|
Uremic Pericarditis
Uremic pericarditis is a form of pericarditis. It causes fibrinous pericarditis. The main cause of the disease is poorly understood.Black, R. 2011. 0. . Signs and symptoms Fibrinous pericarditis is an exudative inflammation. The pericardium is infiltrated by the fibrinous exudate. This consists of fibrin strands and leukocytes. Fibrin describes an amorphous, eosinophilic (pink) network. Leukocytes (white blood cells; mainly neutrophils) are found within the fibrin deposits and intrapericardic. Vascular congestion is also present. Inflammatory cells do not penetrate the myocardium (as is seen with other presentations of pericarditis), and as a result, this particular variant does not present with diffuse ST elevation on ECG (a classic sign of pericarditis known as stage I ECG changes which are seen with other causes) because the inflammatory cells do not penetrate the myocardium. To naked eye examination, this pathology is referred to as having a "Bread and Butter Appearance". Pat ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Pericarditis
Pericarditis is inflammation of the pericardium, the fibrous sac surrounding the heart. Symptoms typically include sudden onset of sharp chest pain, which may also be felt in the shoulders, neck, or back. The pain is typically less severe when sitting up and more severe when lying down or breathing deeply. Other symptoms of pericarditis can include fever, weakness, palpitations, and shortness of breath. The onset of symptoms can occasionally be gradual rather than sudden. The cause of pericarditis often remains unknown but is believed to be most often due to a viral infection. Other causes include bacterial infections such as tuberculosis, uremic pericarditis, heart attack, cancer, autoimmune disorders, and chest trauma. Diagnosis is based on the presence of chest pain, a pericardial rub, specific electrocardiogram (ECG) changes, and fluid around the heart. A heart attack may produce similar symptoms to pericarditis. Treatment in most cases is with NSAIDs and possibly the ant ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Exudative
An exudate is a fluid emitted by an organism through pores or a wound, a process known as exuding or exudation. ''Exudate'' is derived from ''exude'' 'to ooze' from Latin ''exsūdāre'' 'to (ooze out) sweat' (''ex-'' 'out' and ''sūdāre'' 'to sweat'). Medicine An exudate is any fluid that filters from the circulatory system into lesions or areas of inflammation. It can be a pus-like or clear fluid. When an injury occurs, leaving skin exposed, it leaks out of the blood vessels and into nearby tissues. The fluid is composed of serum, fibrin, and leukocytes. Exudate may ooze from cuts or from areas of infection or inflammation. Types * Purulent or suppurative exudate consists of plasma with both active and dead neutrophils, fibrinogen, and necrotic parenchymal cells. This kind of exudate is consistent with more severe infections, and is commonly referred to as pus. * Fibrinous exudate is composed mainly of fibrinogen and fibrin. It is characteristic of rheumatic carditis, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving immune cells, blood vessels, and molecular mediators. The function of inflammation is to eliminate the initial cause of cell injury, clear out necrotic cells and tissues damaged from the original insult and the inflammatory process, and initiate tissue repair. The five cardinal signs are heat, pain, redness, swelling, and Functio laesa, loss of function (Latin ''calor'', ''dolor'', ''rubor'', ''tumor'', and ''functio laesa''). Inflammation is a generic response, and therefore it is considered as a mechanism of innate immune system, innate immunity, as compared to adaptive immune system, adaptive immunity, which is specific for each pathogen. Too little inflammation could lead to progressive tissue destruction by the harmful stimulus (e.g. b ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Fibrin
Fibrin (also called Factor Ia) is a fibrous, non-globular protein involved in the clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerize. The polymerized fibrin, together with platelets, forms a hemostatic plug or clot over a wound site. When the lining of a blood vessel is broken, platelets are attracted, forming a platelet plug. These platelets have thrombin receptors on their surfaces that bind serum thrombin molecules, which in turn convert soluble fibrinogen in the serum into fibrin at the wound site. Fibrin forms long strands of tough insoluble protein that are bound to the platelets. Factor XIII completes the cross-linking of fibrin so that it hardens and contracts. The cross-linked fibrin forms a mesh atop the platelet plug that completes the clot. Fibrin was discovered by Marcello Malpighi in 1666. Role in disease Excessive generation of fibrin due to activation of the coagulation cascade leads to thrombos ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Leukocytes
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from multipotent cells in the bone marrow known as hematopoietic stem cells. Leukocytes are found throughout the body, including the blood and lymphatic system. All white blood cells have nuclei, which distinguishes them from the other blood cells, the anucleated red blood cells (RBCs) and platelets. The different white blood cells are usually classified by cell lineage ( myeloid cells or lymphoid cells). White blood cells are part of the body's immune system. They help the body fight infection and other diseases. Types of white blood cells are granulocytes (neutrophils, eosinophils, and basophils), and agranulocytes (monocytes, and lymphocytes (T cells and B cells)). Myeloid cells (myelocytes) include neutrophils, eosinophils, mast cells, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
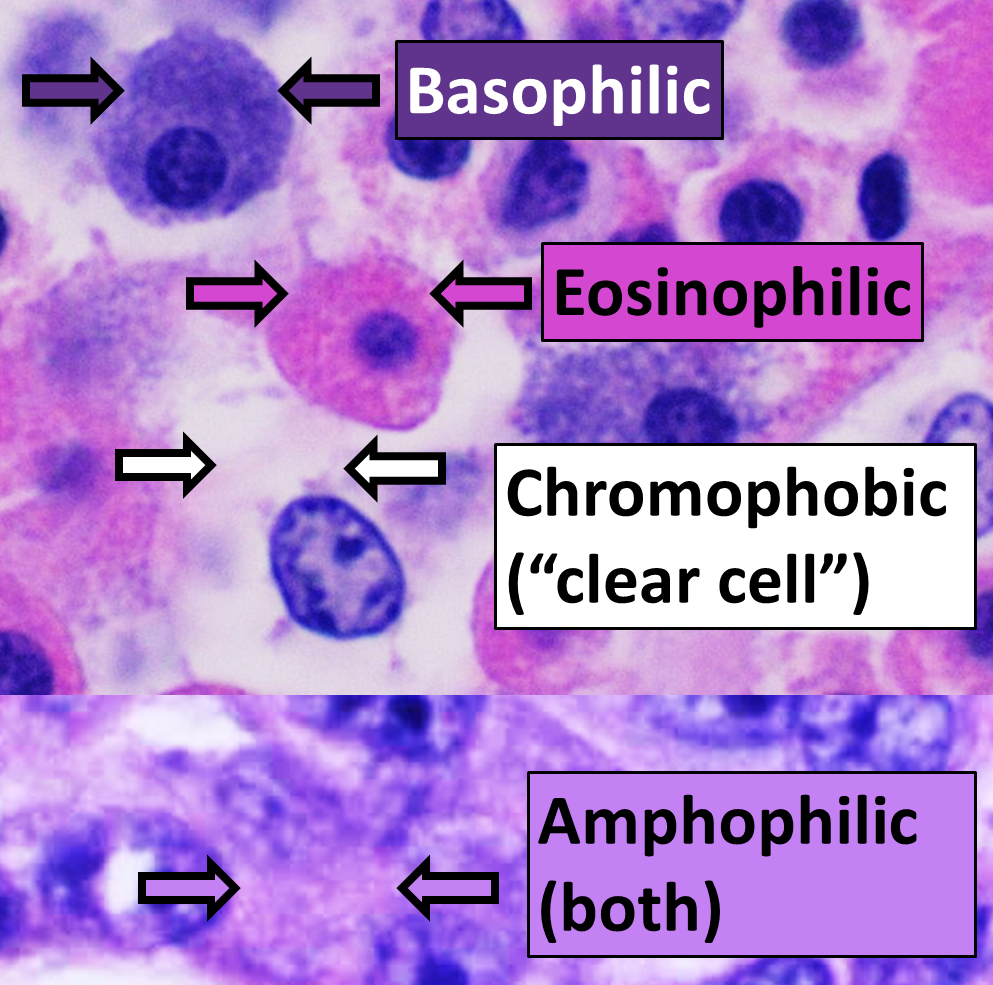
Eosinophilic
Eosinophilic (Greek suffix -phil-, meaning ''loves eosin'') is the staining of tissues, cells, or organelles after they have been washed with eosin, a dye. Eosin is an acidic dye for staining cell cytoplasm, collagen, and muscle fibers. ''Eosinophilic'' describes the appearance of cells and structures seen in histological sections that take up the staining dye eosin. Such eosinophilic structures are, in general, composed of protein. Eosin is usually combined with a stain called hematoxylin to produce a hematoxylin- and eosin-stained section (also called an H&E stain, HE or H+E section). It is the most widely used histological stain for a medical diagnosis. When a pathologist examines a biopsy of a suspected cancer, they will stain the biopsy with H&E. Some structures seen inside cells are described as being eosinophilic; for example, Lewy and Mallory bodies. [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Neutrophils
Neutrophils (also known as neutrocytes or heterophils) are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying in different animals. They are formed from stem cells in the bone marrow and differentiated into subpopulations of neutrophil-killers and neutrophil-cagers. They are short-lived and highly mobile, as they can enter parts of tissue where other cells/molecules cannot. Neutrophils may be subdivided into segmented neutrophils and banded neutrophils (or bands). They form part of the polymorphonuclear cells family (PMNs) together with basophils and eosinophils. The name ''neutrophil'' derives from staining characteristics on hematoxylin and eosin ( H&E) histological or cytological preparations. Whereas basophilic white blood cells stain dark blue and eosinophilic white blood cells stain bright red, neutrophils stain a neutral pink. Normally, n ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Myocardium
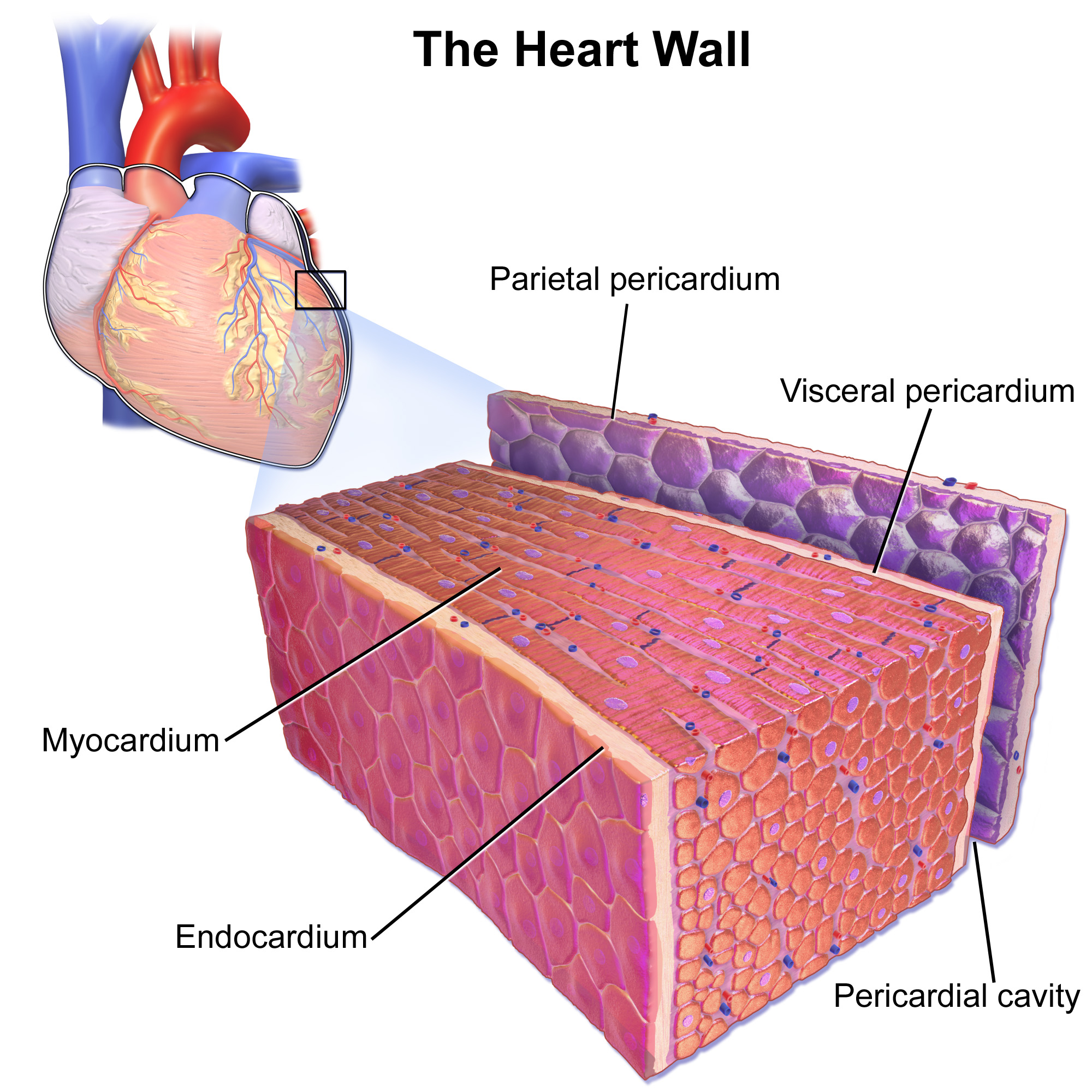
Cardiac muscle (also called heart muscle, myocardium, cardiomyocytes and cardiac myocytes) is one of three types of vertebrate muscle tissues, with the other two being skeletal muscle and smooth muscle. It is an involuntary, striated muscle that constitutes the main tissue of the wall of the heart. The cardiac muscle (myocardium) forms a thick middle layer between the outer layer of the heart wall (the pericardium) and the inner layer (the endocardium), with blood supplied via the coronary circulation. It is composed of individual cardiac muscle cells joined by intercalated discs, and encased by collagen fibers and other substances that form the extracellular matrix. Cardiac muscle contracts in a similar manner to skeletal muscle, although with some important differences. Electrical stimulation in the form of a cardiac action potential triggers the release of calcium from the cell's internal calcium store, the sarcoplasmic reticulum. The rise in calcium causes the cell's m ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Pathology
Pathology is the study of the causes and effects of disease or injury. The word ''pathology'' also refers to the study of disease in general, incorporating a wide range of biology research fields and medical practices. However, when used in the context of modern medical treatment, the term is often used in a narrower fashion to refer to processes and tests that fall within the contemporary medical field of "general pathology", an area which includes a number of distinct but inter-related medical specialties that diagnose disease, mostly through analysis of tissue, cell, and body fluid samples. Idiomatically, "a pathology" may also refer to the predicted or actual progression of particular diseases (as in the statement "the many different forms of cancer have diverse pathologies", in which case a more proper choice of word would be " pathophysiologies"), and the affix ''pathy'' is sometimes used to indicate a state of disease in cases of both physical ailment (as in cardiomy ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Azotemia
Azotemia (''azot'', "nitrogen" + '' -emia'', "blood condition") is a medical condition characterized by abnormally high levels of nitrogen-containing compounds (such as urea, creatinine, various body waste compounds, and other nitrogen-rich compounds) in the blood. It is largely related to insufficient or dysfunctional filtering of blood by the kidneys. It can lead to uremia and acute kidney injury (kidney failure) if not controlled. Types Azotemia has three classifications, depending on its causative origin: prerenal azotemia, renal azotemia, and postrenal azotemia. Measurements of urea and creatinine (Cr) in the blood are used to assess renal function. For historical reasons, the lab test measuring urea is known as "blood urea nitrogen" (BUN). The BUN:Cr ratio is a useful measure in determining the type of azotemia and will be discussed in each section below. A normal BUN:Cr is equal to 15. Prerenal azotemia Prerenal azotemia is caused by a decrease in blood flow (hypoperfusion ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Kidney Failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as either acute kidney failure, which develops rapidly and may resolve; and chronic kidney failure, which develops slowly and can often be irreversible. Symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications of acute and chronic failure include uremia, high blood potassium, and volume overload. Complications of chronic failure also include heart disease, high blood pressure, and anemia. Causes of acute kidney failure include low blood pressure, blockage of the urinary tract, certain medications, muscle breakdown, and hemolytic uremic syndrome. Causes of chronic kidney failure include diabetes, high blood pressure, nephrotic syndrome, and polycystic kidney disease. Diagnosis of acute failure ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hemodialysis
Hemodialysis, also spelled haemodialysis, or simply dialysis, is a process of purifying the blood of a person whose kidneys are not working normally. This type of dialysis achieves the extracorporeal removal of waste products such as creatinine and urea and free water from the blood when the kidneys are in a state of kidney failure. Hemodialysis is one of three renal replacement therapies (the other two being kidney transplant and peritoneal dialysis). An alternative method for extracorporeal separation of blood components such as plasma or cells is apheresis. Hemodialysis can be an outpatient or inpatient therapy. Routine hemodialysis is conducted in a dialysis outpatient facility, either a purpose-built room in a hospital or a dedicated, stand-alone clinic. Less frequently hemodialysis is done at home. Dialysis treatments in a clinic are initiated and managed by specialized staff made up of nurses and technicians; dialysis treatments at home can be self-initiated and managed ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |




.jpg)

