Indications for dental crowns
 Crowns are indicated to:
* Replace existing crowns which have failed.
* Restore the form, function and appearance of badly broken down, worn or fractured teeth, where other simpler forms of restorations are unsuitable or have been found to fail clinically.
* Improve the aesthetics of unsightly teeth which cannot be managed by simpler
Crowns are indicated to:
* Replace existing crowns which have failed.
* Restore the form, function and appearance of badly broken down, worn or fractured teeth, where other simpler forms of restorations are unsuitable or have been found to fail clinically.
* Improve the aesthetics of unsightly teeth which cannot be managed by simpler Restoration of endodontically treated teeth
Traditionally, it has been proposed that teeth which have undergone root canal treatment are more likely to fracture and therefore require cuspal protection by providing occlusal coverage with an indirect restoration like crowns. This led to routine prescribing of crowns for root-treated teeth. However, recent review of literature reveals that there is no strong evidence to show that crowns are better than other routine restorations to restore root-filled teeth. The general advice is that dentists should use their clinical experience in view of the patient's preferences when making the decision of using a crown. As a rule of thumb, the use of crowns and other indirect restorations for root treated teeth is justified when the surface area of the access cavity exceeds one third of the occlusal surface of the tooth, when the lingual or buccal walls are undermined or when the mesial and distal marginal ridges are missing.Clinical stages of dental crown provision
# Assessment # Choice of restoration # Tooth preparation # Construction and fit of temporary restoration # Tooth preparation impressions # Fit of definitive restoration # ReviewAssessment
In order to ensure optimum condition and longevity for the proposed crowns, several factors need to be explored by conducting a thorough and targeted patient history and clinical dental examination. These factors include: * Patient factors ** Patient expectations ** Patient motivation to adhere to the treatment plan and maintain results ** Financial and time costs to the patient * Biological factors ** Periodontal health status and periodontal disease risk ** Pulpal health and endodontic disease risk ** Caries and caries risk ** Occlusion and occlusal problems risk * Mechanical factors ** Amount of remaining tooth structure ** Height and width of tooth to be prepared ** Attachment levels of the tooth to be prepared ** Root shape and length of the tooth to be prepared * Aesthetic factorsChoice of restoration
The choice(s) of crown restoration can be described by: * The dimensions and percentage coverage of the natural crown ** Full crowns ** 3/4 and 7/8 crowns * Material to be used ** Metal ** Metal-ceramic crowns ** Full ceramic crowns3/4 and 7/8 crowns
These restorations are a hybrid between an onlay and a full crown. They are named based on the estimated wall coverage of the walls of the tooth; e.g. the 3/4 crown aims to cover three out of the four walls, with the buccal wall being usually spared, thus reducing sound tooth tissue to be prepared. They are normally fabricated in gold. Grooves or boxes are normally added to the preparations as close to the unprepared wall as possible to increase retention of the crown. Despite its advantages of reducing sound tooth preparation, these crowns are not commonly prescribed in practice because they are technically difficult and have poor patient acceptability due to the metal showing through in their smile.Full metal crowns
As the name suggests, these crowns are entirely cast in a metal alloy. There are a multitude of alloys available and the selection of a particular alloy over another depends on several factors including cost, handling, physical properties, biocompatibility. The American Dental Association categories alloys in three groups: high-noble, noble and base metal alloys.High-noble and noble alloys
 Noble and high-noble alloys used in casting crowns are generally based on alloys of gold. Gold is not used in its pure form as it is too soft and has poor mechanical strength. Other metals included in gold alloys are copper, platinum, palladium, zinc, indium and nickel. All types of gold casting alloys used in prosthodontics (Type I - IV) are categorised by their percentage content of gold and hardness, with Type I being the softest and Type IV the hardest. Generally, Type III and IV alloys (62 - 78% and 60 - 70% gold content respectively) are used in casting of full crowns, as these are hard enough to withstand occlusal forces. Gold crowns (also known as ''gold shell crowns'') are generally indicated for posterior teeth due to aesthetic reasons. They are durable in function and strong in thin sections, therefore require minimal tooth preparation. They also have similar wear properties to enamel, so they are not likely to cause excessive wear to the opposing tooth. They have good dimensional accuracy when cast which minimises chair-side/appointment time and can be relatively easy to polish if any changes are required. Palladium based alloys are also used. These were introduced as a cheaper alternative to gold alloys in the 1970s. Palladium has a strong whitening effect giving most of its alloys a silverish appearance.
Noble and high-noble alloys used in casting crowns are generally based on alloys of gold. Gold is not used in its pure form as it is too soft and has poor mechanical strength. Other metals included in gold alloys are copper, platinum, palladium, zinc, indium and nickel. All types of gold casting alloys used in prosthodontics (Type I - IV) are categorised by their percentage content of gold and hardness, with Type I being the softest and Type IV the hardest. Generally, Type III and IV alloys (62 - 78% and 60 - 70% gold content respectively) are used in casting of full crowns, as these are hard enough to withstand occlusal forces. Gold crowns (also known as ''gold shell crowns'') are generally indicated for posterior teeth due to aesthetic reasons. They are durable in function and strong in thin sections, therefore require minimal tooth preparation. They also have similar wear properties to enamel, so they are not likely to cause excessive wear to the opposing tooth. They have good dimensional accuracy when cast which minimises chair-side/appointment time and can be relatively easy to polish if any changes are required. Palladium based alloys are also used. These were introduced as a cheaper alternative to gold alloys in the 1970s. Palladium has a strong whitening effect giving most of its alloys a silverish appearance.
Base-metal alloys
Cast base-metal alloys are rarely used to make full metal crowns. They are more commonly used as part of metal-ceramic crowns as bonding alloys. When compared to high-noble and noble alloys, they are stronger and harder; they can be used in thinner sections (0.3mm as opposed to 0.5mm) however they are harder to adjust and are more likely to cause excessive wear on real opposing teeth. Furthermore, there may be problems with people who have a nickel allergy. Common base-metal alloys used in dentistry are:
* Silver-palladium
* Silver-palladium-copper
* Nickel-chromium
* Nickel-chromium-beryllium
* Cobalt-chromium
* Titanium
Common base-metal alloys used in dentistry are:
* Silver-palladium
* Silver-palladium-copper
* Nickel-chromium
* Nickel-chromium-beryllium
* Cobalt-chromium
* Titanium
Titanium
Titanium and titanium alloys are highly biocompatible. Its strength, rigidity and ductility are similar to that of other casting alloys used in dentistry. Titanium also readily forms an oxide layer on its surface which gives it anti-corrosive properties and allows it to bond to ceramics, a useful property in the manufacture of metal-ceramic crowns.Full ceramic crowns
Dental ceramics or porcelains are used for crowns manufacture primarily for their aesthetic properties compared to all metal restorations. These materials are generally quite brittle and prone to fracture. Many classifications have been used to categorise dental ceramics, with the simplest, based on the material from which they are made, i.e. silica, alumina or zirconia.Silica
 Silica-based ceramics are highly aesthetic due to their high glass content and excellent optical properties due to the addition of filler particles which enhance opalescence, fluorescence which can mimic the colour of natural enamel and dentine. These ceramics, however, suffer from poor mechanical strength, and therefore often used for veneering stronger substructures.
Examples include aluminosilicate glass, e.g. feldspathic, synthetic porcelain, and leucite reinforced ceramics.
Mechanical properties can be improved by the addition of filler particles, e.g. lithium disilicate, and are therefore termed glass ceramics. Glass-ceramics can be used alone to make all-ceramic restorations either as a single form (termed uni-layered) or can act as a substructures for subsequent veneering (or layering) with weaker feldspathic porcelain (restorations termed bi-layered).
Silica-based ceramics are highly aesthetic due to their high glass content and excellent optical properties due to the addition of filler particles which enhance opalescence, fluorescence which can mimic the colour of natural enamel and dentine. These ceramics, however, suffer from poor mechanical strength, and therefore often used for veneering stronger substructures.
Examples include aluminosilicate glass, e.g. feldspathic, synthetic porcelain, and leucite reinforced ceramics.
Mechanical properties can be improved by the addition of filler particles, e.g. lithium disilicate, and are therefore termed glass ceramics. Glass-ceramics can be used alone to make all-ceramic restorations either as a single form (termed uni-layered) or can act as a substructures for subsequent veneering (or layering) with weaker feldspathic porcelain (restorations termed bi-layered).
Alumina
Alumina (aluminium oxide) was introduced as a dental substructure (core) in 1989 when the material was slip cast, sintered, and infiltrated with glass. More recently, glass-infiltrated alumina cores are produced by electrophoretic deposition, a rapid nanofabricating process. During this process, particles of a slip are brought to the surface of a dental die by an electric current, thereby forming a precision-fitting core greenbody in seconds. Margins are then trimmed and the greenbody is sintered and infiltrated with glass. Glass-infiltrated alumina has significantly higher porcelain bond strength over CAD/CAM produced zirconia and alumina cores without glass. Alumina cores without glass are produced by milling pre-sintered blocks of the material utilizing a CAD/CAM dentistry technique. Cores without glass must be oversized to compensate for shrinkage that occurs when the core is fully sintered. Milled cores are then sintered and shrink to the correct size. All alumina cores are layered with tooth tissue-like feldspathic porcelain to make true-to-life color and shape. Dental artists called ceramists, can customize the "look" of these crowns to individual patient and dentist requirements. Alumina cores have better translucency than zirconia, but worse than lithium disilicate.Zirconia
Yttria-stabilized zirconia, also known simply as zirconia, is a very hard ceramic that is used as a strong base material in some full ceramic restorations. Zirconia is relatively new in dentistry and the published clinical data is correspondingly limited. The zirconia used in dentistry is zirconium oxide (ZrO2) which has been stabilized with the addition of yttrium oxide. Yttria-stabilized zirconia is also known as YSZ. The zirconia substructure (core) is usually designed on a digital representation of the patient's mouth, which is captured with a three-dimensional digital scan of the patient, impression, or model. The core is then milled from a block of zirconia in a soft pre-sintered state. Once milled, the zirconia is
The zirconia substructure (core) is usually designed on a digital representation of the patient's mouth, which is captured with a three-dimensional digital scan of the patient, impression, or model. The core is then milled from a block of zirconia in a soft pre-sintered state. Once milled, the zirconia is Monolithic zirconia
Monolithic zirconia crowns tend to be opaque in appearance with a high value and they lack translucency and fluorescence. For the sake of appearance, many dentists will not use monolithic crowns on anterior (front) teeth. Monolithic zirconia crowns are produced from a color- and structure-graded zirconia block and coated with a thin layer of glaze stains which also provides some kind of fluorescence. The "graded" zirconia crown has a darker cervical area consisting of tetragonal zirconia, a main tooth color in the buccal area, and a translucent incisal edge consisting of cubic zirconia. The only thing a dental technician has to do is to use the proper height of the zirconia block so that the crown fits in all the different color zones. Although on the outside the color gradient mimics natural teeth, they are still far from the optical, physical, biomimetic and esthetic properties of natural teeth. To a large extent, materials selection in dentistry determine the strength and appearance of a crown. Some monolithic zirconia materials produce the strongest crowns in dentistry (the registered strength for some zirconia crown materials is near 1200 MPa), but these crowns are not usually considered to be natural enough for use in the front of the mouth. Although not as strong, some of the newer zirconia materials are better in appearance but generally still not as good as porcelain-fused crowns. By contrast, when porcelain is fused to glass-infiltrated alumina, crowns are very natural-looking and very strong, though not as strong as monolithic zirconia crowns. Zirconia crowns are said to be less abrasive to opposing teeth than metal-ceramic crowns. Other crown material properties to be considered are thermal conductivity and radiolucency. Stability/looseness of fit on the prepared tooth and cement gap at the margin are sometimes related to materials selection, though these crown properties are also commonly related to system and fabricating procedures.Lithium-disilicate
Another monolithic material, lithium disilicate, produces extremely translucent leucite-reinforced crowns that often appear to be too gray in the mouth. To overcome this, the light shade polyvalent colorants take on a distinctly unnatural, bright white appearance.Metal-ceramic crowns (P-F-M Crown)
These are a hybrid of metal and ceramic crowns. The metal part is normally made of a base metal alloy (termed bonding alloy). The properties of the metal alloy chosen should match and complement that of the ceramic to be bonded otherwise problems like delamination or fracturing of the ceramic can occur. To obtain an aesthetic finish which is able to be functional with normal mastication activity, a minimal thickness of ceramic and metallic material is required, which should be planned for during tooth preparation stage. Ceramic bonds to the metal framework by three methods: * Compression fit (via ceramic shrinkage on firing) * Micro-mechanical retention (via surface irregularities) * Chemical union (via oxide formation)Tissue control and gingival retraction
Gingival retraction refers to the displacement of the free gingivae. For crowns with margins which are supragingival, there is no need for gingival retraction, provided there is good moisture control. For crown preparations which have subgingival margins, tissue control is necessary at the preparation stage and impression stage to ensure visibility, good moisture control and ensure enough bulk of impression material can be placed to accurately record the marginal areas.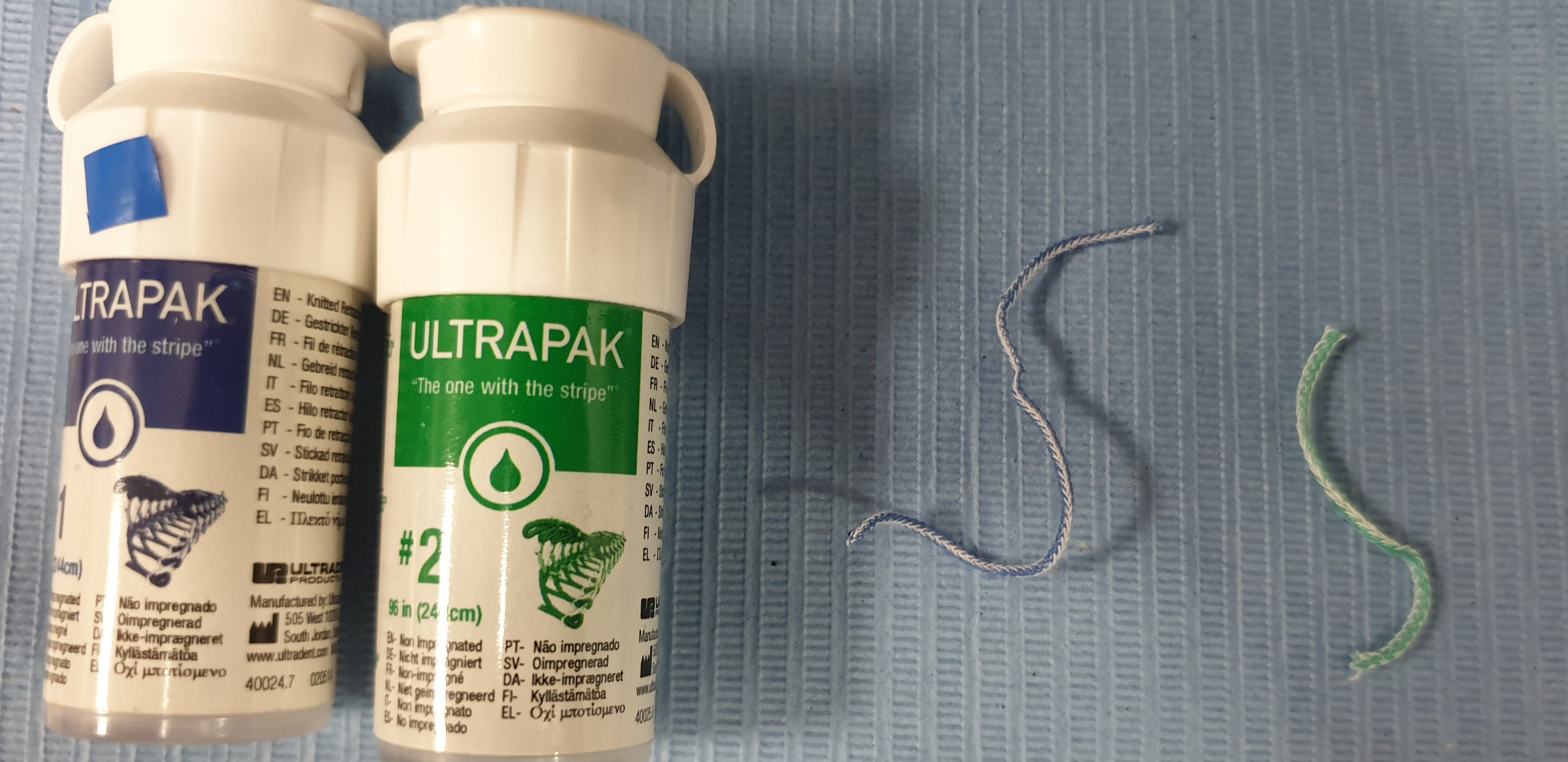 Options available are gingival retraction cord, Magic Foam cord, and ExpaSyl.
Another method to expose the margins of a subgingival preparation is to use electrosurgery or
Options available are gingival retraction cord, Magic Foam cord, and ExpaSyl.
Another method to expose the margins of a subgingival preparation is to use electrosurgery or Tooth preparation
The design of a preparation for a tooth to accept a crown follows five basic principles: # Retention and resistance # Preservation of tooth structure # Structural durability # Marginal integrity # Preservation of the periodontium Aesthetics can also play a role in planning the design.Retention and resistance
As there are currently no biologically compatible cements which are able to hold the crown in place solely through their adhesive properties, the geometric form of the preparation is vital in providing retention and resistance to hold the crown in place. Within the context of prosthodontics, ''retention'' refers to resistance of movement of a restoration along the path of insertion or along the long axis of the tooth. ''Resistance'' refers to the resistance of movement of the crown by forces applied apically or in an oblique direction which prevents movement under occlusal forces. Retention is determined by the relationship between opposing surfaces of the preparation (e.g. the relationship of the buccal and lingual walls).Taper
Theoretically, the more parallel the opposing walls of a preparation, the more retention is achieved. However this is almost impossible to achieve clinically. It is standard for preparations for full coverage crowns to slightly taper or converge in an occlusal direction. This allows the preparation to be visually inspected, prevent undercuts, compensate for crown fabrication inaccuracies and allow, at the cementation stage, for excess cement to escape with the ultimate aim of optimising the seating of the crown on the preparation. Generally axial walls prepared using a long tapered high speed burs confer a 2 - 3° taper on each wall and an overall 4 - 6° taper to the preparation. As taper increases, retention decreases so taper should be kept to a minimum whilst ensuring elimination of undercuts. An overall taper of 16° is said to be clinically achievable and being able to fulfil the aforesaid requirements. Ideally, the taper should not exceed 20 degrees as will negatively impact retention.Length
Occluso-gingival length or height of the crown preparation affects both resistance and retention. Generally, the taller the preparation, the greater the surface area is. For the crown to be retentive enough, the length of the preparation must be greater than the height formed by the arc of the cast pivoting around a point on the margin on the opposite side of the restoration. The arc is affected by the diameter of the tooth prepared, therefore the smaller the diameter, the shorter the length of the crown needs to be to resist removal. Retention of short-walled teeth with a wide diameter can be improved by placing grooves in the axial walls, which has the effect of reducing the size of the arc.Freedom of displacement
Retention can be improved by geometrically limiting the number of paths along which the crown can be removed from the tooth presentation, with maximum retention being reached when only one path of displacement is present. Resistance can be improved by inserting components like grooves.Preservation of tooth structure
Structural durability
In order to last, the crown must be made of enough material to withstand normal masticatory function and should be contained within the space created by the tooth preparation, otherwise problems may arise with aesthetics and occlusal stability (i.e. high restorations) and cause periodontal inflammation. Depending on the material used to create the crown, minimal occlusal and axial reductions are required to house the crown.Occlusal reduction
For gold alloys there should be 1.5mm clearance, whilst metal-ceramic crowns and full ceramic crowns require 2.0 mm. The occlusal clearance should follow the natural outline of the tooth; otherwise there may be areas of the restorations where the material may be too thin.Functional cusp bevel
For posterior teeth, a wide bevel is required on the functional cusps, palatal cusps for maxillary teeth and buccal cusps for mandibular teeth. If this functional cusp bevel is not present and the crown is cast to replicate the correct size of the tooth, bulk of material may be too little at this point to withstand occlusal surfaces.Axial reduction
This should allow enough thickness for the material chosen. Depending on the type of crown to be fitted, there is a minimum preparation thickness. Generally, full metal crowns require at least 0.5mm, whist metal-ceramic and full ceramic crowns require at least 1.2mmMarginal integrity
In order for the cast restoration to last in the oral environment and to protect the underlying tooth structure, the margins between cast and tooth preparation need to be as closely adapted. The marginal line design and position should facilitate plaque control, allow for adequate thickness of the restorative material chosen therefore providing enough strength for the crown at the margin. Several types of finish line configurations have been advocated, each having some advantages and disadvantages (see the table below). Chamfer finish are normally advocated for full metal margins and shoulders are generally required to provide enough bulk for metal-ceramic crowns and full ceramic crown margins. Some evidence suggests adding a bevel to margins, especially where these are heavy, to decrease the distance between the crown and the tooth tissue.Preservation of the periodontium
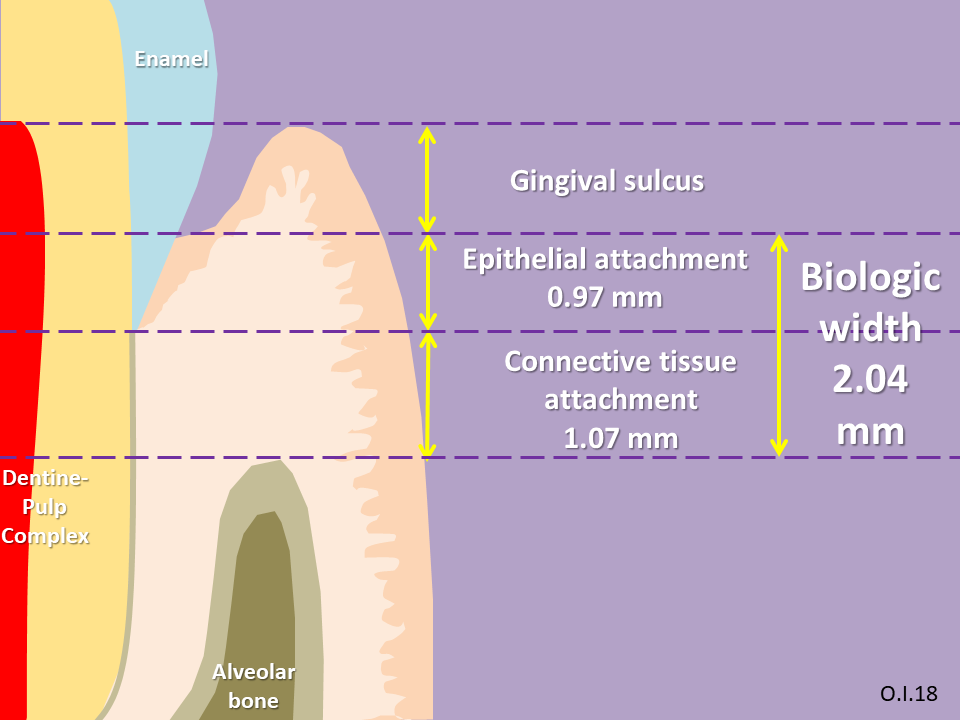 Linked to marginal integrity, placement of the finish line can directly affect the ease of manufacturing the crown and health of the periodontium. Best results are achieved where the finish line is above the gum line as this is fully cleanable. They should also be placed on enamel as this creates a better seal. Where circumstances require the margins to be below the gum line, caution is required as several problems can arise. First, there might be issues in terms of capturing the margin when making impressions during the manufacturing process leading to inaccuracies. Secondly, the
Linked to marginal integrity, placement of the finish line can directly affect the ease of manufacturing the crown and health of the periodontium. Best results are achieved where the finish line is above the gum line as this is fully cleanable. They should also be placed on enamel as this creates a better seal. Where circumstances require the margins to be below the gum line, caution is required as several problems can arise. First, there might be issues in terms of capturing the margin when making impressions during the manufacturing process leading to inaccuracies. Secondly, the 
Special considerations

Ferrule effect
Endodontically-treated teeth, especially those with little sound tooth tissue, are prone to fractures. The successful clinical outcome for these teeth relies not only on adequate root canal treatment, but also on the type of restorative treatment used, including the use of a post and core system and the type of extra-coronal restoration selected. Some evidence advocates the use of a ferrule to optimise the bio-mechanical behaviour of root-filled teeth, especially where a post and core system needs to be used. In dentistry, the ferrule effect is, as defined by Sorensen and Engelman (1990), a "''360° metal collar of the crown surrounding the parallel walls of theStainless steel crowns for posterior primary dentition
Stainless steel preformed metal crowns are the treatment of choice for the restoration of posterior primary teeth. A systemic review found that it has the highest success rate (96.1%). In order to accept a stainless steel crown, the entire occlusal surface should be reduced by 1–1.5 mm and interproximally contacts should be cleared by cutting a thin mesial andHall technique
The Hall technique is a non-invasive treatment for decayed posterior primary teeth where caries are sealed under a preformed stainless steel crown. This technique requires no tooth preparation.Construction and fit of temporary crown restorations
It is very likely that once a tooth has been prepared and whilst waiting for the definitive restoration, the tooth preparation is fitted with a temporary crown.Need for temporary restorations
Temporisation is important after tooth preparation in order to: * Protect from and prevent bacterial invasion of newly exposed dentinal tubules, leading to pulpal inflammation andTypes of temporary crowns
Temporary crowns can be described by: * The expected or planned ''duration'' of temporisation: ** Short term ** Medium term ** Long term * The ''way'' or the ''place'' the temporary restoration is made: ** Direct or chair-side ** Indirect or laboratory-made * The aesthetics or look of the ''material'' of construction ** Metal *** Cast *** Preformed ** Tooth coloured *** Plastic pre-formed (e.g. polycarboxylate and acrylic) *** Resin compositesDuration of temporisation
Temporary crowns can be described as ''short-term'', if used for a few days, ''medium-term'', if their planned use for several weeks and ''long-term'' if their planned use is for several months. The choice in length of temporisation often relates to the complexity of restorative work planned. Short-term temporary crowns are generally appropriate for simple restorative cases whilst complex cases involving more that one tooth often require long-term temporary crowns.Direct vs. indirect restorations
Temporary crowns can either be ''direct'', if constructed by the dentist in the clinic, or ''indirect'' if they are made off-site, usually in a dental laboratory. Generally direct temporary crowns tend to be for short-term use. Where medium-term or long-term temporisation is required, the use of indirect temporary crowns should be considered.Temporary crown materials
There are several materials that can be used to construct temporary crowns. Direct temporary crowns are either made using metal or plastic pre-formed crowns, chemically-cured or light-cured resins or resin composites. Indirect restorations are either made of chemically-cured acrylic, heat-cured acrylic or cast in metal.Cementation of temporary crowns
The purpose of temporary luting agents is to fill the space between the crown preparation and the temporary restoration. Unlike cementation of definitive crowns, temporary crowns should be relatively easy to remove. Adhesive cements should not be used and softer cements are preferred to allow for the easy removal of both temporary cements and crowns. This is crucial as remnants of temporary cement left on the tooth surface can compromise gingival health and interfere with accurate seating of the final restoration and permanent cement attachment. Provisional cements should also be strong enough to avoid being deformed or fractured during the provisional period. Zinc Oxide Eugenol (ZOE) temporary luting cements These are commonly used because of their low tensile strength and lack of adhesion which provides ease of removal. These products should not be used when resin composite is to be planned for bonding the definitive crown as eugenol is able to infiltrate and diffuse through dentine; contaminating tooth surface and compromising bonding by inhibiting polymerisation of resin. Commercially available products include RelyX Temp E (3M ESPE), Temp-Bond (Kerr) and Flow Temp (Premier Dental Products). Non-eugenol temporary luting cements Non-eugenol cements replace eugenol with several types of carboxylic acids which do not inhibit definitive cementation. These cements are compatible with temporary resin materials and definitive resin cements and have increased retention when compared to ZOE containing cements. Examples of commercially available products include RelyX Temp NE (3M ESPE) and Temp-Bond NE (Kerr). Polycarboxylate temporary luting cements This hydrophilic cement has the benefit of minimal effects on temporary resin containing agents and weak adhesion to tooth tissue which increases ease of removal. This cement is the easiest to clean out of all the provisional cement types. Examples include Ultradent and Hy-Bond (Shofu Dental). Resin temporary luting cements The advantages of these cements include superior aesthetics, greater strength, superb retention and ease of cleaning. However, amongst the drawbacks of this cement is the higher rate of discolouration, microleakage and odour experienced. Commercially available examples of temporary resins cements include Systemp.link (Ivoclar Vivadent), Temp-Bond Clear (Kerr) and ImProv (Nobel Biocare).Tooth preparation impressions
Once the tooth in question has been prepared with acceptable dimensions, it is equally important to make an accurate and dimensionally stable record or impression of the preparation or dental implant, surrounding hard and soft tissues as well as the opposing dental arch so that the restoration created will conform to the required dimensions and ensure the fit is as close as possible without having to make many modifications chair-side. Impressions can be made digitally or by conventional technique. With regards to conventional impression techniques, the materials selected should have appropriate physical properties and handling characteristics to allow enough detail reproduction and durability when casting a model, including the ability to withstand effective decontamination procedures. Generally, impressions of the arch where the preparation is made are in addition silicone using the "wash impression" technique; impressions of the opposing arch are made in alginate. Digital impressions can be made using dedicated optical scanners. A review suggests that digital impressions provide the same accuracy as conventional impressions and are found to be more comfortable for patients and easier for dental practitioners.
Crown manufacture using CAD/CAM
* CERECChairside CAD/CAM dentistry
TheCrown removal

Matrix bands
Application of a matrix band which is burnished into the undercuts and pulled vertically.Ultrasonic
An ultrasonic tip can be applied to a cast metal crown to disrupt the cement lute. This method should be avoided with ceramic restorations as this may lead to fractures.Forceps and crown tractors
Crown tractors and forceps can be used to grip the restoration and dislodge it from the tooth preparation. Crown tractors are designed to have rubber grips and powder on their beaks to reduce the risk of damaging ceramic restorations. Crown tractors are quite effective in removing crowns luted with temporary cements.Sticky sweet method or Richwill crown and bridge remover
A thermoplastic pliable resin is softened in warm water then placed on the occlusal surface of the crown to be removed. The patient is then asked to bite down, compressing the resin block to two-thirds of its original thickness. The patient is then asked to open the mouth quickly, which should generate enough force to displace the restoration. This method however, is not very effective and has a risk of damaging restorations on or accidentally extracting the opposing tooth. Therefore, before using this method, it is important to look at the state of the opposing tooth.Tapping and pneumatic tools
Sliding hammers work by using a tip to engage the crown margin and sliding the weight along the shaft and tapping this to loosen the restoration. Several versions are available. Some are weighted, others are spring loaded. This system is uncomfortable for the patient and is not always successful. It is also contraindicated for periodontically involved teeth, as it can cause unwanted extractions. This system can also damage the ceramic margins.Wedging devices
A slot is cut using the side of a long tapered bur, normally on the buccal surface of the crown, all the way into the cement lute. A flat plastic instrument, straight Warrick James, Couplands elevators or dedicated systems such as the WamKey, is inserted into the slot created to wedge the crown apart from the tooth.Metalift crown and bridge removal system
Based on the "jack-screw" principle, the Metalift system works by drilling a precision channel through the occlusal surface of a cast restoration, then with a special bur, the area around the periphery of the hole is undermined before a threaded screw is wound into the space. As the screw comes in contact with the core of the restoration, the continued rotation of the screw results in a jacking force that displaces the crown from the preparation. This system can be used to remove both all metal crowns and metal-ceramic crowns, although, with metal-ceramic crowns care should be taken to remove enough ceramic from the area where the hole created to reduce the chances of fracture. The minimum thickness of metal required for the lifting action is approximately 0.5mm. The damage can repaired with a plastic filling material.Burs
The crown can be simply sectioned using a bur.History
There is evidence of gold dental prosthesis dating back to the Etruscans. Ancient Roman dentists also adopted these tools.See also
* Pediatric crownsReferences
External links
*Dental Health: Dental Crowns
Videos from Sheffield University showing the production of a cast gold crown
{{Authority control Prosthodontology Restorative dentistry