Infective endocarditis on:
[Wikipedia]
[Google]
[Amazon]
Infective endocarditis is an
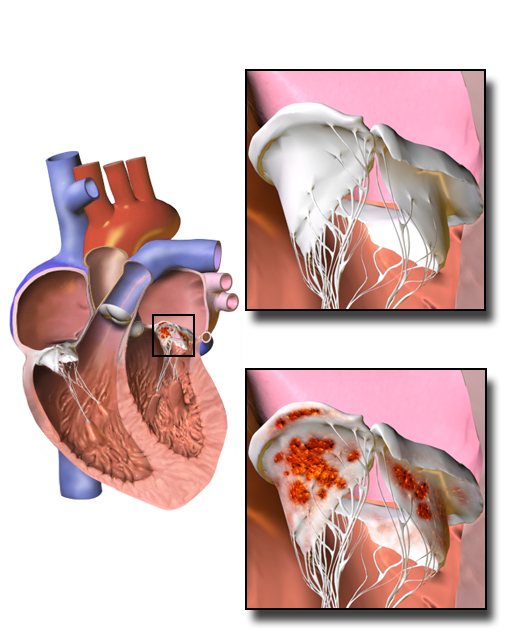 Damaged valves and
Damaged valves and
File:UOTW 27 - Ultrasound of the Week 1.webm, Ultrasound showing infectious endocarditis
File:UOTW 27 - Ultrasound of the Week 2.webm, Ultrasound showing infectious endocarditis
File:UOTW 27 - Ultrasound of the Week 3.webm, Ultrasound showing infectious endocarditis
File:UOTW 60 - Ultrasound of the Week 1.webm, Ultrasound showing another case of infectious endocarditis
 The main indication for surgical treatment is Regurgitation (circulation), regurgitation or stenosis. In active infective endocarditis, the surgery should remove enough leaflet tissue to ensure eradication of the infectious process. Subsequent valve repair can be performed in limited disease. Replacement of the valve with a mechanical or bioprosthetic artificial heart valve is necessary in certain situations:
* Patients with significant valve stenosis or regurgitation causing heart failure
* Evidence of hemodynamic compromise in the form of elevated end-diastolic left ventricular or left atrial pressure or moderate to severe pulmonary hypertension
* Presence of intracardiac complications like paravalvular abscess, conduction defects or destructive penetrating lesions
* Recurrent septic emboli despite appropriate antibiotic treatment
* Large vegetations (> 10 mm)
* Persistently positive blood cultures despite appropriate antibiotic treatment
* Prosthetic valve dehiscence
* Relapsing infection in the presence of a prosthetic valve
* Abscess formation
* Early closure of mitral valve
* Infection caused by fungi or resistant Gram-negative bacteria.
The guidelines were recently updated by both the American College of Cardiology and the European Society of Cardiology. There was a recent meta-analysis published that showed surgical intervention at seven days or less is associated with lower mortality.
The main indication for surgical treatment is Regurgitation (circulation), regurgitation or stenosis. In active infective endocarditis, the surgery should remove enough leaflet tissue to ensure eradication of the infectious process. Subsequent valve repair can be performed in limited disease. Replacement of the valve with a mechanical or bioprosthetic artificial heart valve is necessary in certain situations:
* Patients with significant valve stenosis or regurgitation causing heart failure
* Evidence of hemodynamic compromise in the form of elevated end-diastolic left ventricular or left atrial pressure or moderate to severe pulmonary hypertension
* Presence of intracardiac complications like paravalvular abscess, conduction defects or destructive penetrating lesions
* Recurrent septic emboli despite appropriate antibiotic treatment
* Large vegetations (> 10 mm)
* Persistently positive blood cultures despite appropriate antibiotic treatment
* Prosthetic valve dehiscence
* Relapsing infection in the presence of a prosthetic valve
* Abscess formation
* Early closure of mitral valve
* Infection caused by fungi or resistant Gram-negative bacteria.
The guidelines were recently updated by both the American College of Cardiology and the European Society of Cardiology. There was a recent meta-analysis published that showed surgical intervention at seven days or less is associated with lower mortality.
infection
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable dis ...
of the inner surface of the heart, usually the valves
A valve is a device or natural object that regulates, directs or controls the flow of a fluid (gases, liquids, fluidized solids, or slurries) by opening, closing, or partially obstructing various passageways. Valves are technically fitting ...
. Signs and symptoms may include fever
Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point. There is not a single agreed-upon upper limit for normal temperature with sources using val ...
, small areas of bleeding into the skin, heart murmur
Heart murmurs are unique heart sounds produced when blood flows across a heart valve or blood vessel. This occurs when turbulent blood flow creates a sound loud enough to hear with a stethoscope. Turbulent blood flow is not smooth. The sound di ...
, feeling tired, and low red blood cell count. Complications may include backward blood flow in the heart, heart failure – the heart struggling to pump a sufficient amount of blood to meet the body's needs, abnormal electrical conduction in the heart, stroke, and kidney failure
Kidney failure, also known as end-stage kidney disease, is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as eit ...
.
The cause is typically a bacterial infection
Pathogenic bacteria are bacteria that can cause disease. This article focuses on the bacteria that are pathogenic to humans. Most species of bacteria are harmless and are often beneficial but others can cause infectious diseases. The number ...
and less commonly a fungal infection. Risk factors include valvular heart disease
Valvular heart disease is any cardiovascular disease process involving one or more of the four valves of the heart (the aortic and mitral valves on the left side of heart and the pulmonic and tricuspid valves on the right side of heart). These ...
, including rheumatic disease
Rheumatism or rheumatic disorders are conditions causing chronic, often intermittent pain affecting the joints or connective tissue. Rheumatism does not designate any specific disorder, but covers at least 200 different conditions, including art ...
, congenital heart disease
A congenital heart defect (CHD), also known as a congenital heart anomaly and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital heart defect is classed as a cardiovascular ...
, artificial valves
An artificial heart valve is a one-way valve implanted into a person's heart to replace a heart valve that is not functioning properly (valvular heart disease). Artificial heart valves can be separated into three broad classes: mechanical hear ...
, hemodialysis
Hemodialysis, also spelled haemodialysis, or simply dialysis, is a process of purifying the blood of a person whose kidneys are not working normally. This type of dialysis achieves the extracorporeal removal of waste products such as creatinin ...
, intravenous drug use
Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body (usually intravenously, but also at an intramuscular or subcutaneous location). Intravenous t ...
, and electronic pacemakers. The bacteria most commonly involved are streptococci or staphylococci
''Staphylococcus'' is a genus of Gram-positive bacteria in the family Staphylococcaceae from the order Bacillales. Under the microscope, they appear spherical ( cocci), and form in grape-like clusters. ''Staphylococcus'' species are facultati ...
. Diagnosis is suspected based on symptoms and supported by blood cultures
A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia ...
or ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies ...
of the heart. There is also a noninfective form of endocarditis
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves. Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or the ...
.
The usefulness of antibiotics
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention o ...
following dental procedure
Dentistry, also known as dental medicine and oral medicine, is the branch of medicine focused on the teeth, gums, and mouth. It consists of the study, diagnosis, prevention, management, and treatment of diseases, disorders, and conditions of ...
s for prevention is unclear. Some recommend them for people at high risk. Treatment is generally with intravenous antibiotics. The choice of antibiotics is based on the results of blood cultures. Occasionally heart surgery is required.
The number of people affected is about 5 per 100,000 per year. Rates, however, vary between regions of the world. Infective endocarditis occurs in males more often than in females. The risk of death among those infected is about 25%. Without treatment, it is almost universally fatal.
Classification
Infective endocarditis is divided into the three categories of acute, subacute, and chronic based on the duration of symptoms. Acute infective endocarditis refers to the presence of signs and symptoms of infective endocarditis that are present for days up to six weeks. If these signs and symptoms persist for more than six weeks but less than three months, this is subacute infective endocarditis. Chronic infective endocarditis refers to the presence of such signs and symptoms when they persist for more than three months. * '' Subacute bacterial endocarditis'' (SBE) is often due to streptococci of low virulence (mainlyviridans streptococci
The viridans streptococci are a large group of commensal streptococcal Gram-positive bacteria species that are α-hemolytic, producing a green coloration on blood agar plates (hence the name "viridans", from Latin "vĭrĭdis", green), although ...
) and mild to moderate illness which progresses slowly over weeks and months (>2 weeks) and has low propensity to hematogenously seed extracardiac sites.
* ''Acute bacterial endocarditis'' (ABE) is a fulminant illness over days to weeks (<2 weeks), and is more likely due to '' Staphylococcus aureus'', which has much greater virulence or disease-producing capacity and frequently causes metastatic infection.
This classification is now discouraged, because the ascribed associations (in terms of organism and prognosis) were not strong enough to be relied upon clinically. The terms ''short incubation'' (meaning less than about six weeks) and ''long incubation'' (greater than about six weeks) are preferred.
Culture results
Infective endocarditis may also be classified as ''culture-positive'' or ''culture-negative''. By far the most common cause of "culture-negative" endocarditis is prior administration of antibiotics. Sometimesmicroorganism
A microorganism, or microbe,, ''mikros'', "small") and ''organism'' from the el, ὀργανισμός, ''organismós'', "organism"). It is usually written as a single word but is sometimes hyphenated (''micro-organism''), especially in olde ...
s can take a longer period of time to grow in the culture media, for example Cutibacterium spp. and the HACEK bacteria group. Some organisms are said to be ''fastidious
A fastidious organism is any organism that has complex or particular nutritional requirements. In other words, a fastidious organism will only grow when specific nutrients are included in its medium. The more restrictive term fastidious microorga ...
'' because they have demanding growth requirements. Some examples include pathogens like ''Aspergillus
' () is a genus consisting of several hundred mold species found in various climates worldwide.
''Aspergillus'' was first catalogued in 1729 by the Italian priest and biologist Pier Antonio Micheli. Viewing the fungi under a microscope, Mic ...
'' species, ''Brucella
''Brucella'' is a genus of Gram-negative bacteria, named after David Bruce (1855–1931). They are small (0.5 to 0.7 by 0.6 to 1.5 µm), non encapsulated, non motile, facultatively intracellular coccobacilli.
''Brucella'' spp. are the caus ...
'' species, ''Coxiella burnetii
''Coxiella burnetii'' is an obligate intracellular bacterial pathogen, and is the causative agent of Q fever. The genus ''Coxiella'' is morphologically similar to ''Rickettsia'', but with a variety of genetic and physiological differences. ''C. ...
'', ''Chlamydia
Chlamydia, or more specifically a chlamydia infection, is a sexually transmitted infection caused by the bacterium '' Chlamydia trachomatis''. Most people who are infected have no symptoms. When symptoms do appear they may occur only several we ...
'' species. Due to delay in growth and identification in these cases, patients may be erroneously classified as "culture-negative" endocarditis.
Heart side
Endocarditis can also be classified by the side of the heart affected: * People who intravenously injectopioid
Opioids are substances that act on opioid receptors to produce morphine-like effects. Medically they are primarily used for pain relief, including anesthesia. Other medical uses include suppression of diarrhea, replacement therapy for opioid use ...
s such as heroin or methamphetamine may introduce infection which can travel to the right side of the heart, classically affecting the tricuspid valve
The tricuspid valve, or right atrioventricular valve, is on the right dorsal side of the mammalian heart, at the superior portion of the right ventricle. The function of the valve is to allow blood to flow from the right atrium to the right ven ...
, and most often caused by ''S. aureus''.
* Regardless of cause, left-sided endocarditis is more common in people who inject IV drugs and people who do not use substances than right-sided endocarditis.
Infection setting
Another form of endocarditis is healthcare-associated endocarditis when the infecting organism is believed to be transmitted in a health care setting like hospital, dialysis unit or a residential nursing home. Nosocomial endocarditis is a form of healthcare associated endocarditis in which the infective organism is acquired during a stay in a hospital and it is usually secondary to presence of intravenous catheters,total parenteral nutrition
Parenteral nutrition (PN) is the feeding of nutritional products to a person intravenously, bypassing the usual process of eating and digestion. The products are made by pharmaceutical compounding companies. The person receives a nutritional mix ...
lines, pacemakers
An artificial cardiac pacemaker (or artificial pacemaker, so as not to be confused with the natural cardiac pacemaker) or pacemaker is a medical device that generates electrical impulses delivered by electrodes to the chambers of the heart eit ...
, etc.
Valve type
Finally, the distinction between ''native-valve endocarditis'' and ''prosthetic-valve endocarditis'' is clinically important. Prosthetic valve endocarditis can be early (< 60 days of valvular surgery), intermediate (60 days to 1 year) or late (> 1 year following valvular surgery). * Early prosthetic valve endocarditis is usually due to intraoperative contamination or postoperative bacterial contamination which is usually nosocomial in nature. * Late prosthetic valve endocarditis is usually due to community-acquired microorganisms. Prosthetic valve endocarditis is commonly caused by '' Staphylococcus epidermidis'' as it is capable of growing as abiofilm
A biofilm comprises any syntrophic consortium of microorganisms in which cells stick to each other and often also to a surface. These adherent cells become embedded within a slimy extracellular matrix that is composed of extracellular ...
on plastic surfaces. ''Cutibacterium acnes'' almost exclusively causes endocarditis on prosthetic heart valves.
Signs and symptoms
*Fever
Fever, also referred to as pyrexia, is defined as having a temperature above the normal range due to an increase in the body's temperature set point. There is not a single agreed-upon upper limit for normal temperature with sources using val ...
occurs in 97% of people; malaise and endurance fatigue in 90% of people.
* A new or changing heart murmur
Heart murmurs are unique heart sounds produced when blood flows across a heart valve or blood vessel. This occurs when turbulent blood flow creates a sound loud enough to hear with a stethoscope. Turbulent blood flow is not smooth. The sound di ...
, weight loss
Weight loss, in the context of medicine, health, or physical fitness, refers to a reduction of the total body mass, by a mean loss of fluid, body fat ( adipose tissue), or lean mass (namely bone mineral deposits, muscle, tendon, and other co ...
, and coughing occurs in 35% of people.
* Vascular phenomena: septic embolism (a piece of infected debris or tissue breaking off and traveling through the bloodstream to a distant site) (causing thromboembolic problems such as a stroke or gangrene of the fingers), Janeway lesions (painless hemorrhagic cutaneous lesions on the palms and soles), bleeding in the brain, conjunctiva
The conjunctiva is a thin mucous membrane that lines the inside of the eyelids and covers the sclera (the white of the eye). It is composed of non-keratinized, stratified squamous epithelium with goblet cells, stratified columnar epithelium ...
l hemorrhage, splinter hemorrhages, kidney infarcts, and splenic infarcts. Infective endocarditis can also lead to the formation of mycotic aneurysm
An infected aneurysm is an aneurysm arising from bacterial infection of the arterial wall. It can be a common complication of the hematogenous spread of bacterial infection.
William Osler first used the term "mycotic aneurysm" in 1885 to describe ...
s.
* Immunologic phenomena: glomerulonephritis
Glomerulonephritis (GN) is a term used to refer to several kidney diseases (usually affecting both kidneys). Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the ...
which allows for blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells. Blood in the cir ...
and albumin to enter the urine, Osler's nodes ("ephemeral spots of a painful nodular erythema, chiefly in the skin of the hands and feet"), Roth's spot
Roth's spots, also known as Litten spots or the Litten sign, are non-specific red spots with white or pale centres, seen on the retina and although traditionally associated with infective endocarditis, can occur in a number of other conditions inc ...
s on the retina
The retina (from la, rete "net") is the innermost, light-sensitive layer of tissue of the eye of most vertebrates and some molluscs. The optics of the eye create a focused two-dimensional image of the visual world on the retina, which then ...
, positive serum rheumatoid factor
* Other signs may include night sweats, rigors, anemia, spleen enlargement
Cause
Many microorganisms can cause infective endocarditis. These are generally isolated byblood culture
A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia or ...
, where the patient's blood is drawn and any growth is noted and identified. The term bacterial endocarditis (BE) commonly is used, reflecting the fact that most cases of IE are due to bacteria; however, infective endocarditis (IE) has become the preferred term.
Bacterial
'' Staphylococcus aureus'' is the leading cause of infective endocarditis in most parts of the world and is responsible for about 31% of cases. Staphylococcus aureus is the most common cause of endocarditis in people who use intravenous drugs.Viridans streptococci
The viridans streptococci are a large group of commensal streptococcal Gram-positive bacteria species that are α-hemolytic, producing a green coloration on blood agar plates (hence the name "viridans", from Latin "vĭrĭdis", green), although ...
and Enterococci are the second and third most common organisms responsible for infective endocarditis. Viridans streptococci are a common cause of infective endocarditis in South America. Other ''Streptococci'' are also a frequent cause. Infective endocarditis due to '' Streptococcus bovis'' occurs more commonly in Europe than in North America. HACEK group of bacteria are also rare causes of infective endocarditis in North America.
The viridans group includes ''S. oralis'', ''S. mitis'', ''S. sanguis'', ''S. gordonii'' and ''S. parasanguis''. The primary habitats for these organisms are the oral cavity and upper respiratory tract. These bacteria are present in the normal oral flora and enter the bloodstream due to disruption of tissues in the mouth when dental surgical procedures are performed (tooth extractions) or genitourinary manipulation. Similarly, HACEK organisms are a group of bacteria that live on the dental gums and can be seen with people who inject drugs who contaminate their needles with saliva. Patients may also have a history of poor dental hygiene or pre-existing valvular disease.
Viridans alpha-hemolytic '' streptococci'', that are present in the mouth, are the most frequently isolated microorganisms when the infection is acquired in a community setting. In contrast, '' Staphylococcus'' bloodstream infections are frequently acquired in a health care setting where they can enter the bloodstream through procedures that cause breaks in the integrity of skin, such as surgery, catheterization, or during access of long term indwelling catheters or secondary to intravenous injection of recreational drugs.
''Enterococcus'' can enter the bloodstream as a consequence of abnormalities in the gastrointestinal or genitourinary tracts.
Some organisms, when isolated, give valuable clues to the cause, as they tend to be specific.
* ''Pseudomonas
''Pseudomonas'' is a genus of Gram-negative, Gammaproteobacteria, belonging to the family Pseudomonadaceae and containing 191 described species. The members of the genus demonstrate a great deal of metabolic diversity and consequently are able t ...
'' species, which are very resilient organisms that thrive in water, may contaminate street drugs that have been contaminated with drinking water. '' P. aeruginosa'' can infect a child through foot punctures, and can cause both endocarditis and septic arthritis
Acute septic arthritis, infectious arthritis, suppurative arthritis, osteomyelitis, or joint infection is the invasion of a joint by an infectious agent resulting in joint inflammation. Generally speaking, symptoms typically include redness, h ...
.
* '' S. bovis'' and ''Clostridium septicum
''Clostridium septicum'' is a gram positive, spore forming, obligate anaerobic bacterium.
''Clostridium septicum'' can cause gas gangrene, but unlike other Clostridium species like ''Clostridium perfringens'', no trauma is necessary at the sit ...
'', which are part of the natural flora of the bowel, are associated with colon cancers. When they present as the causative agent in endocarditis, it usually prompts a colonoscopy to be done immediately due to concerns regarding spread of bacteria from the colon through the bloodstream due to the cancer breaking down the barrier between the inside of the colon (lumen) and the blood vessels which drain the bowel.
* Less commonly reported bacteria responsible for so called "culture negative endocarditis" include ''Bartonella
''Bartonella'' is a genus of Gram-negative bacteria. It is the only genus in the family Bartonellaceae. Facultative intracellular parasites, ''Bartonella'' species can infect healthy people, but are considered especially important as opportunis ...
'', ''Chlamydia psittaci
''Chlamydia psittaci'' is a lethal intracellular parasite, intracellular bacterial species that may cause Endemism, endemic Bird, avian chlamydiosis, epizootic outbreaks in mammals, and respiratory psittacosis in humans. Potential hosts include ...
'', and '' Coxiella''. Such bacteria can be identified by serology, culture of the excised valve tissue, sputum, pleural fluid, and emboli, and by polymerase chain reaction or sequencing of bacterial 16S ribosomal RNA.
Multiple case reports of infective endocarditis caused by unusual organisms have been published. '' Cutibacterium'' spp., which are normal skin flora, have been responsible for infective endocarditis, preferably in patients with prosthetic heart valves, in rare cases leading to death.'' Tropheryma whipplei'' has caused endocarditis without gastrointestinal involvement. ''Citrobacter koseri
''Citrobacter koseri'' is a Gram-negative, non-spore-forming bacillus. It is a facultative anaerobe capable of aerobic respiration. It is motile via peritrichous flagella. It is a member of the family of Enterobacteriaceae. The members of t ...
'' was found in an immunocompetent adult. ''Neisseria bacilliformis'' was found in a person with a bicuspid aortic valve
Bicuspid aortic valve (aka BAV) is a form of heart disease in which two of the leaflets of the aortic valve fuse during development in the womb resulting in a two-leaflet (bicuspid) valve instead of the normal three-leaflet (tricuspid) valve. BA ...
.
Fungal
Fungal endocarditis (FE) is often fatal and one of the most serious forms of infective endocarditis. The types of fungi most seen associated with this disease are: ''Candida albicans
''Candida albicans'' is an opportunistic pathogenic yeast that is a common member of the human gut flora. It can also survive outside the human body. It is detected in the gastrointestinal tract and mouth in 40–60% of healthy adults. It is usu ...
'' is found as a spherical or oval budding yeast
Yeasts are eukaryotic, single-celled microorganisms classified as members of the fungus kingdom. The first yeast originated hundreds of millions of years ago, and at least 1,500 species are currently recognized. They are estimated to constit ...
. It is associated with endocarditis in people who inject drugs, patients with prosthetic valves, and immunocompromised
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that a ...
patients. It forms biofilms around thick-walled resting structures like prosthetic heart valves and additionally colonizes and penetrates endothelial
The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel ...
walls. C. albicans is responsible for 24-46% of all the cases of FE, and its mortality rate
Mortality rate, or death rate, is a measure of the number of deaths (in general, or due to a specific cause) in a particular population, scaled to the size of that population, per unit of time. Mortality rate is typically expressed in units of d ...
is 46.6–50%.
Other fungi demonstrated to cause endocarditis are ''Histoplasma capsulatum
''Histoplasma capsulatum'' is a species of dimorphic fungus. Its sexual form is called ''Ajellomyces capsulatus''. It can cause pulmonary and disseminated histoplasmosis.
''H. capsulatum'' is "distributed worldwide, except in Antarctica, but m ...
'' and Aspergillus
' () is a genus consisting of several hundred mold species found in various climates worldwide.
''Aspergillus'' was first catalogued in 1729 by the Italian priest and biologist Pier Antonio Micheli. Viewing the fungi under a microscope, Mic ...
. Aspergillus contributes to roughly 25% of FE cases. Endocarditis with ''Tricosporon asahii'' has also been reported in a case report.
Risk factors
Risk factors for infective endocarditis are based on the premise that in a healthy individual, bacteremia (bacteria entering the bloodstream) is cleared quickly with no adverse consequences. However, if a heart valve is damaged, the bacteria can attach themselves to the valve, resulting in infective endocarditis. Additionally, in individuals with weakened immune systems, the concentration of bacteria in the blood can reach levels high enough to increase the probability that some will attach to the valve. Some significant risk factors are listed here: *Artificial heart valve
An artificial heart valve is a one-way valve implanted into a person's heart to replace a heart valve that is not functioning properly ( valvular heart disease). Artificial heart valves can be separated into three broad classes: mechanical he ...
s
* Intracardiac devices, such as implantable cardioverter-defibrillators
* Unrepaired cyanotic congenital heart defects
A congenital heart defect (CHD), also known as a congenital heart anomaly and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital heart defect is classed as a cardiovascular ...
* History of infective endocarditis
* Neoplastic disease
* Chronic rheumatic heart disease, which is an autoimmune response to repeated ''Streptococcus pyogenes
''Streptococcus pyogenes'' is a species of Gram-positive, aerotolerant bacteria in the genus '' Streptococcus''. These bacteria are extracellular, and made up of non-motile and non-sporing cocci (round cells) that tend to link in chains. They ...
'' infection (mostly in the developing world)
* Age-related degenerative valvular lesions
* Congenital heart valve abnormalities
* Hemodialysis
Hemodialysis, also spelled haemodialysis, or simply dialysis, is a process of purifying the blood of a person whose kidneys are not working normally. This type of dialysis achieves the extracorporeal removal of waste products such as creatinin ...
, a medical procedure that filters the blood of individuals with kidney failure
* Poor oral hygiene
* Coexisting conditions, especially ones that suppress immunity. Diabetes mellitus
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level ( hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
, alcohol use disorder, chronic liver disease, HIV/AIDS
Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual ...
, and intravenous drug use all fall in this category
More detailed descriptions of these and other risk factors are provided below.
Other conditions that result in large numbers of bacteria entering into the bloodstream include colorectal cancer (mostly '' Streptococcus bovis''), serious urinary tract infection
A urinary tract infection (UTI) is an infection that affects part of the urinary tract. When it affects the lower urinary tract it is known as a bladder infection (cystitis) and when it affects the upper urinary tract it is known as a kidne ...
s (mostly enterococci), and drug injection
Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body (usually intravenously, but also at an intramuscular or subcutaneous location). Intravenous t ...
('' Staphylococcus aureus''). With a large number of bacteria, even a normal heart valve may become infected.
A more virulent organism (such as ''Staphylococcus aureus'') can cause infective endocarditis by infecting even a normal heart valve.
People who inject drugs tend to get their right-sided heart valves infected because the vein
Veins are blood vessels in humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenat ...
s that are injected drain into the right side of the heart. In rheumatic heart disease, infection occurs on the aortic and the mitral valves on the left side of the heart.
Other factors that increase the risk of developing infective endocarditis are low levels of white blood cells, immunodeficiency or immunosuppression, malignancy, diabetes mellitus, and excessive alcohol use.
Dental operations
In the past, one in eight cases of infective endocarditis was because of bacteremia caused by dental procedures (in most cases due to '' Streptococcus viridans'', which reside in the oral cavity), such as cleaning or extraction of a tooth. This was thought to be more clinically significant than it actually was. However, it is important that a dentist or a dental hygienist be told of any heart problems before commencing treatment.Antibiotics
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention o ...
are administered to patients with certain heart conditions as a precaution, although this practice has changed in the US, with new American Heart Association guidelines released in 2007, and in the UK as of March 2008 due to new NICE guidelines. Everyday tooth brushing and flossing will similarly cause bacteremia, so a high standard of oral health should be adhered to at all times.
Although there is little evidence to support antibiotic prophylaxis for dental treatment, the current American Heart Association guidelines are highly accepted by clinicians and patients.
Pathogenesis
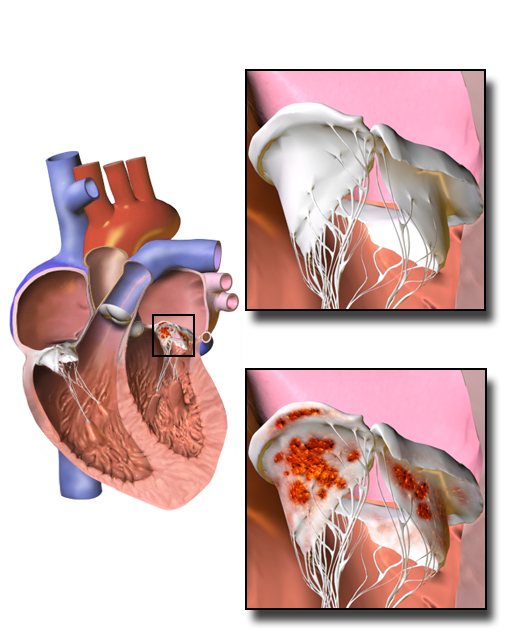 Damaged valves and
Damaged valves and endocardium
The endocardium is the innermost layer of tissue that lines the chambers of the heart. Its cells are embryologically and biologically similar to the endothelial cells that line blood vessels. The endocardium also provides protection to the v ...
contribute to the development of infective endocarditis. Specifically, the damaged part of a heart valve
A heart valve is a one-way valve that allows blood to flow in one direction through the chambers of the heart. Four valves are usually present in a mammalian heart and together they determine the pathway of blood flow through the heart. A heart ...
forms a local blood clot, a condition known as non-bacterial thrombotic endocarditis (NBTE). The platelet and fibrin deposits that form as part of the blood clotting process allow bacteria to take hold and form vegetations. As previously mentioned, the body has no direct methods of combating valvular vegetations because the valves do not have a dedicated blood supply. This combination of damaged valves, bacterial growth, and lack of a strong immune response results in infective endocarditis.
Damage to the valves and endocardium can be caused by:
* Altered, turbulent blood flow. The areas that fibrose, clot, or roughen as a result of this altered flow are known as jet lesions. Altered blood flow is more likely in high pressure areas, so ventricular septal defect
A ventricular septal defect (VSD) is a defect in the ventricular septum, the wall dividing the left and right ventricles of the heart. The extent of the opening may vary from pin size to complete absence of the ventricular septum, creating one ...
s or patent ductus arteriosus
''Patent ductus arteriosus'' (PDA) is a medical condition in which the ''ductus arteriosus'' fails to close after birth: this allows a portion of oxygenated blood from the left heart to flow back to the lungs by flowing from the aorta, which has ...
can create more susceptibility than atrial septal defect
Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria (upper chambers) of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this d ...
s.
* Catheters, electrodes, and other intracardiac prosthetic devices.
* Solid particles from repeated intravenous injections.
* Chronic inflammation. Examples include auto-immune mechanisms and degenerative valvular lesions.
The risk factors
In epidemiology, a risk factor or determinant is a variable associated with an increased risk of disease or infection.
Due to a lack of harmonization across disciplines, determinant, in its more widely accepted scientific meaning, is often use ...
for infective endocarditis provide a more extensive list of conditions that can damage the heart.
Diagnosis
In general, the Duke criteria should be fulfilled in order to establish the diagnosis of endocarditis. Although the Duke criteria are widely used, they have significant limitations. For example, the sensitivity of the Duke criteria for detecting infective endocarditis decreases when prosthetic heart valves are present. As the Duke criteria rely heavily on the results of echocardiography, research has addressed when to order anechocardiogram
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart.
It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Echocardiography has become routinely used in th ...
by using signs and symptoms to predict occult endocarditis among people who inject drugs and among non drug-abusing patients. However, this research is over twenty years old and it is possible that changes in the epidemiology of endocarditis and bacteria such as staphylococci
''Staphylococcus'' is a genus of Gram-positive bacteria in the family Staphylococcaceae from the order Bacillales. Under the microscope, they appear spherical ( cocci), and form in grape-like clusters. ''Staphylococcus'' species are facultati ...
make the following estimates incorrect.
The blood tests C reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin ...
(CRP) and procalcitonin have not been found to be particularly useful in helping make or rule out the diagnosis.
Ultrasound
Echocardiography is the main type of diagnostic imaging used to establish the diagnosis of infective endocarditis. There are two main types of echocardiography used to assist with the diagnosis of IE: transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE). The transthoracic echocardiogram has a sensitivity and specificity of approximately 65% and 95% if the echocardiographer believes there is 'probable' or 'almost certain' evidence of endocarditis. However, in endocarditis involving a prosthetic valve, TTE has a sensitivity of approximately 50%, whereas TEE has a sensitivity exceeding 90%. The TEE also has an important diagnostic role when the TTE does not reveal IE but diagnostic suspicion remains high, since TEE is more sensitive for infective endocarditis and is better able to characterize infection-related damage to the heart valves and surrounding tissues. Guidelines support the initial use of TTE over TEE in people with abnormal blood cultures, a new heart murmur, and suspected infective endocarditis. TEE is the preferred initial form of imaging in people with suspected infective endocarditis who have a moderate to high pretest probability of infective endocarditis, including people with prosthetic heart valves, blood cultures growing '' Staphylococcus'', or have an intracardiac device (such as a pacemaker).Modified Duke criteria
Established in 1994 by the Duke Endocarditis Service and revised in 2000, the Duke criteria are a collection of major and minor criteria used to establish a diagnosis of infective endocarditis. According to the Duke criteria, diagnosis of infective endocarditis can be definite, possible, or rejected. A diagnosis of infective endocarditis is definite if either the following pathological ''or'' clinical criteria are met: One of these pathological criteria: * Histology or culture of cardiac vegetation, embolized vegetation, or intracardiac abscess from the heart finds microorganisms * Active endocarditis One of these combinations of clinical criteria * Two major clinical criteria * One major and three minor criteria * Five minor criteria Diagnosis of infective endocarditis is possible if one of the following combinations of clinical criteria is met: * One major and one minor criteria * Three minor criteria are fulfilledMajor criteria
Positive blood culture with typical IE microorganism, defined as one of the following: * Typical microorganism consistent with IE from two separate blood cultures, as noted below: ** Viridans-group streptococci, or ** '' Streptococcus bovis'' including nutritional variant strains, or ** HACEK group, or ** '' Staphylococcus aureus'', or ** Community-acquired '' enterococci'', in the absence of a primary focus * Microorganisms consistent with IE from persistently positive blood cultures defined as: ** Two positive cultures of blood samples drawn >12 hours apart, or ** Three or a majority of ≥four separate blood cultures (with first and last sample drawn at least one hour apart) ** ''Coxiella burnetii
''Coxiella burnetii'' is an obligate intracellular bacterial pathogen, and is the causative agent of Q fever. The genus ''Coxiella'' is morphologically similar to ''Rickettsia'', but with a variety of genetic and physiological differences. ''C. ...
'' detected by at least one positive blood culture or IgG antibody
Immunoglobulin G (Ig G) is a type of antibody. Representing approximately 75% of serum antibodies in humans, IgG is the most common type of antibody found in blood circulation. IgG molecules are created and released by plasma B cells. Each IgG an ...
titer for Q fever
Q fever or query fever is a disease caused by infection with ''Coxiella burnetii'', a bacterium that affects humans and other animals. This organism is uncommon, but may be found in cattle, sheep, goats, and other domestic mammals, including ...
phase 1 antigen >1:800. This was previously a minor criterion
Evidence of endocardial involvement with positive echocardiogram is defined as
* Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation, or
* Abscess, or
* New partial dehiscence of prosthetic valve or new valvular regurgitation (worsening or changing of preexisting murmur not sufficient)
Minor criteria
* Predisposing factor: known cardiac lesion, recreationaldrug injection
Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body (usually intravenously, but also at an intramuscular or subcutaneous location). Intravenous t ...
* Fever >38 °C
* Vascular
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away f ...
phenomena: arterial emboli, pulmonary
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of ...
infarct
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct
(from the ...
s, Janeway lesions, conjunctiva
The conjunctiva is a thin mucous membrane that lines the inside of the eyelids and covers the sclera (the white of the eye). It is composed of non-keratinized, stratified squamous epithelium with goblet cells, stratified columnar epithelium ...
l hemorrhage
* Immunological phenomena: glomerulonephritis
Glomerulonephritis (GN) is a term used to refer to several kidney diseases (usually affecting both kidneys). Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the ...
, Osler's nodes, Roth's spots, Rheumatoid factor
* Microbiologic evidence: Positive blood culture (that doesn't meet a major criterion) or serologic evidence of infection with organism consistent with IE but not satisfying major criterion
Risk
Among people who do not use intravenous drugs and have a fever in the emergency department, there is a less than 5% chance of occult endocarditis. Mellors in 1987 found no cases of endocarditis nor of staphylococcal bacteremia among 135 febrile patients ''in the emergency room''. The upper confidence interval for 0% of 135 is 5%, so for statistical reasons alone, there is up to a 5% chance of endocarditis among these patients. In contrast, Leibovici found that among 113 non-selected adults ''admitted to the hospital'' because of fever there were two cases (1.8% with 95%CI: 0% to 7%) of endocarditis. Among people who do use intravenous drugs and have a fever in the emergency department, there is about a 10% to 15% prevalence of endocarditis. This estimate is not substantially changed by whether the doctor believes the patient has a trivial explanation for their fever. Weisse found that 13% of 121 patients had endocarditis. Marantz also found a prevalence of endocarditis of 13% among such patients in the emergency department with fever. Samet found a 6% incidence among 283 such patients, but after excluding patients with initially apparent major illness to explain the fever (including 11 cases of manifest endocarditis), there was a 7% prevalence of endocarditis. Among people with staphylococcal bacteremia (SAB), one study found a 29% prevalence of endocarditis in community-acquired SAB versus 5% in nosocomial SAB. However, only 2% of strains were resistant to methicillin and so these numbers may be low in areas of higher resistance.Prevention
Not all people with heart disease require antibiotics to prevent infective endocarditis. Heart diseases have been classified into high, medium and low risk of developing IE. Those falling into high risk category require IE prophylaxis before endoscopies and urinary tract procedures. Diseases listed under high risk include: * Prior endocarditis * Unrepaired cyanotic congenital heart diseases * Completely repaired congenital heart disease in their first 6 months * Prosthetic heart valves * Incompletely repaired congenital heart diseases * Cardiac transplant valvulopathy Following are the antibiotic regimens recommended by the American Heart Association for antibiotic prophylaxis: : Oral amoxicillin one hour before the procedure : Intravenous or intramuscular ampicillin one hour before the procedure :In patients allergic to penicillins :: Azithromycin or clarithromycin orally one hour before the procedure :: Cephalexin orally one hour before the procedure :: Clindamycin orally one hour before the procedure In the UK, NICE clinical guidelines no longer advise prophylaxis because there is no clinical evidence that it reduces the incidence of IE and there are negative effects (e.g. allergy and increased bacterial resistance) of taking antibiotics that may outweigh the benefits. Antibiotics were historically commonly recommended to prevent IE in those with heart problems undergoing dental procedures (known as dental antibiotic prophylaxis). There is, however, insufficient evidence to support whether antibiotics are effective or ineffective at preventing IE when given prior to a dental procedures in people at high risk. They are less commonly recommended for this procedure. In some countries e.g. the US, high risk patients may be given prophylactic antibiotics such as penicillin or clindamycin for penicillin-allergic people prior to dental procedures. Prophylactics should be bactericidal rather thanbacteriostatic
A bacteriostatic agent or bacteriostat, abbreviated Bstatic, is a biological or chemical agent that stops bacteria from reproducing, while not necessarily killing them otherwise. Depending on their application, bacteriostatic antibiotics, disinfect ...
. Such measures are not taken in certain countries e.g. Scotland due to the fear of antibiotic resistance. Because bacteria are the most common cause of infective endocarditis, antibiotics such as penicillin and amoxicillin
Amoxicillin is an antibiotic medication used to treat a number of bacterial infections. These include middle ear infection, strep throat, pneumonia, skin infections, and urinary tract infections among others. It is taken by mouth, or less c ...
(for beta lactamase
Beta-lactamases, (β-lactamases) are enzymes () produced by bacteria that provide multi-resistance to beta-lactam antibiotics such as penicillins, cephalosporins, cephamycins, monobactams and carbapenems (ertapenem), although carbapenem ...
-producing bacteria) are used in prophylaxis.
Treatment
High-dose antibiotics are the cornerstone of treatment for infective endocarditis. These antibiotics are administered by the intravenous (IV) route to maximize diffusion of antibiotic molecules into vegetation(s) from the blood filling the chambers of the heart. This is necessary because neither the heart valves nor the vegetations adhering to them are supplied by blood vessels. Antibiotics are typically continued for two to six weeks depending on the characteristics of the infection and the causativemicroorganism
A microorganism, or microbe,, ''mikros'', "small") and ''organism'' from the el, ὀργανισμός, ''organismós'', "organism"). It is usually written as a single word but is sometimes hyphenated (''micro-organism''), especially in olde ...
s. Antibiotic treatment lowers the risk of embolic complications in people with infective endocarditis.
In acute endocarditis, due to the fulminant inflammation, empirical antibiotic therapy is started immediately after the blood has been drawn for blood culture, culture to clarify the bacterial organisms responsible for the infection. This usually includes vancomycin and ceftriaxone IV infusions until the infecting organism is identified and the susceptibility report with the minimum inhibitory concentration becomes available. Once this information is available, this allows the supervising healthcare professional to modify the antimicrobial therapy to target the specific infecting microorganism. The routine use of gentamicin to treat endocarditis has fallen out of favor due to the lack of evidence to support its use (except in infections caused by ''Enterococcus'' and nutritionally variant '' streptococci'') and the high rate of complications. In cases of subacute endocarditis, where the person's hemodynamic status is usually stable, antibiotic treatment can be delayed until the causative microorganism can be identified.
Viridans group '' streptococci'' and '' Streptococcus bovis'' are usually highly susceptible to penicillin and can be treated with penicillin or ceftriaxone. Relatively resistant strains of viridans streptococci, viridans group ''streptococci'' and ''Streptococcus bovis'' are treated with penicillin or ceftriaxone along with a shorter two-week course of an aminoglycoside during the initial phase of treatment. Highly penicillin-resistant strains of viridans group ''streptococci'', nutritionally variant ''streptococci'' like ''Granulicatella sp.'', ''Gemella sp.'', ''Abiotrophia defectiva'', and ''Enterococci'' are usually treated with a combination therapy consisting of penicillin and an aminoglycoside for the entire duration of 4–6 weeks.
Some people may be treated with a relatively shorter course of treatment (two weeks) with benzyl penicillin IV if infection is caused by viridans group ''streptococci'' or ''Streptococcus bovis'' as long as the following conditions are met:
* Endocarditis of a native valve, not of a prosthetic valve
* A minimum inhibitory concentration, MIC ≤ 0.12 mg/l
* A complication such as heart failure, Heart arrhythmia, arrhythmia, or pulmonary embolism occurs
* No evidence of extracardiac complication like septic thromboembolism
* No vegetations > 5 mm in diameter conduction defects
* Rapid clinical response and clearance of bloodstream infection
Additionally, oxacillin-susceptible ''Staphylococcus aureus'' native valve endocarditis of the right side can also be treated with a short 2-week course of a beta-lactam antibiotic such as nafcillin with or without aminoglycosides.
 The main indication for surgical treatment is Regurgitation (circulation), regurgitation or stenosis. In active infective endocarditis, the surgery should remove enough leaflet tissue to ensure eradication of the infectious process. Subsequent valve repair can be performed in limited disease. Replacement of the valve with a mechanical or bioprosthetic artificial heart valve is necessary in certain situations:
* Patients with significant valve stenosis or regurgitation causing heart failure
* Evidence of hemodynamic compromise in the form of elevated end-diastolic left ventricular or left atrial pressure or moderate to severe pulmonary hypertension
* Presence of intracardiac complications like paravalvular abscess, conduction defects or destructive penetrating lesions
* Recurrent septic emboli despite appropriate antibiotic treatment
* Large vegetations (> 10 mm)
* Persistently positive blood cultures despite appropriate antibiotic treatment
* Prosthetic valve dehiscence
* Relapsing infection in the presence of a prosthetic valve
* Abscess formation
* Early closure of mitral valve
* Infection caused by fungi or resistant Gram-negative bacteria.
The guidelines were recently updated by both the American College of Cardiology and the European Society of Cardiology. There was a recent meta-analysis published that showed surgical intervention at seven days or less is associated with lower mortality.
The main indication for surgical treatment is Regurgitation (circulation), regurgitation or stenosis. In active infective endocarditis, the surgery should remove enough leaflet tissue to ensure eradication of the infectious process. Subsequent valve repair can be performed in limited disease. Replacement of the valve with a mechanical or bioprosthetic artificial heart valve is necessary in certain situations:
* Patients with significant valve stenosis or regurgitation causing heart failure
* Evidence of hemodynamic compromise in the form of elevated end-diastolic left ventricular or left atrial pressure or moderate to severe pulmonary hypertension
* Presence of intracardiac complications like paravalvular abscess, conduction defects or destructive penetrating lesions
* Recurrent septic emboli despite appropriate antibiotic treatment
* Large vegetations (> 10 mm)
* Persistently positive blood cultures despite appropriate antibiotic treatment
* Prosthetic valve dehiscence
* Relapsing infection in the presence of a prosthetic valve
* Abscess formation
* Early closure of mitral valve
* Infection caused by fungi or resistant Gram-negative bacteria.
The guidelines were recently updated by both the American College of Cardiology and the European Society of Cardiology. There was a recent meta-analysis published that showed surgical intervention at seven days or less is associated with lower mortality.
Prognosis
Infective endocarditis is associated with 18% in-hospital mortality. As many as 50% of people with infective endocarditis may experience embolic complications.Epidemiology
In developed country, developed countries, the annual incidence (epidemiology), incidence of infective endocarditis is 3 to 9 cases per 100,000 persons. Infective endocarditis occurs more often in men than in women. There is an increased incidence of infective endocarditis in persons 65 years of age and older, which is probably because people in this age group have a larger number of risk factors for infective endocarditis. In recent years, over one-third of infective endocarditis cases in the United States was healthcare-associated. Another trend observed in developed countries is that chronic Rheumatic fever#Rheumatic heart disease, rheumatic heart disease accounts for less than 10% of cases. Although a history of valve disease has a significant association with infective endocarditis, 50% of all cases develop in people with no known history of valvular disease.History
Lazare Riviére first described infective endocarditis affecting the aortic valve in 1616. In 1806, Jean-Nicolas Corvisart coined the term ''vegetation'' to describe collections of debris found on a mitral valve affected by infective endocarditis. The British physician Joseph Hodgson was the first to describe the embolic complications of infective endocarditis in 1815. It was not until 1878 that Theodor Klebs first suggested that infective endocarditis had a microbial infectious origin. In 1909, William Osler noted that heart valves that experienced degeneration and were sclerotic or poorly functioning had a higher risk of being affected. Later, in 1924, Emanuel Libman and Benjamin Sacks described cases of Libman-Sacks endocarditis, vegetative endocarditis that lacked a clear microbial origin and were often associated with the autoimmune condition systemic lupus erythematosus. In 1944, physicians reported on the first successful use of penicillin to treat a case of infective endocarditis.References
External links
{{DEFAULTSORT:Infective Endocarditis Valvular heart disease Wikipedia medicine articles ready to translate