Hepatic Hydrothorax on:
[Wikipedia]
[Google]
[Amazon]
Hepatic hydrothorax is a rare form of

 The most noticeable symptoms are usually those of cirrhosis and
The most noticeable symptoms are usually those of cirrhosis and

pleural effusion
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung.
Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per kilog ...
that occurs in people with liver cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, chronic liver failure or chronic hepatic failure and end-stage liver disease, is a chronic condition of the liver in which the normal functioning tissue, or parenchyma, is replaced ...
. It is defined as an effusion of over 500 mL in people with liver cirrhosis that is not caused by heart, lung, or pleural disease. It is found in 5–10% of people with liver cirrhosis and 2–3% of people with pleural effusions. In cases of decompensated liver cirrhosis, prevalence rises significantly up to 90%. Over 85% of cases occurring on the right, 13% on the left, and 2% on both. Although it is most common in people with severe ascites
Ascites (; , meaning "bag" or "sac") is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdo ...
, it can also occur in people with mild or no ascites. Symptoms are not specific and mostly involve the respiratory system.
The condition is diagnosed based on the existence of liver cirrhosis and fluid build-up in the abdomen (ascites) and analysis of the fluid. The fluid has a low protein content. Mainly, the condition is treated by medical management, such as diet adjustment and usage of diuretics
A diuretic () is any substance that promotes diuresis, the increased production of urine. This includes forced diuresis. A diuretic tablet is sometimes colloquially called a water tablet. There are several categories of diuretics. All diuretics in ...
. When the condition does not respond, it is known as refractory hepatic hydrothorax: treatment includes inserting a transjugular intrahepatic portosystemic shunt
Transjugular intrahepatic portosystemic shunt (TIPS or TIPSS) is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension (which is ...
(TIPS). The only curative treatment is a liver transplant
Liver transplantation or hepatic transplantation is the replacement of a Liver disease, diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for Cirrhosis, end-stage liver disease and ...
. The prognosis is usually unfavorable, especially in refractory cases, due to the majority of people being unsuitable for transplantation. However, transplantation indicates a favorable prognosis; one case study showed that the condition had no effect on post-transplant outcomes.
Symptoms
The condition has no specific symptoms, as it occurs with ascites and other manifestations of increased pressure in the portal vein caused by liver disease. Pleural fluid causes symptoms far more easily than ascitic fluid, due to the lower volume of the pleural cavity as compared to the abdominal cavity. The main symptoms are usually related to the symptoms of liver cirrhosis and ascites. Less often, it may be the only manifestation of chronic liver disease. The symptoms depend on many factors, such as the effusion's volume, how fast it accumulates, and the presence of cardiopulmonary disease. The condition may cause no symptoms and be incidentally detected by medical scans, or it may cause large pleural effusions that result in respiratory symptoms like cough, shortness of breath, low blood oxygen, and respiratory failure. In general, people are more sensitive to pleural effusions then ascites; much smaller effusions can cause symptoms. Most people have progressive difficulty breathing and reduced exercise tolerance. Rarely, there may be acute cases that accumulate fluid rapidly and result in circulatory collapse.
Causes
The condition is caused by portal hypertension resulting from liver disease. The causative mechanism is unknown, but several have been proposed, which are similar to those behind ascites. The most accepted theory is that fluid originating fromascites
Ascites (; , meaning "bag" or "sac") is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdo ...
travels through defects in the diaphragm into the pleural cavity. These defects exist in the normal population. The defects are usually less than and are more common on the right side, possibly because of the increased prevalence of tendon tissue from its proximity to the liver. Through a microscope, they look like discontinuities in the bundles of collagen that make up the tendon part of the diaphragm. In hepatic hydrothorax, the pressure created by ascites and the thinning of the diaphragm caused by malnutrition cause the defects to become larger. Blebs of peritoneum can herniate through these defects; if they burst, a pleuroperitoneal communication is created. Fluid moves from the abdomen to the pleural cavity via a pressure gradient
In hydrodynamics and hydrostatics, the pressure gradient (typically of air but more generally of any fluid) is a physical quantity that describes in which direction and at what rate the pressure increases the most rapidly around a particular locat ...
between the cavities. If the fluid accumulates faster than it can leave via pleural membrane absorption, hepatic hydrothorax results.
Diagnosis
 The most noticeable symptoms are usually those of cirrhosis and
The most noticeable symptoms are usually those of cirrhosis and portal hypertension
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5� ...
. Most affected people show signs of end-stage liver disease. Diagnosis involves extracting the fluid via thoracentesis; after this, the fluid is analyzed to diagnose and rule out other causes. The fluid can be analyzed for serum, protein, albumin, lactate dehydrogenase, and cell count. The fluid is a transudate
Transudate is extravascular fluid with low protein content and a low specific gravity (< 1.012). It has low nucleated cell counts (less than 500 to 1000 per microliter) and the primary cell types are mononuclear leukocyte, mononuclear cells: macrop ...
and similar to fluid found in ascites. There may be a higher protein and albumin content in hepatic hydrothorax due to the pleura absorbing the water. To rule out heart-related causes of pleural effusion, an echocardiogram
Echocardiography, also known as cardiac ultrasound, is the use of ultrasound to examine the heart. It is a type of medical imaging, using standard ultrasound or Doppler ultrasound. The visual image formed using this technique is called an echo ...
can be performed. Pleuroperitoneal communications are best detected by peritoneal scintigraphy. Hydrothorax without ascites has been reported to occur in as many as 20% of people with cirrhosis but is only detected in 7% of cases via CT scan and ultrasound.
The condition can be mistaken for a chylothorax, which can also occur in people with cirrhosis. Additionally, the fluid in chylothorax is much higher in triglycerides, and has a milky appearance. Another, more serious differential diagnosis, is spontaneous bacterial empyema, carrying a high death rate even with treatment. However, the fluid has a much higher neutrophil
Neutrophils are a type of phagocytic white blood cell and part of innate immunity. More specifically, they form the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. Their functions vary in differe ...
concentration than in hepatic hydrothorax. Spontaneous bacterial empyema can occur even without ascites. Additionally, there may be other symptoms of infection, such as fever.
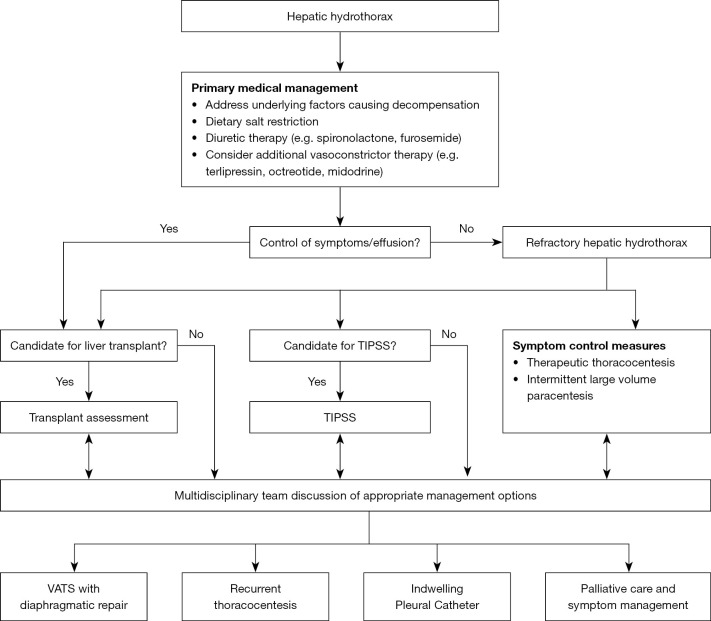
Management
As the condition is caused by leaking ascitic fluid, treatment centers around managing ascites and decompensated liver disease. Some individuals respond to medical management. In up to 26% of cases, the condition does not respond to medical management, in which case it is known as a refractory hepatic hydrothorax. For these individuals, the first treatment of choice is the insertion of a transjugular intrahepatic portosystemic shunt. The only curative treatment is aliver transplant
Liver transplantation or hepatic transplantation is the replacement of a Liver disease, diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for Cirrhosis, end-stage liver disease and ...
. Additionally, treatment involves addressing the underlying cause of the liver disease, such as alcohol use or viral hepatitis.
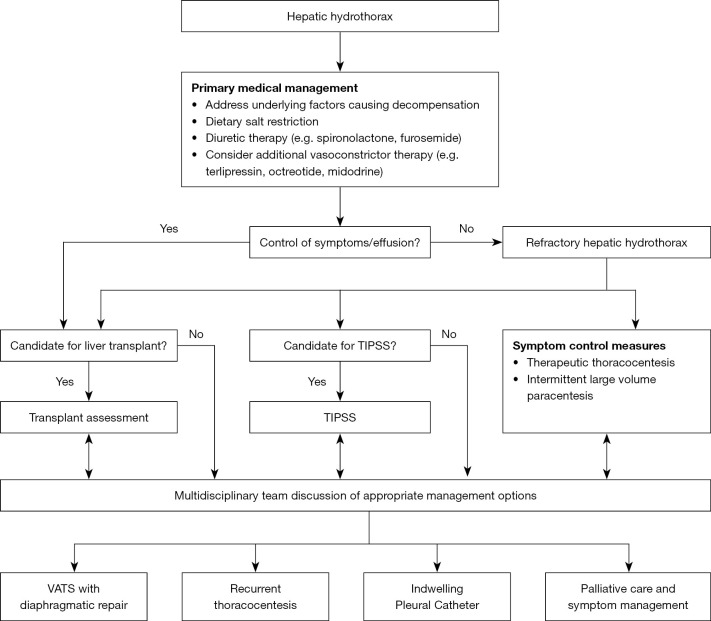
Medical management
Medical management is the main treatment. Although it is simple, cheap, and noninvasive, it has a high rate of failure and comes with a risk ofacute kidney injury
Acute kidney injury (AKI), previously called acute renal failure (ARF), is a sudden decrease in renal function, kidney function that develops within seven days, as shown by an increase in serum creatinine or a decrease in urine output, or both.
...
and kidney failure. Reducing sodium in the diet and using diuretics may help reduce ascites and stop the growth of the effusion. The goal of medical management is a low sodium diet of 70-90 mmol per day and to lose.5 kg/day of weight for patients without edema, and 1 kg/day for patients with edema. Usually, diet modification is not enough; then, diuretics are the next line of treatment. A distal agent and a loop diuretic can be used together to cause the kidneys to excrete least 120 mEq/day of sodium via urine. Aldosterone receptor antagonists like spironolactone
Spironolactone, sold under the brand name Aldactone among others, is classed as a diuretic medication. It can be used to treat edema, fluid build-up due to hepatic cirrhosis, liver disease or kidney disease. It is also used to reduce risk o ...
work by reducing the absorption of sodium in distal kidney tubules. A loop diuretic is added if there is insufficient response. The amount of sodium excreted in urine is monitored before and during treatment to adjust diuretic dosage based on response. Additionally, vasoconstrictors, such as midodrine
Midodrine, sold under the brand names ProAmatine and Orvaten among others, is an antihypotensive medication used to treat orthostatic hypotension (low blood pressure when standing) and urinary incontinence. It is taken oral administration, by m ...
, may help increase salt output by the kidneys.

Refractory hepatic hydrothorax
For people with refractory hepatic hydrothorax, the only definite treatment is aliver transplant
Liver transplantation or hepatic transplantation is the replacement of a Liver disease, diseased liver with the healthy liver from another person (allograft). Liver transplantation is a treatment option for Cirrhosis, end-stage liver disease and ...
. However, the majority of people with this condition are unsuitable for transplantation, and the majority of those who have died awaiting it. However, other treatments can improve symptoms, increase survival, and, ideally, give time until a liver transplant is available. Suitability for liver transplantation is determined by the UKELD score; a score >49 indicates need for transplant listing. Additional indicators include empyema development and a failing synthetic liver.
Transjugular intrahepatic portosystemic shunt
The main treatment in those with refractory hepatic hydrothorax is the insertion of a transjugular intrahepatic portosystemic shunt (TIPS). TIPS decompresses the portal system, reducing portal venous pressure and fluid in the abdomen; it is estimated to work in 70-80% of cases. However, it does not improve the prognosis in those with end-stage liver disease. In people with serious liver dysfunction, TIPS may cause liver failure, as it shunts blood away from the liver.Thoracentesis
Thoracentesis, though typically safe, only provides temporary benefit, as fluid tends to return quickly. Other possible complications may include pain, empyema,hemothorax
A hemothorax (derived from hemo- lood+ thorax hest plural ''hemothoraces'') is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may inc ...
, and subcutaneous emphysema. Repeat usage of thoracentesis increases the risk of complications; a review has indicated that the cumulative risk of complications such as pneumothorax and hemothorax approaches 12%. In cases with ascites, initially performing paracentesis
Paracentesis (from Ancient Greek, Greek κεντάω, "to pierce") is a form of body fluid sampling procedure, generally referring to peritoneocentesis (also called laparocentesis or abdominal paracentesis) in which the peritoneal cavity is punct ...
to drain the ascitic fluid can help reduce the chance of recurrence.
Other treatments
In cases where TIPS is contraindicated, another treatment option is to insert an indwelling pleural catheter (IPC). Pleural treatments generally have a high complication rate; in a case study, those receiving IPC had greater complication rates despite undergoing significantly less procedures. As a last resort, pleurodesis can be used for people without ascites; by irritating the pleura together, it can repair any defects in the diaphragm. However, it requires multiple procedures and general anesthesia. Additionally, the amount of pleural fluid produced can overcome pleurodesis, causing it to fail. Complications may include empyema, sepsis, and septic shock. Chest tubes and intercostal chest drains are contraindicated, as they can cause loss of protein, infection, pneumothorax, hemothorax, and electrolyte imbalances. Additionally, removing them may pose a challenge, as the fluid returns extremely quickly afterward. Palliative care can also help with symptoms; for people resistant to disease-related treatment, no preferred methods exist to manage symptoms for this condition.Prognosis
Prognosis largely depends on the response to treatment. The median survival time for people with this condition is 8–12 months. The pleural fluid can become infected, resulting in spontaneous bacterial pleuritis. A Child-Pugh score greater than or equal to 10,MELD score
The Model for End-Stage Liver Disease, or MELD, is a scoring system for assessing the severity of chronic liver disease. It was initially developed to predict mortality within three months of surgery in patients who had undergone a transjugular in ...
greater than 15 and higher creatinine levels indicates an increased risk of death. Chest tube usage generally indicates a poor prognosis, with 1-year mortality rates of nearly 90% in one case study. However, if the person successfully responds to TIPS or liver transplantation, the prognosis can be more favorable; the condition does not affect post-transplantation outcomes.
Epidemiology
The condition is found in 5–10% of those with cirrhosis and portal hypertension and 2–3% of all pleural effusions. It is most common in the presence of decompensated cirrhosis.References