the early 1960s, some physicians began more aggressive attempts at
 Hemagglutination assay. In generating an immune response to an antigen, the
Hemagglutination assay. In generating an immune response to an antigen, the
 As the study of these 'rejection' sera and "allo"-antigens progressed, certain patterns in the antibody recognition were recognized. The first major observation, in 1969, was that an allotypic antibodies to "4" ("Four") was only found on lymphocytes, while most of the antigens, termed "LA", recognized most cells in the body.
This group "4" antigen on lymphocytes would expand into "4a", "4b" and so on, becoming the "D" series (HLA-D (Class II) antigens) DP, DQ, and DR. This is an interesting history in itself.
The Hu-1 antigens were renamed the Human-lymphoid (HL) allo-antigens (HL-As). Allo-antigen comes from the observation that a tolerated protein in the donor becomes antigenic in the recipient. This can be compared with an
As the study of these 'rejection' sera and "allo"-antigens progressed, certain patterns in the antibody recognition were recognized. The first major observation, in 1969, was that an allotypic antibodies to "4" ("Four") was only found on lymphocytes, while most of the antigens, termed "LA", recognized most cells in the body.
This group "4" antigen on lymphocytes would expand into "4a", "4b" and so on, becoming the "D" series (HLA-D (Class II) antigens) DP, DQ, and DR. This is an interesting history in itself.
The Hu-1 antigens were renamed the Human-lymphoid (HL) allo-antigens (HL-As). Allo-antigen comes from the observation that a tolerated protein in the donor becomes antigenic in the recipient. This can be compared with an
 A series of tests on cultured cells revealed that, within the "LA" group, a donor tissue might have some antigens but not others. For example, an antiserum may react with patterns (on a given tissue):
* A1, A2, A7, A12
* A1, A3, A7, A8
* A1, A11, A8, A5
* A1, A8
But fail to react in the following patterns:
* A1, A2, A3, ...
* A1, A2, A11, ....
* A2, A3, A11, ....
* ... A7, A8, A12
A series of tests on cultured cells revealed that, within the "LA" group, a donor tissue might have some antigens but not others. For example, an antiserum may react with patterns (on a given tissue):
* A1, A2, A7, A12
* A1, A3, A7, A8
* A1, A11, A8, A5
* A1, A8
But fail to react in the following patterns:
* A1, A2, A3, ...
* A1, A2, A11, ....
* A2, A3, A11, ....
* ... A7, A8, A12
Human leukocyte antigen
The human leukocyte antigen (HLA) system or complex is a complex of genes on chromosome 6 in humans which encode cell-surface proteins responsible for the regulation of the immune system. The HLA system is also known as the human version of th ...
s (HLA) began as a list of antigen
In immunology, an antigen (Ag) is a molecule or molecular structure or any foreign particulate matter or a pollen grain that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. ...
s identified as a result of transplant rejection. The antigens were initially identified by categorizing and performing massive statistical analyses on interactions between blood types.Davis, Daniel M. The Compatibility Gene. How Our Bodies Fight Disease, Attract Others, and Define Our Selves. Oxford: Oxford UP, 2014. Print. This process is based upon the principle of serotypes
A serotype or serovar is a distinct variation within a species of bacteria or virus or among immune cells of different individuals. These microorganisms, viruses, or cells are classified together based on their surface antigens, allowing the epi ...
. HLA are not typical antigens, like those found on surface of infectious agent
In biology, a pathogen ( el, πάθος, "suffering", "passion" and , "producer of") in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ ...
s. HLAs are ''allo''antigens, they vary from individual to individual as a result of genetic differences.
An organ called the thymus
The thymus is a specialized primary lymphoid organ of the immune system. Within the thymus, thymus cell lymphocytes or ''T cells'' mature. T cells are critical to the adaptive immune system, where the body adapts to specific foreign invaders. ...
is responsible for ensuring that any T-cells
A T cell is a type of lymphocyte. T cells are one of the important white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell rec ...
that attack self proteins are not allowed to live. In essence, every individual's immune system is tuned to the specific set of HLA and self proteins produced by that individual; where this goes awry is when tissues are transferred to another person. Since individuals almost always have different "banks" of HLAs, the immune system of the recipient recognizes the transplanted tissue as non-self and destroys the foreign tissue, leading to transplant rejection
Transplant rejection occurs when Organ transplant, transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between don ...
. It was through the realization of this that HLAs were discovered.
Discovery
The thought that the mammalian body must have some way of identifying introduced foreign tissues first arose duringWorld War II
World War II or the Second World War, often abbreviated as WWII or WW2, was a world war that lasted from 1939 to 1945. It involved the vast majority of the world's countries—including all of the great powers—forming two opposin ...
. It started with a plane crash in the height of the London Blitz
The Blitz was a German bombing campaign against the United Kingdom in 1940 and 1941, during the Second World War. The term was first used by the British press and originated from the term , the German word meaning 'lightning war'.
The Germa ...
. The pilot sustained severe burns requiring skin grafts; however, skin grafts were a risky business at the time, often being rejected for unknown reasons. Numerous theories were proposed and it wasn't until 1958 that the first of these "identifying" proteins was found. The first standardized naming system was established in 1968 by the WHO
Who or WHO may refer to:
* Who (pronoun), an interrogative or relative pronoun
* Who?, one of the Five Ws in journalism
* World Health Organization
Arts and entertainment Fictional characters
* Who, a creature in the Dr. Seuss book '' Horton He ...
Nomenclature Committee for Factors of the HLA System."HLA Nomenclature @ Hla.alleles.org." HLA Nomenclature @ Hla.alleles.org. Anthony Nolan Research Institute, 10 Nov. 2013. Web. 08 Dec. 2013. HLA research didn't heat up until the 1980s when a group of researchers finally elucidated the shape of the HLA-A*02 protein (just one of many specific HLA proteins). Even more recently, in 2010, the WHO committee responsible for naming all HLA proteins revised their standards for naming to introduce more clarity and specificity in the naming system.
Identification of non-self
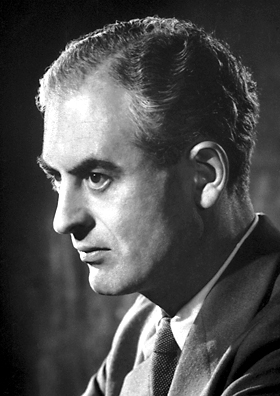
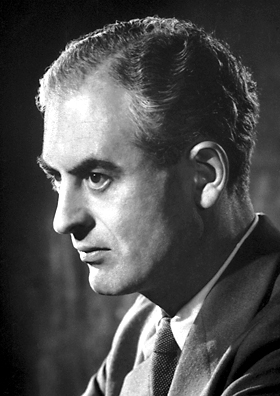
Peter Medawar
Sir Peter Brian Medawar (; 28 February 1915 – 2 October 1987) was a Brazilian-British biologist and writer, whose works on graft rejection and the discovery of acquired immune tolerance have been fundamental to the medical practice of tissue ...
was a zoologist turned clinician, who specialized in burn trauma. A plane crash near his home changed the path of his career, turning his work with burns from mere academia to a full on quest to save lives. Medawar and a Scottish surgeon, Tom Gibson, were tasked with working the Burns Unit of the Glasgow Royal Infirmary. The first insight came when the pair decided to experiment, and grafted part of a wound with the patient's skin, and another part with skin from the patient's brother. Within days the skin grafts from the brother were completely destroyed. Successive skin grafts from the brother were destroyed even faster, a fact that gave them the evidence they needed to implicate the immune system. Medawar later repeated this experiment on rabbits and 625 surgeries later validated their initial conclusions. Medawar then set out in search of the reason why rabbits rejected non-self grafts.
Medawar continued his work, this time with a team of three at the University College London during the 1950s. Medawar's coworkers were Leslie Brent, a PhD student, and Rupert Billingham, Medawar's first graduate student at Oxford several years prior. Through carefully planned experimentation, the trio showed that mice exposed to cells of unrelated mice as fetuses did ''not'' reject skin grafts from those same mice. For this discovery, Medawar and Australian scientist Macfarlane Burnet
Sir Frank Macfarlane Burnet, (3 September 1899 – 31 August 1985), usually known as Macfarlane or Mac Burnet, was an Australian virologist known for his contributions to immunology. He won a Nobel Prize in 1960 for predicting acquired immun ...
earned the 1960 Nobel Prize.
Learned self-tolerance
Burnet, independently of Medawar, came to the conclusion that the immune system must learn to tolerate any self cells, and hypothesized that this must occur during fetal development. For this, he jointly was awarded the Nobel Prize in 1960. Burnet's work continued and in 1957 along withNiels Jerne
Niels is a male given name, equivalent to Nicholas, which is common in Denmark, Belgium, Norway (formerly) and the Netherlands. The Norwegian and Swedish variant is Nils. The name is a developed short form of Nicholas or Greek Nicolaos after Saint ...
published a paper that modified and revolutionized antibody theory. "Burnet speculated that one cell makes one particular shape of antibody and that all our antibody-making immune cells together make an unimaginably vast repertoire of 10 billion antibodies, each having a slightly different shape". Thus, whenever a non-self molecule appears in the human body, one of these antibodies will have an accurate enough shape to bind to that molecule. This idea is known as clonal selection theory
In immunology, clonal selection theory explains the functions of cells of the immune system (lymphocytes) in response to specific antigens invading the body. The concept was introduced by Australian doctor Frank Macfarlane Burnet in 1957, in an ...
. At the time, many leading scientists including Linus Pauling
Linus Carl Pauling (; February 28, 1901August 19, 1994) was an American chemist, biochemist, chemical engineer, peace activist, author, and educator. He published more than 1,200 papers and books, of which about 850 dealt with scientific top ...
and James Watson
James Dewey Watson (born April 6, 1928) is an American molecular biologist, geneticist, and zoologist. In 1953, he co-authored with Francis Crick the academic paper proposing the double helix structure of the DNA molecule. Watson, Crick and ...
completely rejected the idea, but repeated experimentation intended to disprove the theory actually served to build up a large body of evidence supporting Burnet and Jerne's theory.
The biggest weakness in Burnet's theory was that he had no explanation for how the body selected for immune cells that only identified non-self. In 1961, Jacques Miller
Jacques Francis Albert Pierre Miller AC FRS FAA (born 2 April 1931) is a French-Australian research scientist. He is known for having discovered the function of the thymus and for the identification, in mammalian species of the two major subsets ...
published a paper offering an explanation. Miller was a PhD student at the Chester Beatty Research Institute in London. His discovery centered on the thymus. The thymus had long been regarded as nothing more than a repository for dead cells. Miller didn't buy this hypothesis. By removing the thymus of leukemic mice early in life, he found that the mice had a drastically weakened immune system. Taking inspiration from Medawar's skin transplant work, he performed a series of skin-graft experiments that showed that these immunocompromised mice didn't reject skin grafts from non-genetically identical mice. Miller then hypothesized that the thymus was essential in the construction and maintenance of the immune system. At this point Burnet came back into the picture, extending the hypothesis to specify that the dead cells found in the thymus are not any old immune cells, but instead the cells that are activated by self molecules. In other words, any cell that binds to and hence "recognizes" a self molecule is killed before exiting the thymus. These cells were later found to be one of the three types of Lymphocytes
A lymphocyte is a type of white blood cell (leukocyte) in the immune system of most vertebrates. Lymphocytes include natural killer cells (which function in cell-mediated, cytotoxic innate immunity), T cells (for cell-mediated, cytotoxic adap ...
, the T-cells
A T cell is a type of lymphocyte. T cells are one of the important white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell rec ...
(named for their origin, the thymus).
Identification of the first HLAs
In 1958 Jean Dausset, Jon van Rood and Rose Payne published papers in which they describedantibodies
An antibody (Ab), also known as an immunoglobulin (Ig), is a large, Y-shaped protein used by the immune system to identify and neutralize foreign objects such as pathogenic bacteria and viruses. The antibody recognizes a unique molecule of the ...
in human sera that reacted with the leucocytes
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mult ...
from many but not all other tested individuals. In particular, Jean Dausset studied sera from patients who had received multiple blood transfusion
Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but mo ...
s and found seven sera that had a very similar behavior, in that they agglutinated leucocytes from 11 of 19 tested individuals. Thus he detected an alloantigen on human leucocytes which he subsequently named MAC after the initials of three important volunteers for his experiments. Antigen MAC (later known as HLA-A2
HLA-A*02 (A*02) is a human leukocyte antigen serotype within the HLA-A serotype group. The serotype is determined by the antibody recognition of the α2 domain of the HLA-A α-chain. For A*02, the α chain is encoded by the HLA-A*02 gene and the ...
) was present in approximately 60% of French population. For his discovery, Dausset received the Nobel Prize
The Nobel Prizes ( ; sv, Nobelpriset ; no, Nobelprisen ) are five separate prizes that, according to Alfred Nobel's will of 1895, are awarded to "those who, during the preceding year, have conferred the greatest benefit to humankind." Alfr ...
in 1980.
In the follow-up research, Jon van Rood and Rose Payne continued studying sera from multiple women who had given birth multiple times and identified more leucocyte antigens. Namely, in 1962 van Rood analyzed reaction patterns of 60 sera against leucocytes from 100 donors and detected a seemingly diallelic system of two leucocyte antigens which he called 4a and 4b (later known as HLA-Bw4 and HLA-Bw6), while Payne with collaborators in 1964 detected two leucocyte antigen LA1 and LA2 (later HLA-A1 and HLA-A2
HLA-A*02 (A*02) is a human leukocyte antigen serotype within the HLA-A serotype group. The serotype is determined by the antibody recognition of the α2 domain of the HLA-A α-chain. For A*02, the α chain is encoded by the HLA-A*02 gene and the ...
), seemingly controlled by allele
An allele (, ; ; modern formation from Greek ἄλλος ''állos'', "other") is a variation of the same sequence of nucleotides at the same place on a long DNA molecule, as described in leading textbooks on genetics and evolution.
::"The chro ...
s, and suggested the existence of at least one additional antigen which would be controlled by an additional allele at the same gene locus
In genetics, a locus (plural loci) is a specific, fixed position on a chromosome where a particular gene or genetic marker is located. Each chromosome carries many genes, with each gene occupying a different position or locus; in humans, the total ...
. Also, multiple other investigators started identifying more leucocyte antigens around that time.
At this point the researchers all realized that the sheer quantity of data they were capable of obtaining was vastly greater than that of any previous study and so collaboration would be essential. The first international meeting, in 1964, highlighted the difficulties of such massive collaborative work. Different experimental methods and inconsistency in the execution of the same tests and a non-homogeneity of naming systems added together to make collaboration incredibly difficult.
World Health Organization steps in
In 1967 theWorld Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of h ...
(WHO) decided that the HLA research needed an official naming system. This in turn would aid in organization and would more easily facilitate the unification of data being collected at numerous laboratories across the world. This committee is still in existence today and vastly accelerated the rate of HLA research. The first meeting of this committee in 1968 set forth guidelines and rules that govern HLAs. First, compatibility genes were divided into two types, class I and class II. Class I molecules were identified via reactions between blood serum and cells. Class II molecules were identified by mixtures of white blood cells. Second, the compatibility genes were renamed Human Leukocyte Antigens (HLA). Despite this clarification and the ever-increasing number of identified HLAs, nobody knew how they worked.
MHC restriction
 Late in 1973 a pair of researchers in Australia, Rolf Zinkernagel and Peter Doherty made a revelatory discovery that altered the thinking of immunologists forever. The pair was doing research on viral infections in mice and noticed that T-cells that prevented viral infections in some mice wouldn't always prevent the same infection in other mice. After looking at the MHCs present in the mice, they realized that cytotoxic T-cells could only identify virus infections in cells with the right Class I compatibility gene. Traditional thinking was that the immune system identified infections directly but this discovery turned that theory on its head. Compatibility genes were essential in immune system mediated viral clearing. The pair coined the term "MHC Restriction" to describe this relationship between T-cells, specific MHC proteins, and viral detection. In 1975, in an article in the journal ''Lancet'', they introduced the idea of "altered self", meaning that viruses alter the MHC proteins and this alteration is detected by T-cells. For their work they won the 1996 Nobel Prize. It took the work of many others to determine how T-cells made this identification.
Late in 1973 a pair of researchers in Australia, Rolf Zinkernagel and Peter Doherty made a revelatory discovery that altered the thinking of immunologists forever. The pair was doing research on viral infections in mice and noticed that T-cells that prevented viral infections in some mice wouldn't always prevent the same infection in other mice. After looking at the MHCs present in the mice, they realized that cytotoxic T-cells could only identify virus infections in cells with the right Class I compatibility gene. Traditional thinking was that the immune system identified infections directly but this discovery turned that theory on its head. Compatibility genes were essential in immune system mediated viral clearing. The pair coined the term "MHC Restriction" to describe this relationship between T-cells, specific MHC proteins, and viral detection. In 1975, in an article in the journal ''Lancet'', they introduced the idea of "altered self", meaning that viruses alter the MHC proteins and this alteration is detected by T-cells. For their work they won the 1996 Nobel Prize. It took the work of many others to determine how T-cells made this identification.
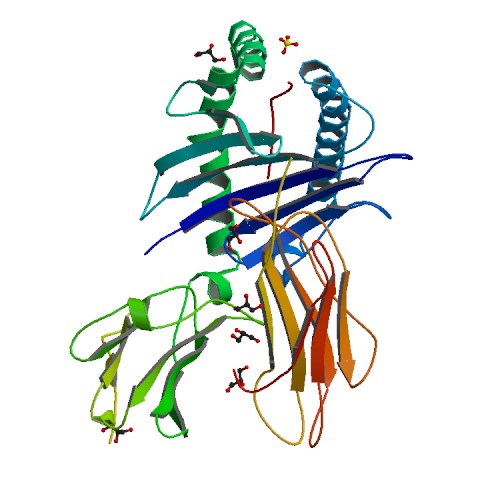
Discovering the protein shape
Nearly all important molecules in the body areproteins
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, respo ...
. Proteins work by each having a specific sequence of amino acids
Amino acids are organic compounds that contain both amino and carboxylic acid functional groups. Although hundreds of amino acids exist in nature, by far the most important are the alpha-amino acids, which comprise proteins. Only 22 alpha am ...
and a specific shape. Determining the order of amino acids is relatively simple. Finding the shape requires the use of x-ray crystallography
X-ray crystallography is the experimental science determining the atomic and molecular structure of a crystal, in which the crystalline structure causes a beam of incident X-rays to diffract into many specific directions. By measuring the angles ...
and is anything but easy.Alberts, Bruce. Essential Cell Biology. New York: Garland Science, 2009. Print. It took a team of three researchers at Harvard, Don Wiley, Jack Strominger, and Pamela Bjorkman
Pamela Jane Bjorkman NAS, AAAS (also spelled Pamela J. Björkman; born 1956, Portland, Oregon) is an American biochemist and molecular biologist. She is the David Baltimore Professor of Biology and Biological Engineering at the California Instit ...
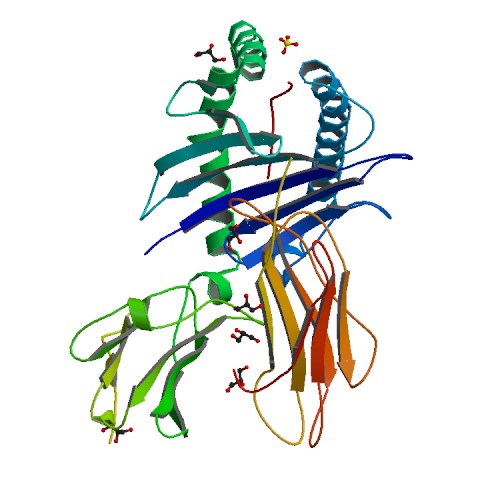
, eight years to ferret out the structure of the HLA protein. They worked specifically with HLA-A*02. Bjorkman did the majority of the leg work and in the seven years managed to piece together the structure of 90% of the protein. That last 10% was elusive though. It took another year of work to finally unveil the complete structure of HLA-A*02. They completed their work in the spring of 1987, discovering that the final 10% made a "cup" (of sorts) located on top of the molecule. It was the perfect size to hold peptides. Other researchers had previously determined that T-Cells can recognize cells infected with a virus, cells injected with a single protein from a virus, and even cells injected with pieces of protein from a virus. The discovery of the HLA protein structure made it starkly clear that the HLA proteins hold viral peptides in their binding groove. But the research team from Harvard wasn't done. They also observed that there was clearly a peptide in the binding groove of the HLA molecules they used to determine the shape. However, the cells they had extracted the protein from were definitely not infected by any disease causing viruses. The conclusion they made and the conclusion that has stuck to this day, is that HLA molecules can bind both self, and non-self peptides.
Nomenclature
Current HLA naming system
The most recent HLA naming system was developed in 2010 by the WHO Committee for Factors of the HLA System. There are two types of MHCs, Class I and Class II. Both are named using the same system. Currently there are 7,678 Class Ialleles
An allele (, ; ; modern formation from Greek ἄλλος ''állos'', "other") is a variation of the same sequence of nucleotides at the same place on a long DNA molecule, as described in leading textbooks on genetics and evolution.
::"The chro ...
and 2,268 Class II alleles.
HLA Naming can be quite confusing at first. All alleles start with "HLA", signifying they are part of the human MHC genes. The next portion (HLA-A or HLA-B) identifies which gene the allele is a modification of. The first two numbers (HLA-A*02) signifies what antigen type that particular allele is, which typically signifies the serological antigen present. In other words, HLAs with the same antigen type (HLA-A*02:101 and HLA-A*02:102) will not react with each other in serological tests. The next set of digits (HLA-A*02:101) indicates what protein the allele codes for, and these are numbered sequentially in the order they are discovered. Any HLA that has a different number here produces a different protein (AKA has a nucleotide change that replaces an amino acid with another). The third set of numbers (HLA-A*02:101:01) indicates an allele variant that has a different DNA sequence but produces the same protein as the normal gene. The final set of numbers (HLA-A*02:101:01:01) is used to designate a single or multiple nucleotide polymorphism in a non-coding region of the gene. The final aspect of HLA naming is a letter (HLA-A*02:101:01:01L). There are six letters, each with a different meaning.
Establishing the system
A person can have 2 antigen proteins per genetic-locus (one gene from each parent). When first discovered, identified antigens were clustered, creating groups in which no more than two antigens per cluster were found in a given person. Serotype group "A" consisted HL-A1, A2, A3, A9, A10, A11. Another cluster, "B", contained A7, A8, A12, A13, A14, A15. HL-A4 antigen was found to occur on lymphoid cells. Since the "HL-Antigens" no longer belonged to a single group, a new naming system was needed. In 1968 the WHO Nomenclature Committee for Factors of the HLA System first met. They established a system that divided the HLAs into HLA-A and HLA-B, A and B corresponding to a group of reactive serotypes. For example, "HL-A2" becameHLA-A2
HLA-A*02 (A*02) is a human leukocyte antigen serotype within the HLA-A serotype group. The serotype is determined by the antibody recognition of the α2 domain of the HLA-A α-chain. For A*02, the α chain is encoded by the HLA-A*02 gene and the ...
, "HL-A7" became HLA-B7 and "HL-A8" became HLA-B8
HLA-B8 (B8) is an HLA- B serotype
A serotype or serovar is a distinct variation within a species of bacteria or virus or among immune cells of different individuals. These microorganisms, viruses, or cells are classified together based on t ...
.
In this arrangement there were cells that were 'blank' or had new specificities, these new antigens were called "W" antigens, and as they were reassigned to new groups, for example "A" serotypes, they became Aw or Bw antigens. It was found that some antigens that behaved like A and B antigens but could be excluded based on '2-type max' exclusion. Thus a new group, "C" was created. Classification of C antigens is still ongoing, and they have retained the name Cw as many serotypes have not been developed.
The classification of the "A4" antigens was complicated. The "A4" subset evolved to become D-region antigens, which was a large cluster of genes that encoded MHC class II. Several renamings occurred. The D-region has 8 major coding loci that combine to form 3 different protein groups; DP, DQ, and DR. DRw antigens were the first to be split, a process made easy by the virtue of having an invariant alpha chain, but complicated by 4 beta chain loci (DRB1, DRB3, DRB4, and DRB5). Serotypes to DQ reacted with alpha and beta chains, or both of certain isoforms. The proper classification was greatly aided by gene sequencing and PCR. Classification and description of DP antigens is ongoing.
Genetics
Genetic complexity typifies HLA
The naming ofhuman leukocyte antigens
The human leukocyte antigen (HLA) system or complex is a complex of genes on chromosome 6 in humans which encode cell-surface proteins responsible for the regulation of the immune system. The HLA system is also known as the human version of th ...
HLA "antigen
In immunology, an antigen (Ag) is a molecule or molecular structure or any foreign particulate matter or a pollen grain that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. ...
s" is deeply rooted in the discovery history of their serotype
A serotype or serovar is a distinct variation within a species of bacteria or virus or among immune cells of different individuals. These microorganisms, viruses, or cells are classified together based on their surface antigens, allowing the epi ...
s and allele
An allele (, ; ; modern formation from Greek ἄλλος ''állos'', "other") is a variation of the same sequence of nucleotides at the same place on a long DNA molecule, as described in leading textbooks on genetics and evolution.
::"The chro ...
s. There is no doubt that HLA terminology can be bewildering, this terminology is a consequence of the complex genetics as well as the way these antigens were characterized.
Historical perspective is important to an understanding of how the HLA were systematized. In organ transplant the goal was to explain graft rejection for recipients, and of course, to prevent future rejection. From this perspective, the cause of rejections were found to be "antigens". In the same way bacterial antigens can cause inflammatory response, HLA antigens from the donor of the organ caused an inflammatory response when placed in a recipient. This is called allograft llo = different, graft(medical) = transplantrejection.
To explain rejection in a nutshell, certain immune system components are highly variable, the agents are called the Major histocompatibility (MHC) antigens. MHC antigens cause rejection of improperly matched organ transplants. The variability stems from genetics. From the perspective of human evolution, why are antigens of the MHC so variable when many other human proteins lack variability? The cause of host-versus-graft-disease may actually stem from the functions of the system.
The use of the word alloantigen actually masks the fact that HLA are infrequently autoantigens in the donor, and therefore their function is not as antigens, but something else. But the naming of these antigens is not borne out of function but the need to match organ donors with recipients.
Transplantation and transplant rejection
organ transplantation
Organ transplantation is a medical procedure in which an organ (anatomy), organ is removed from one body and placed in the body of a recipient, to replace a damaged or missing organ. The donor and recipient may be at the same location, or organ ...
. Knowing little about ''compatibility factors'', they attempted transplantation between humans and between non-humans and humans. Immunosuppressive drugs
Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are medication, drugs that inhibit or prevent activity of the immune system.
Classification
Immunosuppressive drugs can be cla ...
worked for a time, but transplanted organs would either always fail or the patients would die from infections. Patients received skin, white blood cell
White blood cells, also called leukocytes or leucocytes, are the cell (biology), cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and de ...
or kidney donations from other donors (called allograft
Allotransplant (''allo-'' meaning "other" in Greek) is the transplantation of cells, tissues, or organs to a recipient from a genetically non-identical donor of the same species. The transplant is called an allograft, allogeneic transplant, o ...
s, meaning 'of different genetics' grafts). If these allograft
Allotransplant (''allo-'' meaning "other" in Greek) is the transplantation of cells, tissues, or organs to a recipient from a genetically non-identical donor of the same species. The transplant is called an allograft, allogeneic transplant, o ...
s were rejected, it was found that the 'rejection' response was accompanied by an antibody
An antibody (Ab), also known as an immunoglobulin (Ig), is a large, Y-shaped protein used by the immune system to identify and neutralize foreign objects such as pathogenic bacteria and viruses. The antibody recognizes a unique molecule of the ...
mediated agglutination
In linguistics, agglutination is a morphological process in which words are formed by stringing together morphemes, each of which corresponds to a single syntactic feature. Languages that use agglutination widely are called agglutinative lang ...
of red blood cells (See figure). The search for these cell surface antigens began. There are several processes by which antibodies can reduce function:
* Acute rejection - Antibodies could attract lymphocytes and cause them to lyse cells via the immune system's classical complement pathway
The classical complement pathway is one of three pathways which activate the complement system, which is part of the immune system. The classical complement pathway is initiated by antigen-antibody complexes with the antibody isotypes IgG and IgM ...
* Antibodies could bind to and alter function (e.g., flow of a fluid, or prevention of binding of ligands to receptors)
* Cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrin ...
responses that cause systemic responses.
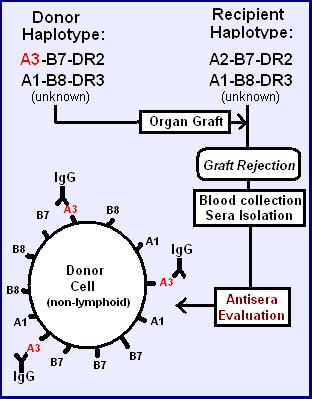
=Different antigens can be identified
= In the accompanying figure, two similarhaplotype
A haplotype ( haploid genotype) is a group of alleles in an organism that are inherited together from a single parent.
Many organisms contain genetic material ( DNA) which is inherited from two parents. Normally these organisms have their DNA or ...
s (unknown to early clinicians) are identical, except for the one ''antigen'' in the top haplotype. The transplant may not be rejected, but if rejection does occur that allotypic protein, the allo''antigen
In immunology, an antigen (Ag) is a molecule or molecular structure or any foreign particulate matter or a pollen grain that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. ...
'', in the donor tissue may have induced the dominant allo-reactive antibody in the recipient.
=Assaying antiserum
= Hemagglutination assay. In generating an immune response to an antigen, the
Hemagglutination assay. In generating an immune response to an antigen, the B-cell
B cells, also known as B lymphocytes, are a type of white blood cell of the lymphocyte subtype. They function in the humoral immunity component of the adaptive immune system. B cells produce antibody molecules which may be either secreted o ...
s go through a process of maturation, from surface IgM production, to serum IgM production, to maturation into a plasma cell
Plasma cells, also called plasma B cells or effector B cells, are white blood cells that originate in the lymphoid organs as B lymphocytes and secrete large quantities of proteins called antibodies in response to being presented specific substan ...
producing IgG. Graft recipients who generate an immune response have both IgM and IgG. The IgM can be used directly in hemagglutination
Hemagglutination, or haemagglutination, is a specific form of agglutination that involves red blood cells (RBCs). It has two common uses in the laboratory: blood typing and the quantification of virus dilutions in a haemagglutination assay.
Blood ...
assays, depicted on the right. IgM has 10 antigen binding regions per molecule, allowing cross-linking of cells. An antiserum specific for HLA-A3 will then agglutinate HLA-A3 bearing red blood cells if the concentration of IgM in the antiserum is sufficiently high. Alternatively, a second antibody to the invariable (Fc) region of the IgG can be used to cross-link antibodies on different cells, causing agglutination.
Complement fixation assay. The complement fixation test
The complement fixation test is an immunological medical test that can be used to detect the presence of either specific antibody or specific antigen in a patient's serum, based on whether complement fixation occurs. It was widely used to diagnos ...
was modified to assay Antiserum mediated RBC lysis.
Chromium release assay. This assay measures the release of (biological) radioactive chromium from cells as a result of killer cell activity. These cells are attracted to class I antigens that either carry foreign antigens, or are foreign to the immune system.
=The role of haplotypes in identifying antigens
= Each person has two HLAhaplotype
A haplotype ( haploid genotype) is a group of alleles in an organism that are inherited together from a single parent.
Many organisms contain genetic material ( DNA) which is inherited from two parents. Normally these organisms have their DNA or ...
s, a cassette of genes passed on from each parent. The haplotype frequencies in Europeans are in strong linkage disequilibrium
In population genetics, linkage disequilibrium (LD) is the non-random association of alleles at different loci in a given population. Loci are said to be in linkage disequilibrium when the frequency of association of their different alleles is h ...
. This means there are much higher frequencies of certain haplotypes relative to the expectation based on random sorting of gene-alleles. This aided the discovery of HLA antigens, but was unknown to the pioneering researchers.
In the tables a fortuitous transplant between two unrelated individual has resulted in an antiserum to single alloantigen. By discovering these close-but-non-identical matches, the process with somewhat related haplotypes surface antigens were identified for HLA A, and in the table below, HLA B at the time however these were all grouped together as HL-Antigens. On the left the "B" and "cw" antigens are matched (B and C are close together so if B matches then C likely also matches), but A antigens are not matched. The antisera that is produced by the recipient is most likely to be A3, but if the direction of transplant is reversed A2 is the likely alloantigen. Two of the first three alloantigens are thus readily easy to detect because of the similarity and frequency of the A2-B7 and A3-B7 haplotypes (see example 1).
In these instances, the A1/A2, A2/A3, A1/A3 are matched, decreasing the probability of a rejection because many are linked to a given haplotype. Occasionally the 'recombinant' A1-Cw7-B7(rare), B7 becomes the alloantigen in a recipient with A1-Cw7-B8(common).
This linkage disequilibrium in Europeans explains why A1, A2, A3, "A7" 7 and "A8" 8were identified, first. It would have taken substantially longer to identify other alleles because frequencies were lower, and haplotypes that migrated into the European population had undergone equilibration or were from multiple sources.
This is the genetic background against which scientists tried to uncover and understand the histocompatibility antigens.
A list of antigens created
In the late 1960s, scientist began reacting sera from patients with rejecting transplants to donor or 'third party' tissues. Their sera (the liquid part of the blood when blood clots) was sensitized to the cells from donors - it was ''alloreactive''. By testing different anti-sera from recipients they were able to uncover some with unique reactivities. As a result, scientists were able to identify a few antigens. At first the first antigens were called the Hu-1 antigens and tentatively tagged as gene products of the Human equivalent of the mouse histocompatibility locus (H2). In 1968, it was discovered that matching these antigens between kidney donor and recipient improved the likelihood of kidney survival in the recipient. The antigen list still exists, although it has been reorganized to fit what we have since learned about genetics, refined, and greatly expanded.Lymphocyte bearing antigens recognized
autoantigen
In immunology, autoimmunity is the system of immune responses of an organism against its own healthy cells, tissues and other normal body constituents. Any disease resulting from this type of immune response is termed an "autoimmune disease". P ...
, in which a person develops antibodies to one or more of their own proteins. This also suggested the donor and recipient have a different genetic makeup for these antigens. The "LA" group thereafter was composed of HL-A1, A2, A3, A5, A6, A7, A8, A9, A10, A11, A12, A13, A14 and A15 until further divisions and renaming were necessary. Some of the antigens above, for example HL-A1, are similar to HLA-A1, as they are the same serotype. Some of the above, like A5, are not mentioned within the last few years, as they have been renamed.
During these early studies it became known that there were associations with many autoimmune diseases. And the HLA A1-B8 haplotype
HLA A1-B8 (Also:''HL A1,8''; ''HL A1,A8''; ''HLA A1-Cw7-B8''; ''HLA A*01-B*08'', ''HLA A*0101-B*0801'', ''HLA A*0101-Cw*0701-B*0801''; ''HLA A*01:01-C*07:01-B*08:01'') is a multigene haplotype that covers the MHC Class I region of the human major ...
is linked to a very long piece of conserved chromosome 6 variant called AH8.1 haplotype. In these studies ''HL-A1,8'' were frequently found co-linked to disease. This linkage is not necessarily a function of either gene, but a consequence of the way AH8.1 evolved.
Subclassification of lymphoid antigens
The HLA serotype series
=Series "A"
= If 2 members of the series (A1, 2, 3, 9, 10, 11) were typed, a reaction with a third member of the series to the donor was not observed. This 'exclusivity' identified series "A".Bach ML, Bach FH. (1970) ''The genetics of histocompatibility''. ''Hosp. Practice'' 5(8): 33-44 One might notice the similarities of this numeric series with the HLA-A series, as series "A" antigens are the first six members ofHLA-A
HLA-A is a group of human leukocyte antigens (HLA) that are encoded by the HLA-A locus, which is located at human chromosome 6p21.3. HLA is a major histocompatibility complex (MHC) antigen specific to humans. HLA-A is one of three major types of ...
. Inadvertently, the scientist had discovered an antibody set that recognized only gene product
A gene product is the biochemical material, either RNA or protein, resulting from expression of a gene. A measurement of the amount of gene product is sometimes used to infer how active a gene is. Abnormal amounts of gene product can be correlated ...
s from one locus, HLA-A gene
HLA-A is a group of human leukocyte antigens (HLA) that are encoded by the HLA-A locus (genetics), locus, which is located at human chromosome 6p21.3. HLA is a major histocompatibility complex (MHC) antigen specific to humans. HLA-A is one of thr ...
the "antigens" being the gene products. The implication is that an alloreactive anti-sera can be a tool for genetic identification.
=Series "B"
= Not long after the series A antigens were separated from the (rapidly expanding) list of antigens, it was determined another group also could be separated along the same ''logical'' lines. This group included HL-A5, A7, A8, A12. This became the series "B". Note the similarity of Series "B" to the first few members HLA-B serotypes. The names of these antigens were necessarily changed to fit the new putative series they were assigned to. From HL-A# to HLA-B#. The problem was that the literature was using "A7" and would soon be using "B7" as shorthand for HLA-B7.=Pseudo-series "w"
= Since it was now certain, by the early 1970s, that the "antigens" were encoded by different series, implicit loci, numeric lists became somewhat cumbersome. Many groups were discovering antigens. In these instances an antigen was assigned a temporary name, like "RoMa2" and after discussion, the next open numeric slot could be assigned, but not to an "A" or "B" series until proper testing had been done. To work around this problem a 'workshop' number "w#" was often assigned while testing continued to determine which series the antigen belonged to.=Series "C"
= Before too long, a series "C" was uncovered. Series C has proved difficult to serotype, and the alleles in the series still carry the "w" tag signifying that status; in addition, it reminds us that Series C were not assigned names the same way as Series A and B, it has its own numeric list Cw1, Cw2, Cw3.Serotype group expansion and refinement
By the mid-1970s, genetic research was finally beginning to make sense of the simple list of antigens, a new series "C" had been discovered and, in turn genetic research had determined the order of HLA-A, C, B and D encoding loci on the human 6p. With new series came new antigens; Cw1 and 2 were quickly populated, although Cw typing lagged. Almost half of the antigens could not be resolved by serotyping in the early 90s. Currently genetics defines 18 groups. At this point, Dw was still being used to identify DR, DQ, and DP antigens. The ability to identify new antigens far exceeded the ability to characterize those new antigens. As technology for transplantation was deployed around the world, it became clear that these antigens were far from a complete set, and in fact hardly useful in some areas of the world (e.g., Africa, or those descended from Africans). Some serotyping antibodies proved to be poor, with broad specificities, and new serotypes were found that identified a smaller set of antigens more precisely. These broad antigen groups, like A9 and B5, were subdivided into "split" antigen groups, A23 & A24 and B51 & B52, respectively. As the HL-A serotyping developed, so did identification of new antigens.Genetic identification
In the early 1980s, it was discovered that a restriction fragment segregates with individuals who bear theHLA-B8
HLA-B8 (B8) is an HLA- B serotype
A serotype or serovar is a distinct variation within a species of bacteria or virus or among immune cells of different individuals. These microorganisms, viruses, or cells are classified together based on t ...
serotype. By 1990, it was discovered that a single amino acid sequence difference between HLA-B44 (B*4401 versus B*4402) could result in allograft rejection. This revelation appeared to make serotyping based matching strategies problematic if many such differences existed. In the case of B44, the antigen had already been split from the B12 broad antigen group. In 1983, the cDNA sequences of HLA-A3
HLA-A3 (A3) is a human leukocyte antigen '' serotype'' within HLA-A serotype group. The serotype is determined by the antibody recognition of α3 subset of HLA-A α-chains. For A3, the alpha, "A", chain are encoded by the HLA-A allele group and ...
and Cw3 All three sequences compared well with mouse MHC class I antigens. The Western European HLA-B7 antigen had been sequenced (although the first sequence had errors and was replaced). In short order, many HLA class I alleles were sequenced
including 2 Cw1 alleles.
By 1990, the full complexity of the HLA class I antigens was beginning to be understood. At the time new serotypes were being determined, the problem with multiple alleles for each serotype was becoming apparent by nucleotide sequencing. RFLP analysis helped determine new alleles, but sequencing was more thorough. Throughout the 1990s, PCR kits, called SSP-PCR kits were developed that allowed, at least under optimal conditions, the purification of DNA, PCR and Agarose Gel identification of alleles within an 8-hour day. Alleles that could not be clearly identified by serotype and PCR could be sequenced, allowing for the refinement of new PCR kits.
Serotypes like B*4401, B*4402, B*4403, each abundant within those with B44 serotypes could be determined with unambiguous accuracy. The molecular genetics has advanced HLA technology markedly over serotyping technology, but serotyping still survives. Serotyping had identified the most similar antigens that now form the HLA subgroups. Serotyping can reveal whether an antigen coded by the relevant HLA gene is expressed. An HLA allele coding non-expressed gene is termed "Null Allele", for example: HLA-B*15:01:01:02N. The expression level can also detected by serotyping, an HLA gene coding for antigens which has low protein expression on the cell surface is termed "Low Expresser", for example: HLA-A*02:01:01:02L.
References
{{DEFAULTSORT:History And Naming Of Human Leukocyte Antigens Scientific terminology