Aortic valve replacement on:
[Wikipedia]
[Google]
[Amazon]
Aortic valve replacement is a procedure whereby the failing

 Surgical aortic valve replacement is conventionally done through a
Surgical aortic valve replacement is conventionally done through a
The Society of Thoracic Surgeons – Aortic Valve
Aortic Valve Replacement Animation
{{Cardiac surgery Cardiology Cardiac surgery Implants (medicine) Prosthetics
aortic valve
The aortic valve is a valve in the heart of humans and most other animals, located between the left ventricle and the aorta. It is one of the four valves of the heart and one of the two semilunar valves, the other being the pulmonary valve. Th ...
of a patient's heart is replaced with an artificial heart valve
An artificial heart valve is a one-way valve implanted into a person's heart to replace a heart valve that is not functioning properly ( valvular heart disease). Artificial heart valves can be separated into three broad classes: mechanical he ...
. The aortic valve may need to be replaced because:
* The valve is leaky (aortic insufficiency
Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a conseq ...
, also known as aortic regurgitation
Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a cons ...
)
* The valve is narrowed and doesn't open fully (aortic stenosis
Aortic stenosis (AS or AoS) is the narrowing of the exit of the left ventricle of the heart (where the aorta begins), such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse ov ...
)
Current methods for aortic valve replacement include open-heart surgery
Cardiac surgery, or cardiovascular surgery, is surgery on the heart or great vessels performed by cardiac surgeons. It is often used to treat complications of ischemic heart disease (for example, with coronary artery bypass grafting); to corr ...
, termed ''minimally invasive cardiac surgery (MICS)'' or ''surgical aortic valve replacement'' (SAVR) and percutaneous or transcatheter aortic valve replacement (TAVR; also PAVR, PAVI, TAVI).
A competent practising cardiologist can evaluate whether a patient could benefit from heart valve repair
Heart valve repair is a cardiac surgery procedure, carried out to repair one or more faulty heart valves. In some valvular heart diseases repair where possible is preferable to valve replacement. A mechanical heart valve is a replacement valve ...
.
History
During the late 1940s and early 1950s, the first surgical approaches towards treating aortic valve stenosis had limited success. The first attempts were valvotomies, (i.e. cutting the valve while the heart is pumping). A ball valve prosthesis placed on thedescending thoracic aorta
The descending thoracic aorta is a part of the aorta located in the thorax. It is a continuation of the aortic arch. It is located within the posterior mediastinal cavity, but frequently bulges into the left pleural cavity. The descending thoraci ...
(heterotopically) was developed by Hufnagel, Harvey and others to address aortic stenosis, but had disastrous complications. Later, with the innovation of cardiopulmonary bypass, the ball valve prosthesis was placed orthotopically (i.e. in same place as the original aortic valve). This first generation of prosthetic valves was durable, but needed intense anti-coagulation, and cardiac hemodynamics were compromised. During the mid-1950s, a single-leaflet prosthesis was developed by Bahnson ''et al''. In early 1960, Ross and Barratt-Boyes used allografts. Tissue prosthetic valves were introduced in 1965 by Binet in Paris, but they degenerated quickly because the tissue was insufficiently preserved. Carpentier solved this problem by introducing glutaraldehyde-preserved stent-mounted porcine valves.
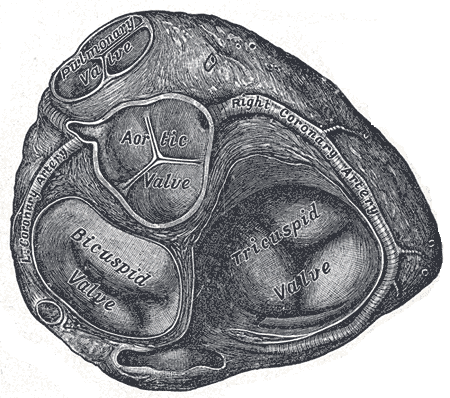
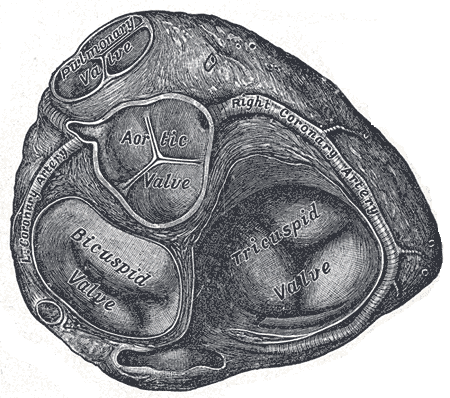
Anatomy, physiology and pathophysiology
The aortic valve is semilunar (half-moon shaped) with three cusps. It separates the heart from theaorta
The aorta ( ) is the main and largest artery in the human body, originating from the left ventricle of the heart and extending down to the abdomen, where it splits into two smaller arteries (the common iliac arteries). The aorta distributes o ...
. Each cusp is attached to the aortic wall creating a sinus; a Valsalva sinus. The origins of the two coronary arteries
The coronary arteries are the arterial blood vessels of coronary circulation, which transport oxygenated blood to the heart muscle. The heart requires a continuous supply of oxygen to function and survive, much like any other tissue or organ ...
are sited in two Valsalva sinuses, each named after the coronary artery they supply. Leaflets are separated by commissure
A commissure () is the location at which two objects abut or are joined. The term is used especially in the fields of anatomy and biology.
* The most common usage of the term refers to the brain's commissures, of which there are five. Such a commi ...
s. The posterior leaflet is in continuation with the anterior leaflet of the mitral valve (the tissue is called the aorto-mitral curtain). The aortic valve is opened during systole, the driving force for it to open is the difference in pressure between the contracting left ventricle of the heart and the aorta. During cardiac diastole (when the heart chamber gets bigger) the aortic valve closes.
Aortic stenosis most commonly is the result of calcification of the cusps. Other reasons for stenosis are the bicuspid valve
The mitral valve (), also known as the bicuspid valve or left atrioventricular valve, is one of the four heart valves. It has two cusps or flaps and lies between the left atrium and the left ventricle of the heart. The heart valves are all one-w ...
(some patients have only two cusps at the aortic valve instead of the usual three) and rheumatic aortic stenosis (now rare in the West). Obstruction at the level of the aortic valve causes increased pressure within the heart's left ventricle. This can lead to hypertrophy and ultimately dysfunction of the heart. While x-ray and ECG might indicate aortic stenosis, echocardiography is the diagnostic procedure of choice. US findings also help in grading the severity of the disease. In cases of symptomatic severe aortic stenosis, AVR is warranted. In cases of asymptomatic but severe aortic stenosis, more factors should be taken into consideration.
Aortic regurgitation, on the other hand, has many causes: degeneration of the cusps, endocarditis, bicuspid aortic valve, aortic root dilatation, trauma, connective tissue disorders such as Marfan syndrome or Ehlers-Danlos lead to imperfect closure of the valve during diastole, hence the blood is returning from the aorta towards the left ventricle of the heart. Acute aortic regurgitation (caused by endocarditis, aortic dissection or trauma) ends up in pulmonary edema, because of the acute increase in left ventricle (LVEDP) that does not have time to adjust to the regurgitation. Chronic regurgitation, by contrast, gives the heart time to change shape, resulting in ''eccentric hypertrophy'', which has disastrous effects on the myocardium. Ultrasound is here also the best diagnostic mobility, either it is transthoracic or transesophageal.
Indications for surgery
Guidelines for aortic valve replacement
As long-term data on the survival and quality of life of people following valve replacement have become available, evidence-based guidelines for aortic valve replacement have been developed. These help healthcare professionals decide when aortic valve replacement is the best option for a patient. Two widely accepted sets of guidelines used by surgeons and cardiologists are the American Heart Association and American College of Cardiology Guidelines for the Management of Patients with Valvular Heart Disease, and the European Society of Cardiology and the European Association for Cardio‑Thoracic Surgery Guidelines for the management of valvular heart disease.Aortic stenosis
Aortic stenosis
Aortic stenosis (AS or AoS) is the narrowing of the exit of the left ventricle of the heart (where the aorta begins), such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse ov ...
is treated with aortic valve replacement in order to avoid angina
Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.
Angina is typically the result of obstr ...
, syncope, or congestive heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, ...
. Individuals with severe aortic stenosis are candidates for aortic valve replacement once they develop symptoms or when their heart function is impacted. Some people with asymptomatic aortic stenosis may also be candidates for aortic valve replacement, especially if symptoms appear during exercise testing. Patients with moderate aortic valve stenosis who need another type of cardiac surgery (i.e. coronary artery bypass surgery
Coronary artery bypass surgery, also known as coronary artery bypass graft (CABG, pronounced "cabbage") is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pai ...
) should also have their valve addressed by the surgical team if echocardiography
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart.
It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Echocardiography has become routinely used in ...
unveils significant heart problems.
Low gradient aortic stenosis with concomitant left ventricular dysfunction poses a significant question to the anesthesiologist and the patient. Stress echocardiography (i.e. with dobutamine infusion) can help determine if the ventricle is dysfunctional because of aortic stenosis, or because the myocardium lost its ability to contract.
Aortic insufficiency
Many people withaortic insufficiency
Aortic regurgitation (AR), also known as aortic insufficiency (AI), is the leaking of the aortic valve of the heart that causes blood to flow in the reverse direction during ventricular diastole, from the aorta into the left ventricle. As a conseq ...
often do not develop symptoms until they have had the condition for many years. Aortic valve replacement is indicated for symptoms such as shortness of breath
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing di ...
, and in cases where the heart has begun to enlarge (dilate) from pumping the increased volume of blood that leaks back through the valve.
Types of valves
There are two basic types of replacement heart valve: tissue (bioprosthetic) valves and mechanical valves.Tissue valves
Tissue heart valves are usually made from animal tissue (heterografts) mounted on a metal or polymer support. Bovine (cow) tissue is most commonly used, but some are made from porcine (pig) tissue. The tissue is treated to prevent rejection and calcification (where calcium builds up on the replacement valve and stops it working properly). Occasionally, alternatives to animal tissue valves are used: aortichomograft
Allotransplant (''allo-'' meaning "other" in Greek) is the transplantation of cells, tissues, or organs to a recipient from a genetically non-identical donor of the same species. The transplant is called an allograft, allogeneic transplant, ...
s and pulmonary autograft
Autotransplantation is the transplantation of organs, tissues, or even particular proteins from one part of the body to another in the same person ('' auto-'' meaning "self" in Greek).
The autologous tissue (also called autogenous, autogen ...
s. An aortic homograft is an aortic valve from a human donor, retrieved either after their death or from their heart if they are undergoing a heart transplant. A pulmonary autograft, also known as the Ross procedure is where the aortic valve is removed and replaced with the patient's own pulmonary valve
The pulmonary valve (sometimes referred to as the pulmonic valve) is a valve of the heart that lies between the right ventricle and the pulmonary artery and has three cusps. It is one of the four valves of the heart and one of the two semilunar v ...
(the valve between the right ventricle and the pulmonary artery). A pulmonary homograft (a pulmonary valve taken from a cadaver) is then used to replace the patient's own pulmonary valve. This procedure was first performed in 1967 and is used primarily in children, as it allows the patient's own pulmonary valve (now in the aortic position) to grow with the child.
Tissue valves can last 10–20 years. However, they tend to deteriorate more quickly in younger patients. New ways of preserving the tissue for longer are being investigated. One such preservation treatment is now being used in a commercially available tissue heart valve. In sheep and rabbit studies, the tissue (called RESILIA tissue) had less calcification
Calcification is the accumulation of calcium salts in a body tissue. It normally occurs in the formation of bone, but calcium can be deposited abnormally in soft tissue,Miller, J. D. Cardiovascular calcification: Orbicular origins. ''Nature M ...
than control tissue. However, long-term durability data in patients are not yet available.
Stented and stentless tissue valves are available. Stented valves come in sizes from 19 mm to 29 mm. Stentless valves are directly sutured at the aortic root. The major advantage of stentless valves is that they limit patient–prosthesis mismatch (when the area of the prosthetic valve is too small in relation to the size of the patient, increasing the pressure inside the valve) and can be helpful when dealing with small aortic root. However, stentless valves take more time than stented valves to implant.
Mechanical valves
Mechanical valves are made from synthetic materials, such as titanium orpyrolytic carbon
Pyrolytic carbon is a material similar to graphite, but with some covalent bonding between its graphene sheets as a result of imperfections in its production.
Pyrolytic carbon is man-made and is thought not to be found in nature.Ratner, Buddy D. ...
. They are more durable than tissue valves, typically lasting 20–30 years. However, the risk of blood clots forming is higher with mechanical valves than with tissue valves. As a result, people with mechanical heart valves must take anticoagulant (blood-thinning) drugs, such as warfarin
Warfarin, sold under the brand name Coumadin among others, is a medication that is used as an anticoagulant (blood thinner). It is commonly used to prevent blood clots such as deep vein thrombosis and pulmonary embolism, and to prevent st ...
, for the rest of their lives, making them more prone to bleeding. The sound of the valve can sometimes be heard, often as clicks, and can be disturbing.
Valve selection
Valve choice is a balance between the lower durability of tissue valves and the increased risk of blood clots and bleeding with mechanical valves. Guidelines suggest that patient age, lifestyle and medical history should all be considered when choosing a valve. Tissue valves deteriorate more rapidly in young patients and during pregnancy, but they are preferable for women who wish to have children because pregnancy increases the risk of blood clots. Typically, a mechanical valve is considered for patients under 60 years old, while a tissue valve is considered for patients over the age of 65 years.Surgical replacement
 Surgical aortic valve replacement is conventionally done through a
Surgical aortic valve replacement is conventionally done through a median sternotomy
Median sternotomy is a type of surgical procedure in which a vertical inline incision is made along the sternum, after which the sternum itself is divided using a sternal saw. This procedure provides access to the heart and lungs for surgical pro ...
, meaning the incision is made by cutting through the breastbone (sternum
The sternum or breastbone is a long flat bone located in the central part of the chest. It connects to the ribs via cartilage and forms the front of the rib cage, thus helping to protect the heart, lungs, and major blood vessels from injury. Sha ...
). Once the protective membrane around the heart (pericardium
The pericardium, also called pericardial sac, is a double-walled sac containing the heart and the roots of the great vessels. It has two layers, an outer layer made of strong connective tissue (fibrous pericardium), and an inner layer made ...
) has been opened, the patient is cannulated (aortic cannulation by a cannula placed on the aorta
The aorta ( ) is the main and largest artery in the human body, originating from the left ventricle of the heart and extending down to the abdomen, where it splits into two smaller arteries (the common iliac arteries). The aorta distributes o ...
and a venous canulation by a single atrial venous cannula inserted through the right atrium). The patient is put on a cardiopulmonary bypass
Cardiopulmonary bypass (CPB) is a technique in which a machine temporarily takes over the function of the heart and lungs during surgery, maintaining the circulation of blood and oxygen to the body. The CPB pump itself is often referred to as a ...
machine, also known as the heart–lung machine. This machine breathes for the patient and pumps their blood around their body while the surgeon replaces the heart valve.
Once on cardiopulmonary bypass, the patient's heart is stopped (cardioplegia
Cardioplegia is intentional and temporary cessation of cardiac activity, primarily for cardiac surgery.
Overview
The word ''cardioplegia'' combines the Greek ''cardio'' meaning the "heart", and ''plegia'' "paralysis". Technically, this means a ...
). This can be done with a Y-type cardioplegic infusion catheter placed on the aorta, de-aired and connected to the cardiopulmonary bypass machine. Alternatively, a retrograde cardioplegic cannula can be inserted at the coronary sinus. Some surgeons also opt to place a vent in the left ventricle through the right superior pulmonary vein, because this helps to prevent left ventricular distention before and after cardiac arrest. When the set-up is ready, the aorta is clamped shut with a cross-clamp to stop blood pumping through the heart and cardioplegia is infused. The surgeon incises the aorta a few milometers above the sinotubular junction (just above the coronary ostia, where the coronary arteries join the aorta) – a process known as aortotomy. After this, cardioplegia is delivered directly through the ostia.
The heart is now still and the surgeon removes the patient's diseased aortic valve. The cusps of the aortic valve are excised, and calcium is removed (debrided) from the aortic annulus. The surgeon measures the size of the aortic annulus and fits a mechanical or tissue valve of the appropriate size. Usually the valve is fixed in place with sutures, although some sutureless valves are available. If the patient's aortic root is very small, the sutures are placed outside of the aortic root instead of at the annulus, to gain some extra space.
Once the valve is in place and the aorta has been closed, patient is placed in a Trendelenburg position
In the Trendelenburg position, the body is lain supine, or flat on the back on a 15–30 degree incline with the feet elevated above the head. The reverse Trendelenburg position, similarly, places the body supine on an incline but with the head ...
and the heart is de-aired and restarted. The patient is taken off the cardiopulmonary bypass machine. Transesophageal echocardiogram
A transesophageal echocardiogram, or TEE (TOE in the United Kingdom and other countries such as Australia and New Zealand, reflecting the British English spelling ''transoesophageal''), is an alternative way to perform an echocardiogram. A speci ...
(an ultrasound of the heart done through the esophagus) can be used to verify that the new valve is functioning properly. Pacing wires are usually put in place, so that the heart can be manually controlled should any complications arise after surgery. Drainage tubes are also inserted, to drain fluids from the chest. These are usually removed within 36 hours, while the pacing wires are generally left in place until right before the patient is discharged from the hospital.
Hospital stay and recovery time
After surgical aortic valve replacement, the patient will usually stay in anintensive care unit
220px, Intensive care unit
An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensi ...
for 12–36 hours. Unless complications arise, the patient is then able to go home after approximately four to seven days. Common complications include disturbances to the heart's rhythm (heart block
Heart block (HB) is a disorder in the heart's rhythm due to a fault in the natural pacemaker. This is caused by an obstruction – a block – in the electrical conduction system of the heart. Sometimes a disorder can be inherited. Despite the se ...
), which typically require the permanent insertion of a cardiac pacemaker
350px, Image showing the cardiac pacemaker or SA node, the primary pacemaker within the electrical_conduction_system_of_the_heart">SA_node,_the_primary_pacemaker_within_the_electrical_conduction_system_of_the_heart.
The_muscle_contraction.htm ...
.
Recovery from aortic valve replacement takes about three months if the patient is in good health. Patients are advised not to lift anything heavier than 10 lbs for several weeks, and not to do any heavy lifting for 4–6 months after surgery to avoid damaging their breastbone. Often patients will be referred to participate in cardiopulmonary rehabilitation
Cardiac rehabilitation (CR) is defined by the World Health Organization (WHO) as "''The sum of activity and interventions required to ensure the best possible physical, mental, and social conditions so that patients with chronic or post-acute cardi ...
, which optimizes recovery and physical function in patients with recent cardiac surgeries. This can be done in an outpatient setting.
Outcomes
Surgery usually relieves the aortic disease symptoms that led the patient to the operating room. The survival curve of patients who undergo aortic valve replacements is slightly inferior to the curve of their corresponding healthy same-aged same sex population. Pre-operative severe left ventricular hypertrophy is a contributing factor to morbidity. The risk of dying as a result of aortic valve replacement is estimated at 1–3%. Combining aortic valve replacement with coronary artery bypass grafting increases the risk of mortality. Older patients, as well as those who are frail and/or have other health problems (comorbidities
In medicine, comorbidity - from Latin morbus ("sickness"), co ("together"), -ity (as if - several sicknesses together) - is the presence of one or more additional conditions often co-occurring (that is, concomitant or concurrent) with a primary ...
), have a higher risk of experiencing complications. Possible problems include cardiac infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may tra ...
or failure, arrhythmia
Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adult ...
or heart block
Heart block (HB) is a disorder in the heart's rhythm due to a fault in the natural pacemaker. This is caused by an obstruction – a block – in the electrical conduction system of the heart. Sometimes a disorder can be inherited. Despite the se ...
typically requiring the permanent insertion of a cardiac pacemaker
350px, Image showing the cardiac pacemaker or SA node, the primary pacemaker within the electrical_conduction_system_of_the_heart">SA_node,_the_primary_pacemaker_within_the_electrical_conduction_system_of_the_heart.
The_muscle_contraction.htm ...
, mediastinal bleeding, stroke
A stroke is a disease, medical condition in which poor cerebral circulation, blood flow to the brain causes cell death. There are two main types of stroke: brain ischemia, ischemic, due to lack of blood flow, and intracranial hemorrhage, hemorr ...
and infection. Late complications include endocarditis
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves. Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or the ...
, thromboembolic events (blood clots
A thrombus (plural thrombi), colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cr ...
), prosthetic valve dysfunction and paravalvular leak (blood flowing between the edge of the prosthetic valve and the cardiac tissue).
Patient–prosthesis mismatch
When dealing with a small aortic annulus, the surgeon might have to insert a prosthetic aortic valve of small size, with an orifice too small in relation to the size of the patient (patient–prosthesis mismatch). This increases the pressure of the blood flowing through the valve, and can lead to worse outcomes. Various techniques, imcluding stentless valves, have been utilized to avoid this problem.Less invasive procedures
Minimally invasive cardiac surgery
Since the late 1990s, some cardiac surgeons have been performing aortic valve replacement using an approach referred to as minimally invasive cardiac surgery (MICS). Using this approach, the surgeon replaces the valve through a smaller chest incision (6–10 cm) than that for a median sternotomy. MICS typically requires shorter recovery times, and produces less visible scarring.Transcatheter aortic valve replacement
Another alternative for many high-risk or elderly patients is transcatheter aortic valve replacement (TAVR, also known as TAVI, transcatheter aortic valve implantation). Rather than removing the existing valve, the new valve is pushed through it in a collapsed state. It is delivered to the site of the existing valve through a tube called a catheter, which may be inserted through the femoral artery in the thigh (transfemoral approach), or using a small incision in the chest and then through a large artery or the tip of the left ventricle (transapical approach). Fluoroscopy and transthoracic echocardiogram (TTE) are visual aids used to guide the process. Once the collapsed replacement valve is in place it is expanded, pushing the old valve's leaflets out of the way. Guidelines suggest TAVR for most patients aged 75 years and older, and surgical aortic valve replacement for most younger patients. Ultimately, the choice of treatment is based on many factors.See also
*Aortic valve repair
Aortic valve repair or aortic valve reconstruction is the reconstruction of both form and function of a dysfunctional aortic valve. Most frequently it is used for the treatment of aortic regurgitation. It can also become necessary for the treatme ...
* Artificial heart valve
An artificial heart valve is a one-way valve implanted into a person's heart to replace a heart valve that is not functioning properly ( valvular heart disease). Artificial heart valves can be separated into three broad classes: mechanical he ...
* Valvular heart disease
Valvular heart disease is any cardiovascular disease process involving one or more of the four valves of the heart (the aortic and mitral valves on the left side of heart and the pulmonic and tricuspid valves on the right side of heart). These ...
* Minimally invasive cardiac surgery
Minimally invasive cardiac surgery, also known as MICS CABG (Minimally Invasive Cardiac Surgery/Coronary Artery Bypass Grafting) or the McGinn technique is heart surgery performed through several small incisions instead of the traditional open-hear ...
* Pericardial heart valves
The pericardial heart valve was invented by Marian Ionescu, a British surgeon working at the General Infirmary in Leeds, England. He created this artificial bioprosthetic heart valve as a three-cusp structure made of chemically treated bovine peri ...
* Open aortic surgery
Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the repl ...
References
Sources
* * * * * * * *External links
The Society of Thoracic Surgeons – Aortic Valve
Aortic Valve Replacement Animation
{{Cardiac surgery Cardiology Cardiac surgery Implants (medicine) Prosthetics