Hysterectomy on:
[Wikipedia]
[Google]
[Amazon]
Hysterectomy is the surgical removal of the
 Hysterectomy is a major surgical procedure that has risks and benefits. It affects the hormonal balance and overall health of patients. Because of this, hysterectomy is normally recommended as a last resort after pharmaceutical or other surgical options have been exhausted to remedy certain intractable and severe uterine/reproductive system conditions. There may be other reasons for a hysterectomy to be requested. Such conditions and/or indications include, but are not limited to:
*
Hysterectomy is a major surgical procedure that has risks and benefits. It affects the hormonal balance and overall health of patients. Because of this, hysterectomy is normally recommended as a last resort after pharmaceutical or other surgical options have been exhausted to remedy certain intractable and severe uterine/reproductive system conditions. There may be other reasons for a hysterectomy to be requested. Such conditions and/or indications include, but are not limited to:
*
pregnancy after hysterectomy
that took place in 2016, although no additional information has been brought forward. On very rare occasions, sexual intercourse after hysterectomy may cause a transvaginal evisceration of the small bowel. The

 Depending on the indication there are alternatives to hysterectomy:
Depending on the indication there are alternatives to hysterectomy:
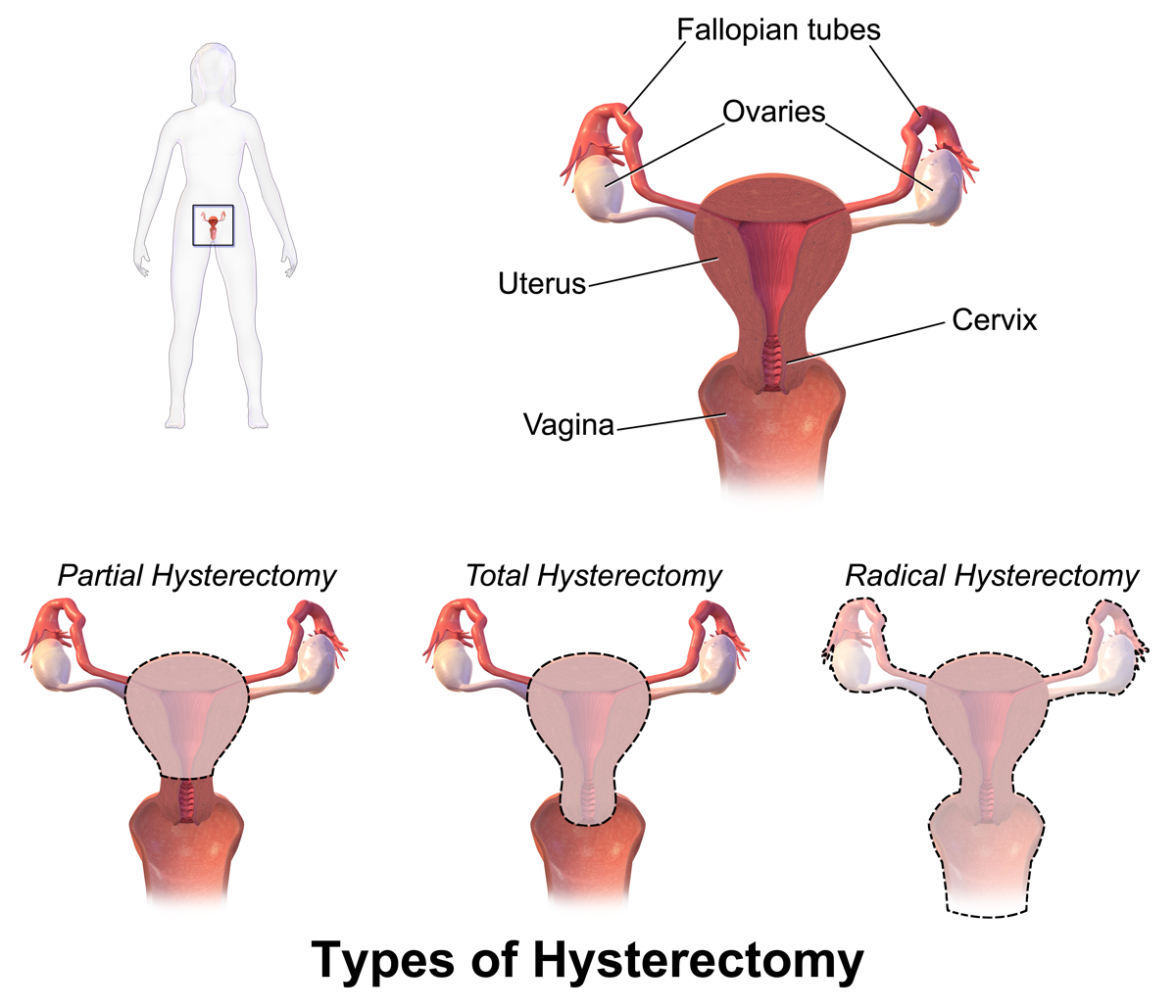
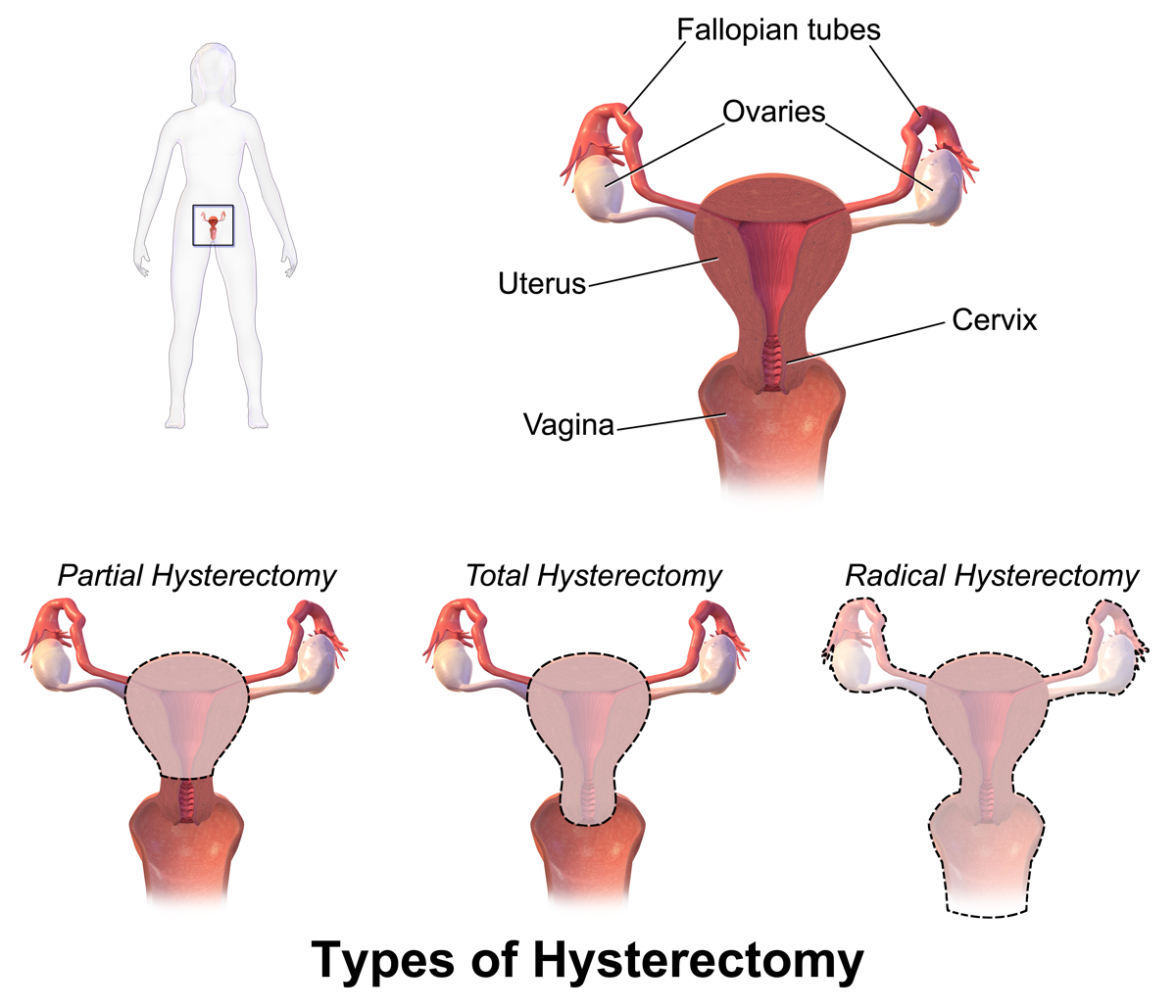
 Hysterectomy, in the literal sense of the word, means merely removal of the uterus. However other organs such as ovaries, fallopian tubes, and the cervix are very frequently removed as part of the surgery.
* Radical hysterectomy: complete removal of the uterus, cervix, upper vagina, and parametrium. Indicated for cancer. Lymph nodes, ovaries, and fallopian tubes are also usually removed in this situation, such as in '.
* Total hysterectomy: complete removal of the uterus and cervix, with or without oophorectomy.
* Subtotal hysterectomy: removal of the uterus, leaving the cervix in situ.
Subtotal (supracervical) hysterectomy was originally proposed with the expectation that it may improve sexual functioning after hysterectomy, it has been postulated that removing the cervix causes excessive neurologic and anatomic disruption, thus leading to vaginal shortening, vaginal vault prolapse, and vaginal cuff granulations. These theoretical advantages were not confirmed in practice, but other advantages over total hysterectomy emerged. The principal disadvantage is that risk of cervical cancer is not eliminated and women may continue cyclical bleeding (although substantially less than before the surgery).
These issues were addressed in a systematic review of total versus supracervical hysterectomy for benign gynecological conditions, which reported the following findings:
* There was no difference in the rates of incontinence, constipation, measures of sexual function, or alleviation of pre-surgery symptoms.
* Length of surgery and amount of blood lost during surgery were significantly reduced during supracervical hysterectomy compared to total hysterectomy, but there was no difference in post-operative transfusion rates.
* Febrile morbidity was less likely and ongoing cyclic vaginal bleeding one year after surgery was more likely after supracervical hysterectomy.
* There was no difference in the rates of other complications, recovery from surgery, or readmission rates.
In the short-term, randomized trials have shown that cervical preservation or removal does not affect the rate of subsequent pelvic organ prolapse.
Supracervical hysterectomy does not eliminate the possibility of having
Hysterectomy, in the literal sense of the word, means merely removal of the uterus. However other organs such as ovaries, fallopian tubes, and the cervix are very frequently removed as part of the surgery.
* Radical hysterectomy: complete removal of the uterus, cervix, upper vagina, and parametrium. Indicated for cancer. Lymph nodes, ovaries, and fallopian tubes are also usually removed in this situation, such as in '.
* Total hysterectomy: complete removal of the uterus and cervix, with or without oophorectomy.
* Subtotal hysterectomy: removal of the uterus, leaving the cervix in situ.
Subtotal (supracervical) hysterectomy was originally proposed with the expectation that it may improve sexual functioning after hysterectomy, it has been postulated that removing the cervix causes excessive neurologic and anatomic disruption, thus leading to vaginal shortening, vaginal vault prolapse, and vaginal cuff granulations. These theoretical advantages were not confirmed in practice, but other advantages over total hysterectomy emerged. The principal disadvantage is that risk of cervical cancer is not eliminated and women may continue cyclical bleeding (although substantially less than before the surgery).
These issues were addressed in a systematic review of total versus supracervical hysterectomy for benign gynecological conditions, which reported the following findings:
* There was no difference in the rates of incontinence, constipation, measures of sexual function, or alleviation of pre-surgery symptoms.
* Length of surgery and amount of blood lost during surgery were significantly reduced during supracervical hysterectomy compared to total hysterectomy, but there was no difference in post-operative transfusion rates.
* Febrile morbidity was less likely and ongoing cyclic vaginal bleeding one year after surgery was more likely after supracervical hysterectomy.
* There was no difference in the rates of other complications, recovery from surgery, or readmission rates.
In the short-term, randomized trials have shown that cervical preservation or removal does not affect the rate of subsequent pelvic organ prolapse.
Supracervical hysterectomy does not eliminate the possibility of having
File:Hysterectomy1.jpg, Uterus prior to hysterectomy
File:Hysterectomy2.jpg, Laparoscopical hysterectomy
File:LASH.jpg, Cervical stump (white) after removal of the uterine corpus at laparoscopic supracervical hysterectomy
File:Total laparoscopical hysterectomy.jpg, Transvaginal extraction of the uterus in total laparoscopical hysterectomy
File:Hysterectomy3.jpg, End of a laparoscopical hysterectomy
Oncolex.org features live footage videos showing radical hysterctomies
{{Authority control Gender-affirming surgery (female-to-male) Gynaecology Gynecological surgery Reproductive system Sterilization (medicine) Surgical oncology Surgical removal procedures
uterus
The uterus (from Latin ''uterus'', plural ''uteri'') or womb () is the organ in the reproductive system of most female mammals, including humans that accommodates the embryonic and fetal development of one or more embryos until birth. The ...
. It may also involve removal of the cervix
The cervix or cervix uteri (Latin, 'neck of the uterus') is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long (~1 inch) and roughly cylindrical in shape, which changes during ...
, ovaries
The ovary is an organ in the female reproductive system that produces an ovum. When released, this travels down the fallopian tube into the uterus, where it may become fertilized by a sperm. There is an ovary () found on each side of the body. T ...
( oophorectomy), Fallopian tube
The fallopian tubes, also known as uterine tubes, oviducts or salpinges (singular salpinx), are paired tubes in the human female that stretch from the uterus to the ovaries. The fallopian tubes are part of the female reproductive system. In o ...
s ( salpingectomy), and other surrounding structures.
Usually performed by a gynecologist
Gynaecology or gynecology (see spelling differences) is the area of medicine that involves the treatment of women's diseases, especially those of the reproductive organs. It is often paired with the field of obstetrics, forming the combined ...
, a hysterectomy may be total (removing the body, fundus, and cervix of the uterus; often called "complete") or partial (removal of the uterine body while leaving the cervix intact; also called "supracervical"). Removal of the uterus renders the patient unable to bear children (as does removal of ovaries
The ovary is an organ in the female reproductive system that produces an ovum. When released, this travels down the fallopian tube into the uterus, where it may become fertilized by a sperm. There is an ovary () found on each side of the body. T ...
and fallopian tube
The fallopian tubes, also known as uterine tubes, oviducts or salpinges (singular salpinx), are paired tubes in the human female that stretch from the uterus to the ovaries. The fallopian tubes are part of the female reproductive system. In o ...
s) and has surgical risks as well as long-term effects, so the surgery is normally recommended only when other treatment options are not available or have failed. It is the second most commonly performed gynecological surgical procedure, after cesarean section, in the United States. Nearly 68 percent were performed for conditions such as endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fa ...
, irregular bleeding, and uterine fibroid
Uterine fibroids, also known as uterine leiomyomas or fibroids, are benign smooth muscle tumors of the uterus. Most women with fibroids have no symptoms while others may have painful or heavy periods. If large enough, they may push on the bl ...
s. It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.
Medical uses
 Hysterectomy is a major surgical procedure that has risks and benefits. It affects the hormonal balance and overall health of patients. Because of this, hysterectomy is normally recommended as a last resort after pharmaceutical or other surgical options have been exhausted to remedy certain intractable and severe uterine/reproductive system conditions. There may be other reasons for a hysterectomy to be requested. Such conditions and/or indications include, but are not limited to:
*
Hysterectomy is a major surgical procedure that has risks and benefits. It affects the hormonal balance and overall health of patients. Because of this, hysterectomy is normally recommended as a last resort after pharmaceutical or other surgical options have been exhausted to remedy certain intractable and severe uterine/reproductive system conditions. There may be other reasons for a hysterectomy to be requested. Such conditions and/or indications include, but are not limited to:
* Endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fa ...
: growth of the uterine lining outside the uterine cavity. This inappropriate tissue growth can lead to pain and bleeding.
* Adenomyosis
Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus ( endometrium) atypically located among the cells of the uterine wall ( myometrium), as a result, thickening of the uterus occurs. ...
: a form of endometriosis, where the uterine lining has grown into and sometimes through the uterine wall musculature. This can thicken the uterine walls and also contribute to pain and bleeding.
* Heavy menstrual bleeding: irregular or excessive menstrual bleeding for greater than a week. It can disturb regular quality of life and may be indicative of a more serious condition.
* Uterine fibroids: benign growths on the uterus wall. These muscular noncancerous tumors can grow in single form or in clusters and can cause extreme pain and bleeding.
* Uterine prolapse: when the uterus sags down due to weakened or stretched pelvic floor muscles potentially causing the uterus to protrude out of the vagina in more severe cases.
* Reproductive system cancer prevention
Cancer prevention is the practice of taking active measures to decrease the incidence of cancer and mortality. The practice of prevention is dependent upon both individual efforts to improve lifestyle and seek preventive screening, and socioeconom ...
: especially if there is a strong family history of reproductive system cancers (especially breast cancer
Breast cancer is cancer that develops from breast tissue. Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, milk rejection, fluid coming from the nipple, a newly inverted nipple, or ...
in conjunction with BRCA1 or BRCA2 mutation), or as part of recovery from such cancers.
* Gynecologic cancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal b ...
: depending on the type of hysterectomy, can aid in treatment of cancer or precancer of the endometrium, cervix, or uterus. In order to protect against or treat cancer of the ovaries, would need an oophorectomy.
* Transgender
A transgender (often abbreviated as trans) person is someone whose gender identity or gender expression does not correspond with their sex assigned at birth. Many transgender people experience dysphoria, which they seek to alleviate through ...
(trans) male affirmation: aids in gender dysphoria
Gender dysphoria (GD) is the distress a person experiences due to a mismatch between their gender identitytheir personal sense of their own genderand their sex assigned at birth. The diagnostic label gender identity disorder (GID) was used unti ...
, prevention of future gynecologic problems, and transition to obtaining new legal gender documentation.
* Severe developmental disabilities: this treatment is controversial at best. In the United States, specific cases of sterilization due to developmental disabilities have been found by state-level Supreme Courts to violate the patient's constitutional and common-law rights.
* Postpartum: to remove either a severe case of placenta praevia (a placenta that has either formed over or inside the birth canal) or placenta percreta (a placenta that has grown into and through the wall of the uterus to attach itself to other organs), as well as a last resort in case of excessive obstetrical haemorrhage.
* Chronic pelvic pain
Pelvic pain is pain in the area of the pelvis. Acute pain is more common than chronic pain. If the pain lasts for more than six months, it is deemed to be chronic pelvic pain. It can affect both the male and female pelvis.
Common causes in include ...
: should try to obtain pain etiology, although may have no known cause.
Risks and adverse effects
In 1995, the short-term mortality (within 40 days of surgery) was reported at 0.38 cases per 1000 when performed for benign causes. Risks for surgical complications were presence of fibroids, younger age (vascular pelvis with higher bleeding risk and larger uterus), dysfunctional uterine bleeding and parity. The mortality rate is several times higher when performed in patients who are pregnant, have cancer or other complications. Long-term effect on all case mortality is relatively small. People under the age of 45 years have a significantly increased long-term mortality that is believed to be caused by the hormonal side effects of hysterectomy and prophylactic oophorectomy., which cites: * This effect is not limited to pre-menopausal people; even people who have already entered menopause were shown to have experienced a decrease in long-term survivability post-oophorectomy. Approximately 35% of people after hysterectomy undergo another related surgery within 2 years. Ureteral injury is not uncommon and occurs in 0.2 per 1,000 cases of vaginal hysterectomy and 1.3 per 1,000 cases of abdominal hysterectomy. The injury usually occurs in the distal ureter close to theinfundibulopelvic ligament
The suspensory ligament of the ovary, also infundibulopelvic ligament (commonly abbreviated IP ligament or simply IP), is a fold of peritoneum that extends out from the ovary to the wall of the pelvis.
Some sources consider it a part of the broad ...
or as a ureter crosses below the uterine artery, often from blind clamping and ligature placement to control hemorrhage.
Recovery
Hospital stay is 3 to 5 days or more for the abdominal procedure and between 1 and 2 days (but possibly longer) for vaginal or laparoscopically assisted vaginal procedures. After the procedure, the American College of Obstetricians and Gynecologists recommends not inserting anything into the vagina for the first 6 weeks (including inserting tampons or having sex).Unintended oophorectomy and premature ovarian failure
Removal of one or both ovaries is performed in a substantial number of hysterectomies that were intended to be ovary sparing. The average onset age ofmenopause
Menopause, also known as the climacteric, is the time in women's lives when menstrual periods stop permanently, and they are no longer able to bear children. Menopause usually occurs between the age of 47 and 54. Medical professionals often d ...
after hysterectomy with ovarian conservation is 3.7 years earlier than average. This has been suggested to be due to the disruption of blood supply to the ovaries after a hysterectomy or due to missing endocrine feedback of the uterus. The function of the remaining ovaries is significantly affected in about 40% of people, some of them even require hormone replacement therapy. Surprisingly, a similar and only slightly weaker effect has been observed for endometrial ablation which is often considered as an alternative to hysterectomy.
A substantial number of people develop benign ovarian cysts after a hysterectomy.
Effects on sexual life and pelvic pain
After hysterectomy for benign indications the majority of patients report improvement in sexual life and pelvic pain. A smaller share of patients report worsening of sexual life and other problems. The picture is significantly different for hysterectomy performed for malignant reasons; the procedure is often more radical with substantial side effects. A proportion of patients who undergo a hysterectomy for chronic pelvic pain continue to have pelvic pain after a hysterectomy and developdyspareunia
Dyspareunia ( ) is painful sexual intercourse due to medical or psychological causes. The term ''dyspareunia'' covers both female dyspareunia and male dyspareunia, but many discussions that use the term without further specification concern the ...
(painful sexual intercourse).
Premature menopause and its effects
Estrogen levels fall sharply when the ovaries are removed, removing the protective effects of estrogen on the cardiovascular and skeletal systems. This condition is often referred to as "surgical menopause", although it is substantially different from a naturally occurring menopausal state; the former is a sudden hormonal shock to the body that causes rapid onset of menopausal symptoms such as hot flashes, while the latter is a gradually occurring decrease of hormonal levels over a period of years with uterus intact and ovaries able to produce hormones even after the cessation of menstrual periods. One study showed that risk of subsequent cardiovascular disease is substantially increased for people who had hysterectomy at age 50 or younger. No association was found for women undergoing the procedure after age 50. The risk is higher when ovaries are removed but still noticeable even when ovaries are preserved. Several other studies have found that osteoporosis (decrease in bone density) and increased risk ofbone fracture
A bone fracture (abbreviated FRX or Fx, Fx, or #) is a medical condition in which there is a partial or complete break in the continuity of any bone in the body. In more severe cases, the bone may be broken into several fragments, known as a '' ...
s are associated with hysterectomies. This has been attributed to the modulatory effect of estrogen on calcium metabolism and the drop in serum estrogen levels after menopause can cause excessive loss of calcium leading to bone wasting.
Hysterectomies have also been linked with higher rates of heart disease and weakened bones. Those who have undergone a hysterectomy with both ovaries removed typically have reduced testosterone levels as compared to those left intact. Reduced levels of testosterone in women are predictive of height loss, which may occur as a result of reduced bone density, while increased testosterone levels in women are associated with a greater sense of sexual desire.
Oophorectomy before the age of 45 is associated with a fivefold mortality from neurologic and mental disorders.
Urinary incontinence and vaginal prolapse
Urinary incontinence and vaginal prolapse are well known adverse effects that develop with high frequency a very long time after the surgery. Typically, those complications develop 10–20 years after the surgery. For this reason exact numbers are not known, and risk factors are poorly understood. It is also unknown if the choice of surgical technique has any effect. It has been assessed that the risk for urinary incontinence is approximately doubled within 20 years after hysterectomy. One long-term study found a 2.4 fold increased risk for surgery to correct urinary stress incontinence following hysterectomy. The risk for vaginal prolapse depends on factors such as number of vaginal deliveries, the difficulty of those deliveries, and the type of labor. Overall incidence is approximately doubled after hysterectomy.Adhesion formation and bowel obstruction
The formation of postoperative adhesions is a particular risk after hysterectomy because of the extent of dissection involved as well as the fact the hysterectomy wound is in the most gravity-dependent part of the pelvis into which a loop of bowel may easily fall. In one review, incidence ofsmall bowel obstruction
Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs an ...
due to intestinal adhesion was found to be 15.6% in non-laparoscopic total abdominal hysterectomies vs. 0.0% in laparoscopic hysterectomies.
Wound infection
Wound infection occurs in approximately 3% of cases of abdominal hysterectomy. The risk is increased by obesity, diabetes, immunodeficiency disorder, use of systemic corticosteroids, smoking, wound hematoma, and preexisting infection such as chorioamnionitis andpelvic inflammatory disease
Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be ...
. Such wound infections mainly take the form of either incisional abscess or wound cellulitis. Typically, both confer erythema, but only an incisional abscess confers purulent drainage. The recommended treatment of an incisional abscess after hysterectomy is by incision and drainage, and then coverage by a thin layer of gauze followed by sterile dressing. The dressing should be changed and the wound irrigated with normal saline at least twice each day. In addition, it is recommended to administer an antibiotic active against staphylococci and streptococci, preferably vancomycin
Vancomycin is a glycopeptide antibiotic medication used to treat a number of bacterial infections. It is recommended intravenously as a treatment for complicated skin infections, bloodstream infections, endocarditis, bone and joint infection ...
when there is a risk of MRSA. The wound can be allowed to close by secondary intention
Wound healing refers to a living organism's replacement of destroyed or damaged tissue by newly produced tissue.
In undamaged skin, the epidermis (surface, epithelial layer) and dermis (deeper, connective layer) form a protective barrier agains ...
. Alternatively, if the infection is cleared and healthy granulation tissue is evident at the base of the wound, the edges of the incision may be reapproximated, such as by using butterfly stitches, staples or sutures. Sexual intercourse remains possible after hysterectomy. Reconstructive surgery remains an option for people who have experienced benign and malignant conditions.
Other rare problems
Hysterectomy may cause an increased risk of the relatively rarerenal cell carcinoma
Renal cell carcinoma (RCC) is a kidney cancer that originates in the lining of the proximal convoluted tubule, a part of the very small tubes in the kidney that transport primary urine. RCC is the most common type of kidney cancer in adults, re ...
. The increased risk is particularly pronounced for young people; the risk was lower after vaginally performed hysterectomies. Hormonal effects or injury of the ureter were considered as possible explanations. In some cases the renal cell carcinoma may be a manifestation of an undiagnosed hereditary leiomyomatosis and renal cell cancer syndrome.
Removal of the uterus without removing the ovaries can produce a situation that on rare occasions can result in ectopic pregnancy
Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptom ...
due to an undetected fertilization that had yet to descend into the uterus before surgery. Two cases have been identified and profiled in an issue of the ''Blackwell Journal of Obstetrics and Gynecology''; over 20 other cases have been discussed in additional medical literature. There is possibly another case of ectopipregnancy after hysterectomy
that took place in 2016, although no additional information has been brought forward. On very rare occasions, sexual intercourse after hysterectomy may cause a transvaginal evisceration of the small bowel. The
vaginal cuff The vaginal cuff is the upper portion of the vagina that opens up into the peritoneum and is sutured shut after the removal of the cervix and uterus during a hysterectomy.
The vaginal cuff is created by suturing together the edges of the surgical ...
is the uppermost region of the vagina that has been sutured closed. A rare complication, it can dehisce and allow the evisceration of the small bowel into the vagina.
Alternatives

 Depending on the indication there are alternatives to hysterectomy:
Depending on the indication there are alternatives to hysterectomy:
Heavy bleeding
Levonorgestrel intrauterine devices are highly effective at controlling dysfunctional uterine bleeding (DUB) or menorrhagia and should be considered before any surgery. Menorrhagia (heavy or abnormal menstrual bleeding) may also be treated with the less invasive endometrial ablation which is an outpatient procedure in which the lining of the uterus is destroyed with heat, mechanically or by radio frequency ablation. Endometrial ablation greatly reduces or eliminates monthly bleeding in ninety percent of patients with DUB. It is not effective for patients with very thick uterine lining or uterine fibroids.Uterine fibroids
Levonorgestrel intrauterine devices are highly effective in limiting menstrual blood flow and improving other symptoms. Side effects are typically very moderate because the levonorgestrel (aprogestin
A progestogen, also referred to as a progestagen, gestagen, or gestogen, is a type of medication which produces effects similar to those of the natural female sex hormone progesterone in the body. A progestin is a ''synthetic'' progestogen. Pro ...
) is released in low concentration locally. There is now substantial evidence that Levongestrel-IUDs provide good symptomatic relief for women with fibroids.
Uterine fibroids may be removed and the uterus reconstructed in a procedure called " myomectomy". A myomectomy may be performed through an open incision, laparoscopically, or through the vagina (hysteroscopy).
'' Uterine artery embolization'' (UAE) is a minimally invasive procedure for treatment of uterine fibroid
Uterine fibroids, also known as uterine leiomyomas or fibroids, are benign smooth muscle tumors of the uterus. Most women with fibroids have no symptoms while others may have painful or heavy periods. If large enough, they may push on the bl ...
s. Under local anesthesia a catheter is introduced into the femoral artery at the groin and advanced under radiographic control into the uterine artery. A mass of microspheres or polyvinyl alcohol
Poly(vinyl alcohol) (PVOH, PVA, or PVAl) is a water- soluble synthetic polymer. It has the idealized formula H2CH(OH)sub>''n''. It is used in papermaking, textile warp sizing, as a thickener and emulsion stabilizer in polyvinyl acetate (PVAc) ...
(PVA) material (an embolus) is injected into the uterine arteries in order to block the flow of blood through those vessels. The restriction in blood supply usually results in significant reduction of fibroids and improvement of heavy bleeding tendency. The 2012 Cochrane review comparing hysterectomy and UAE did not find any major advantage for either procedure. While UAE is associated with shorter hospital stay and a more rapid return to normal daily activities, it was also associated with a higher risk for minor complications later on. There were no differences between UAE and hysterectomy with regards to major complications.
Uterine fibroids can be removed with a non-invasive procedure called Magnetic Resonance guided Focused Ultrasound (MRgFUS).
Uterine prolapse
Prolapse may also be corrected surgically without removal of the uterus. There are several strategies that can be utilized to help strengthen pelvic floor muscles and prevent the worsening of prolapse. These include, but are not limited to, use of " kegel exercises", vaginal pessary, constipation relief, weight management, and care when lifting heavy objects.Types
cervical cancer
Cervical cancer is a cancer arising from the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Early on, typically no symptoms are seen. Later symptoms may include abnormal ...
since the cervix itself is left intact and may be contraindicated in women with increased risk of this cancer; regular pap smears to check for cervical dysplasia
Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is the abnormal growth of cells on the surface of the cervix that could potentially lead to cervical cancer. More specifically, CIN refers to the potentially precancerous t ...
or cancer
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal b ...
are still needed.
Technique
Hysterectomy can be performed in different ways. The oldest known technique is vaginal hysterectomy. The first planned hysterectomy was performed by Konrad Langenbeck - Surgeon General of the Hannovarian army, although there are records of vaginal hysterectomy for prolapse going back as far as 50BC. The first abdominal hysterectomy recorded was by Ephraim McDowell. He performed the procedure in 1809 for a mother of five for a large ovarian mass on her kitchen table. In modern medicine today, laparoscopic vaginal (with additional instruments passing through ports in small abdominal incisions, close or in the navel) and total laparoscopic techniques have been developed.Abdominal hysterectomy
Most hysterectomies in the United States are done vialaparotomy
A laparotomy is a surgical procedure involving a surgical incision through the abdominal wall to gain access into the abdominal cavity. It is also known as a celiotomy.
Origins and history
The first successful laparotomy was performed without ane ...
(abdominal incision, not to be confused with laparoscopy). A transverse (Pfannenstiel) incision is made through the abdominal wall, usually above the pubic bone, as close to the upper hair line of the individual's lower pelvis
The pelvis (plural pelves or pelvises) is the lower part of the trunk, between the abdomen and the thighs (sometimes also called pelvic region), together with its embedded skeleton (sometimes also called bony pelvis, or pelvic skeleton).
The ...
as possible, similar to the incision made for a caesarean section. This technique allows physician
A physician (American English), medical practitioner (Commonwealth English), medical doctor, or simply doctor, is a health professional who practices medicine, which is concerned with promoting, maintaining or restoring health through th ...
s the greatest access to the reproductive structures and is normally done for removal of the entire reproductive complex. The recovery time for an open hysterectomy is 4–6 weeks and sometimes longer due to the need to cut through the abdominal wall. Historically, the biggest problem with this technique was infections, but infection rates are well-controlled and not a major concern in modern medical practice. An open hysterectomy provides the most effective way to explore the abdominal cavity and perform complicated surgeries. Before the refinement of the vaginal and laparoscopic vaginal techniques, it was also the only possibility to achieve subtotal hysterectomy; meanwhile, the vaginal route is the preferable technique in most circumstances.
Vaginal hysterectomy
Vaginal hysterectomy is performed entirely through the vaginal canal and has clear advantages over abdominal surgery such as fewer complications, shorter hospital stays and shorter healing time. Abdominal hysterectomy, the most common method, is used in cases such as after caesarean delivery, when the indication is cancer, when complications are expected, or surgical exploration is required.Laparoscopic-assisted vaginal hysterectomy
With the development of laparoscopic techniques in the 1970s and 1980s, the "laparoscopic-assisted vaginal hysterectomy" (LAVH) has gained great popularity amonggynecologist
Gynaecology or gynecology (see spelling differences) is the area of medicine that involves the treatment of women's diseases, especially those of the reproductive organs. It is often paired with the field of obstetrics, forming the combined ...
s because compared with the abdominal procedure it is less invasive and the post-operative recovery is much faster. It also allows better exploration and slightly more complicated surgeries than the vaginal procedure. LAVH begins with laparoscopy and is completed such that the final removal of the uterus (with or without removing the ovaries) is via the vaginal canal. Thus, LAVH is also a total hysterectomy; the cervix is removed with the uterus. If the cervix is removed along with the uterus, the upper portion of the vagina is sutured together and called the vaginal cuff The vaginal cuff is the upper portion of the vagina that opens up into the peritoneum and is sutured shut after the removal of the cervix and uterus during a hysterectomy.
The vaginal cuff is created by suturing together the edges of the surgical ...
.
Laparoscopic-assisted supracervical hysterectomy
The "laparoscopic-assisted supracervical hysterectomy" (LASH) was later developed to remove the uterus without removing the cervix using a morcellator which cuts the uterus into small pieces that can be removed from the abdominal cavity via the laparoscopic ports.Total laparoscopic hysterectomy
Total laparoscopic hysterectomy (TLH) was developed in the early 90s by Prabhat K. Ahluwalia in Upstate New York. TLH is performed solely through the laparoscopes in the abdomen, starting at the top of the uterus, typically with a uterine manipulator. The entire uterus is disconnected from its attachments using long thin instruments through the "ports". Then all tissue to be removed is passed through the small abdominal incisions.Other techniques
Supracervical (subtotal) laparoscopic hysterectomy (LSH) is performed similar to the total laparoscopic surgery but the uterus is amputated between the cervix and fundus. Dual-port laparoscopy is a form of laparoscopic surgery using two 5 mm midline incisions: the uterus is detached through the two ports and removed through the vagina. "Robotic hysterectomy" is a variant of laparoscopic surgery using special remotely controlled instruments that allow the surgeon finer control as well as three-dimensional magnified vision.Comparison of techniques
Patient characteristics such as the reason for needing a hysterectomy, uterine size, descent of the uterus, presence of diseased tissues surrounding the uterus, previous surgery in the pelvic region, obesity, history of pregnancy, the possibility ofendometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fa ...
, or the need for an oophorectomy, will influence a surgeon's surgical approach when performing a hysterectomy.
Vaginal hysterectomy is recommended over other variants where possible for women with benign diseases. Vaginal hysterectomy was shown to be superior to LAVH and some types of laparoscopic surgery causing fewer short- and long-term complications, more favorable effect on sexual experience with shorter recovery times and fewer costs.
Laparoscopic surgery offers certain advantages when vaginal surgery is not possible but also has the disadvantage of significantly longer time required for the surgery.
In one 2004 study conducted in the UK comparing abdominal (laparotomic) and laparoscopic techniques, laparoscopic surgery was found to cause longer operation time and a higher rate of major complications while offering much quicker healing. In another study conducted in 2014, laparoscopy was found to be "a safe alternative to laparotomy" in patients receiving total hysterectomy for endometrial cancer. Researchers concluded the procedure "offers markedly improved perioperative outcomes with a lower reoperation rate and fewer postoperative complications when the standard of care shifts from open surgery to laparoscopy in a university hospital".
The abdominal technique is very often applied in difficult circumstances or when complications are expected. Given these circumstances the complication rate and time required for surgery compares very favorably with other techniques, however time required for healing is much longer.
Hysterectomy by abdominal laparotomy is correlated with much higher incidence of intestinal adhesions than other techniques.
Time required for completion of surgery in the eVAL trial is reported as follows:
* abdominal 55.2 minutes average, range 19–155
* vaginal 46.6 minutes average, range 14–168
* laparoscopic (all variants) 82.5 minutes average, range 10–325 (combined data from both trial arms)
Morcellation has been widely used especially in laparoscopic techniques and sometimes for the vaginal technique, but now appears to be associated with a considerable risk of spreading benign or malignant tumors. In April 2014, the FDA issued a memo alerting medical practitioners to the risks of power morcellation.
Robotic assisted surgery is presently used in several countries for hysterectomies. Additional research is required to determine the benefits and risks involved, compared to conventional laparoscopic surgery.
A 2014 Cochrane review found that robotic assisted surgery may have a similar complication rate when compared to conventional laparoscopic surgery. In addition, there is evidence to suggest that although the surgery make take longer, robotic assisted surgery may result in shorter hospital stays. More research is necessary to determine if robotic assisted hysterectomies are beneficial for people with cancer.
Previously reported marginal advantages of robotic assisted surgery could not be confirmed; only differences in hospital stay and cost remain statistically significant.
In addition, concerns over widespread misleading marketing claims have been raised.
Incidence
Canada
InCanada
Canada is a country in North America. Its ten provinces and three territories extend from the Atlantic Ocean to the Pacific Ocean and northward into the Arctic Ocean, covering over , making it the world's second-largest country by to ...
, the ''number'' of hysterectomies between 2008 and 2009 was almost 47,000. The national rate for the same timeline was 338 per 100,000 population, down from 484 per 100,000 in 1997. The reasons for hysterectomies differed depending on whether the woman was living in an urban or rural location. Urban women opted for hysterectomies due to uterine fibroid
Uterine fibroids, also known as uterine leiomyomas or fibroids, are benign smooth muscle tumors of the uterus. Most women with fibroids have no symptoms while others may have painful or heavy periods. If large enough, they may push on the bl ...
s and rural women had hysterectomies mostly for menstrual disorders.
United States
Hysterectomy is the second most common major surgery among women in the United States (the first is cesarean section). In the 1980s and 1990s, this statistic was the source of concern among some consumer rights groups and puzzlement among the medical community, and brought about informed choice advocacy groups like Hysterectomy Educational Resources and Services (HERS) Foundation, founded by Nora W. Coffey in 1982. According to theNational Center for Health Statistics
The National Center for Health Statistics (NCHS) is a U.S. government agency that provides statistical information to guide actions and policies to improve the public health of the American people. It is a unit of the Centers for Disease Control ...
, of the 617,000 hysterectomies performed in 2004, 73% also involved the surgical removal of the ovaries. There are currently an estimated 22 million women in the United States who have undergone this procedure. Nearly 68 percent were performed for benign conditions such as endometriosis, irregular bleeding and uterine fibroids. Such rates being highest in the industrialized world has led to the controversy that hysterectomies are being largely performed for unwarranted reasons. More recent data suggests that the number of hysterectomies performed has declined in every state in the United States. From 2010 to 2013, there were 12 percent fewer hysterectomies performed, and the types of hysterectomies were more minimally invasive in nature, reflected by a 17 percent increase in laparoscopic procedures.
United Kingdom
In the UK, 1 in 5 women is likely to have a hysterectomy by the age of 60, and ovaries are removed in about 20% of hysterectomies.Germany
The number of hysterectomies inGermany
Germany,, officially the Federal Republic of Germany, is a country in Central Europe. It is the second most populous country in Europe after Russia, and the most populous member state of the European Union. Germany is situated betwee ...
has been constant for many years. In 2006, 149,456 hysterectomies were performed. Additionally, Of these, 126,743 (84.8%) successfully benefitted the patient without incident. Women between the ages of 40 and 49 accounted for 50 percent of hysterectomies, and those between the ages of 50 and 59 accounted for 20 percent. In 2007, the number of hysterectomies decreased to 138,164. In recent years, the technique of laparoscopic or laparoscopically assisted hysterectomies has been raised into the foreground.
Denmark
InDenmark
)
, song = ( en, "King Christian stood by the lofty mast")
, song_type = National and royal anthem
, image_map = EU-Denmark.svg
, map_caption =
, subdivision_type = Sovereign state
, subdivision_name = Kingdom of Denmark
, establish ...
, the number of hysterectomies from the 1980s to the 1990s decreased by 38 percent. In 1988, there were 173 such surgeries per 100,000 women, and by 1998 this number had been reduced to 107. The proportion of abdominal supracervical hysterectomies in the same time period grew from 7.5 to 41 percent. A total of 67,096 women underwent hysterectomy during these years.
See also
* List of surgeries by typeReferences
External links
* *Oncolex.org features live footage videos showing radical hysterctomies
{{Authority control Gender-affirming surgery (female-to-male) Gynaecology Gynecological surgery Reproductive system Sterilization (medicine) Surgical oncology Surgical removal procedures