|
Single Umbilical Artery
Occasionally, there is only the one single umbilical artery (SUA) present in the umbilical cord. This is sometimes also called a two-vessel umbilical cord, or two-vessel cord. Approximately, this affects between 1 in 100 and 1 in 500 pregnancies, making it the most common umbilical abnormality. Its cause is not known. Most cords have one vein and two arteries. The vein carries oxygenated blood from the placenta to the baby and the arteries carry deoxygenated blood from the baby to the placenta. In approximately 1% of pregnancies there are only two vessels —usually a single vein and single artery. In about 75% of those cases, the baby is entirely normal and healthy. One artery can support a pregnancy and does not necessarily indicate problems. For the other 25%, a 2-vessel cord is a sign that the baby has other abnormalities—sometimes life-threatening and sometimes not. Doctors and midwives often suggest parents take the added precaution of having regular growth scans near term ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Umbilical Cord
In placental mammals, the umbilical cord (also called the navel string, birth cord or ''funiculus umbilicalis'') is a conduit between the developing embryo or fetus and the placenta. During prenatal development, the umbilical cord is physiologically and genetically part of the fetus and (in humans) normally contains two arteries (the umbilical arteries) and one vein (the umbilical vein), buried within Wharton's jelly. The umbilical vein supplies the fetus with oxygenated, nutrient-rich blood from the placenta. Conversely, the fetal heart pumps low-oxygen, nutrient-depleted blood through the umbilical arteries back to the placenta. Structure and development The umbilical cord develops from and contains remnants of the yolk sac and allantois. It forms by the fifth week of development, replacing the yolk sac as the source of nutrients for the embryo. The cord is not directly connected to the mother's circulatory system, but instead joins the placenta, which transfers materi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
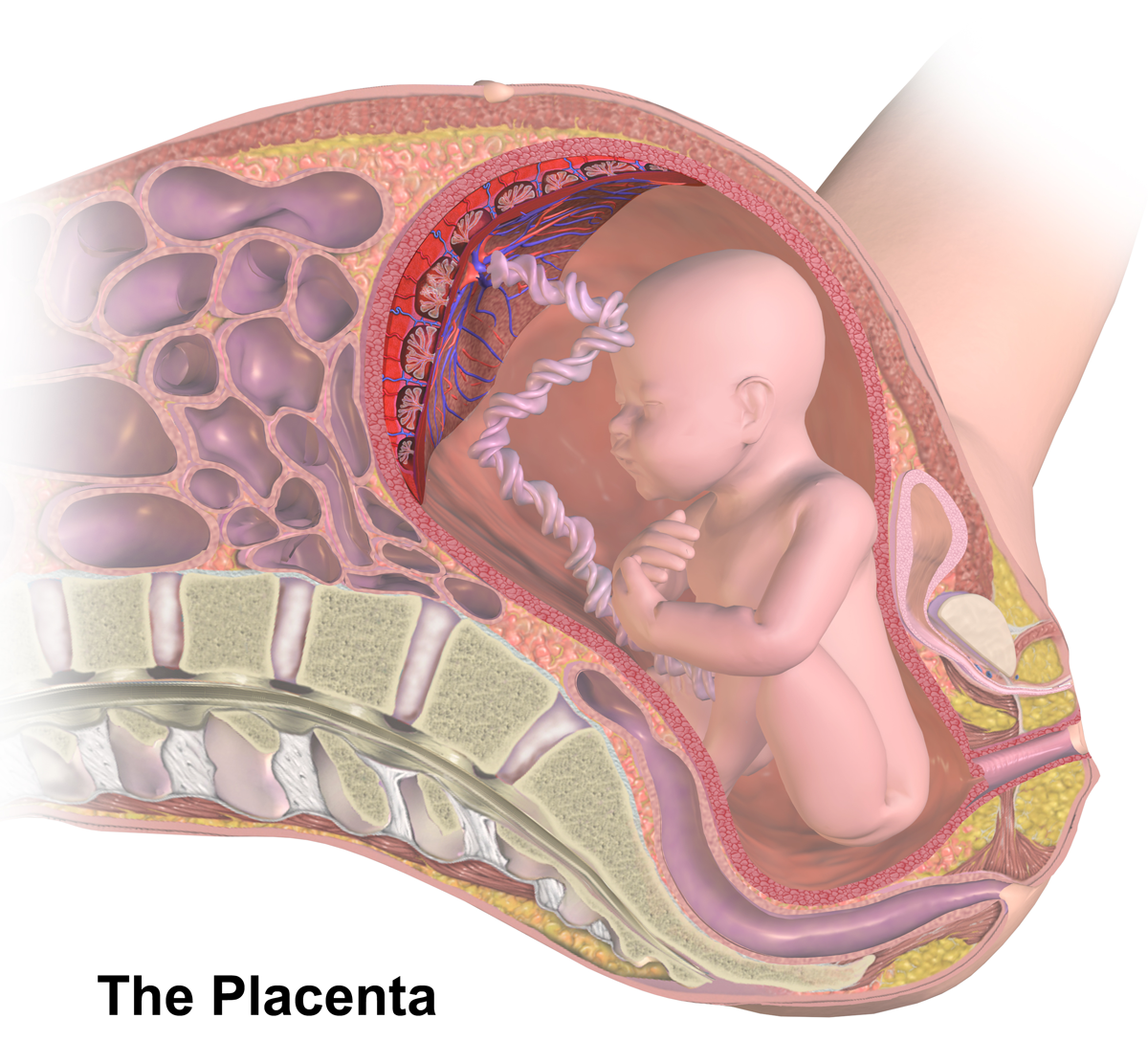
Placenta
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual ( endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth (sometimes incorrectly referred to as the 'maternal part' of the placenta). Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development. Mammalian placentas probably first evolved about 150 million to 200 millio ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Midwives
A midwife is a health professional who cares for mothers and newborns around childbirth, a specialization known as midwifery. The education and training for a midwife concentrates extensively on the care of women throughout their lifespan; concentrating on being experts in what is normal and identifying conditions that need further evaluation. In most countries, midwives are recognized as skilled healthcare providers. Midwives are trained to recognize variations from the normal progress of labor and understand how to deal with deviations from normal. They may intervene in high risk situations such as breech births, twin births, and births where the baby is in a posterior position, using non-invasive techniques. For complications related to pregnancy and birth that are beyond the midwife's scope of practice, including surgical and instrumental deliveries, they refer their patients to physicians or surgeons. In many parts of the world, these professions work in tandem to provid ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Intrauterine Growth Restriction
Intrauterine growth restriction (IUGR), or fetal growth restriction, refers to poor growth of a fetus while in the womb during pregnancy. IUGR is defined by clinical features of malnutrition and evidence of reduced growth regardless of an infant's birth weight percentile. The causes of IUGR are broad and may involve maternal, fetal, or placental complications. At least 60% of the 4 million neonatal deaths that occur worldwide every year are associated with low birth weight (LBW), caused by intrauterine growth restriction (IUGR), preterm delivery, and genetic abnormalities, demonstrating that under-nutrition is already a leading health problem at birth. Intrauterine growth restriction can result in a baby being small for gestational age (SGA), which is most commonly defined as a weight below the 10th percentile for the gestational age. At the end of pregnancy, it can result in a low birth weight. Types There are two major categories of IUGR: pseudo IUGR and true IUGR With pseud ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Congenital Abnormalities
A birth defect, also known as a congenital disorder, is an abnormal condition that is present at birth regardless of its cause. Birth defects may result in disabilities that may be physical, intellectual, or developmental. The disabilities can range from mild to severe. Birth defects are divided into two main types: structural disorders in which problems are seen with the shape of a body part and functional disorders in which problems exist with how a body part works. Functional disorders include metabolic and degenerative disorders. Some birth defects include both structural and functional disorders. Birth defects may result from genetic or chromosomal disorders, exposure to certain medications or chemicals, or certain infections during pregnancy. Risk factors include folate deficiency, drinking alcohol or smoking during pregnancy, poorly controlled diabetes, and a mother over the age of 35 years old. Many are believed to involve multiple factors. Birth defects may be visib ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Edwards Syndrome
Edwards syndrome, also known as trisomy 18, is a genetic disorder caused by the presence of a third copy of all or part of chromosome 18. Many parts of the body are affected. Babies are often born small and have heart defects. Other features include a small head, small jaw, clenched fists with overlapping fingers, and severe intellectual disability. Most cases of Edwards syndrome occur due to problems during the formation of the reproductive cells or during early development. The rate of disease increases with the mother's age. Rarely, cases may be inherited from a person's parents. Occasionally, not all cells have the extra chromosome, known as mosaic trisomy, and symptoms in these cases may be less severe. An ultrasound during pregnancy can increase suspicion for the condition, which can be confirmed by amniocentesis. Treatment is supportive. After having one child with the condition, the risk of having a second is typically around one percent. It is the second-most com ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Echocardiogram
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart. It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound. Echocardiography has become routinely used in the diagnosis, management, and follow-up of patients with any suspected or known heart diseases. It is one of the most widely used diagnostic imaging modalities in cardiology. It can provide a wealth of helpful information, including the size and shape of the heart (internal chamber size quantification), pumping capacity, location and extent of any tissue damage, and assessment of valves. An echocardiogram can also give physicians other estimates of heart function, such as a calculation of the cardiac output, ejection fraction, and diastolic function (how well the heart relaxes). Echocardiography is an important tool in assessing wall motion abnormality in patients with suspected cardiac disease. It is a tool which helps in reaching an earl ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Chorionic Villus Sampling
Chorionic villus sampling (CVS), sometimes called "chorionic ''villous'' sampling" (as "villous" is the adjectival form of the word "villus"), is a form of prenatal diagnosis done to determine chromosomal or genetic disorders in the fetus. It entails sampling of the chorionic villus (placental tissue) and testing it for chromosomal abnormalities, usually with FISH or PCR. CVS usually takes place at 10–12 weeks' gestation, earlier than amniocentesis or percutaneous umbilical cord blood sampling. It is the preferred technique before 15 weeks. CVS was performed for the first time in Milan by Italian biologist Giuseppe Simoni, scientific director of Biocell Center, in 1983. Use as early as eight weeks in special circumstances has been described. It can be performed in a transcervical or transabdominal manner. Although this procedure is mostly associated with testing for Down syndrome, overall, CVS can detect more than 200 disorders. Indications Possi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Amniocentesis
Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation. In this procedure, a thin needle is inserted into the abdomen of the pregnant woman. The needle punctures the amnion, which is the membrane that surrounds the developing fetus. The fluid within the amnion is called amniotic fluid, and because this fluid surrounds the developing fetus, it contains fetal cells. The amniotic fluid is sampled and analyzed via methods such as karyotyping and DNA analysis technology for genetic abnormalities. An amniocentesis is typically performed in the second trimester between the 15th and 20th week of gestation. Women who choose to have this test are pri ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |