Heart failure (HF), also known as congestive heart failure (CHF), is a
syndrome, a group of
signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include
shortness of breath
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing di ...
,
excessive fatigue, and
leg swelling. The shortness of breath may occur with
exertion or while
lying down
"Lying Down" is a song by Canadian singer Celine Dion from her twelfth English-language studio album, ''Courage'' (2019). It was written by David Guetta, Giorgio Tuinfort and Sia, and produced by Guetta and Tuinfort. "Lying Down" was released as ...
, and
may wake people up during the night.
[ Other conditions that may have symptoms similar to heart failure include ]obesity
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's ...
, kidney failure, liver disease, anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, ...
, and thyroid disease.coronary artery disease
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves Ischemia, the reduction of blood flow to the myocardium, heart muscle due to build-up o ...
, heart attack, high blood pressure
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. Long-term high b ...
, atrial fibrillation, valvular heart disease, excessive alcohol consumption, infection
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable d ...
, and cardiomyopathy
Cardiomyopathy is a group of diseases that affect the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. ...
.[ There are different types of heart failure: ]right-sided heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, an ...
, which affects the right heart, left-sided heart failure, which affects the left heart, and biventricular heart failure, which affects both sides of the heart.ejection fraction
An ejection fraction (EF) is the volumetric fraction (mathematics), fraction (or portion of the total) of fluid (usually blood) ejected from a chamber (usually the heart) with each contraction (or cardiac cycle, heartbeat). It can refer to the card ...
or with a preserved ejection fraction.[ Heart failure is not the same as ]cardiac arrest
Cardiac arrest is when the heart suddenly and unexpectedly stops beating. It is a medical emergency that, without immediate medical intervention, will result in sudden cardiac death within minutes. Cardiopulmonary resuscitation (CPR) and possib ...
, in which blood flow stops completely due to the failure of the heart to pump effectively.
Diagnosis is based on symptoms, physical findings, and echocardiography. Blood test
A blood test is a laboratory analysis performed on a blood sample that is usually extracted from a vein in the arm using a hypodermic needle, or via fingerprick. Multiple tests for specific blood components, such as a glucose test or a ch ...
s, and a chest x-ray
A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in me ...
may be useful to determine the underlying cause.[
Treatment depends on severity and case.][ For people with chronic, stable, mild heart failure, treatment usually consists of lifestyle changes, such as not smoking, ]physical exercise
Exercise is a body activity that enhances or maintains physical fitness and overall health and wellness.
It is performed for various reasons, to aid growth and improve strength, develop muscles and the cardiovascular system, hone athletic ...
, and dietary changes, as well as medications.[ Diuretics may also be prescribed to prevent fluid retention and the resulting shortness of breath.][ Depending on the case, an implanted device such as a pacemaker or implantable cardiac defibrillator may sometimes be recommended.][ In some moderate or more severe cases, ]cardiac resynchronization therapy
Cardiac resynchronisation therapy (CRT or CRT-P) is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ve ...
(CRT)[ Also at ] Rates are predicted to increase.[ The risk of death in the first year after diagnosis is about 35%, while the risk of death in the second year is less than 10% in those still alive.][ The risk of death is comparable to that of some cancers.][ In the United Kingdom, the disease is the reason for 5% of emergency hospital admissions.][ Heart failure has been known since ancient times, it is mentioned in the Ebers Papyrus around 1550 BCE.]
Definition
Heart failure is not a disease but a syndrome - a combination of signs and symptoms caused by the failure of the heart to pump blood to support the circulatory system
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, tha ...
at rest or during activity. It develops when the heart fails to properly fill with blood during diastole, resulting in a decrease in intracardiac pressures or in ejection during systole, reducing cardiac output to the rest of the body. The filling failure and high intracardiac pressure can lead to fluid accumulation in the veins and tissue. This manifests as water retention and swelling due to fluid accumulation ( edema) called congestion. Impaired ejection can lead to inadequate blood flow to the body tissues, resulting in ischemia.
Signs and symptoms
 Congestive heart failure is a pathophysiological condition in which the heart's output is insufficient to meet the needs of the body and lungs.
Congestive heart failure is a pathophysiological condition in which the heart's output is insufficient to meet the needs of the body and lungs.
Left-sided failure
The left side of the heart takes oxygen-rich blood from the lungs and pumps it to the rest of the circulatory system
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, tha ...
in the body, except for the pulmonary circulation). Failure of the left side of the heart causes blood to back up into the lungs, causing breathing difficulties and fatigue due to an insufficient supply of oxygenated blood. Common respiratory signs include increased respitatory rate and labored breathing (nonspecific signs of shortness of breath). Rales or crackles heard initially in the lung bases and when severe in all lung fields
A respiratory examination, or lung examination, is performed as part of a physical examination, in response to respiratory symptoms such as shortness of breath, cough, or chest pain, and is often carried out with a cardiac examination.
The four ...
indicate the development of pulmonary edema (fluid in the alveoli). Cyanosis
Cyanosis is the change of body tissue color to a bluish-purple hue as a result of having decreased amounts of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Body tissues that show cyanosis are usually in locations ...
, indicates deficiency of oxygen in the blood, is a late sign of extremely severe pulmonary edema.
Other signs of left ventricular failure include a laterally displaced apex beat (which occurs when the heart is enlarged) and a gallop rhythm
A gallop rhythm refers to a (usually abnormal) rhythm of the heart on auscultation. It includes three or four sounds, thus resembling the sounds of a gallop.
The normal heart rhythm contains two audible heart sounds called S1 and S2 that give ...
(additional heart sounds), which may be heard as a sign of increased blood flow or increased intracardiac pressure. Heart murmurs may indicate the presence of valvular heart disease, either as a cause (e.g., aortic stenosis) or as a consequence (e.g., mitral regurgitation) of heart failure.
''Reverse'' insufficiency of the left ventricle causes congestion in the blood vessels of the lungs, so that symptoms are predominantly respiratory. Reverse insufficiency can be divided into the failure of the left atrium, the left ventricle, or both within the left circuit. Patients will experience shortness of breath ( dyspnea) on exertion and, in severe cases, dyspnea at rest. Increasing breathlessness while lying down, called orthopnea, also occurs. It can be measured by the number of pillows required to lie comfortably, with extreme cases of orthopnea forcing the patient to sleep sitting up. Another symptom of heart failure is paroxysmal nocturnal dyspnea: a sudden nocturnal attack of severe shortness of breath, usually occurring several hours after falling asleep. There may be " cardiac asthma" or wheezing. Impaired left ventricular ''forward'' function can lead to symptoms of poor systemic perfusion such as dizziness, confusion, and cool extremities at rest.
Right-sided failure
 Right-sided heart failure is often caused by pulmonary heart disease (cor pulmonale), which is typically caused by issues with pulmonary circulation such as pulmonary hypertension or pulmonic stenosis. Physical examination may reveal pitting peripheral edema, ascites, liver enlargement, and spleen enlargement. Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by testing hepatojugular reflux. If the right ventricular pressure is increased, a parasternal heave which causes the compensatory increase in contraction strength may be present.
Right-sided heart failure is often caused by pulmonary heart disease (cor pulmonale), which is typically caused by issues with pulmonary circulation such as pulmonary hypertension or pulmonic stenosis. Physical examination may reveal pitting peripheral edema, ascites, liver enlargement, and spleen enlargement. Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by testing hepatojugular reflux. If the right ventricular pressure is increased, a parasternal heave which causes the compensatory increase in contraction strength may be present.anasarca
Anasarca is a severe and generalized form of edema, with subcutaneous tissue swelling throughout the body. Unlike typical edema, which almost everyone will experience at some time and can be relatively benign, anasarca is a pathological process r ...
) and usually affects the dependent parts of the body first, causing foot and ankle swelling in people who are standing up and sacral edema in people who are predominantly lying down. Nocturia (frequent night-time urination) may occur when fluid from the legs is returned to the bloodstream while lying down at night. In progressively severe cases, ascites (fluid accumulation in the abdominal cavity causing swelling) and liver enlargement may develop. Significant liver congestion may result in impaired liver function ( congestive hepatopathy), jaundice, and coagulopathy (problems of decreased or increased blood clotting).
Biventricular failure
Dullness of the lung fields when percussed and reduced breath sounds at the base of the lungs may suggest the development of a pleural effusion (fluid collection between the lung and the chest wall). Though it can occur in isolated left- or right-sided heart failure, it is more common in biventricular failure because pleural veins drain into both the systemic and pulmonary venous systems. When unilateral, effusions are often right-sided.
If a person with a failure of one ventricle lives long enough, it will tend to progress to failure of both ventricles. For example, left ventricular failure allows pulmonary edema and pulmonary hypertension to occur, which increase stress on the right ventricle. Though still harmful, right ventricular failure is not as deleterious to the left side.
Causes
Since heart failure is a syndrome and not a disease, establishing the underlying cause is vital to diagnosis and treatment.coronary artery disease
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves Ischemia, the reduction of blood flow to the myocardium, heart muscle due to build-up o ...
, including a previous myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which ...
(heart attack), high blood pressure
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. Long-term high b ...
, atrial fibrillation, valvular heart disease, excess alcohol use, infection
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable d ...
, and cardiomyopathy
Cardiomyopathy is a group of diseases that affect the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. ...
of an unknown cause.HIV
The human immunodeficiency viruses (HIV) are two species of '' Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immu ...
), chemotherapeutic agents such as daunorubicin, cyclophosphamide, trastuzumab and substance use disorder
Substance use disorder (SUD) is the persistent use of drugs (including alcohol) despite substantial harm and adverse consequences as a result of their use. Substance use disorders are characterized by an array of mental/emotional, physical, and b ...
s of substances such as alcohol, cocaine, and methamphetamine
Methamphetamine (contracted from ) is a potent central nervous system (CNS) stimulant that is mainly used as a recreational drug and less commonly as a second-line treatment for attention deficit hyperactivity disorder and obesity. Meth ...
. An uncommon cause is exposure to certain toxins such as lead
Lead is a chemical element with the Symbol (chemistry), symbol Pb (from the Latin ) and atomic number 82. It is a heavy metals, heavy metal that is density, denser than most common materials. Lead is Mohs scale of mineral hardness#Intermediate ...
and cobalt
Cobalt is a chemical element with the symbol Co and atomic number 27. As with nickel, cobalt is found in the Earth's crust only in a chemically combined form, save for small deposits found in alloys of natural meteoric iron. The free element, ...
. Additionally, infiltrative disorders such as amyloidosis and connective tissue diseases such as systemic lupus erythematosus
Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Comm ...
have similar consequences. Obstructive sleep apnea
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episo ...
(a condition of sleep wherein disordered breathing overlaps with obesity, hypertension, and/or diabetes) is regarded as an independent cause of heart failure. Recent reports from clinical trial
Clinical trials are prospective biomedical or behavioral research studies on human subject research, human participants designed to answer specific questions about biomedical or behavioral interventions, including new treatments (such as novel v ...
s have also linked variation in blood pressure to heart failure and cardiac changes that may give rise to heart failure.
High-output heart failure
High-output heart failure happens when the amount of blood pumped out is more than typical and the heart is unable to keep up.anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, ...
, beriberi (vitamin B1/ thiamine deficiency), hyperthyroidism
Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormones by the thyroid gland. Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidis ...
, cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage causes tissue repai ...
, Paget's disease, multiple myeloma, arteriovenous fistulae, or arteriovenous malformations.
Acute decompensation
 Chronic stable heart failure may easily decompensate. This most commonly results from a concurrent illness (such as
Chronic stable heart failure may easily decompensate. This most commonly results from a concurrent illness (such as myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which ...
(a heart attack) or pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severi ...
), abnormal heart rhythms, uncontrolled hypertension, or a person's failure to maintain a fluid restriction, diet, or medication.
Medications
A number of medications may cause or worsen the disease. This includes NSAIDs, COX-2 inhibitors, a number of anesthetic agents such as ketamine, thiazolidinediones, some cancer medications, several antiarrhythmic medications, pregabalin, alpha-2 adrenergic receptor agonists, minoxidil, itraconazole, cilostazol, anagrelide, stimulant
Stimulants (also often referred to as psychostimulants or colloquially as uppers) is an overarching term that covers many drugs including those that increase activity of the central nervous system and the body, drugs that are pleasurable and inv ...
s (e.g., methylphenidate
Methylphenidate, sold under the brand names Ritalin and Concerta among others, is the most widely prescribed central nervous system (CNS) stimulant medication used to treat attention deficit hyperactivity disorder (ADHD) and, to a lesser extent ...
), tricyclic antidepressant
Tricyclic antidepressants (TCAs) are a class of medications that are used primarily as antidepressants, which is important for the management of depression. They are second-line drugs next to SSRIs. TCAs were discovered in the early 1950s and we ...
s, lithium
Lithium (from el, λίθος, lithos, lit=stone) is a chemical element with the symbol Li and atomic number 3. It is a soft, silvery-white alkali metal. Under standard conditions, it is the least dense metal and the least dense solid ...
, antipsychotic
Antipsychotics, also known as neuroleptics, are a class of psychotropic medication primarily used to manage psychosis (including delusions, hallucinations, paranoia or disordered thought), principally in schizophrenia but also in a range o ...
s, dopamine agonists, TNF inhibitors, calcium channel blockers (especially verapamil
Verapamil, sold under various trade names, is a calcium channel blocker medication used for the treatment of high blood pressure, angina (chest pain from not enough blood flow to the heart), and supraventricular tachycardia. It may also be ...
and diltiazem
Diltiazem, sold under the brand name Cardizem among others, is a calcium channel blocker medication used to treat high blood pressure, angina, and certain heart arrhythmias. It may also be used in hyperthyroidism if beta blockers cannot be ...
prostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are der ...
s, NSAIDs may exacerbate heart failure through several mechanisms, including promotion of fluid retention, increasing blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressur ...
, and decreasing a person's response to diuretic medications.diltiazem
Diltiazem, sold under the brand name Cardizem among others, is a calcium channel blocker medication used to treat high blood pressure, angina, and certain heart arrhythmias. It may also be used in hyperthyroidism if beta blockers cannot be ...
and verapamil
Verapamil, sold under various trade names, is a calcium channel blocker medication used for the treatment of high blood pressure, angina (chest pain from not enough blood flow to the heart), and supraventricular tachycardia. It may also be ...
, are known to decrease the force with which the heart ejects blood, thus are not recommended in people with heart failure with a reduced ejection fraction.
Supplements
Certain alternative medicine
Alternative medicine is any practice that aims to achieve the healing effects of medicine despite lacking biological plausibility, testability, repeatability, or evidence from clinical trials. Complementary medicine (CM), complementary and ...
s carry a risk of exacerbating existing heart failure, and are not recommended.gynura
''Gynura'' is a genus of flowering plants in the daisy family Asteraceae native to Asia. The best known species is ''Gynura aurantiaca
''Gynura aurantiaca'', called purple passion or velvet plant, is a species of flowering plant in the dai ...
, licorice, lily of the valley, tetrandrine
Tetrandrine, a bis-benzylisoquinoline alkaloid, is a calcium channel blocker. It is isolated from the plant ''Stephania tetrandra'', and other Chinese and Japanese herbs.
Pharamacology
It has anti-inflammatory, immunologic and antiallergenic e ...
, and yohimbine.
Pathophysiology
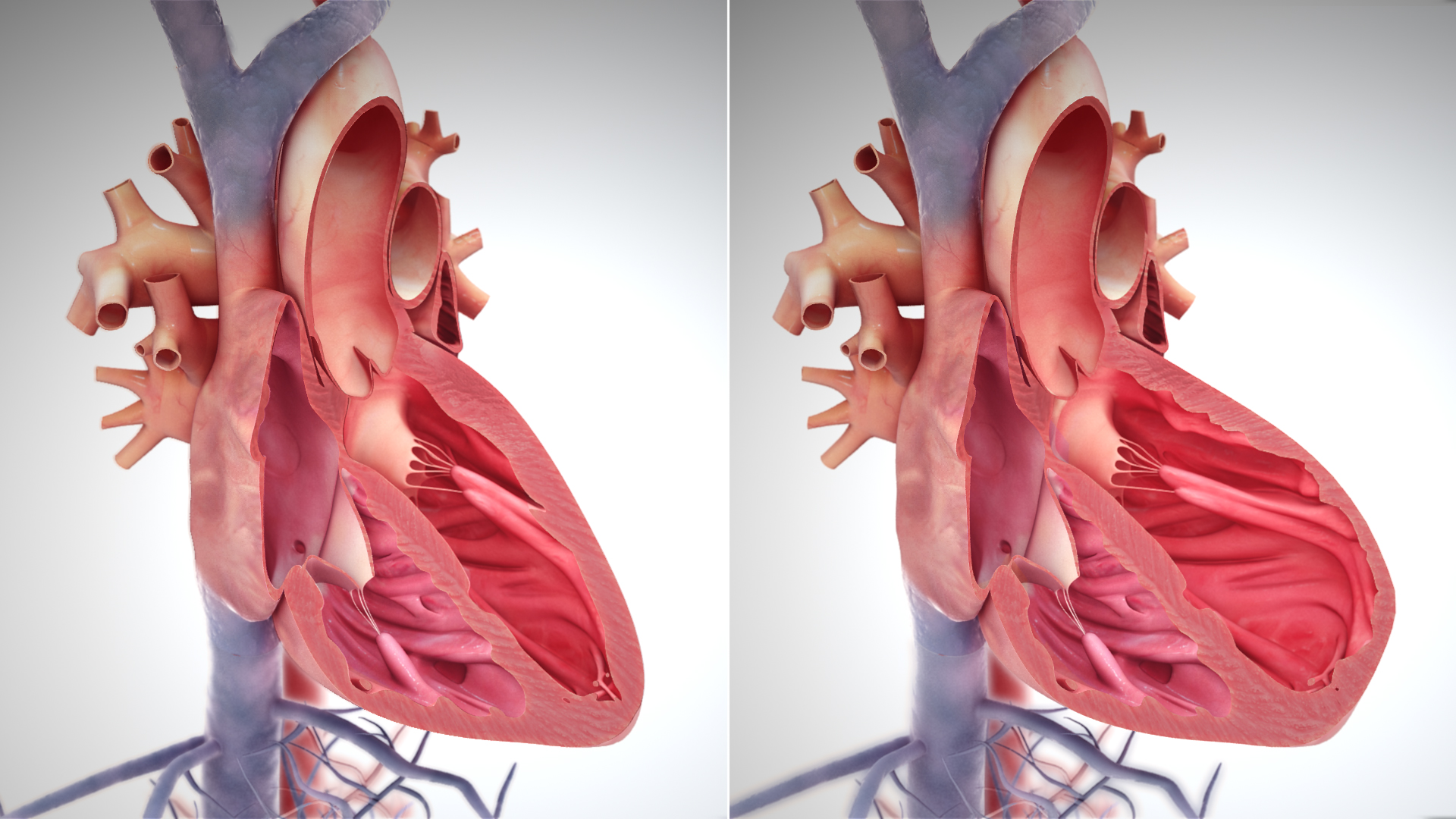 Heart failure is caused by any condition that reduces the efficiency of the heart muscle, through damage or overloading. Over time, these increases in workload, which are mediated by long-term activation of neurohormonal systems such as the renin–angiotensin system and the sympathoadrenal system, lead to fibrosis, dilation, and structural changes in the shape of the left ventricle from elliptical to spherical.
Heart failure is caused by any condition that reduces the efficiency of the heart muscle, through damage or overloading. Over time, these increases in workload, which are mediated by long-term activation of neurohormonal systems such as the renin–angiotensin system and the sympathoadrenal system, lead to fibrosis, dilation, and structural changes in the shape of the left ventricle from elliptical to spherical.actin
Actin is a protein family, family of Globular protein, globular multi-functional proteins that form microfilaments in the cytoskeleton, and the thin filaments in myofibril, muscle fibrils. It is found in essentially all Eukaryote, eukaryotic cel ...
and myosin myofilaments in over-stretched heart muscle.
Diagnosis
No diagnostic criteria have been agreed on as the gold standard
A gold standard is a Backed currency, monetary system in which the standard economics, economic unit of account is based on a fixed quantity of gold. The gold standard was the basis for the international monetary system from the 1870s to the ...
for heart failure. In the UK the National Institute for Health and Care Excellence
The National Institute for Health and Care Excellence (NICE) is an executive non-departmental public body of the Department of Health and Social Care in England that publishes guidelines in four areas:
* the use of health technologies withi ...
recommends measuring brain natriuretic peptide 32 (BNP) followed by an ultrasound of the heart if positive. This is recommended in those with shortness of breath
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing di ...
.[ In those with worsening heart failure, both a measure of BNP and of troponin are recommended to help determine likely outcomes.]
Classification
One historical method of categorizing heart failure is by the side of the heart involved (left heart failure versus right heart failure). Right heart failure was thought to compromise blood flow to the lungs compared to left heart failure compromising blood flow to the aorta and consequently to the brain and the remainder of the body's systemic circulation. However, mixed presentations are common and left heart failure is a common cause of right heart failure.
More accurate classification of heart failure type is made by measuring ejection fraction
An ejection fraction (EF) is the volumetric fraction (mathematics), fraction (or portion of the total) of fluid (usually blood) ejected from a chamber (usually the heart) with each contraction (or cardiac cycle, heartbeat). It can refer to the card ...
, or the proportion of blood pumped out of the heart during a single contraction.Cardiac arrest
Cardiac arrest is when the heart suddenly and unexpectedly stops beating. It is a medical emergency that, without immediate medical intervention, will result in sudden cardiac death within minutes. Cardiopulmonary resuscitation (CPR) and possib ...
and asystole refer to situations in which no cardiac output occurs at all. Without urgent treatment, these events result in sudden death. Myocardial infarction ("Heart attack") refers to heart muscle damage due to insufficient blood supply, usually as a result of a blocked coronary artery. Cardiomyopathy refers specifically to problems within the heart muscle, and these problems can result in heart failure.Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy (HCM, or HOCM when obstructive) is a condition in which the heart becomes thickened without an obvious cause. The parts of the heart most commonly affected are the interventricular septum and the ventricles. This r ...
involves enlargement and ''thickening'' of the heart muscle.
Ultrasound
An echocardiogram (ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies fr ...
of the heart) is commonly used to support a clinical diagnosis of heart failure. This can determine the stroke volume (SV, the amount of blood in the heart that exits the ventricles with each beat), the end-diastolic volume (EDV, the total amount of blood at the end of diastole), and the SV in proportion to the EDV, a value known as the ejection fraction
An ejection fraction (EF) is the volumetric fraction (mathematics), fraction (or portion of the total) of fluid (usually blood) ejected from a chamber (usually the heart) with each contraction (or cardiac cycle, heartbeat). It can refer to the card ...
(EF). In pediatrics, the shortening fraction is the preferred measure of systolic function. Normally, the EF should be between 50 and 70%; in systolic heart failure, it drops below 40%. Echocardiography can also identify valvular heart disease and assess the state of the pericardium (the connective tissue sac surrounding the heart). Echocardiography may also aid in deciding specific treatments, such as medication, insertion of an implantable cardioverter-defibrillator, or cardiac resynchronization therapy
Cardiac resynchronisation therapy (CRT or CRT-P) is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ve ...
. Echocardiography can also help determine if acute myocardial ischemia is the precipitating cause, and may manifest as regional wall motion abnormalities on echo.
File:UOTW 48 - Ultrasound of the Week 1.webm, Ultrasound showing severe systolic heart failure[
File:UOTW 48 - Ultrasound of the Week 3.webm, Ultrasound of the lungs showing edema due to severe systolic heart failure][
File:UOTW 48 - Ultrasound of the Week 4.webm, Ultrasound showing severe systolic heart failure][
File:UOTW 48 - Ultrasound of the Week 5.jpg, Ultrasound showing severe systolic heart failure][
]
Chest X-ray

Chest X-ray
A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in me ...
s are frequently used to aid in the diagnosis of CHF. In a person who is compensated, this may show cardiomegaly (visible enlargement of the heart), quantified as the cardiothoracic ratio (proportion of the heart size to the chest). In left ventricular failure, evidence may exist of vascular redistribution (upper lobe blood diversion or cephalization), Kerley lines, cuffing of the areas around the bronchi, and interstitial edema. Ultrasound of the lung may also be able to detect Kerley lines.
File:CHF2016.png, Congestive heart failure with small bilateral effusions
File:Kerley b lines.jpg, Kerley B lines
Electrophysiology
An electrocardiogram (ECG/EKG) may be used to identify arrhythmias, ischemic heart disease, right
Rights are legal, social, or ethical principles of freedom or entitlement; that is, rights are the fundamental normative rules about what is allowed of people or owed to people according to some legal system, social convention, or ethical th ...
and left ventricular hypertrophy, and presence of conduction delay or abnormalities (e.g. left bundle branch block). Although these findings are not specific to the diagnosis of heart failure, a normal ECG virtually excludes left ventricular systolic dysfunction.
Blood tests
Blood test
A blood test is a laboratory analysis performed on a blood sample that is usually extracted from a vein in the arm using a hypodermic needle, or via fingerprick. Multiple tests for specific blood components, such as a glucose test or a ch ...
s routinely performed include electrolytes (sodium
Sodium is a chemical element with the symbol Na (from Latin ''natrium'') and atomic number 11. It is a soft, silvery-white, highly reactive metal. Sodium is an alkali metal, being in group 1 of the periodic table. Its only stable ...
, potassium
Potassium is the chemical element with the symbol K (from Neo-Latin '' kalium'') and atomic number19. Potassium is a silvery-white metal that is soft enough to be cut with a knife with little force. Potassium metal reacts rapidly with atmosp ...
), measures of kidney function, liver function tests
Liver function tests (LFTs or LFs), also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin t ...
, thyroid function tests, a complete blood count
A complete blood count (CBC), also known as a full blood count (FBC), is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and ...
, and often C-reactive protein if infection is suspected. An elevated brain natriuretic peptide 32 (BNP) is a specific test indicative of heart failure. Additionally, BNP can be used to differentiate between causes of dyspnea due to heart failure from other causes of dyspnea. If myocardial infarction is suspected, various cardiac markers may be used.
BNP is a better indicator than N-terminal pro-BNP for the diagnosis of symptomatic heart failure and left ventricular systolic dysfunction. In symptomatic people, BNP had a sensitivity
Sensitivity may refer to:
Science and technology Natural sciences
* Sensitivity (physiology), the ability of an organism or organ to respond to external stimuli
** Sensory processing sensitivity in humans
* Sensitivity and specificity, statisti ...
of 85% and specificity of 84% in detecting heart failure; performance declined with increasing age.Vasopressin
Human vasopressin, also called antidiuretic hormone (ADH), arginine vasopressin (AVP) or argipressin, is a hormone synthesized from the AVP gene as a peptide prohormone in neurons in the hypothalamus, and is converted to AVP. It then ...
levels are usually increased, along with renin, angiotensin II, and catecholamines to compensate for reduced circulating volume due to inadequate cardiac output. This leads to increased fluid and sodium retention in the body; the rate of fluid retention is higher than the rate of sodium retention in the body, this phenomenon causes hypervolemic hyponatremia (low sodium concentration due to high body fluid retention). This phenomenon is more common in older women with low body mass. Severe hyponatremia can result in accumulation of fluid in the brain, causing cerebral edema and intracranial hemorrhage.
Angiography
Angiography is the X-ray
X-rays (or rarely, ''X-radiation'') are a form of high-energy electromagnetic radiation. In many languages, it is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it in 1895 and named it ' ...
imaging of blood vessel
Blood vessels are the structures of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from ...
s, which is done by injecting contrast agents into the bloodstream through a thin plastic tube ( catheter), which is placed directly in the blood vessel. X-ray images are called angiograms. Heart failure may be the result of coronary artery disease, and its prognosis depends in part on the ability of the coronary arteries to supply blood to the myocardium (heart muscle). As a result, coronary catheterization may be used to identify possibilities for revascularisation through percutaneous coronary intervention or bypass surgery.
Algorithms
Various algorithm
In mathematics and computer science, an algorithm () is a finite sequence of rigorous instructions, typically used to solve a class of specific problems or to perform a computation. Algorithms are used as specifications for performing ...
s are used for the diagnosis of heart failure. For example, the algorithm used by the Framingham Heart Study adds together criteria mainly from physical examination. In contrast, the more extensive algorithm by the European Society of Cardiology weights the difference between supporting and opposing parameters from the medical history
The medical history, case history, or anamnesis (from Greek: ἀνά, ''aná'', "open", and μνήσις, ''mnesis'', "memory") of a patient is information gained by a physician by asking specific questions, either to the patient or to other pe ...
, physical examination, further medical tests, and response to therapy.
Framingham criteria
By the Framingham criteria, diagnosis of congestive heart failure (heart failure with impaired pumping capability)weight loss
Weight loss, in the context of medicine, health, or physical fitness, refers to a reduction of the total body mass, by a mean loss of fluid, body fat (adipose tissue), or lean mass (namely bone mineral deposits, muscle, tendon, and other con ...
more than 4.5 kg in 5 days in response to treatment (sometimes classified as a minor criterion).[ In turn citing: ]
* Minor criteria include
# an abnormally fast heart rate more than 120 beats per minute,
# nocturnal cough,
# difficulty breathing with physical activity,
# pleural effusion,
# a decrease in the vital capacity by one-third from maximum recorded,
# liver enlargement, and
# bilateral ankle edema.chronic lung disease Chronic lung disease may refer to:
* Asthma
* Bronchopulmonary dysplasia
* Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms a ...
, cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage causes tissue repai ...
, ascites, or the nephrotic syndrome.[ The Framingham Heart Study criteria are 100% sensitive and 78% specific for identifying persons with definite congestive heart failure.][
]
ESC algorithm
The ESC algorithm weights these parameters in establishing the diagnosis of heart failure:
Staging
Heart failure is commonly stratified by the degree of functional impairment conferred by the severity of the heart failure (as reflected in the New York Heart Association (NYHA) Functional Classification.) The NYHA functional classes (I–IV) begin with class I, which is defined as a person who experiences no limitation in any activities and has no symptoms from ordinary activities. People with NYHA class II heart failure have slight, mild limitations with everyday activities; the person is comfortable at rest or with mild exertion. With NYHA class III heart failure, a marked limitation occurs with any activity; the person is comfortable only at rest. A person with NYHA class IV heart failure is symptomatic at rest and becomes quite uncomfortable with any physical activity. This score documents the severity of symptoms and can be used to assess response to treatment. While its use is widespread, the NYHA score is not very reproducible and does not reliably predict the walking distance or exercise tolerance on formal testing.
In its 2001 guidelines, the American College of Cardiology/ American Heart Association working group introduced four stages of heart failure:palliative care
Palliative care (derived from the Latin root , or 'to cloak') is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Wi ...
The ACC staging system is useful since stage A encompasses "pre-heart failure" – a stage where intervention with treatment can presumably prevent progression to overt symptoms. ACC stage A does not have a corresponding NYHA class. ACC stage B would correspond to NYHA class I. ACC stage C corresponds to NYHA class II and III, while ACC stage D overlaps with NYHA class IV.
* The degree of coexisting illness: i.e. heart failure/systemic hypertension, heart failure/pulmonary hypertension, heart failure/diabetes, heart failure/kidney failure, etc.
* Whether the problem is primarily increased venous back pressure ( preload), or failure to supply adequate arterial perfusion ( afterload)
* Whether the abnormality is due to low cardiac output with high systemic vascular resistance or high cardiac output with low vascular resistance (low-output heart failure vs. high-output heart failure)
Histopathology
 Histopathology can diagnose heart failure in autopsies. The presence of siderophages indicates chronic left-sided heart failure, but is not specific for it. It is also indicated by congestion of the pulmonary circulation.
Histopathology can diagnose heart failure in autopsies. The presence of siderophages indicates chronic left-sided heart failure, but is not specific for it. It is also indicated by congestion of the pulmonary circulation.
Prevention
A person's risk of developing heart failure is inversely related to level of physical activity. Those who achieved at least 500 MET-minutes/week (the recommended minimum by U.S. guidelines) had lower heart failure risk than individuals who did not report exercising during their free time; the reduction in heart failure risk was even greater in those who engaged in higher levels of physical activity than the recommended minimum.Johns Hopkins
Johns Hopkins (May 19, 1795 – December 24, 1873) was an American merchant, investor, and philanthropist. Born on a plantation, he left his home to start a career at the age of 17, and settled in Baltimore, Maryland where he remained for most ...
and the American Heart Association there are a few ways to help to prevent a cardiac event. Johns Hopkins mentions that stopping tobacco use, reducing high blood pressure, physical activity and your diet can drastically effect the chances of developing heart disease. High blood pressure accounts for most cardiovascular deaths. High blood pressure can be lowered into the normal range by making dietary decisions such as consuming less salt. Exercise also helps to bring blood pressure back down. One of the best ways to help avoid heart failure is to promote healthier eating habits like eating more vegetables, fruits, grains, and lean protein.
Diabetes is a major risk factor for heart failure. For women with Coronary Heart disease (CHD), diabetes was the strongest risk factor for heart failure. Diabetic women with depressed creatinine clearance or elevated BMI were at the highest risk of heart failure. While the annual incidence rate of heart failure for non-diabetic women with no risk factors is 0.4%, the annual incidence rate for diabetic women with elevated body mass index (BMI) and depressed creatinine clearance was 7% and 13%, respectively.
Management
Treatment focuses on improving the symptoms and preventing the progression of the disease. Reversible causes of heart failure also need to be addressed (e.g. infection
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable d ...
, alcohol ingestion, anemia, thyrotoxicosis, arrhythmia, and hypertension). Treatments include lifestyle and pharmacological modalities, and occasionally various forms of device therapy. Rarely, cardiac transplantation is used as an effective treatment when heart failure has reached the end stage.
Acute decompensation
In acute decompensated heart failure, the immediate goal is to re-establish adequate perfusion and oxygen delivery to end organs. This entails ensuring that airway, breathing, and circulation are adequate. Immediate treatments usually involve some combination of vasodilators such as nitroglycerin, diuretics such as furosemide, and possibly noninvasive positive pressure ventilation. Supplemental oxygen is indicated in those with oxygen saturation levels below 90%, but is not recommended in those with normal oxygen levels in normal atmosphere.
Chronic management
The goals of the treatment for people with chronic heart failure are the prolongation of life, prevention of acute decompensation, and reduction of symptoms, allowing for greater activity.
Heart failure can result from a variety of conditions. In considering therapeutic options, excluding reversible causes is of primary importance, including thyroid disease, anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, ...
, chronic tachycardia
Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal ( ...
, alcohol use disorder
Alcoholism is, broadly, any drinking of alcohol that results in significant mental
Mental may refer to:
* of or relating to the mind
Films
* ''Mental'' (2012 film), an Australian comedy-drama
* ''Mental'' (2016 film), a Bangladeshi r ...
, hypertension, and dysfunction of one or more heart valves. Treatment of the underlying cause is usually the first approach to treating heart failure. In the majority of cases, though, either no primary cause is found or treatment of the primary cause does not restore normal heart function. In these cases, behavioral
Behavior (American English) or behaviour (British English) is the range of actions and mannerisms made by individuals, organisms, systems or artificial entities in some environment. These systems can include other systems or organisms as we ...
, medical
Medicine is the science and practice of caring for a patient, managing the diagnosis, prognosis, prevention, treatment, palliation of their injury or disease, and promoting their health. Medicine encompasses a variety of health care practi ...
and device
A device is usually a constructed tool. Device may also refer to:
Technology Computing
* Device, a colloquial term encompassing desktops, laptops, tablets, smartphones, etc.
* Device file, an interface of a device driver
* Peripheral, any devi ...
treatment strategies exist that can provide a significant improvement in outcomes, including the relief of symptoms, exercise tolerance, and a decrease in the likelihood of hospitalization or death. Breathlessness rehabilitation for chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms include shortness of breath and a cough, which may or may not produce ...
and heart failure has been proposed with exercise training as a core component. Rehabilitation should also include other interventions to address shortness of breath including psychological and educational needs of people and needs of caregivers. Iron supplementation appears useful in those with iron deficiency anemia and heart failure.
Advance care planning
The latest evidence indicates that advance care planning (ACP) may help to increase documentation by medical staff regarding discussions with participants, and improve an individual's depression.
Monitoring
The various measures often used to assess the progress of people being treated for heart failure include fluid balance
Fluid balance is an aspect of the homeostasis of organisms in which the amount of water in the organism needs to be controlled, via osmoregulation and behavior, such that the concentrations of electrolytes ( salts in solution) in the variou ...
(calculation of fluid intake and excretion) and monitoring body weight (which in the shorter term reflects fluid shifts). Remote monitoring can be effective to reduce complications for people with heart failure.
Lifestyle
Behavior modification is a primary consideration in chronic heart failure management program, with dietary guidelines
In nutrition, diet is the sum of food consumed by a person or other organism.
The word diet often implies the use of specific intake of nutrition for health or weight-management reasons (with the two often being related). Although humans are o ...
regarding fluid and salt
Salt is a mineral composed primarily of sodium chloride (NaCl), a chemical compound belonging to the larger class of salts; salt in the form of a natural crystalline mineral is known as rock salt or halite. Salt is present in vast quanti ...
intake.
Exercise and physical activity
Exercise should be encouraged and tailored to suit individual's capabilities. A meta-analysis found that centre-based group interventions delivered by a physiotherapist are helpful in promoting physical activity in HF. There is a need for additional training for physiotherapists in delivering behaviour change intervention alongside an exercise programme. An intervention is expected to be more efficacious in encouraging physical activity than the usual care if it includes ''Prompts and cues'' to walk or exercise, like a phone call or a text message. It is extremely helpful if a trusted clinician provides explicit advice to engage in physical activity (''Credible source''). Another highly effective strategy is to place objects that will serve as a cue to engage in physical activity in the everyday environment of the patient (''Adding object to the environment''; e.g., exercise step or treadmill). Encouragement to walk or exercise in various settings beyond CR (e.g., home, neighbourhood, parks) is also promising (''Generalisation of target behaviour''). Additional promising strategies are ''Graded tasks'' (e.g., gradual increase in intensity and duration of exercise training), ''Self-monitoring'', ''Monitoring of physical activity by others without feedback'', ''Action planning'', and ''Goal-setting''. The inclusion of regular physical conditioning as part of a cardiac rehabilitation program can significantly improve quality of life
Quality of life (QOL) is defined by the World Health Organization as "an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards ...
and reduce the risk of hospital admission for worsening symptoms, but no evidence shows a reduction in mortality rates as a result of exercise. Despite cardiac rehabilitation being a recommended treatment for patients with heart failure with reduced ejection fraction (HFrEF), it is still underused. The reasons why this happens are complex, heterogeneous, and encompass healthcare system-, referring physician-, program-, and patient-level barriers. According to Alexandre et al., the main reasons for HFrEF patients not being enrolled in cardiac rehabilitation were no medical referral (31%), concomitant medical problems (28%), patient refusal (11%), and geographical distance to the hospital (9%). Furthermore, whether this evidence can be extended to people with HFpEF or to those whose exercise regimen takes place entirely at home is unclear.life expectancy
Life expectancy is a statistical measure of the average time an organism is expected to live, based on the year of its birth, current age, and other demographic factors like sex. The most commonly used measure is life expectancy at birth ...
.
Medication
Quadruple medical therapy using a combination of angiotensin-receptor neprilysin inhibitors (ARNI), beta blocker
Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms, and to protect the heart from a second heart attack after a first heart attack ( secondary prevention). They are ...
s, mineralocorticoid receptor antagonists (MRA), and sodium glucose cotransporter-2 inhibitors (SGLT2 inhibitors) is now the standard of care as of 2021.
=First line medications
=
First-line therapy for people with heart failure due to reduced systolic function should include angiotensin-converting enzyme (ACE) inhibitors (ACE-I), or angiotensin receptor blockers (ARBs) if the person develops a long-term cough as a side effect of the ACE-I. Use of medicines from these classes is associated with improved survival, fewer hospitalizations for heart failure exacerbations, and improved quality of life in people with heart failure.beta blocker
Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms, and to protect the heart from a second heart attack after a first heart attack ( secondary prevention). They are ...
, and a mineralocorticoid receptor antagonist as it reduces the risks of cardiovascular mortality and hospitalisation for heart failure by a further 4.7% (absolute risk reduction). However, the use of this combination agent requires the cessation of ACE-i or ARB therapy 48 hours before its initiation.
SGLT2 inhibitor is the newest medicine for heart failure.
=Other medications
=
Second-line medications for CHF do not confer a mortality benefit. Digoxin is one such medication. Its narrow therapeutic window, a high degree of toxicity, and the failure of multiple trials to show a mortality benefit have reduced its role in clinical practice. It is now used in only a small number of people with refractory symptoms, who are in atrial fibrillation, and/or who have chronic hypotension.
Diuretics have been a mainstay of treatment against symptoms of fluid accumulation, and include diuretics classes such as loop diuretics (such as furosemide), thiazide-like diuretics, and potassium-sparing diuretics. Although widely used, evidence on their efficacy and safety is limited, with the exception of mineralocorticoid antagonists such as spironolactone.intravenous iron
Iron supplements, also known as iron salts and iron pills, are a number of iron formulations used to treat and prevent iron deficiency including iron deficiency anemia. For prevention they are only recommended in those with poor absorption, ...
if deficiency is found.Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food ...
for the treatment of euvolemic hyponatremia in those with heart failure.[ Ivabradine has been found to reduce the risk of hospitalization for heart failure exacerbations in this subgroup of people with heart failure.][
]
Implanted devices
In people with severe cardiomyopathy (left ventricular ejection fraction below 35%), or in those with recurrent VT or malignant arrhythmias, treatment with an automatic implantable cardioverter-defibrillator (AICD) is indicated to reduce the risk of severe life-threatening arrhythmias. The AICD does not improve symptoms or reduce the incidence of malignant arrhythmias but does reduce mortality from those arrhythmias, often in conjunction with antiarrhythmic medications. In people with left ventricular ejection (LVEF) below 35%, the incidence of ventricular tachycardia
Ventricular tachycardia (V-tach or VT) is a fast heart rate arising from the lower chambers of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short perio ...
or sudden cardiac death is high enough to warrant AICD placement. Its use is therefore recommended in AHA
AHA, Aha, or aha may refer to:
Arts, entertainment and media
* ''Aha!'' (TV program), an information and education TV program in the Philippines
* a-ha, a Norwegian pop music band
* ''Aha!'' (film), a 2007 Bangladeshi film
* Aha (streaming se ...
/ ACC guidelines.QRS complex
The QRS complex is the combination of three of the graphical deflections seen on a typical electrocardiogram (ECG or EKG). It is usually the central and most visually obvious part of the tracing. It corresponds to the depolarization of the r ...
duration (120 ms or less) and has been demonstrated to improve the symptoms, quality of life, and exercise tolerance.cardiac resynchronization therapy
Cardiac resynchronisation therapy (CRT or CRT-P) is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ve ...
(CRT) can initiate a normal sequence of ventricular depolarization. In people with LVEF below 35% and prolonged QRS duration on ECG (LBBB or QRS of 150 ms or more), an improvement in symptoms and mortality occurs when CRT is added to standard medical therapy.
Surgical therapies
People with the most severe heart failure may be candidates for ventricular assist devices, which have commonly been used as a bridge to heart transplantation, but have been used more recently as a destination treatment for advanced heart failure.
Palliative care
People with heart failure often have significant symptoms, such as shortness of breath and chest pain. Palliative care should be initiated early in the HF trajectory, and should not be an option of last resort.power of attorney
A power of attorney (POA) or letter of attorney is a written authorization to represent or act on another's behalf in private affairs (which may be financial or regarding health and welfare), business, or some other legal matter. The person auth ...
and discussed his or her wishes with this individual.[
]
Prognosis
Prognosis in heart failure can be assessed in multiple ways, including clinical prediction rules and cardiopulmonary exercise testing. Clinical prediction rules use a composite of clinical factors such as laboratory tests and blood pressure to estimate prognosis. Among several clinical prediction rules for prognosticating acute heart failure, the 'EFFECT rule' slightly outperformed other rules in stratifying people and identifying those at low risk of death during hospitalization or within 30 days.
Epidemiology
In 2022, heart failure affected about 64 million people globally.[ and in those over the age of 65, this increases to 6–10%.][ Above 75 years old, rates are greater than 10%.][
Rates are predicted to increase.][ Increasing rates are mostly because of increasing lifespan, but also because of increased risk factors (hypertension, diabetes, dyslipidemia, and obesity) and improved survival rates from other types of cardiovascular disease (myocardial infarction, valvular disease, and arrhythmias).]
United States
In the United States, heart failure affects 5.8 million people, and each year 550,000 new cases are diagnosed.
United Kingdom
In the UK, despite moderate improvements in prevention, heart failure rates have increased due to population growth and ageing.
Developing world
In tropical countries, the most common cause of HF is valvular heart disease or some type of cardiomyopathy. As underdeveloped countries have become more affluent, the incidences of diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
, hypertension, and obesity
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's ...
have increased, which have in turn raised the incidence of heart failure.
Sex
Men have a higher incidence of heart failure, but the overall prevalence rate is similar in both sexes since women survive longer after the onset of heart failure.menopause
Menopause, also known as the climacteric, is the time in women's lives when menstrual periods stop permanently, and they are no longer able to bear children. Menopause usually occurs between the age of 47 and 54. Medical professionals often d ...
), they are more likely than men to have diastolic dysfunction, and seem to experience a lower overall quality of life than men after diagnosis.[
]
Ethnicity
Some sources state that people of Asian descent are at a higher risk of heart failure than other ethnic groups. Other sources however have found that rates of heart failure are similar to rates found in other ethnic groups.
History
For centuries, the disease entity which would include many cases of what today would be called heart failure was ''dropsy''; the term denotes generalized edema, a major manifestation of a failing heart, though also caused by other diseases. Writings of ancient civilizations include evidence of their acquaintance with dropsy and heart failure: Egyptians were the first to use bloodletting
Bloodletting (or blood-letting) is the withdrawal of blood from a patient to prevent or cure illness and disease. Bloodletting, whether by a physician or by leeches, was based on an ancient system of medicine in which blood and other bodily flu ...
to relieve fluid accumulation and shortage of breath, and provided what may have been the first documented observations on heart failure in the Ebers papurus (around 1500 BCE);Avicenna
Ibn Sina ( fa, ابن سینا; 980 – June 1037 CE), commonly known in the West as Avicenna (), was a Persian polymath who is regarded as one of the most significant physicians, astronomers, philosophers, and writers of the Islam ...
round 1000 CE,William Harvey
William Harvey (1 April 1578 – 3 June 1657) was an English physician who made influential contributions in anatomy and physiology. He was the first known physician to describe completely, and in detail, the systemic circulation and prope ...
in 1628.Giovanni Maria Lancisi
Giovanni Maria Lancisi (26 October 1654 – 20 January 1720) was an Italian physician, epidemiologist and anatomist who made a correlation between the presence of mosquitoes and the prevalence of malaria. He was also known for his studies about c ...
connected jugular vein distention with right ventricular failure in 1728.x-ray
X-rays (or rarely, ''X-radiation'') are a form of high-energy electromagnetic radiation. In many languages, it is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it in 1895 and named it ' ...
s, discovered by Wilhelm Röntgen in 1895, and electrocardiography, described by Willem Einthoven in 1903, facilitated the investigation of heart failure.Jean-Baptiste de Sénac
Jean-Baptiste de Sénac (1693–1770) was a French physician was born in the district of Lombez in Gascony, France.
Early life and education
Details of his early life are sketchy, however, it is generally thought that he studied medicine at the Un ...
in 1749 recommended opiate
An opiate, in classical pharmacology, is a substance derived from opium. In more modern usage, the term ''opioid'' is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain (including antagonist ...
s for acute shortage of breath due to heart failure.Paracelsus
Paracelsus (; ; 1493 – 24 September 1541), born Theophrastus von Hohenheim (full name Philippus Aureolus Theophrastus Bombastus von Hohenheim), was a Swiss physician, alchemist, lay theologian, and philosopher of the German Renaissance.
H ...
;[Eknoyan G (1996]
Historical note. On the contributions of Paracelsus to nephrology.
''Nephrol Dial Transplant'' 11 (7):1388–94. PMID
8672051
/ref> in the 19th century they were used by noted physicians like John Blackall and William Stokes.
Economics
In 2011, nonhypertensive heart failure was one of the 10 most expensive conditions seen during inpatient hospitalizations in the U.S., with aggregate inpatient hospital costs more than $10.5 billion.
Heart failure is associated with a high health expenditure, mostly because of the cost of hospitalizations; costs have been estimated to amount to 2% of the total budget of the National Health Service
The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom (UK). Since 1948, they have been funded out of general taxation. There are three systems which are referred to using the " ...
in the United Kingdom, and more than $35 billion in the United States.
Research directions
Some research indicates that stem cell therapy may help.
Notes
References
External links
Heart failure
American Heart Association – information and resources for treating and living with heart failure
Heart Failure Matters
– patient information website of the Heart Failure Association of the European Society of Cardiology
Heart failure in children
by Great Ormond Street Hospital, London, UK
*
2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure
- Guideline Hub at American College of Cardiology, jointly with the American Heart Association and the Heart Failure Society of America. JACC article link, quick references, slides, perspectives, education, apps and tools, and patient resources. Apr 01, 2022
2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure
- European Society of Cardiology resource webpage with links to Full Text and Related Materials, Scientific Presentation at ESC Congress 2021, news article, TV interview, slide set, and ESC Pocket Guidelines; plus previous versions. App. 27 Aug 2021
{{DEFAULTSORT:Heart Failure
Aging-associated diseases
Heart diseases
Organ failure
Wikipedia medicine articles ready to translate
Wikipedia emergency medicine articles ready to translate
Disorders causing edema
 Congestive heart failure is a pathophysiological condition in which the heart's output is insufficient to meet the needs of the body and lungs. The term "congestive heart failure" is often used because one of the most common symptoms is congestion or fluid accumulation in the tissues and veins of the lungs or other parts of a person's body. Congestion manifests itself particularly in the form of fluid accumulation and swelling ( edema), both in the form of peripheral edema (causing swollen limbs and feet) and pulmonary edema (causing difficulty breathing) and ascites (swollen abdomen).
Symptoms of heart failure are traditionally divided into left-sided and right-sided because the left and right ventricles supply different parts of the circulation, but sufferers often have both types of signs and symptoms. In biventricular heart failure, both sides of the heart are affected. Left-sided heart failure is the more common.
Congestive heart failure is a pathophysiological condition in which the heart's output is insufficient to meet the needs of the body and lungs. The term "congestive heart failure" is often used because one of the most common symptoms is congestion or fluid accumulation in the tissues and veins of the lungs or other parts of a person's body. Congestion manifests itself particularly in the form of fluid accumulation and swelling ( edema), both in the form of peripheral edema (causing swollen limbs and feet) and pulmonary edema (causing difficulty breathing) and ascites (swollen abdomen).
Symptoms of heart failure are traditionally divided into left-sided and right-sided because the left and right ventricles supply different parts of the circulation, but sufferers often have both types of signs and symptoms. In biventricular heart failure, both sides of the heart are affected. Left-sided heart failure is the more common.
 Right-sided heart failure is often caused by pulmonary heart disease (cor pulmonale), which is typically caused by issues with pulmonary circulation such as pulmonary hypertension or pulmonic stenosis. Physical examination may reveal pitting peripheral edema, ascites, liver enlargement, and spleen enlargement. Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by testing hepatojugular reflux. If the right ventricular pressure is increased, a parasternal heave which causes the compensatory increase in contraction strength may be present.
''Backward'' failure of the right ventricle leads to congestion of systemic capillaries. This generates excess fluid accumulation in the body. This causes swelling under the skin ( peripheral edema or
Right-sided heart failure is often caused by pulmonary heart disease (cor pulmonale), which is typically caused by issues with pulmonary circulation such as pulmonary hypertension or pulmonic stenosis. Physical examination may reveal pitting peripheral edema, ascites, liver enlargement, and spleen enlargement. Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by testing hepatojugular reflux. If the right ventricular pressure is increased, a parasternal heave which causes the compensatory increase in contraction strength may be present.
''Backward'' failure of the right ventricle leads to congestion of systemic capillaries. This generates excess fluid accumulation in the body. This causes swelling under the skin ( peripheral edema or  Chronic stable heart failure may easily decompensate. This most commonly results from a concurrent illness (such as
Chronic stable heart failure may easily decompensate. This most commonly results from a concurrent illness (such as 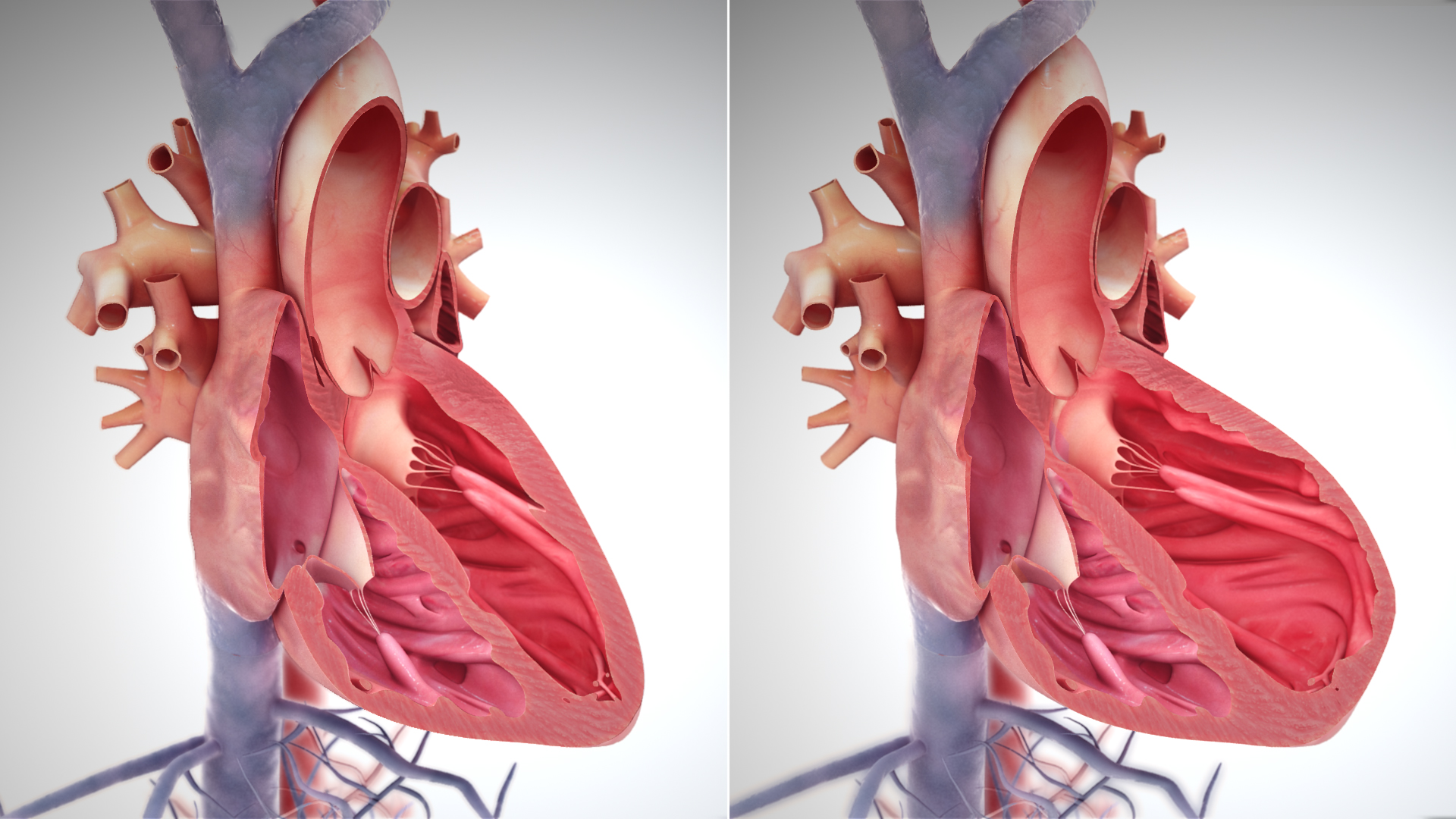 Heart failure is caused by any condition that reduces the efficiency of the heart muscle, through damage or overloading. Over time, these increases in workload, which are mediated by long-term activation of neurohormonal systems such as the renin–angiotensin system and the sympathoadrenal system, lead to fibrosis, dilation, and structural changes in the shape of the left ventricle from elliptical to spherical.
The heart of a person with heart failure may have a reduced force of contraction due to overloading of the ventricle. In a normal heart, increased filling of the ventricle results in increased contraction force by the Frank–Starling law of the heart, and thus a rise in cardiac output. In heart failure, this mechanism fails, as the ventricle is loaded with blood to the point where heart muscle contraction becomes less efficient. This is due to reduced ability to cross-link
Heart failure is caused by any condition that reduces the efficiency of the heart muscle, through damage or overloading. Over time, these increases in workload, which are mediated by long-term activation of neurohormonal systems such as the renin–angiotensin system and the sympathoadrenal system, lead to fibrosis, dilation, and structural changes in the shape of the left ventricle from elliptical to spherical.
The heart of a person with heart failure may have a reduced force of contraction due to overloading of the ventricle. In a normal heart, increased filling of the ventricle results in increased contraction force by the Frank–Starling law of the heart, and thus a rise in cardiac output. In heart failure, this mechanism fails, as the ventricle is loaded with blood to the point where heart muscle contraction becomes less efficient. This is due to reduced ability to cross-link 
 Histopathology can diagnose heart failure in autopsies. The presence of siderophages indicates chronic left-sided heart failure, but is not specific for it. It is also indicated by congestion of the pulmonary circulation.
Histopathology can diagnose heart failure in autopsies. The presence of siderophages indicates chronic left-sided heart failure, but is not specific for it. It is also indicated by congestion of the pulmonary circulation.