A mental disorder, also referred to as a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. Such features may be persistent,
relapsing and remitting, or occur as single episodes. Many disorders have been described, with signs and symptoms that vary widely between specific disorders.
Such disorders may be
diagnosed by a
mental health professional, usually a
clinical psychologist
Clinical psychology is an integration of social science, theory, and clinical knowledge for the purpose of understanding, preventing, and relieving psychologically based distress or dysfunction and to promote subjective well-being and persona ...
or
psychiatrist
A psychiatrist is a physician who specializes in psychiatry, the branch of medicine devoted to the diagnosis, prevention, study, and treatment of mental disorders. Psychiatrists are physicians and evaluate patients to determine whether their sy ...
.
The
causes of mental disorders are often unclear. Theories may incorporate findings from a range of fields. Mental disorders are usually defined by a combination of how a person behaves, feels, perceives, or thinks.
[ This may be associated with particular regions or functions of the brain, often in a social context. A mental disorder is one aspect of ]mental health
Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. It likewise determines how an individual handles Stress (biology), stress, interpersonal relationships, and decision-maki ...
. Cultural and religious beliefs, as well as social norms, should be taken into account when making a diagnosis.community
A community is a social unit (a group of living things) with commonality such as place, norms, religion, values, customs, or identity. Communities may share a sense of place situated in a given geographical area (e.g. a country, village, t ...
, and assessments are carried out by mental health professionals such as psychiatrists, psychologists, psychiatric nurses and clinical social workers, using various methods such as psychometric tests
Psychometrics is a field of study within psychology concerned with the theory and technique of measurement. Psychometrics generally refers to specialized fields within psychology and education devoted to testing, measurement, assessment, and ...
but often relying on observation and questioning. Treatments are provided by various mental health professionals. Psychotherapy
Psychotherapy (also psychological therapy, talk therapy, or talking therapy) is the use of psychological methods, particularly when based on regular personal interaction, to help a person change behavior, increase happiness, and overcome pro ...
and psychiatric medication
A psychiatric or psychotropic medication is a psychoactive drug taken to exert an effect on the chemical makeup of the brain and nervous system. Thus, these medications are used to treat mental illnesses. These medications are typically made of ...
are two major treatment options. Other treatments include lifestyle changes, social interventions, peer support
Peer support occurs when people provide knowledge, experience, emotional, social or practical help to each other. It commonly refers to an initiative consisting of trained supporters (although it can be provided by peers without training), and can ...
, and self-help
Self-help or self-improvement is a self-guided improvement''APA Dictionary of Physicology'', 1st ed., Gary R. VandenBos, ed., Washington: American Psychological Association, 2007.—economically, intellectually, or emotionally—often with a subs ...
. In a minority of cases, there might be involuntary detention or treatment. Prevention programs have been shown to reduce depression.bipolar disorder
Bipolar disorder, previously known as manic depression, is a mental disorder characterized by periods of Depression (mood), depression and periods of abnormally elevated Mood (psychology), mood that last from days to weeks each. If the elevat ...
, which affects about 45 million, dementia
Dementia is a disorder which manifests as a set of related symptoms, which usually surfaces when the brain is damaged by injury or disease. The symptoms involve progressive impairments in memory, thinking, and behavior, which negatively affe ...
, which affects about 50 million, and schizophrenia
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations (typically hearing voices), delusions, and disorganized thinking. Other symptoms include social w ...
and other psychoses, which affects about 20 million people.Neurodevelopmental disorders
Neurodevelopmental disorders are a group of disorders that affect the development of the nervous system, leading to abnormal brain function which may affect emotion, learning ability, self-control, and memory. The effects of neurodevelopmental ...
include intellectual disability
Intellectual disability (ID), also known as general learning disability in the United Kingdom and formerly mental retardation, Rosa's Law, Pub. L. 111-256124 Stat. 2643(2010). is a generalized neurodevelopmental disorder characterized by signif ...
and autism spectrum disorders which usually arise in infancy or childhood.discrimination
Discrimination is the act of making unjustified distinctions between people based on the groups, classes, or other categories to which they belong or are perceived to belong. People may be discriminated on the basis of Racial discrimination, r ...
can add to the suffering and disability associated with mental disorders, leading to various social movements
A social movement is a loosely organized effort by a large group of people to achieve a particular goal, typically a social or political one. This may be to carry out a social change, or to resist or undo one. It is a type of group action and ma ...
attempting to increase understanding and challenge social exclusion
Social exclusion or social marginalisation is the social disadvantage and relegation to the fringe of society. It is a term that has been used widely in Europe and was first used in France in the late 20th century. It is used across discipline ...
.
Definition
The definition and classification of mental disorders are key issues for researchers as well as service providers and those who may be diagnosed. For a mental state to classify as a disorder, it generally needs to cause dysfunction. Most international clinical documents use the term mental "disorder", while "illness" is also common. It has been noted that using the term "mental" (i.e., of the mind
The mind is the set of faculties responsible for all mental phenomena. Often the term is also identified with the phenomena themselves. These faculties include thought, imagination, memory, will, and sensation. They are responsible for various m ...
) is not necessarily meant to imply separateness from the brain or body.
According to DSM-IV
The ''Diagnostic and Statistical Manual of Mental Disorders'' (DSM; latest edition: DSM-5-TR, published in March 2022) is a publication by the American Psychiatric Association (APA) for the classification of mental disorders using a common langu ...
, a mental disorder is a psychological syndrome
A syndrome is a set of medical signs and symptoms which are correlated with each other and often associated with a particular disease or disorder. The word derives from the Greek language, Greek σύνδρομον, meaning "concurrence". When a sy ...
or pattern that is associated with distress (e.g. via a painful symptom
Signs and symptoms are the observed or detectable signs, and experienced symptoms of an illness, injury, or condition. A sign for example may be a higher or lower temperature than normal, raised or lowered blood pressure or an abnormality showi ...
), disability
Disability is the experience of any condition that makes it more difficult for a person to do certain activities or have equitable access within a given society. Disabilities may be cognitive, developmental, intellectual, mental, physical, ...
(impairment in one or more important areas of functioning), increased risk of death, or causes a significant loss of autonomy; however, it excludes normal responses such as grief
Grief is the response to loss, particularly to the loss of someone or some living thing that has died, to which a bond or affection was formed. Although conventionally focused on the emotional response to loss, grief also has physical, cogniti ...
from loss of a loved one and also excludes deviant behavior for political, religious, or societal reasons not arising from a dysfunction in the individual.American Psychiatric Association
The American Psychiatric Association (APA) is the main professional organization of psychiatrists and trainee psychiatrists in the United States, and the largest psychiatric organization in the world. It has more than 37,000 members are invo ...
(APA) redefined mental disorders in the DSM-5
The ''Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition'' (DSM-5), is the 2013 update to the '' Diagnostic and Statistical Manual of Mental Disorders'', the taxonomic and diagnostic tool published by the American Psychiatri ...
as "a syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning." The final draft of ICD-11
The ICD-11 is the eleventh revision of the International Classification of Diseases (ICD). It replaces the ICD-10 as the global standard for recording health information and causes of death. The ICD is developed and annually updated by the World H ...
contains a very similar definition.
The terms "mental breakdown" or "nervous breakdown" may be used by the general population to mean a mental disorder.ICD-10
ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD), a medical classification list by the World Health Organization (WHO). It contains codes for diseases, signs and symptoms ...
, and are nearly absent from scientific literature regarding mental illness.[Hall-Flavin, Daniel K. (26 October 2016)]
"Nervous Breakdown"
''Mayo Clinic''
Archived copy
2 November 2021. Although "nervous breakdown" is not rigorously defined, surveys of laypersons suggest that the term refers to a specific acute time-limited reactive disorder, involving symptoms such as anxiety or depression, usually precipitated by external stressor
A stressor is a chemical or biological agent, environmental condition, external stimulus or an event seen as causing stress to an organism. Psychologically speaking, a stressor can be events or environments that individuals might consider demandin ...
s.
Nervous illness
Additionally to the concept of mental disorder, some people have argued for a return to the old-fashioned concept of nervous illness. In ''How Everyone Became Depressed: The Rise and Fall of the Nervous Breakdown'' (2013), Edward Shorter, a professor of psychiatry and the history of medicine, says:
Classifications
There are currently two widely established systems that classify mental disorders:
*''ICD-11 Chapter 06: Mental, behavioural or neurodevelopmental disorders'', part of the International Classification of Diseases
The International Classification of Diseases (ICD) is a globally used diagnostic tool for epidemiology, health management and clinical purposes. The ICD is maintained by the World Health Organization (WHO), which is the directing and coordinating ...
produced by the WHO (in effect since 1 January 2022).
*''Diagnostic and Statistical Manual of Mental Disorders
The ''Diagnostic and Statistical Manual of Mental Disorders'' (DSM; latest edition: DSM-5-TR, published in March 2022) is a publication by the American Psychiatric Association (APA) for the classification of mental disorders using a common langu ...
'' (DSM-5) produced by the APA since 1952.
Both of these list categories of disorder and provide standardized criteria for diagnosis. They have deliberately converged their codes in recent revisions so that the manuals are often broadly comparable, although significant differences remain. Other classification schemes may be used in non-western cultures, for example, the ''Chinese Classification of Mental Disorders The Chinese Classification of Mental Disorders (CCMD; ), published by the Chinese Society of Psychiatry (CSP), is a clinical guide used in China for the diagnosis of mental disorders. It is on a third version, the CCMD-3, written in Chinese and E ...
'', and other manuals may be used by those of alternative theoretical persuasions, such as the '' Psychodynamic Diagnostic Manual''. In general, mental disorders are classified separately from neurological disorders, learning disabilities or intellectual disability
Intellectual disability (ID), also known as general learning disability in the United Kingdom and formerly mental retardation, Rosa's Law, Pub. L. 111-256124 Stat. 2643(2010). is a generalized neurodevelopmental disorder characterized by signif ...
.
Unlike the DSM and ICD, some approaches are not based on identifying distinct categories of disorder using dichotomous symptom profiles intended to separate the abnormal from the normal. There is significant scientific debate about the relative merits of categorical versus such non-categorical (or hybrid) schemes, also known as continuum or dimensional models. A spectrum approach may incorporate elements of both.
In the scientific and academic literature on the definition or classification of mental disorder, one extreme argues that it is entirely a matter of value judgements (including of what is normal) while another proposes that it is or could be entirely objective and scientific
Science is a systematic endeavor that builds and organizes knowledge in the form of testable explanations and predictions about the universe.
Science may be as old as the human species, and some of the earliest archeological evidence for ...
(including by reference to statistical norms). Common hybrid views argue that the concept of mental disorder is objective even if only a "fuzzy prototype
A prototype is an early sample, model, or release of a product built to test a concept or process. It is a term used in a variety of contexts, including semantics, design, electronics, and software programming. A prototype is generally used to ...
" that can never be precisely defined, or conversely that the concept always involves a mixture of scientific facts and subjective value judgments. Although the diagnostic categories are referred to as 'disorders', they are presented as medical diseases, but are not validated in the same way as most medical diagnoses. Some neurologists argue that classification will only be reliable and valid when based on neurobiological features rather than clinical interview, while others suggest that the differing ideological and practical perspectives need to be better integrated.
Dimensional models
The high degree of comorbidity
In medicine, comorbidity - from Latin morbus ("sickness"), co ("together"), -ity (as if - several sicknesses together) - is the presence of one or more additional conditions often co-occurring (that is, concomitant or concurrent) with a primary ...
between disorders in categorical models such as the DSM and ICD have led some to propose dimensional models. Studying comorbidity between disorders have demonstrated two latent (unobserved) factors or dimensions in the structure of mental disorders that are thought to possibly reflect etiological processes. These two dimensions reflect a distinction between internalizing disorders, such as mood or anxiety symptoms, and externalizing disorders such as behavioral or substance use symptoms. A single general factor of psychopathology, similar to the g factor for intelligence, has been empirically supported. The ''p factor'' model supports the internalizing-externalizing distinction, but also supports the formation of a third dimension of thought disorders such as schizophrenia. Biological evidence also supports the validity of the internalizing-externalizing structure of mental disorders, with twin and adoption studies supporting heritable factors for externalizing and internalizing disorders. A leading dimensional model is the Hierarchical Taxonomy of Psychopathology.
Disorders
There are many different categories of mental disorder, and many different facets of human behavior and personality that can become disordered.[Gazzaniga, M.S., & Heatherton, T.F. (2006). ''Psychological Science''. New York: W.W. Norton & Company, Inc.]
Anxiety disorder
An anxiety disorder is anxiety
Anxiety is an emotion which is characterized by an unpleasant state of inner turmoil and includes feelings of dread over anticipated events. Anxiety is different than fear in that the former is defined as the anticipation of a future threat wh ...
or fear
Fear is an intensely unpleasant emotion in response to perceiving or recognizing a danger or threat. Fear causes physiological changes that may produce behavioral reactions such as mounting an aggressive response or fleeing the threat. Fear ...
that interferes with normal functioning may be classified as an anxiety disorder.phobia
A phobia is an anxiety disorder defined by a persistent and excessive fear of an object or situation. Phobias typically result in a rapid onset of fear and are usually present for more than six months. Those affected go to great lengths to avoi ...
s, generalized anxiety disorder, social anxiety disorder, panic disorder
Panic disorder is a mental and behavioral disorder, specifically an anxiety disorder characterized by reoccurring unexpected panic attacks. Panic attacks are sudden periods of intense fear that may include palpitations, sweating, shaking, short ...
, agoraphobia
Agoraphobia is a mental and behavioral disorder, specifically an anxiety disorder characterized by symptoms of anxiety in situations where the person perceives their environment to be unsafe with no easy way to escape. These situations can i ...
, obsessive-compulsive disorder and post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that can develop because of exposure to a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats o ...
.
Mood disorder
Other affective (emotion/mood) processes can also become disordered. Mood disorder involving unusually intense and sustained sadness, melancholia, or despair is known as major depression (also known as unipolar or clinical depression). Milder, but still prolonged depression, can be diagnosed as dysthymia
Dysthymia ( ), also known as persistent depressive disorder (PDD), is a mental and behavioral disorder, specifically a disorder primarily of mood, consisting of similar cognitive and physical problems as major depressive disorder, but with l ...
. Bipolar disorder
Bipolar disorder, previously known as manic depression, is a mental disorder characterized by periods of Depression (mood), depression and periods of abnormally elevated Mood (psychology), mood that last from days to weeks each. If the elevat ...
(also known as manic depression) involves abnormally "high" or pressured mood states, known as mania
Mania, also known as manic syndrome, is a mental and behavioral disorder defined as a state of abnormally elevated arousal, affect, and energy level, or "a state of heightened overall activation with enhanced affective expression together wi ...
or hypomania
Hypomania (literally "under mania" or "less than mania") is a mental and behavioural disorder, characterised essentially by an apparently non-contextual elevation of mood (euphoria) that contributes to persistently disinhibited behaviour.
Th ...
, alternating with normal or depressed moods. The extent to which unipolar and bipolar mood phenomena represent distinct categories of disorder, or mix and merge along a dimension or spectrum of mood, is subject to some scientific debate.
Psychotic disorder
Patterns of belief, language use and perception of reality can become dysregulated (e.g., delusions
A delusion is a false fixed belief that is not amenable to change in light of conflicting evidence. As a pathology, it is distinct from a belief based on false or incomplete information, confabulation, dogma, illusion, hallucination, or som ...
, thought disorder
A thought disorder (TD) is any disturbance in cognition that adversely affects language and thought content, and thereby communication. A variety of thought disorders were said to be characteristic of people with schizophrenia. A content-though ...
, hallucinations
A hallucination is a perception in the absence of an external stimulus that has the qualities of a real perception. Hallucinations are vivid, substantial, and are perceived to be located in external objective space. Hallucination is a combinati ...
). Psychotic disorders in this domain include schizophrenia
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations (typically hearing voices), delusions, and disorganized thinking. Other symptoms include social w ...
, and delusional disorder
Delusional disorder is a mental illness in which a person has delusions, but with no accompanying prominent hallucinations, thought disorder, mood disorder, or significant flattening of affect.American Psychiatric Association. (2013). ''Diagnostic ...
. Schizoaffective disorder
Schizoaffective disorder (SZA, SZD or SAD) is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis is made when the person has symptoms of both schizophrenia (usually psychosis) and a mood disorder: ...
is a category used for individuals showing aspects of both schizophrenia and affective disorders. Schizotypy
In psychology, schizotypy is a theoretical concept that posits a continuum of personality characteristics and experiences, ranging from normal dissociative, imaginative states to extreme states of mind related to psychosis, especially schizophr ...
is a category used for individuals showing some of the characteristics associated with schizophrenia, but without meeting cutoff criteria.
Personality disorder
Personality
Personality is the characteristic sets of behaviors, cognitions, and emotional patterns that are formed from biological and environmental factors, and which change over time. While there is no generally agreed-upon definition of personality, ...
—the fundamental characteristics of a person that influence thoughts and behaviors across situations and time—may be considered disordered if judged to be abnormally rigid and maladaptive. Although treated separately by some, the commonly used categorical schemes include them as mental disorders, albeit on a separate axis II in the case of the DSM-IV. A number of different personality disorders are listed, including those sometimes classed as ''eccentric'', such as paranoid, schizoid and schizotypal personality disorders; types that have described as dramatic or emotional, such as antisocial, borderline, histrionic
Histrionic may refer to:
* related to or reminiscent of (theatrical) acting, or acting out
* Histrionic personality disorder, a Cluster B personality disorder
* ''Histrionics'' (album), by The Higher
* ''Histrionicus
The harlequin duck (''Hi ...
or narcissistic
Narcissism is a self-centered personality style characterized as having an excessive interest in one's physical appearance or image and an excessive preoccupation with one's own needs, often at the expense of others.
Narcissism exists on a co ...
personality disorders; and those sometimes classed as fear-related, such as anxious-avoidant, dependent, or obsessive-compulsive personality disorders. Personality disorders, in general, are defined as emerging in childhood, or at least by adolescence or early adulthood. The ICD also has a category for enduring personality change after a catastrophic experience or psychiatric illness. If an inability to sufficiently adjust to life circumstances begins within three months of a particular event or situation, and ends within six months after the stressor stops or is eliminated, it may instead be classed as an adjustment disorder
Adjustment disorder is a maladaptive response to a psychosocial stressor. It is classified as a mental disorder. The maladaptive response usually involves otherwise normal emotional and behavioral reactions that manifest more intensely than usua ...
. There is an emerging consensus that personality disorders, similar to personality traits in general, incorporate a mixture of acute dysfunctional behaviors that may resolve in short periods, and maladaptive temperamental traits that are more enduring. Furthermore, there are also non-categorical schemes that rate all individuals via a profile of different dimensions of personality without a symptom-based cutoff from normal personality variation, for example through schemes based on dimensional models.
Eating disorder
Eating disorders involve disproportionate concern in matters of food and weight.anorexia nervosa
Anorexia nervosa, often referred to simply as anorexia, is an eating disorder characterized by low weight, food restriction, body image disturbance, fear of gaining weight, and an overpowering desire to be thin. ''Anorexia'' is a term of Gre ...
, bulimia nervosa
Bulimia nervosa, also known as simply bulimia, is an eating disorder characterized by binge eating followed by purging or fasting, and excessive concern with body shape and weight. The aim of this activity is to expel the body of calories eaten ...
, exercise bulimia or binge eating disorder
Binge eating disorder (BED) is an eating disorder characterized by frequent and recurrent binge eating episodes with associated negative psychological and social problems, but without the compensatory behaviors common to bulimia nervosa, OSFED, ...
.
Sleep disorder
Sleep disorders are associated with disruption to normal sleep
Sleep is a sedentary state of mind and body. It is characterized by altered consciousness, relatively inhibited Perception, sensory activity, reduced muscle activity and reduced interactions with surroundings. It is distinguished from wakefuln ...
patterns. A common sleep disorder is insomnia
Insomnia, also known as sleeplessness, is a sleep disorder in which people have trouble sleeping. They may have difficulty falling asleep, or staying asleep as long as desired. Insomnia is typically followed by daytime sleepiness, low energy, ...
, which is described as difficulty falling and/or staying asleep. Other sleep disorders include narcolepsy
Narcolepsy is a long-term neurological disorder that involves a decreased ability to regulate sleep–wake cycles. Symptoms often include periods of excessive daytime sleepiness and brief involuntary sleep episodes. About 70% of those affect ...
, sleep apnea
Sleep apnea, also spelled sleep apnoea, is a sleep disorder in which pauses in breathing or periods of shallow breathing during sleep occur more often than normal. Each pause can last for a few seconds to a few minutes and they happen many tim ...
, REM sleep behavior disorder, chronic sleep deprivation
Sleep deprivation, also known as sleep insufficiency or sleeplessness, is the condition of not having adequate duration and/or quality of sleep to support decent alertness, performance, and health. It can be either chronic or acute and may vary ...
, and restless leg syndrome.
Narcolepsy is a condition of extreme tendencies to fall asleep whenever and wherever. People with narcolepsy feel refreshed after their random sleep, but eventually get sleepy again. Narcolepsy diagnosis requires an overnight stay at a sleep center for analysis, during which doctors ask for a detailed sleep history and sleep records. Doctors also use actigraphs and polysomnography.obstructive sleep apnea
Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episo ...
, central sleep apnea, and complex sleep apnea. Sleep apnea can be diagnosed at home or with polysomnography at a sleep center. An ear, nose, and throat doctor may further help with the sleeping habits.
Sexuality related
Sexual disorders include dyspareunia
Dyspareunia ( ) is painful sexual intercourse due to medical or psychological causes. The term ''dyspareunia'' covers both female dyspareunia and male dyspareunia, but many discussions that use the term without further specification concern the ...
and various kinds of paraphilia (sexual arousal to objects, situations, or individuals that are considered abnormal or harmful to the person or others).
Other
Impulse control disorder
Impulse-control disorder (ICD) is a class of psychiatric disorders characterized by impulsivity – failure to resist a temptation, an urge, or an impulse; or having the inability to not speak on a thought. Many psychiatric disorders feature impu ...
: People who are abnormally unable to resist certain urges or impulses that could be harmful to themselves or others, may be classified as having an impulse control disorder, and disorders such as kleptomania
Kleptomania is the inability to resist the urge to steal items, usually for reasons other than personal use or financial gain. First described in 1816, kleptomania is classified in psychiatry as an impulse control disorder. Some of the main cha ...
(stealing) or pyromania (fire-setting). Various behavioral addictions, such as gambling addiction, may be classed as a disorder. Obsessive-compulsive disorder can sometimes involve an inability to resist certain acts but is classed separately as being primarily an anxiety disorder.
Substance use disorder
Substance use disorder (SUD) is the persistent use of drugs (including alcohol) despite substantial harm and adverse consequences as a result of their use. Substance use disorders are characterized by an array of mental/emotional, physical, and ...
: This disorder refers to the use of drugs (legal or illegal, including alcohol
Alcohol most commonly refers to:
* Alcohol (chemistry), an organic compound in which a hydroxyl group is bound to a carbon atom
* Alcohol (drug), an intoxicant found in alcoholic drinks
Alcohol may also refer to:
Chemicals
* Ethanol, one of sev ...
) that persists despite significant problems or harm related to its use. Substance dependence
Substance dependence, also known as drug dependence, is a biopsychological situation whereby an individual's functionality is dependent on the necessitated re-consumption of a psychoactive substance because of an adaptive state that has develope ...
and substance abuse
Substance abuse, also known as drug abuse, is the use of a drug in amounts or by methods which are harmful to the individual or others. It is a form of substance-related disorder. Differing definitions of drug abuse are used in public health, ...
fall under this umbrella category in the DSM. Substance use disorder may be due to a pattern of compulsive and repetitive use of a drug that results in tolerance to its effects and withdrawal symptoms when use is reduced or stopped.
Dissociative disorder
Dissociative disorders (DD) are conditions that involve disruptions or breakdowns of memory, awareness, identity, or perception. People with dissociative disorders use dissociation as a defense mechanism, pathologically and involuntarily. The i ...
: People with severe disturbances of their self-identity, memory, and general awareness of themselves and their surroundings may be classified as having these types of disorders, including depersonalization disorder or dissociative identity disorder
Dissociative identity disorder (DID), better known as multiple personality disorder or multiple personality syndrome, is a mental disorder characterized by the presence of at least two distinct and relatively enduring personality states.
The di ...
(which was previously referred to as multiple personality disorder or "split personality").
Cognitive disorder: These affect cognitive abilities, including learning and memory. This category includes delirium
Delirium (also known as acute confusional state) is an organically caused decline from a previous baseline of mental function that develops over a short period of time, typically hours to days. Delirium is a syndrome encompassing disturbances ...
and mild and major neurocognitive disorder (previously termed dementia
Dementia is a disorder which manifests as a set of related symptoms, which usually surfaces when the brain is damaged by injury or disease. The symptoms involve progressive impairments in memory, thinking, and behavior, which negatively affe ...
).
Developmental disorder: These disorders initially occur in childhood. Some examples include autism spectrum
The autism spectrum, often referred to as just autism or in the context of a professional diagnosis autism spectrum disorder (ASD) or autism spectrum condition (ASC), is a neurodevelopmental condition (or conditions) characterized by difficulti ...
disorder, oppositional defiant disorder and conduct disorder
Conduct disorder (CD) is a mental disorder diagnosed in childhood or adolescence that presents itself through a repetitive and persistent pattern of behavior that includes theft, lies, physical violence that may lead to destruction, and reckles ...
, and attention deficit hyperactivity disorder
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterised by excessive amounts of inattention, hyperactivity, and impulsivity that are pervasive, impairing in multiple contexts, and otherwise age-inap ...
(ADHD), which may continue into adulthood. Conduct disorder, if continuing into adulthood, may be diagnosed as antisocial personality disorder (dissocial personality disorder in the ICD). Popular labels such as psychopath
Psychopathy, sometimes considered synonymous with sociopathy, is characterized by persistent antisocial behavior, impaired empathy and remorse, and bold, disinhibited, and egotistical traits. Different conceptions of psychopathy have been ...
(or sociopath) do not appear in the DSM or ICD but are linked by some to these diagnoses.
Somatoform disorders may be diagnosed when there are problems that appear to originate in the body that are thought to be manifestations of a mental disorder. This includes somatization disorder
Somatization disorder is a mental and behavioral disorder characterized by recurring, multiple, and current, clinically significant complaints about somatic symptoms. It was recognized in the DSM-IV-TR classification system, but in the latest ve ...
and conversion disorder
Conversion disorder (CD), or functional neurologic symptom disorder, is a diagnostic category used in some psychiatric classification systems. It is sometimes applied to patients who present with neurological symptoms, such as numbness, blindnes ...
. There are also disorders of how a person perceives their body, such as body dysmorphic disorder
Body dysmorphic disorder (BDD), occasionally still called dysmorphophobia, is a mental disorder characterized by the obsessive idea that some aspect of one's own body part or appearance is severely flawed and therefore warrants exceptional meas ...
. Neurasthenia
Neurasthenia (from the Ancient Greek νεῦρον ''neuron'' "nerve" and ἀσθενής ''asthenés'' "weak") is a term that was first used at least as early as 1829 for a mechanical weakness of the nerves and became a major diagnosis in North A ...
is an old diagnosis involving somatic complaints as well as fatigue and low spirits/depression, which is officially recognized by the ICD-10 but no longer by the DSM-IV.
Factitious disorder
A factitious disorder is a condition in which a person, ''without'' a malingering motive, acts as if they have an illness by deliberately producing, feigning, or exaggerating symptoms, purely to attain (for themselves or for another) a patient' ...
s are diagnosed where symptoms are thought to be reported for personal gain. Symptoms are often deliberately produced or feigned, and may relate to either symptoms in the individual or in someone close to them, particularly people they care for.
There are attempts to introduce a category of relational disorder, where the diagnosis is of a relationship rather than on any one individual in that relationship. The relationship may be between children and their parents, between couples, or others. There already exists, under the category of psychosis, a diagnosis of shared psychotic disorder
Shared may refer to:
* Sharing
* Shared ancestry or Common descent
* Shared care
* Shared-cost service
* Shared decision-making in medicine
* Shared delusion, various meanings
* Shared government
* Shared intelligence or collective intelligence
* ...
where two or more individuals share a particular delusion because of their close relationship with each other.
There are a number of uncommon psychiatric syndromes
A syndrome is a set of medical signs and symptoms which are correlated with each other and often associated with a particular disease or disorder. The word derives from the Greek σύνδρομον, meaning "concurrence". When a syndrome is pai ...
, which are often named after the person who first described them, such as Capgras syndrome
Capgras delusion or Capgras syndrome is a psychiatric disorder in which a person holds a delusion that a friend, spouse, parent, or other close family member (or pet) has been replaced by an identical impostor. It is named after Joseph Capgras ( ...
, De Clerambault syndrome, Othello syndrome
Pathological jealousy, also known as morbid jealousy, Othello syndrome or delusional jealousy, is a psychological disorder in which a person is preoccupied with the thought that their spouse or sexual partner is being unfaithful without having an ...
, Ganser syndrome, Cotard delusion
Cotard's syndrome, also known as Cotard's delusion or walking corpse syndrome, is a rare mental disorder in which the affected person holds the delusional belief that they are dead, do not exist, are putrefying, or have lost their blood or int ...
, and Ekbom syndrome, and additional disorders such as the Couvade syndrome and Geschwind syndrome Geschwind syndrome, also known as Gastaut-Geschwind, is a group of behavioral phenomena evident in some people with temporal lobe epilepsy. It is named for one of the first individuals to categorize the symptoms, Norman Geschwind, who published pr ...
.
Signs and symptoms
Course
The onset of psychiatric disorders usually occurs from childhood to early adulthood. Impulse-control disorders and a few anxiety disorders tend to appear in childhood. Some other anxiety disorders, substance disorders, and mood disorders emerge later in the mid-teens. Symptoms of schizophrenia typically manifest from late adolescence to early twenties.
The likely course and outcome of mental disorders vary and are dependent on numerous factors related to the disorder itself, the individual as a whole, and the social environment. Some disorders may last a brief period of time, while others may be long-term in nature.
All disorders can have a varied course. Long-term international studies of schizophrenia have found that over a half of individuals recover in terms of symptoms, and around a fifth to a third in terms of symptoms and functioning, with many requiring no medication. While some have serious difficulties and support needs for many years, "late" recovery is still plausible. The World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level o ...
(WHO) concluded that the long-term studies' findings converged with others in "relieving patients, carers and clinicians of the chronicity paradigm which dominated thinking throughout much of the 20th century."
Disability
Some disorders may be very limited in their functional effects, while others may involve substantial disability and support needs. The degree of ability or disability may vary over time and across different life domains. Furthermore, continued disability has been linked to institutionalization
In sociology, institutionalisation (or institutionalization) is the process of embedding some conception (for example a belief, norm, social role, particular value or mode of behavior) within an organization, social system, or society as a who ...
, discrimination
Discrimination is the act of making unjustified distinctions between people based on the groups, classes, or other categories to which they belong or are perceived to belong. People may be discriminated on the basis of Racial discrimination, r ...
and social exclusion
Social exclusion or social marginalisation is the social disadvantage and relegation to the fringe of society. It is a term that has been used widely in Europe and was first used in France in the late 20th century. It is used across discipline ...
as well as to the inherent effects of disorders. Alternatively, functioning may be affected by the stress of having to hide a condition in work or school, etc., by adverse effects of medications or other substances, or by mismatches between illness-related variations and demands for regularity.
It is also the case that, while often being characterized in purely negative terms, some mental traits or states labeled as disorders can also involve above-average creativity, non-conformity, goal-striving, meticulousness, or empathy.activities of daily living
Activity may refer to:
* Action (philosophy), in general
* Human activity: human behavior, in sociology behavior may refer to all basic human actions, economics may study human economic activities and along with cybernetics and psychology may s ...
. Including looking after the self (health care, grooming, dressing, shopping, cooking etc.) or looking after accommodation (chores, DIY tasks, etc.)
*Interpersonal relationships
The concept of interpersonal relationship involves social associations, connections, or affiliations between two or more people. Interpersonal relationships vary in their degree of intimacy or self-disclosure, but also in their duration, in t ...
. Including communication skills
Communication (from la, communicare, meaning "to share" or "to be in relation with") is usually defined as the transmission of information. The term may also refer to the message communicated through such transmissions or the field of inqu ...
, ability to form relationships and sustain them, ability to leave the home or mix in crowds or particular settings
*Occupational functioning. Ability to acquire an employment and hold it, cognitive and social skills required for the job, dealing with workplace
A workplace is a location where someone works, for their employer or themselves, a place of employment. Such a place can range from a home office to a large office building or factory. For industrialized societies, the workplace is one of ...
culture, or studying as a student.
In terms of total disability-adjusted life years
The disability-adjusted life year (DALY) is a measure of overall disease burden, expressed as the number of years lost due to ill-health, disability or early death. It was developed in the 1990s as a way of comparing the overall health and life ex ...
(DALYs), which is an estimate of how many years of life are lost due to premature death or to being in a state of poor health and disability, mental disorders rank amongst the most disabling conditions. Unipolar (also known as Major) depressive disorder is the third leading cause of disability worldwide, of any condition mental or physical, accounting for 65.5 million years lost. The first systematic description of global disability arising in youth, in 2011, found that among 10- to 24-year-olds nearly half of all disability (current and as estimated to continue) was due to mental and neurological conditions, including substance use disorders and conditions involving self-harm
Self-harm is intentional behavior that is considered harmful to oneself. This is most commonly regarded as direct injury of one's own skin tissues usually without a suicidal intention. Other terms such as cutting, self-injury and self-mutilati ...
. Second to this were accidental injuries (mainly traffic collisions) accounting for 12 percent of disability, followed by communicable diseases at 10 percent. The disorders associated with most disabilities in high-income countries were unipolar major depression (20%) and alcohol use disorder (11%). In the eastern Mediterranean region, it was unipolar major depression (12%) and schizophrenia (7%), and in Africa it was unipolar major depression (7%) and bipolar disorder (5%).
Suicide, which is often attributed to some underlying mental disorder, is a leading cause of death among teenagers and adults under 35.
Risk factors
The predominant view is that genetic, psychological, and environmental factors all contribute to the development or progression of mental disorders. Different risk factors may be present at different ages, with risk occurring as early as during prenatal period.
Genetics
A number of psychiatric disorders are linked to a family history (including depression, narcissistic personality disorderheritability
Heritability is a statistic used in the fields of breeding and genetics that estimates the degree of ''variation'' in a phenotypic trait in a population that is due to genetic variation between individuals in that population. The concept of her ...
for many mental disorders (especially autism and schizophrenia). Although researchers have been looking for decades for clear linkages between genetics
Genetics is the study of genes, genetic variation, and heredity in organisms.Hartl D, Jones E (2005) It is an important branch in biology because heredity is vital to organisms' evolution. Gregor Mendel, a Moravian Augustinian friar work ...
and mental disorders, that work has not yielded specific genetic biomarker
In biomedical contexts, a biomarker, or biological marker, is a measurable indicator of some biological state or condition. Biomarkers are often measured and evaluated using blood, urine, or soft tissues to examine normal biological processes, p ...
s yet that might lead to better diagnosis and better treatments.
Statistical research looking at eleven disorders found widespread assortative mating
Assortative mating (also referred to as positive assortative mating or homogamy) is a mating pattern and a form of sexual selection in which individuals with similar phenotypes or genotypes mate with one another more frequently than would be ...
between people with mental illness. That means that individuals with one of these disorders were two to three times more likely than the general population to have a partner with a mental disorder. Sometimes people seemed to have preferred partners with the same mental illness. Thus, people with schizophrenia or ADHD are seven times more likely to have affected partners with the same disorder. This is even more pronounced for people with Autism spectrum disorders who are 10 times more likely to have a spouse with the same disorder.
Environment
 During the prenatal stage, factors like unwanted pregnancy, lack of adaptation to pregnancy or substance use during pregnancy increases the risk of developing a mental disorder.
During the prenatal stage, factors like unwanted pregnancy, lack of adaptation to pregnancy or substance use during pregnancy increases the risk of developing a mental disorder.abuse
Abuse is the improper usage or treatment of a thing, often to unfairly or improperly gain benefit. Abuse can come in many forms, such as: physical or verbal maltreatment, injury, assault, violation, rape, unjust practices, crimes, or other t ...
, neglect
In the context of caregiving, neglect is a form of abuse where the perpetrator, who is responsible for caring for someone who is unable to care for themselves, fails to do so. It can be a result of carelessness, indifference, or unwillingness a ...
, bullying
Bullying is the use of force, coercion, hurtful teasing or threat, to abuse, aggressively dominate or intimidate. The behavior is often repeated and habitual. One essential prerequisite is the perception (by the bully or by others) of an ...
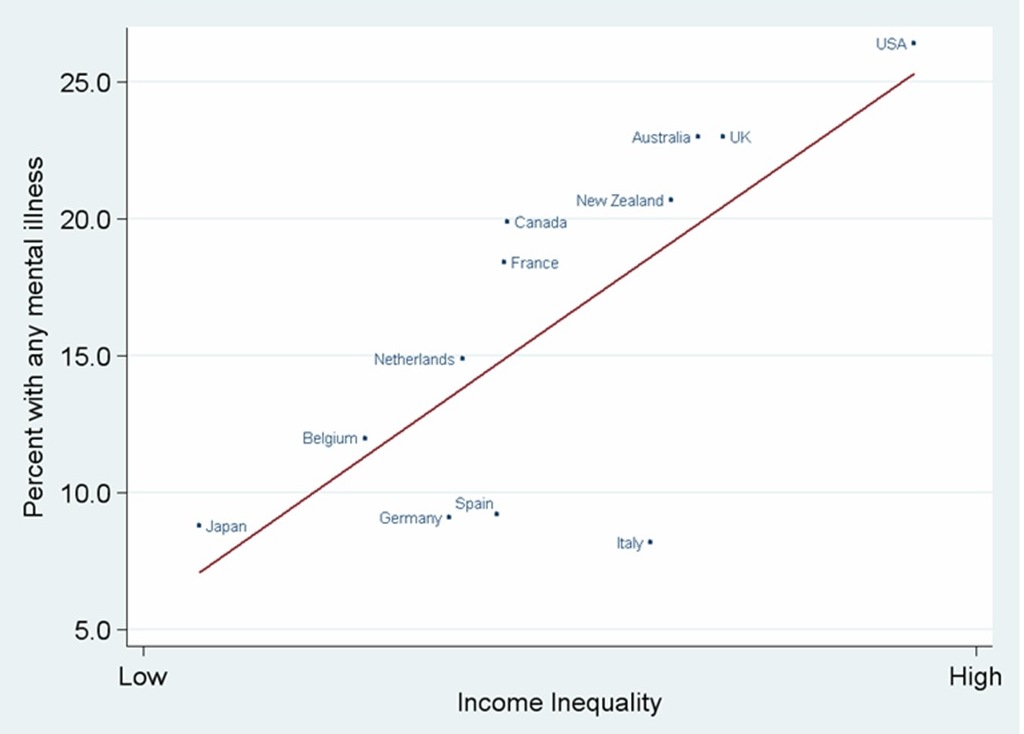
, social stress, traumatic events, and other negative or overwhelming life experiences. Aspects of the wider community have also been implicated,socioeconomic
Socioeconomics (also known as social economics) is the social science that studies how economic activity affects and is shaped by social processes. In general it analyzes how modern societies progress, stagnate, or regress because of their l ...
inequality, lack of social cohesion, problems linked to migration
Migration, migratory, or migrate may refer to: Human migration
* Human migration, physical movement by humans from one region to another
** International migration, when peoples cross state boundaries and stay in the host state for some minimum le ...
, and features of particular societies and cultures. The specific risks and pathways to particular disorders are less clear, however.
Nutrition also plays a role in mental disorders.urbanicity
Urbanization (or urbanisation) refers to the population shift from rural to urban areas, the corresponding decrease in the proportion of people living in rural areas, and the ways in which societies adapt to this change. It is predominantly the ...
.
Drug use
Mental disorders are associated with drug use including: cannabis
''Cannabis'' () is a genus of flowering plants in the family Cannabaceae. The number of species within the genus is disputed. Three species may be recognized: '' Cannabis sativa'', '' C. indica'', and '' C. ruderalis''. Alternative ...
,alcohol
Alcohol most commonly refers to:
* Alcohol (chemistry), an organic compound in which a hydroxyl group is bound to a carbon atom
* Alcohol (drug), an intoxicant found in alcoholic drinks
Alcohol may also refer to:
Chemicals
* Ethanol, one of sev ...
and caffeine
Caffeine is a central nervous system (CNS) stimulant of the methylxanthine chemical classification, class. It is mainly recreational drug use, used recreationally as a Nootropic, cognitive enhancer, increasing alertness and attentional perfor ...
, use of which appears to promote anxiety
Anxiety is an emotion which is characterized by an unpleasant state of inner turmoil and includes feelings of dread over anticipated events. Anxiety is different than fear in that the former is defined as the anticipation of a future threat wh ...
. For psychosis
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavi ...
and schizophrenia, usage of a number of drugs has been associated with development of the disorder, including cannabis, cocaine
Cocaine (from , from , ultimately from Quechua: ''kúka'') is a central nervous system (CNS) stimulant mainly used recreationally for its euphoric effects. It is primarily obtained from the leaves of two Coca species native to South Am ...
, and amphetamines
Substituted amphetamines are a class of compounds based upon the amphetamine structure; it includes all derivative compounds which are formed by replacing, or substituting, one or more hydrogen atoms in the amphetamine core structure with sub ...
.cannabis
''Cannabis'' () is a genus of flowering plants in the family Cannabaceae. The number of species within the genus is disputed. Three species may be recognized: '' Cannabis sativa'', '' C. indica'', and '' C. ruderalis''. Alternative ...
and bipolar disorder. Cannabis has also been associated with depression.
Chronic disease
People living with chronic conditions like HIV and diabetes are at higher risk of developing a mental disorder. People living with diabetes experience significant stress from the biological impact of the disease, which places them at risk for developing anxiety and depression. Diabetic patients also have to deal with emotional stress trying to manage the disease. Conditions like heart disease, stroke, respiratory conditions, cancer, and arthritis increase the risk of developing a mental disorder when compared to the general population.
Personality traits
Risk factors for mental illness include a propensity for high neuroticism
Causal models
Mental disorders can arise from multiple sources, and in many cases there is no single accepted or consistent cause currently established. An eclectic
Eclectic may refer to:
Music
* ''Eclectic'' (Eric Johnson and Mike Stern album), 2014
* ''Eclectic'' (Big Country album), 1996
* Eclectic Method, name of an audio-visual remix act
* Eclecticism in music, the conscious use of styles alien to th ...
or pluralistic mix of models may be used to explain particular disorders.biopsychosocial model
Biopsychosocial models are a class of trans-disciplinary models which look at the interconnection between biology, psychology, and socio-environmental factors. These models specifically examine how these aspects play a role in topics ranging from ...
which incorporates biological, psychological and social factors, although this may not always be applied in practice.
Biological psychiatry
Biological psychiatry or biopsychiatry is an approach to psychiatry that aims to understand mental disorder in terms of the biological function of the nervous system. It is interdisciplinary in its approach and draws on sciences such as neuroscie ...
follows a biomedical
Biomedicine (also referred to as Western medicine, mainstream medicine or conventional medicine) model where many mental disorders are conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience. A common assumption is that disorders may have resulted from genetic and developmental
Development of the human body is the process of growth to maturity. The process begins with fertilization, where an egg released from the ovary of a female is penetrated by a sperm cell from a male. The resulting zygote develops through mitosi ...
vulnerabilities, exposed by stress
Stress may refer to:
Science and medicine
* Stress (biology), an organism's response to a stressor such as an environmental condition
* Stress (linguistics), relative emphasis or prominence given to a syllable in a word, or to a word in a phrase ...
in life (for example in a diathesis–stress model
The diathesis-stress model, also known as the vulnerability–stress model, is a psychological theory that attempts to explain a disorder, or its trajectory, as the result of an interaction between a predispositional vulnerability, the diathesis ...
), although there are various views on what causes differences between individuals. Some types of mental disorders may be viewed as primarily neurodevelopmental disorders
Neurodevelopmental disorders are a group of disorders that affect the development of the nervous system, leading to abnormal brain function which may affect emotion, learning ability, self-control, and memory. The effects of neurodevelopmental ...
.
Evolutionary psychology
Evolutionary psychology is a theoretical approach in psychology that examines cognition and behavior from a modern evolutionary perspective. It seeks to identify human psychological adaptations with regards to the ancestral problems they evo ...
may be used as an overall explanatory theory, while attachment theory
Attachment theory is a psychological, evolutionary and ethological theory concerning relationships between humans. The most important tenet is that young children need to develop a relationship with at least one primary caregiver for normal ...
is another kind of evolutionary-psychological approach sometimes applied in the context of mental disorders. Psychoanalytic theories have continued to evolve alongside and cognitive
Cognition refers to "the mental action or process of acquiring knowledge and understanding through thought, experience, and the senses". It encompasses all aspects of intellectual functions and processes such as: perception, attention, thought ...
-behavioral
Behavior (American English) or behaviour (British English) is the range of actions and mannerisms made by individuals, organisms, systems or artificial entities in some environment. These systems can include other systems or organisms as we ...
and systemic-family approaches. A distinction is sometimes made between a " medical model" or a " social model" of disorder and disability.
Diagnosis
Psychiatrists seek to provide a medical diagnosis
Medical diagnosis (abbreviated Dx, Dx, or Ds) is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. The information r ...
of individuals by an assessment of symptoms
Signs and symptoms are the observed or detectable signs, and experienced symptoms of an illness, injury, or condition. A sign for example may be a higher or lower temperature than normal, raised or lowered blood pressure or an abnormality showi ...
, signs and impairment associated with particular types of mental disorder. Other mental health professionals, such as clinical psychologists, may or may not apply the same diagnostic categories to their clinical formulation of a client's difficulties and circumstances. The majority of mental health problems are, at least initially, assessed and treated by family physicians (in the UK general practitioners) during consultations, who may refer a patient on for more specialist diagnosis in acute (medicine), acute or chronic (medicine), chronic cases.
Routine diagnostic practice in mental health services typically involves an interview known as a mental status examination, where evaluations are made of appearance and behavior, self-reported symptoms, mental health history, and current life circumstances. The views of other professionals, relatives, or other third parties may be taken into account. A physical examination to check for ill health or the effects of medications or other drugs may be conducted. Psychological testing is sometimes used via paper-and-pen or computerized questionnaires, which may include algorithms based on ticking off standardized diagnostic criteria, and in rare specialist cases neuroimaging tests may be requested, but such methods are more commonly found in research studies than routine clinical practice.
Time and budgetary constraints often limit practicing psychiatrists from conducting more thorough diagnostic evaluations. It has been found that most clinicians evaluate patients using an unstructured, open-ended approach, with limited training in Evidence based assessment, evidence-based assessment methods, and that inaccurate diagnosis may be common in routine practice. In addition, comorbidity
In medicine, comorbidity - from Latin morbus ("sickness"), co ("together"), -ity (as if - several sicknesses together) - is the presence of one or more additional conditions often co-occurring (that is, concomitant or concurrent) with a primary ...
is very common in psychiatric diagnosis, where the same person meets the criteria for more than one disorder. On the other hand, a person may have several different difficulties only some of which meet the criteria for being diagnosed. There may be specific problems with accurate diagnosis in developing countries.
More structured approaches are being increasingly used to measure levels of mental illness.
*HoNOS is the most widely used measure in English mental health services, being used by at least 61 trusts. In HoNOS a score of 0–4 is given for each of 12 factors, based on functional living capacity. Research has been supportive of HoNOS, although some questions have been asked about whether it provides adequate coverage of the range and complexity of mental illness problems, and whether the fact that often only 3 of the 12 scales vary over time gives enough subtlety to accurately measure outcomes of treatment.
Criticism
Since the 1980s, Paula Caplan has been concerned about the subjectivity of psychiatric diagnosis, and people being arbitrarily "slapped with a psychiatric label." Caplan says because psychiatric diagnosis is unregulated, doctors are not required to spend much time interviewing patients or to seek a second opinion. The ''Diagnostic and Statistical Manual of Mental Disorders'' can lead a psychiatrist to focus on narrow checklists of symptoms, with little consideration of what is actually causing the person's problems. So, according to Caplan, getting a psychiatric diagnosis and label often stands in the way of recovery.
In 2013, psychiatrist Allen Frances wrote a paper entitled "The New Crisis of Confidence in Psychiatric Diagnosis", which said that "psychiatric diagnosis... still relies exclusively on fallible subjective judgments rather than objective biological tests." Frances was also concerned about "unpredictable overdiagnosis."
Potential routine use of MRI/fMRI in diagnosis
in 2018 the American Psychological Association commissioned a review to reach a consensus on whether modern clinical MRI/fMRI will be able to be used in the diagnosis of mental health disorders. the criteria presented by the APA stated that the Biomarker (medicine), Biomarkers used in diagnosis should:
#"have a sensitivity of at least 80% for detecting a particular psychiatric disorder"
#should "have a specificity of at least 80% for distinguishing this disorder from other psychiatric or medical disorders"
#"should be reliable, reproducible, and ideally be noninvasive, simple to perform, and inexpensive"
#proposed biomarkers should be verified by 2 independent studies each by a different investigator and different population samples and published in a peer-reviewed journal.
the review concluded that although neuroimaging diagnosis may technically be feasible, very large studies are needed to evaluate specific biomarkers which were not available.
Prevention
The 2004 WHO report "Prevention of Mental Disorders" stated that "Prevention of these disorders is obviously one of the most effective ways to reduce the [disease] burden."
The 2011 European Psychiatric Association (EPA) guidance on prevention of mental disorders states "There is considerable evidence that various psychiatric conditions can be prevented through the implementation of effective evidence-based interventions."
A 2011 UK Department of Health report on the economic case for mental health promotion and mental illness prevention found that "many interventions are outstandingly good value for money, low in cost and often become self-financing over time, saving public expenditure".
In 2016, the National Institute of Mental Health re-affirmed prevention as a research priority area.
Parenting may affect the child's mental health, and evidence suggests that helping parents to be more effective with their children can address mental health needs.
Universal prevention (aimed at a population that has no increased risk for developing a mental disorder, such as school programs or mass media campaigns) need very high numbers of people to show effect (sometimes known as the "power" problem). Approaches to overcome this are (1) focus on high-incidence groups (e.g. by targeting groups with high risk factors), (2) use multiple interventions to achieve greater, and thus more statistically valid, effects, (3) use cumulative meta-analyses of many trials, and (4) run very large trials.
Management
 Treatment and support for mental disorders are provided in psychiatric hospitals, clinics or a range of community mental health services. In some countries services are increasingly based on a recovery approach, intended to support individual's personal journey to gain the kind of life they want.
There is a range of different types of treatment and what is most suitable depends on the disorder and the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication. In a minority of cases, individuals may be treated against their will, which can cause particular difficulties depending on how it is carried out and perceived. Compulsory treatment while in the community versus non-compulsory treatment does not appear to make much of a difference except by maybe decreasing victimization.
Treatment and support for mental disorders are provided in psychiatric hospitals, clinics or a range of community mental health services. In some countries services are increasingly based on a recovery approach, intended to support individual's personal journey to gain the kind of life they want.
There is a range of different types of treatment and what is most suitable depends on the disorder and the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication. In a minority of cases, individuals may be treated against their will, which can cause particular difficulties depending on how it is carried out and perceived. Compulsory treatment while in the community versus non-compulsory treatment does not appear to make much of a difference except by maybe decreasing victimization.
Lifestyle
Lifestyle strategies, including dietary changes, exercise and quitting smoking may be of benefit.
Therapy
There is also a wide range of psychotherapists (including family therapy), Licensed Professional Counselor, counselors, and public health professionals. In addition, there are peer support
Peer support occurs when people provide knowledge, experience, emotional, social or practical help to each other. It commonly refers to an initiative consisting of trained supporters (although it can be provided by peers without training), and can ...
roles where personal experience of similar issues is the primary source of expertise.
A major option for many mental disorders is psychotherapy. There are several main types. Cognitive behavioral therapy (CBT) is widely used and is based on modifying the patterns of thought and behavior associated with a particular disorder. Other psychotherapies include dialectic behavioral therapy (DBT) and interpersonal psychotherapy (IPT). Psychoanalysis, addressing underlying psychic conflicts and defenses, has been a dominant school of psychotherapy and is still in use. Systemic therapy or family therapy is sometimes used, addressing a network of significant others as well as an individual.
Some psychotherapies are based on a humanistic psychology, humanistic approach. There are many specific therapies used for particular disorders, which may be offshoots or hybrids of the above types. Mental health professionals often employ an Integrative Psychotherapy, eclectic or integrative approach. Much may depend on the therapeutic relationship, and there may be problems with trust (social sciences), trust, confidentiality and Social engagement, engagement.
Medication
A major option for many mental disorders is psychiatric medication
A psychiatric or psychotropic medication is a psychoactive drug taken to exert an effect on the chemical makeup of the brain and nervous system. Thus, these medications are used to treat mental illnesses. These medications are typically made of ...
and there are several main groups. Antidepressants are used for the treatment of clinical depression, as well as often for anxiety and a range of other disorders. Anxiolytics (including sedatives) are used for anxiety disorders and related problems such as insomnia. Mood stabilizers are used primarily in bipolar disorder. Antipsychotics are used for psychotic disorders, notably for Schizophrenic reaction, positive symptoms in schizophrenia, and also increasingly for a range of other disorders. Stimulants are commonly used, notably for ADHD.
Despite the different conventional names of the drug groups, there may be considerable overlap in the disorders for which they are actually indicated, and there may also be off-label use of medications. There can be problems with adverse effects of medication and Compliance (medicine), adherence to them, and there is also criticism of pharmaceutical marketing and professional conflicts of interest. However, these medications in combination with non-pharmacological methods, such as cognitive-behavioral therapy (CBT) are seen to be most effective in treating mental disorders.
Other
Electroconvulsive therapy (ECT) is sometimes used in severe cases when other interventions for severe intractable depression have failed. ECT is usually indicated for treatment resistant depression, severe vegetative symptoms, psychotic depression, intense suicidal ideation, depression during pregnancy, and catatonia. Psychosurgery is considered experimental but is advocated by some neurologists in certain rare cases.
Counseling (professional) and co-counseling (between peers) may be used. Psychoeducation programs may provide people with the information to understand and manage their problems. Creative therapies are sometimes used, including music therapy, art therapy or drama therapy. Lifestyle adjustments and supportive measures are often used, including peer support, self-help groups for mental health and supported housing or supported employment (including social firms). Some advocate dietary supplements.
Reasonable accommodations (adjustments and supports) might be put in place to help an individual cope and succeed in environments despite potential disability related to mental health problems. This could include an emotional support animal or specifically trained psychiatric service dog. cannabis is specifically not recommended as a treatment.
Epidemiology

 Mental disorders are common. Worldwide, more than one in three people in most countries report sufficient criteria for at least one at some point in their life.
Mental disorders are common. Worldwide, more than one in three people in most countries report sufficient criteria for at least one at some point in their life.
History
Ancient civilizations
Ancient civilizations described and treated a number of mental disorders. Mental illnesses were well known in ancient Mesopotamia,phobia
A phobia is an anxiety disorder defined by a persistent and excessive fear of an object or situation. Phobias typically result in a rapid onset of fear and are usually present for more than six months. Those affected go to great lengths to avoi ...
and developed the humorism theory. Mental disorders were described, and treatments developed, in Persia, Arabia and in the Islamic Golden Age, medieval Islamic world.
Europe
Middle Ages
Conceptions of madness in the Middle Ages in Christian Europe were a mixture of the divine, diabolical, magical and humoral, and transcendental. In the early modern period, some people with mental disorders may have been victims of the witch-hunts. While not every witch and sorcerer accused were mentally ill, all mentally ill were considered to be witches or sorcerers. Many terms for mental disorders that found their way into everyday use first became popular in the 16th and 17th centuries.
Eighteenth century
 By the end of the 17th century and into the Age of Enlightenment, Enlightenment, madness was increasingly seen as an organic physical phenomenon with no connection to the soul or moral responsibility. Asylum care was often harsh and treated people like wild animals, but towards the end of the 18th century a moral treatment movement gradually developed. Clear descriptions of some syndromes may be rare before the 19th century.
By the end of the 17th century and into the Age of Enlightenment, Enlightenment, madness was increasingly seen as an organic physical phenomenon with no connection to the soul or moral responsibility. Asylum care was often harsh and treated people like wild animals, but towards the end of the 18th century a moral treatment movement gradually developed. Clear descriptions of some syndromes may be rare before the 19th century.
Nineteenth century
Industrialization and population growth led to a massive expansion of the number and size of insane asylums in every Western country in the 19th century. Numerous different classification schemes and diagnostic terms were developed by different authorities, and the term psychiatry was coined (1808), though medical superintendents were still known as alienists.
Twentieth century
 The turn of the 20th century saw the development of psychoanalysis, which would later come to the fore, along with Emil Kraepelin, Kraepelin's classification scheme. Asylum "inmates" were increasingly referred to as "patients", and asylums were renamed as hospitals.
The turn of the 20th century saw the development of psychoanalysis, which would later come to the fore, along with Emil Kraepelin, Kraepelin's classification scheme. Asylum "inmates" were increasingly referred to as "patients", and asylums were renamed as hospitals.
Europe and the United States
 Early in the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "Combat stress reaction, shell shock".
World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first ''Diagnostic and Statistical Manual of Mental Disorders''. The International Classification of Diseases (ICD) also developed a section on mental disorders. The term stress (biological), stress, having emerged from endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomy, lobotomies and the neuroleptic chlorpromazine came to be used by mid-century. In the 1960s there were many challenges to the concept of mental illness itself. These challenges came from psychiatrists like Thomas Szasz who argued that mental illness was a myth used to disguise moral conflicts; from sociologists such as Erving Goffman who said that mental illness was merely another example of how society labels and controls non-conformists; from behavioral psychologists who challenged psychiatry's fundamental reliance on unobservable phenomena; and from gay rights activists who criticised the APA's listing of homosexuality as a mental disorder. A study published in ''Science'' by Rosenhan experiment, Rosenhan received much publicity and was viewed as an attack on the efficacy of psychiatric diagnosis.
Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A Psychiatric survivors movement, consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" (later antidepressants) and lithium pharmacology, lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience, genetics, and psychology led to new research agendas. Cognitive behavioral therapy and other psychotherapies developed. The ''DSM'' and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI-type antidepressants became some of the most widely prescribed drugs in the world, as later did antipsychotics. Also during the 1990s, a recovery approach developed.
Early in the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "Combat stress reaction, shell shock".
World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first ''Diagnostic and Statistical Manual of Mental Disorders''. The International Classification of Diseases (ICD) also developed a section on mental disorders. The term stress (biological), stress, having emerged from endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomy, lobotomies and the neuroleptic chlorpromazine came to be used by mid-century. In the 1960s there were many challenges to the concept of mental illness itself. These challenges came from psychiatrists like Thomas Szasz who argued that mental illness was a myth used to disguise moral conflicts; from sociologists such as Erving Goffman who said that mental illness was merely another example of how society labels and controls non-conformists; from behavioral psychologists who challenged psychiatry's fundamental reliance on unobservable phenomena; and from gay rights activists who criticised the APA's listing of homosexuality as a mental disorder. A study published in ''Science'' by Rosenhan experiment, Rosenhan received much publicity and was viewed as an attack on the efficacy of psychiatric diagnosis.
Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A Psychiatric survivors movement, consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" (later antidepressants) and lithium pharmacology, lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience, genetics, and psychology led to new research agendas. Cognitive behavioral therapy and other psychotherapies developed. The ''DSM'' and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI-type antidepressants became some of the most widely prescribed drugs in the world, as later did antipsychotics. Also during the 1990s, a recovery approach developed.
Africa and Nigeria
Most Africans view mental disturbances as external spiritual attack on the person. Those who have a mental illness are thought to be under a spell or bewitched. Often than usual, People view a mentally ill person as possessed of an evil spirit and is seen as more of sociological perspective than a psychological order.
The World Health Organization, WHO estimated that fewer than 10% of mentally ill Nigerians have access to a psychiatrist or health worker, because there is a low ratio of mental-health specialists available in a country of 200 million people. WHO estimates that the number of mentally ill Nigerians ranges from 40 million to 60 million. Disorders such as depression, anxiety, schizophrenia, personality disorder, old age-related disorder, and substance-abuse disorder are common in Nigeria, as in other countries in Africa.
Nigeria is still nowhere near being equipped to solve prevailing mental health challenges. With little scientific research carried out, coupled with insufficient mental-health hospitals in the country, traditional healers provide specialized psychotherapy care to those that require their services and pharmacotherapy
Society and culture
 Different societies or cultures, even different individuals in a subculture, can disagree as to what constitutes optimal versus pathological biological and psychological functioning. Research has demonstrated that cultures vary in the relative importance placed on, for example, happiness, autonomy, or social relationships for pleasure. Likewise, the fact that a behavior pattern is valued, accepted, encouraged, or even statistically normative in a culture does not necessarily mean that it is conducive to optimal psychological functioning.
People in all cultures find some behaviors bizarre or even incomprehensible. But just what they feel is bizarre or incomprehensible is ambiguous and subjective. These differences in determination can become highly contentious. The process by which conditions and difficulties come to be defined and treated as medical conditions and problems, and thus come under the authority of doctors and other health professionals, is known as medicalization or pathologization.
Different societies or cultures, even different individuals in a subculture, can disagree as to what constitutes optimal versus pathological biological and psychological functioning. Research has demonstrated that cultures vary in the relative importance placed on, for example, happiness, autonomy, or social relationships for pleasure. Likewise, the fact that a behavior pattern is valued, accepted, encouraged, or even statistically normative in a culture does not necessarily mean that it is conducive to optimal psychological functioning.
People in all cultures find some behaviors bizarre or even incomprehensible. But just what they feel is bizarre or incomprehensible is ambiguous and subjective. These differences in determination can become highly contentious. The process by which conditions and difficulties come to be defined and treated as medical conditions and problems, and thus come under the authority of doctors and other health professionals, is known as medicalization or pathologization.
Mental illness in the Latin American community
There is a perception in Latin American communities, especially among older people, that discussing problems with mental health can create embarrassment and shame for the family. This results in fewer people seeking treatment.
Latin Americans from the USA, are slightly more likely to have a mental health disorder than first-generation Latin American immigrants, although differences between ethnic groups were found to disappear after adjustment for place of birth.
Religion
Religious, spirituality, spiritual, or transpersonal experiences and beliefs meet many criteria of delusional or psychotic disorders. A belief or experience can sometimes be shown to produce distress or disability—the ordinary standard for judging mental disorders. There is a link between religion and schizophrenia,
Movements
 Controversy has often surrounded psychiatry, and the term anti-psychiatry was coined by the psychiatrist David Cooper (psychiatrist), David Cooper in 1967. The anti-psychiatry message is that psychiatric treatments are ultimately more damaging than helpful to patients, and psychiatry's history involves what may now be seen as dangerous treatments.
Controversy has often surrounded psychiatry, and the term anti-psychiatry was coined by the psychiatrist David Cooper (psychiatrist), David Cooper in 1967. The anti-psychiatry message is that psychiatric treatments are ultimately more damaging than helpful to patients, and psychiatry's history involves what may now be seen as dangerous treatments.[ Electroconvulsive therapy was one of these, which was used widely between the 1930s and 1960s. Lobotomy was another practice that was ultimately seen as too invasive and brutal. Diazepam and other sedatives were sometimes over-prescribed, which led to an epidemic of dependence. There was also concern about the large increase in prescribing psychiatric drugs for children. Some charismatic psychiatrists came to personify the movement against psychiatry. The most influential of these was R.D. Laing who wrote a series of best-selling books, including ''The Divided Self''. Thomas Szasz wrote ''The Myth of Mental Illness''. Some ex-patient groups have become militantly anti-psychiatric, often referring to themselves as Psychiatric survivors movement, survivors.][The Antipsychiatry Coalition. (26 November 2005). The Antipsychiatry Coalition. Retrieved 19 April 2007, from antipsychiatry.org]
Alternatively, a movement for global mental health has emerged, defined as 'the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide'.
Cultural bias
Diagnostic guidelines of the 2000s, namely the DSM and to some extent the ICD, have been criticized as having a fundamentally Euro-American outlook. Opponents argue that even when diagnostic criteria are used across different cultures, it does not mean that the underlying constructs have validity within those cultures, as even reliable application can prove only consistency, not legitimacy.
Laws and policies
Three-quarters of countries around the world have mental health legislation. Compulsory admission to mental health facilities (also known as involuntary commitment) is a controversial topic. It can impinge on personal liberty and the right to choose, and carry the risk of abuse for political, social, and other reasons; yet it can potentially prevent harm to self and others, and assist some people in attaining their right to healthcare when they may be unable to decide in their own interests.
Perception and discrimination
Stigma
The social stigma associated with mental disorders is a widespread problem. The US Surgeon General stated in 1999 that: "Powerful and pervasive, stigma prevents people from acknowledging their own mental health problems, much less disclosing them to others."
Media and general public
Media coverage of mental illness comprises predominantly negative and pejorative depictions, for example, of incompetence, violence or criminality, with far less coverage of positive issues such as accomplishments or human rights issues. Such negative depictions, including in children's cartoons, are thought to contribute to stigma and negative attitudes in the public and in those with mental health problems themselves, although more sensitive or serious cinematic portrayals have increased in prevalence.
In the United States, the Carter Center has created fellowships for journalists in South Africa, the U.S., and Romania, to enable reporters to research and write stories on mental health topics.
Violence
Despite public or media opinion, national studies have indicated that severe mental illness does not independently predict future violent behavior, on average, and is not a leading cause of violence in society. There is a statistical association with various factors that do relate to violence (in anyone), such as substance use and various personal, social, and economic factors.
Mental health
The recognition and understanding of mental health
Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. It likewise determines how an individual handles Stress (biology), stress, interpersonal relationships, and decision-maki ...
conditions have changed over time and across cultures and there are still variations in definition, assessment, and classification of mental disorders, classification, although standard guideline criteria are widely used. In many cases, there appears to be a continuum between mental health and mental illness, making diagnosis complex.[ According to the World Health Organization, over a third of people in most countries report problems at some time in their life which meet the criteria for diagnosis of one or more of the common types of mental disorder.]
Other animals
Psychopathology in non-human primates has been studied since the mid-20th century. Over 20 behavioral patterns in captive chimpanzees have been documented as (statistically) abnormal for frequency, severity or oddness—some of which have also been observed in the wild. Captive great apes show gross behavioral abnormalities such as stereotypy of movements, self-mutilation, disturbed emotional reactions (mainly fear or aggression) towards companions, lack of species-typical communications, and generalized learned helplessness. In some cases such behaviors are hypothesized to be equivalent to symptoms associated with psychiatric disorders in humans such as depression, anxiety disorders, eating disorders and post-traumatic stress disorder. Concepts of antisocial, borderline and schizoid personality disorders have also been applied to non-human great apes.
See also
*List of mental disorders
*Mental illness portrayed in media
**Mental disorders in film
**Mental illness in fiction
*Mental illness in American prisons
*Parity of esteem
*Psychological evaluation
References
Further reading
*
*
*
*
*
*
Stanford Encyclopedia of Philosophy
*
*
*
External links
Overcoming Mental Health Stigma in the Latino Community – Consult QD
clevelandclinic.org
National Institute of Mental Health
{{Authority control
Disability by type
Mental disorders,
Abnormal psychology
Psychopathology
Psychiatric assessment
Suffering
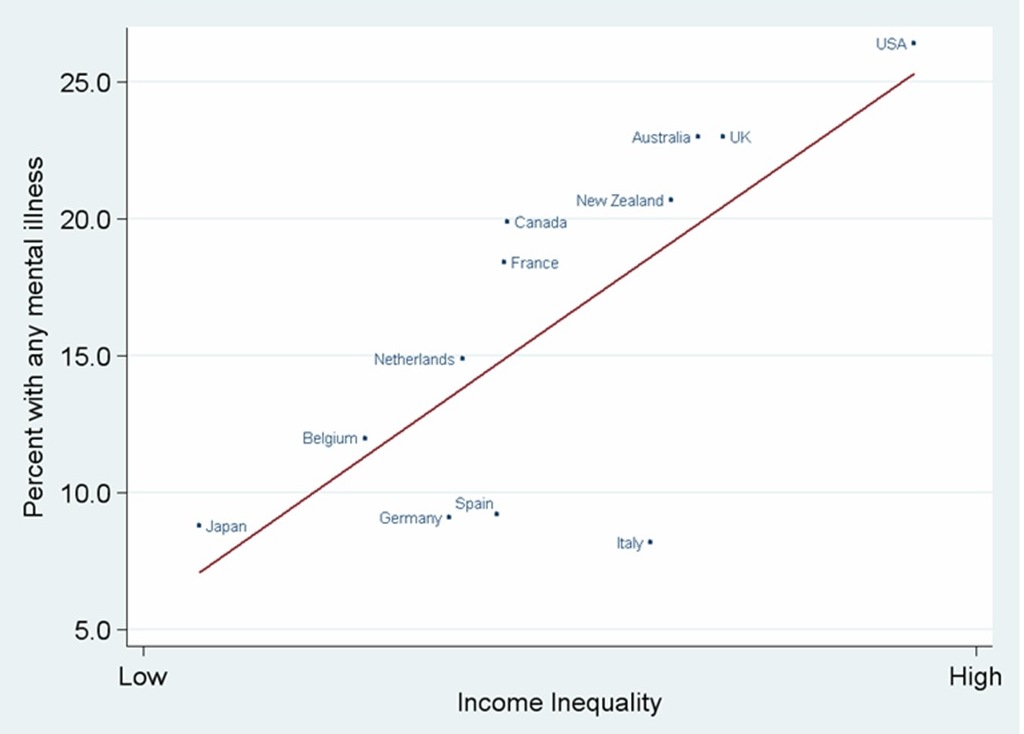 During the prenatal stage, factors like unwanted pregnancy, lack of adaptation to pregnancy or substance use during pregnancy increases the risk of developing a mental disorder. Maternal stress and birth complications including prematurity and infections have also been implicated in increasing susceptibility for mental illness. Infants neglected or not provided optimal nutrition have a higher risk of developing cognitive impairment.
Social influences have also been found to be important, including
During the prenatal stage, factors like unwanted pregnancy, lack of adaptation to pregnancy or substance use during pregnancy increases the risk of developing a mental disorder. Maternal stress and birth complications including prematurity and infections have also been implicated in increasing susceptibility for mental illness. Infants neglected or not provided optimal nutrition have a higher risk of developing cognitive impairment.
Social influences have also been found to be important, including  Treatment and support for mental disorders are provided in psychiatric hospitals, clinics or a range of community mental health services. In some countries services are increasingly based on a recovery approach, intended to support individual's personal journey to gain the kind of life they want.
There is a range of different types of treatment and what is most suitable depends on the disorder and the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication. In a minority of cases, individuals may be treated against their will, which can cause particular difficulties depending on how it is carried out and perceived. Compulsory treatment while in the community versus non-compulsory treatment does not appear to make much of a difference except by maybe decreasing victimization.
Treatment and support for mental disorders are provided in psychiatric hospitals, clinics or a range of community mental health services. In some countries services are increasingly based on a recovery approach, intended to support individual's personal journey to gain the kind of life they want.
There is a range of different types of treatment and what is most suitable depends on the disorder and the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication. In a minority of cases, individuals may be treated against their will, which can cause particular difficulties depending on how it is carried out and perceived. Compulsory treatment while in the community versus non-compulsory treatment does not appear to make much of a difference except by maybe decreasing victimization.
 The turn of the 20th century saw the development of psychoanalysis, which would later come to the fore, along with Emil Kraepelin, Kraepelin's classification scheme. Asylum "inmates" were increasingly referred to as "patients", and asylums were renamed as hospitals.
The turn of the 20th century saw the development of psychoanalysis, which would later come to the fore, along with Emil Kraepelin, Kraepelin's classification scheme. Asylum "inmates" were increasingly referred to as "patients", and asylums were renamed as hospitals.
 Early in the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "Combat stress reaction, shell shock".
World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first ''Diagnostic and Statistical Manual of Mental Disorders''. The International Classification of Diseases (ICD) also developed a section on mental disorders. The term stress (biological), stress, having emerged from endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomy, lobotomies and the neuroleptic chlorpromazine came to be used by mid-century. In the 1960s there were many challenges to the concept of mental illness itself. These challenges came from psychiatrists like Thomas Szasz who argued that mental illness was a myth used to disguise moral conflicts; from sociologists such as Erving Goffman who said that mental illness was merely another example of how society labels and controls non-conformists; from behavioral psychologists who challenged psychiatry's fundamental reliance on unobservable phenomena; and from gay rights activists who criticised the APA's listing of homosexuality as a mental disorder. A study published in ''Science'' by Rosenhan experiment, Rosenhan received much publicity and was viewed as an attack on the efficacy of psychiatric diagnosis.
Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A Psychiatric survivors movement, consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" (later antidepressants) and lithium pharmacology, lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience, genetics, and psychology led to new research agendas. Cognitive behavioral therapy and other psychotherapies developed. The ''DSM'' and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI-type antidepressants became some of the most widely prescribed drugs in the world, as later did antipsychotics. Also during the 1990s, a recovery approach developed.
Early in the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "Combat stress reaction, shell shock".
World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first ''Diagnostic and Statistical Manual of Mental Disorders''. The International Classification of Diseases (ICD) also developed a section on mental disorders. The term stress (biological), stress, having emerged from endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomy, lobotomies and the neuroleptic chlorpromazine came to be used by mid-century. In the 1960s there were many challenges to the concept of mental illness itself. These challenges came from psychiatrists like Thomas Szasz who argued that mental illness was a myth used to disguise moral conflicts; from sociologists such as Erving Goffman who said that mental illness was merely another example of how society labels and controls non-conformists; from behavioral psychologists who challenged psychiatry's fundamental reliance on unobservable phenomena; and from gay rights activists who criticised the APA's listing of homosexuality as a mental disorder. A study published in ''Science'' by Rosenhan experiment, Rosenhan received much publicity and was viewed as an attack on the efficacy of psychiatric diagnosis.
Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A Psychiatric survivors movement, consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" (later antidepressants) and lithium pharmacology, lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience, genetics, and psychology led to new research agendas. Cognitive behavioral therapy and other psychotherapies developed. The ''DSM'' and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI-type antidepressants became some of the most widely prescribed drugs in the world, as later did antipsychotics. Also during the 1990s, a recovery approach developed.
 Controversy has often surrounded psychiatry, and the term anti-psychiatry was coined by the psychiatrist David Cooper (psychiatrist), David Cooper in 1967. The anti-psychiatry message is that psychiatric treatments are ultimately more damaging than helpful to patients, and psychiatry's history involves what may now be seen as dangerous treatments. Electroconvulsive therapy was one of these, which was used widely between the 1930s and 1960s. Lobotomy was another practice that was ultimately seen as too invasive and brutal. Diazepam and other sedatives were sometimes over-prescribed, which led to an epidemic of dependence. There was also concern about the large increase in prescribing psychiatric drugs for children. Some charismatic psychiatrists came to personify the movement against psychiatry. The most influential of these was R.D. Laing who wrote a series of best-selling books, including ''The Divided Self''. Thomas Szasz wrote ''The Myth of Mental Illness''. Some ex-patient groups have become militantly anti-psychiatric, often referring to themselves as Psychiatric survivors movement, survivors. Giorgio Antonucci has questioned the basis of psychiatry through his work on the dismantling of two psychiatric hospitals (in the city of Imola), carried out from 1973 to 1996.
The consumer/survivor movement (also known as user/survivor movement) is made up of individuals (and organizations representing them) who are clients of mental health services or who consider themselves survivors of psychiatric interventions. Activists campaign for improved mental health services and for more involvement and empowerment within mental health services, policies and wider society. Patient advocacy organizations have expanded with increasing deinstitutionalization in developed countries, working to challenge the stereotypes, stigma and exclusion associated with psychiatric conditions. There is also a carers rights movement of people who help and support people with mental health conditions, who may be relatives, and who often work in difficult and time-consuming circumstances with little acknowledgement and without pay. An anti-psychiatry movement fundamentally challenges mainstream psychiatric theory and practice, including in some cases asserting that psychiatric concepts and diagnoses of 'mental illness' are neither real nor useful.The Antipsychiatry Coalition. (26 November 2005). The Antipsychiatry Coalition. Retrieved 19 April 2007, from antipsychiatry.org
Alternatively, a movement for global mental health has emerged, defined as 'the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide'.
Controversy has often surrounded psychiatry, and the term anti-psychiatry was coined by the psychiatrist David Cooper (psychiatrist), David Cooper in 1967. The anti-psychiatry message is that psychiatric treatments are ultimately more damaging than helpful to patients, and psychiatry's history involves what may now be seen as dangerous treatments. Electroconvulsive therapy was one of these, which was used widely between the 1930s and 1960s. Lobotomy was another practice that was ultimately seen as too invasive and brutal. Diazepam and other sedatives were sometimes over-prescribed, which led to an epidemic of dependence. There was also concern about the large increase in prescribing psychiatric drugs for children. Some charismatic psychiatrists came to personify the movement against psychiatry. The most influential of these was R.D. Laing who wrote a series of best-selling books, including ''The Divided Self''. Thomas Szasz wrote ''The Myth of Mental Illness''. Some ex-patient groups have become militantly anti-psychiatric, often referring to themselves as Psychiatric survivors movement, survivors. Giorgio Antonucci has questioned the basis of psychiatry through his work on the dismantling of two psychiatric hospitals (in the city of Imola), carried out from 1973 to 1996.
The consumer/survivor movement (also known as user/survivor movement) is made up of individuals (and organizations representing them) who are clients of mental health services or who consider themselves survivors of psychiatric interventions. Activists campaign for improved mental health services and for more involvement and empowerment within mental health services, policies and wider society. Patient advocacy organizations have expanded with increasing deinstitutionalization in developed countries, working to challenge the stereotypes, stigma and exclusion associated with psychiatric conditions. There is also a carers rights movement of people who help and support people with mental health conditions, who may be relatives, and who often work in difficult and time-consuming circumstances with little acknowledgement and without pay. An anti-psychiatry movement fundamentally challenges mainstream psychiatric theory and practice, including in some cases asserting that psychiatric concepts and diagnoses of 'mental illness' are neither real nor useful.The Antipsychiatry Coalition. (26 November 2005). The Antipsychiatry Coalition. Retrieved 19 April 2007, from antipsychiatry.org
Alternatively, a movement for global mental health has emerged, defined as 'the area of study, research and practice that places a priority on improving mental health and achieving equity in mental health for all people worldwide'.