Campylobacter jejuni on:
[Wikipedia]
[Google]
[Amazon]
''Campylobacter jejuni'' () is a species of pathogenic bacteria, one of the most common causes of food poisoning in Europe and in the US. The vast majority of cases occur as isolated events, not as part of recognized outbreaks. Active surveillance through the Foodborne Diseases Active Surveillance Network (FoodNet) indicates that about 20 cases are ''diagnosed'' each year for each 100,000 people in the US, while many more cases are undiagnosed or unreported; the CDC estimates a total of 1.5 million infections every year. The European Food Safety Authority reported 246,571 cases in 2018, and estimated approximately nine million cases of human campylobacteriosis per year in the European Union.
''Campylobacter'' is a genus of bacteria that is among the most common causes of bacterial infections in humans worldwide. Campylobacter means "curved rod", deriving from the Greek ''kampylos ''(curved) and ''baktron'' (rod). Of its many species, ''C. jejuni'' is considered one of the most important from both a microbiological and public health perspective.
''C. jejuni'' is commonly associated with
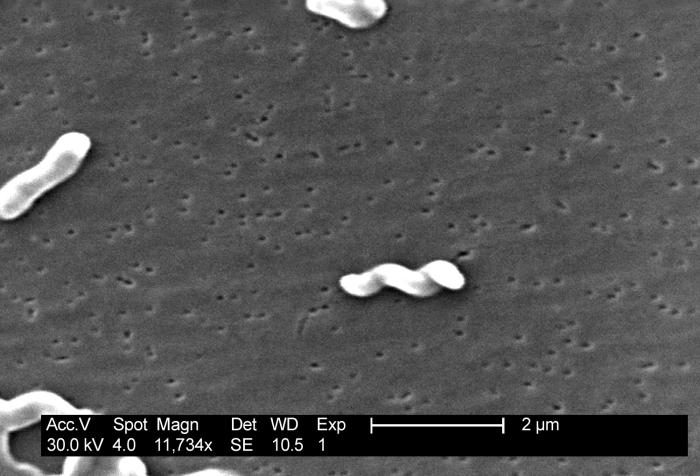 Under light microscopy, ''C. jejuni'' has a characteristic "sea-gull" shape as a consequence of its helical form. ''Campylobacter'' is grown on specially selective "CAMP"
Under light microscopy, ''C. jejuni'' has a characteristic "sea-gull" shape as a consequence of its helical form. ''Campylobacter'' is grown on specially selective "CAMP"
Campylobacter jejuni
genomes and related information a
PATRIC
a Bioinformatics Resource Center funded b
NIAID
* ttp://bacdive.dsmz.de/index.php?search=2121&submit=Search Type strain of ''Campylobacter jejuni'' at Bac''Dive'' - the Bacterial Diversity Metadatabase {{Authority control Campylobacterota Bacteria described in 1931
poultry
Poultry () are domesticated birds kept by humans for their eggs, their meat or their feathers. These birds are most typically members of the superorder Galloanserae (fowl), especially the order Galliformes (which includes chickens, quails, ...
, and is also commonly found in animal feces. ''Campylobacter'' is a helical-shaped, non-spore-forming, Gram-negative
Gram-negative bacteria are bacteria that do not retain the crystal violet stain used in the Gram staining method of bacterial differentiation. They are characterized by their cell envelopes, which are composed of a thin peptidoglycan cell wa ...
, microaerophilic
A microaerophile is a microorganism that requires environments containing lower levels of dioxygen than that are present in the atmosphere (i.e. < 21% O2; typically 2–10% O2) for optimal growth. A more r ...
, nonfermenting motile bacterium
Bacteria (; singular: bacterium) are ubiquitous, mostly free-living organisms often consisting of one biological cell. They constitute a large domain of prokaryotic microorganisms. Typically a few micrometres in length, bacteria were amon ...
with a single flagellum at one or both poles, which are also oxidase-positive and grow optimally at 37 to 42 °C. When exposed to atmospheric oxygen, ''C. jejuni'' is able to change into a coccal form. This species of pathogenic bacteria is one of the most common causes of human gastroenteritis in the world. Food poisoning caused by ''Campylobacter'' species can be severely debilitating, but is rarely life-threatening. It has been linked with subsequent development of Guillain–Barré syndrome
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain oft ...
, which usually develops two to three weeks after the initial illness. Individuals with recent ''C. jejuni'' infections develop Guillain-Barré syndrome at a rate of 0.3 per 1000 infections, about 100 times more often than the general population. Another chronic condition that may be associated with ''Campylobacter'' infection is reactive arthritis
Reactive arthritis, also known as Reiter's syndrome, is a form of inflammatory arthritis that develops in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria and developing an infection can t ...
. Reactive arthritis is a complication strongly associated with a particular genetic make-up. That is, persons who have the human leukocyte antigen B27 (HLA-B27) are most susceptible. Most often, the symptoms of reactive arthritis will occur up to several weeks after infection.
History
In 1886 a pediatrician, Theodor Escherich, observed '' Campylobacters'' from diarrhea samples of children. The first isolation of ''C. jejuni'' was in Brussels, Belgium, from stool samples of a patient with diarrhea.Disease
Campylobacteriosis is an infectious disease caused by bacteria of the genus ''Campylobacter''. In most people who become ill with campylobacteriosis, symptoms develop within two to five days of exposure to the organism and illness typically lasts seven days following onset. Infection with ''C. jejuni'' usually results inenteritis
Enteritis is inflammation of the small intestine. It is most commonly caused by food or drink contaminated with pathogenic microbes,Dugdale, David C., IIII, and George F Longretc"Enteritis" MedlinePlus Medical Encyclopedia, 18 October 2008. Access ...
, which is characterised by abdominal pain, diarrhea, fever, and malaise. Diarrhea itself can vary in severity from loose to bloody stools. The disease is usually self-limiting. However, it does respond to antibiotics
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention o ...
. Severe (accompanying fevers, blood in stools) or prolonged cases may require erythromycin, azithromycin
Azithromycin, sold under the brand names Zithromax (in oral form) and Azasite (as an eye drop), is an antibiotic medication used for the treatment of a number of bacterial infections. This includes middle ear infections, strep throat, pneumo ...
, ciprofloxacin
Ciprofloxacin is a fluoroquinolone antibiotic used to treat a number of bacterial infections. This includes bone and joint infections, intra abdominal infections, certain types of infectious diarrhea, respiratory tract infections, skin inf ...
, or norfloxacin
Norfloxacin, sold under the brand name Noroxin among others, is an antibiotic that belongs to the class of fluoroquinolone antibiotics. It is used to treat urinary tract infections, gynecological infections, inflammation of the prostate gland, g ...
. Fluid replacement via oral rehydration salts may be needed and intravenous fluid may be required for serious cases. Possible complications of campylobacteriosis include Guillain–Barré syndrome
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain oft ...
and reactive arthritis
Reactive arthritis, also known as Reiter's syndrome, is a form of inflammatory arthritis that develops in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria and developing an infection can t ...
.
Pathogenesis
Studies on the pathogenesis of ''C. jejuni'' show that for this organism to cause disease, the susceptibility of the host and the relative virulence of the infecting strain are both important. Infection results from the ingestion of contaminated food or water, and the infective dose can be as low as 800 organisms. To initiate infection, the organism must penetrate the gastrointestinalmucus
Mucus ( ) is a slippery aqueous secretion produced by, and covering, mucous membranes. It is typically produced from cells found in mucous glands, although it may also originate from mixed glands, which contain both serous and mucous cells. It ...
, which it does using its high motility and spiral shape. The bacteria must then adhere to the gut enterocytes and can then induce diarrhea by toxin release. ''C. jejuni'' releases several different toxins, mainly enterotoxin and cytotoxins, which vary from strain to strain and correlate with the severity of the enteritis (inflammation of the small intestine). During infection, levels of all immunoglobulin classes rise. Of these, IgA is the most important because it can cross the gut wall. IgA immobilises organisms, causing them to aggregate and activate complement, and also gives short-term immunity against the infecting strain of organism. The bacteria colonize the small and large intestines, causing inflammatory diarrhea with fever. Stools contain leukocytes and blood. The role of toxins in pathogenesis is unclear. ''C jejuni'' antigens that cross-react with one or more neural structures may be responsible for triggering the Guillain–Barré syndrome
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain oft ...
.
Hypoacylated lipopolysaccharide
Lipopolysaccharides (LPS) are large molecules consisting of a lipid and a polysaccharide that are bacterial toxins. They are composed of an O-antigen, an outer core, and an inner core all joined by a covalent bond, and are found in the outer ...
(LPS) from ''C. jejuni'' induces moderate TLR4
Toll-like receptor 4 is a protein that in humans is encoded by the ''TLR4'' gene. TLR4 is a transmembrane protein, member of the toll-like receptor family, which belongs to the pattern recognition receptor (PRR) family. Its activation leads to an ...
-mediated inflammatory response in macrophages and such LPS bioactivity may eventually result in the failure of local and systemic bacterial clearance in patients. At the same time, moderation of anti-bacterial responses may be advantageous for infected patients in clinical practice, since such an attenuated LPS may not be able to induce severe sepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is follo ...
in susceptible individuals.
One of the most important virulence factor of ''C. jejuni'' are flagella. The flagellar protein FlaA has been proven to be one of the abundant proteins in the cell. Flagella are required for motility, biofilm formation, host cell interactions and host colonization. The production of flagella is energetically costly so the production must be regulated from metabolic standpoint. CsrA is a post-transcriptional regulator that regulates the expression of FlaA by binding to ''flaA'' mRNA and is able to repress its translation. ''CsrA'' mutant strains have been studied and the mutant strains exhibit dysregulation of 120-150 proteins that are included in motility, host cell adherence, host cell invasion, chemotaxis, oxidative stress resistance, respiration and amino acid and acetate metabolism. Transcriptional and post-transcriptional regulation of flagellar synthesis in ''C. jejuni'' enables proper biosynthesis of flagella and it is important for pathogenesis of this bacteria.
Other important virulence factors of ''C. jejuni'' are the ability to produce N-linked glycosylation of more than 30 proteins. These proteins are important for the bacteria colonization, adherence and invasion. ''C. jejuni'' secretes ''Campylobacter'' invasive antigens (Cia) which facilitates the motility. The bacteria produces also cytolethal distending toxins that participate in cell cycle control and induction of host cell apoptosis. ''C. jejuni'' also exploits different adaptation strategies in which the host factors seem to play a role for pathogenesis of this bacteria.
Sources
''Campylobacter jejuni'' is commonly associated withpoultry
Poultry () are domesticated birds kept by humans for their eggs, their meat or their feathers. These birds are most typically members of the superorder Galloanserae (fowl), especially the order Galliformes (which includes chickens, quails, ...
, and it naturally colonises the digestive tract
The gastrointestinal tract (GI tract, digestive tract, alimentary canal) is the tract or passageway of the digestive system that leads from the mouth to the anus. The GI tract contains all the major organs of the digestive system, in humans and ...
of many bird species. All types of poultry and wild birds can become colonized with Campylobacter. One study found that 30% of European starlings
Starlings are small to medium-sized passerine birds in the family Sturnidae. The Sturnidae are named for the genus '' Sturnus'', which in turn comes from the Latin word for starling, ''sturnus''. Many Asian species, particularly the larger ones, ...
in farm settings in Oxfordshire, United Kingdom
The United Kingdom of Great Britain and Northern Ireland, commonly known as the United Kingdom (UK) or Britain, is a country in Europe, off the north-western coast of the European mainland, continental mainland. It comprises England, Scotlan ...
, were carriers of ''C. jejuni''. It is also common in cattle, and although it is normally a harmless commensal
Commensalism is a long-term biological interaction (symbiosis) in which members of one species gain benefits while those of the other species neither benefit nor are harmed. This is in contrast with mutualism, in which both organisms benefit fro ...
of the gastrointestinal tract in these animals, it can cause campylobacteriosis in calves. It has also been isolated from wombat and kangaroo
Kangaroos are four marsupials from the family Macropodidae (macropods, meaning "large foot"). In common use the term is used to describe the largest species from this family, the red kangaroo, as well as the antilopine kangaroo, eastern ...
feces, being a cause of bushwalkers' diarrhea
Diarrhea, also spelled diarrhoea, is the condition of having at least three loose, liquid, or watery bowel movements each day. It often lasts for a few days and can result in dehydration due to fluid loss. Signs of dehydration often begin w ...
. Contaminated drinking water and unpasteurized milk provide an efficient means for distribution. Contaminated food is a major source of isolated infections, with incorrectly prepared meat and poultry as the primary source of the bacteria. Moreover, surveys show that 20 to 100% of retail chickens are contaminated. This is not overly surprising, since many healthy chickens carry these bacteria in their intestinal tracts and often in high concentrations, up to 108 cfu/g. The bacteria contaminate the carcasses due to poor hygiene during the slaughter process. Several studies have shown increased concentrations of ''Campylobacter'' on the carcasses after the evisceration. Studies have investigated the chicken microbiome to understand how, why and when ''Campylobacter'' appears within the chicken gut. The impact of Industrial system production systems on the chicken gut microbiome and ''Campylobacter'' prevalence have also been investigated.
Raw milk is also a source of infections. The bacteria are often carried by healthy cattle and by flies on farms. Unchlorinated water may also be a source of infections. However, properly cooking chicken, pasteurizing milk, and chlorinating drinking water kill the bacteria. ''Campylobacter'' is not, in contrast to ''Salmonella'', transmitted vertically into eggs and therefore humans do not get infected by consuming eggs.
Possible complications
Local complications of ''Campylobacter'' infections occur as a result of direct spread from the gastrointestinal tract and can includecholecystitis
Cholecystitis is inflammation of the gallbladder. Symptoms include right upper abdominal pain, pain in the right shoulder, nausea, vomiting, and occasionally fever. Often gallbladder attacks (biliary colic) precede acute cholecystitis. The pai ...
, pancreatitis
Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic pancr ...
, peritonitis
Peritonitis is inflammation of the localized or generalized peritoneum, the lining of the inner wall of the abdomen and cover of the abdominal organs. Symptoms may include severe pain, swelling of the abdomen, fever, or weight loss. One part o ...
, and massive gastrointestinal hemorrhage
Gastrointestinal bleeding (GI bleed), also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may includ ...
. Extraintestinal manifestations of ''Campylobacter'' infection are quite rare and may include meningitis, endocarditis, septic arthritis, osteomyelitis, and neonatal sepsis. Bacteremia is detected in <1% of patients with ''Campylobacter'' enteritis and is most likely to occur in patients who are immunocompromised or among the very young or very old. Transient bacteremia in immunocompetent hosts with ''C. jejuni'' enteritis may be more common, but not detected because most strains are rapidly cleared by the killing action of normal human serum and because blood cultures are not routinely performed for patients with acute gastrointestinal illness.
Serious systemic illness caused by ''Campylobacter'' infection rarely occurs, but can lead to sepsis and death. The case-fatality rate for ''Campylobacter'' infection is 0.05 per 1000 infections. For instance, one major possible complication that ''C. jejuni'' can cause is Guillain–Barré syndrome, which induces neuromuscular paralysis in a sizeable percentage of those who suffer from it. Over time, the paralysis is typically reversible to some extent; nonetheless, about 20% of patients with GBS are left disabled, and around 5% die. Another chronic condition that may be associated with ''Campylobacter'' infection is reactive arthritis
Reactive arthritis, also known as Reiter's syndrome, is a form of inflammatory arthritis that develops in response to an infection in another part of the body (cross-reactivity). Coming into contact with bacteria and developing an infection can t ...
. Reactive arthritis is a complication strongly associated with a particular genetic make-up. That is, persons who have the human leukocyte antigen B27 (HLA-B27) are most susceptible. Most often, the symptoms of reactive arthritis will occur up to several weeks after infection.
Epidemiology
Frequency
United States
An estimated 2 million cases of ''Campylobacter'' enteritis occur annually, accounting for 5–7% of cases of gastroenteritis. ''Campylobacter'' organisms have a large animal reservoir, with up to 100% of poultry, including chickens, turkeys, and waterfowl, having asymptomatic intestinal infections. The major reservoirs of ''C. fetus'' are cattle and sheep. Nonetheless, the incidence of ''Campylobacter'' infections has been declining. Changes in the incidence of culture-confirmed ''Campylobacter'' infections have been monitored by the Foodborne Diseases Active Surveillance Network (FoodNet) since 1996. In 2010, ''Campylobacter'' incidence showed a 27% decrease compared with 1996–1998. In 2010, the incidence was 13.6 cases per 100,000 population, and this did not change significantly compared with 2006–2008.International
''Campylbacter jejuni'' infections are extremely common worldwide, although exact figures are not available. New Zealand reported the highest national campylobacteriosis rate, which peaked in May 2006 at 400 per 100,000 population.Sex
''Campylobacter'' is more frequently isolated in males than females, and homosexual men appear to have a higher risk of infection by atypical ''Campylobacter''-related species such as '' Helicobacter cinaedi'' and '' Helicobacter fennelliae''.Age
''Campylobacter'' infections can occur in all age groups. Studies show a peak incidence in children younger than 1 year and in people aged 15–29 years. The age-specific attack rate is highest in young children. In the United States, the highest incidence of ''Campylobacter'' infection in 2010 was in children younger than 5 years and was 24.4 cases per 100,000 population, However, the rate of fecal cultures positive for ''Campylobacter'' species is greatest in adults and older children.Treatment
Patients with ''Campylobacter'' infection should drink plenty of fluids as long as the diarrhea lasts to maintain hydration. Patients should also get rest. If he or she cannot drink enough fluids to prevent dehydration or if the symptoms are severe, medical help is indicated. In more severe cases, certain antibiotics can be used and can shorten the duration of symptoms if given early in the illness. Moreover, maintenance of electrolyte balance, not antibiotic treatment, is the cornerstone of treatment for ''Campylobacter'' enteritis. Indeed, most patients with this infection have a self-limited illness and do not require antibiotics at all. Nevertheless, antibiotics should be used in specific clinical circumstances. These include high fevers, bloody stools, prolonged illness (symptoms that last >1 week), pregnancy, infection with HIV, and other immunocompromised states.Prevention
Some simple food-handling practices can help prevent ''Campylobacter'' infections. * Cook all poultry products thoroughly. Make sure that the meat is cooked throughout (no longer pink) and any juices run clear. All poultry should be cooked to reach a minimum internal temperature of . * Wash hands with soap before preparing food. * Wash hands with soap after handling raw foods of animal origin and before touching anything else. * Prevent cross-contamination in the kitchen by using separate cutting boards for foods of animal origin and other foods and by thoroughly cleaning all cutting boards, countertops, and utensils with soap and hot water after preparing raw food of animal origin. * Do not drink unpasteurized milk or untreated surface water. * Make sure that people with diarrhea, especially children, wash their hands carefully and frequently with soap to reduce the risk of spreading the infection. * Wash hands with soap after contact with pet feces.Genome
The genome of ''C. jejuni'' strain NCTC11168 was published in 2000, revealing 1,641,481 base pairs (30.6% G+C) predicted to encode 1,654protein
Proteins are large biomolecules and macromolecules that comprise one or more long chains of amino acid residues. Proteins perform a vast array of functions within organisms, including catalysing metabolic reactions, DNA replication, res ...
s and 54 stable RNA species. The genome is unusual in that virtually no insertion sequence Insertion element (also known as an IS, an insertion sequence element, or an IS element) is a short DNA sequence that acts as a simple transposable element. Insertion sequences have two major characteristics: they are small relative to other transp ...
s or phage
A bacteriophage (), also known informally as a ''phage'' (), is a duplodnaviria virus that infects and replicates within bacteria and archaea. The term was derived from "bacteria" and the Greek φαγεῖν ('), meaning "to devour". Bacter ...
-associated sequences and very few repeat sequences are found. One of the most striking findings in the genome was the presence of hypervariable sequences. These short homopolymer
A polymer (; Greek '' poly-'', "many" + '' -mer'', "part")
is a substance or material consisting of very large molecules called macromolecules, composed of many repeating subunits. Due to their broad spectrum of properties, both synthetic an ...
ic runs of nucleotide
Nucleotides are organic molecules consisting of a nucleoside and a phosphate. They serve as monomeric units of the nucleic acid polymers – deoxyribonucleic acid (DNA) and ribonucleic acid (RNA), both of which are essential biomolecule ...
s were commonly found in genes encoding the biosynthesis or modification of surface structures, or in closely linked genes of unknown function. The apparently high rate of variation of these homopolymeric tracts may be important in the survival strategy of ''C. jejuni''. The genome was re-annotated in 2007 updating 18.2% of product functions. Analysis also predicted the first pathogenicity island in ''C. jejuni'' amongst select strains, harbouring the bacteria's Type VI secretion system and putative cognate effectors.
Initial transposon mutagenesis screens revealed 195 essential genes, although this number is likely to go up with additional analysis.
Natural genetic transformation
''C. jejuni'' is naturally competent for genetic transformation. Natural genetic transformation is a sexual process involving DNA transfer from one bacterium to another through the intervening medium, and the integration of the donor sequence into the recipient genome byhomologous recombination
Homologous recombination is a type of genetic recombination in which genetic information is exchanged between two similar or identical molecules of double-stranded or single-stranded nucleic acids (usually DNA as in cellular organisms but may ...
. ''C. jejuni'' freely takes up foreign DNA harboring genetic information responsible for antibiotic resistance. Antibiotic resistance genes are more frequently transferred in biofilms than between planktonic cells (single cells that float in liquid media).
DNA repair
In the intestinal environment, bile functions as a defensive barrier against colonization by ''C. jejuni''.Gourley CR, Negretti NM, Konkel ME. The food-borne pathogen Campylobacter jejuni depends on the AddAB DNA repair system to defend against bile in the intestinal environment. Sci Rep. 2017 Oct 31;7(1):14777. doi: 10.1038/s41598-017-14646-9. PMID: 29089630; PMCID: PMC5665897 When ''C. jejuni'' is grown in a medium containing the bile aciddeoxycholic acid
Deoxycholic acid is a bile acid. Deoxycholic acid is one of the secondary bile acids, which are metabolic byproducts of intestinal bacteria. The two primary bile acids secreted by the liver are cholic acid and chenodeoxycholic acid. Bacteria ...
, a component of bile, the DNA of ''C. jejuni'' is damaged by a process involving oxidative stress
Oxidative stress reflects an imbalance between the systemic manifestation of reactive oxygen species and a biological system's ability to readily detoxify the reactive intermediates or to repair the resulting damage. Disturbances in the normal ...
. To survive, ''C. jejuni'' cells repair this DNA damage by a system employing proteins AddA and AddB that are needed for repair of DNA double-strand breaks.
Laboratory characteristics
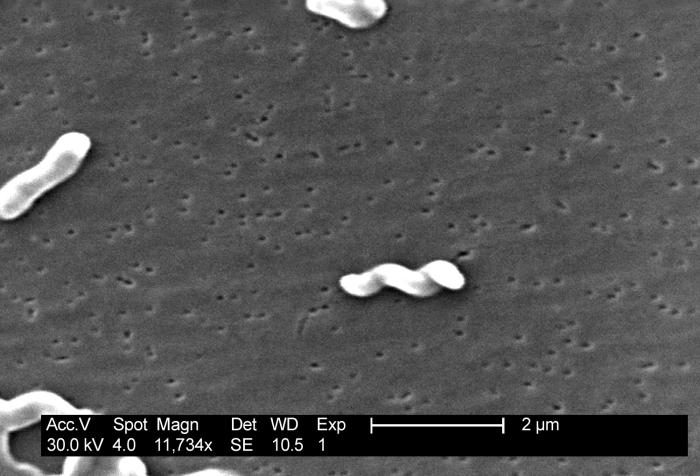 Under light microscopy, ''C. jejuni'' has a characteristic "sea-gull" shape as a consequence of its helical form. ''Campylobacter'' is grown on specially selective "CAMP"
Under light microscopy, ''C. jejuni'' has a characteristic "sea-gull" shape as a consequence of its helical form. ''Campylobacter'' is grown on specially selective "CAMP" agar plate
An agar plate is a Petri dish that contains a growth medium solidified with agar, used to culture microorganisms. Sometimes selective compounds are added to influence growth, such as antibiotics.
Individual microorganisms placed on the plate wil ...
s at 42 °C, the normal avian body temperature, rather than at 37 °C, the temperature at which most other pathogenic bacteria are grown. Since the colonies are oxidase positive, they usually only grow in scanty amounts on the plates. Microaerophilic
A microaerophile is a microorganism that requires environments containing lower levels of dioxygen than that are present in the atmosphere (i.e. < 21% O2; typically 2–10% O2) for optimal growth. A more r ...
conditions are required for luxurious growth. A selective blood agar medium (Skirrow's medium) can be used. Greater selectivity can be gained with an infusion of a cocktail of antibiotics: vancomycin
Vancomycin is a glycopeptide antibiotic medication used to treat a number of bacterial infections. It is recommended intravenously as a treatment for complicated skin infections, bloodstream infections, endocarditis, bone and joint infections, ...
, polymixin-B, trimethoprim
Trimethoprim (TMP) is an antibiotic used mainly in the treatment of bladder infections. Other uses include for middle ear infections and travelers' diarrhea. With sulfamethoxazole or dapsone it may be used for ''Pneumocystis'' pneumonia in peo ...
, and actidione ( reston's agar, and growth under microaerophilic
A microaerophile is a microorganism that requires environments containing lower levels of dioxygen than that are present in the atmosphere (i.e. < 21% O2; typically 2–10% O2) for optimal growth. A more r ...
conditions at 42 °C.
See also
* CampylobacteriosisReferences
External links
Campylobacter jejuni
genomes and related information a
PATRIC
a Bioinformatics Resource Center funded b
NIAID
* ttp://bacdive.dsmz.de/index.php?search=2121&submit=Search Type strain of ''Campylobacter jejuni'' at Bac''Dive'' - the Bacterial Diversity Metadatabase {{Authority control Campylobacterota Bacteria described in 1931