|
Medical Bill
Medical billing is a payment practice within the United States healthcare system. The process involves a healthcare provider obtaining insurance information from a patient and filing, following up on and appealing claims with health insurance companies in order to receive payment for services rendered, such as testing, treatments, and procedures. The same process is used for most insurance companies, whether they are private companies or government sponsored programs. Medical coding reports what the diagnosis and treatment were and prices are applied accordingly. Medical billers are encouraged, but not required by law, to become certified by taking an exam such as the CMRS Exam, RHIA Exam, CPB Exam and others. Certification schools are intended to provide a theoretical grounding for students entering the medical billing field. Some community colleges in the United States offer certificates, or even associate degrees, in the field. Those seeking advancement may be cross-trained ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Healthcare In The United States
The United States far outspends any other nation on health care, measured both in ''per capita'' spending and as a percentage of GDP. Despite this, the country has significantly worse healthcare outcomes when compared to peer nations. The United States is the only developed nation without a system of universal health care, with a large proportion of its population not carrying health insurance, a substantial factor in the country's excess mortality. Healthcare is provided by many distinct organizations, made up of insurance companies, healthcare providers, hospital systems, and independent providers. Health care facilities are largely owned and operated by private sector businesses. 58% of community hospitals in the United States are non-profit, 21% are government-owned, and 21% are for-profit. According to the World Health Organization (WHO), the United States spent $9,403 on health care per capita, and 17.9% on health care as percentage of its GDP in 2014. Healthcare cov ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medical Necessity
Medical necessity is a legal doctrine in the United States related to activities that may be justified as reasonable, necessary, and/or appropriate based on evidence-based clinical standards of care. In contrast, unnecessary health care lacks such justification. Other countries may have medical doctrines or legal rules covering broadly similar grounds. The term clinical medical necessity is also used. Implementations of doctrine Medicare Medicare pays for medical items and services that are "reasonable and necessary" or "appropriate" for a variety of purposes. By statute, Medicare may pay only for items and services that are "reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member" unless there is another statutory authorization for payment. Medicare has a number of policies that describe coverage criteria, including National Coverage Determinations (NCDs) and Local Coverage Determinations (LCD ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Electronic Medical Record
An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information. For several decades, electronic health records (EHRs) have been touted as key to increasing of quality care. Electronic health records are used for other reasons than charting for patients; today, providers are using data from patient records to improve quality outcomes through their care management programs. EHR combines all patients demographics into a large pool, and uses this information to ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Current Procedural Terminology
The Current Procedural Terminology (CPT) code set is a procedural code set developed by the American Medical Association (AMA). It is maintained by the CPT Editorial Panel. The CPT code set describes medical, surgical, and diagnostic services and is designed to communicate uniform information about medical services and procedures among physicians, coders, patients, accreditation organizations, and payers for administrative, financial, and analytical purposes. New editions are released each October, with CPT 2021 being in use since October 2021. It is available in both a standard edition and a professional edition. CPT coding is similar to ICD-10-CM coding, except that it identifies the services rendered, rather than the diagnosis on the claim. Whilst the ICD-10-PCS codes also contains procedure codes, those are only used in the inpatient setting. CPT is identified by the Centers for Medicare and Medicaid Services (CMS) as Level 1 of the Healthcare Common Procedure Coding Syst ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Clinical Coder
A clinical coder—also known as clinical coding officer, diagnostic coder, medical coder, or nosologist—is a health information professional whose main duties are to analyse clinical statements and assign standard codes using a classification system. The Health data produced are an integral part of health information management, and are used by local and national governments, private healthcare organizations and international agencies for various purposes, including medical and health services research, epidemiological studies, health resource allocation, case mix management, public health programming, medical billing, and public education. For example, a clinical coder may use a set of published codes on medical diagnoses and procedures, such as the International Classification of Diseases (ICD), the Healthcare Common procedural Coding System (HCPCS), and Current Procedural Terminology (CPT) for reporting to the health insurance provider of the recipient of the care. The u ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Group Purchasing Organizations
In the United States, a group purchasing organization (GPO) is an entity that is created to leverage the purchasing power of a group of businesses to obtain discounts from vendors based on the collective buying power of the GPO members. Many GPOs are funded by administrative fees that are paid by the vendors that GPOs oversee. Some GPOs are funded by fees paid by the buying members. Some GPOs are funded by a combination of both of these methods. These fees can be set as a percentage of the purchase or set as an annual flat rate. Some GPOs set mandatory participation levels for their members, while others are completely voluntary. Members participate based on their purchasing needs and their level of confidence in what should be competitive pricing negotiated by their GPOs. Group purchasing is used in many industries to purchase raw materials and supplies, but it is common practice in the grocery industry, health care, electronics, industrial manufacturing and agricultura ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medical Billing Infographic
Medicine is the science and practice of caring for a patient, managing the diagnosis, prognosis, prevention, treatment, palliation of their injury or disease, and promoting their health. Medicine encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness. Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technology to diagnose, treat, and prevent injury and disease, typically through pharmaceuticals or surgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others. Medicine has been practiced since prehistoric times, and for most of this time it was an art (an area of skill and knowledge), frequently having connections to the religious and philosophical beliefs of local culture. For example, a medicine man would apply herbs and say prayers for healing, or an ancien ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Out-of-pocket Expenses
An out-of-pocket expense (or out-of-pocket cost, OOP) is the direct payment of money that may or may not be later reimbursed from a third-party source. For example, when operating a vehicle, gasoline, parking fees and tolls are considered out-of-pocket expenses for a trip. Car insurance, oil changes, and interest are not, since the outlay of cash covers expenses accrued over a longer period of time. The services rendered and other in-kind expenses are not considered out-of-pocket expenses; the same goes for depreciation of capital goods or depletion. Organizations often reimburse out-of-pocket expenses incurred on their behalf, especially expenses incurred by employees on their employers' behalf. In the United States, out-of-pocket expenses for such things as charity, medical bills, and education may be deductions on US income taxes, according to IRS regulations. To be out of pocket is to have expended personal resources, often unexpectedly or unfairly, at the end of some ent ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Coinsurance
In insurance, co-insurance or coinsurance is the splitting or spreading of risk among multiple parties. In the United States In the U.S. insurance market, co-insurance is the joint assumption of risk between the insurer and the insured. In title insurance, it also means the sharing of risks between two or more title insurance companies. In health insurance In health insurance, copayment is fixed while co-insurance is the percentage that the insured pays after the insurance policy's deductible is exceeded, up to the policy's stop loss. It can be expressed as a pair of percentages with the insurer's portion stated first, or just a single percentage showing what the insured pays. Once the insured's out-of-pocket expenses equal the stop loss the insurer will assume responsibility for 100% of any additional costs. 70–30, 80–20, and 90–10 insurer-insured co-insurance schemes are common, with stop loss limits of $1,000 to $3,000 after which the insurer covers all expenses. In p ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Deductible
In an insurance policy, the deductible (in British English, the excess) is the amount paid out of pocket by the policy holder before an insurance provider will pay any expenses. In general usage, the term ''deductible'' may be used to describe one of several types of clauses that are used by insurance companies as a threshold for policy payments. Deductibles are typically used to deter the large number of claims that a consumer can be reasonably expected to bear the cost of. By restricting its coverage to events that are significant enough to incur large costs, the insurance firm expects to pay out slightly smaller amounts much less frequently, incurring much higher savings. As a result, insurance premiums are typically cheaper when they involve higher deductibles. For example, health insurance companies offer plans with high premiums and low deductibles, or plans with low premiums and high deductibles. One plan may have a premium of $1,087 a month with a $6,000 deductible, whil ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Copay
A copayment or copay (called a gap in Australian English) is a fixed amount for a covered service, paid by a patient to the provider of service before receiving the service. It may be defined in an insurance policy and paid by an insured person each time a medical service is accessed. It is technically a form of coinsurance, but is defined differently in health insurance where a coinsurance is a percentage payment after the deductible up to a certain limit. It must be paid before any policy benefit is payable by an insurance company. Copayments do not usually contribute towards any policy out-of-pocket maximum, whereas coinsurance payments do. Insurance companies use copayments to share health care costs to prevent moral hazard. It may be a small portion of the actual cost of the medical service but is meant to deter people from seeking medical care that may not be necessary, e.g., an infection by the common cold. In health systems with prices below the market clearing level in w ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
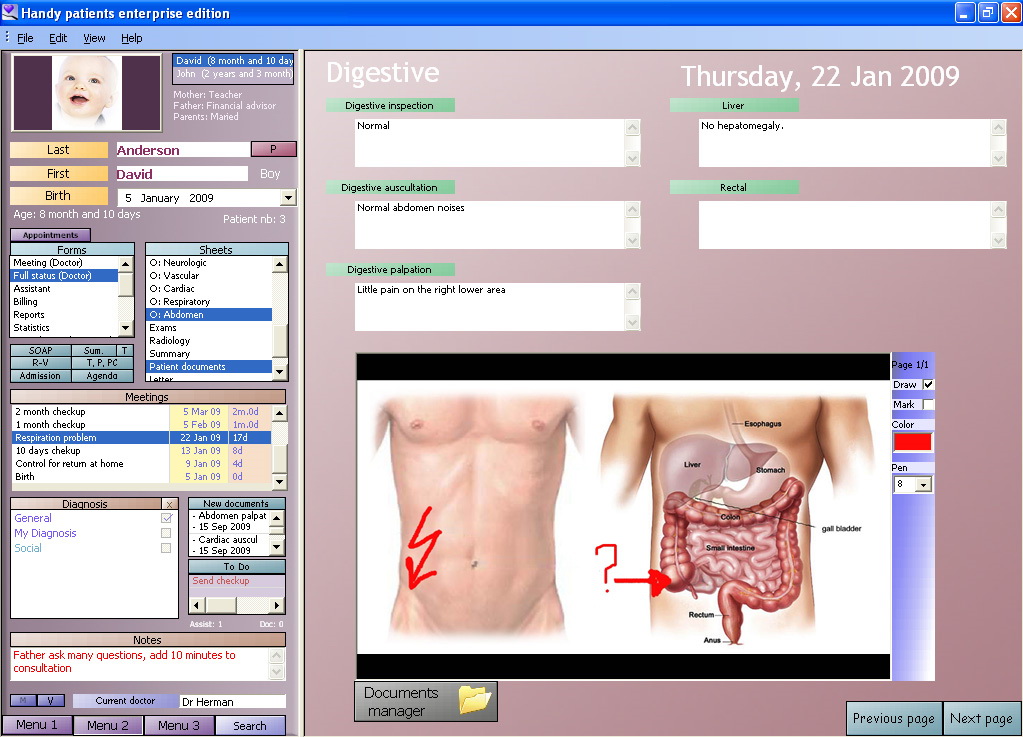
Medical Practice Management Software
Medical practice management software (PMS) is a category of healthcare software that deals with the day-to-day operations of a medical practice including veterinarians. Such software frequently allows users to capture patient demographics, schedule appointments, maintain lists of insurance payors, perform billing tasks, and generate reports. In the United States, most PMS systems are designed for small to medium-sized medical offices. Some of the software is designed for or used by third-party medical billing companies. PMS is often divided among desktop-only software, client-server software, or Internet-based software. The desktop-only variety is intended to be used only on one computer by one or a handful of users sharing access. Client-server software typically necessitates that the practice acquire or lease server equipment and operate the server software on that hardware, while individual users' workstations contain client software that accesses the server. Client-server ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |