|
Thrombocytes
Platelets or thrombocytes () are a part of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping to form a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm from megakaryocytes which reside in bone marrow or lung tissue, and then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates (e.g. birds, amphibians), thrombocytes circulate as intact mononuclear cells. One major function of platelets is to contribute to hemostasis: the process of stopping bleeding at the site where the lining of vessels (endothelium) has been interrupted. Platelets gather at the site and, unless the interruption is physically too large, they plug the hole. First, platelets attach to substances outside the interrupted endothelium: ''adhesion''. Second, they change shape, turn on receptors and secrete chemical messengers: ''activation''. Third, they connect to each other thr ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Platelet Response Animation
Platelets or thrombocytes () are a part of blood whose function (along with the coagulation#Coagulation factors, coagulation factors) is to react to bleeding from blood vessel injury by clumping to form a thrombus, blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm from megakaryocytes which reside in bone marrow or Lung, lung tissue, and then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates (e.g. birds, amphibians), thrombocytes circulate as intact agranulocyte, mononuclear cells. One major function of platelets is to contribute to hemostasis: the process of stopping bleeding at the site where the lining of vessels (endothelium) has been interrupted. Platelets gather at the site and, unless the interruption is physically too large, they plug the hole. First, platelets attach to substances outside the interrupted endothelium: ''adhesion (medicine), adhesion''. Second, they change shape, turn on receptors and secret ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Platelet Inhibition
Platelets or thrombocytes () are a part of blood whose function (along with the coagulation factors) is to react to bleeding from blood vessel injury by clumping to form a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm from megakaryocytes which reside in bone marrow or lung tissue, and then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates (e.g. birds, amphibians), thrombocytes circulate as intact mononuclear cells. One major function of platelets is to contribute to hemostasis: the process of stopping bleeding at the site where the lining of vessels ( endothelium) has been interrupted. Platelets gather at the site and, unless the interruption is physically too large, they plug the hole. First, platelets attach to substances outside the interrupted endothelium: '' adhesion''. Second, they change shape, turn on receptors and secrete chemical messengers: ''activation''. Third, they connect to each other ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Blood
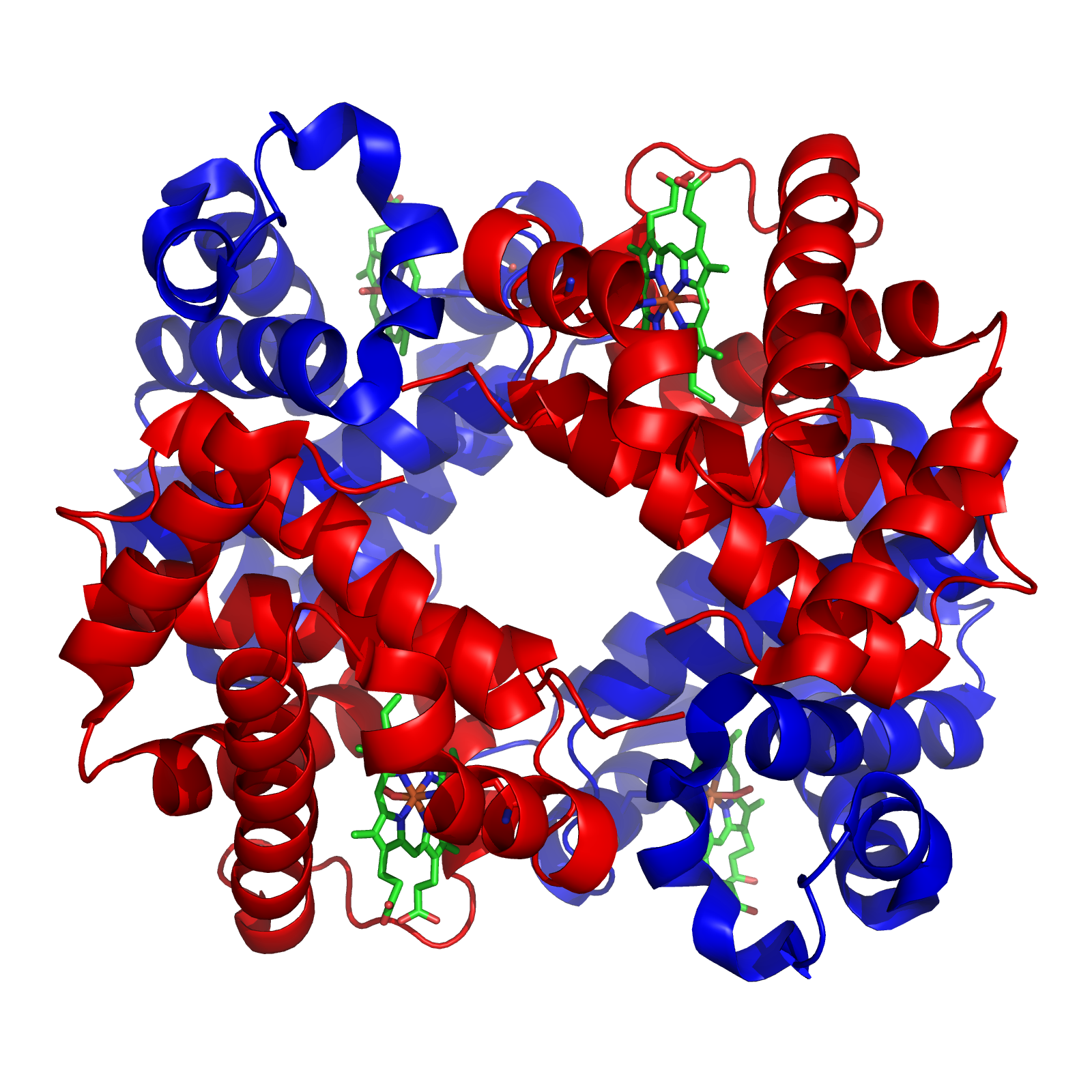
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood is composed of blood cells suspended in blood plasma. Plasma, which constitutes 55% of blood fluid, is mostly water (92% by volume), and contains proteins, glucose, mineral ions, and hormones. The blood cells are mainly red blood cells (erythrocytes), white blood cells (leukocytes), and (in mammals) platelets (thrombocytes). The most abundant cells are red blood cells. These contain hemoglobin, which facilitates oxygen transport by reversibly binding to it, increasing its solubility. Jawed vertebrates have an adaptive immune system, based largely on white blood cells. White blood cells help to resist infections and parasites. Platelets are important in the clotting of blood. Blood is circulated around the body through blood vessels by the ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Platelet Plug
The platelet plug, also known as the hemostatic plug or platelet thrombus, is an aggregation of platelets formed during early stages of hemostasis in response to one or more injuries to blood vessel walls. After platelets are recruited and begin to accumulate around the breakage, their “sticky” nature allows them to adhere to each other. This forms a platelet plug, which prevents more blood from leaving the body as well as any outside contaminants from getting in. The plug provides a temporary blockage of the break in the vasculature. As such, platelet plug formation occurs after vasoconstriction of the blood vessels but before the creation of the fibrin mesh clot, which is the more permanent solution to the injury. The result of the platelet plug formation is the coagulation of blood. It can also be referred to as primary hemostasis. History For many years, the critical role that platelets (also known as thrombocytes) played in hemostasis and blood coagulation went unnotic ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Megakaryocyte
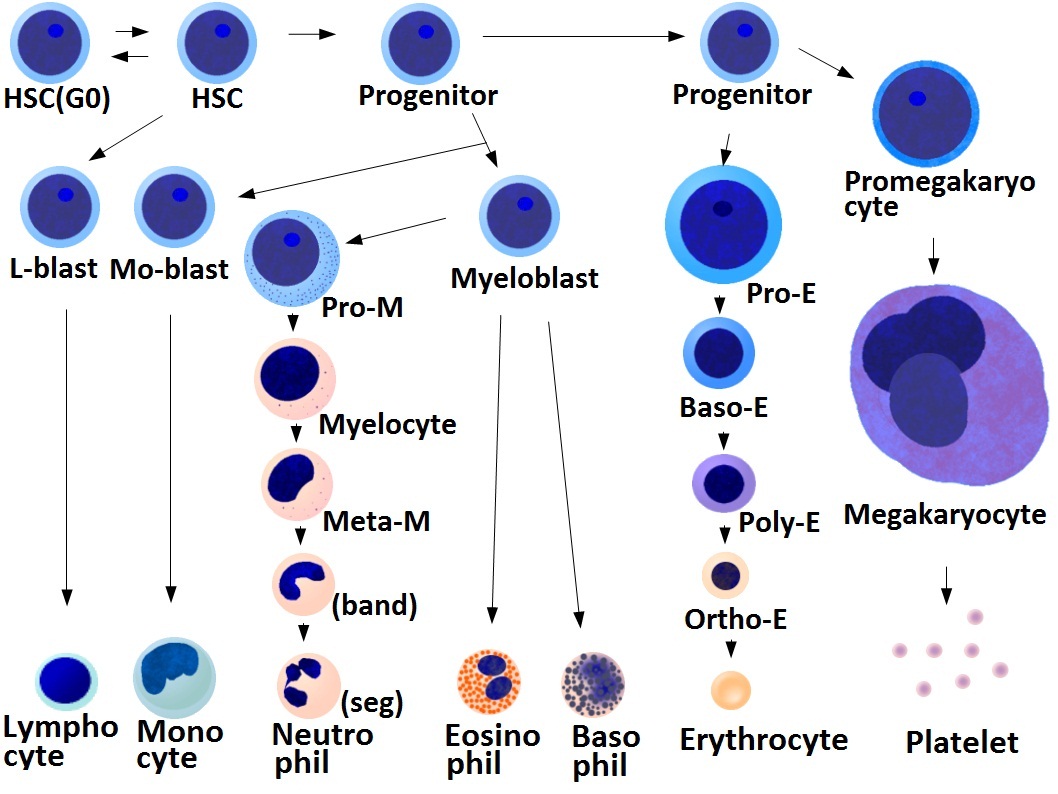
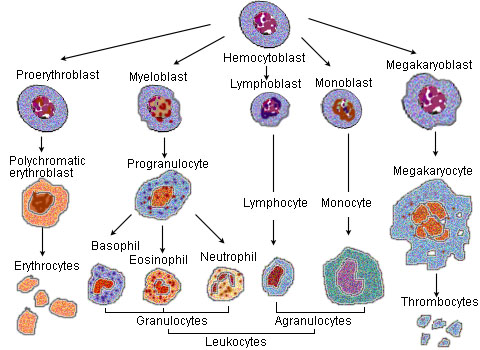
A megakaryocyte () is a large bone marrow cell with a lobation, lobated nucleus that produces blood platelets (thrombocytes), which are necessary for normal blood coagulation, clotting. In humans, megakaryocytes usually account for 1 out of 10,000 bone marrow cells, but can increase in number nearly 10-fold during the course of certain diseases. Owing to variations in neoclassical compound, combining forms and spelling, synonyms include megalokaryocyte and megacaryocyte. Structure In general, megakaryocytes are 10 to 15 times larger than a typical red blood cell, averaging 50–100 μm in diameter. During its maturation, the megakaryocyte grows in size and replicates its DNA without cytokinesis in a process called mitosis#Errors and other variations, endomitosis. As a result, the nucleus of the megakaryocyte can become very large and lobulated, which, under a light microscope, can give the false impression that there are several nuclei. In some cases, the nucleus may contain up to ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Bone Marrow
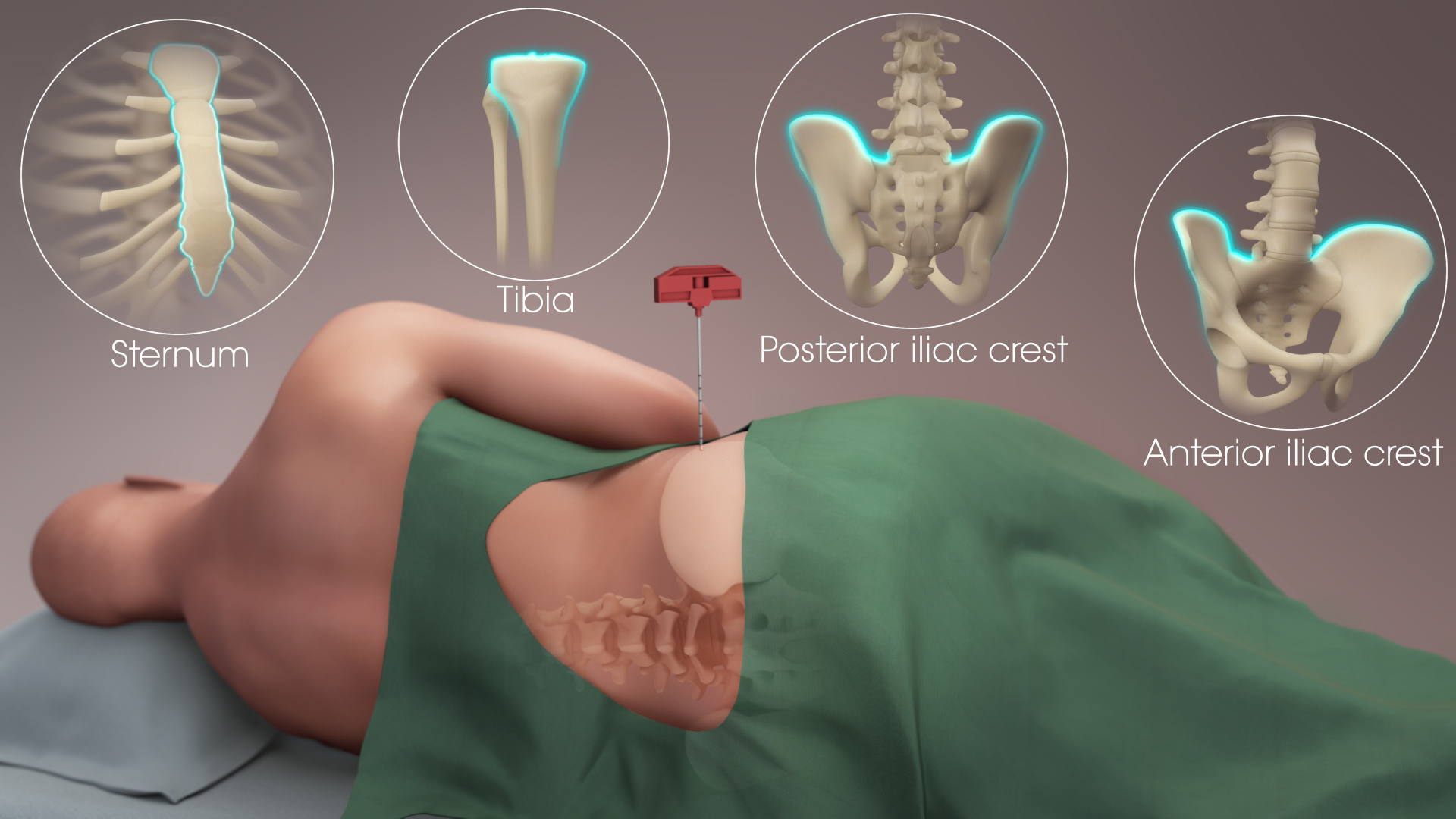
Bone marrow is a semi-solid biological tissue, tissue found within the Spongy bone, spongy (also known as cancellous) portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production (or haematopoiesis). It is composed of Blood cell, hematopoietic cells, marrow adipose tissue, and supportive stromal cells. In adult humans, bone marrow is primarily located in the Rib cage, ribs, vertebrae, sternum, and Pelvis, bones of the pelvis. Bone marrow comprises approximately 5% of total body mass in healthy adult humans, such that a person weighing 73 kg (161 lbs) will have around 3.7 kg (8 lbs) of bone marrow. Human marrow produces approximately 500 billion blood cells per day, which join the Circulatory system, systemic circulation via permeable vasculature sinusoids within the medullary cavity. All types of Hematopoietic cell, hematopoietic cells, including both Myeloid tissue, myeloid and Lymphocyte, lymphoid lineages, are create ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Megakaryocyte
A megakaryocyte () is a large bone marrow cell with a lobation, lobated nucleus that produces blood platelets (thrombocytes), which are necessary for normal blood coagulation, clotting. In humans, megakaryocytes usually account for 1 out of 10,000 bone marrow cells, but can increase in number nearly 10-fold during the course of certain diseases. Owing to variations in neoclassical compound, combining forms and spelling, synonyms include megalokaryocyte and megacaryocyte. Structure In general, megakaryocytes are 10 to 15 times larger than a typical red blood cell, averaging 50–100 μm in diameter. During its maturation, the megakaryocyte grows in size and replicates its DNA without cytokinesis in a process called mitosis#Errors and other variations, endomitosis. As a result, the nucleus of the megakaryocyte can become very large and lobulated, which, under a light microscope, can give the false impression that there are several nuclei. In some cases, the nucleus may contain up to ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Light Microscope
The optical microscope, also referred to as a light microscope, is a type of microscope that commonly uses visible spectrum, visible light and a system of lens (optics), lenses to generate magnified images of small objects. Optical microscopes are the oldest design of microscope and were possibly invented in their present compound form in the 17th century. Basic optical microscopes can be very simple, although many complex designs aim to improve optical resolution, resolution and sample contrast (vision), contrast. The object is placed on a stage and may be directly viewed through one or two eyepieces on the microscope. In high-power microscopes, both eyepieces typically show the same image, but with a stereo microscope, slightly different images are used to create a 3-D effect. A camera is typically used to capture the image (micrograph). The sample can be lit in a variety of ways. Transparent objects can be lit from below and solid objects can be lit with light coming through ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Endothelium
The endothelium (: endothelia) is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel wall. Endothelial cells in direct contact with blood are called vascular endothelial cells whereas those in direct contact with lymph are known as lymphatic endothelial cells. Vascular endothelial cells line the entire circulatory system, from the heart to the smallest capillaries. These cells have unique functions that include fluid filtration, such as in the glomerulus of the kidney, blood vessel tone, hemostasis, neutrophil recruitment, and hormone trafficking. Endothelium of the interior surfaces of the heart chambers is called endocardium. An impaired function can lead to serious health issues throughout the body. Structure The endothelium is a thin layer of single flat (squamous) cells that line the inter ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Adhesion (medicine)
Adhesions are fibrous bands that form between tissues and organs, often as a result of injury during surgery. They may be thought of as internal scar tissue that connects tissues not normally connected. Pathophysiology Adhesions form as a natural part of the body's healing process after surgery in a similar way that a scar forms. The term "adhesion" is applied when the scar extends from within one tissue across to another, usually across a virtual space such as the peritoneal cavity. Adhesion formation post-surgery typically occurs when two injured surfaces are close to one another. According to the "classical paradigm" of adhesion formation, the pathogenesis starts with inflammation and activation of the coagulation system which causes fibrin deposits onto the damaged tissues. The fibrin then connects the two adjacent structures where damage of the tissues occurred. The fibrin acts like a glue to seal the injury and builds the fledgling adhesion, said at this point to be "fi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Fibrin
Fibrin (also called Factor Ia) is a fibrous protein, fibrous, non-globular protein involved in the Coagulation, clotting of blood. It is formed by the action of the protease thrombin on fibrinogen, which causes it to polymerization, polymerize. The polymerized fibrin, together with platelets, forms a hemostasis, hemostatic plug or clot over a wound site. When the lining of a blood vessel is broken, platelets are attracted, forming a platelet plug. These platelets have thrombin receptors on their surfaces that bind serum thrombin molecules, which in turn convert soluble fibrinogen in the serum into fibrin at the wound site. Fibrin forms long strands of tough insoluble protein that are bound to the platelets. Factor XIII completes the cross-linking of fibrin so that it hardens and contracts. The cross-linked fibrin forms a mesh atop the platelet plug that completes the clot. Fibrin was discovered by Marcello Malpighi in 1666. Role in disease Excessive generation of fibrin due ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Ligand (biochemistry)
In biochemistry and pharmacology, a ligand is a substance that forms a complex with a biomolecule to serve a biological purpose. The etymology stems from Latin ''ligare'', which means 'to bind'. In protein-ligand binding, the ligand is usually a molecule which produces a signal by binding to a site on a target protein. The binding typically results in a change of conformational isomerism (conformation) of the target protein. In DNA-ligand binding studies, the ligand can be a small molecule, ion, or protein which binds to the DNA double helix. The relationship between ligand and binding partner is a function of charge, hydrophobicity, and molecular structure. Binding occurs by intermolecular forces, such as ionic bonds, hydrogen bonds and Van der Waals forces. The association or docking is actually reversible through dissociation. Measurably irreversible covalent bonding between a ligand and target molecule is atypical in biological systems. In contrast to the definition o ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |