Epidural anaesthesia on:
[Wikipedia]
[Google]
[Amazon]
Epidural administration (from
 An epidural is injected into the epidural space, inside the bony spinal canal but just outside the dura. In contact with the inner surface of the dura is another membrane called the
An epidural is injected into the epidural space, inside the bony spinal canal but just outside the dura. In contact with the inner surface of the dura is another membrane called the
 Epidural administration is a procedure which requires the person performing the insertion to be technically proficient in order to avoid complications. Proficiency may be trained using bananas or other fruits as a model.
The person receiving the epidural may be seated, or lying on their side or stomach. The level of the spine at which the catheter is placed depends mainly on the site of intended operation – based on the location of the pain. The iliac crest is a commonly used anatomical landmark for lumbar epidural injections, as this level roughly corresponds with the fourth lumbar vertebra, which is usually well below the termination of the spinal cord. The
Epidural administration is a procedure which requires the person performing the insertion to be technically proficient in order to avoid complications. Proficiency may be trained using bananas or other fruits as a model.
The person receiving the epidural may be seated, or lying on their side or stomach. The level of the spine at which the catheter is placed depends mainly on the site of intended operation – based on the location of the pain. The iliac crest is a commonly used anatomical landmark for lumbar epidural injections, as this level roughly corresponds with the fourth lumbar vertebra, which is usually well below the termination of the spinal cord. The
 The first record of an epidural injection is from 1885, when American neurologist James Corning of Acorn Hall in Morristown, NJ used the technique to perform a
The first record of an epidural injection is from 1885, when American neurologist James Corning of Acorn Hall in Morristown, NJ used the technique to perform a
available online
* *
{{Use mdy dates, date=September 2016 Childbirth Regional anesthesia Obstetrical procedures Dosage forms Spanish inventions
Ancient Greek
Ancient Greek includes the forms of the Greek language used in ancient Greece and the ancient world from around 1500 BC to 300 BC. It is often roughly divided into the following periods: Mycenaean Greek (), Dark Ages (), the Archaic pe ...
ἐπί, , upon" + ''dura mater
In neuroanatomy, dura mater is a thick membrane made of dense irregular connective tissue that surrounds the brain and spinal cord. It is the outermost of the three layers of membrane called the meninges that protect the central nervous system. ...
'') is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord
The spinal cord is a long, thin, tubular structure made up of nervous tissue, which extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column (backbone). The backbone encloses the central canal of the sp ...
. The epidural route is used by physicians and nurse anesthetists
A nurse anesthetist is an advanced practice nurse who administers anesthesia for surgery or other medical procedures. They are involved in the administration of anesthesia in a majority of countries, with varying levels of autonomy.
A survey pu ...
to administer local anesthetic
A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general a ...
agents, analgesic
An analgesic drug, also called simply an analgesic (American English), analgaesic (British English), pain reliever, or painkiller, is any member of the group of drugs used to achieve relief from pain (that is, analgesia or pain management). It ...
s, diagnostic
Diagnosis is the identification of the nature and cause of a certain phenomenon. Diagnosis is used in many different disciplines, with variations in the use of logic, analytics, and experience, to determine "cause and effect". In systems enginee ...
medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter
In medicine, a catheter (/ˈkæθətər/) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgi ...
into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés. In the United States, over 50% of childbirths involve the use of epidural anesthesia.
Epidural anaesthesia causes a loss of sensation
Sensation (psychology) refers to the processing of the senses by the sensory system.
Sensation or sensations may also refer to:
In arts and entertainment In literature
* Sensation (fiction), a fiction writing mode
* Sensation novel, a Briti ...
, including pain
Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, ...
, by blocking the transmission of signals through nerve fibres in or near the spinal cord. For this reason, epidurals are commonly used for pain control during childbirth
Childbirth, also known as labour and delivery, is the ending of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million births glob ...
and surgery
Surgery ''cheirourgikē'' (composed of χείρ, "hand", and ἔργον, "work"), via la, chirurgiae, meaning "hand work". is a medical specialty that uses operative manual and instrumental techniques on a person to investigate or treat a pa ...
. The technique is considered safe and effective for providing pain relief during childbirth and surgery, and is considered more effective and safer than giving pain medication by mouth or through an intravenous line. An epidural injection may also be used to administer steroids
A steroid is a biologically active organic compound with four rings arranged in a specific molecular configuration. Steroids have two principal biological functions: as important components of cell membranes that alter membrane fluidity; and ...
for the treatment of inflammatory conditions of the spinal cord. It is not recommended for people with severe bleeding disorders, low platelets, or infections near the intended injection site. Severe complications from epidural administration are rare, but can include problems resulting from improper administration, as well as side effects of the medicines administered. The most common complications of epidural injections include bleeding problems, headache
Headache is the symptom of pain in the face, head, or neck. It can occur as a migraine, tension-type headache, or cluster headache. There is an increased risk of depression in those with severe headaches.
Headaches can occur as a result ...
s, and inadequate pain control. Epidural analgesia during childbirth may also impact the mother's ability to move during labor. Very large doses of anesthetics or analgesics may result in respiratory depression
Hypoventilation (also known as respiratory depression) occurs when ventilation is inadequate (''hypo'' meaning "below") to perform needed respiratory gas exchange. By definition it causes an increased concentration of carbon dioxide (hypercapni ...
.
An epidural injection may be administered at any point of the spine, but most commonly the lumbar spine, below the end of the spinal cord. The specific administration site determines the specific nerve
A nerve is an enclosed, cable-like bundle of nerve fibers (called axons) in the peripheral nervous system.
A nerve transmits electrical impulses. It is the basic unit of the peripheral nervous system. A nerve provides a common pathway for the ...
s affected, and thus the area of the body from which pain will be blocked. Insertion of an epidural catheter consists of threading a needle between bones and ligaments to reach the epidural space without going so far as to puncture the ''dura mater''. Saline or air may be used to confirm placement in the epidural space. Alternatively, direct imaging of the injection area may be performed with a portable ultrasound or fluoroscopy
Fluoroscopy () is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a physician to see the internal structure and function ...
to confirm correct placement. Once placed, medication may be administered in one or more single doses, or may be continually infused over a period of time. When placed properly, an epidural catheter may remain inserted for several days, but is usually removed when the use of less invasive administration methods (such as taking medication by mouth) is a viable alternative.
Uses
upEpidural infusion pump with opioid ( sufentanil)_and_anesthetic_(bupivacaine)_in_a_locked_box.html" ;"title="bupivacaine.html" ;"title="sufentanil) and anesthetic (bupivacaine">sufentanil) and anesthetic (bupivacaine) in a locked box">bupivacaine.html" ;"title="sufentanil) and anesthetic (bupivacaine">sufentanil) and anesthetic (bupivacaine) in a locked boxPain relief during childbirth
Epidural injections are commonly used to provide pain relief (analgesia) during childbirth. This usually involves epidural injection of a local anesthetic and opioids, commonly called an "epidural". This is more effective than oral or Intravenous therapy, intra venal (IV) opioids and other common modalities of analgesia in childbirth. After an epidural is administered, a woman may not feel pain, but may still feel pressure. Epiduralclonidine
Clonidine, sold under the brand name Catapres among others, is an α2-adrenergic agonist medication used to treat high blood pressure, ADHD, drug withdrawal ( alcohol, opioids, or nicotine), menopausal flushing, diarrhea, spasticity, and c ...
is rarely used but has been extensively studied for management of analgesia during labor.
Epidural analgesia is considered a safer and more effective method of relieving pain in labor as compared to intravenous or oral analgesia. In a 2018 Cochrane review
Cochrane (previously known as the Cochrane Collaboration) is a British international charitable organisation formed to organise medical research findings to facilitate evidence-based choices about health interventions involving health professi ...
of studies which compared epidural analgesia with oral
The word oral may refer to:
Relating to the mouth
* Relating to the mouth, the first portion of the alimentary canal that primarily receives food and liquid
** Oral administration of medicines
** Oral examination (also known as an oral exam or or ...
opiates, some advantages of epidural analgesia included better efficacy, fewer instances of naloxone
Naloxone, sold under the brand names Narcan (4 mg) and Kloxxado (8 mg) among others, is a medication used to reverse or reduce the effects of opioids. It is commonly used to counter decreased breathing in opioid overdose. Effects begin withi ...
use in newborns, and decreased risk of maternal hyperventilation. Some disadvantages of epidurals included an increase in the number of Caesarian sections required due to fetal distress, a longer labor, increased need for oxytocin
Oxytocin (Oxt or OT) is a peptide hormone and neuropeptide normally produced in the hypothalamus and released by the posterior pituitary. It plays a role in social bonding, reproduction, childbirth, and the period after childbirth. Oxytoc ...
to stimulate uterine contractions, an increased risk of low blood pressure and muscle weakness, as well as fever. However, the review found no difference in overall Caesarean delivery rates, and no evidence of negative effects to the baby soon after birth. Furthermore, the occurrence of long-term backache was unchanged after epidural use. Complications of epidural analgesia are rare, but may include headaches, dizziness, difficulty breathing and seizures for the mother. The child may experience a slow heartbeat, decreased ability to regulate temperature, and potential exposure to the drugs administered to the mother.
There is no overall difference in outcomes based on the time the epidural is administered to the mother, specifically no change in the rate of caesarean section, birth which must be assisted by instruments, and duration of labor. There is also no change in the Apgar score
The Apgar score is a quick way for doctors to evaluate the health of all newborns at 1 and 5 minutes after birth and in response to resuscitation. It was originally developed in 1952 by an anesthesiologist at Columbia University, Virginia Apgar ...
of the newborn between early and late epidural administration. Epidurals other than low-dose ambulatory epidurals also impact the ability of the mother to move during labor. Movement such as walking or changing positions may help improve labor comfort and decrease the risk of complications.
Pain relief during other surgery
Epidural analgesia has been demonstrated to have several benefits after other surgeries, including decreasing the need for the use of oral or systemic opioids, and reducing the risk of postoperative respiratory problems, chest infections,blood transfusion
Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but mo ...
requirements, and myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which ma ...
s. Use of epidural analgesia after surgery in place of systemic analgesia is less likely to decrease intestinal motility Gastrointestinal physiology is the branch of human physiology that addresses the physical function of the gastrointestinal (GI) tract. The function of the GI tract is to process ingested food by mechanical and chemical means, extract nutrients and ...
which would occur with systemic opioid therapy through blockade of the sympathetic nervous system. Some surgeries that spinal analgesia may be used in include lower abdominal surgery, lower limb surgery, cardiac surgery, and perineal surgery.
Others
The injection of steroids into the epidural space is sometimes used to treat nerve root pain, radicular pain andinflammation
Inflammation (from la, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants, and is a protective response involving immune cells, blood vessels, and molec ...
caused by conditions such as spinal disc herniation, degenerative disc disease, and spinal stenosis. The risk of complications from steroid administration is low and complications are usually minor. The specific drug, dose, and frequency of administration impacts the risk for and severity of complications. Complications of epidural steroid administration are similar to the side effects of steroids administered in other manners, and can include higher than normal blood sugar, especially in patients with type 2 diabetes
Type 2 diabetes, formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urinatio ...
.
An epidural blood patch consists of a small amount of a person's own blood is injected into the epidural space. This is done as a method of sealing a hole or leak in the epidural. The injected blood clots at the site of the puncture, closes the leak, and modulates CSF pressure. This may be used to treat post-dural-puncture headache and leakage of cerebrospinal fluid
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
CSF is produced by specialised ependymal cells in the choroid plexus of the ventricles of the ...
due to dural puncture, which occurs in approximately 1.5% of epidural analgesia procedures.
Contraindications
The use of epidural analgesia and anesthetic is considered safe and effective in most situations. Epidural analgesia is contraindicated in people who have complications such as cellulitis near the injection site or severe coagulopathy. In some cases, it may be contraindicated in people with low platelets, increasedintracranial pressure
Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury ( mmHg) and at rest, is normally 7–15 mmHg for a supine adul ...
, or decreased cardiac output
In cardiac physiology, cardiac output (CO), also known as heart output and often denoted by the symbols Q, \dot Q, or \dot Q_ , edited by Catherine E. Williamson, Phillip Bennett is the volumetric flow rate of the heart's pumping output: th ...
. Due to the risk of disease progression, it is also potentially contraindicated in people with preexisting progressive neurologic disease. Some heart conditions such as stenosis
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
of the aortic or mitral valves are also a contraindication to the use of epidural administration, as is low blood pressure or hypovolemia
Hypovolemia, also known as volume depletion or volume contraction, is a state of abnormally low extracellular fluid in the body. This may be due to either a loss of both salt and water or a decrease in blood volume. Hypovolemia refers to the los ...
. An epidural is generally not used in people who are being administered anticoagulation therapy as it increases the risk of complications from the epidural.
Risks and complications
In addition to blocking nerves which carry pain signals, local anesthetics may block nerves which carry other signals, though sensory nerve fibers are more sensitive to the effects of the local anesthetics than motor nerve fibers. For this reason, adequate pain control can usually be attained without blocking the motor neurons, which would cause a loss of muscle control if it occurred. Depending on the drug and dose administered, the effects may last only a few minutes or up to several hours. As such, an epidural can provide pain control without as much of an effect on muscle strength. For example, a woman in labor who is being administered continuous analgesia via an epidural may not have impairment to her ability to move. Larger doses of medication are more likely to result in side effects. Very large doses of some medications can cause paralysis of the intercostal muscles andthoracic diaphragm
The thoracic diaphragm, or simply the diaphragm ( grc, διάφραγμα, diáphragma, partition), is a sheet of internal skeletal muscle in humans and other mammals that extends across the bottom of the thoracic cavity. The diaphragm is the m ...
responsible for breathing, which may lead to respiratory depression or arrest. It may also result in loss of sympathetic nerve input to the heart, which may cause a significant decrease in heart rate and blood pressure. Obese people, those who have given birth prior, those with a history of opiate use, or those with cervical dilation of more than 7 cm are at a higher risk of inadequate pain control.
If the dura is accidentally punctured during administration, it may cause cerebrospinal fluid to leak into the epidural space, causing a post-dural-puncture headache. This occurs in approximately 1 in 100 epidural procedures. Such a headache may be severe and last several days, or rarely weeks to months, and is caused by a reduction in CSF pressure. Mild post-dural-puncture headaches may be treated with caffeine and gabapentin, while severe headaches may be treated with an epidural blood patch, though most cases resolve spontaneously with time. Less common but more severe complications include subdural hematoma and cerebral venous thrombosis
Cerebral venous sinus thrombosis (CVST), cerebral venous and sinus thrombosis or cerebral venous thrombosis (CVT), is the presence of a blood clot in the dural venous sinuses (which drain blood from the brain), the cerebral veins, or both. Symp ...
. The epidural catheter may also rarely be inadvertently placed in the subarachnoid space, which occurs in less than 1 in 1000 procedures. If this occurs, cerebrospinal fluid can be freely aspirated from the catheter, and this is used to detect misplacement. When this occurs, the catheter is withdrawn and replaced elsewhere, though occasionally no fluid may be aspirated despite a dural puncture. If dural puncture is not recognized, large doses of anesthetic may be delivered directly into the cerebrospinal fluid. This may result in a high block, or, more rarely, a ''total spinal'', where anesthetic is delivered directly to the brainstem, causing unconsciousness and sometimes seizures
An epileptic seizure, informally known as a seizure, is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with lo ...
.
Epidural administrations can also cause bleeding issues, including "bloody tap", which occurs in approximately 1 in 30–50 people. This occurs when epidural veins are inadvertently punctured with the needle during the insertion. It is a common occurrence and is not usually considered a problem in people who have normal blood clotting. Permanent neurological problems from bloody tap are extremely rare, estimated at less than 0.07% of occurrences. However, people who have a coagulopathy
Coagulopathy (also called a bleeding disorder) is a condition in which the blood's ability to coagulate (form clots) is impaired. This condition can cause a tendency toward prolonged or excessive bleeding ( bleeding diathesis), which may occur s ...
may have a risk of epidural hematoma, and those with thrombocytopenia might bleed more than expected. A 2018 Cochrane review found no evidence regarding the effect of platelet transfusion
Platelet transfusion, also known as platelet concentrate, is used to prevent or treat bleeding in people with either a low platelet count or poor platelet function. Often this occurs in people receiving cancer chemotherapy. Preventive transfus ...
s prior to a lumbar puncture
Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is ...
or epidural anesthesia for participants that have thrombocytopenia
Thrombocytopenia is a condition characterized by abnormally low levels of platelets, also known as thrombocytes, in the blood. It is the most common coagulation disorder among intensive care patients and is seen in a fifth of medical patients a ...
. It is unclear whether major surgery-related bleeding within 24 hours and the surgery-related complications up to 7 days after the procedure are affected by epidural use.
Rare complications of epidural administration include formation of an epidural abscess (1 in 145,000) or epidural hematoma (1 in 168,000), neurological injury lasting longer than 1 year (1 in 240,000), paraplegia
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek ()
"half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neur ...
(1 in 250,000), and arachnoiditis, Rarely, an epidural may cause death (1 in 100,000).
Medication-specific
If bupivacaine, a medication commonly administered via epidural, is inadvertently administered into a vein, it can cause excitation, nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, or seizures as well as central nervous system depression, loss of consciousness, respiratory depression and apnea. Bupivacaine intended for epidural administration has been implicated in cardiac arrests resulting in death when accidentally administered into a vein instead of the epidural space. The administration of large doses of opioids into the epidural space may causeitching
Itch (also known as pruritus) is a sensation that causes the desire or reflex to scratch. Itch has resisted many attempts to be classified as any one type of sensory experience. Itch has many similarities to pain, and while both are unpleasan ...
and respiratory depression. The sensation of needing to urinate is often significantly diminished or completely absent after administration of epidural local anesthetics or opioids. Because of this, a urinary catheter is often placed for the duration of the epidural infusion.
In many women given epidural analgesia during labor oxytocin is also used to augment uterine contractions. In one study which examined the rate of breastfeeding two days following epidural anesthesia during childbirth, epidural analgesia used in combination with oxytocin resulted in lower maternal oxytocin and prolactin levels in response to breastfeeding on the second day following birth. This results in a decrease in the amount of milk produced.
Technique
Anatomy
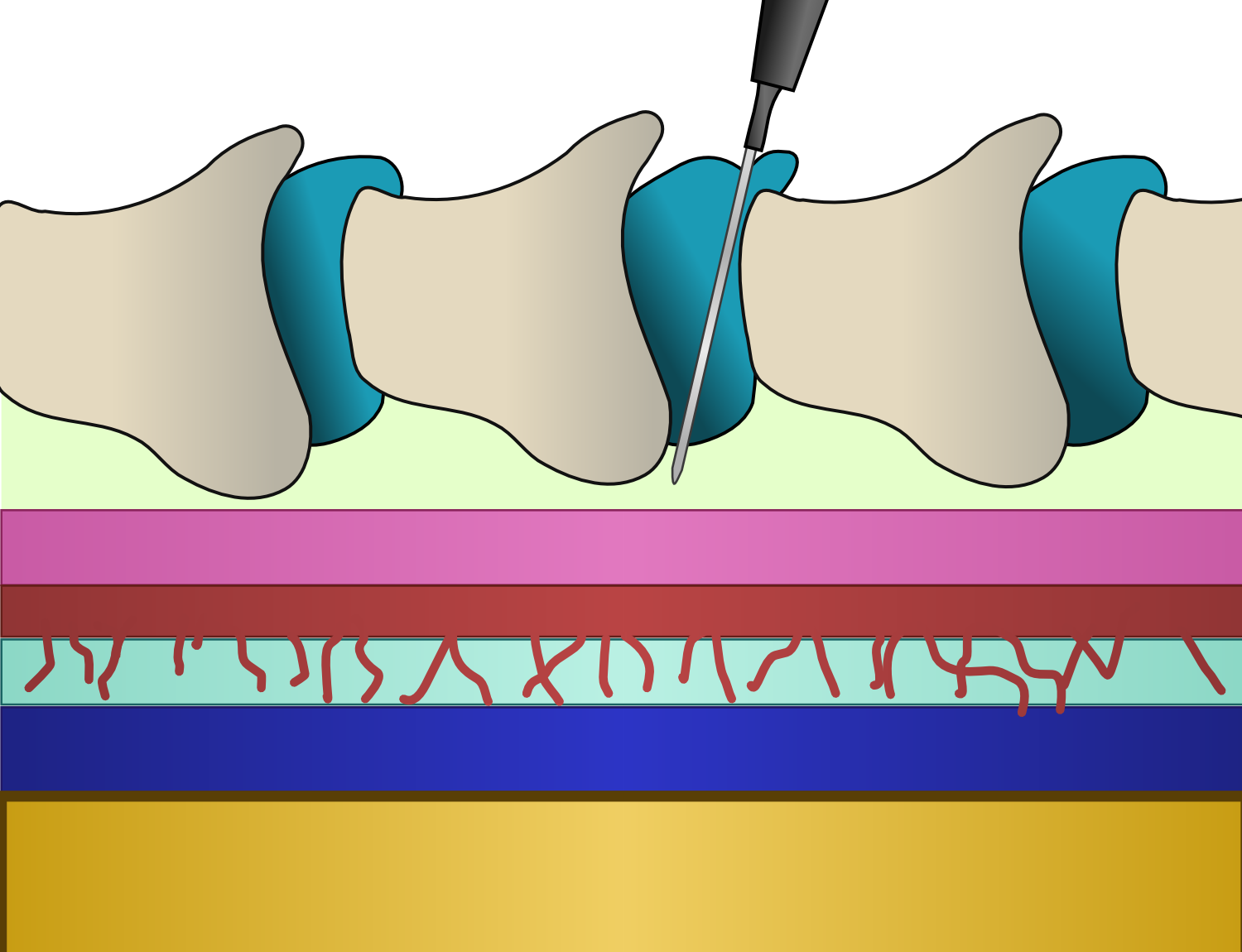
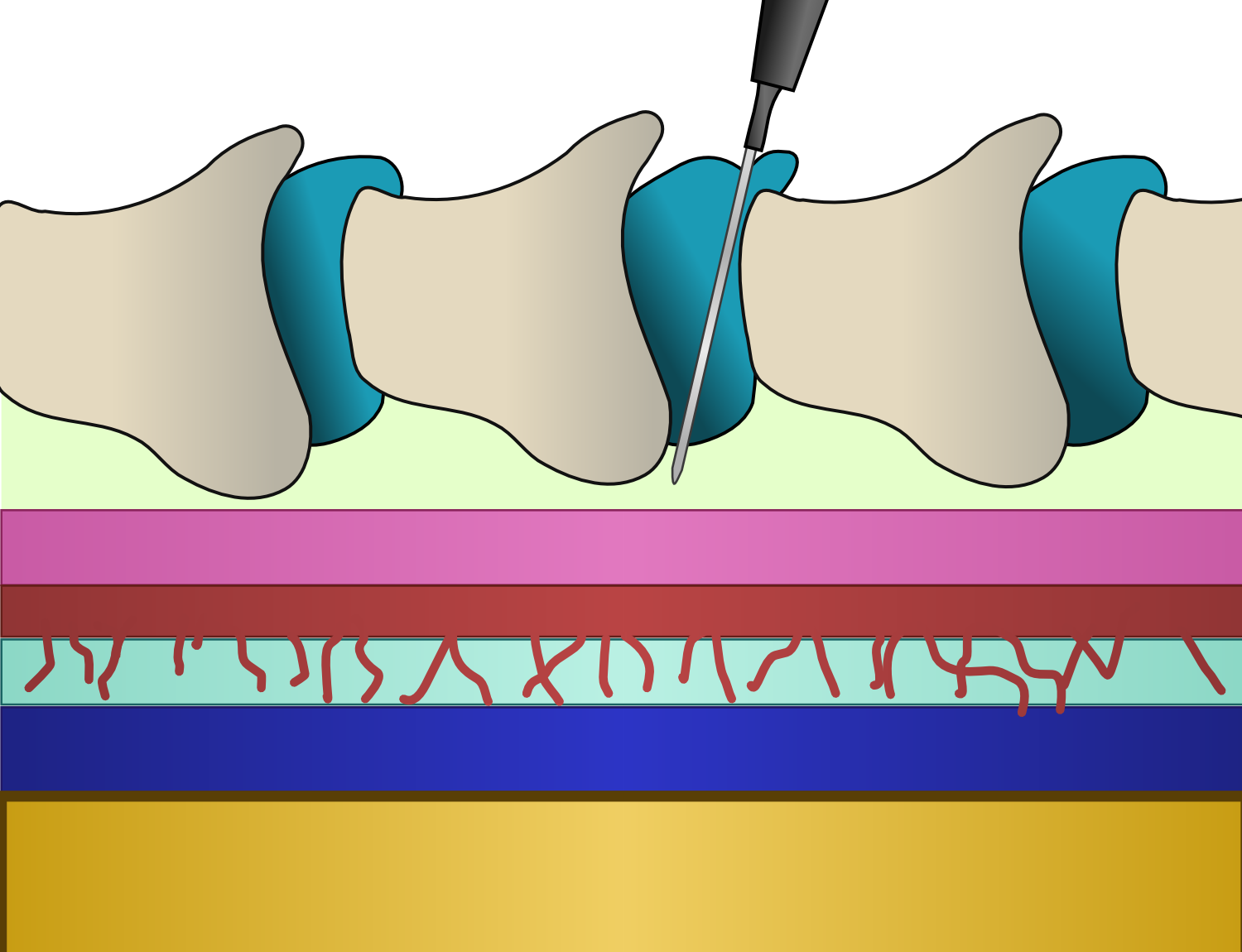 An epidural is injected into the epidural space, inside the bony spinal canal but just outside the dura. In contact with the inner surface of the dura is another membrane called the
An epidural is injected into the epidural space, inside the bony spinal canal but just outside the dura. In contact with the inner surface of the dura is another membrane called the arachnoid mater
The arachnoid mater (or simply arachnoid) is one of the three meninges, the protective membranes that cover the brain and spinal cord. It is so named because of its resemblance to a spider web. The arachnoid mater is a derivative of the neura ...
, which contains the cerebrospinal fluid. In adults, the spinal cord terminates around the level of the disc between L1 and L2, while in neonates it extends to L3 but can reach as low as L4. Below the spinal cord there is a bundle of nerves known as the cauda equina or "horse's tail". Hence, lumbar epidural injections carry a low risk of injuring the spinal cord. Insertion of an epidural needle involves threading a needle between the bones, through the ligaments and into the epidural space without puncturing the layer immediately below containing CSF under pressure.
Insertion
 Epidural administration is a procedure which requires the person performing the insertion to be technically proficient in order to avoid complications. Proficiency may be trained using bananas or other fruits as a model.
The person receiving the epidural may be seated, or lying on their side or stomach. The level of the spine at which the catheter is placed depends mainly on the site of intended operation – based on the location of the pain. The iliac crest is a commonly used anatomical landmark for lumbar epidural injections, as this level roughly corresponds with the fourth lumbar vertebra, which is usually well below the termination of the spinal cord. The
Epidural administration is a procedure which requires the person performing the insertion to be technically proficient in order to avoid complications. Proficiency may be trained using bananas or other fruits as a model.
The person receiving the epidural may be seated, or lying on their side or stomach. The level of the spine at which the catheter is placed depends mainly on the site of intended operation – based on the location of the pain. The iliac crest is a commonly used anatomical landmark for lumbar epidural injections, as this level roughly corresponds with the fourth lumbar vertebra, which is usually well below the termination of the spinal cord. The Tuohy needle
A Tuohy (/tOO-ee/) needle is a hollow hypodermic needle
A hypodermic needle (from Greek ὑπο- (''hypo-'' = under), and δέρμα (''derma'' = skin)), one of a category of medical tools which enter the skin, called sharps, is a very ...
, designed with a 90-degree curved tip and side hole to redirect the inserted catheter vertically along the axis of the spine, may be inserted in the midline, between the spinous process
The spinal column, a defining synapomorphy shared by nearly all vertebrates, Hagfish are believed to have secondarily lost their spinal column is a moderately flexible series of vertebrae (singular vertebra), each constituting a characteristic ...
es. When using a paramedian approach, the tip of the needle passes along a shelf of vertebral bone called the lamina until just before reaching the ligamentum flavum and the epidural space.
Along with a sudden loss of resistance to pressure on the plunger of the syringe, a slight clicking sensation may be felt by the operator as the tip of the needle breaches the ligamentum flavum and enters the epidural space. Saline or air may be used to identify placement in the epidural space. A systematic review from 2014 showed no difference in terms of safety or efficacy between the use of saline and air for this purpose. In addition to the loss of resistance technique, direct imaging of the placement may be used. This may be conducted with a portable ultrasound scanner or fluoroscopy
Fluoroscopy () is an imaging technique that uses X-rays to obtain real-time moving images of the interior of an object. In its primary application of medical imaging, a fluoroscope () allows a physician to see the internal structure and function ...
(moving X-ray pictures). After placement of the tip of the needle, a catheter or small tube is threaded through the needle into the epidural space. The needle is then withdrawn over the catheter. The catheter is generally inserted 4–6 cm into the epidural space, and is typically secured to the skin with adhesive tape, similar to an intravenous line.
Use and removal
If a short duration of action is desired, a single dose of medication called a bolus may be administered. Thereafter, this bolus may be repeated if necessary provided the catheter remains undisturbed. For a prolonged effect, a continuous infusion of medication may be used. There is some evidence that an automated intermittent bolus technique may provide better pain control than a continuous infusion technique even when the total doses administered are identical. Typically, the effects of the epidural block are noted below a specific level or portion of the body, determined by the site of injection. A higher injection may result in sparing of nerve function in the lowerspinal nerve
A spinal nerve is a mixed nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. In the human body there are 31 pairs of spinal nerves, one on each side of the vertebral column. These are grouped into the ...
s. For example, a thoracic epidural performed for upper abdominal surgery may not have any effect on the area surrounding the genitals or pelvic organs.
Combined spinal-epidural techniques
For some procedures where both the rapid onset of a spinal anesthetic and the post-operative analgesic effects of an epidural are desired, both techniques may be used in combination. This is called combined spinal and epidural anesthesia (CSE). The spinal anesthetic may be administered in one location, and the epidural at an adjacent location. Alternatively, after locating the epidural space with the Tuohy needle, a spinal needle may be inserted through the Tuohy needle into thesubarachnoid space
In anatomy, the meninges (, ''singular:'' meninx ( or ), ) are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in ...
. The spinal dose is then given, the spinal needle withdrawn, and the epidural catheter inserted as normal. This method, known as the "needle-through-needle" technique, may be associated with a slightly higher risk of placing the catheter into the subarachnoid space.
Recovery
Epidural analgesia is generally well tolerated, with recovery time quick after administration is complete and the epidural is removed. The epidural catheter is usually removed when it is possible to safely switch to oral administration of medications, though catheters can safely remain in place for several days with little risk of bacterial infection, particularly if the skin is prepared with achlorhexidine
Chlorhexidine (CHX) (commonly known by the salt forms chlorhexidine gluconate and chlorhexidine digluconate (CHG) or chlorhexidine acetate) is a disinfectant and antiseptic that is used for skin disinfection before surgery and to sterilize surgi ...
solution. Subcutaneously tunneled epidural catheters may be safely left in place for longer periods, with a low risk of infection or other complications. Regardless of the length of use, the effects of a medicine administered epidurally, including numbness if used for analgesia, usually wear off within a few hours of the epidural being stopped, with full recovery of normal function within 24 hours.
The use of epidural analgesia during a birth does not have any effect on whether a caesarean section must be performed during future births. Epidural analgesia during childbirth also generally has no negative effects on the long-term health of the mother or child. Use of epidural analgesia versus oral analgesia or no analgesia has no effect on the normal length of hospital stay after childbirth, the only difference being that care must be performed around the epidural insertion site to prevent infection. Following epidural analgesia used for gastrointestinal surgery, the time to recovery of normal gastrointestinal function is not significantly different from recovery time after intravenous analgesia. The use of epidural analgesia during cardiac surgeries may shorten the amount of time a person requires ventilator support following surgery, but it is unknown whether it shortens the overall post-surgery hospital stay overall.
History
 The first record of an epidural injection is from 1885, when American neurologist James Corning of Acorn Hall in Morristown, NJ used the technique to perform a
The first record of an epidural injection is from 1885, when American neurologist James Corning of Acorn Hall in Morristown, NJ used the technique to perform a neuraxial blockade Neuraxial anesthesia is local anaesthesia placed around the nerves of the central nervous system, such as spinal anaesthesia, caudal anaesthesia, epidural anaesthesia, and combined spinal and epidural anaesthesia. The technique is used in surgery, ...
. Corning inadvertently injected 111 mg of cocaine into the epidural space of a healthy male volunteer, although at the time he believed he was injecting it into the subarachnoid space. Following this, in 1901 Fernand Cathelin first reported intentionally blocking the lowest sacral and coccygeal nerves through the epidural space by injecting local anesthetic through the sacral hiatus. The loss of resistance technique was first described by Achile Dogliotti in 1933, following which Alberto Gutiérrez described the hanging drop technique. Both techniques are now used to identify when the needle has correctly been placed in the epidural space.
In 1921 Fidel Pagés, a military surgeon from Spain, developed the technique of "single-shot" lumbar epidural anesthesia, which was later popularized by Italian surgeon Achille Mario Dogliotti. Later, in 1931 Eugen Aburel described using a continuous epidural catheter for pain relief during childbirth. In 1941, Robert Hingson and Waldo Edwards recorded the use of continuous caudal anesthesia using an indwelling needle, following which they described the use of a flexible catheter for continuous caudal anesthesia in a woman in labor in 1942. In 1947, Manuel Curbelo described placement of a lumbar epidural catheter, and in 1979, Behar reported the first use of an epidural to administer narcotics.
Society and culture
Some people continue to be concerned that women who are administered epidural analgesia during labor are more likely to require a cesarean delivery, based on older observational studies. However, evidence has shown that the use of epidural analgesia during labor does not have any statistically significant effect on the necessity to perform a cesarean delivery. A 2018 Cochrane review found no increase in the rate of Caesarean delivery when epidural analgesia was employed. However, epidural analgesia does lengthen the second stage of labor by 15 to 30 minutes, which may increase the risk a delivery must be assisted by instruments. In the United States in 1998, it was reported that over half of childbirths involved the use of epidural analgesia, and by 2008 this had increased to 61% of births. In the United Kingdom, epidurals have been offered through theNational Health Service
The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom (UK). Since 1948, they have been funded out of general taxation. There are three systems which are referred to using the " ...
for all women during childbirth since 1980. By 1998, epidural analgesia was used in the UK for almost 25% of childbirths. In Japan, most childbirths take place in primary or secondary hospitals in which epidural analgesia is not offered.
In some developed countries, over 70% of childbirths involve epidural analgesia. Other studies have shown that minority women and immigrants are less likely to receive epidural analgesia during childbirth. Even in countries with universal healthcare coverage such as Canada, socioeconomic factors such as race, financial stability, and education influence the rate at which women receive epidural analgesia. One survey in 2014 found that over half of pregnant women in a Nigerian antenatal clinic (79.5%) did not know what epidural analgesia was or what it was used for, while 76.5% of them would utilize epidural analgesia if offered after it was explained to them.
References
Further reading
* Boqing Chen and Patrick M. Foye, UMDNJ: New Jersey Medical School, ''Epidural Steroid Injections: Non-surgical Treatment of Spine Pain'', eMedicine: Physical Medicine and Rehabilitation (PM&R), August 2005. Alsavailable online
* *
External links
{{Use mdy dates, date=September 2016 Childbirth Regional anesthesia Obstetrical procedures Dosage forms Spanish inventions