|
Effective Circulating Volume
The effective circulating volume (ECV) is the volume of arterial blood effectively perfusing tissue. ECV is a dynamic quantity and not a measurable, distinct compartment. This concept is useful for discussion of cardiovascular and renal physiology. Though ECV normally varies with extracellular fluid (ECF), they become uncoupled in diseases, such as congestive heart failure (CHF) or hepatic cirrhosis. In such cases, decreased ECV may lead to volume depletion responses and edema. Decreased ECV can stimulate renin secretion or stimulate a sympathetic nervous system response or prostaglandin release (all of which help mediate renal blood flow and glomerular filtration rate among other things). See also * Blood plasma Blood plasma is a light amber-colored liquid component of blood in which blood cells are absent, but contains proteins and other constituents of whole blood in suspension. It makes up about 55% of the body's total blood volume. It is the intra ... References {{re ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Arterial
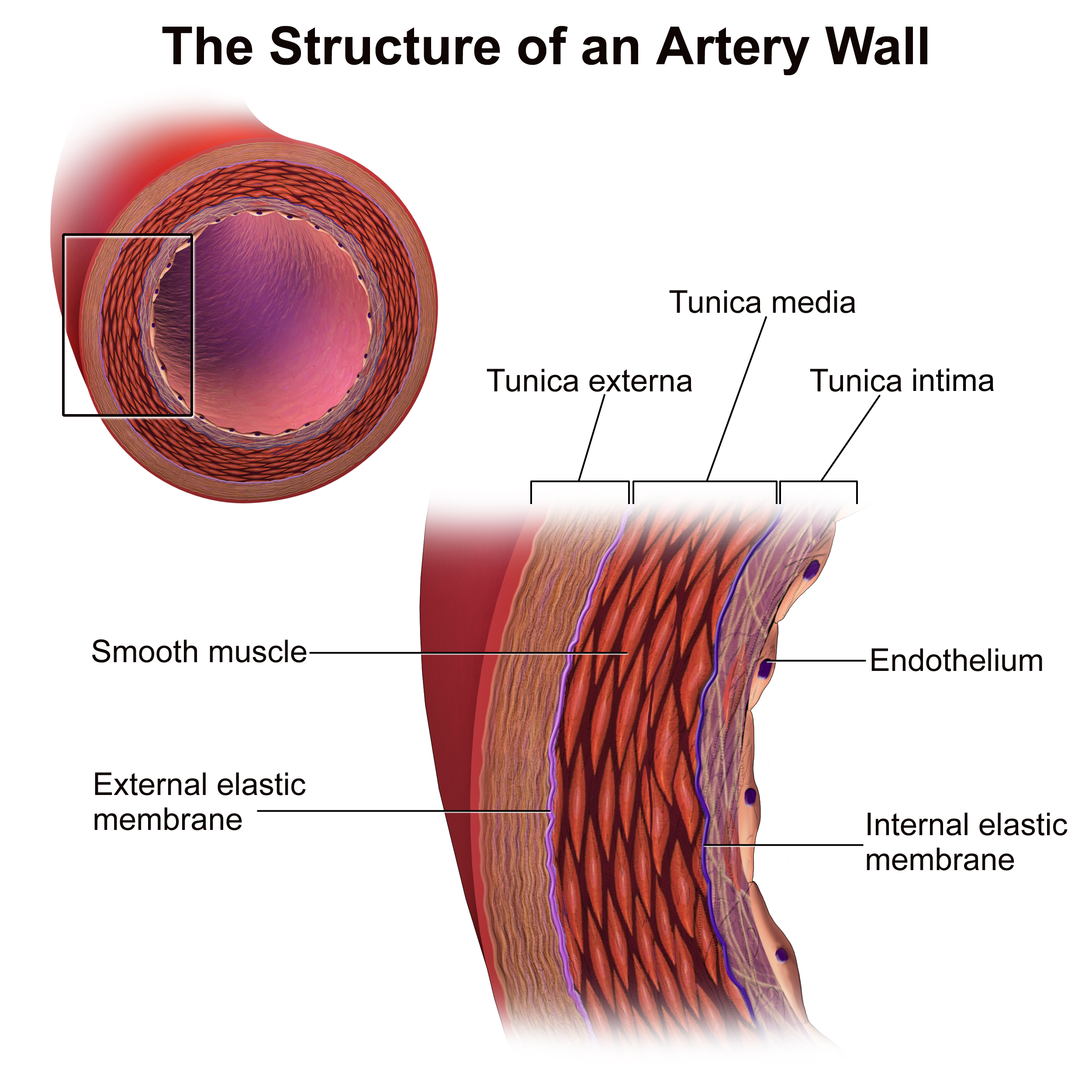
An artery (plural arteries) () is a blood vessel in humans and most animals that takes blood away from the heart to one or more parts of the body (tissues, lungs, brain etc.). Most arteries carry oxygenated blood; the two exceptions are the pulmonary and the umbilical arteries, which carry deoxygenated blood to the organs that oxygenate it (lungs and placenta, respectively). The effective arterial blood volume is that extracellular fluid which fills the arterial system. The arteries are part of the circulatory system, that is responsible for the delivery of oxygen and nutrients to all cells, as well as the removal of carbon dioxide and waste products, the maintenance of optimum blood pH, and the circulation of proteins and cells of the immune system. Arteries contrast with veins, which carry blood back towards the heart. Structure The anatomy of arteries can be separated into gross anatomy, at the macroscopic level, and microanatomy, which must be studied with a microscop ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the circulatory system is also known as ''peripheral blood'', and the blood cells it carries, ''peripheral blood cells''. Blood is composed of blood cells suspended in blood plasma. Plasma, which constitutes 55% of blood fluid, is mostly water (92% by volume), and contains proteins, glucose, mineral ions, hormones, carbon dioxide (plasma being the main medium for excretory product transportation), and blood cells themselves. Albumin is the main protein in plasma, and it functions to regulate the colloidal osmotic pressure of blood. The blood cells are mainly red blood cells (also called RBCs or erythrocytes), white blood cells (also called WBCs or leukocytes) and platelets (also called thrombocytes). The most abundant cells in vertebrate blo ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Perfusion
Perfusion is the passage of fluid through the circulatory system or lymphatic system to an organ or a tissue, usually referring to the delivery of blood to a capillary bed in tissue. Perfusion is measured as the rate at which blood is delivered to tissue, or volume of blood per unit time (blood flow) per unit tissue mass. The SI unit is m3/(s·kg), although for human organs perfusion is typically reported in ml/min/g. The word is derived from the French verb "perfuser" meaning to "pour over or through". All animal tissues require an adequate blood supply for health and life. Poor perfusion (malperfusion), that is, ischemia, causes health problems, as seen in cardiovascular disease, including coronary artery disease, cerebrovascular disease, peripheral artery disease, and many other conditions. Tests verifying that adequate perfusion exists are a part of a patient's assessment process that are performed by medical or emergency personnel. The most common methods include evalua ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cardiovascular
The blood circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, that consists of the heart and blood vessels (from Greek ''kardia'' meaning ''heart'', and from Latin ''vascula'' meaning ''vessels''). The circulatory system has two divisions, a systemic circulation or circuit, and a pulmonary circulation or circuit. Some sources use the terms ''cardiovascular system'' and ''vascular system'' interchangeably with the ''circulatory system''. The network of blood vessels are the great vessels of the heart including large elastic arteries, and large veins; other arteries, smaller arterioles, capillaries that join with venules (small veins), and other veins. The circulatory system is closed in vertebrates, which means that the blood never leaves the network of blood vessels. Some invertebrates such as arthro ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Renal Physiology
Renal physiology (Latin ''rēnēs'', "kidneys") is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D. Much of renal physiology is studied at the level of the nephron, the smallest functional unit of the kidney. Each nephron begins with a filtration component that filters the blood entering the kidney. This filtrate then flows along the length of the nephron, which is a tubular structure lined by a single layer of specialized cells and surrounded by capillaries. The major functions of these lining cells are the reabsorption of water and small molecules from the filtrate into the blood, and the secretion of wastes f ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Extracellular Fluid
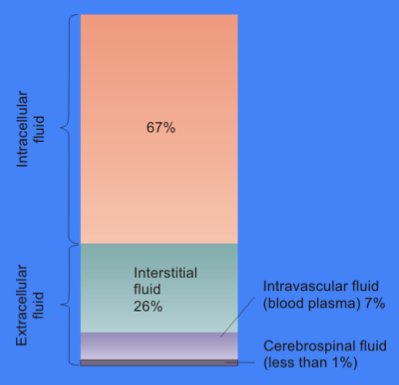
In cell biology, extracellular fluid (ECF) denotes all body fluid outside the cells of any multicellular organism. Total body water in healthy adults is about 60% (range 45 to 75%) of total body weight; women and the obese typically have a lower percentage than lean men. Extracellular fluid makes up about one-third of body fluid, the remaining two-thirds is intracellular fluid within cells. The main component of the extracellular fluid is the interstitial fluid that surrounds cells. Extracellular fluid is the internal environment of all multicellular animals, and in those animals with a blood circulatory system, a proportion of this fluid is blood plasma. Plasma and interstitial fluid are the two components that make up at least 97% of the ECF. Lymph makes up a small percentage of the interstitial fluid. The remaining small portion of the ECF includes the transcellular fluid (about 2.5%). The ECF can also be seen as having two components – plasma and lymph as a delivery system ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Congestive Heart Failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, and leg swelling. The shortness of breath may occur with exertion or while lying down, and may wake people up during the night. Chest pain, including angina, is not usually caused by heart failure, but may occur if the heart failure was caused by a heart attack. The severity of the heart failure is measured by the severity of symptoms during exercise. Other conditions that may have symptoms similar to heart failure include obesity, kidney failure, liver disease, anemia, and thyroid disease. Common causes of heart failure include coronary artery disease, heart attack, high blood pressure, atrial fibrillation, valvular heart disease, excessive alcohol consumption, infection, and cardiomyopathy. These cause heart failure by altering ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage causes tissue repair and subsequent formation of scar tissue, which over time can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen may become spontaneously infected. More serious complications include hepatic encephalopathy, bleeding from dilated veins ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Volume Depletion
Hypovolemia, also known as volume depletion or volume contraction, is a state of abnormally low extracellular fluid in the body. This may be due to either a loss of both salt and water or a decrease in blood volume. Hypovolemia refers to the loss of extracellular fluid and should not be confused with dehydration. Hypovolemia is caused by a variety of events, but these can be simplified into two categories: those that are associated with kidney function and those that are not. The signs and symptoms of hypovolemia worsen as the amount of fluid lost increases. Immediately or shortly after mild fluid loss (from blood donation, diarrhea, vomiting, bleeding from trauma, etc.), one may experience headache, fatigue, weakness, dizziness, or thirst. Untreated hypovolemia or excessive and rapid losses of volume may lead to hypovolemic shock. Signs and symptoms of hypovolemic shock include increased heart rate, low blood pressure, pale or cold skin, and altered mental status. When these s ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Edema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's Tissue (biology), tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area may feel heavy, and joint stiffness. Other symptoms depend on the underlying cause. Causes may include Chronic venous insufficiency, venous insufficiency, heart failure, kidney problems, hypoalbuminemia, low protein levels, liver problems, deep vein thrombosis, infections, angioedema, certain medications, and lymphedema. It may also occur after prolonged sitting or standing and during menstruation or pregnancy. The condition is more concerning if it starts suddenly, or pain or shortness of breath is present. Treatment depends on the underlying cause. If the underlying mechanism involves Hypernatremia, sodium retention, decreased salt intake and a diuretic may be used. Elevating the legs and support stockings may be useful ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Renin
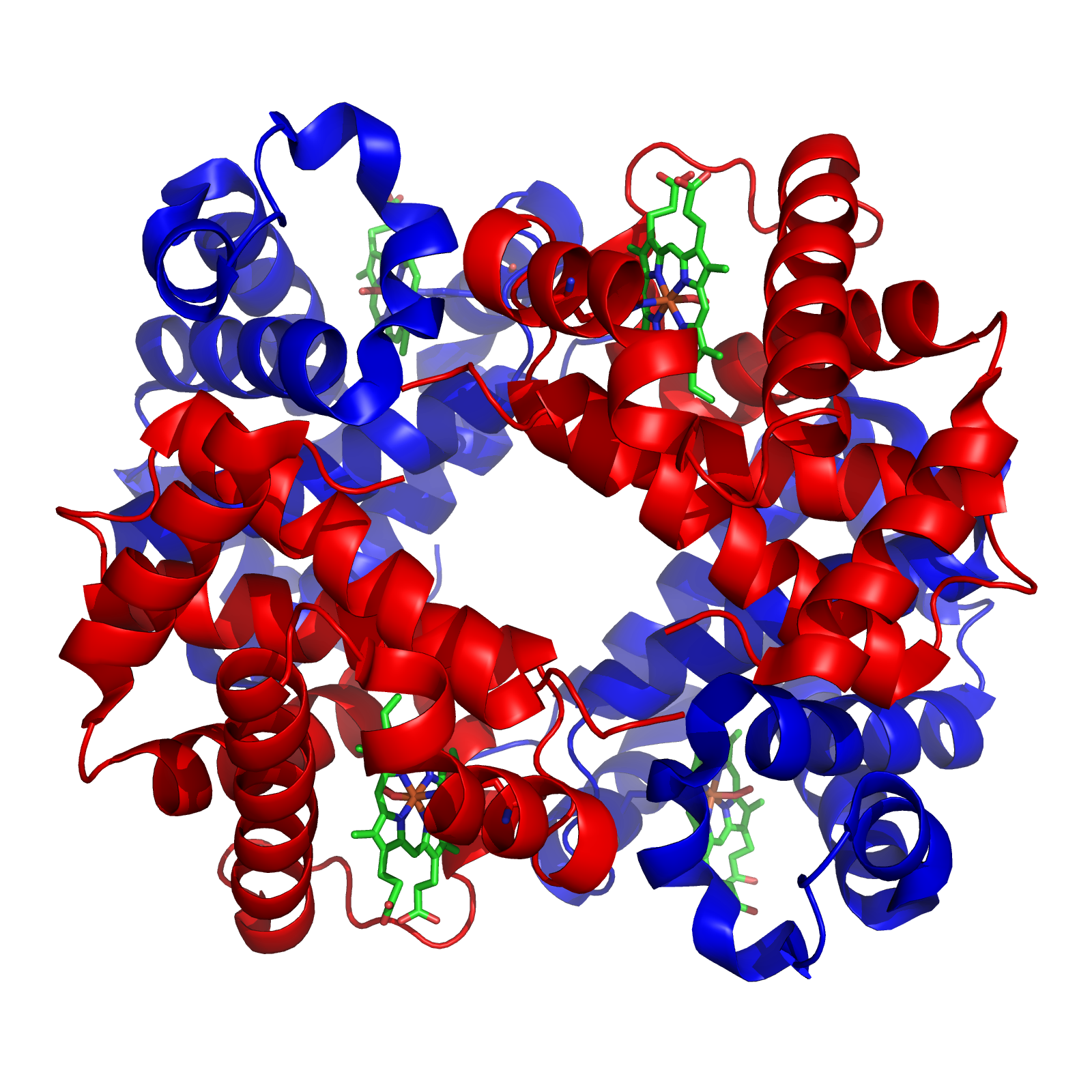
Renin (etymology and pronunciation), also known as an angiotensinogenase, is an aspartic protease protein and enzyme secreted by the kidneys that participates in the body's renin–angiotensin–aldosterone system (RAAS)—also known as the renin–angiotensin–aldosterone axis—that increases the volume of extracellular fluid (blood plasma, lymph and interstitial fluid) and causes arterial vasoconstriction. Thus, it increases the body's mean arterial blood pressure. Renin is not commonly referred to as a hormone, albeit it having a receptor, the (pro)renin receptor, also known as the renin receptor and prorenin receptor (see also below), as well as enzymatic activity with which it hydrolyzes angiotensinogen to angiotensin I. Biochemistry and physiology Structure The primary structure of renin precursor consists of 406 amino acids with a pre- and a pro-segment carrying 20 and 46 amino acids, respectively. Mature renin contains 340 amino acids and has a mass of 37 kDa. ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Sympathetic Nervous System
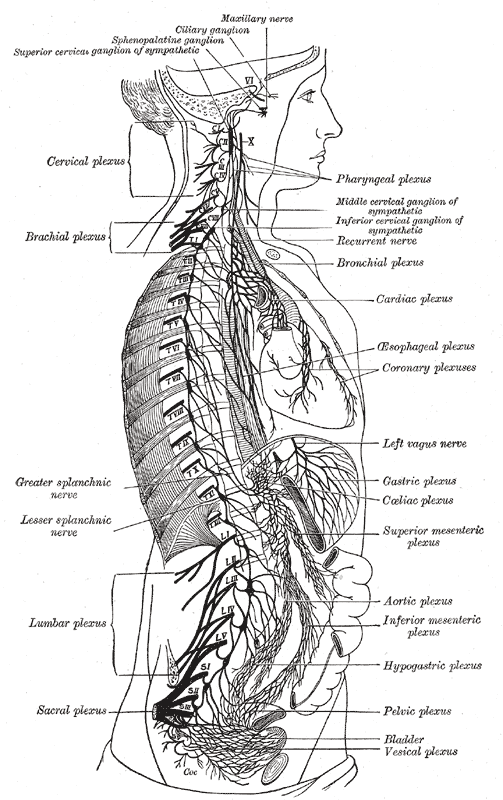
The sympathetic nervous system (SNS) is one of the three divisions of the autonomic nervous system, the others being the parasympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system. The autonomic nervous system functions to regulate the body's unconscious actions. The sympathetic nervous system's primary process is to stimulate the body's fight or flight response. It is, however, constantly active at a basic level to maintain homeostasis. The sympathetic nervous system is described as being antagonistic to the parasympathetic nervous system which stimulates the body to "feed and breed" and to (then) "rest-and-digest". Structure There are two kinds of neurons involved in the transmission of any signal through the sympathetic system: pre-ganglionic and post-ganglionic. The shorter preganglionic neurons originate in the thoracolumbar division o ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |