Cystocele on:
[Wikipedia]
[Google]
[Amazon]
A cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's
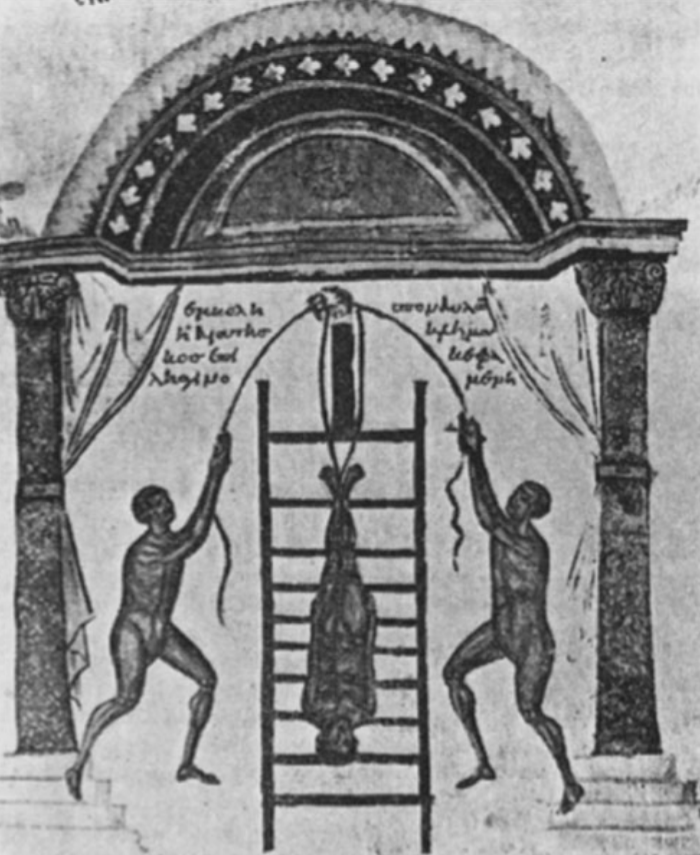 Notable is the mention of cystocele in many older cultures and locations. In 1500 B.C. Egyptians wrote about the "falling of the womb". In 400 B.C. a Greek physician documented his observations and treatments:
"After the patient had been tied to a ladder-like frame, she was tipped upward so that her head was toward the bottom of the frame. The frame was then moved upward and downward more or less rapidly for approximately 3–5 min. As the patient was in an inverted position, it was thought that the prolapsing organs of the genital tract would be returned to their normal position by the force of gravity and the shaking motion."
Notable is the mention of cystocele in many older cultures and locations. In 1500 B.C. Egyptians wrote about the "falling of the womb". In 400 B.C. a Greek physician documented his observations and treatments:
"After the patient had been tied to a ladder-like frame, she was tipped upward so that her head was toward the bottom of the frame. The frame was then moved upward and downward more or less rapidly for approximately 3–5 min. As the patient was in an inverted position, it was thought that the prolapsing organs of the genital tract would be returned to their normal position by the force of gravity and the shaking motion."
Using splinting to support and diminish pain while coughing
Craven and Hirnle's Fundamentals of Nursing: Human Health and Function, 6th edition
Cystocele, Pelvic Organ Prolapse
{{Diseases of the pelvis, genitals and breasts, state=colllapsed Noninflammatory disorders of female genital tract Vagina Wikipedia medicine articles ready to translate Women's health Urology Incontinence Gynecological surgery Reproductive system Oncology Urinary bladder disorders Urinary incontinence Urinary system Surgery
bladder
The urinary bladder, or simply bladder, is a hollow organ in humans and other vertebrates that stores urine from the kidneys before disposal by urination. In humans the bladder is a distensible organ that sits on the pelvic floor. Urine enters ...
bulges into her vagina
In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vestibule to the cervix. The outer vaginal opening is normally partly covered by a thin layer of mucosal tissue called the hymen ...
. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geri ...
, or frequent urination
Frequent urination, or urinary frequency (sometimes called pollakiuria), is the need to urinate more often than usual. Diuretics are medications that increase urinary frequency. Nocturia is the need of frequent urination at night. The most common c ...
. Complications may include recurrent urinary tract infection
A urinary tract infection (UTI) is an infection that affects part of the urinary tract. When it affects the lower urinary tract it is known as a bladder infection (cystitis) and when it affects the upper urinary tract it is known as a kidne ...
s and urinary retention
Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladd ...
. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life
Quality of life (QOL) is defined by the World Health Organization as "an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards ...
.
Causes include childbirth
Childbirth, also known as labour and delivery, is the ending of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million births glob ...
, constipation
Constipation is a bowel dysfunction that makes bowel movements infrequent or hard to pass. The stool is often hard and dry. Other symptoms may include abdominal pain, bloating, and feeling as if one has not completely passed the bowel movement ...
, chronic cough
Chronic cough is long-term coughing, sometimes defined as more than several weeks or months. The term can be used to describe the different causes related to coughing, the three main ones being upper airway cough syndrome, asthma and gastroesopha ...
, heavy lifting, hysterectomy, genetics
Genetics is the study of genes, genetic variation, and heredity in organisms.Hartl D, Jones E (2005) It is an important branch in biology because heredity is vital to organisms' evolution. Gregor Mendel, a Moravian Augustinian friar wor ...
, and being overweight. The underlying mechanism involves weakening of muscles
Skeletal muscles (commonly referred to as muscles) are organs of the vertebrate muscular system and typically are attached by tendons to bones of a skeleton. The muscle cells of skeletal muscles are much longer than in the other types of musc ...
and connective tissue between the bladder and vagina. Diagnosis is often based on symptoms and examination.
If the cystocele causes few symptoms, avoiding heavy lifting or straining may be all that is recommended. In those with more significant symptoms a vaginal pessary
A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage and to treat pelvic organ prolapse to maintain the locati ...
, pelvic muscle exercise
Kegel exercise, also known as pelvic-floor exercise, involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise can be performed many t ...
s, or surgery may be recommended. The type of surgery typically done is known as a colporrhaphy
Colporrhaphy (also vaginal wall repair, anterior and/or posterior colporrhaphy, anterior and/or posterior vaginal wall repair, or simply A/P repair or A&P repair) is a surgical procedure in humans that repairs a defect in the wall of the vagina. It ...
. The condition becomes more common with age. About a third of women over the age of 50 are affected to some degree.
Signs and symptoms
The symptoms of a cystocele may include: * a vaginal bulge * the feeling that something is falling out of the vagina * the sensation of pelvic heaviness or fullness * difficulty starting a urine stream * a feeling of incomplete urination * frequent or urgent urination * fecal incontinence * frequent urinary tract infections * back and pelvic pain * fatigue * painful sexual intercourse * bleeding A bladder that has dropped from its normal position and into the vagina can cause some forms of incontinence and incomplete emptying of the bladder.Complications
Complications may includeurinary retention
Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladd ...
, recurring urinary tract infections and incontinence. The anterior vaginal wall may actually protrude though the vaginal introitus (opening). This can interfere with sexual activity. Recurrent urinary tract infections are common for those who have urinary retention. In addition, though cystocele can be treated, some treatments may not alleviate troubling symptoms, and further treatment may need to be performed. Cystocele may affect the quality of life, women who have cystocele tend to avoid leaving their home and avoid social situations. The resulting incontinence puts women at risk of being placed in a nursing home or long-term care facility.
Cause
A cystocele occurs when the muscles, fascia,tendon
A tendon or sinew is a tough, high-tensile-strength band of dense fibrous connective tissue that connects muscle to bone. It is able to transmit the mechanical forces of muscle contraction to the skeletal system without sacrificing its ability ...
s and connective tissues between a woman's bladder and vagina weaken, or detach. The type of cystocele that can develop can be due to one, two or three vaginal wall attachment failures: the midline defect, the paravaginal defect, and the transverse defect. The midline defect is a cystocele caused by the overstretching of the vaginal wall; the paravaginal defect is the separation of the vaginal connective tissue at the arcus tendineus fascia pelvis; the transverse defect is when the pubocervical fascia becomes detached from the top (apex) of the vagina. There is some pelvic prolapse in 40–60% of women who have given birth. Muscle injuries have been identified in women with cystocele. These injuries are more likely to occur in women who have given birth than those who have not. These muscular injuries result in less support to the anterior vaginal wall.
Some women with connective tissue disorders are predisposed to developing anterior vaginal wall collapse. Up to one third of women with Marfan syndrome have a history of vaginal wall collapse. Ehlers-Danlos syndrome in women is associated with a rate of 3 out of 4.
Risk factors
Risk factors for developing a cystocele are: * an occupation involving or history of heavy lifting * pregnancy andchildbirth
Childbirth, also known as labour and delivery, is the ending of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million births glob ...
* chronic lung disease
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side ...
/smoking
* family history of cystocele
* exercising incorrectly
* ethnicity (risk is greater for Hispanic and whites)
* hypoestrogenism
Hypoestrogenism, or estrogen deficiency, refers to a lower than normal level of estrogen. It is an umbrella term used to describe estrogen deficiency in various conditions. Estrogen deficiency is also associated with an increased risk of cardiova ...
* pelvic floor trauma
* connective tissue disorders
* spina bifida
Spina bifida (Latin for 'split spine'; SB) is a birth defect in which there is incomplete closing of the spine and the membranes around the spinal cord during early development in pregnancy. There are three main types: spina bifida occulta, men ...
* hysterectomy
* cancer treatment of pelvic organs
* childbirth
Childbirth, also known as labour and delivery, is the ending of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million births glob ...
; correlates to the number of births
* forceps delivery
* age
* chronically high intra-abdominal pressures
** chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms include shortness of breath and a cough, which may or may not produce ...
** constipation
** obesity
Connective tissue disorders predispose women to developing cystocele and other pelvic organ prolapse. The tissues tensile strength of the vaginal wall decreases when the structure of the collagen fibers change and become weaker.
Diagnosis
There are two types of cystocele. The first is distension. This is thought to be due to the overstretching of the vaginal wall and is most often associated with aging, menopause and vaginal delivery. It can be observed when the rugae are less visible or even absent. The second type is displacement. Displacement is the detachment or abnormal elongation of supportive tissue. The initial assessment of cystocele can include apelvic exam
A pelvic examination is the physical examination of the external and internal female pelvic organs. It is frequently used in gynecology for the evaluation of symptoms affecting the female reproductive and urinary tract, such as pain, bleeding, d ...
to evaluate leakage of urine when the women is asked to bear down or give a strong cough (Valsalva maneuver
The Valsalva maneuver is performed by a forceful attempt of exhalation against a closed airway, usually done by closing one's mouth and pinching one's nose shut while expelling air out as if blowing up a balloon. Variations of the maneuver can ...
), and the anterior vaginal wall measured and evaluated for the appearance of a cystocele. If a woman has difficulty emptying her bladder, the clinician may measure the amount of urine left in the woman's bladder after she urinates called the postvoid residual. This is measured by ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies ...
. A voiding cystourethrogram
In urology, voiding cystourethrography (VCUG) is a frequently performed technique for visualizing a person's urethra and urinary bladder while the person urinates (voids). It is used in the diagnosis of vesicoureteral reflux (kidney reflux), am ...
is a test that involves taking x-rays of the bladder during urination. This x-ray
An X-ray, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 picometers to 10 nanometers, corresponding to frequencies in the range 30&nb ...
shows the shape of the bladder and lets the doctor see any problems that might block the normal flow of urine. A urine culture and sensitivity test will assess the presence of a urinary tract infection that may be related to urinary retention. Other tests may be needed to find or rule out problems in other parts of the urinary system. Differential diagnosis will be improved by identifying possible inflammation of the Skene's gland
In female human anatomy, Skene's glands or the Skene glands ( , also known as the lesser vestibular glands, paraurethral glands) are glands located around the lower end of the urethra. The glands are surrounded by tissue that swells with blood d ...
s and Bartholin gland
The Bartholin's glands (named after Caspar Bartholin the Younger; also called Bartholin glands or greater vestibular glands) are two pea sized compound alveolar glandsManual of Obstetrics. (3rd ed.). Elsevier. pp. 1-16. . located slightly poster ...
s.
Grading
A number of scales exist to grade the severity of a cystocele. The pelvic organ prolapse quantification (POP-Q) assessment, developed in 1996, quantifies the descent of the cystocele into the vagina. The POP-Q provides reliable description of the support of the anterior, posterior and apical vaginal wall. It uses objective and precise measurements to the reference point, thehymen
The hymen is a thin piece of mucosal tissue that surrounds or partially covers the external vaginal opening. It forms part of the vulva, or external genitalia, and is similar in structure to the vagina.
In children, a common appearance of the ...
. Cystocele and prolapse of the vagina from other causes is staged using POP-Q criteria can range from good support (no descent into the vagina) reported as a POP-Q stage 0 or I to a POP-Q score of IV which includes prolapse beyond the hymen. It also used to quantifies the movement of other structures into the vaginal lumen and their descent.
The Baden–Walker Halfway Scoring System is used as the second most used system and assigns the classifications as mild (grade 1) when the bladder droops only a short way into the vagina; (grade 2) cystocele, the bladder sinks far enough to reach the opening of the vagina; and (grade 3) when the bladder bulges out through the opening of the vagina.
Classifications
Cystocele can be further described as being apical, medial, lateral, or mediolateral. Apical cystocele is located upper third of the vagina. The structures involved are the endopelvic fascia and ligaments. Thecardinal ligament
The cardinal ligament (or Mackenrodt's ligament, lateral cervical ligament, or transverse cervical ligament) is a major ligament of the uterus. It is located at the base of the broad ligament of the uterus. There are a pair of cardinal ligaments ...
s and the uterosacral ligament
The uterosacral ligaments (or rectouterine ligaments) belong to the major ligaments of uterus.
Structure
The rectouterine folds contain a considerable amount of fibrous tissue and non-striped muscular fibers which are attached to the front of the ...
s suspend the upper vaginal-dome. The cystocele in this region of the vagina is thought to be due to a cardinal ligament defect.
Medial cystocele forms in the mid-vagina and is related to a defect in the suspension provided by to a sagittal suspension system defect in the uterosacral ligaments and pubocervical fascia. The pubocervical fascia may thin or tear and create the cystocele. An aid in diagnosis is the creation of a 'shiny' spot on the epithelium of the vagina. This defect can be assessed by MRI
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves ...
.
Lateral cystocele forms when both the pelviperineal muscle and its ligamentous–fascial develop a defect. The ligamentous– fascial creates a 'hammock-like' suspension and support for the lateral sides of the vagina. Defects in this lateral support system results in a lack of bladder support. Cystocele that develops laterally is associated with an anatomic imbalance between anterior vaginal wall and the arcus tendineus fasciae pelvis – the essential ligament structure.
Prevention
Cystocele may be mild enough not to result in symptoms that are troubling to a woman. In this case, steps to prevent it from worsening include: * smoking cessation * losing weight * pelvic floor strengthening * treatment of a chronic cough * maintaining healthy bowel habits ** eating high fiber foods ** avoiding constipation and strainingTreatment
Treatment options range from no treatment for a mild cystocele to surgery for a more extensive cystocele. If a cystocele is not bothersome, the clinician may only recommend avoiding heavy lifting or straining that could cause the cystocele to worsen. If symptoms are moderately bothersome, the doctor may recommend apessary
A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage and to treat pelvic organ prolapse to maintain the locati ...
, a device placed in the vagina to hold the bladder in place and to block protrusion. Treatment can consist of a combination of non-surgical and surgical management. Treatment choice is also related to age, desire to have children, severity of impairment, desire to continue sexual intercourse and other diseases that a woman may have.
Non-surgical
Cystocele is often treated by non-surgical means: * Pessary – This is a removable device inserted into the vagina to support the anterior vaginal wall. Pessaries come in many different shapes and sizes. There are sometimes complications with the use of a pessary. * Pelvic floor muscle therapy – Pelvic floor exercises to strengthen vaginal support can be of benefit. Specialized physical therapy can be prescribed to help strengthen the pelvic floor muscles. * Dietary changes – Ingesting high fiber foods will aid in promotingbowel movement
Defecation (or defaecation) follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus. The act has a variety of names ranging fro ...
s.
* Estrogen – intravaginal administration helps to prevent pelvic muscle atrophy
Surgery
The surgery to repair the anterior vaginal wall may be combined with other procedures that will repair the other points of pelvic organ support such as anterior-posterior repair and anterior colporrhaphy. Treatment of cystocele often accompanies the more invasive hysterectomy. Since the failure rate in cystocele repair remains high, additional surgery may be needed. Women who have surgery to repair a cystocele have a 17% of needing another operation within the next ten years. The surgical treatment of cystocele will depend on the cause of the defect and whether it occurs at the top (apex), middle, or lower part of the anterior vaginal wall. The type of surgery will also depend on the type of damage that exists between supporting structures and the vaginal wall. One of the most common surgical repairs iscolporrhaphy
Colporrhaphy (also vaginal wall repair, anterior and/or posterior colporrhaphy, anterior and/or posterior vaginal wall repair, or simply A/P repair or A&P repair) is a surgical procedure in humans that repairs a defect in the wall of the vagina. It ...
. This surgical procedure consists of making a longitudinal folding of the vaginal tissue, suturing it into place and creating a stronger point of resistance to the intruding bladder wall. Surgical mesh is sometimes used to strengthen the anterior vaginal wall. It has a 10–50% failure rate. In some cases a surgeon may choose to use surgical mesh to strengthen the repair.
During surgery, the repair of the vaginal wall consists of folding over and then suturing the existing tissue between the vagina and bladder to strengthen it. This tightens the layers of tissue to promote the replacement of the pelvic organs into their normal place. The surgery also provides more support for the bladder. This surgery is done by a surgeon specializing in gynecology and is performed in a hospital. Anesthesia varies according to the needs of each woman. Recovery may take four to six weeks. Other surgical treatment may be performed to treat cystocele. Support for the vaginal wall is accomplished with the paravaginal defect repair. This is a surgery, usually laproscopic, that is done to the ligaments and fascia through the abdomen. The lateral ligaments and supportive structures are repaired, sometimes shortened to provide additional support to the vaginal wall.
Sacrocolpopexy is a procedure that stabilizes the vaginal vault (the uppermost portion of the vagina) and is often chosen as the treatment for cystocele, especially if previous surgeries were not successful. The procedure consists of attaching the vaginal vault to the sacrum. It has a success rate of 90%. Some women choose not to have surgery to close the vagina. This surgery, called colpocleisis
Colpocleisis is a procedure involving closure of the vagina.
It is used to treat vaginal prolapse.
In older women who are no longer sexually active a simple procedure for reducing prolapse is a partial colpocleisis. The procedure was described by ...
, treats cystocele by closing the vaginal opening. This can be an option for women who no longer want to have vaginal intercourse.
If an enterocele
An enterocele is a protrusion of the small intestines and peritoneum into the vaginal canal.
It may be treated transvaginally or by laparoscopy.
An enterocele may also obstruct the rectum, leading to symptoms of obstructed defecation. Enteroceles ...
/sigmoidocele
Sigmoidocele (also known as Pouch of Douglas descent) refers to a condition where the sigmoid colon descends (prolapses) into the lower pelvic cavity. This can obstruct the rectum and cause symptoms of obstructed defecation.
Pathophysiology
Th ...
, or prolapse of the rectum/colon, is also present, the surgical treatment will take this concurrent condition into account while planning and performing the repairs. Estrogen that is administered vaginally before surgical repair can strengthen the vaginal tissue providing a more successful outcome when mesh or sutures are used for the repair. Vaginal thickness increases after estrogen therapy. Another review on the surgical management of cystocele describes a more successful treatment that more strongly attaches the ligaments and fascia to the vagina to lift and stabilize it.
Post surgical complications can develop. The complications following surgical treatment of cystocele are:
* side effects or reactions to anesthesia
* bleeding
* infection
* painful intercourse
* Urinary incontinence
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geri ...
* constipation
* bladder injuries
* urethral injuries
* urinary tract infection.
* vaginal erosion due to mesh
After surgery, a woman is instructed to restrict her activities and monitor herself for signs of infection such as an elevated temperature, discharge with a foul odor and consistent pain. Clinicians may recommend that sneezing, coughing, and constipation are to be avoided. Splinting the abdomen while coughing provides support to an incised area and decreases pain on coughing. This is accomplished by applying gentle pressure to the surgical site for bracing during a cough.
Recurrent surgery on the pelvic organs may not be due to a failure of the surgery to correct the cystocele. Subsequent surgeries can be directly or indirectly relating to the primary surgery. Prolapse can occur at a different site in the vagina. Further surgery after the initial repair can be to treat complications of mesh displacement, pain, or bleeding. Further surgery may be needed to treat incontinence.
One goal of surgical treatment is to restore the vagina and other pelvic organs to their anatomically normal positions. This may not be the outcome that is most important to the woman being treated who may only want relief of symptoms and an improvement in her quality of life. The International Urogynecological Association (IUGA) has recommended that the data collected regarding the success of cystocele and pelvic organ repairs include the presence or absence of symptoms, satisfaction and Quality of Life. Other measures of a successful outcome should include perioperative data, such as operative time and hospital stay. Standardized Healthcare Quality of Life should be part of the measure of a successful resolution of cystocele. Data regarding short- and long-term complications is included in the recommendations of the IUGA to better assess the risk–benefit ratio of each procedure. Current investigations into the superiority of using biological grafting versus native tissue or surgical mesh indicates that using grafts provides better results.
Epidemiology
A large study found a rate of 29% over the lifetime of a woman. Other studies indicate a recurrence rate as low as 3%. In the US, greater than 200,000 surgeries are performed each year for pelvic organ prolapse and 81% of these are to correct cystocele. Cystocele occurs most frequently compared to the prolapse of other pelvic organs and structure. Cystocele is found to be three times as common as vaginal vault prolapse and twice as often as posterior vaginal wall defects. The incidence of cystocele is around 9 per 100 women-years. The highest incidence of symptoms occurs between ages of 70 and 79 years. Based on population growth statistics, the number of women with prolapse will increase by a minimum of 46% by the year 2050 in the US. Surgery to correct prolapse after hysterectomy is 3.6 per 1,000 women-years.History
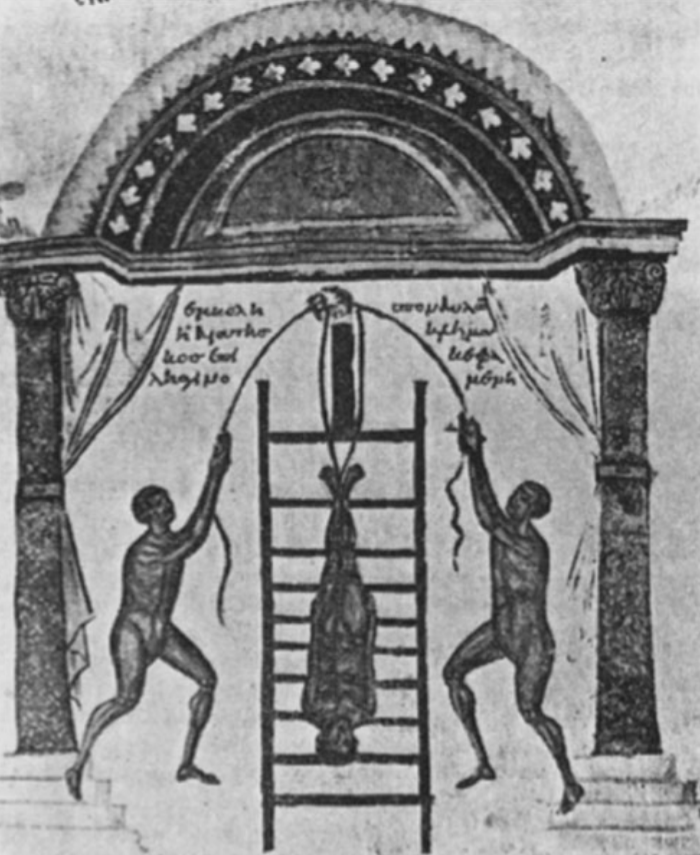 Notable is the mention of cystocele in many older cultures and locations. In 1500 B.C. Egyptians wrote about the "falling of the womb". In 400 B.C. a Greek physician documented his observations and treatments:
"After the patient had been tied to a ladder-like frame, she was tipped upward so that her head was toward the bottom of the frame. The frame was then moved upward and downward more or less rapidly for approximately 3–5 min. As the patient was in an inverted position, it was thought that the prolapsing organs of the genital tract would be returned to their normal position by the force of gravity and the shaking motion."
Notable is the mention of cystocele in many older cultures and locations. In 1500 B.C. Egyptians wrote about the "falling of the womb". In 400 B.C. a Greek physician documented his observations and treatments:
"After the patient had been tied to a ladder-like frame, she was tipped upward so that her head was toward the bottom of the frame. The frame was then moved upward and downward more or less rapidly for approximately 3–5 min. As the patient was in an inverted position, it was thought that the prolapsing organs of the genital tract would be returned to their normal position by the force of gravity and the shaking motion."
Hippocrates
Hippocrates of Kos (; grc-gre, Ἱπποκράτης ὁ Κῷος, Hippokrátēs ho Kôios; ), also known as Hippocrates II, was a Greek physician of the classical period who is considered one of the most outstanding figures in the history o ...
had his own theories regarding the cause of prolapse. He thought that recent childbirth, wet feet, 'sexual excesses', exertion, and fatigue may have contributed to the condition. Polybus, Hippocrates's son-in-law, wrote: "a prolapsed uterus was treated by using local astringent lotions, a natural sponge packed into the vagina, or placement of half a pomegranate in the vagina." In 350 A.D., another practitioner named Soranus described his treatments which stated that the pomegranate should be dipped into vinegar before insertion. Success could be enhanced if the woman was on bed rest and reduced intake of fluid and food. If the treatment was still not successful, the woman's legs were tied together for three days.
In 1521, Berengario da Carpi
Jacopo Berengario da Carpi (also known as Jacobus Berengarius Carpensis, Jacopo Barigazzi, Giacomo Berengario da Carpi or simply Carpus; c. 1460 – c. 1530) was an Italian physician. His book "''Isagoge breves''" published in 1522 made him the mo ...
performed the first surgical treatment for prolapse. This was to tie a rope around the prolapse, tighten it for two days until it was no longer viable and cut it off. Wine, aloe, and honey were then applied to the stump.
In the 1700s, a Swiss gynecologist, Peyer, published a description of a cystocele. He was able to describe and document both cystocele and uterine prolapse. In 1730, Halder associated cystocele with childbirth. During this same time, efforts began to standardize the terminology that is still familiar today. In the 1800s, the surgical advancements of anesthesia, suturing, suturing materials and acceptance of Joseph Lister's theories of antisepsis
An antiseptic (from Greek ἀντί ''anti'', "against" and σηπτικός ''sēptikos'', "putrefactive") is an antimicrobial substance or compound that is applied to living tissue/skin to reduce the possibility of infection, sepsis, or putr ...
improved outcomes for women with cystocele. The first surgical techniques were practiced on female cadavers. In 1823, Geradin proposed that an incision and resection may provide treatment. In 1830, the first dissection of the vagina was performed by Dieffenbach on a living woman. In 1834, Mendé proposed that dissecting and repair of the edges of the tissues could be done. In 1859, Huguier proposed the amputation of the cervix was going to solve the problem for elongation.
In 1866, a method of correcting a cystocele was proposed that resembled current procedures. Sim subsequently developed another procedure that did not require the full-thickness dissection of the vaginal wall. In 1888, another method of treating anterior vaginal wall Manchester combined an anterior vaginal wall repair with an amputation of the cervix and a perineorrhaphy. In 1909, White noted the high rate of recurrence of cystocele repair. At this time it was proposed that reattaching the vagina to support structures was more successful and resulted in less recurrence. This same proposal was proposed again in 1976 but further studies indicated that the recurrence rate was not better.
In 1888, treatments were tried that entered the abdomen to make reattachments. Some did not agree with this and suggested an approach through the inguinal canal
The inguinal canals are the two passages in the anterior abdominal wall of humans and animals which in males convey the spermatic cords and in females the round ligament of the uterus. The inguinal canals are larger and more prominent in males. ...
. In 1898, further abdominal approaches were proposed. No further advances have been noted until 1961 when reattachment of the anterior vaginal wall to Cooper's ligament began to be used. Unfortunately, posterior vaginal wall prolapse occurred in some patients even though the anterior repair was successful.
In 1955, using mesh to support pelvic structures came into use. In 1970, tissue from pigs began to be used to strengthen the anterior vaginal wall in surgery. Beginning in 1976, improvement in suturing began along with the surgical removal of the vagina being used to treat prolapse of the bladder. In 1991, assumptions about the detailed anatomy of the pelvic support structures began to be questioned regarding the existence of some pelvic structures and the non-existence of others. More recently, the use of stem cells, robot-assisted laparoscopic surgery are being used to treat cystocele.
See also
* Hysterectomy *Fecal incontinence
Fecal incontinence (FI), or in some forms encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referre ...
* Sigmoidocele
Sigmoidocele (also known as Pouch of Douglas descent) refers to a condition where the sigmoid colon descends (prolapses) into the lower pelvic cavity. This can obstruct the rectum and cause symptoms of obstructed defecation.
Pathophysiology
Th ...
* Urethropexy
A urethropexy is a surgical procedure where support is provided to the urethra.
One form is the " Burch urethropexy".
It is sometimes performed in the treatment of incontinence
Incontinence or Incontinent may refer to:
*Fecal incontinence, the ...
References
Further reading
Using splinting to support and diminish pain while coughing
Craven and Hirnle's Fundamentals of Nursing: Human Health and Function, 6th edition
External links
Cystocele, Pelvic Organ Prolapse
{{Diseases of the pelvis, genitals and breasts, state=colllapsed Noninflammatory disorders of female genital tract Vagina Wikipedia medicine articles ready to translate Women's health Urology Incontinence Gynecological surgery Reproductive system Oncology Urinary bladder disorders Urinary incontinence Urinary system Surgery