Sterilisation (microbiology) on:
[Wikipedia]
[Google]
[Amazon]
Sterilization refers to any process that removes, kills, or deactivates all forms of life (particularly microorganisms such as fungi, bacteria, 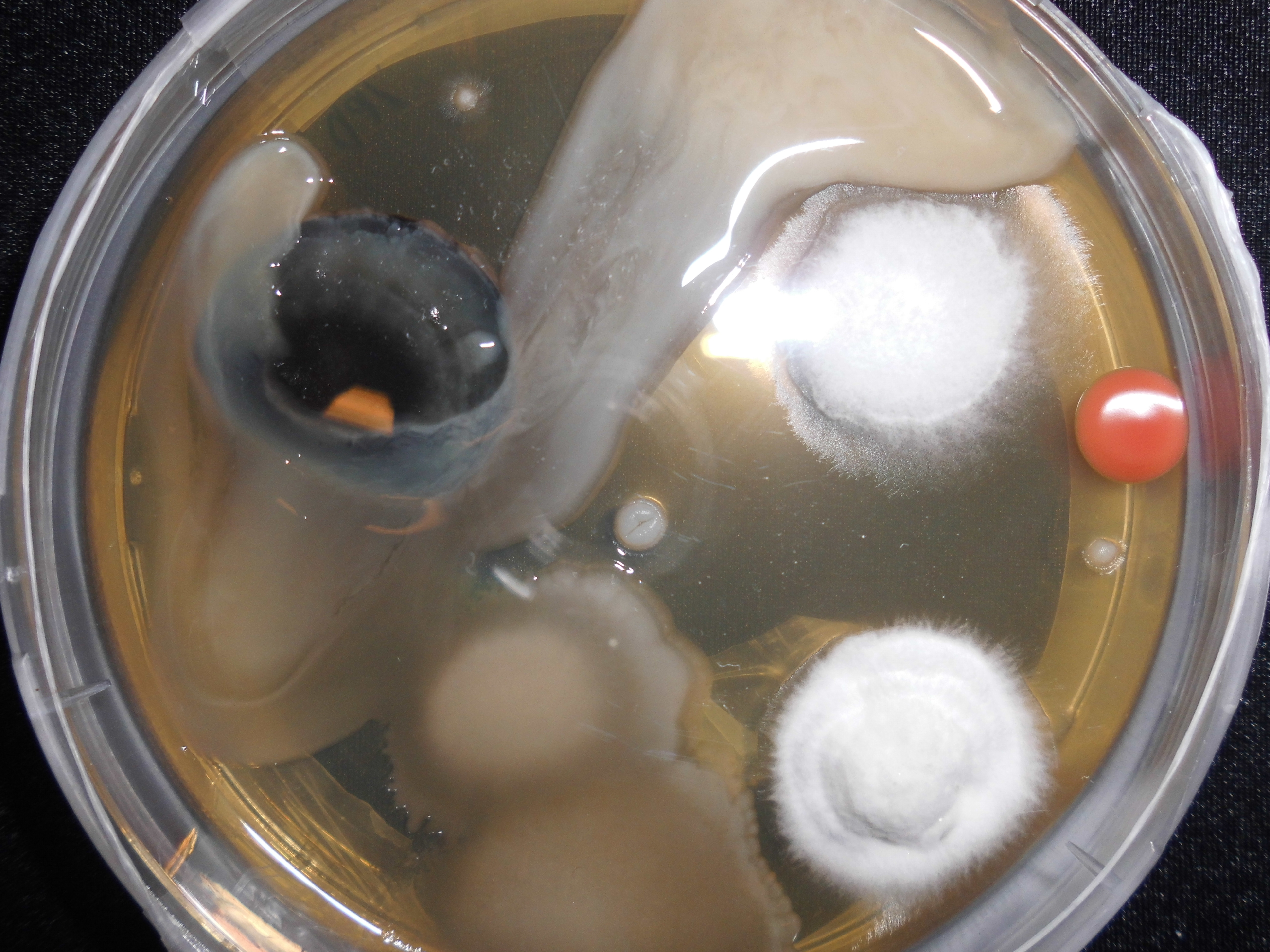
 In general, surgical instruments and medications that enter an already aseptic part of the body (such as the bloodstream, or penetrating the skin) must be sterile. Examples of such instruments include scalpels, hypodermic needles, and artificial pacemakers. This is also essential in the manufacture of parenteral pharmaceuticals.
Preparation of injectable medications and intravenous solutions for fluid replacement therapy requires not only sterility but also well-designed containers to prevent entry of adventitious agents after initial product sterilization.
Most medical and surgical devices used in healthcare facilities are made of materials that are able to go under
In general, surgical instruments and medications that enter an already aseptic part of the body (such as the bloodstream, or penetrating the skin) must be sterile. Examples of such instruments include scalpels, hypodermic needles, and artificial pacemakers. This is also essential in the manufacture of parenteral pharmaceuticals.
Preparation of injectable medications and intravenous solutions for fluid replacement therapy requires not only sterility but also well-designed containers to prevent entry of adventitious agents after initial product sterilization.
Most medical and surgical devices used in healthcare facilities are made of materials that are able to go under
In comparison, pre-vacuum cycles draw a vacuum in the chamber to remove cool dry air prior to injecting saturated steam, resulting in faster heating and shorter cycle times. Typical steam sterilization cycles are between 3 and 30 minutes at at , but adjustments may be made depending on the bioburden of the article being sterilized, its resistance ( D-value) to steam sterilization, the article's heat tolerance, and the required sterility assurance level. Following the completion of a cycle, liquids in a pressurized autoclave must be cooled slowly to avoid boiling over when the pressure is released. This may be achieved by gradually depressurizing the sterilization chamber and allowing liquids to evaporate under a negative pressure, while cooling the contents. Proper autoclave treatment will inactivate all resistant bacterial
 Dry heat was the first method of sterilization and is a longer process than moist heat sterilization. The destruction of microorganisms through the use of dry heat is a gradual phenomenon. With longer exposure to lethal temperatures, the number of killed microorganisms increases. Forced ventilation of hot air can be used to increase the rate at which heat is transferred to an organism and reduce the temperature and amount of time needed to achieve sterility. At higher temperatures, shorter exposure times are required to kill organisms. This can reduce heat-induced damage to food products.
The standard setting for a hot air oven is at least two hours at . A rapid method heats air to for 6 minutes for unwrapped objects and 12 minutes for wrapped objects. Dry heat has the advantage that it can be used on powders and other heat-stable items that are adversely affected by steam (e.g. it does not cause rusting of steel objects).
Dry heat was the first method of sterilization and is a longer process than moist heat sterilization. The destruction of microorganisms through the use of dry heat is a gradual phenomenon. With longer exposure to lethal temperatures, the number of killed microorganisms increases. Forced ventilation of hot air can be used to increase the rate at which heat is transferred to an organism and reduce the temperature and amount of time needed to achieve sterility. At higher temperatures, shorter exposure times are required to kill organisms. This can reduce heat-induced damage to food products.
The standard setting for a hot air oven is at least two hours at . A rapid method heats air to for 6 minutes for unwrapped objects and 12 minutes for wrapped objects. Dry heat has the advantage that it can be used on powders and other heat-stable items that are adversely affected by steam (e.g. it does not cause rusting of steel objects).
 Chemicals are also used for sterilization. Heating provides a reliable way to rid objects of all transmissible agents, but it is not always appropriate if it will damage heat-sensitive materials such as biological materials, fiber optics, electronics, and many plastics. In these situations chemicals, either in a gaseous or liquid form, can be used as sterilants. While the use of gas and liquid chemical sterilants avoids the problem of heat damage, users must ensure that the article to be sterilized is chemically compatible with the sterilant being used and that the sterilant is able to reach all surfaces that must be sterilized (typically cannot penetrate packaging). In addition, the use of chemical sterilants poses new challenges for workplace safety, as the properties that make chemicals effective sterilants usually make them harmful to humans. The procedure for removing sterilant residue from the sterilized materials varies depending on the chemical and process that is used.
Chemicals are also used for sterilization. Heating provides a reliable way to rid objects of all transmissible agents, but it is not always appropriate if it will damage heat-sensitive materials such as biological materials, fiber optics, electronics, and many plastics. In these situations chemicals, either in a gaseous or liquid form, can be used as sterilants. While the use of gas and liquid chemical sterilants avoids the problem of heat damage, users must ensure that the article to be sterilized is chemically compatible with the sterilant being used and that the sterilant is able to reach all surfaces that must be sterilized (typically cannot penetrate packaging). In addition, the use of chemical sterilants poses new challenges for workplace safety, as the properties that make chemicals effective sterilants usually make them harmful to humans. The procedure for removing sterilant residue from the sterilized materials varies depending on the chemical and process that is used.
 The safety of irradiation facilities is regulated by the
The safety of irradiation facilities is regulated by the
 Instruments that have undergone sterilization can be maintained in such condition by containment in sealed packaging until use.
Aseptic technique is the act of maintaining sterility during procedures.
Instruments that have undergone sterilization can be maintained in such condition by containment in sealed packaging until use.
Aseptic technique is the act of maintaining sterility during procedures.
WHO - Infection Control Guidelines for Transmissible Spongiform Encephalopathies
Retrieved Jul 10, 2010 *
Control of microbes
*
Innovative Technologies for the Biofunctionalisation and Terminal Sterilisation of Medical DevicesSterilization of liquids, solids, waste in disposal bags and hazardous biological substances
*Pharmaceutical Filtration - The Management of Organism Removal, Meltzer TH, Jornitz MW, PDA/DHI 1998 *"Association for Advancement of Medical Instrumentation ANSI/AAMI ST41-Ehylene Oxyde Sterilization in Healthcare facilities: Safety and Effectiveness. Arlington, VA: Association for Advancement of Medical Instrumentation; 2000." *“US Department of Labor, Occupational Safety and Health Administration.29 CFR 1910.1020. Access to Employee Medical Records.". October 26, 2007. *Perioperative Standards and Recommended Practices, AORN 2013, {{DEFAULTSORT:Sterilization (Microbiology) Biocides Electron beam Hygiene Microbiology
spore
In biology, a spore is a unit of sexual or asexual reproduction that may be adapted for dispersal and for survival, often for extended periods of time, in unfavourable conditions. Spores form part of the life cycles of many plants, algae, f ...
s, and unicellular eukaryotic organisms) and other biological agents such as prion
Prions are misfolded proteins that have the ability to transmit their misfolded shape onto normal variants of the same protein. They characterize several fatal and transmissible neurodegenerative diseases in humans and many other animals. It ...
s present in or on a specific surface, object, or fluid. Sterilization can be achieved through various means, including heat, chemicals, irradiation, high pressure, and filtration
Filtration is a physical separation process that separates solid matter and fluid from a mixture using a ''filter medium'' that has a complex structure through which only the fluid can pass. Solid particles that cannot pass through the filter ...
. Sterilization is distinct from disinfection, sanitization, and pasteurization
Pasteurization or pasteurisation is a process of food preservation in which packaged and non-packaged foods (such as milk and fruit juices) are treated with mild heat, usually to less than , to eliminate pathogens and extend shelf life.
The ...
, in that those methods reduce rather than eliminate all forms of life and biological agents present. After sterilization, an object is referred to as being sterile or aseptic.
Applications
Foods
One of the first steps toward modernized sterilization was made by Nicolas Appert, who discovered that application of heat over a suitable period slowed the decay of foods and various liquids, preserving them for safe consumption for a longer time than was typical.Canning
Canning is a method of food preservation in which food is processed and sealed in an airtight container (jars like Mason jars, and steel and tin cans). Canning provides a shelf life that typically ranges from one to five years, although u ...
of foods is an extension of the same principle and has helped to reduce food borne illness
Foodborne illness (also foodborne disease and food poisoning) is any illness resulting from the spoilage of contaminated food by pathogenic bacteria, viruses, or parasites that contaminate food,
as well as prions (the agents of mad cow disea ...
("food poisoning"). Other methods of sterilizing foods include food irradiation
Food irradiation is the process of exposing food and food packaging to ionizing radiation, such as from gamma rays, x-rays, or electron beams. Food irradiation improves food safety and extends product shelf life (preservation) by effectively ...
and high pressure ( pascalization).
Medicine and surgery
 In general, surgical instruments and medications that enter an already aseptic part of the body (such as the bloodstream, or penetrating the skin) must be sterile. Examples of such instruments include scalpels, hypodermic needles, and artificial pacemakers. This is also essential in the manufacture of parenteral pharmaceuticals.
Preparation of injectable medications and intravenous solutions for fluid replacement therapy requires not only sterility but also well-designed containers to prevent entry of adventitious agents after initial product sterilization.
Most medical and surgical devices used in healthcare facilities are made of materials that are able to go under
In general, surgical instruments and medications that enter an already aseptic part of the body (such as the bloodstream, or penetrating the skin) must be sterile. Examples of such instruments include scalpels, hypodermic needles, and artificial pacemakers. This is also essential in the manufacture of parenteral pharmaceuticals.
Preparation of injectable medications and intravenous solutions for fluid replacement therapy requires not only sterility but also well-designed containers to prevent entry of adventitious agents after initial product sterilization.
Most medical and surgical devices used in healthcare facilities are made of materials that are able to go under steam
Steam is a substance containing water in the gas phase, and sometimes also an aerosol of liquid water droplets, or air. This may occur due to evaporation or due to boiling, where heat is applied until water reaches the enthalpy of vaporization ...
sterilization. However, since 1950, there has been an increase in medical devices and instruments made of materials (e.g., plastics) that require low-temperature sterilization. Ethylene oxide gas has been used since the 1950s for heat- and moisture-sensitive medical devices. Within the past 15 years, a number of new, low-temperature sterilization systems (e.g., vaporized hydrogen peroxide, peracetic acid immersion, ozone) have been developed and are being used to sterilize medical devices.
Spacecraft
There are strict international rules to protect the contamination of Solar System bodies from biological material from Earth. Standards vary depending on both the type of mission and its destination; the more likely a planet is considered to behabitable
Habitability refers to the adequacy of an environment for human living. Where housing is concerned, there are generally local ordinances which define habitability. If a residence complies with those laws it is said to be habitable. In extreme e ...
, the stricter the requirements are.
Many components of instruments used on spacecraft cannot withstand very high temperatures, so techniques not requiring excessive temperatures are used as tolerated, including heating to at least , chemical sterilization, oxidization, ultraviolet, and irradiation.
Quantification
The aim of sterilization is the reduction of initially present microorganisms or other potential pathogens. The degree of sterilization is commonly expressed by multiples of the decimal reduction time, or D-value, denoting the time needed to reduce the initial number to one tenth () of its original value. Then the number of microorganisms after sterilization time is given by: :. The D-value is a function of sterilization conditions and varies with the type of microorganism, temperature, water activity, pH etc.. For steam sterilization (see below) typically the temperature, in degreesCelsius
The degree Celsius is the unit of temperature on the Celsius scale (originally known as the centigrade scale outside Sweden), one of two temperature scales used in the International System of Units (SI), the other being the Kelvin scale. The ...
, is given as an index.
Theoretically, the likelihood of the survival of an individual microorganism is never zero. To compensate for this, the overkill method is often used. Using the overkill method, sterilization is performed by sterilizing for longer than is required to kill the bioburden present on or in the item being sterilized. This provides a sterility assurance level In microbiology, sterility assurance level (SAL) is the probability that a single unit that has been subjected to sterilization nevertheless remains nonsterile.
It is never possible to prove that all organisms have been destroyed, as the likelihoo ...
(SAL) equal to the probability of a non-sterile unit.
For high-risk applications, such as medical devices and injections, a sterility assurance level of at least 10−6 is required by the United States Food and Drug Administration (FDA).
Heat
Steam
Steam sterilization, also known as moist heat sterilization, uses heated saturated steam under pressure to inactivate or kill microorganisms via denaturation of macromolecules, primarily proteins. This method is a faster process than dry heat sterilization. Steam sterilization is performed using an autoclave, sometimes called a converter or steam sterilizer. The article is placed in the autoclave chamber, which is then sealed and heated using pressurized steam to a temperature set point for a defined period of time. Steam sterilization cycles can be categorized as either pre-vacuum or gravity displacement. Gravity displacement cycles rely on the lower density of the injected steam to force cooler, denser air out of the chamber draiIn comparison, pre-vacuum cycles draw a vacuum in the chamber to remove cool dry air prior to injecting saturated steam, resulting in faster heating and shorter cycle times. Typical steam sterilization cycles are between 3 and 30 minutes at at , but adjustments may be made depending on the bioburden of the article being sterilized, its resistance ( D-value) to steam sterilization, the article's heat tolerance, and the required sterility assurance level. Following the completion of a cycle, liquids in a pressurized autoclave must be cooled slowly to avoid boiling over when the pressure is released. This may be achieved by gradually depressurizing the sterilization chamber and allowing liquids to evaporate under a negative pressure, while cooling the contents. Proper autoclave treatment will inactivate all resistant bacterial
spore
In biology, a spore is a unit of sexual or asexual reproduction that may be adapted for dispersal and for survival, often for extended periods of time, in unfavourable conditions. Spores form part of the life cycles of many plants, algae, f ...
s in addition to fungi, bacteria, and viruses, but is not expected to eliminate all prion
Prions are misfolded proteins that have the ability to transmit their misfolded shape onto normal variants of the same protein. They characterize several fatal and transmissible neurodegenerative diseases in humans and many other animals. It ...
s, which vary in their resistance. For prion elimination, various recommendations state for 60 minutes or for at least 18 minutes. The 263K scrapie prion is inactivated relatively quickly by such sterilization procedures; however, other strains of scrapie, and strains of Creutzfeldt-Jakob disease (CKD) and bovine spongiform encephalopathy (BSE) are more resistant. Using mice
A mouse ( : mice) is a small rodent. Characteristically, mice are known to have a pointed snout, small rounded ears, a body-length scaly tail, and a high breeding rate. The best known mouse species is the common house mouse (''Mus musculus' ...
as test animals, one experiment showed that heating BSE positive brain tissue at for 18 minutes resulted in only a 2.5 log decrease in prion infectivity.
Most autoclaves have meters and charts that record or display information, particularly temperature and pressure as a function of time. The information is checked to ensure that the conditions required for sterilization have been met. Indicator tape is often placed on the packages of products prior to autoclaving, and some packaging incorporates indicators. The indicator changes color when exposed to steam, providing a visual confirmation.
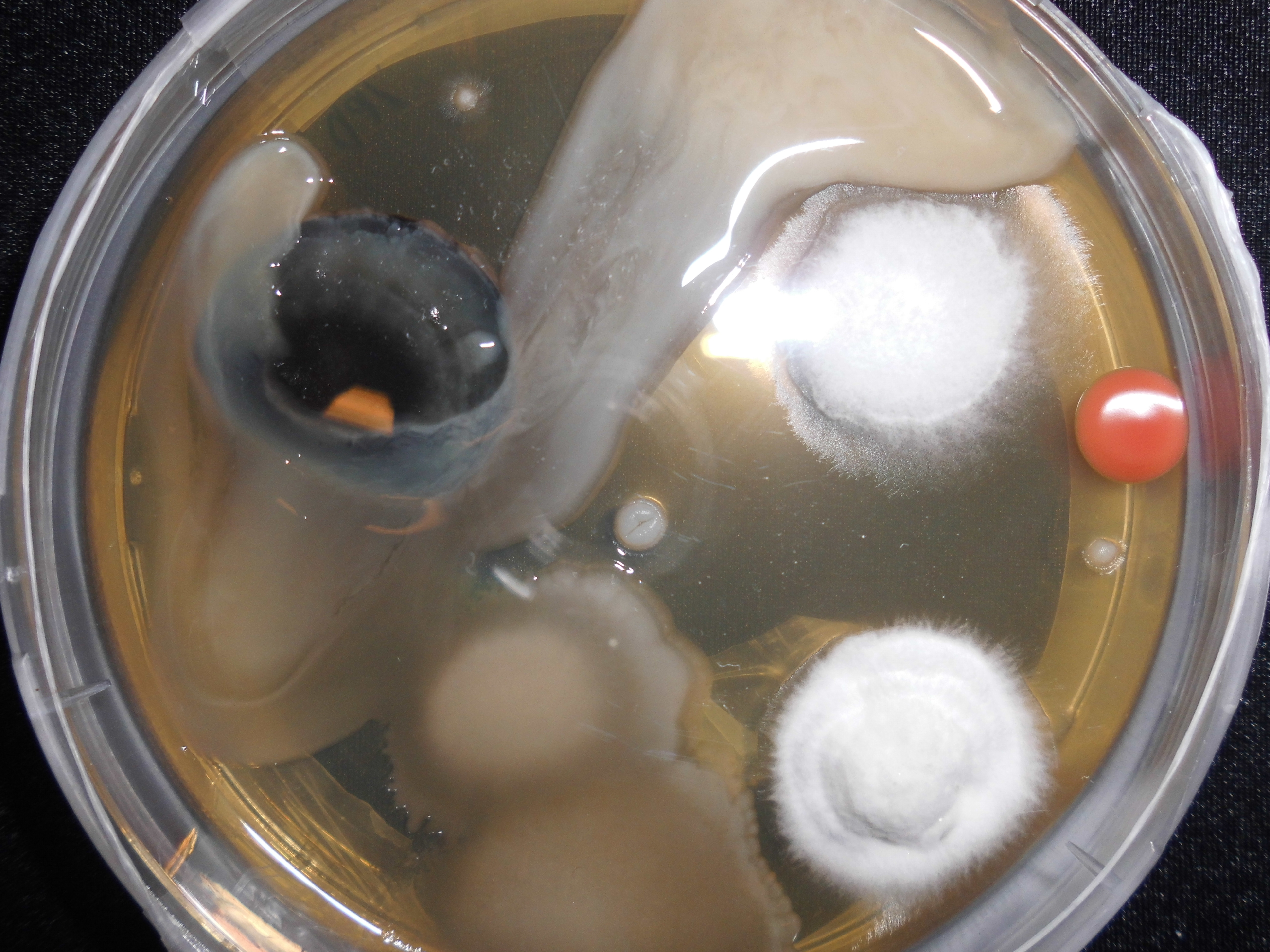
Biological indicators can also be used to independently confirm autoclave performance. Simple biological indicator devices are commercially available, based on microbial spores. Most contain spores of the heat-resistant microbe '' Geobacillus stearothermophilus'' (formerly ''Bacillus stearothermophilus''), which is extremely resistant to steam sterilization. Biological indicators may take the form of glass vials of spores and liquid media, or as spores on strips of paper inside glassine envelopes. These indicators are placed in locations where it is difficult for steam to reach to verify that steam is penetrating there.
For autoclaving, cleaning is critical. Extraneous biological matter or grime may shield organisms from steam penetration. Proper cleaning can be achieved through physical scrubbing, sonication, ultrasound, or pulsed air.
Pressure cooking and canning
Canning is a method of food preservation in which food is processed and sealed in an airtight container (jars like Mason jars, and steel and tin cans). Canning provides a shelf life that typically ranges from one to five years, although u ...
is analogous to autoclaving, and when performed correctly renders food sterile.
To sterilize waste materials that are chiefly composed of liquid, a purpose-built effluent decontamination system can be utilized. These devices can function using a variety of sterilants, although using heat via steam is most common.
Dry
Flaming
Flaming is done to inoculation loops and straight-wires in microbiology labs for streaking. Leaving the loop in the flame of a Bunsen burner oralcohol burner
An alcohol burner or spirit lamp is a piece of laboratory equipment used to produce an open flame. It can be made from brass, glass, stainless steel or aluminium.
Uses
Alcohol burners are preferred for some uses over Bunsen burners for safety p ...
until it glows red ensures that any infectious agent is inactivated. This is commonly used for small metal or glass objects, but not for large objects (see Incineration below). However, during the initial heating, infectious material may be sprayed from the wire surface before it is killed, contaminating nearby surfaces and objects. Therefore, special heaters have been developed that surround the inoculating loop with a heated cage, ensuring that such sprayed material does not further contaminate the area. Another problem is that gas flames may leave carbon or other residues on the object if the object is not heated enough. A variation on flaming is to dip the object in a 70% or more concentrated solution of ethanol, then briefly touch the object to a Bunsen burner flame. The ethanol will ignite and burn off rapidly, leaving less residue than a gas flame
Incineration
Incineration is a waste treatment process that involves the combustion of organic substances contained in waste materials. This method also burns any organism to ash. It is used to sterilize medical and other biohazardous waste before it is discarded with non-hazardous waste. Bacteria incinerators are mini furnaces that incinerate and kill off any microorganisms that may be on an inoculating loop or wire.Tyndallization
Named afterJohn Tyndall
John Tyndall FRS (; 2 August 1820 – 4 December 1893) was a prominent 19th-century Irish physicist. His scientific fame arose in the 1850s from his study of diamagnetism. Later he made discoveries in the realms of infrared radiation and the p ...
, Tyndallization is an obsolete and lengthy process designed to reduce the level of activity of sporulating bacteria that are left by a simple boiling water method. The process involves boiling for a period (typically 20 minutes) at atmospheric pressure, cooling, incubating for a day, and then repeating the process a total of three to four times. The incubation periods are to allow heat-resistant spores surviving the previous boiling period to germinate to form the heat-sensitive vegetative (growing) stage, which can be killed by the next boiling step. This is effective because many spores are stimulated to grow by the heat shock. The procedure only works for media that can support bacterial growth, and will not sterilize non-nutritive substrates like water. Tyndallization is also ineffective against prions.
Glass bead sterilizers
Glass bead sterilizers work by heating glass beads to . Instruments are then quickly doused in these glass beads, which heat the object while physically scraping contaminants off their surface. Glass bead sterilizers were once a common sterilization method employed in dental offices as well as biological laboratories, but are not approved by the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) to be used as a sterilizers since 1997. They are still popular in European and Israeli dental practices, although there are no current evidence-based guidelines for using this sterilizer.Chemical sterilization
Ethylene oxide
Ethylene oxide (EO, EtO) gas treatment is one of the common methods used to sterilize, pasteurize, or disinfect items because of its wide range of material compatibility. It is also used to process items that are sensitive to processing with other methods, such as radiation (gamma, electron beam, X-ray), heat (moist or dry), or other chemicals. Ethylene oxide treatment is the most common chemical sterilization method, used for approximately 70% of total sterilizations, and for over 50% of all disposable medical devices. Ethylene oxide treatment is generally carried out between with relative humidity above 30% and a gas concentration between 200 and 800 mg/L. Typically, the process lasts for several hours. Ethylene oxide is highly effective, as it penetrates all porous materials, and it can penetrate through some plastic materials and films. Ethylene oxide kills all known microorganisms, such as bacteria (including spores), viruses, and fungi (including yeasts and moulds), and is compatible with almost all materials even when repeatedly applied. It is flammable, toxic, and carcinogenic; however, only with a reported potential for some adverse health effects when not used in compliance with published requirements. Ethylene oxide sterilizers and processes require biologicalvalidation
Validation may refer to:
* Data validation, in computer science, ensuring that data inserted into an application satisfies defined formats and other input criteria
* Forecast verification, validating and verifying prognostic output from a numerica ...
after sterilizer installation, significant repairs or process changes.
The traditional process consists of a preconditioning phase (in a separate room or cell), a processing phase (more commonly in a vacuum vessel and sometimes in a pressure rated vessel), and an aeration phase (in a separate room or cell) to remove EO residues and lower by-products such as ethylene chlorohydrin
2-Chloroethanol (also called ethylene chlorohydrin or glycol chlorohydrin) is an organic chemical compound with the chemical formula HOCH2CH2Cl and the ''simplest'' beta-halohydrin (chlorohydrin). This colorless liquid has a pleasant ether-like od ...
(EC or ECH) and, of lesser importance, ethylene glycol (EG). An alternative process, known as all-in-one processing, also exists for some products whereby all three phases are performed in the vacuum or pressure rated vessel. This latter option can facilitate faster overall processing time and residue dissipation.
The most common EO processing method is the gas chamber method. To benefit from economies of scale, EO has traditionally been delivered by filling a large chamber with a combination of gaseous EO either as pure EO, or with other gases used as diluents; diluents include chlorofluorocarbons (CFCs
Chlorofluorocarbons (CFCs) and hydrochlorofluorocarbons (HCFCs) are fully or partly halogenated hydrocarbons that contain carbon (C), hydrogen (H), chlorine (Cl), and fluorine (F), produced as volatile derivatives of methane, ethane, and propan ...
), hydrochlorofluorocarbons (HCFCs), and carbon dioxide.
Ethylene oxide is still widely used by medical device manufacturers. Since EO is explosive at concentrations above 3%, EO was traditionally supplied with an inert
Inert may refer to:
* Chemically inert, not chemically reactive
** Inert gas
** Noble gas, historically called inert gas
* Inert knowledge, information which one can express but not use
* Inert waste, waste which is neither chemically nor biol ...
carrier gas, such as a CFC or HCFC. The use of CFCs or HCFCs as the carrier gas was banned because of concerns of ozone depletion
Ozone depletion consists of two related events observed since the late 1970s: a steady lowering of about four percent in the total amount of ozone in Earth's atmosphere, and a much larger springtime decrease in stratospheric ozone (the ozone l ...
. These halogenated hydrocarbons are being replaced by systems using 100% EO, because of regulations and the high cost of the blends. In hospitals, most EO sterilizers use single-use cartridges because of the convenience and ease of use compared to the former plumbed gas cylinders of EO blends.
It is important to adhere to patient and healthcare personnel government specified limits of EO residues in and/or on processed products, operator exposure after processing, during storage and handling of EO gas cylinders, and environmental emissions produced when using EO.
The U.S. Occupational Safety and Health Administration (OSHA) has set the permissible exposure limit (PEL) at 1 ppm – calculated as an eight-hour time-weighted average (TWA) – and 5 ppm as a 15-minute excursion limit (EL). The National Institute for Occupational Safety and Health's (NIOSH) immediately dangerous to life and health limit (IDLH) for EO is 800 ppm. The odor threshold is around 500 ppm, so EO is imperceptible until concentrations are well above the OSHA PEL. Therefore, OSHA recommends that continuous gas monitoring systems be used to protect workers using EO for processing.
Nitrogen dioxide
Nitrogen dioxide (NO2) gas is a rapid and effective sterilant for use against a wide range of microorganisms, including common bacteria, viruses, and spores. The unique physical properties of NO2 gas allow for sterilant dispersion in an enclosed environment at room temperature and atmospheric pressure. The mechanism for lethality is the degradation of DNA in the spore core through nitration of the phosphate backbone, which kills the exposed organism as it absorbs NO2. This degradations occurs at even very low concentrations of the gas. NO2 has a boiling point of at sea level, which results in a relatively highly saturated vapour pressure at ambient temperature. Because of this, liquid NO2 may be used as a convenient source for the sterilant gas. Liquid NO2 is often referred to by the name of its dimer,dinitrogen tetroxide
Dinitrogen tetroxide, commonly referred to as nitrogen tetroxide (NTO), and occasionally (usually among ex-USSR/Russia rocket engineers) as amyl, is the chemical compound N2O4. It is a useful reagent in chemical synthesis. It forms an equilibrium ...
(N2O4). Additionally, the low levels of concentration required, coupled with the high vapour pressure, assures that no condensation
Condensation is the change of the state of matter from the gas phase into the liquid phase, and is the reverse of vaporization. The word most often refers to the water cycle. It can also be defined as the change in the state of water vapor to ...
occurs on the devices being sterilized. This means that no aeration of the devices is required immediately following the sterilization cycle. NO2 is also less corrosive than other sterilant gases, and is compatible with most medical materials and adhesives.
The most-resistant organism (MRO) to sterilization with NO2 gas is the spore of '' Geobacillus stearothermophilus'', which is the same MRO for both steam and hydrogen peroxide sterilization processes. The spore form of ''G. stearothermophilus'' has been well characterized over the years as a biological indicator
A bioindicator is any species (an indicator species) or group of species whose function, population, or status can reveal the qualitative status of the environment. The most common indicator species are animals. For example, copepods and other sma ...
in sterilization applications. Microbial inactivation of ''G. stearothermophilus'' with NO2 gas proceeds rapidly in a log-linear fashion, as is typical of other sterilization processes. Noxilizer, Inc. has commercialized this technology to offer contract sterilization services for medical devices at its Baltimore, Maryland (U.S.) facility. This has been demonstrated in Noxilizer’s lab in multiple studies and is supported by published reports from other labs. These same properties also allow for quicker removal of the sterilant and residual gases through aeration of the enclosed environment. The combination of rapid lethality and easy removal of the gas allows for shorter overall cycle times during the sterilization (or decontamination) process and a lower level of sterilant residuals than are found with other sterilization methods.
Eniware, LLC has developed a portable, power-free sterilizer that uses no electricity, heat or water. The 25 liter unit makes sterilization of surgical instruments possible for austere forward surgical teams, in health centers throughout the world with intermittent or no electricity and in disaster relief and humanitarian crisis situations. The four hour cycle uses a single use gas generation ampoule and a disposable scrubber to remove nitrogen dioxide gas.
Ozone
Ozone is used in industrial settings to sterilize water and air, as well as a disinfectant for surfaces. It has the benefit of being able to oxidize most organic matter. On the other hand, it is a toxic and unstable gas that must be produced on-site, so it is not practical to use in many settings. Ozone offers many advantages as a sterilant gas; ozone is a very efficient sterilant because of its strong oxidizing properties ( E=2.076 vs SHE) capable of destroying a wide range of pathogens, including prions, without the need for handling hazardous chemicals since the ozone is generated within the sterilizer from medical-grade oxygen. The high reactivity of ozone means that waste ozone can be destroyed by passing over a simple catalyst that reverts it to oxygen and ensures that the cycle time is relatively short. The disadvantage of using ozone is that the gas is very reactive and very hazardous. The NIOSH's immediately dangerous to life and health limit (IDLH) for ozone is smaller than the IDLH for ethylene oxide. NIOSH and OSHA has set the PEL for ozone at , calculated as an time-weighted average. The sterilant gas manufacturers include many safety features in their products but prudent practice is to provide continuous monitoring of exposure to ozone, in order to provide a rapid warning in the event of a leak. Monitors for determining workplace exposure to ozone are commercially available.Glutaraldehyde and formaldehyde
Glutaraldehyde and formaldehyde solutions (also used as fixatives) are accepted liquid sterilizing agents, provided that the immersion time is sufficiently long. To kill all spores in a clear liquid can take up to 22 hours with glutaraldehyde and even longer with formaldehyde. The presence of solid particles may lengthen the required period or render the treatment ineffective. Sterilization of blocks of tissue can take much longer, due to the time required for the fixative to penetrate. Glutaraldehyde and formaldehyde are volatile, and toxic by both skin contact and inhalation. Glutaraldehyde has a short shelf-life (<2 weeks), and is expensive. Formaldehyde is less expensive and has a much longer shelf-life if somemethanol
Methanol (also called methyl alcohol and wood spirit, amongst other names) is an organic chemical and the simplest aliphatic alcohol, with the formula C H3 O H (a methyl group linked to a hydroxyl group, often abbreviated as MeOH). It is a ...
is added to inhibit polymerization to paraformaldehyde, but is much more volatile. Formaldehyde is also used as a gaseous sterilizing agent; in this case, it is prepared on-site by depolymerization of solid paraformaldehyde. Many vaccines, such as the original Salk polio vaccine
Polio vaccines are vaccines used to prevent poliomyelitis (polio). Two types are used: an inactivated poliovirus given by injection (IPV) and a weakened poliovirus given by mouth (OPV). The World Health Organization (WHO) recommends all chil ...
, are sterilized with formaldehyde.
Hydrogen peroxide
Hydrogen peroxide, in both liquid and as vaporized hydrogen peroxide (VHP), is another chemical sterilizing agent. Hydrogen peroxide is a strong oxidant, which allows it to destroy a wide range of pathogens. Hydrogen peroxide is used to sterilize heat- or temperature-sensitive articles, such as rigid endoscopes. In medical sterilization, hydrogen peroxide is used at higher concentrations, ranging from around 35% up to 90%. The biggest advantage of hydrogen peroxide as a sterilant is the short cycle time. Whereas the cycle time for ethylene oxide may be 10 to 15 hours, some modern hydrogen peroxide sterilizers have a cycle time as short as 28 minutes. Drawbacks of hydrogen peroxide include material compatibility, a lower capability for penetration and operator health risks. Products containing cellulose, such as paper, cannot be sterilized using VHP and products containing nylon may become brittle. The penetrating ability of hydrogen peroxide is not as good as ethylene oxide and so there are limitations on the length and diameter of the lumen of objects that can be effectively sterilized. Hydrogen peroxide is a primary irritant and the contact of the liquid solution with skin will cause bleaching or ulceration depending on the concentration and contact time. It is relatively non-toxic when diluted to low concentrations, but is a dangerous oxidizer at high concentrations (> 10% w/w). The vapour is also hazardous, primarily affecting the eyes and respiratory system. Even short term exposures can be hazardous and NIOSH has set the IDLH at 75 ppm, less than one tenth the IDLH for ethylene oxide (800 ppm). Prolonged exposure to lower concentrations can cause permanent lung damage and consequently, OSHA has set the permissible exposure limit to 1.0 ppm, calculated as an eight-hour time-weighted average. Sterilizer manufacturers go to great lengths to make their products safe through careful design and incorporation of many safety features, though there are still workplace exposures of hydrogen peroxide from gas sterilizers documented in the FDA MAUDE database. When using any type of gas sterilizer, prudent work practices should include good ventilation, a continuous gas monitor for hydrogen peroxide and good work practices and training. Vaporized hydrogen peroxide (VHP) is used to sterilize large enclosed and sealed areas, such as entire rooms and aircraft interiors. Although toxic, VHP breaks down in a short time to water and oxygen.Peracetic acid
Peracetic acid (0.2%) is a recognized sterilant by the FDA for use in sterilizing medical devices such as endoscopes. Peracetic acid which is also known as peroxyacetic acid is a chemical compound often used in disinfectants such as sanitizers. It is most commonly produced by the reaction ofacetic acid
Acetic acid , systematically named ethanoic acid , is an acidic, colourless liquid and organic compound with the chemical formula (also written as , , or ). Vinegar is at least 4% acetic acid by volume, making acetic acid the main component ...
and hydrogen peroxide with each other by using an acid catalyst. Peracetic acid is never sold in unstabilized solutions which is why it is considered to be environmentally friendly. Peracetic acid is a colorless liquid and the molecular formula of peracetic acid is C2H4O3 or CH3COOOH. More recently, peracetic acid is being used throughout the world as more people are using fumigation to decontaminate surfaces to reduce the risk of Covid-19 and other diseases.
Potential for chemical sterilization of prions
Prions are highly resistant to chemical sterilization. Treatment with aldehydes, such as formaldehyde, have actually been shown to increase prion resistance. Hydrogen peroxide (3%) for one hour was shown to be ineffective, providing less than 3 logs (10−3) reduction in contamination.Iodine
Iodine is a chemical element with the symbol I and atomic number 53. The heaviest of the stable halogens, it exists as a semi-lustrous, non-metallic solid at standard conditions that melts to form a deep violet liquid at , and boils to a vi ...
, formaldehyde, glutaraldehyde, and peracetic acid also fail this test (one hour treatment). Only chlorine, phenolic compounds
In organic chemistry, phenols, sometimes called phenolics, are a class of chemical compounds consisting of one or more hydroxyl groups (— O H) bonded directly to an aromatic hydrocarbon group. The simplest is phenol, . Phenolic compounds are c ...
, guanidinium thiocyanate, and sodium hydroxide reduce prion levels by more than 4 logs; chlorine (too corrosive to use on certain objects) and sodium hydroxide are the most consistent. Many studies have shown the effectiveness of sodium hydroxide.
Radiation sterilization
Sterilization can be achieved using electromagnetic radiation, such as ultraviolet light, X-rays and gamma rays, or irradiation bysubatomic particle
In physical sciences, a subatomic particle is a particle that composes an atom. According to the Standard Model of particle physics, a subatomic particle can be either a composite particle, which is composed of other particles (for example, a pr ...
s such as by electron beam
Cathode rays or electron beam (e-beam) are streams of electrons observed in discharge tubes. If an evacuated glass tube is equipped with two electrodes and a voltage is applied, glass behind the positive electrode is observed to glow, due to ele ...
s. Electromagnetic or particulate radiation can be energetic enough to ionize atoms or molecules (ionizing radiation
Ionizing radiation (or ionising radiation), including nuclear radiation, consists of subatomic particles or electromagnetic waves that have sufficient energy to ionize atoms or molecules by detaching electrons from them. Some particles can travel ...
), or less energetic ( non-ionizing radiation).
Non-ionizing radiation sterilization
Ultraviolet light irradiation (UV, from agermicidal lamp
A germicidal lamp (also known as disinfection lamp or sterilizer lamp) is an electric light that produces ultraviolet C (UVC) light. This short-wave ultraviolet light disrupts DNA base pairing, causing formation of pyrimidine dimers, and lead ...
) is useful for sterilization of surfaces and some transparent objects. Many objects that are transparent to visible light absorb UV. UV irradiation is routinely used to sterilize the interiors of biological safety cabinets between uses, but is ineffective in shaded areas, including areas under dirt (which may become polymerized after prolonged irradiation, so that it is very difficult to remove). It also damages some plastics, such as polystyrene
Polystyrene (PS) is a synthetic polymer made from monomers of the aromatic hydrocarbon styrene. Polystyrene can be solid or foamed. General-purpose polystyrene is clear, hard, and brittle. It is an inexpensive resin per unit weight. It is a ...
foam if exposed for prolonged periods of time.
Ionizing radiation sterilization
 The safety of irradiation facilities is regulated by the
The safety of irradiation facilities is regulated by the International Atomic Energy Agency
The International Atomic Energy Agency (IAEA) is an intergovernmental organization that seeks to promote the peaceful use of nuclear energy and to inhibit its use for any military purpose, including nuclear weapons. It was established in 1957 ...
of the United Nations and monitored by the different national Nuclear Regulatory Commission
The Nuclear Regulatory Commission (NRC) is an independent agency of the United States government tasked with protecting public health and safety related to nuclear energy. Established by the Energy Reorganization Act of 1974, the NRC began operat ...
s (NRC). The radiation exposure accidents that have occurred in the past are documented by the agency and thoroughly analyzed to determine the cause and improvement potential. Such improvements are then mandated to retrofit existing facilities and future design.
Gamma radiation
A gamma ray, also known as gamma radiation (symbol γ or \gamma), is a penetrating form of electromagnetic radiation arising from the radioactive decay of atomic nuclei. It consists of the shortest wavelength electromagnetic waves, typically s ...
is very penetrating, and is commonly used for sterilization of disposable medical equipment, such as syringes, needles, cannulas and IV sets, and food. It is emitted by a radioisotope, usually cobalt-60 (60Co) or caesium-137 (137Cs), which have photon energies of up to 1.3 and 0.66 MeV, respectively.
Use of a radioisotope requires shielding for the safety of the operators while in use and in storage. With most designs, the radioisotope is lowered into a water-filled source storage pool, which absorbs radiation and allows maintenance personnel to enter the radiation shield. One variant keeps the radioisotope under water at all times and lowers the product to be irradiated in the water in hermetically-sealed bells; no further shielding is required for such designs. Other uncommonly used designs use dry storage, providing movable shields that reduce radiation levels in areas of the irradiation chamber. An incident in Decatur, Georgia
Decatur is a city in, and the county seat of, DeKalb County, Georgia, which is part of the Atlanta metropolitan area. With a population of 24,928 in the 2020 census, the municipality is sometimes assumed to be larger since multiple ZIP Codes in ...
, US, where water-soluble caesium-137 leaked into the source storage pool, requiring NRC intervention has led to use of this radioisotope being almost entirely discontinued in favour of the more costly, non-water-soluble cobalt-60. Cobalt-60 gamma photons have about twice the energy, and hence greater penetrating range, of caesium-137-produced radiation.
Electron beam processing is also commonly used for sterilization. Electron beams use an on-off technology and provide a much higher dosing rate than gamma or X-rays. Due to the higher dose rate, less exposure time is needed and thereby any potential degradation to polymers is reduced. Because electrons carry a charge, electron beams are less penetrating than both gamma and X-rays. Facilities rely on substantial concrete shields to protect workers and the environment from radiation exposure.
High-energy X-rays
High-energy X-rays or HEX-rays are very hard X-rays, with typical energies of 80–1000 keV (1 MeV), about one order of magnitude higher than conventional X-rays used for X-ray crystallography (and well into gamma-ray energies over 120 k ...
(produced by '' bremsstrahlung'') allow irradiation of large packages and pallet
A pallet (also called a skid) is a flat transport structure, which supports goods in a stable fashion while being lifted by a forklift, a pallet jack, a front loader, a jacking device, or an erect crane. A pallet is the structural foundat ...
loads of medical devices. They are sufficiently penetrating to treat multiple pallet loads of low-density packages with very good dose uniformity ratios. X-ray sterilization does not require chemical or radioactive material: high-energy X-rays are generated at high intensity by an X-ray generator that does not require shielding when not in use. X-rays are generated by bombarding a dense material (target) such as tantalum or tungsten with high-energy electrons, in a process known as ''bremsstrahlung'' conversion. These systems are energy-inefficient, requiring much more electrical energy than other systems for the same result.
Irradiation with X-rays, gamma rays, or electrons does not make materials radioactive, because the energy used is too low. Generally an energy of at least 10 MeV is needed to induce radioactivity in a material. Neutrons and very high-energy particles can make materials radioactive, but have good penetration, whereas lower energy particles (other than neutrons) cannot make materials radioactive, but have poorer penetration.
Sterilization by irradiation with gamma rays may however affect material properties.
Irradiation is used by the United States Postal Service to sterilize mail in the Washington, D.C. area. Some foods (e.g. spices and ground meats) are sterilized by irradiation.
Subatomic particles may be more or less penetrating and may be generated by a radioisotope or a device, depending upon the type of particle.
Sterile filtration
Fluids that would be damaged by heat, irradiation or chemical sterilization, such as drug solution, can be sterilized by microfiltration using membrane filters. This method is commonly used for heat labile pharmaceuticals and protein solutions in medicinal drug processing. A microfilter with pore size of usually 0.22µm
The micrometre ( international spelling as used by the International Bureau of Weights and Measures; SI symbol: μm) or micrometer (American spelling), also commonly known as a micron, is a unit of length in the International System of Unit ...
will effectively remove microorganisms
A microorganism, or microbe,, ''mikros'', "small") and ''organism'' from the el, ὀργανισμός, ''organismós'', "organism"). It is usually written as a single word but is sometimes hyphenated (''micro-organism''), especially in olde ...
.
Some staphylococcal species have, however, been shown to be flexible enough to pass through 0.22 µm filters. In the processing of biologics, viruses must be removed or inactivated, requiring the use of nanofilters with a smaller pore size (20–50 nm). Smaller pore sizes lower the flow rate, so in order to achieve higher total throughput or to avoid premature blockage, pre-filters might be used to protect small pore membrane filters. Tangential flow filtration (TFF) and alternating tangential flow (ATF) systems also reduce particulate accumulation and blockage.
Membrane filters used in production processes are commonly made from materials such as mixed cellulose ester
Cellulose is an organic compound with the formula , a polysaccharide consisting of a linear chain of several hundred to many thousands of β(1→4) linked D-glucose units. Cellulose is an important structural component of the primary cell wall ...
or polyethersulfone (PES). The filtration equipment and the filters themselves may be purchased as pre-sterilized disposable units in sealed packaging or must be sterilized by the user, generally by autoclaving at a temperature that does not damage the fragile filter membranes. To ensure proper functioning of the filter, the membrane filters are integrity tested post-use and sometimes before use. The nondestructive integrity test assures the filter is undamaged and is a regulatory requirement. Typically, terminal pharmaceutical sterile filtration is performed inside of a cleanroom to prevent contamination.
Preservation of sterility
 Instruments that have undergone sterilization can be maintained in such condition by containment in sealed packaging until use.
Aseptic technique is the act of maintaining sterility during procedures.
Instruments that have undergone sterilization can be maintained in such condition by containment in sealed packaging until use.
Aseptic technique is the act of maintaining sterility during procedures.
See also
* Antibacterial soap * Asepsis * Aseptic processing * Contamination control * Electron irradiation * Food packaging *Food preservation
Food preservation includes processes that make food more resistant to microorganism growth and slow the oxidation of fats. This slows down the decomposition and rancidification process. Food preservation may also include processes that inhibit ...
*Food safety
Food safety (or food hygiene) is used as a scientific method/discipline describing handling, preparation, and storage of food in ways that prevent food-borne illness. The occurrence of two or more cases of a similar illness resulting from t ...
*Spaulding classification Earle Spaulding of Temple University (Philadelphia, Pennsylvania) in a 1939 paper on disinfection of surgical instruments in a chemical solution proposed "a strategy for sterilization or disinfection of inanimate objects and surfaces based on the d ...
*Sterilant gas monitoring Sterilant gas monitoring is the detection of hazardous gases used by health care and other facilities to sterilize medical supplies that cannot be sterilized by heat or steam methods. The current FDA approved sterilant gases are ethylene oxide, hy ...
References
Other references
WHO - Infection Control Guidelines for Transmissible Spongiform Encephalopathies
Retrieved Jul 10, 2010 *
Control of microbes
*
Innovative Technologies for the Biofunctionalisation and Terminal Sterilisation of Medical Devices
*Pharmaceutical Filtration - The Management of Organism Removal, Meltzer TH, Jornitz MW, PDA/DHI 1998 *"Association for Advancement of Medical Instrumentation ANSI/AAMI ST41-Ehylene Oxyde Sterilization in Healthcare facilities: Safety and Effectiveness. Arlington, VA: Association for Advancement of Medical Instrumentation; 2000." *“US Department of Labor, Occupational Safety and Health Administration.29 CFR 1910.1020. Access to Employee Medical Records.". October 26, 2007. *Perioperative Standards and Recommended Practices, AORN 2013, {{DEFAULTSORT:Sterilization (Microbiology) Biocides Electron beam Hygiene Microbiology