Spirometry on:
[Wikipedia]
[Google]
[Amazon]
 Spirometry (meaning ''the measuring of breath'') is the most common of the
Spirometry (meaning ''the measuring of breath'') is the most common of the

ATS/ERS Standardisation of Spirometry
Generally, the patient is asked to take the deepest breath they can, and then exhale into the sensor as hard as possible, for as long as possible, preferably at least 6 seconds. It is sometimes directly followed by a rapid inspiration, (inhalation) in particular when assessing possible
 Peak expiratory flow (PEF) is the maximal flow (or speed) achieved during the maximally forced expiration initiated at full inspiration, measured in liters per minute or in liters per second.
Peak expiratory flow (PEF) is the maximal flow (or speed) achieved during the maximally forced expiration initiated at full inspiration, measured in liters per minute or in liters per second.
Forced Expiratory Time (FET) measures the length of the expiration in seconds. Slow vital capacity (SVC)
Slow
Pmax is the asymptotically maximal pressure that can be developed by the respiratory muscles at any lung volume and Pi is the maximum inspiratory pressure that can be developed at specific lung volumes. This measurement also requires pressure transducers in addition. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition. A derived parameter is the coefficient of retraction (CR) which is Pmax/TLC . Mean transit time (MTT)
Mean transit time is the area under the flow-volume curve divided by the forced vital capacity. Maximal inspiratory pressure (MIP) MIP, also known as negative inspiratory force (NIF), is the maximum pressure that can be generated against an occluded airway beginning at functional residual capacity (FRC). It is a marker of respiratory muscle function and strength. Represented by centimeters of water pressure (cmH2O) and measured with a
American Thoracic Society
(ATS)
European Respiratory Society
(ERS) {{Respiratory system procedures Pulmonary function testing Respiratory physiology Respiratory therapy
pulmonary function test
Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity ...
s (PFTs). It measures lung
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of t ...
function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma
Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, co ...
, pulmonary fibrosis
Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failu ...
, cystic fibrosis
Cystic fibrosis (CF) is a rare genetic disorder that affects mostly the lungs, but also the pancreas, liver, kidneys, and intestine. Long-term issues include difficulty breathing and coughing up mucus as a result of frequent lung infections. O ...
, and COPD
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms include shortness of breath and a cough, which may or may not produce ...
. It is also helpful as part of a system of health surveillance Health surveillance may refer to:
* Public health surveillance
* Workplace health surveillance
Workplace health surveillance or occupational health surveillance (U.S.) is the ongoing systematic collection, analysis, and dissemination of exposure ...
, in which breathing patterns are measured over time.
Spirometry generates pneumotachographs, which are charts that plot the volume and flow of air coming in and out of the lungs from one inhalation and one exhalation.
Indications
Spirometry is indicated for the following reasons: * to diagnose or manage asthma * to detect respiratory disease in patients presenting with symptoms of breathlessness, and to distinguish respiratory fromcardiac disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, hea ...
as the cause
* to measure bronchial responsiveness in patients suspected of having asthma
* to diagnose and differentiate between obstructive lung disease
Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessiv ...
and restrictive lung disease
Restrictive lung diseases are a category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenat ...
* to follow the natural history of disease
The natural history of disease is the course a disease takes in individual people from its pathological onset ("inception") until its resolution (either through complete recovery or eventual death). The inception of a disease is not a firmly defin ...
in respiratory conditions
* to assess of impairment from occupational asthma
Occupational asthma is new onset asthma or the recurrence of previously quiescent asthma directly caused by exposure to an agent at workplace. It is an occupational lung disease and a type of work-related asthma. Agents that can induce occupationa ...
* to identify those at risk from pulmonary barotrauma
Barotrauma is physical damage to body tissues caused by a difference in pressure between a gas space inside, or contact with, the body and the surrounding gas or liquid. The initial damage is usually due to over-stretching the tissues in tens ...
while scuba diving
Scuba diving is a mode of underwater diving whereby divers use breathing equipment that is completely independent of a surface air supply. The name "scuba", an acronym for " Self-Contained Underwater Breathing Apparatus", was coined by Chr ...
* to conduct pre-operative risk assessment before anaesthesia or cardiothoracic surgery
Cardiothoracic surgery is the field of medicine involved in surgical treatment of organs inside the thoracic cavity — generally treatment of conditions of the heart (heart disease), lungs ( lung disease), and other pleural or mediastinal str ...
* to measure response to treatment of conditions which spirometry detects
* to diagnose the vocal cord dysfunction
Vocal cord dysfunction (VCD) is a pathology affecting the vocal folds (commonly referred to as the vocal cords) characterized by full or partial vocal fold closure causing difficulty and distress during respiration, especially during inhalation.
...
.
Contraindications
Forced expiratory maneuvers may aggravate some medical conditions. Spirometry should not be performed when the individual presents with: * Hemoptysis of unknown origin * Pneumothorax * Unstable cardiovascular status (angina, recent myocardial infarction, etc.) * Thoracic, abdominal, or cerebral aneurysms * Cataracts or recent eye surgery * Recent thoracic or abdominal surgery * Nausea, vomiting, or acute illness * Recent or current viral infection * Undiagnosed hypertensionSpirometry testing

Spirometer
The spirometry test is performed using a device called aspirometer
A spirometer is an apparatus for measuring the volume of air inspired and expired by the lungs. A spirometer measures ventilation, the movement of air into and out of the lungs. The spirogram will identify two different types of abnormal ventilat ...
, which comes in several different varieties. Most spirometers display the following graphs, called spirograms:
* a ''volume-time curve'', showing volume (litres) along the Y-axis and time (seconds) along the X-axis
* a ''flow-volume loop'', which graphically depicts the rate of airflow on the Y-axis and the total volume inspired or expired on the X-axis
Procedure
The basic forced volume vital capacity (FVC) test varies slightly depending on the equipment used, either closed circuit or open circuit, but should follow thATS/ERS Standardisation of Spirometry
Generally, the patient is asked to take the deepest breath they can, and then exhale into the sensor as hard as possible, for as long as possible, preferably at least 6 seconds. It is sometimes directly followed by a rapid inspiration, (inhalation) in particular when assessing possible
upper airway obstruction
Airway obstruction is a blockage of respiration in the airway that hinders the free flow of air. It can be broadly classified into being either in the upper airway (UPA) or lower airway (LOA).
Airway obstruction is a life-threatening condition a ...
. Sometimes, the test will be preceded by a period of quiet breathing in and out from the sensor (tidal volume), or the rapid breath in (forced inspiratory part) will come before the forced expiration.
During the test, soft nose clips may be used to prevent air escaping through the nose. Filter mouthpieces may be used to prevent the spread of microorganisms.
Limitations of test
The maneuver is highly dependent on patient cooperation and effort, and is normally repeated at least three times to ensure reproducibility. Since results are dependent on patient cooperation, FVC can only be underestimated, never overestimated. Due to the patient cooperation required, spirometry can only be used on children old enough to comprehend and follow the instructions given (6 years old or more), and only on patients who are able to understand and follow instructions — thus, this test is not suitable for patients who are unconscious, heavily sedated, or have limitations that would interfere with vigorous respiratory efforts. Other types of lung function tests are available for infants and unconscious persons. Another major limitation is the fact that many intermittent or mild asthmatics have normal spirometry between acute exacerbation, limiting spirometry's usefulness as a diagnostic. It is more useful as a monitoring tool: a sudden decrease in FEV1 or other spirometric measure in the same patient can signal worsening control, even if the raw value is still normal. Patients are encouraged to record their personal best measures.Related tests
Spirometry can also be part of abronchial challenge test
A bronchial challenge test is a medical test used to assist in the diagnosis of asthma. The patient breathes in nebulized methacholine or histamine. Thus the test may also be called a methacholine challenge test or histamine challenge test respec ...
, used to determine bronchial
A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi pronounced (BRAN-KAI) to branch from the trachea at the carina are the right main bronchus and the left main bronchus. ...
hyperresponsiveness to either rigorous exercise, inhalation of cold/dry air, or with a pharmaceutical agent such as methacholine
Methacholine ( INN, USAN) (trade name Provocholine), also known as Acetyl-β-methylcholine, is a synthetic choline ester that acts as a non-selective muscarinic receptor agonist in the parasympathetic nervous system.
Medical uses
Methacholine ...
or histamine
Histamine is an organic nitrogenous compound involved in local immune responses, as well as regulating physiological functions in the gut and acting as a neurotransmitter for the brain, spinal cord, and uterus. Since histamine was discovered ...
.
Sometimes, to assess the reversibility of a particular condition, a bronchodilator
A bronchodilator or broncholytic (although the latter occasionally includes secretory inhibition as well) is a substance that dilates the bronchi and bronchioles, decreasing resistance in the respiratory airway and increasing airflow to the lung ...
is administered before performing another round of tests for comparison. This is commonly referred to as a ''reversibility test'', or a ''post bronchodilator test
The post bronchodilator test (Post BD), also commonly referred to as a reversibility test, is a test that utilizes spirometry to assess possible reversibility of bronchoconstriction in diseases such as asthma.
Indications
This procedure is indica ...
'' (Post BD), and is an important part in diagnosing asthma versus COPD.
Other complementary lung functions tests include plethysmography
A plethysmograph is an instrument for measuring changes in volume within an organ or whole body (usually resulting from fluctuations in the amount of blood or air it contains). The word is derived from the Greek "plethysmos" (increasing, enlar ...
and nitrogen washout
Nitrogen washout (or Fowler's method) is a test for measuring anatomic dead space in the lung during a respiratory cycle, as well as some parameters related to the closure of airways.
Procedure
A nitrogen washout can be performed with a single n ...
.
Parameters
The most common parameters measured in spirometry are Vital capacity (VC), Forced vital capacity (FVC), Forced expiratory volume (FEV) at timed intervals of 0.5, 1.0 (FEV1), 2.0, and 3.0 seconds, forced expiratory flow 25–75% (FEF 25–75) and maximal voluntary ventilation (MVV), also known as Maximum breathing capacity. Other tests may be performed in certain situations. Results are usually given in both raw data (litres, litres per second) and percent predicted—the test result as a percent of the "predicted values" for the patients of similar characteristics (height, age, sex, and sometimes race and weight). The interpretation of the results can vary depending on the physician and the source of the predicted values. Generally speaking, results nearest to 100% predicted are the most normal, and results over 80% are often considered normal. Multiple publications of predicted values have been published and may be calculated based on age, sex, weight and ethnicity. However, review by a doctor is necessary for accurate diagnosis of any individual situation. A bronchodilator is also given in certain circumstances and a pre/post graph comparison is done to assess the effectiveness of the bronchodilator. See the example printout.Functional residual capacity
Functional residual capacity (FRC) is the volume of air present in the lungs at the end of passive expiration. At FRC, the opposing elastic recoil forces of the lungs and chest wall are in equilibrium and there is no exertion by the diaphragm ...
(FRC) cannot be measured via spirometry, but it can be measured with a plethysmograph
A plethysmograph is an instrument for measuring changes in volume within an organ or whole body (usually resulting from fluctuations in the amount of blood or air it contains). The word is derived from the Greek "plethysmos" (increasing, enla ...
or dilution tests (for example, helium dilution test).
Forced vital capacity (FVC)
Forcedvital capacity
Vital capacity (VC) is the maximum amount of air a person can inhale after a maximum exhalation. It is equal to the sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume. It is approximately equal to Forced Vital Capacity ( ...
(FVC) is the volume of air that can forcibly be blown out after full inspiration, measured in liters. FVC is the most basic maneuver in spirometry tests.
Forced expiratory volume in 1 second (FEV1)
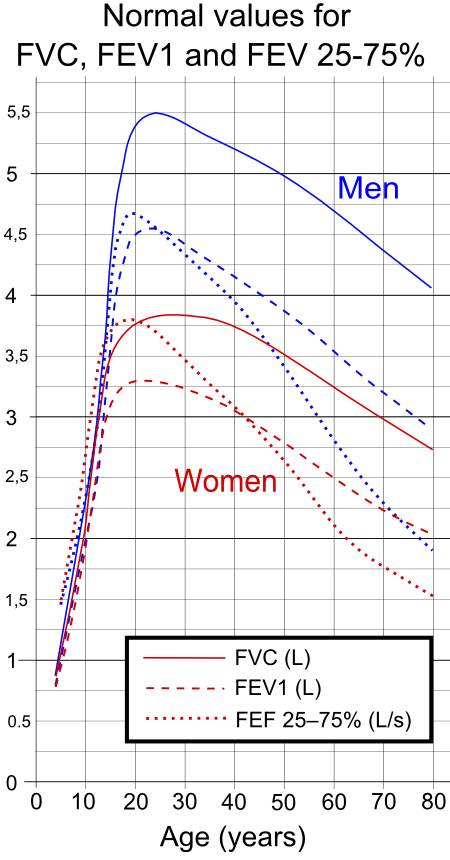
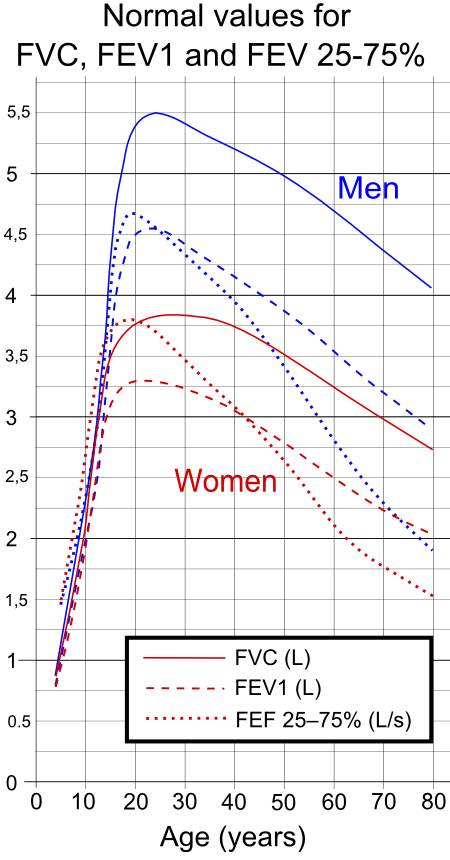
FEV1 is the volume of air that can forcibly be blown out in first 1-second, after full inspiration. Average values for FEV1 in healthy people depend mainly on sex and age, according to the diagram. Values of between 80% and 120% of the average value are considered normal.LUNGFUNKTION — Practice compendium for semester 6. Department of Medical Sciences, Clinical Physiology, Academic Hospital, Uppsala, Sweden. Retrieved 2010. Predicted normal values for FEV1 can be calculated and depend on age, sex, height, mass and ethnicity as well as the research study that they are based on.FEV1/FVC ratio
FEV1/FVC
The FEV1/FVC ratio, also called Tiffeneau-Pinelli index, is a calculated ratio used in the diagnosis of obstructive and restrictive lung disease. It represents the proportion of a person's vital capacity that they are able to expire in the firs ...
is the ratio of FEV1 to FVC. In healthy adults this should be approximately 70–80% (declining with age). In obstructive diseases (asthma, COPD, chronic bronchitis, emphysema) FEV1 is diminished because of increased airway resistance to expiratory flow; the FVC may be decreased as well, due to the premature closure of airway in expiration, just not in the same proportion as FEV1 (for instance, both FEV1 and FVC are reduced, but the former is more affected because of the increased airway resistance). This generates a reduced value (<70%, often ~45%). In restrictive diseases (such as pulmonary fibrosis
Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failu ...
) the FEV1 and FVC are both reduced proportionally and the value may be normal or even increased as a result of decreased lung compliance.
A derived value of FEV1 is FEV1% predicted (FEV1%), which is defined as FEV1 of the patient divided by the average FEV1 in the population for any person of the same age, height, gender, and race.
Forced expiratory flow (FEF)
Forced expiratory flow (FEF) is the flow (or speed) of air coming out of the lung during the middle portion of a forced expiration. It can be given at discrete times, generally defined by what fraction of the forced vital capacity (FVC) has been exhaled. The usual discrete intervals are 25%, 50% and 75% (FEF25, FEF50 and FEF75), or 25% and 50% of FVC that has been exhaled. It can also be given as a mean of the flow during an interval, also generally delimited by when specific fractions remain of FVC, usually 25–75% (FEF25–75%). Average ranges in the healthy population depend mainly on sex and age, with FEF25–75% shown in diagram at left. Values ranging from 50 to 60% and up to 130% of the average are considered normal. Predicted normal values for FEF can be calculated and depend on age, sex, height, mass and ethnicity as well as the research study that they are based on. MMEF or MEF stands for maximal (mid-)expiratory flow and is the peak of expiratory flow as taken from the flow-volume curve and measured in liters per second. It should theoretically be identical to peak expiratory flow (PEF), which is, however, generally measured by a peak flow meter and given in liters per minute.Interpretation model — compendium at Uppsala Academic Hospital. By H. Hedenström. 2009-02-04 Recent research suggests that FEF25-75% or FEF25-50% may be a more sensitive parameter than FEV1 in the detection of obstructive small airway disease. However, in the absence of concomitant changes in the standard markers, discrepancies in mid-range expiratory flow may not be specific enough to be useful, and current practice guidelines recommend continuing to use FEV1, VC, and FEV1/VC as indicators of obstructive disease. More rarely, forced expiratory flow may be given at intervals defined by how much remains of total lung capacity. In such cases, it is usually designated as e.g. FEF70%TLC, FEF60%TLC and FEF50%TLC.Forced inspiratory flow 25–75% or 25–50%
Forced inspiratory flow 25–75% or 25–50% (FIF 25–75% or 25–50%) is similar to FEF 25–75% or 25–50% except the measurement is taken during inspiration.Peak expiratory flow (PEF)
Tidal volume (TV)
Tidal volume
Tidal volume (symbol VT or TV) is the volume of air moved into or out of the lungs during a normal breath. In a healthy, young human adult, tidal volume is approximately 500 ml per inspiration or 7 ml/kg of body mass.
Mechanical vent ...
is the amount of air inhaled or exhaled normally at rest.
Total lung capacity (TLC)
Total lung capacity
Lung volumes and lung capacities refer to the volume of air in the lungs at different phases of the respiratory cycle.
The average total lung capacity of an adult human male is about 6 litres of air.
Tidal breathing is normal, resting breathi ...
(TLC) is the maximum volume of air present in the lungs.
Diffusing capacity (DLCO)
Diffusing capacity
Diffusing capacity of the lung (DL) (also known as Transfer factor is another expression for the formerly used diffusing capacity.) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a c ...
(or DLCO DLCO or TLCO ( diffusing capacity or transfer factor of the lung for carbon monoxide (CO),) is the extent to which oxygen passes from the air sacs of the lungs into the blood. Commonly, it refers to the test used to determine this parameter. It was ...
) is the carbon monoxide uptake from a single inspiration in a standard time (usually 10 seconds). During the test the person inhales a test gas mixture that consisting of regular air that includes an inert tracer gas
A tracer-gas leak testing method is a nondestructive testing method that detects gas leaks. A variety of methods with different sensitivities exist. Tracer-gas leak testing is used in the petrochemical industry, the automotive industry, and in the ...
and CO, less than one percent. Since hemoglobin has a greater affinity to CO than oxygen the breath-hold time can be only 10 seconds, which is a sufficient amount of time for this transfer of CO to occur. Since the inhaled amount of CO is known, the exhaled CO is subtracted to determine the amount transferred during the breath-hold time. The tracer gas is analyzed simultaneously with CO to determine the distribution of the test gas mixture. This test will pick up diffusion impairments, for instance in pulmonary fibrosis. This must be corrected for anemia (a low hemoglobin concentration will reduce DLCO) and pulmonary hemorrhage (excess RBC's in the interstitium or alveoli can absorb CO and artificially increase the DLCO capacity). Atmospheric pressure and/or altitude will also affect measured DLCO, and so a correction factor is needed to adjust for standard pressure.
Maximum voluntary ventilation (MVV)
Maximum voluntary ventilation (MVV) is a measure of the maximum amount of air that can be inhaled and exhaled within one minute. For the comfort of the patient this is done over a 15-second time period before being extrapolated to a value for one minute expressed as liters/minute. Average values for males and females are 140–180 and 80–120 liters per minute respectively.Static lung compliance (Cst)
When estimating static lung compliance, volume measurements by the spirometer needs to be complemented bypressure transducer
A pressure sensor is a device for pressure measurement of gases or liquids. Pressure is an expression of the force required to stop a fluid from expanding, and is usually stated in terms of force per unit area. A pressure sensor usually act ...
s in order to simultaneously measure the transpulmonary pressure Transpulmonary pressure is the difference between the alveolar pressure and the intrapleural pressure in the pleural cavity. During human ventilation, air flows because of pressure gradients.
Ptp = Palv – Pip. Where Ptp is transpulmonary pressu ...
. When having drawn a curve with the relations between changes in volume to changes in transpulmonary pressure, Cst is the slope of the curve during any given volume, or, mathematically, ΔV/ΔP. Static lung compliance is perhaps the most sensitive parameter for the detection of abnormal pulmonary mechanics. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition.
In those with acute respiratory failure on mechanical ventilation, "the static compliance of the total respiratory system is conventionally obtained by dividing the tidal volume by the difference between the 'plateau' pressure measured at the airway opening (PaO) during an occlusion at end-inspiration and positive end-expiratory pressure (PEEP) set by the ventilator".
Others
Forced Expiratory Time (FET)Forced Expiratory Time (FET) measures the length of the expiration in seconds. Slow vital capacity (SVC)
Slow
vital capacity
Vital capacity (VC) is the maximum amount of air a person can inhale after a maximum exhalation. It is equal to the sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume. It is approximately equal to Forced Vital Capacity ( ...
(SVC) is the maximum volume of air that can be exhaled slowly after slow maximum inhalation.
Maximal pressure (Pmax and Pi)
Pmax is the asymptotically maximal pressure that can be developed by the respiratory muscles at any lung volume and Pi is the maximum inspiratory pressure that can be developed at specific lung volumes. This measurement also requires pressure transducers in addition. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition. A derived parameter is the coefficient of retraction (CR) which is Pmax/TLC . Mean transit time (MTT)
Mean transit time is the area under the flow-volume curve divided by the forced vital capacity. Maximal inspiratory pressure (MIP) MIP, also known as negative inspiratory force (NIF), is the maximum pressure that can be generated against an occluded airway beginning at functional residual capacity (FRC). It is a marker of respiratory muscle function and strength. Represented by centimeters of water pressure (cmH2O) and measured with a
manometer
Pressure measurement is the measurement of an applied force by a fluid (liquid or gas) on a surface. Pressure is typically measured in units of force per unit of surface area. Many techniques have been developed for the measurement of pressu ...
. Maximum inspiratory pressure is an important and noninvasive index of diaphragm strength and an independent tool for diagnosing many illnesses. Typical maximum inspiratory pressures in adult males can be estimated from the equation, MIP = 142 - (1.03 x Age) cmH2O, where age is in years.
Technologies used in spirometers
* Volumetric Spirometers ** Water bell **Bellows
A bellows or pair of bellows is a device constructed to furnish a strong blast of air. The simplest type consists of a flexible bag comprising a pair of rigid boards with handles joined by flexible leather sides enclosing an approximately airtig ...
wedge
* Flow measuring Spirometers
** Fleisch-pneumotach
** Lilly (screen) pneumotach
** Turbine
A turbine ( or ) (from the Greek , ''tyrbē'', or Latin ''turbo'', meaning vortex) is a rotary mechanical device that extracts energy from a fluid flow and converts it into useful work. The work produced by a turbine can be used for generating ...
/Stator Rotor (normally incorrectly referred to as a turbine. Actually a rotating vane which spins because of the air flow generated by the subject. The revolutions of the vane are counted as they break a light beam)
** Pitot tube
A pitot ( ) tube (pitot probe) measures fluid flow velocity. It was invented by a French engineer, Henri Pitot, in the early 18th century, and was modified to its modern form in the mid-19th century by a French scientist, Henry Darcy. It ...
** Hot-wire anemometer
In meteorology, an anemometer () is a device that measures wind speed and direction. It is a common instrument used in weather stations. The earliest known description of an anemometer was by Italian architect and author Leon Battista Alberti ...
** Ultrasound
Ultrasound is sound waves with frequencies higher than the upper audible limit of human hearing. Ultrasound is not different from "normal" (audible) sound in its physical properties, except that humans cannot hear it. This limit varies ...
See also
* Peak flow meter *Nitrogen washout
Nitrogen washout (or Fowler's method) is a test for measuring anatomic dead space in the lung during a respiratory cycle, as well as some parameters related to the closure of airways.
Procedure
A nitrogen washout can be performed with a single n ...
References
Further reading
*External links
American Thoracic Society
(ATS)
European Respiratory Society
(ERS) {{Respiratory system procedures Pulmonary function testing Respiratory physiology Respiratory therapy