Strep B on:
[Wikipedia]
[Google]
[Amazon]
Group B streptococcal infection, also known as Group B streptococcal disease or just Group B strep, is the
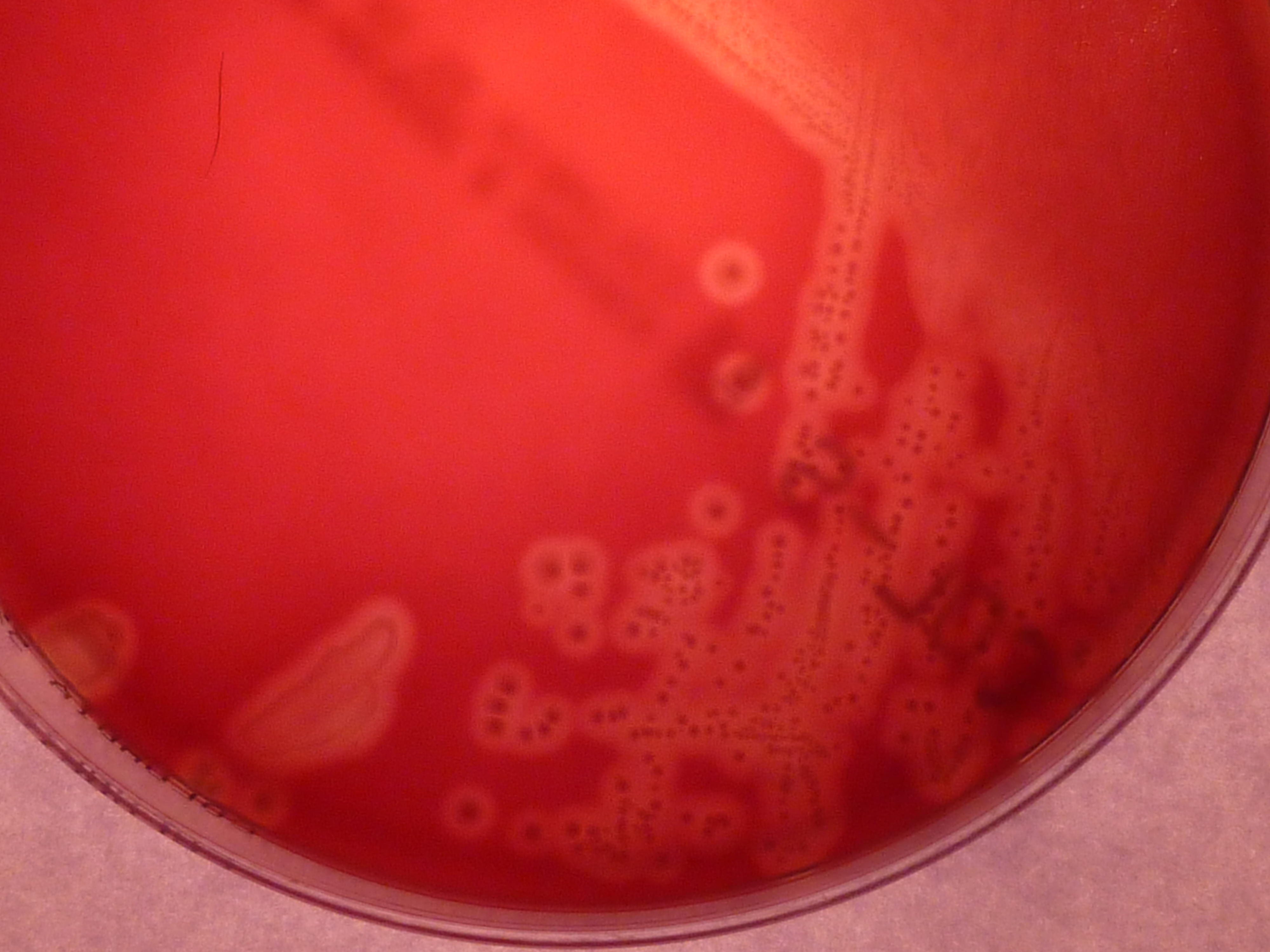
 As mentioned, ''S. agalactiae'' is a Gram-positive coccus with a tendency to form chains, beta-haemolytic, catalase-negative, and facultative anaerobe. GBS grows readily on blood agar plates as microbial colonies surrounded by a narrow zone of β- haemolysis.
GBS is characterized by the presence in the
As mentioned, ''S. agalactiae'' is a Gram-positive coccus with a tendency to form chains, beta-haemolytic, catalase-negative, and facultative anaerobe. GBS grows readily on blood agar plates as microbial colonies surrounded by a narrow zone of β- haemolysis.
GBS is characterized by the presence in the
UK Group B Strep Association
{{Diseases of maternal transmission Health issues in pregnancy Streptococcal infections Infections specific to the perinatal period Neonatology
infection
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable dise ...
caused by the bacterium
Bacteria (; singular: bacterium) are ubiquitous, mostly free-living organisms often consisting of one biological cell. They constitute a large domain of prokaryotic microorganisms. Typically a few micrometres in length, bacteria were among ...
''Streptococcus agalactiae
''Streptococcus agalactiae'' (also known as group B streptococcus or GBS) is a gram-positive coccus (round bacterium) with a tendency to form chains (as reflected by the genus name ''Streptococcus''). It is a beta-hemolytic, catalase-negative, a ...
'' (''S. agalactiae'') (also known as group B streptococcus or GBS). GBS infection can cause serious illness and sometimes death, especially in newborns, the elderly, and people with compromised immune systems.
As other virulent bacteria, GBS harbours an important number of virulence factors
Virulence factors (preferably known as pathogenicity factors or effectors in plant science) are cellular structures, molecules and regulatory systems that enable microbial pathogens (bacteria, viruses, fungi, and protozoa) to achieve the following ...
,
The most important are the capsular polysaccharide (rich in sialic acid Sialic acids are a class of alpha-keto acid sugars with a nine-carbon backbone.
The term "sialic acid" (from the Greek for saliva, - ''síalon'') was first introduced by Swedish biochemist Gunnar Blix in 1952. The most common member of this gr ...
), and a pore-forming toxin
A toxin is a naturally occurring organic poison produced by metabolic activities of living cells or organisms. Toxins occur especially as a protein or conjugated protein. The term toxin was first used by organic chemist Ludwig Brieger (1849– ...
, β- haemolysin.
The GBS capsule is probably the key virulence factor because it helps GBS escape from the host defence mechanisms interfering with phagocytic killing of GBS by human phagocytes
Phagocytes are cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or dying cells. Their name comes from the Greek ', "to eat" or "devour", and "-cyte", the suffix in biology denoting "cell", from the Greek '' ...
.
The GBS β-haemolysin is considered almost identical to the GBS pigment (granadaene
Granadaene is the trivial name of a non-isoprenoid polyene that constitutes the red pigment characteristic of ''Streptococcus agalactiae'' (group B streptococcus).
Characteristics
Granadaene contains a conjugated system made up of a linear chai ...
).
GBS was recognized as a pathogen
In biology, a pathogen ( el, πάθος, "suffering", "passion" and , "producer of") in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ ...
in cattle by Edmond Nocard and Mollereau in the late 1880s. It can cause bovine mastitis (inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
of the udder) in dairy cows. The species name "agalactiae" meaning "no milk", alludes to this.
Its significance as a human pathogen was first described in 1938, when Fry reported three fatal cases of puerperal
The postpartum (or postnatal) period begins after childbirth and is typically considered to end within 6 weeks as the mother's body, including hormone levels and uterus size, returns to a non-pregnant state. The terms puerperium, puerperal perio ...
infections caused by GBS. In the early 1960s, GBS was recognized as a main cause of infections in newborns.
In general, GBS is a harmless commensal bacterium
Bacteria (; singular: bacterium) are ubiquitous, mostly free-living organisms often consisting of one biological cell. They constitute a large domain of prokaryotic microorganisms. Typically a few micrometres in length, bacteria were among ...
being part of the human microbiota
Microbiota are the range of microorganisms that may be commensal, symbiotic, or pathogenic found in and on all multicellular organisms, including plants. Microbiota include bacteria, archaea, protists, fungi, and viruses, and have been found t ...
colonizing the gastrointestinal and genitourinary tracts of up to 30% of healthy human adults (asymptomatic carriers
An asymptomatic carrier is a person or other organism that has become infection, infected with a pathogen, but shows no signs or symptoms.
Although unaffected by the pathogen, carriers can transmit it to others or develop symptoms in later stage ...
).
Laboratory identification
 As mentioned, ''S. agalactiae'' is a Gram-positive coccus with a tendency to form chains, beta-haemolytic, catalase-negative, and facultative anaerobe. GBS grows readily on blood agar plates as microbial colonies surrounded by a narrow zone of β- haemolysis.
GBS is characterized by the presence in the
As mentioned, ''S. agalactiae'' is a Gram-positive coccus with a tendency to form chains, beta-haemolytic, catalase-negative, and facultative anaerobe. GBS grows readily on blood agar plates as microbial colonies surrounded by a narrow zone of β- haemolysis.
GBS is characterized by the presence in the cell wall
A cell wall is a structural layer surrounding some types of cells, just outside the cell membrane. It can be tough, flexible, and sometimes rigid. It provides the cell with both structural support and protection, and also acts as a filtering mech ...
of the group B antigen
In immunology, an antigen (Ag) is a molecule or molecular structure or any foreign particulate matter or a pollen grain that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. ...
of the Lancefield classification
Lancefield grouping is a system of classification that classifies catalase-negative Gram-positive cocci based on the carbohydrate composition of bacterial antigens found on their cell walls. The system, created by Rebecca Lancefield, was historical ...
(Lancefield grouping
Lancefield grouping is a system of classification that classifies catalase-negative Gram-positive cocci based on the carbohydrate composition of bacterial antigens found on their cell walls. The system, created by Rebecca Lancefield, was historic ...
) that can be detected directly in intact bacteria using latex agglutination tests.
The CAMP test
The CAMP test (Christie–Atkins–Munch-Peterson) is a test to identify group B β-hemolytic streptococci (''Streptococcus agalactiae'')
based on their formation of a substance (CAMP factor) that enlarges the area of hemolysis formed by the β ...
is also another important test for the identification of GBS. The CAMP factor acts synergistically with the staphylococcal β-haemolysin inducing enhanced haemolysis of sheep or bovine erythrocytes.
GBS is also able to hydrolyse hippurate, and this test can also be used to identify GBS.
Haemolytic GBS strains produce an orange-brick-red nonisoprenoid
The terpenoids, also known as isoprenoids, are a class of naturally occurring organic chemicals derived from the 5-carbon compound isoprene and its derivatives called terpenes, diterpenes, etc. While sometimes used interchangeably with "terpenes", ...
polyene pigment (ornythinrhamnododecaene) (granadaene
Granadaene is the trivial name of a non-isoprenoid polyene that constitutes the red pigment characteristic of ''Streptococcus agalactiae'' (group B streptococcus).
Characteristics
Granadaene contains a conjugated system made up of a linear chai ...
) when cultivated on granada medium
Granada (,, DIN: ; grc, Ἐλιβύργη, Elibýrgē; la, Illiberis or . ) is the capital city of the province of Granada, in the autonomous community of Andalusia, Spain. Granada is located at the foot of the Sierra Nevada mountains, at the c ...
that allows its straightforward identification.
Identification of GBS could also be carried out easily using modern methods as matrix-assisted laser desorption ionization-time of flight (MALDI-TOF
In mass spectrometry, matrix-assisted laser desorption/ionization (MALDI) is an ionization technique that uses a laser energy absorbing matrix to create ions from large molecules with minimal fragmentation. It has been applied to the analysis of b ...
) mass spectrometry
Mass spectrometry (MS) is an analytical technique that is used to measure the mass-to-charge ratio of ions. The results are presented as a ''mass spectrum'', a plot of intensity as a function of the mass-to-charge ratio. Mass spectrometry is use ...
. and Nucleic Acid Amplification Techniques (NAATs).
Additionally GBS colonies can be tentatively identified after their appearance in chromogenic agar media. Nevertheless, GBS-like colonies that develop in chromogenic media should be confirmed as GBS using additional reliable tests (e.g.latex agglutination or the CAMP test) to avoid potential mis-identification.
A summary of the laboratory techniques for GBS identification is depicted in Ref 18.
Colonization versus infection
GBS is found in the gastrointestinal and genitourinary tract of humans and is normal component of the intestinal and vaginalmicrobiota
Microbiota are the range of microorganisms that may be commensal, symbiotic, or pathogenic found in and on all multicellular organisms, including plants. Microbiota include bacteria, archaea, protists, fungi, and viruses, and have been found t ...
in some women.
In different studies, GBS vaginal colonization rate ranges from 4 to 36%, with most studies reporting rates over 20%.
Vaginal or rectal colonization may be intermittent, transitory, or persistent. These variations in the reported prevalence of asymptomatic
In medicine, any disease is classified asymptomatic if a patient tests as carrier for a disease or infection but experiences no symptoms. Whenever a medical condition fails to show noticeable symptoms after a diagnosis it might be considered asy ...
(presenting no symptoms of disease) colonization could be related to the different detection methods used, and differences in populations studied.
Though GBS is an asymptomatic and harmless colonizer of the gastrointestinal human tract in up to 30% of otherwise healthy adults, including pregnant women, this opportunistic harmless bacterium can, in some circumstances, cause severe invasive infections.
Pregnancy
Though GBS colonization isasymptomatic
In medicine, any disease is classified asymptomatic if a patient tests as carrier for a disease or infection but experiences no symptoms. Whenever a medical condition fails to show noticeable symptoms after a diagnosis it might be considered asy ...
and, in general, does not cause problems, it can sometimes cause serious illness for the mother and the baby during gestation and after delivery. GBS infections in the mother can cause chorioamnionitis
Chorioamnionitis, also known as intra-amniotic infection (IAI), is inflammation of the fetal membranes ( amnion and chorion), usually due to bacterial infection. In 2015, a National Institute of Child Health and Human Development Workshop expert ...
(intra-amniotic infection or severe infection of the placental tissues) infrequently, postpartum infections (after birth) and it had been related with prematurity and fetal death.
GBS urinary tract infections, more than 100.000 CFU (colony forming units
In microbiology, colony-forming unit (CFU, cfu or Cfu) is a unit which estimates the number of microbial cells (bacteria, fungi, viruses etc.) in a sample that are viable, able to multiply via binary fission under the controlled conditions. Count ...
) /mL, may induce labour in pregnant women and cause premature delivery (preterm birth
Preterm birth, also known as premature birth, is the Childbirth, birth of a baby at fewer than 37 weeks Gestational age (obstetrics), gestational age, as opposed to full-term delivery at approximately 40 weeks. Extreme preterm is less than 28 we ...
) and miscarriage
Miscarriage, also known in medical terms as a spontaneous abortion and pregnancy loss, is the death of an embryo or fetus before it is able to survive independently. Miscarriage before 6 weeks of gestation is defined by ESHRE as biochemical lo ...
and requires antibiotic treatment. The presence of GBS in the urine of a pregnant woman, in any colony count, should be considered a marker of heavy GBS colonization and an indication for intra partum antibiotic prophylaxis (IAP).
Newborns
In the western world, GBS (in the absence of effective prevention measures) is the main cause of bacterial infections in newborns, such assepsis
Sepsis, formerly known as septicemia (septicaemia in British English) or blood poisoning, is a life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs. This initial stage is follo ...
, pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity ...
, and meningitis
Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges. The most common symptoms are fever, headache, and neck stiffness. Other symptoms include confusion or ...
, which can lead to death or long-term after effects
Adobe After Effects is a digital visual effects, motion graphics, and compositing application developed by Adobe Inc., and used in the post-production process of film making, video games and television production. Among other things, After Eff ...
.
GBS infections in newborns are separated into two clinical types, early-onset disease (GBS-EOD) and late-onset disease (GBS-LOD). GBS-EOD manifests from 0 to 7 living days in the newborn, most of the cases of EOD being apparent within 24 h from birth. GBS-LOD starts between 7 and 90 days after birth.
Roughly 50% of newborns of GBS colonized mothers are also GBS colonized and (without prevention measures) 1-2% of these newborns will develop GBS-EOD.
The most common clinical syndromes
A syndrome is a set of medical signs and symptoms which are correlated with each other and often associated with a particular disease or disorder. The word derives from the Greek σύνδρομον, meaning "concurrence". When a syndrome is paire ...
of GBS-EOD are sepsis without apparent location, pneumonia, and less frequently meningitis. Bacteremia
Bloodstream infections (BSIs), which include bacteremias when the infections are bacterial and fungemias when the infections are fungal, are infections present in the blood. Blood is normally a sterile environment, so the detection of microb ...
without a focus occurs in 80-85%, pneumonia in 10-15%, and meningitis in 5-10% of cases. The initial clinical findings are respiratory signs in more than 80% of cases. Neonates with meningitis often have an initial clinical presentation identical to presentation in those without meningeal affectation. An exam of the cerebrospinal fluid
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
CSF is produced by specialised ependymal cells in the choroid plexus of the ventricles of the bra ...
is often necessary to rule out meningitis.
Colonization with GBS during labour is the primary risk factor for the development of GBS-EOD. GBS-EOD is acquired vertically (vertical transmission Vertical transmission of symbionts is the transfer of a microbial symbiont from the parent directly to the offspring. Many metazoan species carry symbiotic bacteria which play a mutualistic, commensal, or parasitic role. A symbiont is acquire ...
), through exposure of the fetus or the baby to GBS from the vagina of a colonized woman, either ''in utero'' (because of ascending infection) or during birth, after rupture of membranes. Infants can also be infected during passage through the birth canal; however, newborns who acquire GBS through this route can only become colonized, and these colonized infants usually do not develop GBS-EOD.
Though maternal GBS colonization is the key determinant for GBS-EOD, other factors also increase the risk. These factors are:
* Onset of labour before 37 weeks of gestation (premature birth
Preterm birth, also known as premature birth, is the birth of a baby at fewer than 37 weeks gestational age, as opposed to full-term delivery at approximately 40 weeks. Extreme preterm is less than 28 weeks, very early preterm birth is between 2 ...
)
* Prolonged rupture of membranes
Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complicati ...
(longer duration of membrane rupture) (≥18 h before delivery)
* GBS bacteriuria during pregnancy
* Intrapartum (during childbirth) fever (>38 °C, >100.4 °F)
* Amniotic infections (chorioamnionitis)
* Young maternal age
* Maternal HIV-infection
Nevertheless, most babies who develop GBS-EOD are born to colonized mothers without any of these risk factors.
Heavy GBS vaginal colonization may be associated with a higher risk for GBS-EOD. Women who had one of these risk factors but who are not GBS colonized at labour are at low risk for GBS-EOD compared to women who were colonized prenatally, but had none of the aforementioned risk factors.
Presence of low levels of anticapsular antibodies
An antibody (Ab), also known as an immunoglobulin (Ig), is a large, Y-shaped protein used by the immune system to identify and neutralize foreign objects such as pathogenic bacteria and viruses. The antibody recognizes a unique molecule of the ...
against GBS in the mother are also of great importance for the development of GBS-EOD.
Because of that, a previous sibling with GBS-EOD is also an important risk factor for the development of the infection in subsequent deliveries, probably reflecting the lack of protective antibodies in the mother.
Overall, the case fatality rates from GBS-EOD have declined, from 50% observed in studies from the 1970s to between 2 and 10% in recent years, mainly as a consequence of improvements in therapy and management. Fatal neonatal infections by GBS are more frequent among premature infants.
Today, the mortality associated with GBS EOD in the US is 2.1% among term newborns and 19.2% among preterm newborns.
GBS-LOD affects infants from 7 days to 3 months of age and has a lower case fatality rate (1%-6%) than GBS-EOD. Clinical syndromes of GBS-LOD are bacteremia without a focus (65%), meningitis (25%), cellulitis, osteoarthritis
Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone which affects 1 in 7 adults in the United States. It is believed to be the fourth leading cause of disability in the w ...
, and pneumonia.
Prematurity has been reported to be the main risk factor. Each week of decreasing gestation increases the risk by a factor of 1.34 for developing GBS-LOD.
GBS-LOD can not only be acquired through vertical transmission during delivery; it can also be acquired later from the mother from breast milk or from environmental and community sources.
GBS-LOD commonly shows nonspecific signs, and diagnosis should be made obtaining blood cultures
A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia or ...
in febrile newborns. ''S.agalactiae'' neonatal meningitis does not present with the hallmark sign of adult meningitis, a stiff neck; rather, it presents with nonspecific symptoms, such as fever, vomiting and irritability, and can consequently lead to a late diagnosis. Hearing loss and mental impairment can be a long-term consequence of GBS meningitis.
In contrast with GBS-EOD, the incidence of GBS-LOD has remained stable in the US at 0.31 per 1000 live births from 2006 to 2015.
Prevention of neonatal infection
Currently, the only reliable way to prevent GBS-EOD is administration of intrapartum antibiotics before delivery, that is to say, intrapartumantibiotic prophylaxis
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention of ...
(IAP). IAP interrupts vertical transmission of GBS from the mother to the newborn and decreases the incidence of GBS-EOD.
Administration of intravenous
Intravenous therapy (abbreviated as IV therapy) is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutrie ...
(IV) antibiotics during labour. Intravenous penicillin
Penicillins (P, PCN or PEN) are a group of β-lactam antibiotics originally obtained from ''Penicillium'' moulds, principally '' P. chrysogenum'' and '' P. rubens''. Most penicillins in clinical use are synthesised by P. chrysogenum using ...
or ampicillin
Ampicillin is an antibiotic used to prevent and treat a number of bacterial infections, such as respiratory tract infections, urinary tract infections, meningitis, salmonellosis, and endocarditis. It may also be used to prevent group B strepto ...
given at the onset of labour and then again every four hours until delivery to GBS colonized women have been proven to be very effective at preventing vertical transmission of GBS from mother to baby and GBS-EOD
(penicillin G, 5 million units IV initial dose, then 3 million units every 4 hours until delivery or ampicillin, 2 g IV initial dose, then 1 g IV every 4 hours until delivery).
Penicillin-allergic
Allergies, also known as allergic diseases, refer a number of conditions caused by the hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic derma ...
women without a history of anaphylaxis
Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the follow ...
( angioedema, respiratory distress
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing disc ...
, or urticaria) following administration of a penicillin or a cephalosporin
The cephalosporins (sg. ) are a class of β-lactam antibiotics originally derived from the fungus ''Acremonium'', which was previously known as ''Cephalosporium''.
Together with cephamycins, they constitute a subgroup of β-lactam antibiotics ...
(low risk of anaphylaxis) could receive cefazolin (2 g IV initial dose, then 1 g IV every 8 hours until delivery) instead of penicillin or ampicillin. If the woman has a severe allergy to beta-lactams then intravenous vancomycin (1 g every 12 hours) is recommended. Neither Clindamycin
Clindamycin is an antibiotic medication used for the treatment of a number of bacterial infections, including osteomyelitis (bone) or joint infections, pelvic inflammatory disease, strep throat, pneumonia, acute otitis media (middle ear infec ...
nor Erythromycin
Erythromycin is an antibiotic used for the treatment of a number of bacterial infections. This includes respiratory tract infections, skin infections, chlamydia infections, pelvic inflammatory disease, and syphilis. It may also be used duri ...
are recommended today because the high proportion of GBS resistance to erythromycin (up to 44.8%), Testing for penicillin allergy and can be helpful for all GBS carrying pregnant women and will cancel the frequent use of other antibiotics for GBS-EOD IAP.
Neither oral nor intramuscular antibiotics are effective in reducing the risk GBS-EOD.
Antibiotic susceptibility testing
Antibiotic sensitivity testing or antibiotic susceptibility testing is the measurement of the susceptibility of bacteria to antibiotics. It is used because bacteria may have resistance to some antibiotics. Sensitivity testing results can allow ...
of GBS isolates is crucial for appropriate antibiotic selection for IAP in penicillin-allergic women, because resistance to clindamycin, the most common agent used (in penicillin-allergic women), is increasing among GBS isolates. Appropriate methodologies (including inducible clindamycin resistance) for testing are important, because resistance to clyndamicin ( antimicrobial resistance) can occur in some GBS strains that appear susceptible ( antibiotic sensitivity) in certain susceptibility tests.
For women who are at risk of anaphylaxis after exposure to penicillin, the laboratory requisitions should indicate clearly the presence of penicillin allergy to ensure that the laboratory is aware for the need of testing GBS isolates for clindamycin susceptibility.
Vancomycin
Vancomycin is a glycopeptide antibiotic medication used to treat a number of bacterial infections. It is recommended intravenously as a treatment for complicated skin infections, bloodstream infections, endocarditis, bone and joint infections, ...
(20 mg/Kg every 8 hours until delivery) is used to prevent GBS-EOD in infants born to penicillin-allergic mothers.
If appropriate IAP in GBS colonized women starts as soon as possible once labour starts or waters have broken. When the first dose is given at least 4 hours before delivery, the risk of neonatal infection is reduced; when given between 2–4 hours before delivery the risk is partially reduced.
True penicillin allergy is rare with an estimated frequency of anaphylaxis of one to five episodes per 10,000 cases of penicillin therapy.
Penicillin administered to a woman with no history of β-lactam
A beta-lactam (β-lactam) ring is a four-membered lactam. A ''lactam'' is a cyclic amide, and ''beta''-lactams are named so because the nitrogen atom is attached to the Β carbon, β-carbon atom relative to the carbonyl. The simplest β-lactam p ...
allergy has a risk of anaphylaxis of 0.04 to 4 per 100,000. Maternal anaphylaxis associated with GBS IAP occurs, but any morbidity associated with anaphylaxis is offset greatly by reductions in the incidence of GBS-EOD.
IAPs have been considered to be associated with the emergence of resistant bacterial strains and with an increase in the incidence of early-onset infections caused by other pathogens, mainly Gram-negative
Gram-negative bacteria are bacteria that do not retain the crystal violet stain used in the Gram staining method of bacterial differentiation. They are characterized by their cell envelopes, which are composed of a thin peptidoglycan cell wall ...
bacteria such as ''Escherichia coli
''Escherichia coli'' (),Wells, J. C. (2000) Longman Pronunciation Dictionary. Harlow ngland Pearson Education Ltd. also known as ''E. coli'' (), is a Gram-negative, facultative anaerobic, rod-shaped, coliform bacterium of the genus ''Escher ...
''. Nevertheless, most studies have not found an increased rate of non-GBS early-onset sepsis related to the widespread use of IAP.
Other strategies to prevent GBS-EOD have been studied, and chlorhexidine intrapartum vaginal cleansing has been proposed to help preventing GBS-EOD, nevertheless no evidence has been shown for the effectiveness of this approach.
Identifying candidates to receive IAP
Two ways are used to select female candidates to IAP: the culture-based screening approach and the risk-based approach. The culture-based screening approach identifies candidates using lower vaginal and rectal cultures obtained between 35 and 37 weeks of gestation (or 36-37), and IAP is administered to all GBS colonized women. The risk-based strategy identifies candidates to receive IAP by the aforementioned risk factors known to increase the probability of GBS-EOD without considering if the mother is or is not a GBS carrier. IAP is also recommended for women with intrapartum risk factors if their GBS carrier status is not known at the time of delivery, and for women with GBS bacteriuria (in any colony count) during their pregnancy, and for women who have had an infant with GBS-EOD previously. The risk-based approach is, in general, less effective than the culture-based approach, because in most cases, GBS-EOD develops among newborns who have been born to mothers without risk factors. IAP is not required for women undergoing planned caesarean section in the absence of labour and with intact membranes, irrespective of the known GBS carriage status. Routine screening of pregnant women is performed in most developed countries such as the United States, France, Spain, Belgium, Canada, and Australia, and data have shown falling incidences of GBS-EOD following the introduction of screening-based measures to prevent GBS-EOD. The risk-based strategy is advocated, among other counties, in the United Kingdom, the Netherlands, New Zealand, and Argentina. The issue of cost-effectiveness of both strategies for identifying candidates for IAP is less clear-cut, and some studies have indicated that testing low risk women, plus IAP administered to high-risk women, and to those found to carry GBS is more cost-effective than the current UK practice. Other evaluations have also found the culture-based approach to be more cost-effective than the risk-based approach for the prevention of GBS-EOD. Testing pregnant women to detect GBS carriers and giving IAP to those carrying GBS and to high-risk women has also been proposed and this approach is significantly more cost-effective than the use of the risk-factor approach. One research paper calculated an expected net benefit to the UK government of such an approach of around £37 million a year, compared with the current RCOG approach. It has been reported that IAP does to not prevent all cases of GBS-EOD; its efficacy is estimated at 80%. The risk-based prevention strategy does not prevent about 33% of cases with no risk factors. Up to 90% of cases of GBS-EOD would be preventable if IAP were offered to all GBS carriers identified by universal screening late in pregnancy, plus to the mothers in higher risk situations. Where insufficient intravenous antibiotics are given before delivery, the baby may be given antibiotics immediately after birth, although evidence is inconclusive as to whether this practice is effective or not.Home births and water birth
Home births are becoming increasingly popular in the UK. Recommendations for preventing GBS infections in newborns are the same for home births as for hospital births. Around 25% of women having home births probably carry GBS in their vaginas at delivery without knowing, and it could be difficult to follow correctly the recommendations of IAP and to deal with the risk of a severe allergic reaction to the antibiotics outside of a hospital setting. The RCOG and the ACOG guidelines suggest that birth in a pool is not contraindicated for GBS carriers who have been offered the appropriate IAP if no other contraindications to water immersion are presentScreening for colonization
Approximately 10–30% of women are colonized with GBS during pregnancy. Nevertheless, during pregnancy, colonization can be temporary, intermittent, or continual. Because the GBS colonization status of women can change during pregnancy, only cultures carried out ≤5 weeks before delivery predict quite accurately the GBS carrier status at delivery. In contrast, if the prenatal culture is carried out more than 5 weeks before delivery, it is unreliable for accurately predicting the GBS carrier status at delivery. Because of that, testing for GBS colonization in pregnant women is recommended by the CDC at 36–37 weeks of gestation. It is important to note that the ACOG now recommends performing universal GBS screening between 36 and 37 weeks of gestation. This new recommendation provides a 5-week window for valid culture results that includes births that occur up to a gestational age of at least 41 weeks. The clinical samples recommended for culture of GBS are swabs collected from the lowervagina
In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vestibule to the cervix. The outer vaginal opening is normally partly covered by a thin layer of mucosal tissue called the hymen ...
and rectum
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the Gastrointestinal tract, gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the s ...
through the external anal sphincter
The external anal sphincter (or sphincter ani externus ) is a flat plane of skeletal muscle fibers, elliptical in shape and intimately adherent to the skin surrounding the margin of the anus.
Anatomy
The external anal sphincter measures about 8 ...
.Vaginal-rectal samples should be collected using a flocked swab preferably. Compared with fiber swab, these swabs releases samples and microorganisms more efficiently than conventional fiber swabs.
The sample should be collected swabbing the lower vagina (vaginal introitus) followed by the rectum (i.e., inserting the swab through the anal sphincter) using the same swab or two different swabs. Cervical, perianal, perirectal, or perineal specimens are not acceptable, and a speculum should not be used for sample collection.
Samples can be taken by healthcare professionals, or by the mother herself with appropriate instruction.
Following the recommendations of the CDC, these swabs should be placed into a non-nutritive transport medium. When feasible, specimens should be refrigerated and sent to the laboratory as soon as possible. Appropriate transport systems are commercially available, and in these transport media, GBS can remain viable for several days at room temperature. However, the recovery of GBS declines over one to four days, especially at elevated temperatures, which can lead to false-negative results.
Culture methods
Samples (vaginal, rectal, or vaginorectal swabs) should be inoculated into a selective enrichment broth, ( Todd Hewitt broth with selective antibiotics, enrichment culture). This involves growing the samples in a selective enriched broth medium to improve the viability of the GBS and simultaneously impairing the growth of other naturally occurring bacteria.Appropriate enrichment broths, commercially available, are Todd-Hewitt with gentamicin and nalidixic acid, or with colistin and nalidixic acid (Lim broth). After incubation (18–24 hours, 35-37 °C), the enrichment broth is subcultured overnight in blood agar plates and GBS-like colonies (big colonies, 3-4 millimeters diameter, surrounded by narrow zone of hemolysis) are identified by the CAMP test or using latex agglutination with GBS antiserum or MALDI-TOF. In the UK, this is the method described by the Public Health England's UK Standards for Microbiology Investigations After incubation, the enrichment broth can also be subcultured togranada medium
Granada (,, DIN: ; grc, Ἐλιβύργη, Elibýrgē; la, Illiberis or . ) is the capital city of the province of Granada, in the autonomous community of Andalusia, Spain. Granada is located at the foot of the Sierra Nevada mountains, at the c ...
agar where GBS grows as pinkish-red colonies
or to chromogenic agars, where GBS grows as coloured colonies.
Nevertheless, GBS-like colonies that develop in chromogenic media should be confirmed as GBS using additional reliable tests to avoid mis-identification.
Inoculating directly the vaginal and rectal swabs or the vaginorectal swab in a plate of an appropriate culture medium (blood agar, granada medium or chromogenic media) is also possible. However, this method (bypassing the selective enrichment broth step) can lead to some false-negative results, and this approach should be taken only in addition to, and not instead of, inoculation into selective broth.
Today, in the UK, the detection of GBS colonization using the enrichment broth technique is not offered from most laboratories serving the NHS. However, the implementation of this test seems to be a viable option. At present, culture for GBS (using enriched culture medium) at 35–37 weeks to define an at-risk group of women appears to be the most cost-effective strategy.
The charitable organization
A charitable organization or charity is an organization whose primary objectives are philanthropy and social well-being (e.g. educational, Religion, religious or other activities serving the public interest or common good).
The legal definitio ...
Group B Strep Support have published a list of hospitals in the UK that offer the detection of GBS using the enrichment broth culture method (enrichment culture medium, ECM). This test is also available privately from around £35 per test for a home-testing pack, and it is offered by private clinics. The test is also available privately, for a UK-wide postal service.
Point-of-care testing, POCT
No current culture-based test is both accurate enough and fast enough to be recommended for detecting GBS once labour starts. Plating of swab samples requires time for the bacteria to grow, meaning that this is unsuitable to be used as an intrapartum point-of-care test (POCT or bedside testing). Alternative methods to detect GBS in clinical samples (as vaginorectal swabs) rapidly have been developed, such are the methods based onnucleic acid amplification tests
A nucleic acid test (NAT) is a technique used to detect a particular nucleic acid sequence and thus usually to detect and identify a particular species or subspecies of organism, often a virus or bacterium that acts as a pathogen in blood, tiss ...
, such as polymerase chain reaction
The polymerase chain reaction (PCR) is a method widely used to rapidly make millions to billions of copies (complete or partial) of a specific DNA sample, allowing scientists to take a very small sample of DNA and amplify it (or a part of it) t ...
(PCR) tests, and DNA hybridization probes. These tests can also be used to detect GBS directly from broth media, after the enrichment step, avoiding the subculture of the incubated enrichment broth to an appropriate agar plate.
Testing women for GBS colonization using vaginal or rectal swabs at 35–37 weeks of gestation and culturing them in an enriched media is not as rapid as a PCR test that would check whether the pregnant woman is carrying GBS at delivery. PCR tests would allow starting IAP on admission to the labour ward in those women for whom it is not known if they are GBS carriers. PCR testing for GBS carriage could, in the future, be sufficiently accurate to guide IAP. However, the PCR technology to detect GBS must be improved and simplified to make the method cost-effective and fully useful as a point-of-care test. These tests still cannot replace antenatal culture for the accurate detection of GBS.
POCT for detection of GBS carriers requires additionally that maternity units should provide 24/7 laboratory means required to perform rapid testing.
Nevertheless, point-of-care testing may be used for women who present in labor with an unknown GBS status and without risk factors for ascertaining the use of IAP.
Missed opportunities of prevention
The important factors for successful prevention of GBS-EOD using IAP and the universal screening approach are: * Reach most pregnant women for antenatal screens * Proper sample collection * Using an appropriate procedure for detecting GBS * Administering a correct IAP to GBS carriers Most cases of GBS-EOD occur in term infants born to mothers who screened negative for GBS colonization and in preterm infants born to mothers who were not screened, though some false-negative results observed in the GBS screening tests can be due to the test limitations and to the acquisition of GBS between the time of screening and delivery. These data show that improvements in specimen collection and processing methods for detecting GBS are still necessary in some settings. False-negative screening test, along with failure to receive IAP in women delivering preterm with unknown GBS colonization status, and the administration of inappropriate IAP agents to penicillin-allergic women account for most missed opportunities for prevention of cases of GBS-EOD. GBS-EOD infections presented in infants whose mothers had been screened as GBS culture-negative are particularly worrying, and may be caused by incorrect sample collection, delay in processing the samples, incorrect laboratory techniques, recent antibiotic use, or GBS colonization after the screening was carried out.Epidemiology
In 2000–2001, the reported overall incidence of GBS infection in newborn babies in the UK was 0.72 per 1,000 live births, 0.47 per 1,000 for GBS-EOD and 0.25 per 1,000 for GBS-LOD. Very marked variations were observed, the incidence in Scotland was 0.42 per 1,000, whilst in Northern Ireland, it was 0.9 per 1,000 live births. Nevertheless, it may be a serious underestimation of the real incidence of GBS infections in newborns. A plausible explanation of this is that a considerable number of infants with probable GBS-EOD had negative cultures as a result of a previous maternal antibiotic treatment that inhibits the growth of GBS in blood and cerebrospinal fluid cultures, but does not mask clinical symptoms. Data collected prospectively for neonates that required a septic screen in the first 72 hrs of life in the UK, indicated a combined rate of definite and probable GBS-EOD infection of 3.6 per 1,000 live births. Another study on the epidemiology of invasive GBS infections in England and Wales, reported a rise in the incidence of GBS-EOD between 2000 and 2010 from 0.28 to 0.41 per 1,000 live births. Rates of GBS-LOD also increased between 1991 and 2010 from 0.11 to 0.29 per 1,000 live births in England and Wales. In the past, the incidence of GBS-EOD ranged from 0.7 to 3.7 per thousand live births in the US, and from 0.2 to 3.25 per thousand in Europe. In 2008, after widespread use of antenatal screening and intrapartum antibiotic prophylaxis, theCenters for Disease Control and Prevention
The Centers for Disease Control and Prevention (CDC) is the national public health agency of the United States. It is a United States federal agency, under the Department of Health and Human Services, and is headquartered in Atlanta, Georgi ...
in the United States reported an incidence of 0.28 cases of GBS-EOD per thousand live births in the US. From 2006 to 2015 the incidence of GBS EOD decreased to 0.37 to 0.23 per thousand live births in the US. In contrast, the incidence of GBS-LOD has remained unchanged at 0.26-0.31 per 1,000 live births in the US.
In Spain, the incidence of GBS vertical sepsis declined by 73.6%, from 1.25/1,000 live births in 1996 to 0.33/1,000 in 2008. The "Grupo de Hospitales Fundación Castrillo" has also reported in 2018 an incidence of GBS EOD of 0.17/1000 live births and 0,05/1000 GBS LOD.
In the Barcelona area between 2004 and 2010, the incidence of GBS-EOD was 0.29 per thousand living newborns, with no significant differences along the years. The mortality rate was 8.16%.
In France since 2001, a rapid decrease in the incidence of the neonatal GBS infections has also been reported after widespread use of IAP, from 0.7 to 0.2 per 1,000 births between 1997 and 2006.
Since 2012 the incidence of neonatal GBS infection has been estimated as 0.53 per 1,000 births in the European region, 0.67 in America, and 0.15 in Australasia. Countries reporting no use of IAP had a 2.2-fold higher incidence of GBS-EOD compared with those reporting any use of IAP. Estimates of the incidence of GBS EOD per 1,000 births differs among countries, Japan 0.09, Panama 0,58, Hong Kong 0,76, and 2.35 in the Dominican Republic. Overall, rates are highest in Africa and lowest in Asia. The estimate of the global incidence of GBS LOD is 0.26 cases per 1,000 live births.
It has been appraised that GBS infections cause at least 409.000 maternal/fetal/infant cases and 147.000 stillbirths and infant deaths worldwide annually.
The following are estimates of the chances that a baby will be infected with a GBS neonatal infection if no preventive measures are taken and no other risk factors are present:
* One in 1,000 where the woman is not a known GBS carrier
* One in 400 where the woman carries GBS during the pregnancy
* One in 300 where the woman carries GBS at delivery
* One in 100 where the woman had a previous baby infected with GBS
If a woman who carries GBS is given IAP during labour, the baby's risk is reduced significantly:
* One in 8,000 where the mother carries GBS during pregnancy;
* One in 6,000 where the mother carries GBS at delivery; and
* One in 2,200 where the mother has previously had a baby infected with GBS
Guidelines
United Kingdom
= Royal College of Obstetricians and Gynaecologists (RCOG)
= TheRoyal College of Obstetricians and Gynaecologists
The Royal College of Obstetricians and Gynaecologists (RCOG) is a professional association based in London, United Kingdom. Its members, including people with and without medical degrees, work in the field of obstetrics and gynaecology, that is ...
(RCOG) first issued their Green Top Guideline No 36 "Prevention of early onset neonatal Group B streptococcal disease" in 2003. This guideline clearly stated: "Routine bacteriological screening of all pregnant women for antenatal GBS carriage is not recommended, and vaginal swabs should not be taken during pregnancy unless there is a clinical indication to do so." But, "Intrapartum antibiotic prophylaxis should be offered if GBS is detected on a vaginal swab in the current pregnancy."
Nevertheless, this guideline uses minimum incidence figures from a study undertaken in 2000–2001, so it could not only have underestimated the true incidence of GBS infection, but it could also have underestimated the risks to babies from GBS infection.
GBS infection in babies has increased in England, Wales, and Northern Ireland since 2003 (when the guideline was introduced). Voluntarily reported cases from the Communicable Disease Report/Health Protection Agency show 0.48 cases per 1,000 live births in 2003, and this figure increased to 0.64 per 1,000 in 2009.
In 2007, the RCOG published the findings of their audit to evaluate practice in the UK obstetric units against their recommendations.
The audit started out by comparing international guidelines for prevention of GBS-EOD: highlighting the fact that, in contrast to the UK and New Zealand guidelines, most of the other countries recommended identifying women for IAP by offering effective tests to all pregnant women. The audit reviewed hospitals' protocols against GBS infection in newborns. Of the 161 UK units, which submitted their protocol, four units did not even have a protocol for GBS, of those that did, 35% did not mention the 2003 RCOG guideline, and only a minority of units had protocols entirely consistent with the guideline.
Further UK research published in 2010 looked at the opportunities for prevention of GBS-EOD following the introduction of the RCOG guideline. They found that, in the 48 cases of GBS during 2004 to 2007 (0.52/1,000 live births), only 19% of the mothers in whom risk factors were present were given adequate IAP. The researchers stated: "if all women with risk factors received prophylaxis, 23 cases (48%) may have been prevented."
The 2003 RCOG guideline was reviewed in July 2012 and again in September 2017 with substantial changes.
The second and final audit report into GBS (Audit of current practice in preventing GBS EOD in the UK) has been published. As a result of the audit, the RCOG have recommended that the national guidelines for preventing GBS infection in newborns should be updated.
In the UK, the RCOG still does not recommend bacteriological screening of all pregnant women for antenatal GBS carriage in its 2017 guidelines, although it does state that women who tested positive in a previous pregnancy and the baby was well should be offered the option of testing and being offered intrapartum antimicrobial prophylaxis or having the IAP without testing
Nevertheless, it is stated that if GBS carriage is detected incidentally or by intentional testing, women should be offered IAP. And that all pregnant women should be provided with an appropriate information leaflet about GBS and pregnancy (published in December 2017).
Instead, women are treated according to their risk in labour. IAP is offered to women in labout where GBS has been found from their urine or vaginal/rectal swabs taken during the pregnancy, and to women who have previously had a baby with GBS disease. Immediate induction of labour and IAP should be offered to all women with prelabour rupture of membranes at 37 weeks of gestation or more, to women whose membranes are ruptured more than 18 hours and to those who have fever in labour.
Women who are pyrexial in labour should be offered broad-spectrum antibiotics including an antibiotic appropriate for preventing EOD-GBS.
=NICE guidelines
= The UK's National Institute for Health and Care Excellence (NICE) does not recommend routine testing for GBS, stating: "Pregnant women should not be offered routine antenatal screening for group B streptococcus because evidence of its clinical and cost effectiveness remains uncertain." However, the guideline states that "At the first antenatal (booking) appointment (and later if appropriate), discuss and give information on .... infections that can impact on the baby in pregnancy or during birth (such as group B streptococcus, herpes simplex and cytomegalovirus)" Nevertheless, the NICE Neonatal Infection guideline states: "Offer antibiotics during labour to women who: * are in pre-term labour or * have group B streptococcal colonisation, bacteriuria or infection during the current pregnancy or * have had group B streptococcal colonisation, bacteriuria or infection in a previous pregnancy, and have not had a negative test for group B streptococcus by enrichment culture or PCR on a rectovaginal swab samples collected between 35 and 37 weeks' gestation or 3-5 weeks before the anticipated delivery date in the current pregnancy or * have had a previous baby with an invasive group B streptococcal infection or * have a clinical diagnosis of chorioamnionitis.021
021 is:
* in Brazil, the telephone area code for the city of Rio de Janeiro and surrounding cities (Greater Rio de Janeiro)
* in China, the telephone area code for the city of Shanghai.
* in Indonesia, the area code for the city of Jakarta and su ...
''".
= National Screening Committee
= The UK National Screening Committee's current policy position on GBS is: "screening should not be offered to all pregnant women. This policy was reviewed in 2012, and despite receiving 212 responses, of which 93% advocated screening, the NSC has decided to not recommend antenatal screening. This decision was strongly criticized by the charity Group B Strep Support as ignoring both the wishes of the public and the rising incidence rates of GBS infection in the UK.United States
Recommendations for IAP to prevent perinatal GBS disease were issued in 1996 by the CDC. In these guidelines, the use of one of two prevention methods was recommended: either a risk-based approach or a culture-based screening approach. The CDC issued updated guidelines in 2002; these guidelines recommended the universal culture-based screening of all pregnant women at 35–37 weeks' gestation to optimize the identification of women who must receive IAP. CDC also recommended that women with unknown GBS colonization status at the time of delivery be managed according to the presence of intrapartum risk factors. Because of this strategy, the US has seen a major reduction in the incidence of GBS-EOD. The CDC issued updated guidelines again in 2010, however, the foundations of prevention in the CDC's 2010 guidelines remained unchanged. The following were the main additions in the 2010 guidelines: * Expanded options for laboratory detection of GBS include the use of pigmented media and PCR assays. * A revised colony count threshold was set for laboratories to report GBS in the urine of pregnant women. * Revised algorithms for GBS screening and use of IAP for women with threatened preterm delivery include one algorithm for preterm labor and one for preterm premature rupture of membranes. * Recommendations for IAP agents are presented in an algorithm format in an effort to promote the use of the most appropriate antibiotic for penicillin-allergic women. * A minor change has been made to penicillin dosing to facilitate implementation in facilities with different packaged penicillin products. * The neonatal management algorithm's scope was expanded to apply to all newborns. * Management recommendations depend upon clinical appearance of the neonate and other risk factors such as maternal chorioamnionitis, adequacy of IAP if indicated for the mother, gestational age, and duration of membrane rupture. * Changes were made to the algorithm to reduce unnecessary evaluations in well-appearing newborns at relatively low risk for GBS-EOD. In 2018, the task of revising and updating the GBS prophylaxis guidelines were transferred from the CDC to ACOG, to theAmerican Academy of Pediatrics
The American Academy of Pediatrics (AAP) is an American professional association of pediatricians, headquartered in Itasca, Illinois. It maintains its Department of Federal Affairs office in Washington, D.C.
Background
The Academy was founded ...
, AAP and to the American Society for Microbiology, ASM.
The ACOG committee issued an updated document on Prevention of Group B Streptococcal Early-Onset Disease in Newborns in 2019.
ACOG's guidance replaced the 2010 guidelines published by CDC.
This document does not introduce important changes from the CDC guidelines. The key measures necessary for preventing neonatal GBS early onset disease continue to be universal prenatal screening by culture of GBS from swabs collected from the lower vagina and rectum, correct collection and microbiological processing of the samples, and proper implementation of intrapartum antibiotic prophylaxis. It is also important to note that the ACOG recommended performing universal GBS screening between 36 and 37 weeks of gestation. This new recommendation provides a 5-week window for valid culture results that includes births that occur up to a gestational age of at least 41 weeks.
In 2019, American Academy of Pediatrics
The American Academy of Pediatrics (AAP) is an American professional association of pediatricians, headquartered in Itasca, Illinois. It maintains its Department of Federal Affairs office in Washington, D.C.
Background
The Academy was founded ...
(AAP) published a new clinical report—Management of Infants at Risk for GBS neonatal disease. This AAP's Clinical Report replaces the 2010 guidelines published by CDC.
Following the CDC commission the American Society for Microbiology (ASM) published in 2020 Guidelines for the Detection and Identification of Group B Streptococcus. In this guidelines it is said that "laboratory practices for GBS screening have not changed substantially since 2010" and culture is still the main technique for GBS detection and direct detection of GBS from vagino-rectal samples using NAATs is not recommended.
Other guidelines
National guidelines in most developed countries advocate the use of universal screening of pregnant women late in pregnancy to detect GBS carriage and use of IAP in all colonized mothers. e.g. Canada, Spain, Switzerland, Germany, Poland, Czech Republic, France, and Belgium. In contrast, risk factor-based guidelines were issued (in addition to the UK) in the Netherlands, TheRoyal Australian and New Zealand College of Obstetricians and Gynaecologists
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) is a not-for-profit organisation dedicated to the establishment of high standards of practice in obstetrics and gynaecology and women’s health. The Col ...
does not recommend clearly one of both prevention strategies -either the risk-based or the culture-based approach to identify pregnant women for IAP, and allow practitioners to choose according jurisdictional guidelines.
Adults
GBS is also an important infectious agent able to cause invasive infections in adults. Serious life-threatening invasive GBS infections are increasingly recognized in the elderly and in individuals compromised by underlying diseases such as diabetes,cirrhosis
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage causes tissue repai ...
and cancer.
GBS infections in adults include urinary tract infection, skin and soft-tissue infection (skin and skin structure infection Skin and skin structure infections (SSSIs), also referred to as skin and soft tissue infections (SSTIs), or acute bacterial skin and skin structure infections (ABSSSIs), are infections of skin and associated soft tissues (such as loose connective ti ...
) bacteremia without focus, osteomyelitis, meningitis and endocarditis
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves. Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or the ...
.
GBS infection in adults can be serious, and mortality is higher among adults than among neonates.
In general, penicillin is the antibiotic of choice for treatment of GBS infections. Erythromycin or clindamycin should not be used for treatment in penicillin-allergic patients unless susceptibility of the infecting GBS isolate to these agents is documented. Gentamicin
Gentamicin is an antibiotic used to treat several types of bacterial infections. This may include bone infections, endocarditis, pelvic inflammatory disease, meningitis, pneumonia, urinary tract infections, and sepsis among others. It is not e ...
plus penicillin (for antibiotic synergy) in patients with life-threatening GBS infections may be used.
Invasive GBS infections in non-pregnant adults convey a rising hardship in most developed countries. Vaccination to prevent GBS infection could be a crucial approach to prevent GBS disease in adults.
Toxic shock syndrome (TSS) is an acute multisystem life-threatening disease resulting in multiple organ failure. The severity of this disease frequently warrants immediate medical treatment. TSS is caused primarily by some strains of ''Staphylococcus aureus
''Staphylococcus aureus'' is a Gram-positive spherically shaped bacterium, a member of the Bacillota, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin. It is often positive ...
'' and '' Streptococcus pyogenes'' that produce exotoxins. Nevertheless, invasive GBS infection can be complicated, though quite infrequently, by streptococcal toxic shock-like syndrome (STLS)
Society and culture
July has been recognised as Group B Strep Awareness Month, a time when information about group B Strep aimed at families and health professionals is shared, predominantly in the UK and the US. In the UK, this is led by Group B Strep SupportVaccine
Though the introduction of national guidelines to screen pregnant women for GBS carriage and the use of IAP has significantly reduced the burden of GBS-EOD disease, it has had no effect on preventing either GBS-LOD in infants or GBS infections in adults. Because of this, if an effective vaccine against GBS were available, it would be an effective means of controlling not only GBS disease in infants, but also infections in adults. There are a number of problems with givingantibiotic
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention of ...
s to women in labor. Such antibiotic exposure risks included severe allergic reactions and difficulties screening pregnant women for GBS. If pregnant women could be given a vaccine against GBS, this could potentially prevent most cases of GBS without the need for antibiotics or screening.
Vaccination
Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating ...
is considered an ideal solution to prevent not only early- and late-onset disease but also GBS infections in adults at risk.
Development of GBS vaccines for maternal immunization has been identified as a priority by the World Health Organization
The World Health Organization (WHO) is a specialized agency of the United Nations responsible for international public health. The WHO Constitution states its main objective as "the attainment by all peoples of the highest possible level of h ...
on the basis of high unmet need. It has been estimated that such a vaccine could potentially prevent 231,000 infant and maternal GBS cases.
As early as 1976, low levels of maternal antibodies against the GBS capsular polysaccharide were shown to be correlated with susceptibility to GBS-EOD and GBS-LOD. Maternal-specific antibodies, transferred from the mother to the newborn, were able to confer protection to babies against GBS infection.
The capsular
In botany a capsule is a type of simple, dry, though rarely fleshy dehiscent fruit produced by many species of angiosperms (flowering plants).
Origins and structure
The capsule (Latin: ''capsula'', small box) is derived from a compound (multica ...
polysaccharide
Polysaccharides (), or polycarbohydrates, are the most abundant carbohydrates found in food. They are long chain polymeric carbohydrates composed of monosaccharide units bound together by glycosidic linkages. This carbohydrate can react with wa ...
of GBS, which is an important virulence factor, is also an excellent candidate for the development of an effective vaccine.
GBS protein-based vaccines are also in development and are greatly promising as they will be able to protect against GBS infection of any serotype.
At present, the licensing of GBS vaccines is difficult because of the challenge in conducting clinical trials in humans due to the low incidence of GBS neonatal diseases.
Nevertheless, though research and clinical trials for the development of an effective vaccine to prevent GBS infections are underway, no vaccine is available as of 2021.
Nonhuman infections
GBS has been found in many mammals and other animals such as camels, dogs, cats, seals, dolphins, and crocodiles.Cattle
In cattle, GBS causes mastitis, an infection of the udder. It can produce an acute febrile disease or a subacute, more chronic disease. Both lead to diminishing milk production (hence its name: ''agalactiae'' meaning "no milk"). Mastitis associated with GBS can have an important effect on the quantity and quality of milk produced, and is also associated with elevated somatic cell count and total bacteria count in the milk. Outbreaks in herds are common, and as this is of major significance for the dairy industry, programs to reduce the impact of GBS have been enforced in many countriesFish
GBS it is also an important pathogen in a diversity of fish species, leading to serious economic losses in many species of fish worldwide. GBS causes severe epidemics in farmed fish, causing sepsis and external and internal hemorrhages. GBS infection has been reported from wild and captive fish and has been involved inepizootics
In epizoology, an epizootic (from Greek: ''epi-'' upon + ''zoon'' animal) is a disease event in a nonhuman animal population analogous to an epidemic in humans. An epizootic may be restricted to a specific locale (an "outbreak"), general (an "epi ...
in many countries. Vaccines to protect fish against GBS infections are under development.
References
External links
UK Group B Strep Association
{{Diseases of maternal transmission Health issues in pregnancy Streptococcal infections Infections specific to the perinatal period Neonatology