Spinal anaesthesia on:
[Wikipedia]
[Google]
[Amazon]
Spinal anaesthesia (or spinal anesthesia), also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial
Effect of Glucose Concentration on the Intrathecal Spread of 0.5% Bupivacaine
/ref>
Transparent reality simulation of spinal anaesthesia
Various diagrams of needles for Lumbar puncture, Epidural, Spinal Anesthesia, etc
{{DEFAULTSORT:Spinal Anaesthesia Regional anesthesia
regional anaesthesia
Local anesthesia is any technique to induce the absence of sensation in a specific part of the body, generally for the aim of inducing local analgesia, that is, local insensitivity to pain, although other local senses may be affected as well. It ...
involving the injection
Injection or injected may refer to:
Science and technology
* Injective function, a mathematical function mapping distinct arguments to distinct values
* Injection (medicine), insertion of liquid into the body with a syringe
* Injection, in broadca ...
of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathic) blockade.
Administering analgesics (opioid, alpha2-adrenoreceptor agonist) in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation (incomplete analgesia), some autonomic blockade (parasympathetic plexi), but no sensory or motor block.
Locoregional analgesia, due to mainly the absence of motor and sympathic block may be preferred over locoregional anaesthesia in some postoperative care settings.
The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available (Whitacre, Sprotte, Gertie Marx and others).
Indications
Spinal anaesthesia is a commonly used technique, either on its own or in combination with sedation or general anaesthesia. It is most commonly used for surgeries below the umbilicus, however recently its uses have extended to some surgeries above the umbilicus as well as for postoperative analgesia. Procedures which use spinal anesthesia include: *Orthopaedic
Orthopedic surgery or orthopedics ( alternatively spelt orthopaedics), is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal ...
surgery on the pelvis, hip, femur
The femur (; ), or thigh bone, is the proximal bone of the hindlimb in tetrapod vertebrates. The head of the femur articulates with the acetabulum in the pelvic bone forming the hip joint, while the distal part of the femur articulates wit ...
, knee, tibia, and ankle
The ankle, or the talocrural region, or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joi ...
, including arthroplasty
Arthroplasty (literally " e-orming of joint") is an orthopedic surgical procedure where the articular surface of a musculoskeletal joint is replaced, remodeled, or realigned by osteotomy or some other procedure. It is an elective procedure that i ...
and joint replacement
Replacement arthroplasty (from Greek ''arthron'', joint, limb, articulate, + ''plassein'', to form, mould, forge, feign, make an image of), or joint replacement surgery, is a procedure of orthopedic surgery in which an arthritic or dysfunctional ...
* Vascular surgery on the legs
* Endovascular aortic aneurysm repair
* Hernia ( inguinal or epigastric
In anatomy, the epigastrium (or epigastric region) is the upper central region of the abdomen. It is located between the costal margins and the subcostal plane. Pain may be referred to the epigastrium from damage to structures derived from the f ...
)
* Haemorrhoidectomy
* Nephrectomy
A nephrectomy is the surgical removal of a kidney, performed to treat a number of kidney diseases including kidney cancer. It is also done to remove a normal healthy kidney from a living or deceased donor, which is part of a kidney transplant pr ...
and cystectomy
Cystectomy is a medical term for surgical removal of all or part of the urinary bladder. It may also be rarely used to refer to the removal of a cyst. The most common condition warranting removal of the urinary bladder is bladder cancer.
Two mai ...
in combination with general anaesthesia
* Transurethral resection of the prostate
Transurethral resection of the prostate (commonly known as a TURP, plural TURPs, and rarely as a transurethral prostatic resection, TUPR) is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, ...
and transurethral resection of bladder tumours
* Hysterectomy in different techniques used
* Caesarean sections
* Pain management during vaginal birth and delivery
* Urology cases
* Examinations under anaesthesia
Spinal anaesthesia is the technique of choice for Caesarean section as it avoids a general anaesthetic and the risk of failed intubation (which is probably a lot lower than the widely quoted 1 in 250 in pregnant women). It also means the mother is conscious and the partner is able to be present at the birth of the child. The post operative analgesia from intrathecal opioids in addition to non-steroidal anti-inflammatory drugs is also good.
Spinal anesthesia may be favored when the surgical site is amenable to spinal blockade for patients with severe respiratory disease such as COPD
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms include shortness of breath and a cough, which may or may not produce ...
as it avoids the potential respiratory consequences of intubation and ventilation. It may also be useful in patients where anatomical abnormalities may make tracheal intubation relatively difficult.
In pediatric patients, spinal anesthesia is particularly useful in children with difficult airways and those who are poor candidates for endotracheal anesthesia such as increased respiratory risks or presence of full stomach.
This can also be used to effectively treat and prevent pain following surgery, particularly thoracic, abdominal pelvic, and lower extremity orthopedic procedures.
Contraindications
Prior to receiving spinal anesthesia, it is important to provide a thorough medical evaluation to ensure there are no absolute contraindications and to minimize risks and complications. Although contraindications are rare, below are some of them: * Patient refusal * Local infection or sepsis at the site of injection * Bleeding disorders, thrombocytopaenia, or systemic anticoagulation (secondary to an increased risk of a spinalepidural hematoma
Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain (dura mater) and the skull. Often there is loss of consciousness following a head injury, a brief regaining of consciousness, and then loss of consciou ...
)
* Severe aortic stenosis
* Increased intracranial pressure
* Space occupying lesions of the brain
* Anatomical disorders of the spine such as scoliosis (although where pulmonary function is also impaired, spinal anaesthesia may be favored)
* Hypovolaemia e.g. following massive haemorrhage, including in obstetric patients
* Allergy
Relative Contraindication
* Ehlers Danlos Syndrome, or other disorders causing resistance to local anesthesia
Risks and complications
Complications of spinal anesthesia can result from the physiologic effects on the nervous system and can also be related to placement technique. Most of the common side effects are minor and are self-resolving or easily treatable while major complications can result in more serious and permanent neurological damage and rarely death. These symptoms can occur immediately after administration of the anesthetic or be delayed. Common and minor complications include: * Mildhypotension
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure (the top number) and the dia ...
* Bradycardia
* Nausea and vomiting
* Transient neurological symptoms (lower back pain with pain in the legs)
* Post-dural-puncture headache or post-spinal headache - Associated with the size and type of spinal needle used. A 2020 meta analysis recommended use of the 26G atraumatic spinal needle to lower the risk of PDPH - specifically, the Braun Atraucan 26G needle.
Serious and permanent complications are rare but are usually related to physiologic effects on the cardiovascular system and neurological system or when the injection has been unintentionally at the wrong site. The following are some major complications:
* Nerve injuries: Cauda equina
The cauda equina () is a bundle of spinal nerves and spinal nerve rootlets, consisting of the second through fifth lumbar nerve pairs, the first through fifth sacral nerve pairs, and the coccygeal nerve, all of which arise from the lumbar enlarg ...
syndrome, radiculopathy
* Cardiac arrest
Cardiac arrest is when the heart suddenly and unexpectedly stops beating. It is a medical emergency that, without immediate medical intervention, will result in sudden cardiac death within minutes. Cardiopulmonary resuscitation (CPR) and poss ...
* Severe hypotension
* Spinal epidural hematoma
Spinal extradural haematoma or spinal epidural hematoma (SEH) is bleeding into the epidural space in the spine. These may arise spontaneously (e.g. during childbirth), or as a rare complication of epidural anaesthesia or of surgery (such as lamin ...
, with or without subsequent neurological sequelae due to compression of the spinal nerves.
* Epidural abscess
* Infection (e.g. meningitis)
Technique
Regardless of theanaesthetic
An anesthetic (American English) or anaesthetic (British English; see spelling differences) is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two ...
agent (drug) used, the desired effect is to block the transmission of afferent nerve signals from peripheral nociceptor
A nociceptor ("pain receptor" from Latin ''nocere'' 'to harm or hurt') is a sensory neuron that responds to damaging or potentially damaging stimuli by sending "possible threat" signals to the spinal cord and the brain. The brain creates the sens ...
s. Sensory signals from the site are blocked, thereby eliminating pain. The degree of neuronal blockade depends on the amount and concentration of local anaesthetic used and the properties of the axon
An axon (from Greek ἄξων ''áxōn'', axis), or nerve fiber (or nerve fibre: see spelling differences), is a long, slender projection of a nerve cell, or neuron, in vertebrates, that typically conducts electrical impulses known as action p ...
. Thin unmyelinated C-fibres associated with pain are blocked first, while thick, heavily myelinated A-alpha motor neurons are blocked moderately. Heavily myelinated, small preganglionic sympathetic fibers are blocked last. The desired result is total numbness of the area. A pressure sensation is permissible and often occurs due to incomplete blockade of the thicker A-beta mechanoreceptors. This allows surgical procedures to be performed with no painful sensation to the person undergoing the procedure.
Some sedation is sometimes provided to help the patient relax and pass the time during the procedure, but with a successful spinal anaesthetic the surgery can be performed with the patient wide awake.
Anatomy
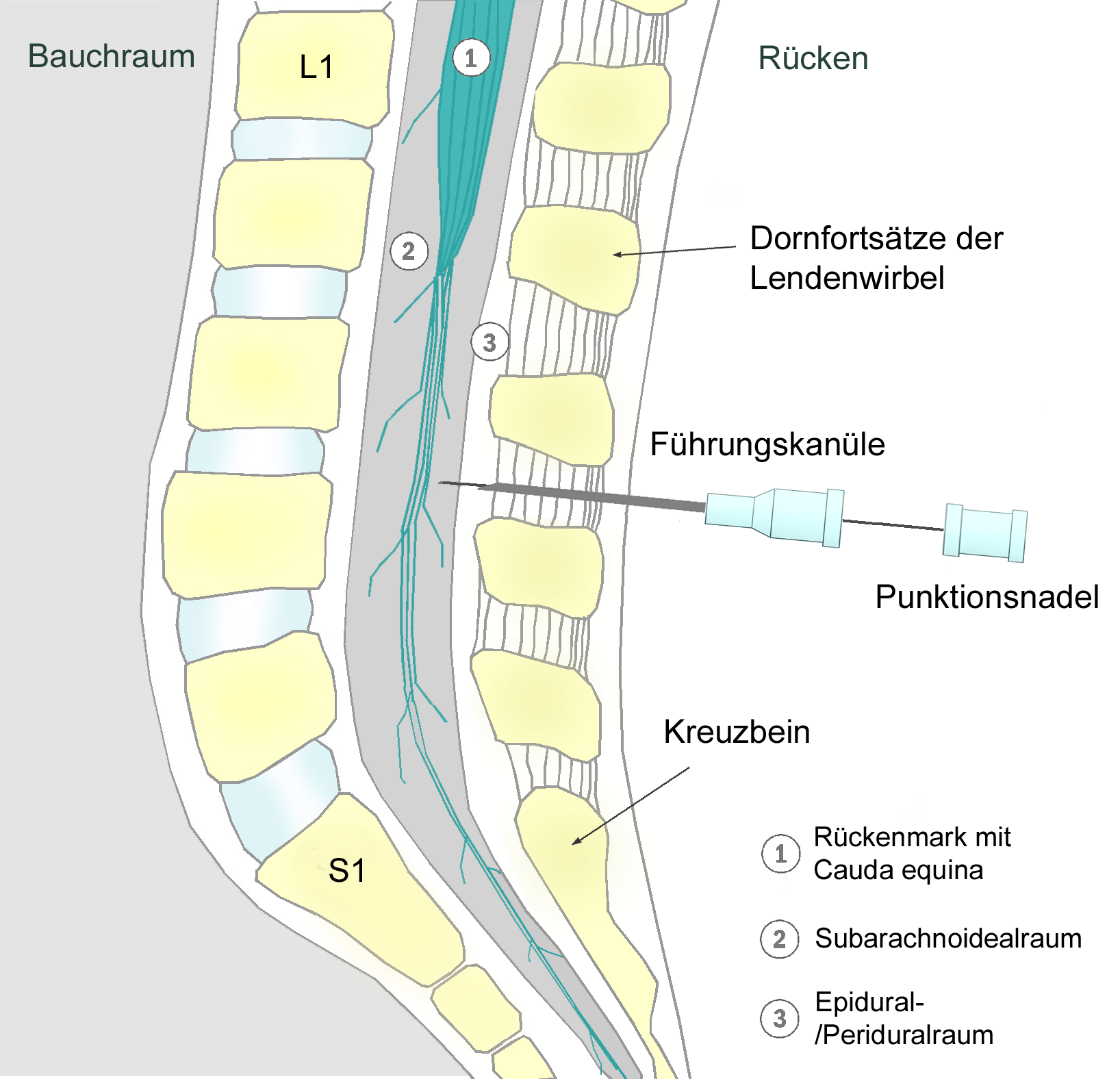
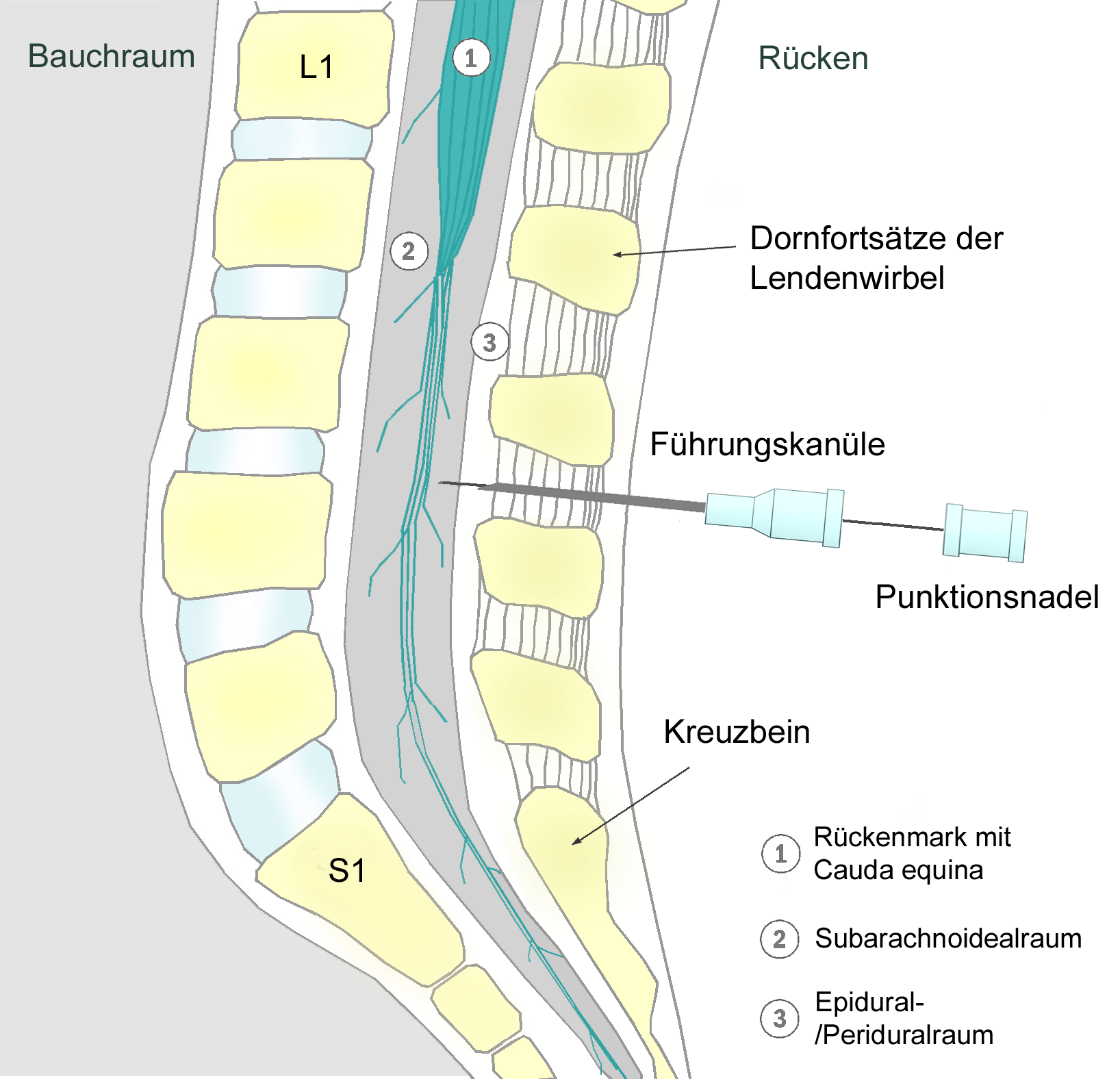
In spinal anesthesia, the needle is placed past the dura mater in subarachnoid space and between lumbar vertebrae. In order to reach this space, the needle must pierce through several layers of tissue and ligaments which include the supraspinous ligament, interspinous ligament, and ligamentum flavum. Because the spinal cord ( conus medullaris) is typically at the L1 or L2 level of the spine, the needle should be inserted below this between L3 and L4 space or L4 and L5 space in order to avoid injury to the spinal cord.Positioning
Patient positioning is essential to the success of the procedure and can affect how the anesthetic spreads following administration. There are 3 different positions which are used: sitting, lateral decubitus, and prone. The sitting and lateral decubitus positions are the most common. Sitting- The patient sits upright at the edge of the exam table with their back facing the provider and their legs hanging off the end of the table and feet resting on a stool. Patients should roll their shoulders and upper back forward. Lateral decubitus- In this position, the patient lays on their side with their back at the edge of the bed and facing the provider. The patient should curl their shoulder and legs and arch out their lower back. Prone- The patient is positioned face down and their back facing upwards in a jackknife position.Limitations
Spinal anaesthetics are typically limited to procedures involving most structures below the upperabdomen
The abdomen (colloquially called the belly, tummy, midriff, tucky or stomach) is the part of the body between the thorax (chest) and pelvis, in humans and in other vertebrates. The abdomen is the front part of the abdominal segment of the to ...
. To administer a spinal anaesthetic to higher levels may affect the ability to breathe by paralysing the intercostal respiratory muscles, or even the diaphragm in extreme cases (called a "high spinal", or a "total spinal", with which consciousness is lost), as well as the body's ability to control the heart rate
Heart rate (or pulse rate) is the frequency of the heartbeat measured by the number of contractions (beats) of the heart per minute (bpm). The heart rate can vary according to the body's physical needs, including the need to absorb oxygen and excr ...
via the cardiac accelerator fibres. Also, injection of spinal anaesthesia higher than the level of L1 can cause damage to the spinal cord, and is therefore usually not done.
Differences with epidural anaesthesia
Epidural anaesthesia
Epidural administration (from Ancient Greek ἐπί, , upon" + ''dura mater'') is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians an ...
is a technique whereby a local anaesthetic drug is injected through a catheter
In medicine, a catheter (/ˈkæθətər/) is a thin tubing (material), tube made from medical grade materials serving a broad range of functions. Catheters are medical devices that can be inserted in the body to treat diseases or perform a surgi ...
placed into the epidural space
In anatomy, the epidural space is the potential space between the dura mater and vertebrae (spine).
The anatomy term "epidural space" has its origin in the Ancient Greek language; , "on, upon" + dura mater also known as "epidural cavity", "e ...
. This technique is similar to spinal anaesthesia as both are neuraxial, and the two techniques may be easily confused with each other. Differences include:
* A spinal anaesthetic delivers drug to the subarachnoid space and into the cerebrospinal fluid, allowing it to act on the spinal cord directly. An epidural delivers drugs outside the dura (outside CSF), and has its main effect on nerve roots leaving the dura at the level of the epidural, rather than on the spinal cord itself.
* A spinal gives profound block of all motor and sensory function below the level of injection, whereas an epidural blocks a 'band' of nerve roots around the site of injection, with normal function above, and close-to-normal function below the levels blocked.
* The injected dose for an epidural is larger, being about 10–20 mL compared to 1.5–3.5 mL in a spinal.
* In an epidural, an indwelling catheter may be placed that allows for redosing injections, while a spinal is almost always a one-shot only. Therefore, spinal anaesthesia is more often used for shorter procedures relative to procedures which require epidural anaesthesia.
* The onset of analgesia is approximately 25–30 minutes in an epidural, while it is approximately 5 minutes in a spinal.
* An epidural often does not cause as significant a neuromuscular block as a spinal, unless specific local anaesthetics are also used which block motor fibres as readily as sensory nerve fibres.
* An epidural may be given at a cervical, thoracic
The thorax or chest is a part of the anatomy of humans, mammals, and other tetrapod animals located between the neck and the abdomen. In insects, crustaceans, and the extinct trilobites, the thorax is one of the three main divisions of the crea ...
, or lumbar site, while a spinal must be injected below L2 to avoid piercing the spinal cord.
Injected substances
Bupivacaine
Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease feeling in a specific area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural space. I ...
(Marcaine) is the local anaesthetic most commonly used, although lidocaine (lignocaine
Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lidoca ...
), tetracaine
Tetracaine, also known as amethocaine, is an ester local anesthetic used to numb the eyes, nose, or throat. It may also be applied to the skin before starting an intravenous (injection) to decrease pain from the procedure. Typically it is applied ...
, procaine
Procaine is a local anesthetic drug of the amino ester group. It is most commonly used in dental procedures to numb the area around a tooth and is also used to reduce the pain of intramuscular injection of penicillin. Owing to the ubiquity ...
, ropivacaine
Ropivacaine (rINN) is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed ''S''-enantiomer. Ropivacaine hydrochloride is commonly marketed by AstraZeneca under the brand na ...
, levobupivicaine, prilocaine
Prilocaine () is a local anesthetic of the amino amide type first prepared by Claes Tegner and Nils Löfgren. In its injectable form (trade name Citanest), it is often used in dentistry. It is also often combined with lidocaine as a topical ...
, or cinchocaine may also be used. Commonly opioids are added to improve the block and provide post-operative pain relief, examples include morphine
Morphine is a strong opiate that is found naturally in opium, a dark brown resin in poppies (''Papaver somniferum''). It is mainly used as a pain medication, and is also commonly used recreationally, or to make other illicit opioids. T ...
, fentanyl
Fentanyl, also spelled fentanil, is a very potent synthetic opioid used as a pain medication. Together with other drugs, fentanyl is used for anesthesia. It is also used illicitly as a recreational drug, sometimes mixed with heroin, cocain ...
, diamorphine, and buprenorphine
Buprenorphine is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection (intravenous and subcutaneous), as a skin patch (transdermal ...
. Non-opioids like clonidine or epinephrine may also be added to prolong the duration of analgesia (although Clonidine may cause hypotension). In the United Kingdom
The United Kingdom of Great Britain and Northern Ireland, commonly known as the United Kingdom (UK) or Britain, is a country in Europe, off the north-western coast of the European mainland, continental mainland. It comprises England, Scotlan ...
, since 2004 the National Institute for Health and Care Excellence
The National Institute for Health and Care Excellence (NICE) is an executive non-departmental public body of the Department of Health and Social Care in England that publishes guidelines in four areas:
* the use of health technologies withi ...
recommends that spinal anaesthesia for Caesarean section is supplemented with intrathecal diamorphine and this combination is now the modal form of anaesthesia for this indication in that country. In the United States Morphine is used for cesareans for the same purpose since diamorphine (heroin) is not used in clinical practice in the US.
Baricity refers to the density of a substance compared to the density of human cerebrospinal fluid. Baricity is used in anaesthesia to determine the manner in which a particular drug will spread in the intrathecal
Intrathecal administration is a route of administration for drugs via an injection into the spinal canal, or into the subarachnoid space so that it reaches the cerebrospinal fluid (CSF) and is useful in spinal anesthesia, chemotherapy, or pain ma ...
space. Usually, the hyperbaric, (for example, hyperbaric bupivacaine) is chosen, as its spread can be effectively and predictably controlled by the Anaesthesiologist, by tilting the patient. Hyperbaric solutions are made more dense by adding glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, u ...
to the mixture.
Baricity is one factor that determines the spread of a spinal anaesthetic but the effect of adding a solute to a solvent, i.e. solvation or dissolution
Dissolution may refer to:
Arts and entertainment Books
* ''Dissolution'' (''Forgotten Realms'' novel), a 2002 fantasy novel by Richard Lee Byers
* ''Dissolution'' (Sansom novel), a 2003 historical novel by C. J. Sansom Music
* Dissolution, in mu ...
, also has an effect on the spread of the spinal anaesthetic. In tetracaine
Tetracaine, also known as amethocaine, is an ester local anesthetic used to numb the eyes, nose, or throat. It may also be applied to the skin before starting an intravenous (injection) to decrease pain from the procedure. Typically it is applied ...
spinal anaesthesia, it was discovered that the rate of onset of analgesia was faster and the maximum level of analgesia was higher with a 10% glucose solution than with a 5% glucose spinal anaesthetic solution. Also, the amount of ephedrine
Ephedrine is a central nervous system (CNS) stimulant that is often used to prevent low blood pressure during anesthesia. It has also been used for asthma, narcolepsy, and obesity but is not the preferred treatment. It is of unclear benefit in ...
required was less in the patients who received the 5% glucose solution. In another study this time with 0.5% bupivacaine
Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease feeling in a specific area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural space. I ...
the mean maximum extent of sensory block was significantly higher with 8% glucose (T3.6) than with 0.83% glucose (T7.2) or 0.33% glucose (T9.5). Also the rate of onset of sensory block to T12 was fastest with solutions containing 8% glucose./ref>
History
The first spinal analgesia was administered in 1885 by James Leonard Corning (1855–1923), a neurologist in New York.Corning J. L. N.Y. Med. J. 1885, 42, 483 (reprinted in 'Classical File', ''Survey of Anesthesiology'' 1960, 4, 332) He was experimenting withcocaine
Cocaine (from , from , ultimately from Quechua: ''kúka'') is a central nervous system (CNS) stimulant mainly used recreationally for its euphoric effects. It is primarily obtained from the leaves of two Coca species native to South Ameri ...
on the spinal nerves
A spinal nerve is a mixed nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. In the human body there are 31 pairs of spinal nerves, one on each side of the vertebral column. These are grouped into the ...
of a dog when he accidentally pierced the dura mater
In neuroanatomy, dura mater is a thick membrane made of dense irregular connective tissue that surrounds the brain and spinal cord. It is the outermost of the three layers of membrane called the meninges that protect the central nervous system. ...
.
The first planned spinal anaesthesia for surgery on a human was administered by August Bier (1861–1949) on 16 August 1898, in Kiel
Kiel () is the capital and most populous city in the northern German state of Schleswig-Holstein, with a population of 246,243 (2021).
Kiel lies approximately north of Hamburg. Due to its geographic location in the southeast of the Jutland ...
, when he injected 3 ml of 0.5% cocaine solution into a 34-year-old labourer.Bier A. Versuche über Cocainisirung des Rückenmarkes. ''Deutsch Zeitschrift für Chirurgie'' 1899;51:361. (translated and reprinted in 'Classical File', ''Survey of Anesthesiology'' 1962, 6, 352) After using it on 6 patients, he and his assistant each injected cocaine into the other's spine. They recommended it for surgeries of legs, but gave it up due to the toxicity of cocaine.
See also
*Combined spinal and epidural anaesthesia
Combined spinal and epidural anaesthesia (CSE) is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. ...
* Epidural
Epidural administration (from Ancient Greek ἐπί, , upon" + ''dura mater'') is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians an ...
* Intrathecal administration
Intrathecal administration is a route of administration for drugs via an injection into the spinal canal, or into the subarachnoid space so that it reaches the cerebrospinal fluid (CSF) and is useful in spinal anesthesia, chemotherapy, or pain m ...
* Lumbar puncture
References
External links
Transparent reality simulation of spinal anaesthesia
Various diagrams of needles for Lumbar puncture, Epidural, Spinal Anesthesia, etc
{{DEFAULTSORT:Spinal Anaesthesia Regional anesthesia