Cholera outbreaks and pandemics on:
[Wikipedia]
[Google]
[Amazon]
 Seven cholera pandemics have occurred in the past 200 years, with the first pandemic originating in
Seven cholera pandemics have occurred in the past 200 years, with the first pandemic originating in
 The
The
 The epidemic of cholera, cause unknown and prognosis dire, had reached its peak. Cholera afflicted Mexico's populations in 1833 and 1850, prompting officials to quarantine some populations and fumigate buildings, particularly in major urban centers, but nonetheless the epidemics were disastrous.
During this pandemic, the scientific community varied in its beliefs about the causes of cholera. In France doctors believed cholera was associated with the poverty of certain communities or poor environment. Russians believed the disease was contagious, although doctors did not understand how it spread. The United States believed that cholera was brought by recent immigrants, specifically the Irish, and epidemiologists understand they were carrying disease from British ports. Lastly, some British thought the disease might rise from divine intervention.
The social importance of the government having a direct role in the development and application of science was demonstrated through the U.S. Government's support of efforts to control the epidemic.
The epidemic of cholera, cause unknown and prognosis dire, had reached its peak. Cholera afflicted Mexico's populations in 1833 and 1850, prompting officials to quarantine some populations and fumigate buildings, particularly in major urban centers, but nonetheless the epidemics were disastrous.
During this pandemic, the scientific community varied in its beliefs about the causes of cholera. In France doctors believed cholera was associated with the poverty of certain communities or poor environment. Russians believed the disease was contagious, although doctors did not understand how it spread. The United States believed that cholera was brought by recent immigrants, specifically the Irish, and epidemiologists understand they were carrying disease from British ports. Lastly, some British thought the disease might rise from divine intervention.
The social importance of the government having a direct role in the development and application of science was demonstrated through the U.S. Government's support of efforts to control the epidemic.
 The
The
. UCLA School of Public Health. A two-year outbreak began in
 The
The
 * January 2009: The Mpumalanga province of
* January 2009: The Mpumalanga province of
. March 31, 2009.
WHO Zimbabwe Daily Cholera Update, 16 April 2009
. According to the
. Those for the period 8 April to 16 April list 1375 new cases and 62 deaths (and a resulting CFR of 4.5%).WHO Zimbabwe Daily Cholera Update, 16 April 2009
. The CFR had remained above 4.7% for most of January and early February 2009.
, Circle of Blue, 2010 By November 2010, the disease had spread into the neighboring Dominican Republic. As of August 2016, the epidemic has officially sickened at least 790,000 people and killed more than 9,000 in Haiti. The real burden is probably much higher. In the neighboring Dominican Republic, there have been at least 32,000 suspected cases and 500 related deaths. In Haiti, the outbreak was worsened by Hurricane Matthew, which hit the southern portion of Haiti in fall 2016. The UN has acknowledged its role in the epidemic. In August 2016, the UN pledged to fight the disease and provide assistance for victims through a $400 million fund; But, as of April 2017, member states had contributed a meagre $10 million of the $400 million pledged. * In January 2011, about 411
 Seven cholera pandemics have occurred in the past 200 years, with the first pandemic originating in
Seven cholera pandemics have occurred in the past 200 years, with the first pandemic originating in India
India, officially the Republic of India (Hindi: ), is a country in South Asia. It is the seventh-largest country by area, the second-most populous country, and the most populous democracy in the world. Bounded by the Indian Ocean on the so ...
in 1817. The seventh cholera pandemic
The seventh cholera pandemic (also called by some the 1961–1975 cholera pandemic) is the seventh major outbreak of cholera and occurred principally from the years 1961 to 1975; but the strain involved persists to the present. WHO and some other ...
is officially a current pandemic and has been ongoing since 1961, according to a World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of ...
factsheet in March 2022. Additionally, there have been many documented major local cholera outbreaks, such as a 1991–1994 outbreak in South America and, more recently, the 2016–2021 Yemen cholera outbreak.
Although much is known about the mechanisms behind the spread of cholera, this has not led to a full understanding of what makes cholera outbreaks happen in some places and not others. Lack of treatment of human feces and lack of treatment of drinking water greatly facilitate its spread. Bodies of water have been found to serve as a reservoir
A reservoir (; from French ''réservoir'' ) is an enlarged lake behind a dam. Such a dam may be either artificial, built to store fresh water or it may be a natural formation.
Reservoirs can be created in a number of ways, including contro ...
, and seafood shipped long distances can spread the disease.
Between 1816 and 1923, the first six cholera pandemics occurred consecutively and continuously over time. Increased commerce, migration, and pilgrimage are credited for its transmission. Late in this period (particularly 1879–1883), major scientific breakthroughs toward the treatment of cholera develop: the first immunization by Pasteur
Louis Pasteur (, ; 27 December 1822 – 28 September 1895) was a French chemist and microbiologist renowned for his discoveries of the principles of vaccination, microbial fermentation and pasteurization, the latter of which was named after ...
, the development of the first cholera vaccine, and identification of the bacterium ''Vibrio cholerae'' by Filippo Pacini
Filippo Pacini (25 May 1812 – 9 July 1883) was an Italian anatomist, posthumously famous for isolating the cholera bacterium ''Vibrio cholerae'' in 1854, well before Robert Koch's more widely accepted discoveries 30 years later.
Pacini was born ...
and Robert Koch
Heinrich Hermann Robert Koch ( , ; 11 December 1843 – 27 May 1910) was a German physician and microbiologist. As the discoverer of the specific causative agents of deadly infectious diseases including tuberculosis, cholera (though the bacteri ...
. After a long hiatus, a seventh cholera pandemic
The seventh cholera pandemic (also called by some the 1961–1975 cholera pandemic) is the seventh major outbreak of cholera and occurred principally from the years 1961 to 1975; but the strain involved persists to the present. WHO and some other ...
spread in 1961. The pandemic subsided in the 1970s, but continued on a smaller scale. Outbreaks occur across the developing world to the current day. Epidemics occurred after wars, civil unrest, or natural disasters, when water and food supplies had become contaminated with ''Vibrio cholerae'', and also due to crowded living conditions and poor sanitation.
Deaths in India
India, officially the Republic of India (Hindi: ), is a country in South Asia. It is the seventh-largest country by area, the second-most populous country, and the most populous democracy in the world. Bounded by the Indian Ocean on the so ...
between 1817 and 1860 in the first three pandemics of the nineteenth century, are estimated to have exceeded 15 million people. Another 23 million died between 1865 and 1917, during the next three pandemics. Cholera deaths in the Russian Empire
The Russian Empire was an empire and the final period of the Russian monarchy from 1721 to 1917, ruling across large parts of Eurasia. It succeeded the Tsardom of Russia following the Treaty of Nystad, which ended the Great Northern War. ...
during a similar time period exceeded 2 million.
Pandemics
Thefirst cholera pandemic
First or 1st is the ordinal form of the number one (#1).
First or 1st may also refer to:
*World record, specifically the first instance of a particular achievement
Arts and media Music
* 1$T, American rapper, singer-songwriter, DJ, and reco ...
occurred in the Bengal region of India, near Calcutta
Kolkata (, or , ; also known as Calcutta , List of renamed places in India#West Bengal, the official name until 2001) is the Capital city, capital of the Indian States and union territories of India, state of West Bengal, on the eastern ba ...
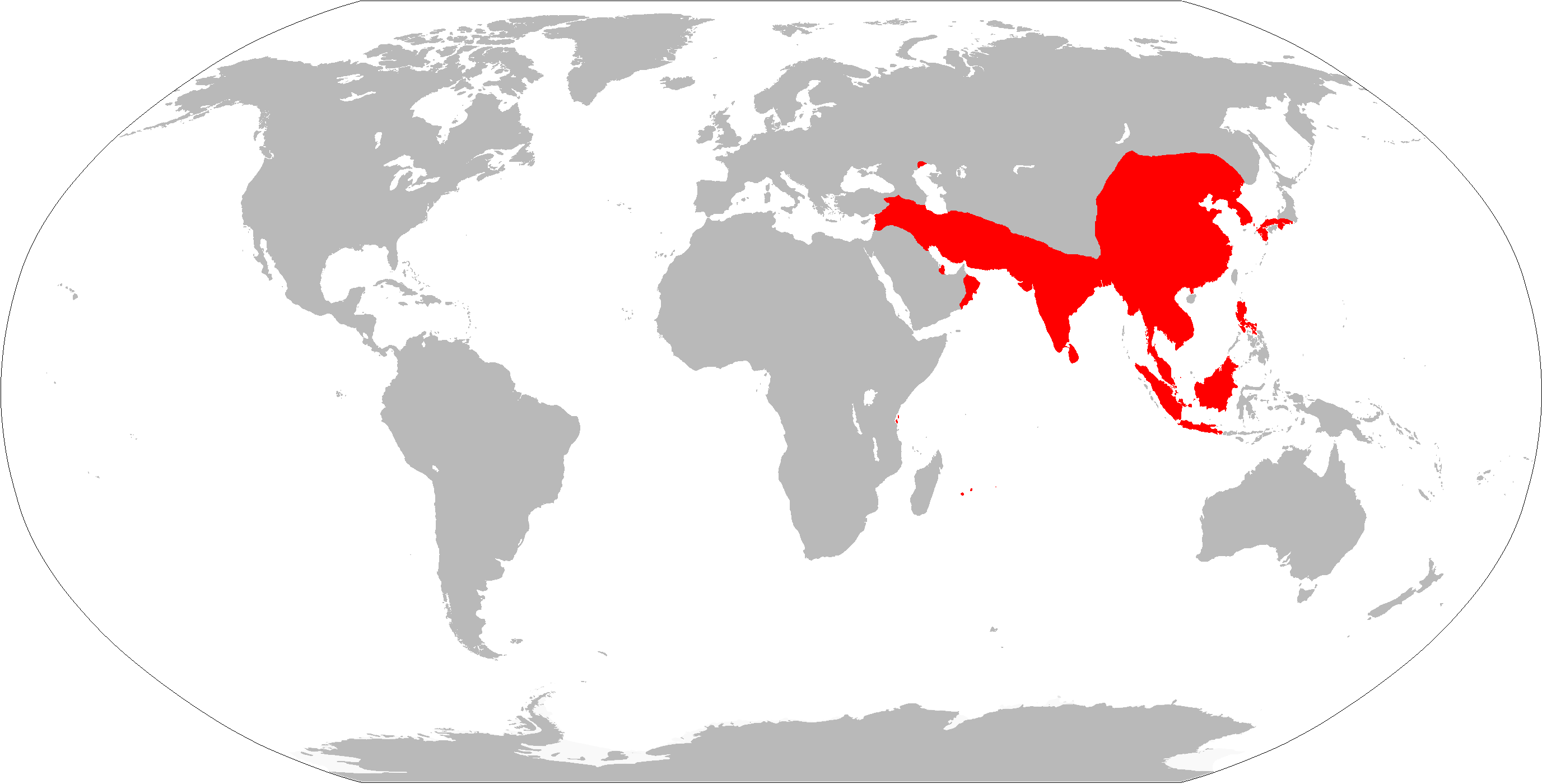
(now Kolkata), starting in 1817 through 1824. The disease dispersed from India to Southeast Asia, the Middle East, Europe, and Eastern Africa through trade routes. The second pandemic lasted from 1826 to 1837 and particularly affected North America and Europe, due to the result of advancements in transportation and global trade, and increased human migration, including soldiers. The third pandemic erupted in 1846, persisted until 1860, extended to North Africa, and reached South America, for the first time specifically affecting Brazil. The fourth pandemic lasted from 1863 to 1875, and spread from India to Naples and Spain, and to the US in 1873. The fifth pandemic was from 1881 to 1896 and started in India and spread to Europe, Asia, and South America. The sixth pandemic started in India and lasted from 1899 to 1923. These epidemics were less fatal due to a greater understanding of the cholera bacteria. Egypt, the Arabian peninsula, Persia, India, and the Philippines were hit hardest during these epidemics, while other areas, such as Germany in 1892 and Naples from 1910 to 1911, also suffered severe outbreaks. The seventh pandemic originated in 1961 in Indonesia and is marked by the emergence of a new strain, nicknamed ''El Tor'', which still persists (as of 2019) in developing countries.
Cholera did not occur in the Americas
The Americas, which are sometimes collectively called America, are a landmass comprising the totality of North and South America. The Americas make up most of the land in Earth's Western Hemisphere and comprise the New World.
Along with th ...
for most of the 20th century after the early 1900s in New York City. It reappeared in the Caribbean toward the end of that century and seems likely to persist.
First, 1817–1824
first cholera pandemic
First or 1st is the ordinal form of the number one (#1).
First or 1st may also refer to:
*World record, specifically the first instance of a particular achievement
Arts and media Music
* 1$T, American rapper, singer-songwriter, DJ, and reco ...
, though previously restricted, began in Bengal
Bengal ( ; bn, বাংলা/বঙ্গ, translit=Bānglā/Bôngô, ) is a geopolitical, cultural and historical region in South Asia, specifically in the eastern part of the Indian subcontinent at the apex of the Bay of Bengal, predom ...
, and then spread across India
India, officially the Republic of India (Hindi: ), is a country in South Asia. It is the seventh-largest country by area, the second-most populous country, and the most populous democracy in the world. Bounded by the Indian Ocean on the so ...
by 1820. Hundreds of thousands of Indians and ten thousand British troops
The British Army is the principal land warfare force of the United Kingdom, a part of the British Armed Forces along with the Royal Navy and the Royal Air Force. , the British Army comprises 79,380 regular full-time personnel, 4,090 Gurkhas ...
died during this pandemic. The cholera outbreak extended as far as China, Indonesia
Indonesia, officially the Republic of Indonesia, is a country in Southeast Asia and Oceania between the Indian and Pacific oceans. It consists of over 17,000 islands, including Sumatra, Java, Sulawesi, and parts of Borneo and New Guine ...
(where more than 100,000 people succumbed on the island of Java
Java (; id, Jawa, ; jv, ꦗꦮ; su, ) is one of the Greater Sunda Islands in Indonesia. It is bordered by the Indian Ocean to the south and the Java Sea to the north. With a population of 151.6 million people, Java is the world's mos ...
alone) and the Caspian Sea
The Caspian Sea is the world's largest inland body of water, often described as the world's largest lake or a full-fledged sea. An endorheic basin, it lies between Europe and Asia; east of the Caucasus, west of the broad steppe of Central Asia ...
in Europe, before receding.
Second, 1829–1837
Asecond cholera pandemic
The second (symbol: s) is the unit of time in the International System of Units (SI), historically defined as of a day – this factor derived from the division of the day first into 24 hours, then to 60 minutes and finally to 60 seconds each ...
reached Russia (see Cholera Riots
Cholera Riots refers to civil disturbances associated with an outbreak or epidemic of cholera.
In Russia
The Cholera Riots (''Холерные бунты'' in Russian) were the riots of the urban population, peasants and soldiers in 1830–18 ...
), Hungary
Hungary ( hu, Magyarország ) is a landlocked country in Central Europe. Spanning of the Pannonian Basin, Carpathian Basin, it is bordered by Slovakia to the north, Ukraine to the northeast, Romania to the east and southeast, Serbia to the ...
(about 100,000 deaths) and Germany
Germany,, officially the Federal Republic of Germany, is a country in Central Europe. It is the second most populous country in Europe after Russia, and the most populous member state of the European Union. Germany is situated betwe ...
in 1831; it killed 130,000 people in Egypt
Egypt ( ar, مصر , ), officially the Arab Republic of Egypt, is a transcontinental country spanning the northeast corner of Africa and southwest corner of Asia via a land bridge formed by the Sinai Peninsula. It is bordered by the Medit ...
that year. In 1832 it reached London
London is the capital and List of urban areas in the United Kingdom, largest city of England and the United Kingdom, with a population of just under 9 million. It stands on the River Thames in south-east England at the head of a estuary dow ...
and the United Kingdom (where more than 55,000 people died) and Paris
Paris () is the Capital city, capital and List of communes in France with over 20,000 inhabitants, most populous city of France, with an estimated population of 2,165,423 residents in 2019 in an area of more than 105 km² (41 sq mi), ma ...
. In London, the disease claimed 6,536 victims and came to be known as "King Cholera"; in Paris, 20,000 died (of a population of 650,000), and total deaths in France amounted to 100,000. In 1833, a cholera epidemic killed many Pomo people
The Pomo are an Indigenous people of California. Historical Pomo territory in Northern California was large, bordered by the Pacific Coast to the west, extending inland to Clear Lake, and mainly between Cleone and Duncans Point. One small gr ...
which are a Native American tribe. The epidemic reached Quebec
Quebec ( ; )According to the Canadian government, ''Québec'' (with the acute accent) is the official name in Canadian French and ''Quebec'' (without the accent) is the province's official name in Canadian English is one of the thirtee ...
, Ontario
Ontario ( ; ) is one of the thirteen provinces and territories of Canada.Ontario is located in the geographic eastern half of Canada, but it has historically and politically been considered to be part of Central Canada. Located in Central C ...
, Nova Scotia
Nova Scotia ( ; ; ) is one of the thirteen provinces and territories of Canada. It is one of the three Maritime provinces and one of the four Atlantic provinces. Nova Scotia is Latin for "New Scotland".
Most of the population are native Eng ...
and New York in the same year, and the Pacific coast of North America by 1834. In the center of the country, it spread through the cities linked by the rivers and steamboat traffic.
Similarly, in Washington DC (where there are no reliable mortality figures), Michael Shiner, an enslaved laborer at the Washington Navy Yard
The Washington Navy Yard (WNY) is the former shipyard and Weapon, ordnance plant of the United States Navy in Southeast, Washington, D.C., Southeast Washington, D.C. It is the oldest shore establishment of the U.S. Navy.
The Yard currently serv ...
recorded, “The time the colery holerabroke out in about June and July August and September 1832 it Raged in the City of Washington and every day they wher eretwelve or 13 carried out to they heirgraves a day." By late July 1832 cholera had spread to Virginia and on 7 August 1832, Commodore Lewis Warrington
Lewis Warrington (3 November 1782 – 12 October 1851) was an officer in the United States Navy during the Barbary Wars and the War of 1812. He later became a Captain. He temporarily served as the Secretary of the Navy. His highest rank ...
confirmed to the Secretary of the Navy Levi Woodbury cholera was at the Gosport Navy Yard, “Between noon of that day, Augustand the morning of Friday August when all work on board her USS ''Fairchild'' stopped, several deaths by cholera occurred and fifteen or sixteen cases (of less violence) were reported." The epidemic of cholera, cause unknown and prognosis dire, had reached its peak. Cholera afflicted Mexico's populations in 1833 and 1850, prompting officials to quarantine some populations and fumigate buildings, particularly in major urban centers, but nonetheless the epidemics were disastrous.
During this pandemic, the scientific community varied in its beliefs about the causes of cholera. In France doctors believed cholera was associated with the poverty of certain communities or poor environment. Russians believed the disease was contagious, although doctors did not understand how it spread. The United States believed that cholera was brought by recent immigrants, specifically the Irish, and epidemiologists understand they were carrying disease from British ports. Lastly, some British thought the disease might rise from divine intervention.
The social importance of the government having a direct role in the development and application of science was demonstrated through the U.S. Government's support of efforts to control the epidemic.
The epidemic of cholera, cause unknown and prognosis dire, had reached its peak. Cholera afflicted Mexico's populations in 1833 and 1850, prompting officials to quarantine some populations and fumigate buildings, particularly in major urban centers, but nonetheless the epidemics were disastrous.
During this pandemic, the scientific community varied in its beliefs about the causes of cholera. In France doctors believed cholera was associated with the poverty of certain communities or poor environment. Russians believed the disease was contagious, although doctors did not understand how it spread. The United States believed that cholera was brought by recent immigrants, specifically the Irish, and epidemiologists understand they were carrying disease from British ports. Lastly, some British thought the disease might rise from divine intervention.
The social importance of the government having a direct role in the development and application of science was demonstrated through the U.S. Government's support of efforts to control the epidemic.
Third, 1846–1860
 The
The third cholera pandemic
Third or 3rd may refer to:
Numbers
* 3rd, the ordinal form of the cardinal number 3
* , a fraction of one third
* 1⁄60 of a ''second'', or 1⁄3600 of a ''minute''
Places
* 3rd Street (disambiguation)
* Third Avenue (disambiguation)
* Hig ...
deeply affected Russia, with over one million deaths. Over 15,000 people died of cholera in Mecca
Mecca (; officially Makkah al-Mukarramah, commonly shortened to Makkah ()) is a city and administrative center of the Mecca Province of Saudi Arabia, and the holiest city in Islam. It is inland from Jeddah on the Red Sea, in a narrow ...
in 1846.Asiatic Cholera Pandemic of 1846–63. UCLA School of Public Health. A two-year outbreak began in
England and Wales
England and Wales () is one of the three legal jurisdictions of the United Kingdom. It covers the constituent countries England and Wales and was formed by the Laws in Wales Acts 1535 and 1542. The substantive law of the jurisdiction is Eng ...
in 1848, and claimed 52,000 lives.
In 1849, a second major outbreak occurred in France. In London, it was the worst outbreak in the city's history, claiming 14,137 lives, over twice as many as the 1832 outbreak. Cholera hit Ireland
Ireland ( ; ga, Éire ; Ulster Scots dialect, Ulster-Scots: ) is an island in the Atlantic Ocean, North Atlantic Ocean, in Northwestern Europe, north-western Europe. It is separated from Great Britain to its east by the North Channel (Grea ...
in 1849 and killed many of the Irish Famine
The Great Famine ( ga, an Gorta Mór ), also known within Ireland as the Great Hunger or simply the Famine and outside Ireland as the Irish Potato Famine, was a period of starvation and disease in Ireland from 1845 to 1852 that constituted a h ...
survivors, already weakened by starvation and fever. In 1849, cholera claimed 5,308 lives in the major port city of Liverpool
Liverpool is a city and metropolitan borough in Merseyside, England. With a population of in 2019, it is the 10th largest English district by population and its metropolitan area is the fifth largest in the United Kingdom, with a populat ...
, England
England is a country that is part of the United Kingdom. It shares land borders with Wales to its west and Scotland to its north. The Irish Sea lies northwest and the Celtic Sea to the southwest. It is separated from continental Europe b ...
, an embarkation point for immigrants to North America, and 1,834 in Hull, England. In Vietnam and Cambodia, cholera hit in summer 1849, killing approximately 589,000 to 800,000 people within one year, along with its consequential famine.
An outbreak in North America took the life of former U.S. President James K. Polk
James Knox Polk (November 2, 1795 – June 15, 1849) was the 11th president of the United States, serving from 1845 to 1849. He previously was the 13th speaker of the House of Representatives (1835–1839) and ninth governor of Tennessee (183 ...
. Cholera, believed spread from Irish immigrant ships from England, spread throughout the Mississippi river system
The Mississippi River System, also referred to as the Western Rivers, is a mostly riverine network of the United States which includes the Mississippi River and connecting waterways. The Mississippi River is the largest drainage basin in the Unit ...
, killing over 4,500 in St. Louis
St. Louis () is the second-largest city in Missouri, United States. It sits near the confluence of the Mississippi and the Missouri Rivers. In 2020, the city proper had a population of 301,578, while the bi-state metropolitan area, which e ...
and over 3,000 in . Thousands died in New York, a major destination for Irish immigrants. Cholera claimed 200,000 victims in Mexico
Mexico (Spanish: México), officially the United Mexican States, is a country in the southern portion of North America. It is bordered to the north by the United States; to the south and west by the Pacific Ocean; to the southeast by Guatema ...
.
That year, cholera was transmitted along the California
California is a state in the Western United States, located along the Pacific Coast. With nearly 39.2million residents across a total area of approximately , it is the most populous U.S. state and the 3rd largest by area. It is also the m ...
, Mormon
Mormons are a religious and cultural group related to Mormonism, the principal branch of the Latter Day Saint movement started by Joseph Smith in upstate New York during the 1820s. After Smith's death in 1844, the movement split into severa ...
and Oregon Trail
The Oregon Trail was a east–west, large-wheeled wagon route and emigrant trail in the United States that connected the Missouri River to valleys in Oregon. The eastern part of the Oregon Trail spanned part of what is now the state of Kans ...
s as 6,000 to 12,000 are believed to have died on their way to the California Gold Rush, Utah
Utah ( , ) is a state in the Mountain West subregion of the Western United States. Utah is a landlocked U.S. state bordered to its east by Colorado, to its northeast by Wyoming, to its north by Idaho, to its south by Arizona, and to it ...
and Oregon
Oregon () is a state in the Pacific Northwest region of the Western United States. The Columbia River delineates much of Oregon's northern boundary with Washington, while the Snake River delineates much of its eastern boundary with Idaho. T ...
in the cholera years of 1849–1855. It is believed more than 150,000 Americans died during the two pandemics between 1832 and 1849.
In 1851, a ship coming from Cuba carried the disease to Gran Canaria
Gran Canaria (, ; ), also Grand Canary Island, is the third-largest and second-most-populous island of the Canary Islands, an archipelago off the Atlantic coast of Northwest Africa which is part of Spain. the island had a population of that ...
. It is considered that more than 6,000 people died in the island during summer, out of a population of 58,000.
In 1852, cholera spread east to the Dutch East Indies and later was carried to Japan in 1854. The Philippines
The Philippines (; fil, Pilipinas, links=no), officially the Republic of the Philippines ( fil, Republika ng Pilipinas, links=no),
* bik, Republika kan Filipinas
* ceb, Republika sa Pilipinas
* cbk, República de Filipinas
* hil, Republ ...
were infected in 1858 and Korea
Korea ( ko, 한국, or , ) is a peninsular region in East Asia. Since 1945, it has been divided at or near the 38th parallel, with North Korea (Democratic People's Republic of Korea) comprising its northern half and South Korea (Republic o ...
in 1859. In 1859, an outbreak in Bengal contributed to transmission of the disease by travelers and troops to Iran
Iran, officially the Islamic Republic of Iran, and also called Persia, is a country located in Western Asia. It is bordered by Iraq and Turkey to the west, by Azerbaijan and Armenia to the northwest, by the Caspian Sea and Turkmeni ...
, Iraq
Iraq,; ku, عێراق, translit=Êraq officially the Republic of Iraq, '; ku, کۆماری عێراق, translit=Komarî Êraq is a country in Western Asia. It is bordered by Turkey to the north, Iran to the east, the Persian Gulf and K ...
, Arabia
The Arabian Peninsula, (; ar, شِبْهُ الْجَزِيرَةِ الْعَرَبِيَّة, , "Arabian Peninsula" or , , "Island of the Arabs") or Arabia, is a peninsula of Western Asia, situated northeast of Africa on the Arabian Plat ...
and Russia. Japan suffered at least seven major outbreaks of cholera between 1858 and 1902. Between 100,000 and 200,000 people died of cholera in Tokyo
Tokyo (; ja, 東京, , ), officially the Tokyo Metropolis ( ja, 東京都, label=none, ), is the capital and List of cities in Japan, largest city of Japan. Formerly known as Edo, its metropolitan area () is the most populous in the world, ...
in an outbreak in 1858–1860.
In 1854, an outbreak of cholera in Chicago
(''City in a Garden''); I Will
, image_map =
, map_caption = Interactive Map of Chicago
, coordinates =
, coordinates_footnotes =
, subdivision_type = Country
, subdivision_name ...
took the lives of 5.5 percent of the population (about 3,500 people). Providence, Rhode Island
Providence is the capital and most populous city of the U.S. state of Rhode Island. One of the oldest cities in New England, it was founded in 1636 by Roger Williams, a Reformed Baptist theologian and religious exile from the Massachusetts ...
suffered an outbreak so widespread that for the next thirty years, 1854 was known there as "The Year of Cholera." In 1853–1854, London's epidemic claimed 10,739 lives. The 1854 Broad Street Cholera outbreak in London ended after the physician John Snow identified a neighborhood Broad Street pump
Soho is an area of the City of Westminster, part of the West End of London. Originally a fashionable district for the aristocracy, it has been one of the main entertainment districts in the capital since the 19th century.
The area was develop ...
as contaminated and convinced officials to remove its handle to prevent people from drawing water there. His study proved contaminated water was the main agent spreading cholera, although he did not identify the contaminant. It would take many years for this message to be believed and fully acted upon. In Spain
, image_flag = Bandera de España.svg
, image_coat = Escudo de España (mazonado).svg
, national_motto = ''Plus ultra'' (Latin)(English: "Further Beyond")
, national_anthem = (English: "Royal March")
, i ...
, over 236,000 died of cholera in the epidemic of 1854–1855. The disease reached South America in 1854 and 1855, with victims in Venezuela and Brazil. During the third pandemic, residents of Tunisia
)
, image_map = Tunisia location (orthographic projection).svg
, map_caption = Location of Tunisia in northern Africa
, image_map2 =
, capital = Tunis
, largest_city = capital
, ...
, which had not been affected by the two previous pandemics, thought Europeans had brought the disease. They blamed their sanitation practices. Some United States scientists began to believe that cholera was somehow associated with African Americans, as the disease was prevalent in the South in areas of black populations. Current researchers note their populations were underserved in terms of sanitation infrastructure and health care, and they lived near the waterways by which travelers and ships carried the disease.
From November 10, 1855 to December 1856, the disease spread through Puerto Rico, claiming 25,820 victims. Cemeteries were expanded to allow for the burial of victims of cholera. In Arecibo
Arecibo (; ) is a city and municipality on the northern coast of Puerto Rico, on the shores of the Atlantic Ocean, located north of Utuado and Ciales; east of Hatillo; and west of Barceloneta and Florida. It is about west of San Juan, th ...
, a large municipality of Puerto Rico, the number of people dying in the streets was so great that the city could not keep up. A man named Ulanga made it his responsibility to collect and carry the dead to the provisional .
Fourth, 1863–1875
Thefourth cholera pandemic
Fourth or the fourth may refer to:
* the ordinal form of the number 4
* ''Fourth'' (album), by Soft Machine, 1971
* Fourth (angle), an ancient astronomical subdivision
* Fourth (music), a musical interval
* ''The Fourth'' (1972 film), a Sovie ...
of the century began in the Ganges Delta of the Bengal
Bengal ( ; bn, বাংলা/বঙ্গ, translit=Bānglā/Bôngô, ) is a geopolitical, cultural and historical region in South Asia, specifically in the eastern part of the Indian subcontinent at the apex of the Bay of Bengal, predom ...
region and traveled with Muslim pilgrims to Mecca
Mecca (; officially Makkah al-Mukarramah, commonly shortened to Makkah ()) is a city and administrative center of the Mecca Province of Saudi Arabia, and the holiest city in Islam. It is inland from Jeddah on the Red Sea, in a narrow ...
. In its first year, the epidemic claimed 30,000 of 90,000 Mecca pilgrims. Cholera spread throughout the Middle East and was carried to Russia, Europe, Africa and North America, in each case spreading from port cities and along inland waterways.
The pandemic reached Northern Africa in 1865 and spread to sub-Saharan Africa, killing 70,000 in Zanzibar
Zanzibar (; ; ) is an insular semi-autonomous province which united with Tanganyika in 1964 to form the United Republic of Tanzania. It is an archipelago in the Indian Ocean, off the coast of the mainland, and consists of many small islan ...
in 1869–1870.
Cholera claimed 90,000 lives in Russia in 1866. The epidemic of cholera that spread with the Austro-Prussian War (1866) is estimated to have taken 165,000 lives in the Austrian Empire
The Austrian Empire (german: link=no, Kaiserthum Oesterreich, modern spelling , ) was a Central-Eastern European multinational great power from 1804 to 1867, created by proclamation out of the realms of the Habsburgs. During its existence ...
, including 30,000 each in Hungary and Belgium and 20,000 in the Netherlands. Other deaths from cholera at the time included 115,000 in Germany, 90,000 in Russia, and 30,000 in Belgium.
In London in June 1866, a localized epidemic in the East End claimed 5,596 lives, just as the city was completing construction of its major sewage and water treatment systems (see London sewerage system
The London sewer system is part of the water infrastructure serving London, England. The modern system was developed during the late 19th century, and as London has grown the system has been expanded. It is currently owned and operated by Thames ...
); the East End section was not quite complete. Epidemiologist William Farr
William Farr CB (30 November 1807 – 14 April 1883) was a British epidemiologist, regarded as one of the founders of medical statistics.
Early life
William Farr was born in Kenley, Shropshire, to poor parents. He was effectively adopted b ...
identified the East London Water Company as the source of the contamination. Farr made use of prior work by John Snow and others pointing to contaminated drinking water as the likely cause of cholera in an 1854 outbreak. Quick action prevented further deaths. In the same year, the use of contaminated canal water in local water works caused a minor outbreak at Ystalyfera
Ystalyfera is a former industrial village and community (Wales), community in the upper Swansea Valley, on the River Tawe, about northeast of Swansea. It is an ward (politics), electoral ward and a community (Wales), community in the unitary a ...
in South Wales. Workers associated with the company and their families were most affected, and 119 died.
In 1867, Italy lost 113,000 lives; and 80,000 died of the disease in Algeria. Outbreaks in North America in the 1870s killed some 50,000 Americans as cholera spread from New Orleans to other ports along the Mississippi River and its tributaries. None of the cities had adequate sanitation systems, and cholera spread through the water supply and contact. (New citation needed—citation (#15) "The 1832 Cholera Epidemic – Part 2" does not mention the 1870s outbreak briefly mentioned here).
Fifth, 1881–1896
 The
The fifth cholera pandemic
Fifth is the ordinal form of the number five.
Fifth or The Fifth may refer to:
* Fifth Amendment to the United States Constitution, as in the expression "pleading the Fifth"
* Fifth column, a political term
* Fifth disease, a contagious rash that ...
- according to Dr A. J. Wall, the 1883–1887 part of the epidemic cost 250,000 lives in Europe and at least 50,000 in the Americas. Cholera claimed 267,890 lives in Russia (1892); 120,000 in Spain
, image_flag = Bandera de España.svg
, image_coat = Escudo de España (mazonado).svg
, national_motto = ''Plus ultra'' (Latin)(English: "Further Beyond")
, national_anthem = (English: "Royal March")
, i ...
; 90,000 in Japan, and over 60,000 in Persia
Iran, officially the Islamic Republic of Iran, and also called Persia, is a country located in Western Asia. It is bordered by Iraq and Turkey to the west, by Azerbaijan and Armenia to the northwest, by the Caspian Sea and Turkmeni ...
. In Egypt
Egypt ( ar, مصر , ), officially the Arab Republic of Egypt, is a transcontinental country spanning the northeast corner of Africa and southwest corner of Asia via a land bridge formed by the Sinai Peninsula. It is bordered by the Medit ...
, cholera claimed more than 58,000 lives. The 1892 outbreak in Hamburg
(male), (female) en, Hamburger(s),
Hamburgian(s)
, timezone1 = Central (CET)
, utc_offset1 = +1
, timezone1_DST = Central (CEST)
, utc_offset1_DST = +2
, postal ...
killed 8,600 people. Although the city government was generally held responsible for the virulence of the epidemic, it was not changed. This was the last serious European cholera outbreak, as cities improved their sanitation and water systems.
Sixth, 1899–1923
Thesixth cholera pandemic
Sixth is the ordinal form of the number six.
* The Sixth Amendment, to the U.S. Constitution
* A keg of beer, equal to 5 U.S. gallons or barrel
* The fraction
Music
* Sixth interval (music)s:
** major sixth, a musical interval
** minor sixth ...
, which was due to the classical strain of O1, had little effect in western Europe because of advances in sanitation and public health
Public health is "the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals". Analyzing the det ...
, but major Russian cities and the Ottoman Empire
The Ottoman Empire, * ; is an archaic version. The definite article forms and were synonymous * and el, Оθωμανική Αυτοκρατορία, Othōmanikē Avtokratoria, label=none * info page on book at Martin Luther University) ...
particularly suffered a high rate of cholera deaths. More than 500,000 people died of cholera in Russia from 1900 to 1925, which was a time of extreme social disruption because of revolution and warfare.
The 1902–1904 cholera epidemic claimed 200,000 lives in the Philippines
The Philippines (; fil, Pilipinas, links=no), officially the Republic of the Philippines ( fil, Republika ng Pilipinas, links=no),
* bik, Republika kan Filipinas
* ceb, Republika sa Pilipinas
* cbk, República de Filipinas
* hil, Republ ...
, including their revolutionary hero and first prime minister Apolinario Mabini
Apolinario Mabini y Maranan (, July 23, 1864 – May 13, 1903) was a Filipino revolutionary leader, educator, lawyer, and statesman who served first as a legal and constitutional adviser to the Revolutionary Government, and then as the firs ...
. Cholera broke out 27 times during the hajj at Mecca
Mecca (; officially Makkah al-Mukarramah, commonly shortened to Makkah ()) is a city and administrative center of the Mecca Province of Saudi Arabia, and the holiest city in Islam. It is inland from Jeddah on the Red Sea, in a narrow ...
from the 19th century to 1930. The sixth pandemic killed more than 800,000 in India
India, officially the Republic of India (Hindi: ), is a country in South Asia. It is the seventh-largest country by area, the second-most populous country, and the most populous democracy in the world. Bounded by the Indian Ocean on the so ...
.
The last outbreak of cholera in the United States was in 1910–1911, when the steamship ''Moltke'' brought infected people from Naples to New York City. Vigilant health authorities isolated the infected in quarantine on Swinburne Island. Eleven people died, including a health care worker at the hospital on the island.
In 1913, the Romanian Army
The Romanian Land Forces ( ro, Forțele Terestre Române) is the army of Romania, and the main component of the Romanian Armed Forces. In recent years, full professionalisation and a major equipment overhaul have transformed the nature of the Lan ...
, while invading Bulgaria
Bulgaria (; bg, България, Bǎlgariya), officially the Republic of Bulgaria,, ) is a country in Southeast Europe. It is situated on the eastern flank of the Balkans, and is bordered by Romania to the north, Serbia and North Macedo ...
during the Second Balkan War
The Second Balkan War was a conflict which broke out when Bulgaria, dissatisfied with its share of the spoils of the First Balkan War, attacked its former allies, Serbia and Greece, on 16 ( O.S.) / 29 (N.S.) June 1913. Serbian and Greek armies r ...
, suffered a cholera outbreak that resulted in 1,600 deaths.
During the outbreak, due to cholera frequently being spread by immigrants and tourists, the disease became associated with either outsiders or marginalized groups in societies. In Italy, some blamed Jews
Jews ( he, יְהוּדִים, , ) or Jewish people are an ethnoreligious group and nation originating from the Israelites Israelite origins and kingdom: "The first act in the long drama of Jewish history is the age of the Israelites""The ...
and Romani, while in British India
The provinces of India, earlier presidencies of British India and still earlier, presidency towns, were the administrative divisions of British governance on the Indian subcontinent. Collectively, they have been called British India. In one ...
numerous Anglo-Indians ascribed the spread of cholera to Hindu
Hindus (; ) are people who religiously adhere to Hinduism. Jeffery D. Long (2007), A Vision for Hinduism, IB Tauris, , pages 35–37 Historically, the term has also been used as a geographical, cultural, and later religious identifier for ...
pilgrims, and in the United States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territori ...
many accused Filipino immigrants of introducing the disease.
Seventh, 1961–?
As of March 2022, theWorld Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of ...
(WHO) continues to define this outbreak as a current pandemic, noting that cholera has become endemic
Endemism is the state of a species being found in a single defined geographic location, such as an island, state, nation, country or other defined zone; organisms that are indigenous to a place are not endemic to it if they are also found else ...
in many countries. In 2017, WHO announced a global strategy aimed at this pandemic with the goal of reducing cholera deaths by 90% by 2030.
The seventh cholera pandemic
The seventh cholera pandemic (also called by some the 1961–1975 cholera pandemic) is the seventh major outbreak of cholera and occurred principally from the years 1961 to 1975; but the strain involved persists to the present. WHO and some other ...
began in Indonesia
Indonesia, officially the Republic of Indonesia, is a country in Southeast Asia and Oceania between the Indian and Pacific oceans. It consists of over 17,000 islands, including Sumatra, Java, Sulawesi, and parts of Borneo and New Guine ...
, called El Tor
El Tor is a particular strain of the bacterium ''Vibrio cholerae'', the causative agent of cholera. Also known as ''V. cholerae'' biotype eltor, it has been the dominant strain in the seventh global cholera pandemic. It is distinguished from t ...
after the strain, and reached East Pakistan
East Pakistan was a Pakistani province established in 1955 by the One Unit Policy, renaming the province as such from East Bengal, which, in modern times, is split between India and Bangladesh. Its land borders were with India and Myanmar, wi ...
(now Bangladesh
Bangladesh (}, ), officially the People's Republic of Bangladesh, is a country in South Asia. It is the eighth-most populous country in the world, with a population exceeding 165 million people in an area of . Bangladesh is among the mos ...
) in 1963, India in 1964, and the Soviet Union
The Soviet Union,. officially the Union of Soviet Socialist Republics. (USSR),. was a List of former transcontinental countries#Since 1700, transcontinental country that spanned much of Eurasia from 1922 to 1991. A flagship communist state, ...
in 1966. From South America
South America is a continent entirely in the Western Hemisphere and mostly in the Southern Hemisphere, with a relatively small portion in the Northern Hemisphere at the northern tip of the continent. It can also be described as the sout ...
, it spread into Italy by 1973. In the late 1970s, there were small outbreaks in Japan and in the South Pacific. There was an outbreak in Odessa in July 1970, and there were also many reports of a cholera outbreak near Baku in 1972, but information about it was suppressed in the Soviet Union. In 1970, a cholera outbreak struck the Sağmalcılar district of Istanbul
)
, postal_code_type = Postal code
, postal_code = 34000 to 34990
, area_code = +90 212 (European side) +90 216 (Asian side)
, registration_plate = 34
, blank_name_sec2 = GeoTLD
, blank_i ...
, then an impoverished slum, claiming more than 50 lives. Because this incident was notorious, the district was renamed as Bayrampaşa. Also in August 1970, a few cases were reported in Jerusalem
Jerusalem (; he, יְרוּשָׁלַיִם ; ar, القُدس ) (combining the Biblical and common usage Arabic names); grc, Ἱερουσαλήμ/Ἰεροσόλυμα, Hierousalḗm/Hierosóluma; hy, Երուսաղեմ, Erusałēm. i ...
.
Other outbreaks
''Vibrio cholerae
''Vibrio cholerae'' is a species of Gram-negative, facultative anaerobe and comma-shaped bacteria. The bacteria naturally live in brackish or saltwater where they attach themselves easily to the chitin-containing shells of crabs, shrimps, and oth ...
'' has shown to be a very potent pathogenic bacterium causing many pandemics and epidemics over the past three centuries. However, most outbreaks are known to be self-limiting, meaning they come to an end after peaking, without human intervention. One of the mechanisms significantly determining the course of epidemics is phage predation. This process is strongly dependent on successful recognition of the bacteria by lytic phages, in which cell surface receptors play a crucial role. Bacteria can reduce their susceptibility by changing their surface receptors and preventing phage adsorption. In the case of ''V. cholerae'', the changed receptor gene expression is due to an alteration in cell-density during its infection cycle, a process called quorum sensing (QS). The stool samples collected from patients contain clumps of bacterial cells, demonstrating the occurrence of cell-cell interaction in the latter stage of the infection cycle. QS is strongly regulated by two auto-inducer molecules, AI-2 and CAI-1. Evidently, these molecules will have a significant effect on the success of phage predation in ''V. cholerae'' infections.
A previous study has unravelled the mode of action of auto-inducers on preventing predation on the level of phage entry. The study has shown that the aforementioned auto-inducers downregulate the ten biosynthetic genes of the surface O-antigen, which is primarily used as a phage receptor for Vibriophages. This mechanism results in an increased phage resistance. It can be stated that the loss of the ability to produce the receptor, reduces the possibility of a phage-dependent limitation or even elimination of ''V. cholerae''. This should be kept in mind when developing a treatment for enteric bacterial infections with phages as an intervention tool. Future approaches may include additional quorum regulators that operate as “quorum quenchers” to reduce quorum-mediated phage resistance.
1990s
* January 1991 – September 1994: Outbreak inSouth America
South America is a continent entirely in the Western Hemisphere and mostly in the Southern Hemisphere, with a relatively small portion in the Northern Hemisphere at the northern tip of the continent. It can also be described as the sout ...
, apparently initiated when a Chinese ship discharged ballast water
Ballast is used in ships to provide moment to resist the lateral forces on the hull. Insufficiently ballasted boats tend to tip or heel excessively in high winds. Too much heel may result in the vessel capsizing. If a sailing vessel needs to voy ...
. Beginning in Peru
, image_flag = Flag of Peru.svg
, image_coat = Escudo nacional del Perú.svg
, other_symbol = Great Seal of the State
, other_symbol_type = National seal
, national_motto = "Firm and Happy f ...
, there were 1.04 million identified cases and almost 10,000 deaths. The causative agent was an O1, El Tor strain, with small differences from the seventh pandemic strain.
In 1992 a new strain appeared in Asia, a non-O1, nonagglutinable vibrio (NAG), which was named O139 Bengal. It was first identified in Tamil Nadu
Tamil Nadu (; , TN) is a state in southern India. It is the tenth largest Indian state by area and the sixth largest by population. Its capital and largest city is Chennai. Tamil Nadu is the home of the Tamil people, whose Tamil language ...
, India, and for a while displaced El Tor in southern Asia. It decreased in prevalence from 1995 to around 10 percent of all cases. It is considered to be an intermediate between El Tor and the classic strain, and occurs in a new serogroup. Scientists warn of evidence of wide-spectrum resistance by cholera bacteria to drugs such as trimethoprim
Trimethoprim (TMP) is an antibiotic used mainly in the treatment of bladder infections. Other uses include for middle ear infections and travelers' diarrhea. With sulfamethoxazole or dapsone it may be used for ''Pneumocystis'' pneumonia in peo ...
, sulfamethoxazole and streptomycin
Streptomycin is an antibiotic medication used to treat a number of bacterial infections, including tuberculosis, ''Mycobacterium avium'' complex, endocarditis, brucellosis, ''Burkholderia'' infection, plague, tularemia, and rat bite fever. F ...
.
* An outbreak in Goma, Democratic Republic of Congo
The Democratic Republic of the Congo (french: République démocratique du Congo (RDC), colloquially "La RDC" ), informally Congo-Kinshasa, DR Congo, the DRC, the DROC, or the Congo, and formerly and also colloquially Zaire, is a country in ...
in July 1994 claimed 12,000 lives by mid-August. During the worst period, it is estimated that as many as 3,000 people were dying per day from cholera.
* A persistent strain of Gulf Coast cholera, 01, has been found in the brackish waters of marshes in Louisiana
Louisiana , group=pronunciation (French: ''La Louisiane'') is a state in the Deep South and South Central regions of the United States. It is the 20th-smallest by area and the 25th most populous of the 50 U.S. states. Louisiana is borde ...
and Texas
Texas (, ; Spanish: ''Texas'', ''Tejas'') is a state in the South Central region of the United States. At 268,596 square miles (695,662 km2), and with more than 29.1 million residents in 2020, it is the second-largest U.S. state by ...
in the United States. It could possibly be transmitted by shipments of seafood from those areas to other parts of the country. Medical personnel were advised to think of cholera when assessing symptoms for people who had not been traveling. There have been occurrences of this cholera in the South but no major outbreaks because of good sanitation and warning systems. There were more cases in two years from the Latin American epidemic, the El Tor strain, than in 20 years from the Gulf Coast strain.
2000s
* In 2000, some 140,000 cholera cases were officially reported toWHO
Who or WHO may refer to:
* Who (pronoun), an interrogative or relative pronoun
* Who?, one of the Five Ws in journalism
* World Health Organization
Arts and entertainment Fictional characters
* Who, a creature in the Dr. Seuss book '' Horton He ...
. Countries in Africa
Africa is the world's second-largest and second-most populous continent, after Asia in both cases. At about 30.3 million km2 (11.7 million square miles) including adjacent islands, it covers 6% of Earth's total surface area ...
accounted for 87 percent of these cases.
* July–December 2007: A lack of clean drinking water in Iraq
Iraq,; ku, عێراق, translit=Êraq officially the Republic of Iraq, '; ku, کۆماری عێراق, translit=Komarî Êraq is a country in Western Asia. It is bordered by Turkey to the north, Iran to the east, the Persian Gulf and K ...
led to an outbreak
In epidemiology, an outbreak is a sudden increase in occurrences of a disease when cases are in excess of normal expectancy for the location or season. It may affect a small and localized group or impact upon thousands of people across an entire ...
of cholera. As of 2 December 2007, the UN had reported 22 deaths and 4,569 laboratory-confirmed cases.
* August 2007: The cholera epidemic started in Orissa, India
Odisha (English: , ), formerly Orissa ( the official name until 2011), is an Indian state located in Eastern India. It is the 8th largest state by area, and the 11th largest by population. The state has the third largest population of ...
. The outbreak affected Rayagada, Koraput and Kalahandi districts, where more than 2,000 people were admitted to hospitals.
* March–April 2008: 2,490 people from 20 provinces throughout Vietnam
Vietnam or Viet Nam ( vi, Việt Nam, ), officially the Socialist Republic of Vietnam,., group="n" is a country in Southeast Asia, at the eastern edge of mainland Southeast Asia, with an area of and population of 96 million, making i ...
were hospitalized with acute diarrhea. Of those hospitalized, 377 patients tested positive for cholera.
* August–October 2008: As of 29 October 2008, a total of 644 laboratory-confirmed cholera cases, including eight deaths, had been verified in Iraq
Iraq,; ku, عێراق, translit=Êraq officially the Republic of Iraq, '; ku, کۆماری عێراق, translit=Komarî Êraq is a country in Western Asia. It is bordered by Turkey to the north, Iran to the east, the Persian Gulf and K ...
.
* November 2008: Médecins Sans Frontières
(MSF; pronounced ), also known as Doctors Without Borders, is a humanitarian medical non-governmental organisation (NGO) or charity of French origin known for its projects in conflict zones and in countries affected by endemic diseases. ...
reported an outbreak of cholera in a refugee camp in the Democratic Republic of the Congo
The Democratic Republic of the Congo (french: République démocratique du Congo (RDC), colloquially "La RDC" ), informally Congo-Kinshasa, DR Congo, the DRC, the DROC, or the Congo, and formerly and also colloquially Zaire, is a country in ...
's eastern provincial capital of Goma
Goma is the capital of North Kivu province in the eastern Democratic Republic of the Congo. It is located on the northern shore of Lake Kivu, next to the Rwandan city of Gisenyi. The lake and the two cities are in the Albertine Rift, the ...
. Some 45 cases were reportedly treated between November 7 and 9.
 * January 2009: The Mpumalanga province of
* January 2009: The Mpumalanga province of South Africa
South Africa, officially the Republic of South Africa (RSA), is the Southern Africa, southernmost country in Africa. It is bounded to the south by of coastline that stretch along the Atlantic Ocean, South Atlantic and Indian Oceans; to the ...
confirmed over 381 new cases of cholera, bringing the total number of cases treated since November 2008 to 2276. Nineteen people died in the province since the outbreak.
* August 2008 – April 2009: In the 2008 Zimbabwean cholera outbreak, which continued into 2009, an estimated 96,591 people in the country
A country is a distinct part of the world, such as a state, nation, or other political entity. It may be a sovereign state or make up one part of a larger state. For example, the country of Japan is an independent, sovereign state, while ...
were infected with cholera and, by 16 April 2009, 4,201 deaths had been reported.World Health Organization. Cholera in Zimbabwe: Epidemiological Bulletin Number 16 Week 13 (22–28 March 2009). March 31, 2009.
WHO Zimbabwe Daily Cholera Update, 16 April 2009
. According to the
World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of ...
, during the week of 22–28 March 2009, the "Crude Case Fatality Ratio (CFR)" had dropped from 4.2% to 3.7%. The daily updates for the period 29 March 2009 to 7 April 2009, list 1748 cases and 64 fatalities, giving a weekly CFR of 3.66% (see table above).World Health Organization: Zimbabwe Daily Cholera Updates. Those for the period 8 April to 16 April list 1375 new cases and 62 deaths (and a resulting CFR of 4.5%).WHO Zimbabwe Daily Cholera Update, 16 April 2009
. The CFR had remained above 4.7% for most of January and early February 2009.
2010s
* August 2010: Cholera inNigeria
Nigeria ( ), , ig, Naìjíríyà, yo, Nàìjíríà, pcm, Naijá , ff, Naajeeriya, kcg, Naijeriya officially the Federal Republic of Nigeria, is a country in West Africa. It is situated between the Sahel to the north and the Gulf o ...
was reaching epidemic proportions after widespread confirmation of the disease outbreaks in 12 of its 36 states. 6400 cases were reported with 352 reported deaths. The health ministry blamed the outbreak on heavy seasonal rainfall and poor sanitation.
* October 2010 – present, Haiti and Dominican Republic
The Dominican Republic ( ; es, República Dominicana, ) is a country located on the island of Hispaniola in the Greater Antilles archipelago of the Caribbean region. It occupies the eastern five-eighths of the island, which it shares with ...
: Late in October 2010, an outbreak
In epidemiology, an outbreak is a sudden increase in occurrences of a disease when cases are in excess of normal expectancy for the location or season. It may affect a small and localized group or impact upon thousands of people across an entire ...
was reported in Haiti. As of November 16, the Haitian Health Ministry reported the number of dead to be 1,034, with hospitalizations for cholera symptoms totaling over 16,700. The outbreak was blamed on a camp of Nepalese United Nations peacekeepers; this was disputed, but since acknowledged by the United Nations. The outbreak started on the upper Artibonite River
The Artibonite River ( Spanish: '' Río Artibonito''; Haitian Creole: ''Latibonit'') is the longest river in Haiti, and the longest on the island of Hispaniola. It is also the second-longest river in the Caribbean, behind the Cauto River in Cuba. ...
; people first contracted the disease by taking water from this river. In addition, some scientists think the hurricane and weather conditions in Haiti worsened the consequences of the outbreak, and damaged sanitation systems, allowing it to spread.Aubrey Ann Parker, "Cholera in Haiti: the Climate Connection", Circle of Blue, 2010 By November 2010, the disease had spread into the neighboring Dominican Republic. As of August 2016, the epidemic has officially sickened at least 790,000 people and killed more than 9,000 in Haiti. The real burden is probably much higher. In the neighboring Dominican Republic, there have been at least 32,000 suspected cases and 500 related deaths. In Haiti, the outbreak was worsened by Hurricane Matthew, which hit the southern portion of Haiti in fall 2016. The UN has acknowledged its role in the epidemic. In August 2016, the UN pledged to fight the disease and provide assistance for victims through a $400 million fund; But, as of April 2017, member states had contributed a meagre $10 million of the $400 million pledged. * In January 2011, about 411
Venezuela
Venezuela (; ), officially the Bolivarian Republic of Venezuela ( es, link=no, República Bolivariana de Venezuela), is a country on the northern coast of South America, consisting of a continental landmass and many islands and islets in th ...
n citizens attended a wedding in the Dominican Republic, where they ate ceviche (raw fish cured in lemon juice) at the celebration. By the time they returned to Caracas and other Venezuelan cities, some of these travelers were suffering from symptoms of cholera. By January 28, almost 111 cases had been confirmed by the Venezuelan Health Authorities, who quickly set up an 800 number for people to call who wondered whether they were infected. Internationally, Colombia secured its eastern border against immigrants and probable transmission of the disease. Dominican officials started a nationwide study to determine the cause of the outbreak, and warned residents of the imminent danger associated with the consumption of raw fish and shellfish. As of January 29, 2011, none of the cases in Venezuela proved fatal, but two patients were hospitalized. Since the victims had quickly sought help, the outbreak was detected and contained.
* 2011: Nigeria
Nigeria ( ), , ig, Naìjíríyà, yo, Nàìjíríà, pcm, Naijá , ff, Naajeeriya, kcg, Naijeriya officially the Federal Republic of Nigeria, is a country in West Africa. It is situated between the Sahel to the north and the Gulf o ...
and Democratic Republic of Congo
The Democratic Republic of the Congo (french: République démocratique du Congo (RDC), colloquially "La RDC" ), informally Congo-Kinshasa, DR Congo, the DRC, the DROC, or the Congo, and formerly and also colloquially Zaire, is a country in ...
have had outbreaks; the latter has suffered years of disruption from warfare. Somalia
Somalia, , Osmanya script: 𐒈𐒝𐒑𐒛𐒐𐒘𐒕𐒖; ar, الصومال, aṣ-Ṣūmāl officially the Federal Republic of SomaliaThe ''Federal Republic of Somalia'' is the country's name per Article 1 of thProvisional Constituti ...
has suffered a double hit of cholera and famine
A famine is a widespread scarcity of food, caused by several factors including war, natural disasters, crop failure, population imbalance, widespread poverty, an economic catastrophe or government policies. This phenomenon is usually accompani ...
, associated with the refugee camps, limited sanitation, and severe drought, causing famine and lowered resistance.
* Cholera outbreak in 2011 and 2012 in multiple African nations, in all regions except North Africa; among the affected nations, Ghana
Ghana (; tw, Gaana, ee, Gana), officially the Republic of Ghana, is a country in West Africa. It abuts the Gulf of Guinea and the Atlantic Ocean to the south, sharing borders with Ivory Coast in the west, Burkina Faso in the north, and To ...
has led an intense campaign for handwashing. In Sierra Leone
Sierra Leone,)]. officially the Republic of Sierra Leone, is a country on the southwest coast of West Africa. It is bordered by Liberia to the southeast and Guinea surrounds the northern half of the nation. Covering a total area of , Sierr ...
, some 21,500 cases, with 290 deaths reported in 2012.
* On August 21, 2013, the United States State Department
The United States Department of State (DOS), or State Department, is an executive department of the U.S. federal government responsible for the country's foreign policy and relations. Equivalent to the ministry of foreign affairs of other nat ...
issued a security message warning U.S. citizens in or traveling to Cuba about an outbreak of cholera in Havana
Havana (; Spanish: ''La Habana'' ) is the capital and largest city of Cuba. The heart of the La Habana Province, Havana is the country's main port and commercial center.
. It may be linked to a reported outbreak of cholera in eastern Cuba.
* An ongoing cholera outbreak in Ghana in 2014, hitting hard the capital Accra, has claimed some 100 lives and over 11,000 cases by September. It did not gain much notice because of being overshadowed by Ebola news in nearby countries. In 2011 and 2012 Ghana had cholera epidemics combined that totaled 16,000 cases and 130 deaths.
* September 2015: Ongoing cholera epidemic in Tanzania resulting in 13 deaths and almost 1000 cases so far—mainly in Dar es Salaam, but also in Morogoro and Iringa, caused by the O1 Ogawa strain. There had been an earlier outbreak in the lake Tanganyika area, starting in the refugee population who had fled from Burundi. 30 deaths and 4400 cases were reported in May 2015.
* Somalia, 2017: An ongoing outbreak started in January 2017 in Somalia. By the end of May, there were more than 50,000 cases, associated with 880 deaths; the case fatality rate is 1.7% (2.1% in children). Sixteen of the country's eighteen regions are involved, with the worst affected being Bay and Togdheer
Togdheer ( so, Togdheer, ar, تُوْجْدَيْر, Tūjdayr) is an administrative region ('' gobol'') in central Somaliland. Togdheer is bordered by Maroodi Jeex to the west, Saaxil to the north, Sanaag to the northeast, Sool to the east a ...
.
* In April 2017, an outbreak resurged in Yemen
Yemen (; ar, ٱلْيَمَن, al-Yaman), officially the Republic of Yemen,, ) is a country in Western Asia. It is situated on the southern end of the Arabian Peninsula, and borders Saudi Arabia to the Saudi Arabia–Yemen border, north and ...
(it had started in October 2016). UNICEF
UNICEF (), originally called the United Nations International Children's Emergency Fund in full, now officially United Nations Children's Fund, is an agency of the United Nations responsible for providing humanitarian and developmental aid to ...
and the World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of ...
(WHO) estimated that, by 24 June 2017, the total cases in the country exceeded 200,000, with 1,300 deaths. UNICEF and WHO attributed the outbreak to malnutrition, disrupted sanitation, and interrupted access to clean water due to the country's ongoing civil war
A civil war or intrastate war is a war between organized groups within the same state (or country).
The aim of one side may be to take control of the country or a region, to achieve independence for a region, or to change government policies ...
. The effects of the outbreak were exacerbated by the collapse of Yemeni health services; many health workers have remained unpaid for months. The outbreak occurred ten days after the sewerage systems in the Yemeni capital of Sana'a
Sanaa ( ar, صَنْعَاء, ' , Yemeni Arabic: ; Old South Arabian: 𐩮𐩬𐩲𐩥 ''Ṣnʿw''), also spelled Sana'a or Sana, is the capital and largest city in Yemen and the centre of Sanaa Governorate. The city is not part of the Gover ...
stopped working on 17 April. Approximately half of the cases, and a quarter of the deaths, were among children. On 14 August, WHO
Who or WHO may refer to:
* Who (pronoun), an interrogative or relative pronoun
* Who?, one of the Five Ws in journalism
* World Health Organization
Arts and entertainment Fictional characters
* Who, a creature in the Dr. Seuss book '' Horton He ...
stated that about 500,000 people in Yemen were affected by cholera. WHO called it "the worst cholera outbreak in the world".
* In August 2018, the Algerian Ministry of Health announced that 56 cases of cholera were confirmed in the regions of the capital Algiers and surrounding provinces of Tipaza, Blida, Bouira, Medea and Ain Defla, with reports of 2 deaths as a result of this epidemic. A water source in the town of Hamr El-Ain, Tipaza was found to have been the origin of cholera contamination. The access to the water source was restricted.
*On September 6, 2018, a cholera outbreak was declared in Zimbabwe. The Government declared a state of emergency on September 11, 2018. The outbreak has so far killed 48 people, and there are at least 98 confirmed cases as of September 27, 2018.
2020s
* An ongoing cholera outbreak was reported in several regions ofNiger
)
, official_languages =
, languages_type = National languagesPossible 2022 Mariupol cholera outbreak.
* Following the
June 2022 Afghanistan earthquake
A deep earthquake measuring magnitude () 6.2 struck southeastern Afghanistan on 22 June 2022 at 01:24:36 AFT (on 21 June 2022 at 20:54:36 UTC). It affected the provinces of Paktika and Khost, and parts of Khyber Pakhtunkhwa, Pakistan. It was f ...
, the United Nations warned of a possible outbreak in the affected areas. In August 2022, over 400 cases were reported, and eight people died.
* In September 2022, a cholera outbreak believed to be linked to irrigation of crops using contaminated water broke out in several regions in Syria. The United Nations said it presented a "serious threat to people in Syria and the region". Twenty-nine people died and a total of 338 cases were recorded. In October, 2022 Lebanon recorded two cholera cases in Akkar
Akkar District ( ar, قضاء عكار) is the only district in Akkar Governorate, Lebanon. It is coextensive with the governorate and covers an area of . The UNHCR estimated the population of the district to be 389,899 in 2015, including 106,935 ...
province, bordering Syria.
* In October 2022, Haiti experienced a cholera outbreak.
False reports
A persistenturban myth
An urban legend (sometimes contemporary legend, modern legend, urban myth, or urban tale) is a genre of folklore comprising stories or fallacious claims circulated as true, especially as having happened to a "friend of a friend" or a family m ...
states 90,000 people died in Chicago of cholera and typhoid fever
Typhoid fever, also known as typhoid, is a disease caused by '' Salmonella'' serotype Typhi bacteria. Symptoms vary from mild to severe, and usually begin six to 30 days after exposure. Often there is a gradual onset of a high fever over several ...
in 1885, but this story has no factual basis. In 1885, a torrential rainstorm flushed the Chicago River
The Chicago River is a system of rivers and canals with a combined length of that runs through the city of Chicago, including its center (the Chicago Loop). Though not especially long, the river is notable because it is one of the reasons for ...
and its attendant pollutants into Lake Michigan far enough that the city's water supply was contaminated. But, as cholera was not present in the city, there were no cholera-related deaths. As a result of the pollution, the city made changes to improve its treatment of sewage and avoid similar events.
In popular culture
Unliketuberculosis
Tuberculosis (TB) is an infectious disease usually caused by '' Mycobacterium tuberculosis'' (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, i ...
("consumption"), which in literature and the arts was often romanticized as a disease of denizens of the demimondaine
is French for "half-world". The term derives from a play called , by Alexandre Dumas , published in 1855. The play dealt with the way that prostitution at that time threatened the institution of marriage. The was the world occupied by elite me ...
or those with an artistic temperament, Sontag Susan (1977) ''Illness as Metaphor
''Illness as Metaphor'' is a 1978 work of critical theory by Susan Sontag, in which she challenged the victim-blaming in the language that is often used to describe diseases and the people affected by them.
Teasing out the similarities between p ...
/ AIDS and Its Metaphors
''AIDS and Its Metaphors'' is a 1989 work of critical theory by Susan Sontag. In this companion book to her ''Illness as Metaphor'' (1978), Sontag extends her arguments about the metaphors attributed to cancer to the AIDS crisis. Sontag explores ...
''. New York: Picador. cholera is a disease that today almost entirely affects the lower-classes living in filth and poverty. This, and the unpleasant course of the disease – which includes voluminous "rice-water" diarrhea, the hemorrhaging of liquids from the mouth, and violent muscle contractions which continue even after death – has discouraged the disease being romanticized. It is seldom presented at all in popular culture.
*The 1889 novel '' Mastro-don Gesualdo'' by Giovanni Verga
Giovanni Carmelo Verga di Fontanabianca (; 2 September 1840 – 27 January 1922) was an Italian realist ('' verista'') writer, best known for his depictions of life in his native Sicily, especially the short story and later play ''Cavalleria ...
presents the course of a cholera epidemic across the island of Sicily
(man) it, Siciliana (woman)
, population_note =
, population_blank1_title =
, population_blank1 =
, demographics_type1 = Ethnicity
, demographics1_footnotes =
, demographi ...
, but does not show the suffering of the victims.
*In Thomas Mann
Paul Thomas Mann ( , ; ; 6 June 1875 – 12 August 1955) was a German novelist, short story writer, social critic, philanthropist, essayist, and the 1929 Nobel Prize in Literature laureate. His highly symbolic and ironic epic novels and novell ...
's novella ''Death in Venice
''Death in Venice ''(German: ''Der Tod in Venedig'') is a novella by German author Thomas Mann, published in 1912. It presents an ennobled writer who visits Venice and is liberated, uplifted, and then increasingly obsessed by the sight of a Poli ...
'', first published in 1912 as ''Der Tod in Venedig'', Mann "presented the disease as emblematic of the final 'bestial degradation' of the sexually transgressive author Gustav von Aschenbach." Contrary to the facts of how violently cholera kills, Mann has his protagonist die peacefully on a beach in a deck chair. Luchino Visconti
Luchino Visconti di Modrone, Count of Lonate Pozzolo (; 2 November 1906 – 17 March 1976) was an Italian filmmaker, stage director, and screenwriter. A major figure of Italian art and culture in the mid-20th century, Visconti was one of the ...
's 1971 film version also hid from the audience the graphic course of the disease. Mann's novella was also adapted as an opera by Benjamin Britten
Edward Benjamin Britten, Baron Britten (22 November 1913 – 4 December 1976, aged 63) was an English composer, conductor, and pianist. He was a central figure of 20th-century British music, with a range of works including opera, other ...
in 1973, his last one; and as a ballet by John Neumeier
John Neumeier (born February 24, 1939) is an American ballet dancer, choreographer, and director. He has been the director and chief choreographer of Hamburg Ballet since 1973. Five years later he founded the Hamburg Ballet School, which also in ...
for his Hamburg Ballet
The Hamburg Ballet is a ballet company based in Hamburg, Germany. Since 1973, it has been directed by the American dancer and choreographer John Neumeier. In addition there is a ballet school, , established in 1978. The performances of the Hamb ...
company, in December 2003.*
*W. Somerset Maugham's novel '' The Painted Veil'' (1925), explores a British couple's marriage against the work of the husband as a doctor in China during a 20th-century cholera epidemic. It was most recently adapted as a film of the same name (2006), starring Edward Norton
Edward Harrison Norton (born August 18, 1969) is an American actor and filmmaker. He has received numerous awards and nominations, including a Golden Globe Award and three Academy Award nominations.
Born in Boston, Massachusetts and raised ...
and Naomi Watts
Naomi Ellen Watts (born 28 September 1968) is a British actress. After her family moved to Australia, she made her film debut there in the drama '' For Love Alone'' (1986) and then appeared in three television series, '' Hey Dad..!'' (1990), '' ...
. It did show people suffering the physical effects of the disease. Earlier adaptations in 1934 and 1957 kept the disease out of sight.
*In Gabriel Garcia Márquez's 1985 novel ''Love in the Time of Cholera
''Love in the Time of Cholera'' ( es, El amor en los tiempos del cólera) is a novel written in Spanish by Colombian Nobel Prize-winning author Gabriel García Márquez and published in 1985. Edith Grossman's English translation was published by ...
'', cholera is "a looming background presence rather than a central figure requiring vile description." The novel was adapted in 2007 for the film of the same name directed by Mike Newell.
* The Horseman on the Roof (Le Hussard sur Le toit) by Jean Giono is about a cholera epidemic in the south of France.
See also
* List of epidemicsReferences
Further reading
* * * * {{History of infectious diseases Bacterial diseases *outbreaks Gastroenterology Intestinal infectious diseases