|
List Of Disorders Included In Newborn Screening Programs
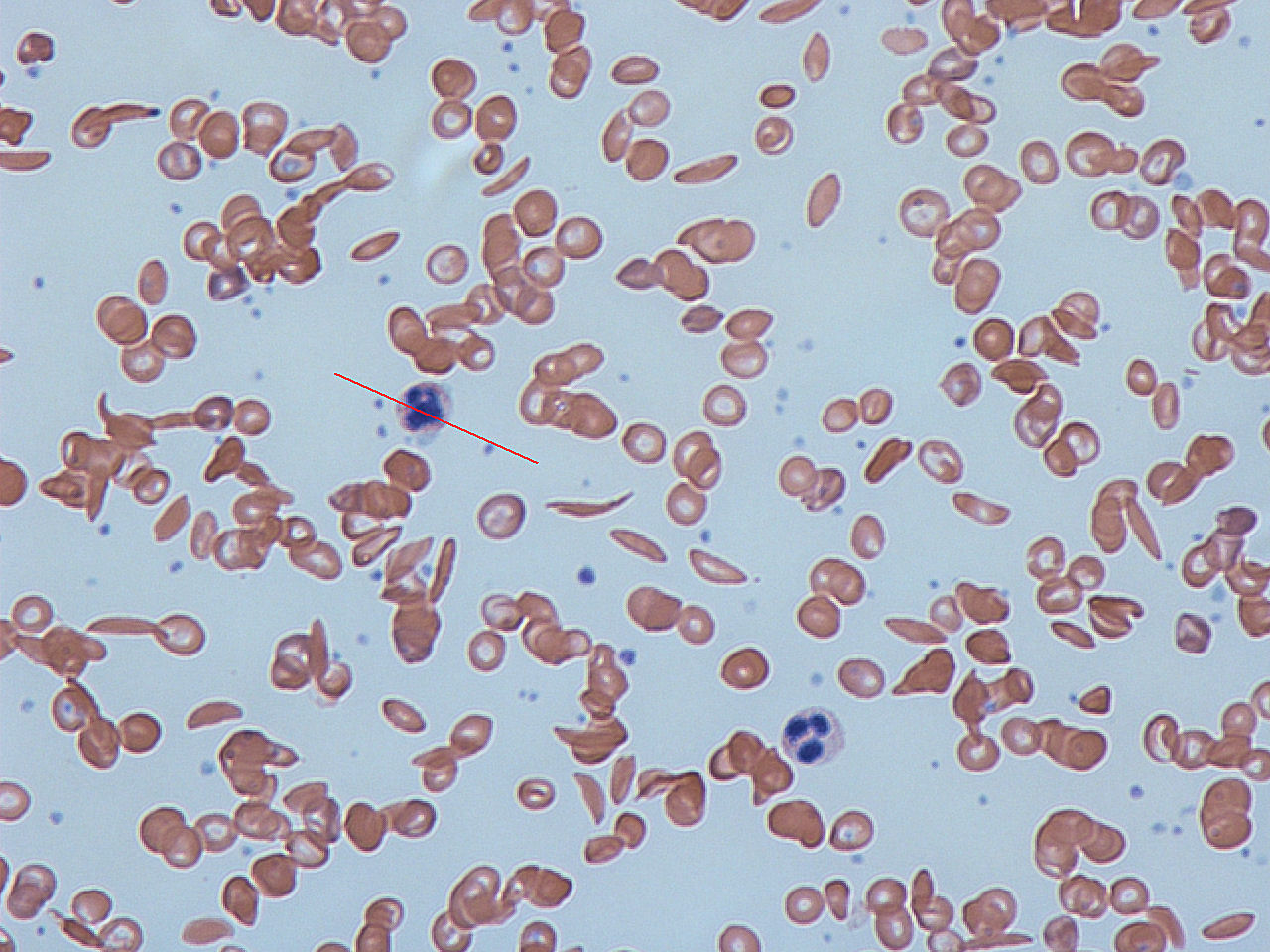
This is a list of disorders included in newborn screening programs around the world, along with information on testing methodologies, disease incidence and rationale for being included in screening programs. American College of Medical Genetics recommendations Core panel The following conditions and disorders were recommended as a "core panel" by the 2005 report of the American College of Medical Genetics (ACMG). The incidences reported below are from the full report, though the rates may vary in different populations. Blood cell disorders * Sickle cell anemia (Hb SS) > 1 in 5,000; among African-Americans 1 in 400 * Sickle-cell disease (Hb S/C) > 1 in 25,000 * Hb S/Beta-Thalassemia (Hb S/Th) > 1 in 50,000 Inborn errors of amino acid metabolism * Tyrosinemia I (TYR I) 1 in 25,000 * Classical galactosemia (GALT) > 1 in 50,000 Newborn screening by other methods than blood testing * Congenital deafness (HEAR) > 1 in 5,000 Secondary targets The following disorders ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Newborn Screening
Newborn screening (NBS) is a public health program of screening in infants shortly after birth for conditions that are treatable, but not clinically evident in the newborn period. The goal is to identify infants at risk for these conditions early enough to confirm the diagnosis and provide intervention that will alter the clinical course of the disease and prevent or ameliorate the clinical manifestations. NBS started with the discovery that the amino acid disorder phenylketonuria (PKU) could be treated by dietary adjustment, and that early intervention was required for the best outcome. Infants with PKU appear normal at birth, but are unable to metabolize the essential amino acid phenylalanine, resulting in irreversible intellectual disability. In the 1960s, Robert Guthrie developed a simple method using a bacterial inhibition assay that could detect high levels of phenylalanine in blood shortly after a baby was born. Guthrie also pioneered the collection of blood on filte ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
3-Methylcrotonyl-CoA Carboxylase Deficiency
3-Methylcrotonyl-CoA carboxylase deficiency also known as 3-Methylcrotonylglycinuria or BMCC deficiency is an inherited disorder in which the body is unable to process certain proteins properly. People with this disorder have inadequate levels of an enzyme that helps break down proteins containing the amino acid leucine. This condition affects an estimated 1 in 50,000 individuals worldwide. Presentation Infants with this disorder appear normal at birth but usually develop signs and symptoms during the first year of life or in early childhood. The characteristic features of this condition, which can range from mild to life-threatening, include feeding difficulties, recurrent episodes of vomiting and diarrhea, excessive tiredness (lethargy), and weak muscle tone (hypotonia). If untreated, this disorder can lead to delayed development, seizures, and coma. Early detection and lifelong management (following a low-protein diet and using appropriate supplements) may prevent many of these c ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Congenital Hypothyroidism
Congenital hypothyroidism (CH) is thyroid hormone deficiency present at birth. If untreated for several months after birth, severe congenital hypothyroidism can lead to growth failure and permanent intellectual disability. Infants born with congenital hypothyroidism may show no effects, or may display mild effects that often go unrecognized as a problem. Significant deficiency may cause excessive sleeping, reduced interest in nursing, poor muscle tone, low or hoarse cry, infrequent bowel movements, significant jaundice, and low body temperature. Causes of congenital hypothyroidism include iodine deficiency and a developmental defect in the thyroid gland, either due to a genetic defect or of unknown cause. Treatment consists of a daily dose of thyroid hormone (thyroxine) by mouth. Because the treatment is simple, effective, and inexpensive, most of the developed world utilizes newborn screening with blood thyroid stimulating hormone (TSH) levels to detect congenital hypothyr ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cystic Fibrosis
Cystic fibrosis (CF) is a rare genetic disorder that affects mostly the lungs, but also the pancreas, liver, kidneys, and intestine. Long-term issues include difficulty breathing and coughing up mucus as a result of frequent lung infections. Other signs and symptoms may include sinus infections, poor growth, fatty stool, clubbing of the fingers and toes, and infertility in most males. Different people may have different degrees of symptoms. Cystic fibrosis is inherited in an autosomal recessive manner. It is caused by the presence of mutations in both copies of the gene for the cystic fibrosis transmembrane conductance regulator (CFTR) protein. Those with a single working copy are carriers and otherwise mostly healthy. CFTR is involved in the production of sweat, digestive fluids, and mucus. When the CFTR is not functional, secretions which are usually thin instead become thick. The condition is diagnosed by a sweat test and genetic testing. Screening of infants at bi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Carnitine Uptake Defect
Systemic primary carnitine deficiency (SPCD)Systemic primary carnitine deficiency is an inborn error of fatty acid transport caused by a defect in the transporter responsible for moving across the . Carnitine is an important amino acid for fatty acid metabolism. When carnitine cann ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Trifunctional Protein Deficiency
Mitochondrial trifunctional protein deficiency (MTP deficiency or MTPD) is an autosomal recessive fatty acid oxidation disordersubscription needed that prevents the body from converting certain fats to energy, particularly during periods without food. People with this disorder have inadequate levels of an enzyme that breaks down a certain group of fats called long-chain fatty acids. Signs and symptoms The presentation of mitochondrial trifunctional protein deficiency may begin during infancy, features that occur are: low blood sugar, weak muscle tone, and liver problems. Infants with this disorder are at risk for heart problems, breathing difficulties, and pigmentary retinopathy. Signs and symptoms of mitochondrial trifunctional protein deficiency that may begin ''after'' infancy include hypotonia, muscle pain, a breakdown of muscle tissue, and a loss of sensation in the extremities called peripheral neuropathy. Some who have MTP deficiency show a progressive course associated wit ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Very-long-chain Acyl-CoA Dehydrogenase Deficiency
Very long-chain acyl-coenzyme A dehydrogenase deficiency is a fatty-acid metabolism disorder which prevents the body from converting certain fats to energy, particularly during periods without food. Those affected by this disorder have inadequate levels of an enzyme that breaks down a group of fats called very long-chain fatty acids. Signs and symptoms Signs and symptoms can include: * hypoglycemia * lethargy * hepatomegaly * muscle pain * cardiomyopathy *Early onset-pericardial effusion *heart arrhythmias *vomiting *Coma *Death *Rhabdomyolysis *Hypoketotic Hypoglycemia Causes VLCAD (very long-chain-acyl-dehydrogenase) deficiency is exclusively linked to genetic mutations in DNA. A change of the gene that codes for very long-chain-acyl-CoA-dehydrogenase (VLCAD) results in a deficiency or malfunction of the produced VLCAD enzyme. This mutation occurs on chromosome 17 and can be altered via a variety of pathways. These can range from frameshift mutations, deletion mutations, i ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medium-chain Acyl-CoA Dehydrogenase Deficiency
Medium-chain acyl-CoA dehydrogenase deficiency (MCAD deficiency or MCADD) is a disorder of fatty acid oxidation that impairs the body's ability to break down medium-chain fatty acids into acetyl-CoA. The disorder is characterized by hypoglycemia and sudden death without timely intervention, most often brought on by periods of fasting or vomiting. Prior to expanded newborn screening, MCADD was an underdiagnosed cause of sudden death in infants. Individuals who have been identified prior to the onset of symptoms have an excellent prognosis. MCADD is most prevalent in individuals of Northern European Caucasian descent, with an incidence of 1:4000 to 1:17,000 depending on the population. Treatment of MCADD is mainly preventive, by avoiding fasting and other situations where the body relies on fatty acid oxidation to supply energy. Signs and symptoms MCADD presents in early childhood with hypoketotic hypoglycemia and liver dysfunction, often preceded by extended periods of fas ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Long-chain Hydroxyacyl-CoA Dehydrogenase Deficiency
Long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency is a rare autosomal recessive fatty acid oxidation disorder that prevents the body from converting certain fats into energy. This can become life-threatening, particularly during periods of fasting. Symptoms and signs Typically, initial signs and symptoms of this disorder occur during infancy or early childhood and can include feeding difficulties, lethargy, hypoglycemia, hypotonia, liver problems, and abnormalities in the retina. Muscle pain, a breakdown of muscle tissue, and abnormalities in the nervous system that affect arms and legs (peripheral neuropathy) may occur later in childhood. There is also a risk for complications such as life-threatening heart and breathing problems, coma, and sudden unexpected death. Episodes of LCHAD deficiency can be triggered by periods of fasting or by illnesses such as viral infections. Genetics Mutations in the ''HADHA'' gene lead to inadequate levels of an enzyme called lon ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Inborn Errors Of Fatty Acid Metabolism
Numerous genetic disorders are caused by errors in fatty acid metabolism. These disorders may be described as fatty oxidation disorders or as a ''lipid storage disorders'', and are any one of several inborn errors of metabolism that result from enzyme defects affecting the ability of the body to oxidize fatty acids in order to produce energy within muscles, liver, and other cell types. Some of the more common fatty acid metabolism disorders are: Coenzyme A dehydrogenase deficiencies * Very long-chain acyl-coenzyme A dehydrogenase deficiency (VLCAD) - Very long-chain acyl-coenzyme A dehydrogenase * Long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency (LCHAD) - Long-chain 3-hydroxyacyl-coenzyme A * Medium-chain acyl-coenzyme A dehydrogenase deficiency (MCAD) - Medium-chain acyl-coenzyme A dehydrogenase * Short-chain acyl-coenzyme A dehydrogenase deficiency (SCAD) - Short-chain acyl-coenzyme A dehydrogenase * 3-hydroxyacyl-coenzyme A dehydrogenase deficiency (HADH) - 3 ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Multiple Carboxylase Deficiency
Multiple carboxylase deficiency is a form of metabolic disorder involving failures of carboxylation enzymes. The deficiency can be in biotinidase or holocarboxylase synthetase. These conditions respond to biotin. Forms include: * Holocarboxylase synthetase deficiency - neonatal; * Biotinidase deficiency - late onset; If left untreated, the symptoms can include feeding problems, decreased body tone, generalized red rash with skin exfoliation and baldness, failure to thrive, seizure, coma, developmental delay, foul smelling urine, lactic acidosis, and high levels of ketones and ammonia Ammonia is an inorganic compound of nitrogen and hydrogen with the formula . A stable binary hydride, and the simplest pnictogen hydride, ammonia is a colourless gas with a distinct pungent smell. Biologically, it is a common nitrogeno ... in the blood. References External links * http://www.pmh.health.wa.gov.au/services/newborn/health_professionals/disorders/mcd_prof.htm V ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Propionic Acidemia
Propionic acidemia, also known as propionic aciduria or propionyl-CoA carboxylase deficiency (PCC deficiency), is a rare autosomal recessive metabolic disorder, classified as a branched-chain organic acidemia. The disorder presents in the early neonatal period with poor feeding, vomiting, lethargy, and lack of muscle tone. Without treatment, death can occur quickly, due to secondary hyperammonemia, infection, cardiomyopathy, or brain damage. Symptoms and signs Propionic acidemia can vary in severity. Severe propionic acidemia lead to symptoms already seen in newborns. Symptoms include poor feeding, vomiting, dehydration, acidosis, low muscle tone (hypotonia), seizures, and lethargy. The effects of propionic acidemia quickly become life-threatening. Long-term complications can include chronic kidney disease, cardiomyopathy, and prolonged QTc interval. Pathophysiology In healthy individuals, enzyme propionyl-CoA carboxylase converts propionyl-CoA to methylmalonyl-CoA. This ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |