Compounding on:
[Wikipedia]
[Google]
[Amazon]
 In the field of
In the field of
U.S. Concern Over Compounders Predates Outbreak of Meningitis
New York Times. In 2002, the
Pharmacies Fought Controls; Industry at the Focus of Meningitis Outbreak Beat Back More Federal Oversight
Wall Street Journal In August 2013 further reports tied to the
Scant Oversight of Drug Maker in Fatal Meningitis Outbreak
New York Times. An FDA spokesperson stated, "The methods of these companies seem far more consistent with those of drug manufacturers than with those of retail pharmacies. Some firms make large amounts of compounded drugs that are copies or near copies of FDA-approved, commercially available drugs. Other firms sell to physicians and patients with whom they have only a remote professional relationship." The head of the FDA has recently requested the following authority from Congress: Various ideas have been proposed to expand federal US regulation in this area, including laws making it easier to identify misuse or misnomered-use and/or stricter enforcement of the longstanding distinction between ''compounding'' versus ''manufacturing''. Some US states have also taken initiatives to strengthen oversight of compounding pharmacies. A major source of opposition to new Food and Drug Administration regulation on compounding is makers of
America's Shadow Pharmacies
Businessweek. Retrieved on 2013-05-13.
International Academy of Compounding PharmacistsInternational Journal of Pharmaceutical CompoundingDrug Compounding: FDA Authority and Possible Issues for Congress
from the
 In the field of
In the field of pharmacy
Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medication, medicines. It is a miscellaneous science as it ...
, compounding (performed in compounding pharmacies) is preparation of custom medications to fit unique needs of patients that cannot be met with mass-produced formulations. This may be done, for example, to provide medication in a form easier for a given patient to ingest (e.g., liquid vs. tablet), or to avoid a non-active ingredient a patient is allergic to, or to provide an exact dose that isn't otherwise available. This kind of patient-specific compounding, according to a prescriber's specifications, is referred to as "traditional" compounding. The nature of patient need for such customization can range from absolute necessity (e.g. avoiding allergy) to individual optimality (e.g. ideal dose level) to even preference (e.g. flavor or texture).
Hospital pharmacies typically engage in compounding medications for intravenous
Intravenous therapy (abbreviated as IV therapy) is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutr ...
administration, whereas outpatient or community pharmacies typically engage in compounding medications for oral
The word oral may refer to:
Relating to the mouth
* Relating to the mouth, the first portion of the alimentary canal that primarily receives food and liquid
**Oral administration of medicines
** Oral examination (also known as an oral exam or ora ...
or topical administration. Due to the rising cost of compounding and drug shortages, some hospitals outsource
Outsourcing is a business practice in which company, companies use external providers to carry out business processes that would otherwise be handled internally. Outsourcing sometimes involves transferring employees and assets from one firm to ...
their compounding needs to large-scale compounding pharmacies, particularly of sterile-injectable medications.
Compounding preparations of a given formulation in advance batches, as opposed to preparation for a specific patient on demand, is known as "non-traditional" compounding and is akin to small-scale manufacturing. Jurisdictions have varying regulations that apply to drug manufacturer
The pharmaceutical industry is a Medicine, medical industry that discovers, develops, produces, and markets pharmaceutical goods such as medications and medical devices. Medications are then administered to (or Self-medicate, self-administered b ...
s and pharmacies that do advance bulk compounding.
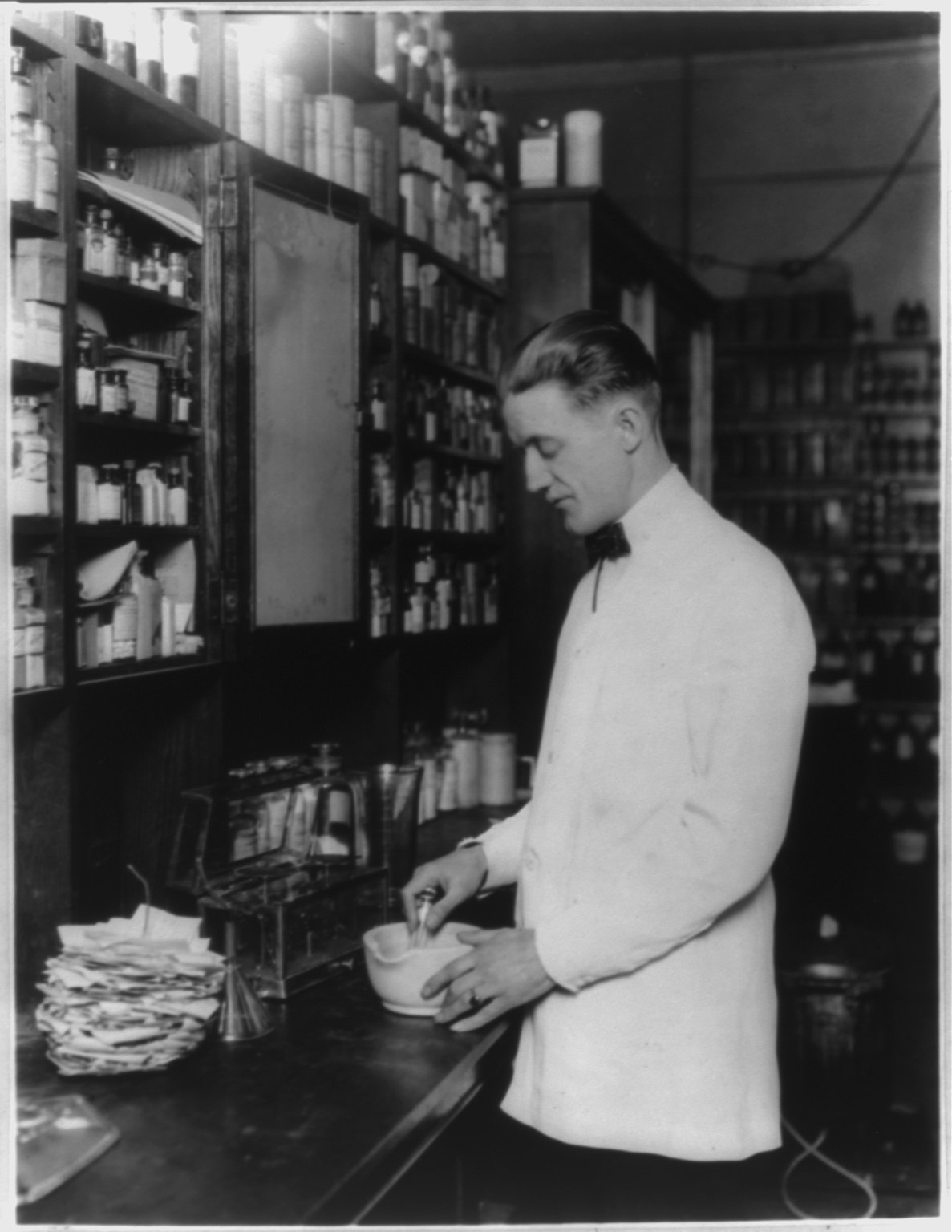
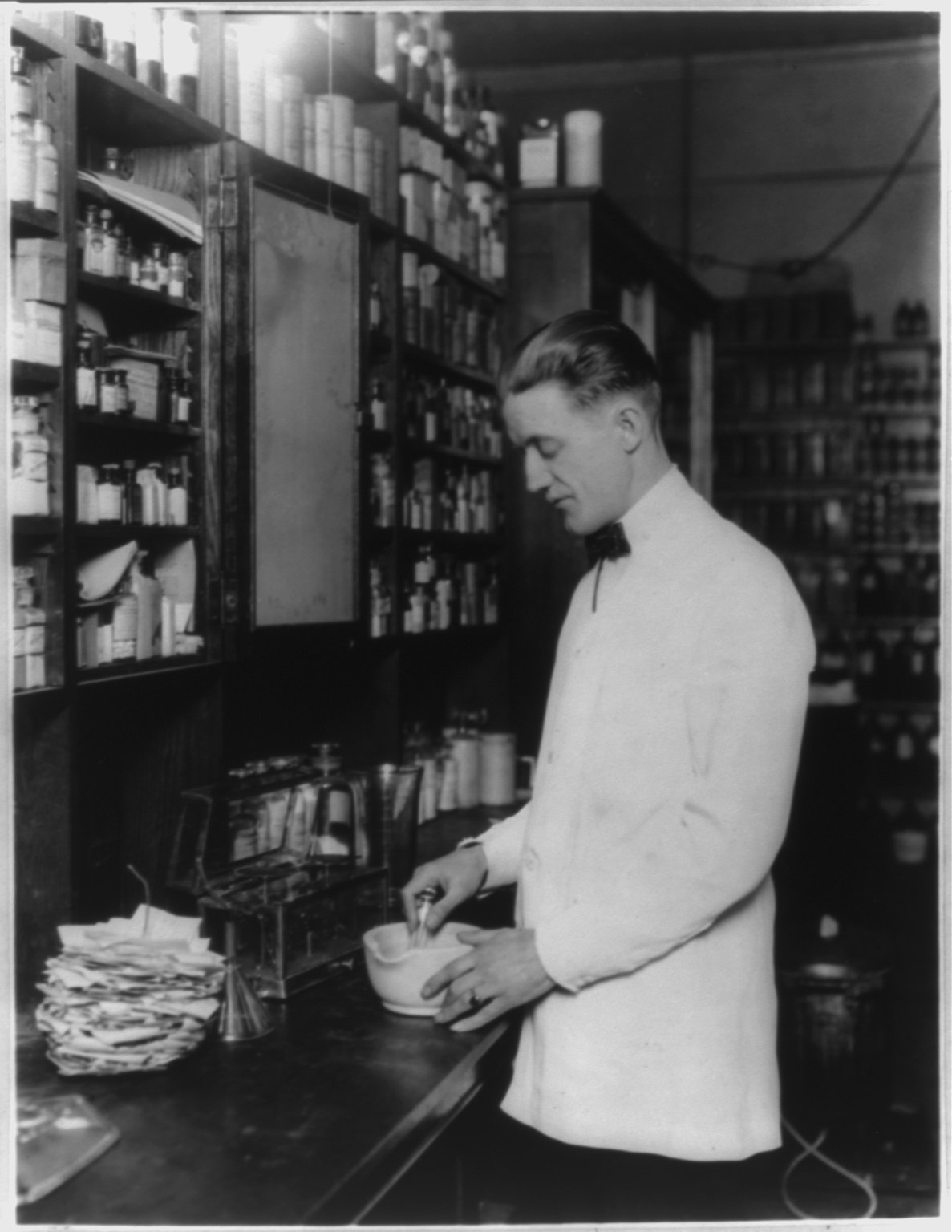
History
The earliestchemist
A chemist (from Greek ''chēm(ía)'' alchemy; replacing ''chymist'' from Medieval Latin ''alchemist'') is a graduated scientist trained in the study of chemistry, or an officially enrolled student in the field. Chemists study the composition of ...
s were familiar with various natural substances and their uses. They compounded a variety of preparations such as medications, dyes, incense, perfumes, ceremonial compounds, preservatives and cosmetics. In the medieval Islamic world in particular, Muslim pharmacists and chemists developed advanced methods of compounding drugs. The first drugstores were opened by Muslim pharmacists in Baghdad
Baghdad ( or ; , ) is the capital and List of largest cities of Iraq, largest city of Iraq, located along the Tigris in the central part of the country. With a population exceeding 7 million, it ranks among the List of largest cities in the A ...
in 754.Information taken from the abstract of The modern age of pharmacy compounding began in the 19th century with the isolation of various compounds from coal tar
Coal tar is a thick dark liquid which is a by-product of the production of coke and coal gas from coal. It is a type of creosote. It has both medical and industrial uses. Medicinally it is a topical medication applied to skin to treat psoria ...
for the purpose of producing synthetic dyes. From this came the earliest antibacterial
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention ...
sulfa drugs, phenol
Phenol (also known as carbolic acid, phenolic acid, or benzenol) is an aromatic organic compound with the molecular formula . It is a white crystalline solid that is volatile and can catch fire.
The molecule consists of a phenyl group () ...
ic compounds made famous by Joseph Lister, and plastic
Plastics are a wide range of synthetic polymers, synthetic or Semisynthesis, semisynthetic materials composed primarily of Polymer, polymers. Their defining characteristic, Plasticity (physics), plasticity, allows them to be Injection moulding ...
s.
During the 1800s, pharmacists specialized in the raising, preparation and compounding of crude drugs. Crude drugs, like opium
Opium (also known as poppy tears, or Lachryma papaveris) is the dried latex obtained from the seed Capsule (fruit), capsules of the opium poppy ''Papaver somniferum''. Approximately 12 percent of opium is made up of the analgesic alkaloid mor ...
, are from natural sources and usually contain several chemical compounds
A chemical compound is a chemical substance composed of many identical molecules (or molecular entities) containing atoms from more than one chemical element held together by chemical bonds. A molecule consisting of atoms of only one element ...
. The pharmacist extracted these drugs using solvents such as water
Water is an inorganic compound with the chemical formula . It is a transparent, tasteless, odorless, and Color of water, nearly colorless chemical substance. It is the main constituent of Earth's hydrosphere and the fluids of all known liv ...
or alcohol
Alcohol may refer to:
Common uses
* Alcohol (chemistry), a class of compounds
* Ethanol, one of several alcohols, commonly known as alcohol in everyday life
** Alcohol (drug), intoxicant found in alcoholic beverages
** Alcoholic beverage, an alco ...
to form extract
An extract (essence) is a substance made by extracting a part of a raw material, often by using a solvent such as ethanol, oil or water. Extracts may be sold as tinctures or absolutes or dried and powdered.
The aromatic principles of ma ...
s, concoctions and decoctions. They eventually began isolating and identifying the active ingredient
An active ingredient is any ingredient that provides biologically active or other direct effect in the diagnosis, cure, mitigation, treatment, or prevention of disease or to affect the structure or any function of the body of humans or animals.
...
s in these drug concoctions. Using fractionation
Fractionation is a separation process in which a certain quantity of a mixture (of gasses, solids, liquids, enzymes, or isotopes, or a suspension) is divided during a phase transition, into a number of smaller quantities (fractions) in which t ...
or recrystallization, they separated an active ingredient from the crude preparation, and compounded a medication using this active ingredient.
With the isolation of medications from the raw material
A raw material, also known as a feedstock, unprocessed material, or primary commodity, is a basic material that is used to produce goods, finished goods, energy, or intermediate materials/Intermediate goods that are feedstock for future finished ...
s or crude drugs came the birth of the modern pharmaceutical company. Pharmacists were trained to compound the preparations made by the drug companies, but they could not do it efficiently on a small scale. So economies of scale
In microeconomics, economies of scale are the cost advantages that enterprises obtain due to their scale of operation, and are typically measured by the amount of Productivity, output produced per unit of cost (production cost). A decrease in ...
, not lack of skill or knowledge, produced the modern pharmaceutical industry
The pharmaceutical industry is a medical industry that discovers, develops, produces, and markets pharmaceutical goods such as medications and medical devices. Medications are then administered to (or self-administered by) patients for curing ...
. With the turn of the 20th century came greater government regulation
Regulation is the management of complex systems according to a set of rules and trends. In systems theory, these types of rules exist in various fields of biology and society, but the term has slightly different meanings according to context. Fo ...
of the practice of medicine. These new regulations forced the drug companies to prove that any new medication they brought to market was safe. With the discovery of penicillin
Penicillins (P, PCN or PEN) are a group of beta-lactam antibiotic, β-lactam antibiotics originally obtained from ''Penicillium'' Mold (fungus), moulds, principally ''Penicillium chrysogenum, P. chrysogenum'' and ''Penicillium rubens, P. ru ...
, modern marketing techniques and brand
A brand is a name, term, design, symbol or any other feature that distinguishes one seller's goods or service from those of other sellers. Brands are used in business, marketing, and advertising for recognition and, importantly, to create and ...
promotion, the drug manufacturing industry came of age. Pharmacists continued to compound most prescriptions until the early 1950s when the majority of dispensed drugs came directly from the large pharmaceutical companies.
Roles
A physician may choose to prescribe a compounded medication for a patient with an unusual health need that cannot be met with commercially manufactured products. The physician may choose to prescribe a compounded medication for reasons such as *Patients requiring an individualized compounded formulation to be developed by the pharmacist *Patients who cannot take commercially prepared prescriptions of a drug *Patients requiring limited dosage strengths, such as a very small dose for infants *Patients requiring a different formulation, such as turning apill
Pill or The Pill may refer to:
Drugs
* Pill (pharmacy), referring to anything small for a specific dose of medicine
* "The Pill", a general nickname for the combined oral contraceptive pill
Film and television
* ''The Pill'' (film), a 2011 fil ...
into a liquid or transdermal gel for people who cannot swallow pills due to disability
*Patients requiring an allergen-free medication, such as one without gluten
Gluten is a structural protein naturally found in certain Cereal, cereal grains. The term ''gluten'' usually refers to the elastic network of a wheat grain's proteins, gliadin and glutenin primarily, that forms readily with the addition of water ...
or colored dyes
*Patients who absorb or excrete medications abnormally
*Patients who need drugs that have been discontinued by pharmaceutical manufacturers because of low profitability
*Patients facing a supply shortage of their normal drug
*Children who want flavored additives in liquid drugs, usually so that the medication tastes like candy or fruit
*Veterinary medicine, for a change in dose, change to a more easily administered form (such as from a pill to a liquid or transdermal gel), or to add a flavor more palatable to the animal. In the United States, compounded veterinary medicine must meet the standards set forth in the Animal Medicinal Drug Use Clarification Act (AMDUCA)
* Many types of bioidentical hormone replacement therapy
*Patients who require multiple medications combined in various doses
IV compounding in hospitals
In hospitals, pharmacists and pharmacy technicians often make compounded sterile preparations (CSPs) using manual methods. The error rate for manually compounded sterile IV products is high. The Institute for Safe Medication Practices (ISMP) has expressed concern with manual methods, particularly the error-prone nature of the syringe pull-back method of verifying sterile preparations. To increase accuracy, some U.S. hospitals have adopted IV workflow management systems and robotic compounding systems. These technologies use barcode scanning to identify each ingredient and gravimetric weight measurement to confirm the proper dose amount. The workflow management systems incorporate software to guide pharmacy technicians through the process of preparing IV medications. The robotic systems prepare IV syringes and bags in an ISO Class 5 environment, and support sterility and dose accuracy by removing human error and contamination from the process.Regulation in Australia
In Australia the Pharmacy Board of Australia is responsible for registration of pharmacists and professional practice including compounding. Although almost all pharmacies are able to prepare at least simple compounded medicines, some pharmacy staff undertake further training and education to be able to prepare more complex products. Although pharmacists who have undertaken further training to do complex compounding are not yet easily identified, the Board has been working to put a credentialing system in place. In 2011 the Pharmacy Board convened a Compounding Working Party to advise on revised compounding standards. Draft compounding guidelines for comment were released in April 2014. Pharmacists must comply with current guidelines or may be sanctioned by the Board. Both sterile and non-sterile compounding are legal provided the compounding is done for therapeutic use in a particular patient, and the compounded product is supplied on or from the compounding pharmacy. There are additional requirements for sterile compounding. Not only must a laminar flow cabinet aminar flow hoodbe used, but the environment in which the hood is located must be strictly controlled for microbial and particulate contamination and all procedures, equipment and personnel must be validated to ensure the safe preparation of sterile products. In non-sterile compounding, a powder containment hood is required when any hazardous material (e.g. hormones) are prepared or when there is a risk of cross-contamination of the compounded product. Pharmacists preparing compounded products must comply with these requirements and others published in the Australian Pharmaceutical Formulary & Handbook.Regulation in the United States
In theUnited States
The United States of America (USA), also known as the United States (U.S.) or America, is a country primarily located in North America. It is a federal republic of 50 U.S. state, states and a federal capital district, Washington, D.C. The 48 ...
, compounding pharmacies are licensed and regulated by states. National standards have been created by Pharmacy Compounding Accreditation Board (PCAB), however, obtaining accreditation is not mandatory and inspections for compliance occur only every three years. The Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a List of United States federal agencies, federal agency of the United States Department of Health and Human Services, Department of Health and Human Services. The FDA is respo ...
(FDA) has authority to regulate "manufacturing" of pharmaceutical products—which applies when drug products are not made or modified as to be ''tailored in some way to the individual patient''—regardless of whether this is done at a factory or at a pharmacy.
In the Drug Quality and Security Act (DQSA) of 2013 (H.R. 3204), Congress amended the Federal Food, Drug, and Cosmetic Act (FFDCA) to clarify limits of FDA jurisdiction over patient-specific compounding, and to provide an optional pathway for "non-traditional" or bulk compounders to operate. The law established that pharmacies compounding only "patient-specific" preparations made in response to a prescription (503A pharmacies) cannot be required to obtain FDA approval for such products, as they will remain exclusively under state-level pharmacy regulation. At the same time, section 503B of the law regulates "outsourcing facilities" which conduct bulk compounding or are used as outsourcing for compounding by other pharmacies. These outsourcing facilities can be explicitly authorized by the Food and Drug Administration under specified circumstances, while being exempted from certain requirements otherwise imposed on mass-producers. In any pharmacy, compounding is not permitted for a drug product that is "essentially a copy" of a mass-produced drug product, however outsourcing pharmacies are subject to a broader definition of "essentially a copy". For traditional/patient-specific compounding, 503A's definition of "copy" retains its original focus on drug ''products'' or ultimate dosage forms rather than drug substances or active ingredients, and in any event it explicitly excludes from its definition any compounded drug product that a given patient's prescribing practitioner determines makes a "significant difference" for the patient.
The FDA weighs the following factors in deciding whether it has authority to "exercise its discretion" to require approval for a custom-compounded drug product:
# Compounding in anticipation of receiving prescriptions
# Compounding drugs removed from the market for safety reasons
# Compounding from bulk ingredients not approved by FDA
# Receiving, storing, or using drugs not made in an FDA-registered facility
# Receiving, storing, or using drugs' components not determined to meet compendia requirements
# Using commercial-scale manufacturing or testing equipment
# Compounding for third parties for resale
# Compounding drugs that are essentially the same as commercially available products
# Failing to operate in conformance with applicable state law
Outsourcing facilities
The DQSA amended the FFDCA to create a new class of FDA-regulated entities known as "outsourcing facilities" whose compounding activities "may ''or'' may not" be patient-specific based on individualized prescriptions. Registered outsourcing facilities, unlike traditional compounding facilities, are subject to the FDA's oversight. In addition to being subjected to Food and Drug Administration inspections, registration, fees, and specified reporting requirements, other requirements of outsourcing facilities include: # Drugs are compounded by or under the direct supervision of a licensed pharmacist # The facility does not compound using "bulk drug substances" (unless certain exceptions apply) and its drugs are manufactured by an FDA-registered establishment # Other ingredients used in compounding the drug must comply with the standards of the applicable United States Pharmacopeia or National Formulary monograph, if a monograph exists # The drug does not appear on a list published by FDA of unsafe or ineffective drugs # The drug is not "essentially a copy" of one or more marketed drugs (as defined uniquely in section 503B, notably more broadly and with narrower exclusions than for "traditional" compounding) # The drug does not appear on the FDA list of drugs or categories of drugs that present "demonstrable difficulties" for compounding # The compounding pharmacist demonstrates that he or she will use controls comparable to the controls applicable under any applicable risk evaluation and mitigation strategy (REMS) # The drug will not be sold or transferred by an entity other than the outsourcing facility # The label of the drug states that it is a compounded drug, as well as the name of the outsourcing facility, the lot or batch number of the drug, dosage form and strength, and other key informationDrug testing and reporting of incidents
Poor practices on the part of drug compounders can result in contamination of products, or products that do not meet their stated strength, purity, or quality. Unless a complaint is filed or a patient is harmed, drugs made by compounders are seldom tested. In Texas, one of only two states that does random testing, significant problems have been found. Random tests by the state's pharmacy board over the last several years have found that as many as one in four compounded drugs was either too weak or too strong. In Missouri, the only other state that does testing, potency varied by as much as 300 percent.Bogdanich, Walt and Tavernise, Sabrina (2012-10-22)U.S. Concern Over Compounders Predates Outbreak of Meningitis
New York Times. In 2002, the
Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a List of United States federal agencies, federal agency of the United States Department of Health and Human Services, Department of Health and Human Services. The FDA is respo ...
, concerned about the rising number of accidents related to compounded medications, identified "red flag" factors and issued a guide devoted to human pharmacy compounding, These factors include instances where pharmacists are:
* Compounding drug products that have been pulled from the market because they were found to be unsafe or ineffective
* Compounding drugs that are essentially copies of a commercially available drug product
* Compounding drugs in advance of receiving prescriptions, except in very limited quantities relating to the amounts of drugs previously compounded based on valid prescriptions
* Compounding finished drugs from bulk active ingredients that aren't components of FDA-approved drugs, without an FDA-sanctioned, investigational new-drug application
* Receiving, storing, or using drug substances without first obtaining written assurance from the supplier that each lot of the drug substance has been made in an FDA-registered facility
* Failing to conform to applicable state law regulating the practice of pharmacy
New England Compounding Center incident
In October 2012 news reports surfaced of an outbreak of fungal meningitis tied to the New England Compounding Center, a pharmacy which engaged in bulk compounding. At that time it was also disclosed that the United States and Massachusetts state health regulators were aware in 2002 that steroid treatments from the New England Compounding Center could cause adverse patient reactions. It was further disclosed that in 2001–02, four people died, more than a dozen were injured and hundreds exposed after they received back-pain injections tainted with a common fungus dispensed by two compounding pharmacies in California and South Carolina.Burtin, T. M.; Grimaldi, J. V. and Martin, T. W. (2012-10-14)Pharmacies Fought Controls; Industry at the Focus of Meningitis Outbreak Beat Back More Federal Oversight
Wall Street Journal In August 2013 further reports tied to the
New England
New England is a region consisting of six states in the Northeastern United States: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont. It is bordered by the state of New York (state), New York to the west and by the ...
compounding center said that about 750 people were sickened, including 63 deaths, and that infections were linked to more than 17,600 doses of methylprednisolone acetate steroid
A steroid is an organic compound with four fused compound, fused rings (designated A, B, C, and D) arranged in a specific molecular configuration.
Steroids have two principal biological functions: as important components of cell membranes t ...
injections used to treat back and joint
A joint or articulation (or articular surface) is the connection made between bones, ossicles, or other hard structures in the body which link an animal's skeletal system into a functional whole.Saladin, Ken. Anatomy & Physiology. 7th ed. McGraw- ...
pain that were shipped to 23 states. At that time, another incident was reported after at least 15 people at two Texas
Texas ( , ; or ) is the most populous U.S. state, state in the South Central United States, South Central region of the United States. It borders Louisiana to the east, Arkansas to the northeast, Oklahoma to the north, New Mexico to the we ...
hospitals developed bacterial infections. All lots of medications dispensed since May 9, 2013, made by Specialty Compounding, LLC of Cedar Park, Texas
Cedar Park is a city and a suburb of Austin, Texas, Austin in the U.S. state of Texas, approximately northwest of the center of Austin. According to the 2020 United States census, 2020 U.S. census, the city's population was 77,595, and in 2022 ...
were recalled. The hospitals reported affected were Corpus Christi Medical Center Bay Area and Corpus Christi Medical Center Doctors Regional. The patients had received intravenous infusions of calcium gluconate, a drug used to treat calcium
Calcium is a chemical element; it has symbol Ca and atomic number 20. As an alkaline earth metal, calcium is a reactive metal that forms a dark oxide-nitride layer when exposed to air. Its physical and chemical properties are most similar to it ...
deficiencies and too much potassium
Potassium is a chemical element; it has Symbol (chemistry), symbol K (from Neo-Latin ) and atomic number19. It is a silvery white metal that is soft enough to easily cut with a knife. Potassium metal reacts rapidly with atmospheric oxygen to ...
in the blood. Implicated in these cases is the Rhodococcus
''Rhodococcus'' is a genus of aerobic, nonsporulating, nonmotile Gram-positive bacteria closely related to ''Mycobacterium'' and ''Corynebacterium''. While a few species are pathogenic, most are benign, and have been found to thrive in a broad ...
bacteria, which can cause symptoms such as fever and pain.
Misuse prompting regulatory changes
The FDA, among others, claims that larger compounding pharmacies act like drug manufacturers and yet circumvent FDA regulations under the banner of compounding. Drugs from compounding pharmacies can be cheaper or alleviate shortages, but can pose greater risk of contamination due in part to the lack of oversight. "Non-traditional" compounders behave like drug manufacturers in some cases by having sales teams that market non-personalized drug products or production capability to doctors, by making drugs that are essentially the same as commercially available mass-produced drug products, or by preparing large batches of a given drug product in anticipation of additional prescriptions before actually receiving them.Grady, Denise; Pollack, Andrew and Tavernise, Sabrina (2012-10-07)Scant Oversight of Drug Maker in Fatal Meningitis Outbreak
New York Times. An FDA spokesperson stated, "The methods of these companies seem far more consistent with those of drug manufacturers than with those of retail pharmacies. Some firms make large amounts of compounded drugs that are copies or near copies of FDA-approved, commercially available drugs. Other firms sell to physicians and patients with whom they have only a remote professional relationship." The head of the FDA has recently requested the following authority from Congress: Various ideas have been proposed to expand federal US regulation in this area, including laws making it easier to identify misuse or misnomered-use and/or stricter enforcement of the longstanding distinction between ''compounding'' versus ''manufacturing''. Some US states have also taken initiatives to strengthen oversight of compounding pharmacies. A major source of opposition to new Food and Drug Administration regulation on compounding is makers of
dietary supplement
A dietary supplement is a manufactured product intended to supplement a person's diet by taking a pill (pharmacy), pill, capsule (pharmacy), capsule, tablet (pharmacy), tablet, powder, or liquid. A supplement can provide nutrients eithe ...
s.Barrett, Paul M. (2012-11-14America's Shadow Pharmacies
Businessweek. Retrieved on 2013-05-13.
See also
*Apothecary
''Apothecary'' () is an Early Modern English, archaic English term for a medicine, medical professional who formulates and dispenses ''materia medica'' (medicine) to physicians, surgeons and patients. The modern terms ''pharmacist'' and, in Brit ...
- the ancestral practitioner of compounding, and their shop
* Bioidentical hormone replacement therapy - Compounding is involved in the surrounding controversy
* New England Compounding Center meningitis outbreak
* Professional Compounding Centers of America
References
External links
International Academy of Compounding Pharmacists
from the
Congressional Research Service
The Congressional Research Service (CRS) is a public policy research institute of the United States Congress. Operating within the Library of Congress, it works primarily and directly for members of Congress and their committees and staff on a ...
and Federation of American Scientists
{{Pharmacy
Pharmacy