deep-vein thrombosis on:
[Wikipedia]
[Google]
[Amazon]
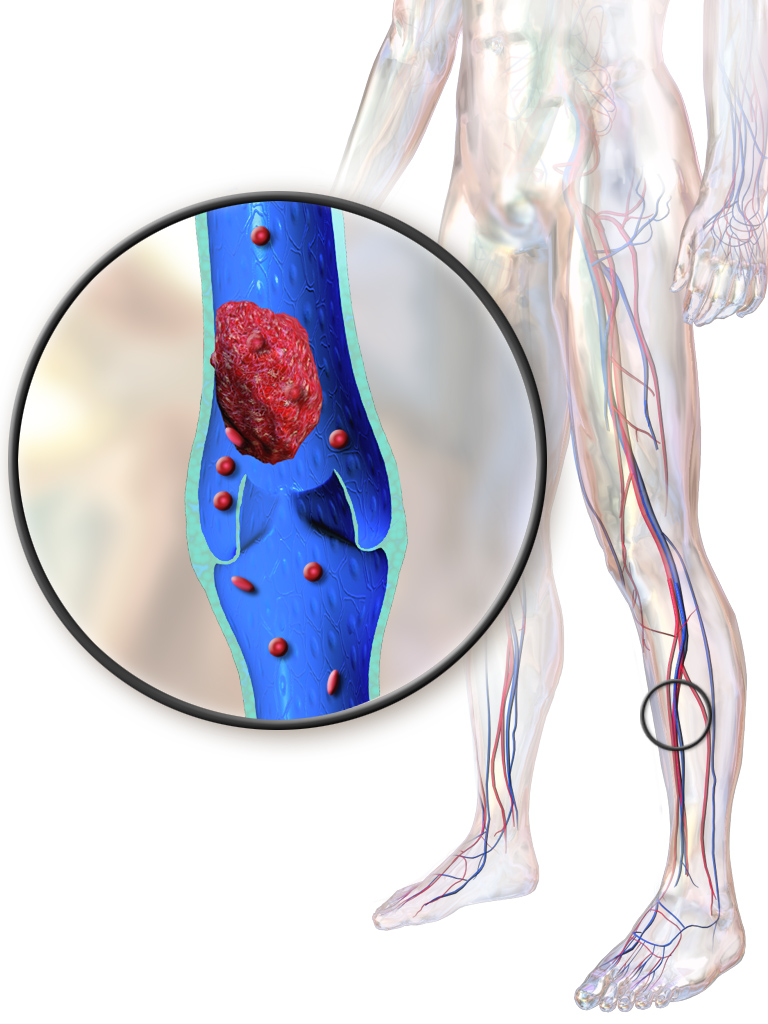
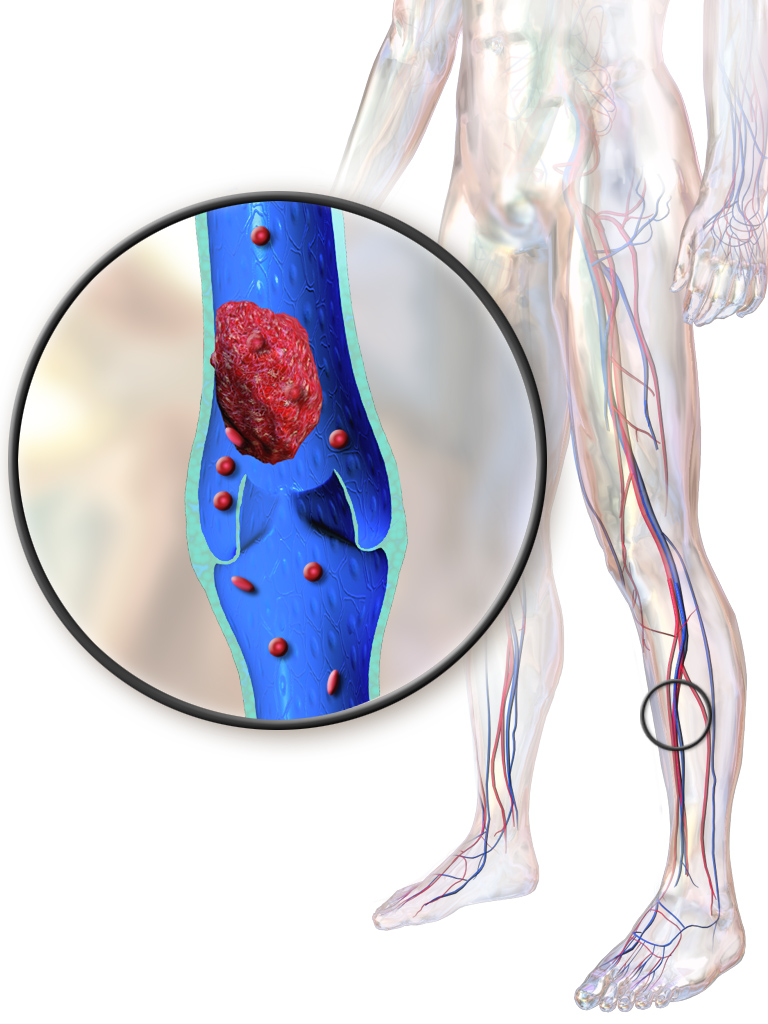
Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms. The most common life-threatening concern with DVT is the potential for a clot to embolize (detach from the veins), travel as an embolus through the right side of the heart, and become lodged in a
 Symptoms classically affect a leg and typically develop over hours or days, though they can develop suddenly or over a matter of weeks. The legs are primarily affected, with 4–10% of DVT occurring in the arms. Despite the signs and symptoms being highly variable, the typical symptoms are pain, swelling, and redness. However, these symptoms might not manifest in the lower limbs of those unable to walk. In those who are able to walk, DVT can reduce one's ability to do so. The pain can be described as throbbing and can worsen with weight-bearing, prompting one to bear more weight with the unaffected leg. Additional signs and symptoms include tenderness, pitting edema (''see image''), dilation of surface veins, warmth, discoloration, a "pulling sensation", and even
Symptoms classically affect a leg and typically develop over hours or days, though they can develop suddenly or over a matter of weeks. The legs are primarily affected, with 4–10% of DVT occurring in the arms. Despite the signs and symptoms being highly variable, the typical symptoms are pain, swelling, and redness. However, these symptoms might not manifest in the lower limbs of those unable to walk. In those who are able to walk, DVT can reduce one's ability to do so. The pain can be described as throbbing and can worsen with weight-bearing, prompting one to bear more weight with the unaffected leg. Additional signs and symptoms include tenderness, pitting edema (''see image''), dilation of surface veins, warmth, discoloration, a "pulling sensation", and even
File:SaddlePE.PNG, alt=A computed tomography image depicting PE in the pulmonary arteries, A CT image with red arrows indicating PE (grey) in the pulmonary arteries (white)
File:PCD2016.jpg, alt=Image showing marked discoloration of a leg with phlegmasia cerulea dolens, A case of phlegmasia cerulea dolens in the left leg
Patent-foramen-ovale-en.png, alt=A drawing depicting a patent foramen ovale, A depiction of a patent foramen ovale
 DVT and PE are the two manifestations of the
DVT and PE are the two manifestations of the
and has limited clinical significance compared to proximal DVT. Calf DVT makes up about half of DVTs. Iliofemoral DVT has been described as involving either the iliac or common femoral vein; elsewhere, it has been defined as involving at a minimum the
 Traditionally, the three factors of
Traditionally, the three factors of  Dozens of genetic risk factors have been identified, and they account for approximately 50 to 60% of the variability in VTE rates. As such,
Dozens of genetic risk factors have been identified, and they account for approximately 50 to 60% of the variability in VTE rates. As such,
 Blood has a natural tendency to clot when blood vessels are damaged (
Blood has a natural tendency to clot when blood vessels are damaged ( In arterial thrombosis, blood vessel wall damage is required, as it initiates
In arterial thrombosis, blood vessel wall damage is required, as it initiates
DVTUS.PNG, An ultrasound with a blood clot visible in the left common femoral vein. (The common femoral vein is distal to the external iliac vein.)
Ultrasonography of deep vein thrombosis of the femoral vein -annotated.jpg,
"NICE Guideline 158: Venous thromboembolic diseases: diagnosis, management and thrombophilia testing
London, 26 March 2020. It is not recommended practice to obtain tumor markers or a CT of the abdomen and pelvis in asymptomatic individuals. NICE recommends that further investigations are unwarranted in those without relevant signs or symptoms.
"NICE Interventional procedures guidance 651: Percutaneous mechanical thrombectomy for acute deep vein thrombosis of the leg
London, 12 June 2019. Catheter-directed thrombolysis with thrombectomy against iliofemoral DVT has been associated with a reduction in the severity of post-thrombotic syndrome at an estimated cost-effectiveness ratio of about $138,000 per gained QALY. Phlegmasia cerulea dolens might be treated with catheter-directed thrombolysis and/or thrombectomy. In DVT in the arm, the first (topmost) rib can be surgically removed as part of the typical treatment when the DVT is due to thoracic outlet syndrome or Paget–Schroetter syndrome. This treatment involves initial anticoagulation followed by thrombolysis of the subclavian vein and staged first rib resection to relieve the thoracic outlet compression and prevent recurrent DVT.
File:Gray966.png, The first rib, which is removed in a first rib resection surgery, is labeled 1 in this image
File:A-case-of-Paget-Schroetter-syndrome-(PSS)-in-a-young-judo-tutor-a-case-report-13256 2016 848 Fig1 HTML.jpg, A venogram before catheter-directed thrombolysis for Paget–Schroetter syndrome, a rare and severe arm DVT shown here in a judo practitioner, with highly restricted blood flow shown in the vein
File:A-case-of-Paget-Schroetter-syndrome-(PSS)-in-a-young-judo-tutor-a-case-report-13256 2016 848 Fig2 HTML.jpg, After treatment with catheter-directed thrombolysis, blood flow in the axillary vein, axillary and subclavian vein were significantly improved. Afterwards, a first rib resection allowed decompression. This reduces the risk of recurrent DVT and other sequelae from thoracic outlet compression.
 The placement of an inferior vena cava filter (IVC filter) is possible when either the standard treatment for acute DVT, anticoagulation, is absolutely contraindicated (not possible), or if someone develops a PE despite being anticoagulated. However, a 2020 NICE review found "little good evidence" for their use. A 2018 study associated IVC filter placement with a 50% reduction in PE, a 70% increase in DVT, and an 18% increase in 30 day mortality when compared to no IVC placement. Other studies including a systematic review and meta-analysis did not find a difference in mortality with IVC placement. If someone develops a PE despite being anticoagulated, care should be given to optimize anticoagulation treatment and address other related concerns before considering IVC filter placement.
The placement of an inferior vena cava filter (IVC filter) is possible when either the standard treatment for acute DVT, anticoagulation, is absolutely contraindicated (not possible), or if someone develops a PE despite being anticoagulated. However, a 2020 NICE review found "little good evidence" for their use. A 2018 study associated IVC filter placement with a 50% reduction in PE, a 70% increase in DVT, and an 18% increase in 30 day mortality when compared to no IVC placement. Other studies including a systematic review and meta-analysis did not find a difference in mortality with IVC placement. If someone develops a PE despite being anticoagulated, care should be given to optimize anticoagulation treatment and address other related concerns before considering IVC filter placement.
 Major orthopedic surgery—total hip replacement, total knee replacement, or Hip fracture#Management, hip fracture surgery—has a high risk of causing VTE. If prophylaxis is not used after these surgeries, symptomatic VTE has about a 4% chance of developing within 35 days. Following major orthopedic surgery, a blood thinner or aspirin is typically paired with intermittent pneumatic compression, which is the preferred mechanical prophylaxis over graduated compression stockings.
Options for VTE prevention in people following non-orthopedic surgery include early walking, mechanical prophylaxis, and blood thinners (low-molecular-weight heparin and low-dose-unfractionated heparin) depending upon the risk of VTE, risk of major bleeding, and person's preferences. After low-risk surgeries, early and frequent walking is the best preventive measure.
Major orthopedic surgery—total hip replacement, total knee replacement, or Hip fracture#Management, hip fracture surgery—has a high risk of causing VTE. If prophylaxis is not used after these surgeries, symptomatic VTE has about a 4% chance of developing within 35 days. Following major orthopedic surgery, a blood thinner or aspirin is typically paired with intermittent pneumatic compression, which is the preferred mechanical prophylaxis over graduated compression stockings.
Options for VTE prevention in people following non-orthopedic surgery include early walking, mechanical prophylaxis, and blood thinners (low-molecular-weight heparin and low-dose-unfractionated heparin) depending upon the risk of VTE, risk of major bleeding, and person's preferences. After low-risk surgeries, early and frequent walking is the best preventive measure.
 Travelling "is an often cited yet relatively uncommon" cause of VTE. Suggestions for at-risk long-haul travelers include calf exercises, frequent walking, and aisle seating in airplanes to ease walking. See section 6.0, Long-Distance Travel Graduated compression stockings have sharply reduced the levels of asymptomatic DVT in airline passengers, but the effect on symptomatic DVT, PE, or mortality is unknown, as none of the individuals studied developed these outcomes. However, graduated compression stockings are not suggested for long-haul travelers (>4 hours) without risk factors for VTE. Likewise, neither aspirin nor anticoagulants are suggested in the general population undertaking long-haul travel. Those with significant VTE risk factors undertaking long-haul travel are suggested to use either graduated compression stockings or LMWH for VTE prevention. If neither of these two methods are feasible, then aspirin is suggested.
Travelling "is an often cited yet relatively uncommon" cause of VTE. Suggestions for at-risk long-haul travelers include calf exercises, frequent walking, and aisle seating in airplanes to ease walking. See section 6.0, Long-Distance Travel Graduated compression stockings have sharply reduced the levels of asymptomatic DVT in airline passengers, but the effect on symptomatic DVT, PE, or mortality is unknown, as none of the individuals studied developed these outcomes. However, graduated compression stockings are not suggested for long-haul travelers (>4 hours) without risk factors for VTE. Likewise, neither aspirin nor anticoagulants are suggested in the general population undertaking long-haul travel. Those with significant VTE risk factors undertaking long-haul travel are suggested to use either graduated compression stockings or LMWH for VTE prevention. If neither of these two methods are feasible, then aspirin is suggested.
 Being on blood thinners because of DVT can be life-changing because it can prevent lifestyle activities such as contact or winter sports to prevent bleeding after potential injuries. Head injuries prompting brain bleeds are of particular concern. This has caused NASCAR driver Brian Vickers to forego participation in races. Professional basketball players including NBA players Chris Bosh and hall of famer Hakeem Olajuwon have dealt with recurrent blood clots, and Bosh's career was significantly hampered by DVT and PE.
Tennis star Serena Williams was hospitalized in 2011 for PE thought to have originated from DVT. Years later, in 2017, due to her knowledge of DVT and PE, Serena accurately Patient advocacy, advocated for herself to have a PE diagnosed and treated. During this encounter with VTE, she was hospitalized after a C-section surgery and was off of blood thinners. After feeling the sudden onset of a PE symptom, shortness of breath, she told her nurse and requested CT pulmonary angiogram, a CT scan and an IV heparin drip, all while gasping for air. She started to receive an ultrasound to look for DVT in the legs, prompting her to express dissatisfaction to the medical staff that they were not looking for clots where she had symptoms (her lungs), and they were not yet treating her presumed PE. After being diagnosed with PE and not DVT, and after receiving heparin by IV, the coughing from the PE caused her C-section surgical site to open and the heparin contributed to bleeding at the site. Serena later received an IVC filter while in the hospital.
Other notable people have been affected by DVT. Former United States (US) President Richard Nixon had recurrent DVT, and so has former Secretary of State Hillary Clinton. She was first diagnosed while First Lady of the United States, First Lady in 1998 and again in 2009. Dick Cheney was diagnosed with an episode while Vice President of the United States, Vice President, and TV show host Regis Philbin had DVT after hip-replacement surgery. DVT has also contributed to the deaths of famous people. For example, DVT and PE played a role in rapper Heavy D's death at age 44. NBC journalist David Bloom died at age 39 while covering the Iraq War from a PE that was thought to have progressed from a missed DVT, and actor Jimmy Stewart had DVT that progressed to a PE when he was 89.
Being on blood thinners because of DVT can be life-changing because it can prevent lifestyle activities such as contact or winter sports to prevent bleeding after potential injuries. Head injuries prompting brain bleeds are of particular concern. This has caused NASCAR driver Brian Vickers to forego participation in races. Professional basketball players including NBA players Chris Bosh and hall of famer Hakeem Olajuwon have dealt with recurrent blood clots, and Bosh's career was significantly hampered by DVT and PE.
Tennis star Serena Williams was hospitalized in 2011 for PE thought to have originated from DVT. Years later, in 2017, due to her knowledge of DVT and PE, Serena accurately Patient advocacy, advocated for herself to have a PE diagnosed and treated. During this encounter with VTE, she was hospitalized after a C-section surgery and was off of blood thinners. After feeling the sudden onset of a PE symptom, shortness of breath, she told her nurse and requested CT pulmonary angiogram, a CT scan and an IV heparin drip, all while gasping for air. She started to receive an ultrasound to look for DVT in the legs, prompting her to express dissatisfaction to the medical staff that they were not looking for clots where she had symptoms (her lungs), and they were not yet treating her presumed PE. After being diagnosed with PE and not DVT, and after receiving heparin by IV, the coughing from the PE caused her C-section surgical site to open and the heparin contributed to bleeding at the site. Serena later received an IVC filter while in the hospital.
Other notable people have been affected by DVT. Former United States (US) President Richard Nixon had recurrent DVT, and so has former Secretary of State Hillary Clinton. She was first diagnosed while First Lady of the United States, First Lady in 1998 and again in 2009. Dick Cheney was diagnosed with an episode while Vice President of the United States, Vice President, and TV show host Regis Philbin had DVT after hip-replacement surgery. DVT has also contributed to the deaths of famous people. For example, DVT and PE played a role in rapper Heavy D's death at age 44. NBC journalist David Bloom died at age 39 while covering the Iraq War from a PE that was thought to have progressed from a missed DVT, and actor Jimmy Stewart had DVT that progressed to a PE when he was 89.
 The book ''Sushruta Samhita'', an Ayurvedic text published around 600–900 BC, contains what has been cited as the first description of DVT. In 1271, DVT symptoms in the leg of a 20-year-old male were described in a French manuscript, which has been cited as the first case or the first Western reference to DVT.
In 1856, German physician and pathologist Rudolf Virchow published his analysis after the insertion of foreign bodies into the jugular veins of dogs, which migrated to the pulmonary arteries. These foreign bodies caused pulmonary emboli, and Virchow was focused on explaining their consequences. He cited three factors, which are now understood as hypercoaguability, stasis, and endothelial injury. It was not until 1950 that this framework was cited as Virchow's triad, but the teaching of Virchow's triad has continued in light of its utility as a theoretical framework and as a recognition of the significant progress Virchow made in expanding the understanding of VTE.
Methods to observe DVT by ultrasound were established in the 1960s. Diagnoses were commonly performed by impedance plethysmography in the 1970s and 1980s, but ultrasound, particularly after utility of probe compression was demonstrated in 1986, became the preferred diagnostic method. Yet, in the mid-1990s, contrast venography and impedance plethysmography were still described as common.
The book ''Sushruta Samhita'', an Ayurvedic text published around 600–900 BC, contains what has been cited as the first description of DVT. In 1271, DVT symptoms in the leg of a 20-year-old male were described in a French manuscript, which has been cited as the first case or the first Western reference to DVT.
In 1856, German physician and pathologist Rudolf Virchow published his analysis after the insertion of foreign bodies into the jugular veins of dogs, which migrated to the pulmonary arteries. These foreign bodies caused pulmonary emboli, and Virchow was focused on explaining their consequences. He cited three factors, which are now understood as hypercoaguability, stasis, and endothelial injury. It was not until 1950 that this framework was cited as Virchow's triad, but the teaching of Virchow's triad has continued in light of its utility as a theoretical framework and as a recognition of the significant progress Virchow made in expanding the understanding of VTE.
Methods to observe DVT by ultrasound were established in the 1960s. Diagnoses were commonly performed by impedance plethysmography in the 1970s and 1980s, but ultrasound, particularly after utility of probe compression was demonstrated in 1986, became the preferred diagnostic method. Yet, in the mid-1990s, contrast venography and impedance plethysmography were still described as common.
 Multiple pharmacological therapies for DVT were introduced in the 20th century: oral anticoagulants in the 1940s, subcutaneous injections of LDUH in 1962 and subcutaneous injections of LMWH in 1982. 1974 was when vascular inflammation and venous thrombosis were first proposed to be interrelated. For around 50 years, a months-long warfarin (Coumadin) regimen was the mainstay of pharmacological treatment. To avoid the blood monitoring required with warfarin and the injections required by heparin and heparin-like medicines, direct oral anticoagulants (DOACs) were developed. In the late 2000s to early 2010s, DOACs—including rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa)—came to the market. ''The New York Times'' described a "furious battle" among the three makers of these drugs "for the prescription pads of doctors".
Multiple pharmacological therapies for DVT were introduced in the 20th century: oral anticoagulants in the 1940s, subcutaneous injections of LDUH in 1962 and subcutaneous injections of LMWH in 1982. 1974 was when vascular inflammation and venous thrombosis were first proposed to be interrelated. For around 50 years, a months-long warfarin (Coumadin) regimen was the mainstay of pharmacological treatment. To avoid the blood monitoring required with warfarin and the injections required by heparin and heparin-like medicines, direct oral anticoagulants (DOACs) were developed. In the late 2000s to early 2010s, DOACs—including rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa)—came to the market. ''The New York Times'' described a "furious battle" among the three makers of these drugs "for the prescription pads of doctors".
pulmonary artery
A pulmonary artery is an artery in the pulmonary circulation that carries deoxygenated blood from the right side of the heart to the lungs. The largest pulmonary artery is the ''main pulmonary artery'' or ''pulmonary trunk'' from the heart, and ...
that supplies blood to the lungs. This is called a pulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing ...
(PE). DVT and PE comprise the cardiovascular disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, ...
of venous thromboembolism (VTE). About two-thirds of VTE manifests as DVT only, with one-third manifesting as PE with or without DVT. The most frequent long-term DVT complication is post-thrombotic syndrome, which can cause pain, swelling, a sensation of heaviness, itching, and in severe cases, ulcers
An ulcer is a discontinuity or break in a bodily membrane that impedes normal function of the affected organ. According to Robbins's pathology, "ulcer is the breach of the continuity of skin, epithelium or mucous membrane caused by sloughing o ...
. Recurrent VTE occurs in about 30% of those in the ten years following an initial VTE.
The mechanism behind DVT formation typically involves some combination of decreased blood flow, increased tendency to clot, changes to the blood vessel wall, and inflammation. Risk factors include recent surgery, older age, active cancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bl ...
, obesity
Obesity is a medical condition, sometimes considered a disease, in which excess body fat has accumulated to such an extent that it may negatively affect health. People are classified as obese when their body mass index (BMI)—a person's ...
, infection, inflammatory diseases, antiphospholipid syndrome
Antiphospholipid syndrome, or antiphospholipid antibody syndrome (APS or APLS), is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS provokes blood clots ( thrombosis) in both arteries and veins as well as pregna ...
, personal history and family history
Genealogy () is the study of families, family history, and the tracing of their lineages. Genealogists use oral interviews, historical records, genetic analysis, and other records to obtain information about a family and to demonstrate kinsh ...
of VTE, trauma, injuries, lack of movement, hormonal birth control
Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones, although in India one selective estrogen receptor modulator is marketed as a contraceptive. The orig ...
, pregnancy
Pregnancy is the time during which one or more offspring develops ( gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.
Pregnancy usually occurs by sexual intercourse, but ...
, and the period following birth. VTE has a strong genetic component, accounting for approximately 50 to 60% of the variability in VTE rates. Genetic factors include non-O blood type
A blood type (also known as a blood group) is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrat ...
, deficiencies of antithrombin, protein C
Protein C, also known as autoprothrombin IIA and blood coagulation factor XIX, is a zymogen, that is, an inactive enzyme. The activated form plays an important role in regulating anticoagulation, inflammation, and cell death and maintain ...
, and protein S
Protein S (also known as PROS) is a vitamin K-dependent plasma glycoprotein synthesized in the liver. In the circulation, Protein S exists in two forms: a free form and a complex form bound to complement protein C4b-binding protein (C4BP). In ...
and the mutations of factor V Leiden and prothrombin G20210A. In total, dozens of genetic risk factors have been identified.
People suspected of having DVT can be assessed using a prediction rule such as the Wells score. A D-dimer test can also be used to assist with excluding the diagnosis or to signal a need for further testing. Diagnosis is most commonly confirmed by ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies fr ...
of the suspected veins. VTE becomes much more common with age. The condition is rare in children, but occurs in almost 1% of those ≥ age 85 annually. Asian, Asian-American, Native American, and Hispanic individuals have a lower VTE risk than Whites or Blacks. Populations in Asia have VTE rates at 15 to 20% of what is seen in Western countries.
Using blood thinners
Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where t ...
is the standard treatment. Typical medications include rivaroxaban, apixaban, and warfarin
Warfarin, sold under the brand name Coumadin among others, is a medication that is used as an anticoagulant (blood thinner). It is commonly used to prevent blood clots such as deep vein thrombosis and pulmonary embolism, and to prevent ...
. Beginning warfarin treatment requires an additional non-oral anticoagulant, often injections of heparin
Heparin, also known as unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. Since heparins depend on the activity of antithrombin, they are considered anticoagulants. Specifically it is also used in the trea ...
. Guyatt et al. 2012, p. 20S: 2.4. Prevention of VTE for the general population includes avoiding obesity and maintaining an active lifestyle. Preventive efforts following low-risk surgery include early and frequent walking. Riskier surgeries generally prevent VTE with a blood thinner or aspirin
Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and/or inflammation, and as an antithrombotic. Specific inflammatory conditions which aspirin is used to treat in ...
combined with intermittent pneumatic compression.
Signs and symptoms
 Symptoms classically affect a leg and typically develop over hours or days, though they can develop suddenly or over a matter of weeks. The legs are primarily affected, with 4–10% of DVT occurring in the arms. Despite the signs and symptoms being highly variable, the typical symptoms are pain, swelling, and redness. However, these symptoms might not manifest in the lower limbs of those unable to walk. In those who are able to walk, DVT can reduce one's ability to do so. The pain can be described as throbbing and can worsen with weight-bearing, prompting one to bear more weight with the unaffected leg. Additional signs and symptoms include tenderness, pitting edema (''see image''), dilation of surface veins, warmth, discoloration, a "pulling sensation", and even
Symptoms classically affect a leg and typically develop over hours or days, though they can develop suddenly or over a matter of weeks. The legs are primarily affected, with 4–10% of DVT occurring in the arms. Despite the signs and symptoms being highly variable, the typical symptoms are pain, swelling, and redness. However, these symptoms might not manifest in the lower limbs of those unable to walk. In those who are able to walk, DVT can reduce one's ability to do so. The pain can be described as throbbing and can worsen with weight-bearing, prompting one to bear more weight with the unaffected leg. Additional signs and symptoms include tenderness, pitting edema (''see image''), dilation of surface veins, warmth, discoloration, a "pulling sensation", and even cyanosis
Cyanosis is the change of body tissue color to a bluish-purple hue as a result of having decreased amounts of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Body tissues that show cyanosis are usually in locations ...
(a blue or purplish discoloration) with fever. DVT can also exist without causing any symptoms. Signs and symptoms help in determining the likelihood of DVT, but they are not used alone for diagnosis.
At times, DVT can cause symptoms in both arms or both legs, as with bilateral DVT. Rarely, a clot in the inferior vena cava
The inferior vena cava is a large vein that carries the deoxygenated blood from the lower and middle body into the right atrium of the heart. It is formed by the joining of the right and the left common iliac veins, usually at the level of th ...
can cause both legs to swell. Superficial vein thrombosis, also known as superficial thrombophlebitis
Superficial thrombophlebitis is a thrombosis and inflammation of superficial veins which presents as a painful induration with erythema, often in a linear or branching configuration forming cords.
Superficial thrombophlebitis is due to inflammat ...
, is the formation of a blood clot (thrombus) in a vein close to the skin. It can co-occur with DVT and can be felt as a "palpable cord". Migratory thrombophlebitis (Trousseau's syndrome) is a noted finding in those with pancreatic cancer
Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of panc ...
and is associated with DVT.
Acute complications
Apulmonary embolism
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing ...
(PE) occurs when a blood clot from a deep vein (a DVT) detaches from a vein ( embolizes), travels through the right side of the heart, and becomes lodged as an embolus in a pulmonary artery
A pulmonary artery is an artery in the pulmonary circulation that carries deoxygenated blood from the right side of the heart to the lungs. The largest pulmonary artery is the ''main pulmonary artery'' or ''pulmonary trunk'' from the heart, and ...
that supplies deoxygenated blood to the lungs for oxygenation. Up to one-fourth of PE cases are thought to result in sudden death. When not fatal, PE can cause symptoms such as sudden onset shortness of breath
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing di ...
or chest pain
Chest pain is pain or discomfort in the chest, typically the front of the chest. It may be described as sharp, dull, pressure, heaviness or squeezing. Associated symptoms may include pain in the shoulder, arm, upper abdomen, or jaw, along with ...
, coughing up blood (hemoptysis
Hemoptysis is the coughing up of blood or blood-stained mucus from the bronchi, larynx, trachea, or lungs. In other words, it is the airway bleeding. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia ...
), and fainting ( syncope). The chest pain can be pleuritic (worsened by deep breaths) and can vary based upon where the embolus is lodged in the lungs. An estimated 30–50% of those with PE have detectable DVT by compression ultrasound.
A rare and massive DVT that causes significant obstruction and discoloration (including cyanosis) is phlegmasia cerulea dolens
Phlegmasia cerulea dolens (PCD) (literally: 'painful blue inflammation'), not to be confused with preceding phlegmasia alba dolens, is an uncommon severe form of lower extremity deep venous thrombosis (DVT) that obstructs blood outflow from a vei ...
. It is life-threatening, limb-threatening, and carries a risk of venous gangrene
Gangrene is a type of tissue death caused by a lack of blood supply. Symptoms may include a change in skin color to red or black, numbness, swelling, pain, skin breakdown, and coolness. The feet and hands are most commonly affected. If the gan ...
. Phlegmasia cerulea dolens can occur in the arm but more commonly affects the leg. If found in the setting of acute compartment syndrome, an urgent fasciotomy is warranted to protect the limb. Superior vena cava syndrome is a rare complication of arm DVT.
DVT is thought to be able to cause a stroke in the presence of a heart defect. This is called a paradoxical embolism because the clot abnormally travels from the pulmonary circuit to the systemic circuit while inside the heart. The defect of a patent foramen ovale
Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria (upper chambers) of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this do ...
is thought to allow clots to travel through the interatrial septum from the right atrium
The atrium ( la, ātrium, , entry hall) is one of two upper chambers in the heart that receives blood from the circulatory system. The blood in the atria is pumped into the heart ventricles through the atrioventricular valves.
There are two a ...
into the left atrium.
Differential diagnosis
In most suspected cases, DVT is ruled out after evaluation.Cellulitis
Cellulitis is usually a bacterial infection involving the inner layers of the skin. It specifically affects the dermis and subcutaneous fat. Signs and symptoms include an area of redness which increases in size over a few days. The borders of ...
is a frequent mimic of DVT, with its triad
Triad or triade may refer to:
* a group of three
Businesses and organisations
* Triad (American fraternities), certain historic groupings of seminal college fraternities in North America
* Triad (organized crime), a Chinese transnational orga ...
of pain, swelling, and redness. Symptoms concerning for DVT are more often due to other causes, including cellulitis, ruptured Baker's cyst, hematoma
A hematoma, also spelled haematoma, or blood suffusion is a localized bleeding outside of blood vessels, due to either disease or trauma including injury or surgery and may involve blood continuing to seep from broken capillaries. A hematoma is ...
, lymphedema, and chronic venous insufficiency. Other differential diagnoses include tumors, venous or arterial aneurysm
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus ...
s, connective tissue disorders, superficial vein thrombosis, muscle vein thrombosis, and varicose veins.
Classification
 DVT and PE are the two manifestations of the
DVT and PE are the two manifestations of the cardiovascular disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, ...
venous thromboembolism (VTE). VTE can occur as DVT only, DVT with PE, or PE only. About two-thirds of VTE manifests as DVT only, with one-third manifesting as PE with or without DVT. VTE, along with superficial vein thrombosis, are common types of venous thrombosis.
DVT is classified as acute when the clots are developing or have recently developed, whereas chronic DVT persists more than 28 days. Differences between these two types of DVT can be seen with ultrasound. An episode of VTE after an initial one is classified as recurrent. Bilateral DVT refers to clots in both limbs while unilateral means only a single limb is affected.
DVT in the legs is proximal
Standard anatomical terms of location are used to unambiguously describe the anatomy of animals, including humans. The terms, typically derived from Latin or Greek roots, describe something in its standard anatomical position. This position ...
when above the knee and distal (or calf) when below the knee. DVT below the popliteal vein, a proximal vein behind the knee, is classified as distaland has limited clinical significance compared to proximal DVT. Calf DVT makes up about half of DVTs. Iliofemoral DVT has been described as involving either the iliac or common femoral vein; elsewhere, it has been defined as involving at a minimum the
common iliac vein
In human anatomy, the common iliac veins are formed by the external iliac veins and internal iliac veins. The left and right common iliac veins come together in the abdomen at the level of the fifth lumbar vertebra, forming the inferior vena ...
, which is near the top of the pelvis.
DVT can be classified into provoked and unprovoked categories. For example, DVT that occurs in association with cancer or surgery can be classified as provoked. However, the European Society of Cardiology in 2019 urged for this dichotomy to be abandoned to encourage more personalized risk assessments for recurrent VTE. The distinction between these categories is not always clear.
Causes
 Traditionally, the three factors of
Traditionally, the three factors of Virchow's triad
Virchow's triad or the triad of Virchow () describes the three broad categories of factors that are thought to contribute to thrombosis.
*Hypercoagulability
* Hemodynamic changes (stasis, turbulence)
* Endothelial injury/dysfunction
It is named ...
— venous stasis, hypercoagulability
Thrombophilia (sometimes called hypercoagulability or a prothrombotic state) is an abnormality of blood coagulation that increases the risk of thrombosis (blood clots in blood vessels). Such abnormalities can be identified in 50% of people who ...
, and changes in the endothelial blood vessel lining—contribute to VTE and were used to explain its formation. More recently, inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
has been identified as playing a clear causal role. Other related causes include activation of immune system
The immune system is a network of biological processes that protects an organism from diseases. It detects and responds to a wide variety of pathogens, from viruses to parasitic worms, as well as Tumor immunology, cancer cells and objects such ...
components, the state of microparticle
Microparticles are particles between 0.1 and 100 μm in size. Commercially available microparticles are available in a wide variety of materials, including ceramics, glass, polymers, and metals. Microparticles encountered in daily life includ ...
s in the blood, the concentration of oxygen, and possible platelet
Platelets, also called thrombocytes (from Greek θρόμβος, "clot" and κύτος, "cell"), are a component of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping, thereby i ...
activation. Various risk factors contribute to VTE, including genetic and environmental factors, though many with multiple risk factors never develop it.
Acquired risk factors include the strong risk factor of older age, which alters blood composition to favor clotting. Previous VTE, particularly unprovoked VTE, is a strong risk factor. A leftover clot from a prior DVT increases the risk of a subsequent DVT. Major surgery and trauma increase risk because of tissue factor from outside the vascular system entering the blood. Minor injuries, lower limb amputation, hip fracture
A hip fracture is a break that occurs in the upper part of the femur (thigh bone). Symptoms may include pain around the hip, particularly with movement, and shortening of the leg. Usually the person cannot walk.
They most often occur as a re ...
, and long bone fractures are also risks. In orthopedic surgery
Orthopedic surgery or orthopedics ( alternatively spelt orthopaedics), is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal ...
, venous stasis can be temporarily provoked by a cessation of blood flow as part of the procedure. Inactivity and immobilization contribute to venous stasis, as with orthopedic cast
An orthopedic cast, or simply cast, is a shell, frequently made from plaster or fiberglass, that encases a limb (or, in some cases, large portions of the body) to stabilize and hold anatomical structures—most often a broken bone (or bones), i ...
s, paralysis, sitting, long-haul travel, bed rest, hospitalization, catatonia
Catatonia is a complex neuropsychiatric behavioral syndrome that is characterized by abnormal movements, immobility, abnormal behaviors, and withdrawal. The onset of catatonia can be acute or subtle and symptoms can wax, wane, or change during ...
, and in survivors of acute stroke. Conditions that involve compromised blood flow in the veins are May–Thurner syndrome, where a vein of the pelvis is compressed, and venous thoracic outlet syndrome, which includes Paget–Schroetter syndrome, where compression occurs near the base of the neck.
Infections, including sepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is foll ...
, COVID-19
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by a virus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first known case was identified in Wuhan, China, in December 2019. The disease quickl ...
, HIV
The human immunodeficiency viruses (HIV) are two species of '' Lentivirus'' (a subgroup of retrovirus) that infect humans. Over time, they cause acquired immunodeficiency syndrome (AIDS), a condition in which progressive failure of the immu ...
, and active tuberculosis
Tuberculosis (TB) is an infectious disease usually caused by ''Mycobacterium tuberculosis'' (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, in w ...
, increase risk. Chronic inflammatory diseases and some autoimmune disease
An autoimmune disease is a condition arising from an abnormal immune response to a functioning body part. At least 80 types of autoimmune diseases have been identified, with some evidence suggesting that there may be more than 100 types. Nearly ...
s, such as inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, Crohn's disease and ulcerative colitis being the principal types. Crohn's disease affects the small intestine and large intestine, as wel ...
, systemic sclerosis
Systemic scleroderma, or systemic sclerosis, is an autoimmune rheumatic disease characterised by excessive production and accumulation of collagen, called fibrosis, in the skin and internal organs and by injuries to small arteries. There are tw ...
, Behçet's syndrome, primary antiphospholipid syndrome
Antiphospholipid syndrome, or antiphospholipid antibody syndrome (APS or APLS), is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS provokes blood clots ( thrombosis) in both arteries and veins as well as pregna ...
, and systemic lupus erythematosus
Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Comm ...
(SLE) increase risk. SLE itself is frequently associated with secondary antiphospholipid syndrome.
Cancer can grow in and around veins, causing venous stasis, and can also stimulate increased levels of tissue factor. Cancers of the blood, lung, pancreas, brain, stomach, and bowel are associated with high VTE risk. Solid tumors such as adenocarcinoma
Adenocarcinoma (; plural adenocarcinomas or adenocarcinomata ) (AC) is a type of cancerous tumor that can occur in several parts of the body. It is defined as neoplasia of epithelial tissue that has glandular origin, glandular characteristics, o ...
s can contribute to both VTE and disseminated intravascular coagulation. In severe cases, this can lead to simultaneous clotting and bleeding. Chemotherapy
Chemotherapy (often abbreviated to chemo and sometimes CTX or CTx) is a type of cancer treatment that uses one or more anti-cancer drugs (chemotherapeutic agents or alkylating agents) as part of a standardized chemotherapy regimen. Chemothe ...
treatment also increases risk. Obesity increases the potential of blood to clot, as does pregnancy. In the postpartum, placenta
The placenta is a temporary embryonic and later fetal organ (anatomy), organ that begins embryonic development, developing from the blastocyst shortly after implantation (embryology), implantation. It plays critical roles in facilitating nutrien ...
l tearing releases substances that favor clotting. Oral contraceptives and hormonal replacement therapy
Hormone replacement therapy (HRT), also known as menopausal hormone therapy or postmenopausal hormone therapy, is a form of hormone therapy used to treat symptoms associated with female menopause. These symptoms can include hot flashes, vagina ...
increase the risk through a variety of mechanisms, including altered blood coagulation protein levels and reduced fibrinolysis.
 Dozens of genetic risk factors have been identified, and they account for approximately 50 to 60% of the variability in VTE rates. As such,
Dozens of genetic risk factors have been identified, and they account for approximately 50 to 60% of the variability in VTE rates. As such, family history
Genealogy () is the study of families, family history, and the tracing of their lineages. Genealogists use oral interviews, historical records, genetic analysis, and other records to obtain information about a family and to demonstrate kinsh ...
of VTE is a risk factor for a first VTE. Factor V Leiden, which makes factor V resistant to inactivation by activated protein C, mildly increases VTE risk by about three times. Deficiencies of three proteins that normally prevent blood from clotting—protein C
Protein C, also known as autoprothrombin IIA and blood coagulation factor XIX, is a zymogen, that is, an inactive enzyme. The activated form plays an important role in regulating anticoagulation, inflammation, and cell death and maintain ...
, protein S
Protein S (also known as PROS) is a vitamin K-dependent plasma glycoprotein synthesized in the liver. In the circulation, Protein S exists in two forms: a free form and a complex form bound to complement protein C4b-binding protein (C4BP). In ...
, and antithrombin—contribute to VTE. These deficiencies in antithrombin, protein C
Protein C, also known as autoprothrombin IIA and blood coagulation factor XIX, is a zymogen, that is, an inactive enzyme. The activated form plays an important role in regulating anticoagulation, inflammation, and cell death and maintain ...
, and protein S
Protein S (also known as PROS) is a vitamin K-dependent plasma glycoprotein synthesized in the liver. In the circulation, Protein S exists in two forms: a free form and a complex form bound to complement protein C4b-binding protein (C4BP). In ...
are rare but strong, or moderately strong, risk factors. They increase risk by about 10 times. Having a non-O blood type roughly doubles VTE risk. Non-O blood type is common globally, making it an important risk factor. Individuals without O blood type have higher blood levels of von Willebrand factor and factor VIII
Factor VIII (FVIII) is an essential blood-clotting protein, also known as anti-hemophilic factor (AHF). In humans, factor VIII is encoded by the ''F8'' gene. Defects in this gene result in hemophilia A, a recessive X-linked coagulation disorder ...
than those with O blood type, increasing the likelihood of clotting. Those homozygous
Zygosity (the noun, zygote, is from the Greek "yoked," from "yoke") () is the degree to which both copies of a chromosome or gene have the same genetic sequence. In other words, it is the degree of similarity of the alleles in an organism.
Mo ...
for the common fibrinogen gamma gene
Fibrinogen gamma chain, also known as fibrinogen gamma gene (FGG), is a human gene found on chromosome 4.
The protein encoded by this gene is the gamma component of fibrinogen, a blood-borne glycoprotein composed of three pairs of nonidentical po ...
variant rs2066865 have about a 1.6 times higher risk of VTE. The genetic variant prothrombin G20210A, which increases prothrombin levels, increases risk by about 2.5 times. Additionally, approximately 5% of people have been identified with a background genetic risk comparable to the factor V Leiden and prothrombin G20210A mutations.
Blood alterations including dysfibrinogenemia, low free protein S, activated protein C resistance, homocystinuria, hyperhomocysteinemia, high fibrinogen
Fibrinogen (factor I) is a glycoprotein complex, produced in the liver, that circulates in the blood of all vertebrates. During tissue and vascular injury, it is converted enzymatically by thrombin to fibrin and then to a fibrin-based blood ...
levels, high factor IX levels, and high factor XI levels are associated with increased risk. Other associated conditions include heparin-induced thrombocytopenia, catastrophic antiphospholipid syndrome
Catastrophic antiphospholipid syndrome (CAPS), also known as Asherson's syndrome, is a rare autoimmune disease in which widespread, intravascular clotting causes multi-organ failure. The syndrome is caused by antiphospholipid antibodies that targe ...
, paroxysmal nocturnal hemoglobinuria, nephrotic syndrome, chronic kidney disease
Chronic kidney disease (CKD) is a type of kidney disease in which a gradual loss of kidney function occurs over a period of months to years. Initially generally no symptoms are seen, but later symptoms may include leg swelling, feeling tired, ...
, polycythemia vera, essential thrombocythemia, intravenous drug use, and smoking.
Some risk factors influence the location of DVT within the body. In isolated distal DVT, the profile of risk factors appears distinct from proximal DVT. Transient factors, such as surgery and immobilization, appear to dominate, whereas thrombophilias and age do not seem to increase risk. Common risk factors for having an upper extremity DVT include having an existing foreign body (such as a central venous catheter, a pacemaker, or a triple-lumen PICC line), cancer, and recent surgery.
Pathophysiology
 Blood has a natural tendency to clot when blood vessels are damaged (
Blood has a natural tendency to clot when blood vessels are damaged (hemostasis
In biology, hemostasis or haemostasis is a process to prevent and stop bleeding, meaning to keep blood within a damaged blood vessel (the opposite of hemostasis is hemorrhage). It is the first stage of wound healing. This involves coagulation, wh ...
) to minimize blood loss. Clotting is activated by the coagulation cascade
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanis ...
and the clearing of clots that are no longer needed is accomplished by the process of fibrinolysis. Reductions in fibrinolysis or increases in coagulation can increase the risk of DVT.
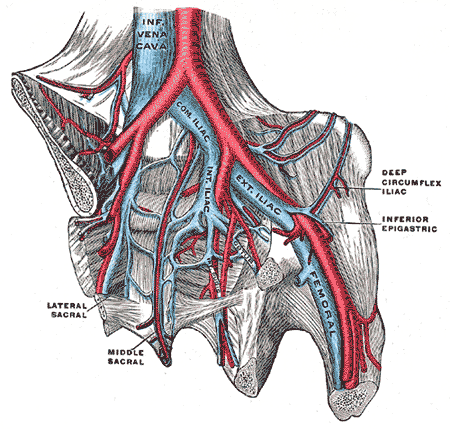
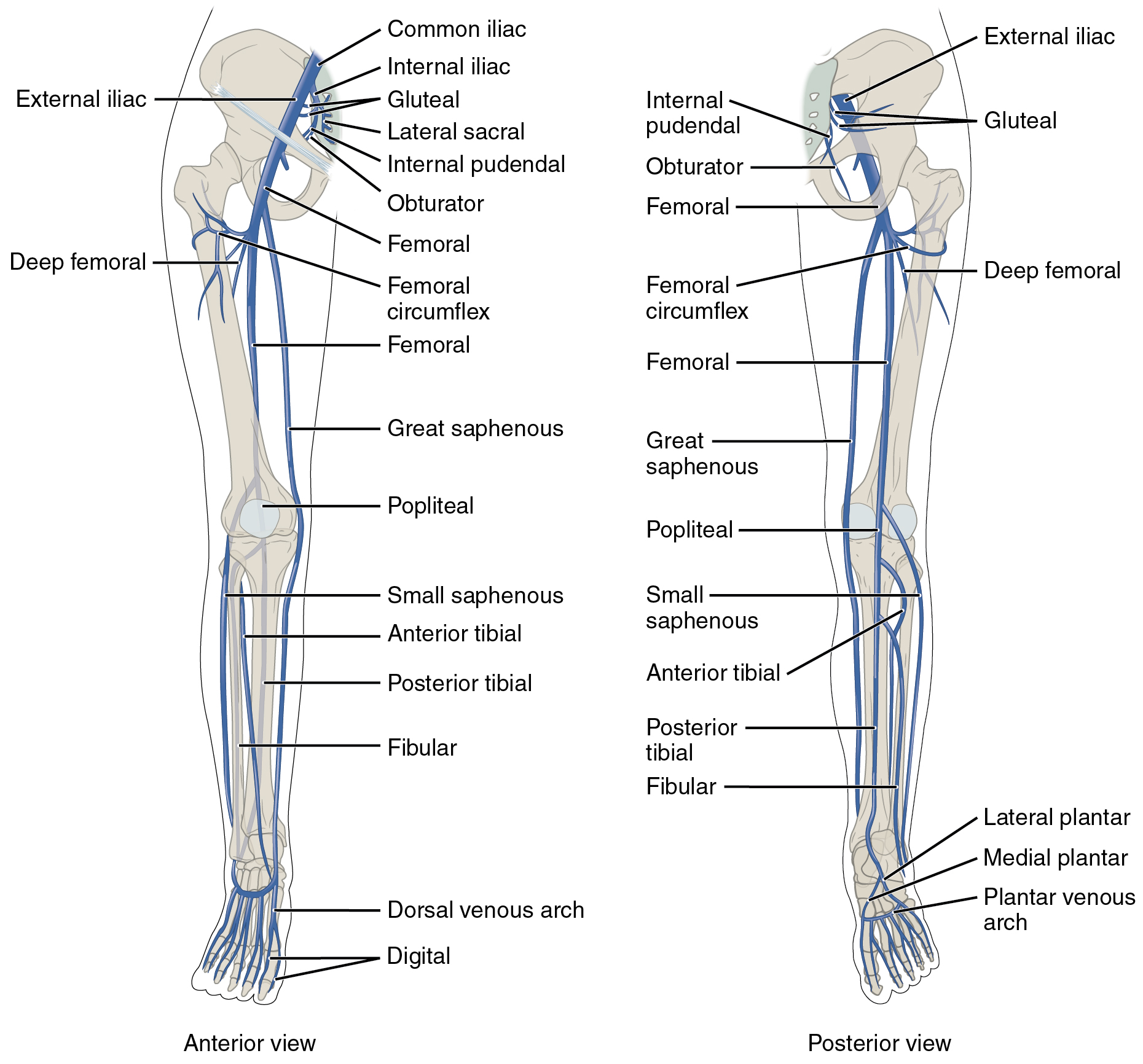
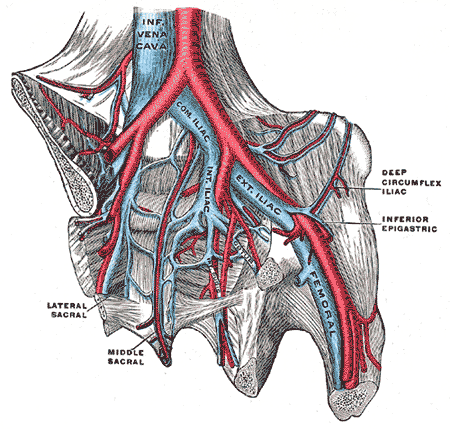
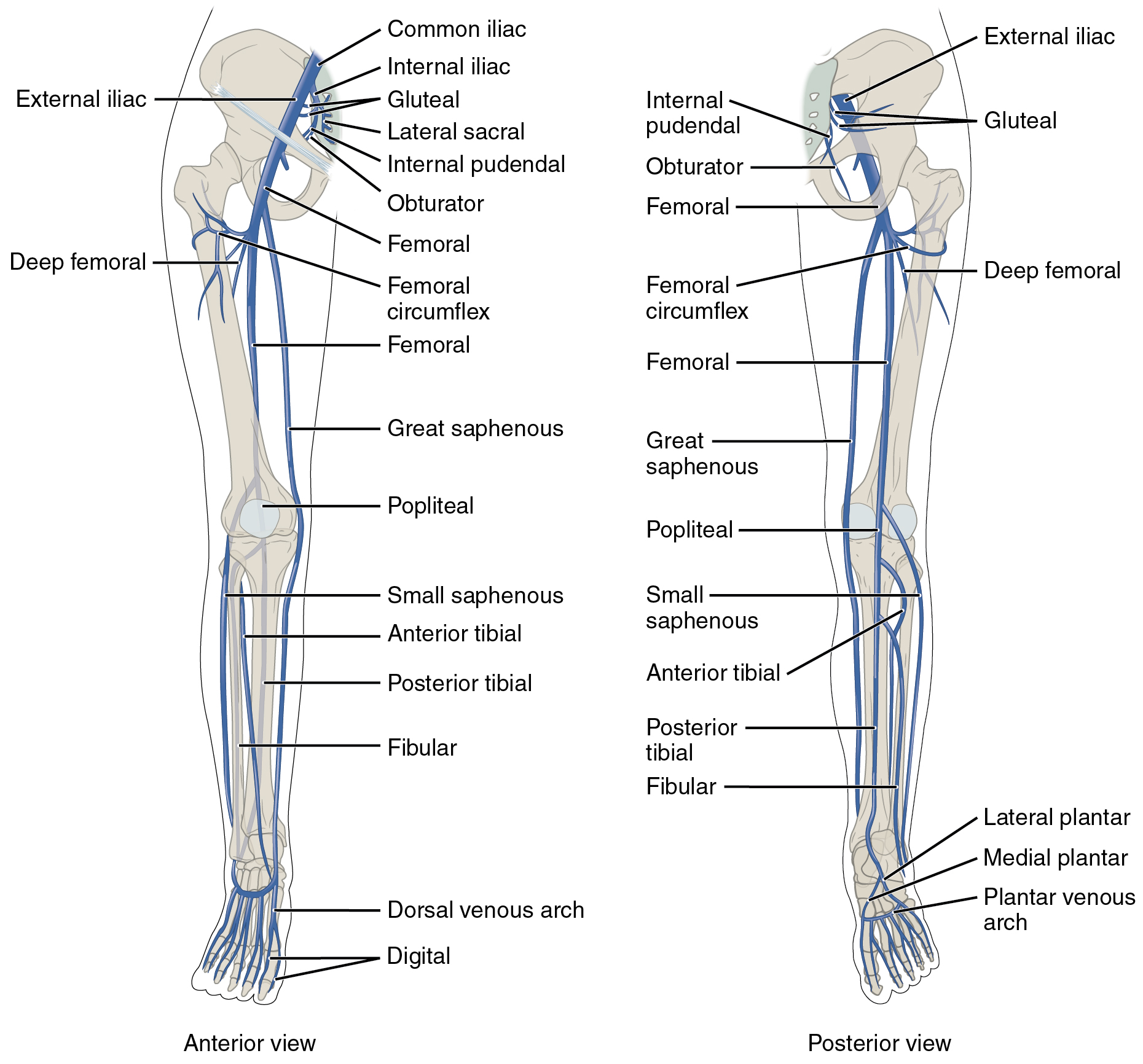
DVT often develops in the calf veins and "grows" in the direction of venous flow, towards the heart. DVT most frequently affects veins in the leg or pelvis including the popliteal vein (behind the knee), femoral vein (of the thigh), and iliac veins of the pelvis. Extensive lower-extremity DVT can even reach into the inferior vena cava
The inferior vena cava is a large vein that carries the deoxygenated blood from the lower and middle body into the right atrium of the heart. It is formed by the joining of the right and the left common iliac veins, usually at the level of th ...
(in the abdomen). Upper extremity DVT most commonly affects the subclavian, axillary, and jugular vein
The jugular veins are veins that take deoxygenated blood from the head back to the heart via the superior vena cava. The internal jugular vein descends next to the internal carotid artery and continues posteriorly to the sternocleidomast ...
s.
The process of fibrinolysis, where DVT clots can be dissolved back into the blood, acts to temper the process of thrombus growth. This is the preferred process. Aside from the potentially deadly process of embolization, a clot can resolve through organization, which can damage the valves of veins, cause vein fibrosis, and result in non-compliant veins. Organization of a thrombus into the vein can occur at the third stage of its pathological development, in which collagen becomes the characteristic component. The first pathological stage is marked by red blood cells, and the second is characterized by medium-textured fibrin.
 In arterial thrombosis, blood vessel wall damage is required, as it initiates
In arterial thrombosis, blood vessel wall damage is required, as it initiates coagulation
Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanis ...
, but clotting in the veins mostly occurs without any such mechanical damage. The beginning of venous thrombosis is thought to arise from "activation of endothelial cells, platelets, and leukocytes, with initiation of inflammation and formation of microparticles that trigger the coagulation system" via tissue factor. Vein wall inflammation is likely the inciting event. Importantly, the activated endothelium Endothelial activation is a proinflammatory and procoagulant state of the endothelial cells lining the lumen of blood vessels. It is most characterized by an increase in interactions with white blood cells (leukocytes), and it is associated with th ...
of veins interacts with circulating white blood cells (leukocytes). While leukocytes normally help prevent blood from clotting (as does normal endothelium), upon stimulation, leukocytes facilitate clotting. Neutrophils are recruited early in the process of venous thrombi formation. They release pro-coagulant granules and neutrophil extracellular traps
Neutrophil extracellular traps (NETs) are networks of extracellular fibers, primarily composed of DNA from neutrophils, which bind pathogens. Neutrophils are the immune system's first line of defense against infection and have conventionally b ...
(NETs) or their components, which play a role in venous thrombi formation. NET components are pro-thrombotic through both the intrinsic and extrinsic coagulation pathways. NETs provide "a scaffold for adhesion" of platelets, red blood cells, and multiple factors that potentiate platelet activation. In addition to the pro-coagulant activities of neutrophils, multiple stimuli cause monocytes
Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and conventional dendritic cells. As a part of the vertebrate innate immune system monocytes also infl ...
to release tissue factor. Monocytes are also recruited early in the process.
Tissue factor, via the tissue factor– factor VIIa complex, activates the extrinsic pathway of coagulation and leads to conversion of prothrombin to thrombin, followed by fibrin deposition. Fresh venous clots are red blood cell
Red blood cells (RBCs), also referred to as red cells, red blood corpuscles (in humans or other animals not having nucleus in red blood cells), haematids, erythroid cells or erythrocytes (from Greek ''erythros'' for "red" and ''kytos'' for "holl ...
and fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with pla ...
rich. Platelets and white blood cell
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mult ...
s are also components. Platelets are not as prominent in venous clots as they are in arterial ones, but they can play a role. In cancer, tissue factor is produced by cancer cells. Cancer also produces unique substances that stimulate factor Xa, cytokines that promote endothelial dysfunction, and plasminogen activator inhibitor-1
Plasminogen activator inhibitor-1 (PAI-1) also known as endothelial plasminogen activator inhibitor or serpin E1 is a protein that in humans is encoded by the ''SERPINE1'' gene. Elevated PAI-1 is a risk factor for thrombosis and atherosclerosis
P ...
, which inhibits the breakdown of clots (fibrinolysis).
Often, DVT begins in the valves of veins. The blood flow pattern in the valves can cause low oxygen concentrations in the blood (hypoxemia
Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the bod ...
) of a valve sinus. Hypoxemia, which is worsened by venous stasis, activates pathways—ones that include hypoxia-inducible factor-1
Hypoxia-inducible factors (HIFs) are transcription factors that respond to decreases in available oxygen in the cellular environment, or hypoxia. They are only present in parahoxozoan animals.
Discovery
The HIF transcriptional complex wa ...
and early-growth-response protein 1
EGR-1 (Early growth response protein 1) also known as ZNF268 (zinc finger protein 268) or NGFI-A (nerve growth factor-induced protein A) is a protein that in humans is encoded by the ''EGR1'' gene.
EGR-1 is a mammalian transcription factor. It ...
. Hypoxemia also results in the production of reactive oxygen species
In chemistry, reactive oxygen species (ROS) are highly reactive chemicals formed from diatomic oxygen (). Examples of ROS include peroxides, superoxide, hydroxyl radical, singlet oxygen, and alpha-oxygen.
The reduction of molecular oxygen ...
, which can activate these pathways, as well as nuclear factor-κB
Nuclear may refer to:
Physics
Relating to the nucleus of the atom:
*Nuclear engineering
*Nuclear physics
*Nuclear power
*Nuclear reactor
*Nuclear weapon
*Nuclear medicine
*Radiation therapy
*Nuclear warfare
Mathematics
*Nuclear space
*Nuclear ...
, which regulates hypoxia-inducible factor-1 transcription. Hypoxia-inducible factor-1 and early-growth-response protein 1 contribute to monocyte association with endothelial proteins, such as P-selectin, prompting monocytes to release tissue factor-filled microvesicles, which presumably begin clotting after binding to the endothelial surface.
D-dimers are a fibrin degradation product, a natural byproduct of fibrinolysis that is typically found in the blood. An elevated level can result from plasmin
Plasmin is an important enzyme () present in blood that degrades many blood plasma proteins, including fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein (in the zymogen form of plasminogen) is encode ...
dissolving a clot—or other conditions. Hospitalized patients often have elevated levels for multiple reasons. Anticoagulation, the standard treatment for DVT, prevents further clot growth and PE, but does not act directly on existing clots.
Diagnosis
Aclinical probability assessment A clinical prediction rule or clinical probability assessment specifies how to use medical signs, symptoms, and other findings to estimate the probability of a specific disease or clinical outcome.
Physicians have difficulty in estimated risks of ...
using the Wells score (see column in the table below) to determine if a potential DVT is "likely" or "unlikely" is typically the first step of the diagnostic process. The score is used in suspected first lower extremity DVT (without any PE symptoms) in primary care and outpatient settings, including the emergency department. The numerical result (possible score −2 to 9) is most commonly grouped into either "unlikely" or "likely" categories. A Wells score of two or more means DVT is considered "likely" (about a 28% chance), while those with a lower score are considered "unlikely" to have DVT (about a 6% chance). In those unlikely to have DVT, a diagnosis is excluded by a negative D-dimer blood test. In people with likely DVT, ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies fr ...
is the standard imaging
Imaging is the representation or reproduction of an object's form; especially a visual representation (i.e., the formation of an image).
Imaging technology is the application of materials and methods to create, preserve, or duplicate images.
...
used to confirm or exclude a diagnosis. Imaging is also needed for hospital inpatients with suspected DVT and those initially categorized as unlikely to have DVT but who have a positive D-dimer test.
While the Wells score is the predominant and most studied clinical prediction rule for DVT, it does have drawbacks. The Wells score requires a subjective assessment regarding the likelihood of an alternate diagnosis and performs less well in the elderly and those with a prior DVT. The Dutch Primary Care Rule has also been validated for use. It contains only objective criteria but requires obtaining a D-dimer value. With this prediction rule, three points or less means a person is at low risk for DVT. A result of four or more points indicates an ultrasound is needed. Instead of using a prediction rule, experienced physicians can make a DVT pre-test probability assessment using clinical assessment and gestalt, but prediction rules are more reliable.
Compression ultrasonography for suspected deep vein thrombosis
Ultrasonography in suspected deep vein thrombosis focuses primarily on the femoral vein and the popliteal vein, because thrombi in these veins are associated with the greatest risk of harmful pulmonary embolism.
Medical uses
The risk of d ...
is the standard diagnostic method, and it is highly sensitive for detecting an initial DVT. A compression ultrasound is considered positive when the vein walls of normally compressible veins do not collapse under gentle pressure. Clot visualization is sometimes possible, but is not required. Three compression ultrasound scanning techniques can be used, with two of the three methods requiring a second ultrasound some days later to rule out the diagnosis. Whole-leg ultrasound is the option that does not require a repeat ultrasound, but proximal compression ultrasound is frequently used because distal DVT is only rarely clinically significant. Ultrasound methods including duplex
Duplex (Latin, 'double') may refer to:
Arts and entertainment
* ''Duplex'' (film), or ''Our House'', a 2003 American black comedy film
* Duplex (band), a Dutch electronic music duo
* Duplex (Norwegian duo)
* Duplex!, a Canadian children's music ...
and color flow Doppler
Doppler ultrasonography is medical ultrasonography that employs the Doppler effect to perform imaging of the movement of tissues and body fluids (usually blood), and their relative velocity to the probe. By calculating the frequency shift of a ...
can be used to further characterize the clot and Doppler ultrasound is especially helpful in the non-compressible iliac veins.
CT scan venography
Computed tomography angiography (also called CT angiography or CTA) is a computed tomography technique used for angiography—the visualization of arteries and veins—throughout the human body. Using contrast injected into the blood vessels, im ...
, MRI venography, or a non-contrast MRI are also diagnostic possibilities. The gold standard
A gold standard is a Backed currency, monetary system in which the standard economics, economic unit of account is based on a fixed quantity of gold. The gold standard was the basis for the international monetary system from the 1870s to the ...
for judging imaging methods is contrast venography, which involves injecting a peripheral vein of the affected limb with a contrast agent and taking X-rays, to reveal whether the venous supply has been obstructed. Because of its cost, invasiveness, availability, and other limitations, this test is rarely performed.
Doppler ultrasonography
Doppler ultrasonography is medical ultrasonography that employs the Doppler effect to perform imaging of the movement of tissues and body fluids (usually blood), and their relative velocity to the probe. By calculating the frequency shift of ...
showing absence of flow and hyperechogenic content in a clotted femoral vein (labeled subsartorial) distal to the branching point of the deep femoral vein
The profunda femoris vein (or deep femoral vein) is a large deep vein in the thigh. It collects blood from the inner thigh, passing superiorly and medially alongside the profunda femoris artery before emptying into the femoral vein.
Anatomy
...
. When compared to this clot, clots that instead obstruct the common femoral vein (proximal to this branching point) cause more severe effects due to impacting a significantly larger portion of the leg.
Iliac vein deep vein thrombosis.JPEG, An abdominal CT scan demonstrating an iliofemoral DVT, with the clot in the right common iliac vein of the pelvis
Management
Treatment for DVT is warranted when the clots are either proximal, distal and symptomatic, or upper extremity and symptomatic. Providing anticoagulation, or blood-thinning medicine, is the typical treatment after patients are checked to make sure they are not subject tobleeding
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vag ...
. However, treatment varies depending upon the location of DVT. For example, in cases of isolated distal DVT, ultrasound surveillance (a second ultrasound after 2 weeks to check for proximal clots), might be used instead of anticoagulation. Although, those with isolated distal DVT at a high-risk of VTE recurrence are typically anticoagulated as if they had proximal DVT. Those at a low-risk for recurrence might receive a four to six week course of anticoagulation, lower doses, or no anticoagulation at all. In contrast, those with proximal DVT should receive at least 3 months of anticoagulation.
Some anticoagulants can be taken by mouth, and these oral medicines include warfarin
Warfarin, sold under the brand name Coumadin among others, is a medication that is used as an anticoagulant (blood thinner). It is commonly used to prevent blood clots such as deep vein thrombosis and pulmonary embolism, and to prevent ...
(a vitamin K antagonist
Vitamin K antagonists (VKA) are a group of substances that reduce blood clotting by reducing the action of vitamin K. The term "vitamin K antagonist" is technically a misnomer, as the drugs do not directly antagonise the action of vitamin K in ...
), rivaroxaban (a factor Xa inhibitor
Direct factor Xa inhibitors (xabans) are anticoagulants (blood thinning drugs), used to both treat and prevent blood clots in veins, and prevent stroke and embolism in people with atrial fibrillation (AF).
Medical use
Direct factor Xa inhibit ...
), apixaban (a factor Xa inhibitor), dabigatran
Dabigatran, sold under the brand name Pradaxa among others, is an anticoagulant used to treat and prevent blood clots and to prevent stroke in people with atrial fibrillation. Specifically it is used to prevent blood clots following hip or ...
(a direct thrombin inhibitor), and edoxaban (a factor Xa inhibitor). Other anticoagulants cannot be taken by mouth. These parenteral
A route of administration in pharmacology and toxicology is the way by which a drug, fluid, poison, or other substance is taken into the body.
Routes of administration are generally classified by the location at which the substance is applied. ...
(non-oral) medicines include low-molecular-weight heparin, fondaparinux, and unfractionated heparin. Some oral medicines are sufficient when taken alone, while others require the use of an additional parenteral blood thinner. Rivaroxaban and apixaban are the typical first-line medicines, and they are sufficient when taken orally. Rivaroxaban is taken once daily, and apixaban is taken twice daily. Warfarin, dabigatran, and edoxaban require the use of a parenteral anticoagulant to initiate oral anticoagulant therapy. When warfarin is initiated for VTE treatment, a 5-day minimum of a parenteral anticoagulant together with warfarin is given, which is followed by warfarin-only therapy. Warfarin is taken to maintain an international normalized ratio (INR) of 2.0–3.0, with 2.5 as the target. The benefit of taking warfarin declines as the duration of treatment extends, and the risk of bleeding increases with age. Periodic INR monitoring is not necessary when first-line direct oral anticoagulants are used. Overall, anticoagulation therapy is complex and many circumstances can affect how these therapies are managed.
The duration of anticoagulation therapy (whether it will last 4 to 6 weeks, 6 to 12 weeks, 3 to 6 months, or indefinitely) is a key factor in clinical decision making
In psychology, decision-making (also spelled decision making and decisionmaking) is regarded as the cognitive process resulting in the selection of a belief or a course of action among several possible alternative options. It could be either ra ...
. When proximal DVT is provoked by surgery or trauma a 3-month course of anticoagulation is standard. When a first VTE is proximal DVT that is either unprovoked or associated with transient non-surgical risk factor, low-dose anticoagulation beyond 3 to 6 months might be used. In those with an annual risk of VTE in excess of 9%, as after an unprovoked episode, extended anticoagulation is a possibility. Those who finish warfarin treatment after idiopathic VTE with an elevated D-dimer level show an increased risk of recurrent VTE (about 9% vs about 4% for normal results), and this result might be used in clinical decision making. Thrombophilia test results rarely play a role in the length of treatment.
Treatment for acute leg DVT is suggested to continue at home for uncomplicated DVT instead of hospitalization. Factors that favor hospitalization include severe symptoms or additional medical issues. Early walking is suggested over bedrest. Graduated compression stockings—which apply higher pressure at the ankles and a lower pressure around the knees can be trialed for symptomatic management of acute DVT symptoms, but they are not recommended for reducing the risk of post-thrombotic syndrome, as the potential benefit of using them for this goal "may be uncertain". Nor are compression stockings likely to reduce VTE recurrence. They are, however, recommended in those with isolated distal DVT.
If someone decides to stop anticoagulation after an unprovoked VTE instead of being on lifelong anticoagulation, aspirin can be used to reduce the risk of recurrence, but it is only about 33% as effective as anticoagulation in preventing recurrent VTE. Statin
Statins, also known as HMG-CoA reductase inhibitors, are a class of lipid-lowering medications that reduce illness and mortality in those who are at high risk of cardiovascular disease. They are the most common cholesterol-lowering drugs.
L ...
s have also been investigated for their potential to reduce recurrent VTE rates, with some studies suggesting effectiveness.
Investigations for cancer
An unprovoked VTE might signal the presence of an unknown cancer, as it is an underlying condition in up to 10% of unprovoked cases. A thorough clinical assessment is needed and should include a physical examination, a review of medical history, and universal cancer screening done in people of that age. A review of prior imaging is considered worthwhile, as is "reviewing baseline blood test results including full blood count, renal function, renal and hepatic function, Prothrombin time, PT and activated partial thromboplastin time, APTT."National Institute for Health and Care Excellence"NICE Guideline 158: Venous thromboembolic diseases: diagnosis, management and thrombophilia testing
London, 26 March 2020. It is not recommended practice to obtain tumor markers or a CT of the abdomen and pelvis in asymptomatic individuals. NICE recommends that further investigations are unwarranted in those without relevant signs or symptoms.
Interventions
Thrombolysis is the injection of an enzyme into the veins to dissolve blood clots, and while this treatment has been proven effective against the life-threatening emergency clots of stroke and heart attacks, randomized controlled trials have not established a net benefit in those with acute proximal DVT. Drawbacks of catheter-directed thrombolysis (the preferred method of administering the clot-busting enzyme) include a risk of bleeding, complexity, and the cost of the procedure. Although, while anticoagulation is the preferred treatment for DVT, thrombolysis is a treatment option for those with the severe DVT form of phlegmasia cerula dorens (''bottom left image'') and in some younger patients with DVT affecting the iliac and common femoral veins. Of note, a variety of Thrombolysis#Contraindications, contraindications to thrombolysis exist. In 2020, NICE kept their 2012 recommendations that catheter-directed thrombolysis should be considered in those with iliofemoral DVT who have "symptoms lasting less than 14 days, good functional status, a life expectancy of 1 year or more, and a low risk of bleeding." A mechanical thrombectomy device can remove DVT clots, particularly in acute iliofemoral DVT (DVT of the major veins in the pelvis), but there is limited data on its efficacy. It is usually combined with thrombolysis, and sometimes temporary IVC filters are placed to protect against PE during the procedure.National Institute for Health and Care Excellence"NICE Interventional procedures guidance 651: Percutaneous mechanical thrombectomy for acute deep vein thrombosis of the leg
London, 12 June 2019. Catheter-directed thrombolysis with thrombectomy against iliofemoral DVT has been associated with a reduction in the severity of post-thrombotic syndrome at an estimated cost-effectiveness ratio of about $138,000 per gained QALY. Phlegmasia cerulea dolens might be treated with catheter-directed thrombolysis and/or thrombectomy. In DVT in the arm, the first (topmost) rib can be surgically removed as part of the typical treatment when the DVT is due to thoracic outlet syndrome or Paget–Schroetter syndrome. This treatment involves initial anticoagulation followed by thrombolysis of the subclavian vein and staged first rib resection to relieve the thoracic outlet compression and prevent recurrent DVT.
 The placement of an inferior vena cava filter (IVC filter) is possible when either the standard treatment for acute DVT, anticoagulation, is absolutely contraindicated (not possible), or if someone develops a PE despite being anticoagulated. However, a 2020 NICE review found "little good evidence" for their use. A 2018 study associated IVC filter placement with a 50% reduction in PE, a 70% increase in DVT, and an 18% increase in 30 day mortality when compared to no IVC placement. Other studies including a systematic review and meta-analysis did not find a difference in mortality with IVC placement. If someone develops a PE despite being anticoagulated, care should be given to optimize anticoagulation treatment and address other related concerns before considering IVC filter placement.
The placement of an inferior vena cava filter (IVC filter) is possible when either the standard treatment for acute DVT, anticoagulation, is absolutely contraindicated (not possible), or if someone develops a PE despite being anticoagulated. However, a 2020 NICE review found "little good evidence" for their use. A 2018 study associated IVC filter placement with a 50% reduction in PE, a 70% increase in DVT, and an 18% increase in 30 day mortality when compared to no IVC placement. Other studies including a systematic review and meta-analysis did not find a difference in mortality with IVC placement. If someone develops a PE despite being anticoagulated, care should be given to optimize anticoagulation treatment and address other related concerns before considering IVC filter placement.
Field of medicine
Patients with a history of DVT might be managed by primary care, general internal medicine, hematology, cardiology, vascular surgery, or vascular medicine. Patients suspected of having an acute DVT are often referred to the emergency department for evaluation. Interventional radiology is the specialty that typically places and retrieves IVC filters, and vascular surgery might do catheter directed thrombosis for some severe DVTs.Prevention
For the prevention of blood clots in the general population, incorporating leg exercises while sitting down for long periods, or having breaks from a sitting position and walking around, having an active lifestyle, and maintaining a healthy body weight are recommended. Walking increases blood flow through the leg veins. Excess body weight is modifiable unlike most risk factors, and interventions or lifestyle modifications that help someone who is overweight or obese Weight loss, lose weight reduce DVT risk. Avoiding both smoking and a Western pattern diet are thought to reduce risk. Statins have been investigated for primary prevention (prevention of a first VTE), and the JUPITER trial, which used rosuvastatin, has provided some tentative evidence of effectiveness. Of the statins, rosuvastatin appears to be the only one with the potential to reduce VTE risk. If so, it appears to reduce risk by about 15%. However, the number needed to treat to prevent one initial VTE is about 2000, limiting its applicability.Hospital (non-surgical) patients
Acutely ill hospitalized patients are suggested to receive a parenteral anticoagulant, although the potential net benefit is uncertain. Critically ill hospitalized patients are recommended to either receive unfractionated heparin or low-molecular weight heparin instead of foregoing these medicines.After surgery
 Major orthopedic surgery—total hip replacement, total knee replacement, or Hip fracture#Management, hip fracture surgery—has a high risk of causing VTE. If prophylaxis is not used after these surgeries, symptomatic VTE has about a 4% chance of developing within 35 days. Following major orthopedic surgery, a blood thinner or aspirin is typically paired with intermittent pneumatic compression, which is the preferred mechanical prophylaxis over graduated compression stockings.
Options for VTE prevention in people following non-orthopedic surgery include early walking, mechanical prophylaxis, and blood thinners (low-molecular-weight heparin and low-dose-unfractionated heparin) depending upon the risk of VTE, risk of major bleeding, and person's preferences. After low-risk surgeries, early and frequent walking is the best preventive measure.
Major orthopedic surgery—total hip replacement, total knee replacement, or Hip fracture#Management, hip fracture surgery—has a high risk of causing VTE. If prophylaxis is not used after these surgeries, symptomatic VTE has about a 4% chance of developing within 35 days. Following major orthopedic surgery, a blood thinner or aspirin is typically paired with intermittent pneumatic compression, which is the preferred mechanical prophylaxis over graduated compression stockings.
Options for VTE prevention in people following non-orthopedic surgery include early walking, mechanical prophylaxis, and blood thinners (low-molecular-weight heparin and low-dose-unfractionated heparin) depending upon the risk of VTE, risk of major bleeding, and person's preferences. After low-risk surgeries, early and frequent walking is the best preventive measure.
Pregnancy
The risk of VTE is increased in pregnancy by about four to five times because of a more hypercoagulable state that protects against fatal postpartum hemorrhage. Preventive measures for pregnancy-related VTE were suggested by the American Society of Hematology in 2018. Warfarin, a common vitamin K antagonist, can cause birth defects and is not used for prevention during pregnancy.Travelers
 Travelling "is an often cited yet relatively uncommon" cause of VTE. Suggestions for at-risk long-haul travelers include calf exercises, frequent walking, and aisle seating in airplanes to ease walking. See section 6.0, Long-Distance Travel Graduated compression stockings have sharply reduced the levels of asymptomatic DVT in airline passengers, but the effect on symptomatic DVT, PE, or mortality is unknown, as none of the individuals studied developed these outcomes. However, graduated compression stockings are not suggested for long-haul travelers (>4 hours) without risk factors for VTE. Likewise, neither aspirin nor anticoagulants are suggested in the general population undertaking long-haul travel. Those with significant VTE risk factors undertaking long-haul travel are suggested to use either graduated compression stockings or LMWH for VTE prevention. If neither of these two methods are feasible, then aspirin is suggested.
Travelling "is an often cited yet relatively uncommon" cause of VTE. Suggestions for at-risk long-haul travelers include calf exercises, frequent walking, and aisle seating in airplanes to ease walking. See section 6.0, Long-Distance Travel Graduated compression stockings have sharply reduced the levels of asymptomatic DVT in airline passengers, but the effect on symptomatic DVT, PE, or mortality is unknown, as none of the individuals studied developed these outcomes. However, graduated compression stockings are not suggested for long-haul travelers (>4 hours) without risk factors for VTE. Likewise, neither aspirin nor anticoagulants are suggested in the general population undertaking long-haul travel. Those with significant VTE risk factors undertaking long-haul travel are suggested to use either graduated compression stockings or LMWH for VTE prevention. If neither of these two methods are feasible, then aspirin is suggested.
Prognosis
DVT is most frequently a disease of older age that occurs in the context of nursing homes, hospitals, and active cancer. It is associated with a 30-day mortality rate of about 6%, with PE being the cause of most of these deaths. Proximal DVT is frequently associated with PE, unlike distal DVT, which is rarely if ever associated with PE. Around 56% of those with proximal DVT also have PE, although a chest CT is not needed simply because of the presence of DVT. If proximal DVT is left untreated, in the following 3 months approximately half of people will experience symptomatic PE. Another frequent complication of proximal DVT, and the most frequent chronic complication, is post-thrombotic syndrome, where individuals have chronic venous symptoms. Symptoms can include pain, itching, swelling, paresthesia, a sensation of heaviness, and in severe cases, leg ulcers. After proximal DVT, an estimated 20–50% of people develop the syndrome, with 5–10% experiencing severe symptoms. Post-thrombotic syndrome can also be a complication of distal DVT, though to a lesser extent than with proximal DVT. In the 10 years following an initial VTE, about 30% of people will have a recurrence. VTE recurrence in those with prior DVT is more likely to recur as DVT than PE. Cancer and unprovoked DVT are strong risk factors for recurrence. After initial proximal unprovoked DVT with and without PE, 16–17% of people will have recurrent VTE in the 2 years after they complete their course of anticoagulants. VTE recurrence is less common in distal DVT than proximal DVT. In upper extremity DVT, annual VTE recurrence is about 2–4%. After surgery, a provoked proximal DVT or PE has an annual recurrence rate of only 0.7%.Epidemiology
About 1.5 out of 1000 adults a year have a first VTE in high-income countries. The condition becomes much more common with age. VTE rarely occurs in children, but when it does, it predominantly affects hospitalized children. Children in North America and the Netherlands have VTE rates that range from 0.07 to 0.49 out of 10,000 children annually. Meanwhile, almost 1% of those aged 85 and above experience VTE each year. About 60% of all VTEs occur in those 70 years of age or older. Incidence is about 18% higher in males than in females, though there are ages when VTE is more prevalent in women. VTE occurs in association with hospitalization or nursing home residence about 60% of the time, active cancer about 20% of the time, and a central venous catheter or transvenous pacemaker about 9% of the time. During pregnancy and after childbirth, acute VTE occurs in about 1.2 of 1000 deliveries. Despite it being relatively rare, it is a leading cause of maternal morbidity and Maternal mortality, mortality. After surgery with preventive treatment, VTE develops in about 10 of 1000 people after total or partial knee replacement, and in about 5 of 1000 after total or partial hip replacement. About 400,000 Americans develop an initial VTE each year, with 100,000 deaths or more attributable to PE. Asian, Asian-American, Native American, and Hispanic individuals have a lower VTE risk than Whites or Blacks. Populations in Asia have VTE rates at 15 to 20% of what is seen in Western countries, with an increase in incidence seen over time. In North American and European populations, around 4–8% of people have a thrombophilia, most commonly factor V leiden and prothrombin G20210A. For populations in China, Japan, and Thailand, deficiences in protein S, protein C, and antithrombin predominate. Non-O blood type is present in around 50% of the general population and Blood type distribution by country, varies with ethnicity, and it is present in about 70% of those with VTE. DVT occurs in the upper extremities in about 4–10% of cases, with an incidence of 0.4–1.0 people out of 10,000 a year. A minority of upper extremity DVTs are due to Paget–Schroetter syndrome, also called effort thrombosis, which occurs in 1–2 people out of 100,000 a year, usually in athletic males around 30 years of age or in those who do significant amounts of overhead manual labor.Social
 Being on blood thinners because of DVT can be life-changing because it can prevent lifestyle activities such as contact or winter sports to prevent bleeding after potential injuries. Head injuries prompting brain bleeds are of particular concern. This has caused NASCAR driver Brian Vickers to forego participation in races. Professional basketball players including NBA players Chris Bosh and hall of famer Hakeem Olajuwon have dealt with recurrent blood clots, and Bosh's career was significantly hampered by DVT and PE.
Tennis star Serena Williams was hospitalized in 2011 for PE thought to have originated from DVT. Years later, in 2017, due to her knowledge of DVT and PE, Serena accurately Patient advocacy, advocated for herself to have a PE diagnosed and treated. During this encounter with VTE, she was hospitalized after a C-section surgery and was off of blood thinners. After feeling the sudden onset of a PE symptom, shortness of breath, she told her nurse and requested CT pulmonary angiogram, a CT scan and an IV heparin drip, all while gasping for air. She started to receive an ultrasound to look for DVT in the legs, prompting her to express dissatisfaction to the medical staff that they were not looking for clots where she had symptoms (her lungs), and they were not yet treating her presumed PE. After being diagnosed with PE and not DVT, and after receiving heparin by IV, the coughing from the PE caused her C-section surgical site to open and the heparin contributed to bleeding at the site. Serena later received an IVC filter while in the hospital.
Other notable people have been affected by DVT. Former United States (US) President Richard Nixon had recurrent DVT, and so has former Secretary of State Hillary Clinton. She was first diagnosed while First Lady of the United States, First Lady in 1998 and again in 2009. Dick Cheney was diagnosed with an episode while Vice President of the United States, Vice President, and TV show host Regis Philbin had DVT after hip-replacement surgery. DVT has also contributed to the deaths of famous people. For example, DVT and PE played a role in rapper Heavy D's death at age 44. NBC journalist David Bloom died at age 39 while covering the Iraq War from a PE that was thought to have progressed from a missed DVT, and actor Jimmy Stewart had DVT that progressed to a PE when he was 89.
Being on blood thinners because of DVT can be life-changing because it can prevent lifestyle activities such as contact or winter sports to prevent bleeding after potential injuries. Head injuries prompting brain bleeds are of particular concern. This has caused NASCAR driver Brian Vickers to forego participation in races. Professional basketball players including NBA players Chris Bosh and hall of famer Hakeem Olajuwon have dealt with recurrent blood clots, and Bosh's career was significantly hampered by DVT and PE.
Tennis star Serena Williams was hospitalized in 2011 for PE thought to have originated from DVT. Years later, in 2017, due to her knowledge of DVT and PE, Serena accurately Patient advocacy, advocated for herself to have a PE diagnosed and treated. During this encounter with VTE, she was hospitalized after a C-section surgery and was off of blood thinners. After feeling the sudden onset of a PE symptom, shortness of breath, she told her nurse and requested CT pulmonary angiogram, a CT scan and an IV heparin drip, all while gasping for air. She started to receive an ultrasound to look for DVT in the legs, prompting her to express dissatisfaction to the medical staff that they were not looking for clots where she had symptoms (her lungs), and they were not yet treating her presumed PE. After being diagnosed with PE and not DVT, and after receiving heparin by IV, the coughing from the PE caused her C-section surgical site to open and the heparin contributed to bleeding at the site. Serena later received an IVC filter while in the hospital.
Other notable people have been affected by DVT. Former United States (US) President Richard Nixon had recurrent DVT, and so has former Secretary of State Hillary Clinton. She was first diagnosed while First Lady of the United States, First Lady in 1998 and again in 2009. Dick Cheney was diagnosed with an episode while Vice President of the United States, Vice President, and TV show host Regis Philbin had DVT after hip-replacement surgery. DVT has also contributed to the deaths of famous people. For example, DVT and PE played a role in rapper Heavy D's death at age 44. NBC journalist David Bloom died at age 39 while covering the Iraq War from a PE that was thought to have progressed from a missed DVT, and actor Jimmy Stewart had DVT that progressed to a PE when he was 89.
History
 The book ''Sushruta Samhita'', an Ayurvedic text published around 600–900 BC, contains what has been cited as the first description of DVT. In 1271, DVT symptoms in the leg of a 20-year-old male were described in a French manuscript, which has been cited as the first case or the first Western reference to DVT.
In 1856, German physician and pathologist Rudolf Virchow published his analysis after the insertion of foreign bodies into the jugular veins of dogs, which migrated to the pulmonary arteries. These foreign bodies caused pulmonary emboli, and Virchow was focused on explaining their consequences. He cited three factors, which are now understood as hypercoaguability, stasis, and endothelial injury. It was not until 1950 that this framework was cited as Virchow's triad, but the teaching of Virchow's triad has continued in light of its utility as a theoretical framework and as a recognition of the significant progress Virchow made in expanding the understanding of VTE.
Methods to observe DVT by ultrasound were established in the 1960s. Diagnoses were commonly performed by impedance plethysmography in the 1970s and 1980s, but ultrasound, particularly after utility of probe compression was demonstrated in 1986, became the preferred diagnostic method. Yet, in the mid-1990s, contrast venography and impedance plethysmography were still described as common.
The book ''Sushruta Samhita'', an Ayurvedic text published around 600–900 BC, contains what has been cited as the first description of DVT. In 1271, DVT symptoms in the leg of a 20-year-old male were described in a French manuscript, which has been cited as the first case or the first Western reference to DVT.
In 1856, German physician and pathologist Rudolf Virchow published his analysis after the insertion of foreign bodies into the jugular veins of dogs, which migrated to the pulmonary arteries. These foreign bodies caused pulmonary emboli, and Virchow was focused on explaining their consequences. He cited three factors, which are now understood as hypercoaguability, stasis, and endothelial injury. It was not until 1950 that this framework was cited as Virchow's triad, but the teaching of Virchow's triad has continued in light of its utility as a theoretical framework and as a recognition of the significant progress Virchow made in expanding the understanding of VTE.
Methods to observe DVT by ultrasound were established in the 1960s. Diagnoses were commonly performed by impedance plethysmography in the 1970s and 1980s, but ultrasound, particularly after utility of probe compression was demonstrated in 1986, became the preferred diagnostic method. Yet, in the mid-1990s, contrast venography and impedance plethysmography were still described as common.
 Multiple pharmacological therapies for DVT were introduced in the 20th century: oral anticoagulants in the 1940s, subcutaneous injections of LDUH in 1962 and subcutaneous injections of LMWH in 1982. 1974 was when vascular inflammation and venous thrombosis were first proposed to be interrelated. For around 50 years, a months-long warfarin (Coumadin) regimen was the mainstay of pharmacological treatment. To avoid the blood monitoring required with warfarin and the injections required by heparin and heparin-like medicines, direct oral anticoagulants (DOACs) were developed. In the late 2000s to early 2010s, DOACs—including rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa)—came to the market. ''The New York Times'' described a "furious battle" among the three makers of these drugs "for the prescription pads of doctors".
Multiple pharmacological therapies for DVT were introduced in the 20th century: oral anticoagulants in the 1940s, subcutaneous injections of LDUH in 1962 and subcutaneous injections of LMWH in 1982. 1974 was when vascular inflammation and venous thrombosis were first proposed to be interrelated. For around 50 years, a months-long warfarin (Coumadin) regimen was the mainstay of pharmacological treatment. To avoid the blood monitoring required with warfarin and the injections required by heparin and heparin-like medicines, direct oral anticoagulants (DOACs) were developed. In the late 2000s to early 2010s, DOACs—including rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa)—came to the market. ''The New York Times'' described a "furious battle" among the three makers of these drugs "for the prescription pads of doctors".
Economics
VTE costs the US healthcare system about $7 to 10 billion dollars annually. Initial and average DVT costs for a hospitalized US patient is about $10,000 (2015 estimate). In Europe, the costs for an initial VTE hospitalization are significantly less, costing about Euro, €2000 to 4000 (2011 estimate). Post-thrombotic syndrome is a significant contributor to DVT follow-up costs. Outpatient treatment significantly reduces costs, and treatment costs for PE exceed those of DVT.Research directions
A 2019 study published in ''Nature Genetics'' reported more than doubling the known Locus (genetics), genetic loci associated with VTE. In their updated 2018 clinical practice guidelines, the American Society of Hematology identified 29 separate research priorities, most of which related to patients who are acutely or critically ill. Inhibition of factor XI, P-selectin, E-selectin, and a reduction in formation ofneutrophil extracellular traps
Neutrophil extracellular traps (NETs) are networks of extracellular fibers, primarily composed of DNA from neutrophils, which bind pathogens. Neutrophils are the immune system's first line of defense against infection and have conventionally b ...
are potential therapies that might treat VTE without increasing bleeding risk.
Notes
References
Cited literature * * {{Vascular diseases Coagulopathies Diseases of veins, lymphatic vessels and lymph nodes Hematology Wikipedia medicine articles ready to translate