A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the
anus
The anus (Latin, 'ring' or 'circle') is an opening at the opposite end of an animal's digestive tract from the mouth. Its function is to control the expulsion of feces, the residual semi-solid waste that remains after food digestion, which, d ...
and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depending on whether the prolapsed section is visible externally, and whether the full or only partial thickness of the rectal wall is involved.
Rectal prolapse may occur without any symptoms, but depending upon the nature of the prolapse there may be
mucous discharge (mucus coming from the anus),
rectal bleeding
Rectal bleeding refers to bleeding in the rectum. There are many causes of rectal hemorrhage, including inflamed hemorrhoids (which are dilated vessels in the perianal fat pads), rectal varices, proctitis (of various causes), stercoral ulcers an ...
, degrees of
fecal incontinence and
obstructed defecation symptoms.
Rectal prolapse is generally more common in elderly women, although it may occur at any age and in either sex. It is very rarely life-threatening, but the symptoms can be debilitating if left untreated.
Most external prolapse cases can be treated successfully, often with a surgical procedure. Internal prolapses are traditionally harder to treat and surgery may not be suitable for many patients.
Classification
The different kinds of rectal prolapse can be difficult to grasp, as different definitions are used and some recognize some subtypes and others do not. Essentially, rectal prolapses may be:
* full thickness (complete), where all the layers of the rectal wall prolapse, or involve the mucosal layer only (partial)
* external if they protrude from the anus and are visible externally, or internal if they do not
* circumferential, where the whole circumference of the rectal wall prolapse, or segmental if only parts of the circumference of the rectal wall prolapse
* present at rest, or occurring during straining.
External (complete) rectal prolapse (rectal procidentia, full thickness rectal prolapse, external rectal prolapse) is
a full thickness, circumferential, true intussusception of the rectal wall which protrudes from the anus and is visible externally.
Internal rectal intussusception (occult rectal prolapse, internal procidentia) can be defined as a funnel shaped infolding of the upper rectal (or lower
sigmoid) wall that can occur during
defecation
Defecation (or defaecation) follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus. The act has a variety of names ranging f ...
.
This infolding is perhaps best visualised as folding a sock inside out,
creating "a tube within a tube".
Another definition is "where the rectum collapses but does not exit the anus". Many sources differentiate between internal rectal intussusception and mucosal prolapse, implying that the former is a full thickness prolapse of rectal wall. However, a publication by the
American Society of Colon and Rectal Surgeons stated that internal rectal intussusception involved the
mucosa
A mucous membrane or mucosa is a membrane that lines various cavities in the body of an organism and covers the surface of internal organs. It consists of one or more layers of epithelial cells overlying a layer of loose connective tissue. It is ...
l and
submucosa
The submucosa (or tela submucosa) is a thin layer of tissue (biology), tissue in various organ (anatomy), organs of the gastrointestinal tract, gastrointestinal, respiratory tract, respiratory, and genitourinary system, genitourinary tracts. It i ...
l layers separating from the underlying
muscularis mucosa layer attachments, resulting in the separated portion of rectal lining "sliding" down.
This may signify that authors use the terms internal rectal prolapse and internal mucosal prolapse to describe the same phenomena.
Mucosal prolapse (partial rectal mucosal prolapse)
refers to prolapse of the loosening of the submucosal attachments to the muscularis propria of the distal rectummucosal layer of the rectal wall. Most sources define mucosal prolapse as an external, segmental prolapse which is easily confused with prolapsed (3rd or 4th degree)
hemorrhoids (piles).
However, both internal mucosal prolapse (see below) and circumferential mucosal prolapse are described by some.
Others do not consider mucosal prolapse a true form of rectal prolapse.
Internal mucosal prolapse (rectal internal mucosal prolapse, RIMP) refers to prolapse of the mucosal layer of the rectal wall which does not protrude externally. There is some controversy surrounding this condition as to its relationship with hemorrhoidal disease, or whether it is a separate entity.
The term "mucosal hemorrhoidal prolapse" is also used.
Solitary rectal ulcer syndrome (SRUS, solitary rectal ulcer, SRU) occurs with internal rectal intussusception and is part of the spectrum of rectal prolapse conditions.
It describes
ulceration of the rectal lining caused by repeated frictional damage as the internal intussusception is forced into the anal canal during straining. SRUS can be considered a consequence of internal intussusception, which can be demonstrated in 94% of cases.
Mucosal prolapse syndrome (MPS) is recognized by some. It includes solitary rectal ulcer syndrome, rectal prolapse, proctitis cystica profunda, and inflammatory polyps.
It is classified as a chronic benign inflammatory disorder.
Rectal prolapse and internal rectal intussusception has been classified according to the size of the prolapsed section of rectum, a function of rectal mobility from the sacrum and infolding of the rectum. This classification also takes into account sphincter relaxation:
* Grade I: nonrelaxation of the sphincter mechanism (
anismus)
* Grade II: mild intussusception
* Grade III: moderate intussusception
* Grade IV: severe intussusception
* Grade V: rectal prolapse
Rectal internal mucosal prolapse has been graded according to the level of descent of the intussusceptum, which was predictive of symptom severity:
* first degree prolapse is detectable below the anorectal ring on straining
* second degree when it reached the dentate line
* third degree when it reached the anal verge
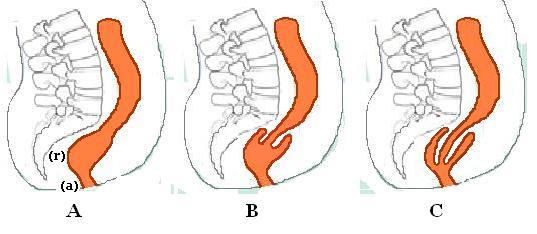
The most widely used classification of internal rectal prolapse is according to the height on the rectal/sigmoid wall from which they originate and by whether the intussusceptum remains within the rectum or extends into the
anal canal. The height of intussusception from the anal canal is usually estimated by
defecography.
Recto-rectal (high) intussusception (intra-rectal intussusception) is where the intussusception starts in the rectum, does not protrude into the anal canal, but stays within the rectum. (i.e. the intussusceptum originates in the rectum and does not extend into the anal canal. The intussuscipiens includes rectal lumen distal to the intussusceptum only). These are usually intussusceptions that originate in the upper rectum or lower
sigmoid.
Recto-anal (low) intussusception (intra-anal intussusception) is where the intussusception starts in the rectum and protrudes into the anal canal (i.e. the intussusceptum originates in the rectum, and the intussuscipiens includes part of the anal canal)
An Anatomico-Functional Classification of internal rectal intussusception has been described,
with the argument that other factors apart from the height of intussusception above the anal canal appear to be important to predict symptomology. The parameters of this classification are anatomic descent, diameter of intussuscepted bowel, associated rectal hyposensitivity and associated delayed colonic transit:
* Type 1: Internal recto-rectal intussusception
** Type 1W Wide lumen
** Type 1N Narrowed lumen
* Type 2: Internal recto-anal intussusception
** Type 2W Wide Lumen
** Type 2N Narrowed lumen
** Type 2M Narrowed internal lumen with associated rectal hyposensitivity or early megarectum
* Type 3: Internal-external recto-anal intussusception
Diagnosis
History
Patients may have associated gynecological conditions which may require multidisciplinary management.
History of constipation is important because some of the operations may worsen constipation. Fecal incontinence may also influence the choice of management.
Physical examination
Rectal prolapse may be confused easily with prolapsing hemorrhoids.
Mucosal prolapse also differs from prolapsing (3rd or 4th degree) hemorrhoids, where there is a segmental prolapse of the hemorrhoidal tissues at the 3, 7 and 11 o'clock positions.
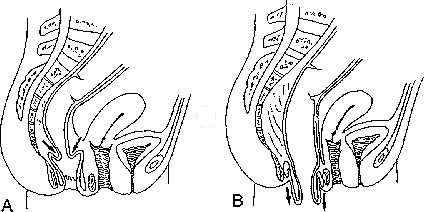
Mucosal prolapse can be differentiated from a full thickness external rectal prolapse (a complete rectal prolapse) by the orientation of the folds (furrows) in the prolapsed section. In full thickness rectal prolapse, these folds run circumferential. In mucosal prolapse, these folds are radially.
The folds in mucosal prolapse are usually associated with internal hemorrhoids. Furthermore, in rectal prolapse, there is a sulcus present between the prolapsed bowel and the anal verge, whereas in hemorrhoidal disease there is no sulcus.
Prolapsed, incarcerated hemorrhoids are extremely painful, whereas as long as a rectal prolapse is not strangulated, it gives little pain and is easy to reduce.
The prolapse may be obvious, or it may require straining and squatting to produce it.
The anus is usually patulous, (loose, open) and has reduced resting and squeeze pressures.
Sometimes it is necessary to observe the patient while they strain on a toilet to see the prolapse happen
(the perineum can be seen with a mirror or by placing an endoscope in the bowl of the toilet).
A phosphate enema may need to be used to induce straining.
The perianal skin may be macerated (softening and whitening of skin that is kept constantly wet) and show
excoriation
A skin condition, also known as cutaneous condition, is any medical condition that affects the integumentary system—the organ system that encloses the body and includes skin, nails, and related muscle and glands. The major function of this sy ...
.
Proctoscopy/sigmoidoscopy/colonoscopy
These may reveal congestion and
edema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's Tissue (biology), tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels t ...
(swelling) of the distal rectal mucosa,
and in 10-15% of cases there may be a solitary rectal ulcer on the anterior rectal wall.
Localized inflammation or ulceration can be biopsied and may lead to a diagnosis of SRUS or colitis cystica profunda.
Rarely, a
neoplasm (tumour) may form on the leading edge of the intussusceptum. In addition, patients are frequently elderly and therefore have increased incidence of
colorectal cancer
Colorectal cancer (CRC), also known as bowel cancer, colon cancer, or rectal cancer, is the development of cancer from the colon or rectum (parts of the large intestine). Signs and symptoms may include blood in the stool, a change in bowel m ...
. Full length colonoscopy is usually carried out in adults prior to any surgical intervention.
These investigations may be used with contrast media (
barium enema) which may show the associated mucosal abnormalities.
Videodefecography
This investigation is used to diagnose internal intussusception, or demonstrate a suspected external prolapse that could not be produced during the examination.
It is usually not necessary with obvious external rectal prolapse.
may demonstrate associated conditions like
cystocele
A cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complicat ...
, vaginal vault prolapse or
enterocele.
Colonic transit studies
Colonic transit studies may be used to rule out
colonic inertia if there is a history of severe constipation.
Continent prolapse patients with slow transit constipation, and who are fit for surgery may benefit from subtotal colectomy with rectopexy.
Anorectal manometry
This investigation objectively documents the functional status of the sphincters. However, the clinical significance of the findings are disputed by some.
It may be used to assess for pelvic floor dyssenergia,
(
anismus is a contraindication for certain surgeries, e.g. STARR), and these patients may benefit from post-operative
biofeedback
Biofeedback is the process of gaining greater awareness of many physiology, physiological functions of one's own body by using Electronics, electronic or other instruments, and with a goal of being able to Manipulation (psychology), manipulate t ...
therapy. Decreased squeeze and resting pressures are usually the findings, and this may predate the development of the prolapse.
Resting tone is usually preserved in patients with mucosal prolapse.
In patients with reduced resting pressure, levatorplasty may be combined with prolapse repair to further improve continence.
Anal electromyography/pudendal nerve testing
It may be used to evaluate incontinence, but there is disagreement about what relevance the results may show, as rarely do they mandate a change of surgical plan.
There may be denervation of striated musculature on the electromyogram.
Increased nerve conduction periods (nerve damage), this may be significant in predicting post-operative incontinence.
Complete rectal prolapse

Rectal prolapse is a "falling down" of the rectum so that it is visible externally. The appearance is of a reddened, proboscis-like object through the anal sphincters. Patients find the condition embarrassing.
The symptoms can be socially debilitating without treatment,
but it is rarely life-threatening.
The true incidence of rectal prolapse is unknown, but it is thought to be uncommon. As most affected people are elderly, the condition is generally under-reported. It may occur at any age, even in children,
but there is peak onset in the fourth and seventh decades.
Women over 50 are six times more likely to develop rectal prolapse than men. It is rare in men over 45 and in women under 20.
When males are affected, they tend to be young and report significant bowel function symptoms, especially
obstructed defecation,
or have a predisposing disorder (e.g., congenital
anal atresia).
When children are affected, they are usually under the age of 3.
35% of women with rectal prolapse have never had children,
suggesting that pregnancy and labour are not significant factors. Anatomical differences such as the wider pelvic outlet in females may explain the skewed gender distribution.
Associated conditions, especially in younger patients include autism, developmental delay syndromes and psychiatric conditions requiring several medications.
Signs and symptoms
Signs and symptoms include:
* history of a protruding mass.
* degrees of
fecal incontinence, (50-80% of patients)
which may simply present as a
mucous discharge.
*
constipation (20-50% of patients)
also described as
tenesmus (a sensation of incomplete evacuation of stool) and
obstructed defecation.
* a feeling of bearing down.
*
rectal bleeding
Rectal bleeding refers to bleeding in the rectum. There are many causes of rectal hemorrhage, including inflamed hemorrhoids (which are dilated vessels in the perianal fat pads), rectal varices, proctitis (of various causes), stercoral ulcers an ...
*
diarrhea and erratic bowel habits.
Initially, the mass may protrude through the anal canal only during defecation and straining, and spontaneously return afterwards. Later, the mass may have to be pushed back in following defecation. This may progress to a chronically prolapsed and severe condition, defined as spontaneous prolapse that is difficult to keep inside, and occurs with walking, prolonged standing,
coughing or sneezing (
Valsalva
The Valsalva maneuver is performed by a forceful attempt of exhalation against a closed airway, usually done by closing one's mouth and pinching one's nose shut while expelling air out as if blowing up a balloon. Variations of the maneuver can ...
maneuvers).
A chronically prolapsed rectal tissue may undergo pathological changes such as thickening, ulceration and bleeding.
If the prolapse becomes trapped externally outside the anal sphincters, it may become strangulated and there is a risk of perforation.
This may require an urgent surgical operation if the prolapse cannot be manually reduced.
Applying granulated sugar on the exposed rectal tissue can reduce the
edema
Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's Tissue (biology), tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels t ...
(swelling) and facilitate this.
Cause

The precise cause is unknown,
and has been much debated.
In 1912 Moschcowitz proposed that rectal prolapse was a sliding hernia through a pelvic
fascia
A fascia (; plural fasciae or fascias; adjective fascial; from Latin: "band") is a band or sheet of connective tissue, primarily collagen, beneath the skin that attaches to, stabilizes, encloses, and separates muscles and other internal organs. ...
l defect.
This theory was based on the observation that rectal prolapse patients have a mobile and unsupported pelvic floor, and a hernia sac of peritoneum from the Pouch of Douglas and rectal wall can be seen.
Other adjacent structures can sometimes be seen in addition to the rectal prolapse.
Although a
pouch of Douglas hernia, originating in the cul de sac of Douglas, may protrude from the anus (via the anterior rectal wall),
this is a different situation from rectal prolapse.
Shortly after the invention of
defecography, In 1968 Broden and Snellman used
cinedefecography to show that rectal prolapse begins as a circumferential intussusception of the rectum,
which slowly increases over time.
The leading edge of the intussusceptum may be located at 6–8 cm or at 15–18 cm from the
anal verge.
This proved an older theory from the 18th century by
John Hunter and
Albrecht von Haller
Albrecht von Haller (also known as Albertus de Haller; 16 October 170812 December 1777) was a Swiss anatomist, physiologist, naturalist, encyclopedist, bibliographer and poet. A pupil of Herman Boerhaave, he is often referred to as "the fa ...
that this condition is essentially a full-thickness rectal intussusception, beginning about 3 inches above the
dentate line and protruding externally.
Since most patients with rectal prolapse have a long history of constipation,
it is thought that prolonged, excessive and repetitive straining during defecation may predispose to rectal prolapse.
Since rectal prolapse itself causes functional obstruction, more straining may result from a small prolapse, with increasing damage to the anatomy.
This excessive straining may be due to predisposing pelvic floor dysfunction (e.g.
obstructed defecation) and anatomical factors:
* Abnormally low descent of the peritoneum covering the anterior rectal wall
* poor posterior rectal fixation, resulting in loss of posterior fixation of the rectum to the sacral curve
* loss of the normal horizontal position of the rectum
with lengthening (redundant rectosigmoid)
and downward displacement of the sigmoid and rectum
* long rectal mesentery
* a deep cul-de-sac
* levator diastasis
* a patulous, weak anal sphincter
Some authors question whether these abnormalities are the cause, or secondary to the prolapse.
Other predisposing factors/associated conditions include:
* pregnancy
(although 35% of women who develop rectal prolapse are
nulliparous)
(have never given birth)
* previous surgery
(30-50% of females with the condition underwent previous gynecological surgery)
* pelvic neuropathies and neurological disease
* high gastrointestinal
helminth
Parasitic worms, also known as helminths, are large macroparasites; adults can generally be seen with the naked eye. Many are intestinal worms that are soil-transmitted and infect the gastrointestinal tract. Other parasitic worms such as schi ...
loads (e.g.
Whipworm)
* COPD
* cystic fibrosis
The association with uterine prolapse (10-25%) and cystocele (35%) may suggest that there is some underlying abnormality of the pelvic floor that affects multiple pelvic organs.
Proximal bilateral pudendal neuropathy has been demonstrated in patients with rectal prolapse who have fecal incontinence.
This finding was shown to be absent in healthy subjects, and may be the cause of denervation-related atrophy of the external anal sphincter. Some authors suggest that
pudendal nerve damage is the cause for pelvic floor and anal sphincter weakening, and may be the underlying cause of a spectrum of pelvic floor disorders.
Sphincter function in rectal prolapse is almost always reduced.
This may be the result of direct sphincter injury by chronic stretching of the prolapsing rectum. Alternatively, the intussuscepting rectum may lead to chronic stimulation of the rectoanal inhibitory reflex (RAIR - contraction of the external anal sphincter in response to stool in the rectum). The RAIR was shown to be absent or blunted. Squeeze (maximum voluntary contraction) pressures may be affected as well as the resting tone. This is most likely a denervation injury to the external anal sphincter.
The assumed mechanism of
fecal incontinence in rectal prolapse is by the chronic stretch and trauma to the anal sphincters and the presence of a direct conduit (the intussusceptum) connecting rectum to the external environment which is not guarded by the sphincters.
The assumed mechanism of obstructed defecation is by disruption to the rectum and anal canal's ability to contract and fully evacuate rectal contents. The intussusceptum itself may mechanically obstruct the rectoanal
lumen, creating a blockage that straining, anismus and colonic dysmotility exacerbate.
Some believe that internal rectal intussusception represents the initial form of a progressive spectrum of disorders the extreme of which is external rectal prolapse. The intermediary stages would be gradually increasing sizes of intussusception. However, internal intussusception rarely progresses to external rectal prolapse.
The factors that result in a patient progressing from internal intussusception to a full thickness rectal prolapse remain unknown.
Defecography studies demonstrated that degrees of internal intussusception are present in 40% of asymptomatic subjects, raising the possibility that it represents a normal variant in some, and may predispose patients to develop symptoms, or exacerbate other problems.
Treatment
Conservative
Surgery is thought to be the only option to potentially cure a complete rectal prolapse.
For people with medical problems that make them unfit for surgery, and those who have minimal symptoms, conservative measures may be beneficial. Dietary adjustments, including increasing dietary fiber may be beneficial to reduce constipation, and thereby reduce straining.
A bulk forming agent (e.g.
psyllium) or stool softener can also reduce constipation.
Surgical
Surgery is often required to prevent further damage to the anal sphincters. The goals of surgery are to restore the normal anatomy and to minimize symptoms. There is no globally agreed consensus as to which procedures are more effective,
and there have been over 50 different operations described.
Surgical approaches in rectal prolapse can be either perineal or abdominal. A perineal approach (or trans-perineal) refers to surgical access to the rectum and sigmoid colon via an incision around the anus and
perineum (the area between the genitals and the anus).
Abdominal approach (trans-abdominal approach) involves the surgeon cutting into the
abdomen and gaining surgical access to the
pelvic cavity. Procedures for rectal prolapse may involve fixation of the bowel (rectopexy), or resection (a portion removed), or both.
Trans-anal (endo-anal) procedures are also described where access to the internal rectum is gained through the anus itself.
Abdominal procedures are associated with lower risk of postoperative recurrence of the prolapse, compared with perineal procedures (6.1% vs 16.3% in patients who are younger than 65 years of age at the time of surgery).
=Abdominal procedures
=
The abdominal approach carries a small risk of impotence in males (e.g. 1-2% in abdominal rectopexy).
Abdominal operations may be open or
laparoscopic (keyhole surgery).
Laparoscopic procedures
Recovery time following laparoscopic surgery is shorter and less painful than following traditional abdominal surgery.
Instead of opening the pelvic cavity with a wide incision (laparotomy), a laparoscope (a thin, lighted tube) and surgical instruments are inserted into the pelvic cavity via small incisions.
Rectopexy and anterior resection have been performed laparoscopically with good results.
=Perineal procedures
=
The perineal approach generally results in less post-operative pain and complications, and a reduced length of hospital stay. These procedures generally carry a higher recurrence rate and poorer functional outcome.
The perineal procedures include perineal rectosigmoidectomy and Delorme repair.
Elderly, or other medically high-risk patients are usually treated by perineal procedures,
as they can be performed under a
regional anesthetic, or even
local anesthetic with
intravenous sedation
Sedation is the reduction of irritability or agitation by administration of sedative drugs, generally to facilitate a medical procedure or diagnostic procedure. Examples of drugs which can be used for sedation include isoflurane, diethyl ether, ...
, thus avoid the risks of a
general anesthetic.
Alternatively, perineal procedures may be selected to reduce risk of nerve damage, for example in young male patients for whom sexual dysfunction may be a major concern.
Perineal rectosigmoidectomy
The goal of Perineal rectosigmoidectomy is to resect or remove the redundant bowel. This is done through the perineum. The lower rectum is anchored to the sacrum through fibrosis in order to prevent future prolapse.
The full thickness of the rectal wall is incised at a level just above the dentate line. Redundant rectal and sigmoid wall is removed and the new edge of colon is reconnected (anastomosed) with the anal canal with stitches or staples.
This procedure may be combined with levatorplasty, to tighten the pelvic muscles.
A combined a perineal proctosigmoidectomy with anterior levatorplasty is also called an Altemeier procedure.
Levatorplasty is performed to correct levator diastasis which is commonly associated with rectal prolapse.
Perineal rectosigmoidectomy was first introduced by Mikulicz in 1899, and it remained the preferred treatment in Europe for many years.
It was Popularized by Altemeier.
The procedure is simple, safe and effective.
Continence levatorplasty may enhance restoration of continence (2/3 of patients).
Complications occur in less than 10% of cases, and include pelvic bleeding, pelvic abscess and anastomotic dehiscence (splitting apart of the stitches inside), bleeding or leak at a dehiscence
Mortality is low.
Recurrence rates are higher than for abdominal repair,
16-30%, but more recent studies give lower recurrence rates.
Additional levatorplasty can reduce recurrence rates to 7%.
Delorme Procedure
This is a modification of the perineal rectosigmoidectomy, differing in that only the mucosa and submucosa are excised from the prolapsed segment, rather than full thickness resection.
The prolapse is exposed if it is not already present, and the mucosal and submucosal layers are stripped from the redundant length of bowel. The muscle layer that is left is plicated (folded) and placed as a buttress above the pelvic floor.
The edges of the mucosal are then stitched back together. "Mucosal proctectomy" was first discussed by Delorme in 1900,
now it is becoming more popular again as it has low morbidity and avoids an abdominal incision, while effectively repairing the prolapse.
The procedure is ideally suited to those patients with full-thickness prolapse limited to partial circumference (e.g., anterior wall) or less-extensive prolapse (perineal rectosigmoidectomy may be difficult in this situation).
Fecal incontinence is improved following surgery (40%–75% of patients).
Post operatively, both mean resting and squeeze pressures were increased.
Constipation is improved in 50% of cases,
but often urgency and tenesmus are created. Complications, including infection, urinary retention, bleeding,
anastomotic
An anastomosis (, plural anastomoses) is a connection or opening between two things (especially cavities or passages) that are normally diverging or branching, such as between blood vessels, leaf veins, or streams. Such a connection may be normal ...
dehiscence (opening of the stitched edges inside), stricture (narrowing of the gut lumen), diarrhea, and fecal impaction occur in 6-32% of cases.
Mortality occurs in 0–2.5% cases.
There is a higher recurrence rate than abdominal approaches (7-26% cases).
Anal encirclement (Thirsch procedure)
This procedure can be carried out under
local anaesthetic. After reduction of the prolapse, a subcutaneous suture (a stich under the skin) or other material is placed encircling the anus, which is then made taut to prevent further prolapse.
Placing silver wire around the anus first described by Thiersch in 1891.
Materials used include nylon, silk, silastic rods, silicone, Marlex mesh, Mersilene mesh, fascia, tendon, and Dacron.
This operation does not correct the prolapse itself, it merely supplements the anal sphincter, narrowing the anal canal with the aim of preventing the prolapse from becoming external, meaning it remains in the rectum.
This goal is achieved in 54-100% cases. Complications include breakage of the encirclement material, fecal impaction, sepsis, and erosion into the skin or anal canal. Recurrence rates are higher than the other perineal procedures. This procedure is most often used for people who have a severe condition or who have a high risk of adverse effects from general anesthetic,
and who may not tolerate other perineal procedures.
Internal rectal intussusception
Internal rectal intussusception (rectal intussusception, internal intussusception, internal rectal prolapse, occult rectal prolapse, internal rectal
procidentia and rectal invagination) is a medical condition defined as a funnel shaped infolding of the
rectal wall that can occur during
defecation
Defecation (or defaecation) follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus. The act has a variety of names ranging f ...
.
This phenomenon was first described in the late 1960s when
defecography was first developed and became widespread.
Degrees of internal intussusception have been demonstrated in 40% of asymptomatic subjects, raising the possibility that it represents a normal variant in some, and may predispose patients to develop symptoms, or exacerbate other problems.
Symptoms
Internal intussusception may be
asymptomatic
In medicine, any disease is classified asymptomatic if a patient tests as carrier for a disease or infection but experiences no symptoms. Whenever a medical condition fails to show noticeable symptoms after a diagnosis it might be considered asy ...
, but common symptoms include:
*
Fecal leakage
* Sensation of
obstructed defecation (
tenesmus).
* Pelvic pain.
*
Rectal bleeding
Rectal bleeding refers to bleeding in the rectum. There are many causes of rectal hemorrhage, including inflamed hemorrhoids (which are dilated vessels in the perianal fat pads), rectal varices, proctitis (of various causes), stercoral ulcers an ...
.
Recto-rectal intussusceptions may be
asymptomatic
In medicine, any disease is classified asymptomatic if a patient tests as carrier for a disease or infection but experiences no symptoms. Whenever a medical condition fails to show noticeable symptoms after a diagnosis it might be considered asy ...
, apart from mild obstructed defecation. "interrupted defaecation" in the morning is thought by some to be characteristic.
Recto-anal intussusceptions commonly give more severe symptoms of straining, incomplete evacuation, need for digital evacuation of stool, need for support of the
perineum during defecation, urgency, frequency or intermittent
fecal incontinence.
It has been observed that intussusceptions of thickness ≥3 mm, and those that appear to cause obstruction to rectal evacuation may give clinical symptoms.
Cause
There are two schools of thought regarding the nature of internal intussusception, viz: whether it is a primary phenomenon, or secondary to (a consequence of) another condition.
Some believe that it represents the initial form of a progressive spectrum of disorders the extreme of which is external rectal prolapse. The intermediary stages would be gradually increasing sizes of intussusception. The folding section of rectum can cause repeated trauma to the mucosa, and can cause
solitary rectal ulcer syndrome.
However, internal intussusception rarely progress to external rectal prolapse.
Others argue that the majority of patients appear to have rectal intussusception as a consequence of obstructed defecation rather than a cause, possibly related to excessive straining in patients with obstructed defecation.
Patients with other causes of obstructed defecation (
outlet obstruction) like
anismus also tend to have higher incidence of internal intussusception.
Enteroceles are coexistent in 11% of patients with internal intussusception. Symptoms of internal intussusception overlap with those of
rectocele, indeed the 2 conditions can occur together.
Patients with
solitary rectal ulcer syndrome combined with internal intussusception (as 94% of SRUS patients have) were shown to have altered rectal wall biomechanics compared to patients with internal intussusception alone. The presumed mechanism of the
obstructed defecation is by telescoping of the intussusceptum, occluding the rectal lumen during attempted defecation.
One study analysed resected rectal wall specimens in patients with obstructed defecation associated with rectal intussusception undergoing
stapled trans-anal rectal resection
A rectal prolapse occurs when walls of the rectum have prolapsed to such a degree that they protrude out of the anus and are visible outside the body. However, most researchers agree that there are 3 to 5 different types of rectal prolapse, depen ...
. They reported abnormalities of the
enteric nervous system and
estrogen receptors
Estrogen receptors (ERs) are a group of proteins found inside cells. They are receptors that are activated by the hormone estrogen ( 17β-estradiol). Two classes of ER exist: nuclear estrogen receptors (ERα and ERβ), which are members of the ...
.
One study concluded that intussusception of the
anterior
Standard anatomical terms of location are used to unambiguously describe the anatomy of animals, including humans. The terms, typically derived from Latin or Greek roots, describe something in its standard anatomical position. This position prov ...
rectal wall shares the same cause as
rectocele, namely deficient recto-vaginal ligamentous support.
Comorbidities and complications
The following conditions occur more commonly in patients with internal rectal intussusception than in the general population:
*
Rectocele
*
Solitary rectal ulcer syndrome.
Diagnosis
Unlike external rectal prolapse, internal rectal intussusception is not visible externally, but it may still be diagnosed by
digital rectal examination
Digital rectal examination (DRE; la, palpatio per anum, PPA) is an internal examination of the rectum, performed by a healthcare provider. Prior to a 2018 report from the U.S. Preventive Services Task Force, the DRE was a common and "dreaded" co ...
, while the patient strains as if to defecate.
Imaging such as a
defecating proctogram or dynamic MRI defecography can demonstrate the abnormal folding of the rectal wall. Some have advocated the use of anorectal physiology testing (
anorectal manometry).
Treatment
Non surgical measures to treat internal intussusception include pelvic floor retraining, a
bulking agent
Food additives are substances added to food to preserve flavor or enhance taste, appearance, or other sensory qualities. Some additives have been used for centuries as part of an effort to preserve food, for example vinegar (pickling), salt (salt ...
(e.g.
psyllium),
suppositories
A suppository is a dosage form used to deliver medications by insertion into a body orifice where it dissolves or melts to exert local or systemic effects. There are three types of suppositories, each to insert into a different sections: rectal su ...
or
enemas to relieve constipation and straining.
If there is
incontinence
Incontinence or Incontinent may refer to:
* Fecal incontinence, the involuntary excretion of bowel contents
* Urinary incontinence, the involuntary excretion of urine
* Lack of moderation or self-control, especially related to sexual desire - see ...
(
fecal leakage or more severe FI), or paradoxical contraction of the pelvic floor (
anismus), then biofeedback retraining is indicated.
Some researchers advise that internal intussusception be managed conservatively, compared to external rectal prolapse which usually requires surgery.
As with external rectal prolapse, there are a great many different surgical interventions described. Generally, a section of rectal wall can be
resected (removed), or the rectum can be fixed (rectopexy) to its original position against the
sacral vertebrae
The sacrum (plural: ''sacra'' or ''sacrums''), in human anatomy, is a large, triangular bone at the base of the spine that forms by the fusing of the sacral vertebrae (S1S5) between ages 18 and 30.
The sacrum situates at the upper, back part ...
, or a combination of both methods. Surgery for internal rectal prolapse can be via the abdominal approach or the transanal approach.
It is clear that there is a wide spectrum of symptom severity, meaning that some patients may benefit from surgery and others may not. Many procedures receive conflicting reports of success, leading to a lack of any consensus about the best way to manage this problem.
Relapse of the intussusception after treatment is a problem. Two of the most commonly employed procedures are discussed below.
laparoscopic ventral (mesh) rectopexy (LVR)
This procedure aims to "
orrectthe descent of the posterior and middle pelvic compartments combined with reinforcement of the rectovaginal septum".
Rectopexy has been shown to improve anal incontinence (
fecal leakage) in patients with rectal intussusception. The operation has been shown to have low recurrence rate (around 5%).
It also improves obstructed defecation symptoms.
Complications include constipation, which is reduced if the technique does not use posterior rectal mobilization (freeing the rectum from its attached back surface).
The advantage of the laparoscopic approach is decreased healing time and less complications.
Stapled trans-anal rectal resection (STARR)
This operation aims to "remove the anorectal mucosa circumferential and reinforce the anterior anorectal junction wall with the use of a circular stapler".
In contrast to other methods, STARR does not correct the descent of the rectum, it removes the redundant tissue.
The technique was developed from a similar stapling procedure for prolapsing
hemorrhoids. Since, specialized circular staplers have been developed for use in external rectal prolapse and internal rectal intussusception.
Complications, sometimes serious, have been reported following STARR,
but the procedure is now considered safe and effective.
STARR is
contraindicated in patients with weak sphincters (fecal incontinence and urgency are a possible complication) and with
anismus (paradoxical contraction of the pelvic floor during attempted defecation).
The operation has been shown to improve rectal sensitivity and decrease rectal volume, the reason thought to create urgency.
90% of patients do not report urgency 12 months after the operation. The anal sphincter may also be stretched during the operation. STARR was compared with biofeedback and found to be more effective at reducing symptoms and improving quality of life.
Mucosal prolapse
Rectal mucosal prolapse (mucosal prolapse, anal mucosal prolapse) is a sub-type of rectal prolapse, and refers to abnormal descent of the
rectal mucosa
A mucous membrane or mucosa is a membrane that lines various cavities in the body of an organism and covers the surface of internal organs. It consists of one or more layers of epithelial cells overlying a layer of loose connective tissue. It is ...
through the
anus
The anus (Latin, 'ring' or 'circle') is an opening at the opposite end of an animal's digestive tract from the mouth. Its function is to control the expulsion of feces, the residual semi-solid waste that remains after food digestion, which, d ...
.
It is different to an internal intussusception (occult prolapse) or a complete rectal prolapse (external prolapse, procidentia) because these conditions involve the full thickness of the rectal wall, rather than only the mucosa (lining).
Mucosal prolapse is a different condition to prolapsing (3rd or 4th degree)
hemorrhoids
Hemorrhoids (or haemorrhoids), also known as piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term ''hemo ...
,
although they may look similar.
Rectal mucosal prolapse can be a cause of
obstructed defecation (outlet obstruction).
and
rectal malodor
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the sigmoid colon) at the l ...
.
Symptoms
Symptom severity increases with the size of the prolapse, and whether it spontaneously reduces after defecation, requires manual reduction by the patient, or becomes irreducible. The symptoms are identical to advanced hemorrhoidal disease,
and include:
*
Fecal leakage causing staining of undergarments
*
Rectal bleeding
Rectal bleeding refers to bleeding in the rectum. There are many causes of rectal hemorrhage, including inflamed hemorrhoids (which are dilated vessels in the perianal fat pads), rectal varices, proctitis (of various causes), stercoral ulcers an ...
* Mucous
rectal discharge
*
Rectal pain
*
Pruritus ani
Cause
The condition, along with complete rectal prolapse and
internal rectal intussusception, is thought to be related to chronic straining during
defecation
Defecation (or defaecation) follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus. The act has a variety of names ranging f ...
and
constipation.
Mucosal prolapse occurs when the results from loosening of the submucosal attachments (between the mucosal layer and the
muscularis propria) of the
distal
Standard anatomical terms of location are used to unambiguously describe the anatomy of animals, including humans. The terms, typically derived from Latin or Greek roots, describe something in its standard anatomical position. This position pro ...
rectum
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the Gastrointestinal tract, gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the s ...
.
The section of prolapsed rectal mucosa can become ulcerated, leading to bleeding.
Diagnosis
Mucosal prolapse can be differentiated from a full thickness external rectal prolapse (a complete rectal prolapse) by the orientation of the folds (furrows) in the prolapsed section. In full thickness rectal prolapse, these folds run circumferential. In mucosal prolapse, these folds are radially.
The folds in mucosal prolapse are usually associated with internal hemorrhoids.
Treatment
EUA (examination under anesthesia) of anorectum and banding of the mucosa with rubber bands.
Solitary rectal ulcer syndrome and colitis cystica profunda
Solitary rectal ulcer syndrome (SRUS, SRU), is a disorder of the
rectum
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the Gastrointestinal tract, gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the s ...
and
anal canal, caused by straining and increased pressure during
defecation
Defecation (or defaecation) follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus. The act has a variety of names ranging f ...
. This increased pressure causes the anterior portion of the rectal lining to be forced into the anal canal (an
internal rectal intussusception). The lining of the rectum is repeatedly damaged by this friction, resulting in
ulceration. SRUS can therefore be considered to be a consequence of internal intussusception (a sub type of rectal prolapse), which can be demonstrated in 94% of cases. It may be
asymptomatic
In medicine, any disease is classified asymptomatic if a patient tests as carrier for a disease or infection but experiences no symptoms. Whenever a medical condition fails to show noticeable symptoms after a diagnosis it might be considered asy ...
, but it can cause
rectal pain,
rectal bleeding
Rectal bleeding refers to bleeding in the rectum. There are many causes of rectal hemorrhage, including inflamed hemorrhoids (which are dilated vessels in the perianal fat pads), rectal varices, proctitis (of various causes), stercoral ulcers an ...
,
rectal malodor
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the sigmoid colon) at the l ...
, incomplete evacuation and
obstructed defecation (rectal outlet obstruction).
Symptoms
Symptoms include:
defecation
Defecation (or defaecation) follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus. The act has a variety of names ranging f ...
* Mucous rectal discharge
* Rectal bleeding
Rectal bleeding refers to bleeding in the rectum. There are many causes of rectal hemorrhage, including inflamed hemorrhoids (which are dilated vessels in the perianal fat pads), rectal varices, proctitis (of various causes), stercoral ulcers an ...
* Sensation of incomplete evacuation ( tenesmus)
* constipation, or more rarely diarrhea
* fecal incontinence (rarely)
Prevalence
The condition is thought to be uncommon. It usually occurs in young adults, but children can be affected too.
Cause
The essential cause of SRUS is thought to be related to too much straining during defecation.
Overactivity of the anal sphincter during defecation causes the patient to require more effort to expel stool. This pressure is produced by the modified valsalva manovoure (attempted forced exhalation against a closed glottis, resulting in increased abdominal and intra-rectal pressure). Patiest with SRUS were shown to have higher intra-rectal pressures when straining than healthy controls. SRUS is also associated with prolonged and incomplete evacuation of stool.ischemia
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems wi ...
), combined with repeated frictional trauma from the prolapsing lining, and exposure to increased pressure are thought to cause ulceration. Trauma from hard stools may also contribute.
The site of the ulcer is typically on the anterior
Standard anatomical terms of location are used to unambiguously describe the anatomy of animals, including humans. The terms, typically derived from Latin or Greek roots, describe something in its standard anatomical position. This position prov ...
wall of the rectal ampulla
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the sigmoid colon) at the le ...
, about 7–10 cm from the anus. However, the area may of ulceration may be closer to the anus, deeper inside, or on the lateral or posterior rectal walls. The name "solitary" can be misleading since there may be more than one ulcer present. Furthermore, there is a "preulcerative phase" where there is no ulcer at all.
Pathological specimens of sections of rectal wall taken from SRUS patients show thickening and replacement of muscle with fibrous tissue and excess collagen. Rarely, SRUS can present as polyps in the rectum.
SRUS is therefore associated and with internal, and more rarely, external rectal prolapse.cystica profunda Cystica profunda is a rare disease of the gut lining. It is characterized by formation of mucin cysts in the muscle layers of the gut lining, and it can occur anywhere along the gastrointestinal tract.
When the condition occurs in the stomach, it m ...
in the rectum. Cystica profunda is characterized by formation of mucin cysts in the muscle layers of the gut lining, and it can occur anywhere along the gastrointestinal tract. When it occurs in the rectum, some believe to be an interchangeable diagnosis with SRUS since the histologic
Histology,
also known as microscopic anatomy or microanatomy, is the branch of biology which studies the microscopic anatomy of biological tissues. Histology is the microscopic counterpart to gross anatomy, which looks at larger structures vis ...
features of the conditions overlap.
Complications
Complications are uncommon, but include massive rectal bleeding, ulceration into the prostate gland or formation of a stricture. Very rarely, cancer can arise on the section of prolapsed rectal lining.
Diagnosis and investigations
SRUS is commonly misdiagnosed, and the diagnosis is not made for 5–7 years.endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, f ...
* inflammatory granuloma
A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious ...
s
* infectious disorders
* drug-induced colitis
* mucus-producing adenocarcinoma
Adenocarcinoma (; plural adenocarcinomas or adenocarcinomata ) (AC) is a type of cancerous tumor that can occur in several parts of the body. It is defined as neoplasia of epithelial tissue that has glandular origin, glandular characteristics, or ...
Defecography, sigmoidoscopy, transrectal ultrasound, mucosal biopsy, anorectal manometry and electromyography
Electromyography (EMG) is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyog ...
have all been used to diagnose and study SRUS.
Treatment
Although SRUS is not a medically serious disease, it can be the cause of significantly reduced quality of life for patients. It is difficult to treat, and treatment is aimed at minimizing symptoms.
Stopping straining during bowel movements, by use of correct posture, dietary fiber
Dietary fiber (in British English fibre) or roughage is the portion of plant-derived food that cannot be completely broken down by human digestive enzymes. Dietary fibers are diverse in chemical composition, and can be grouped generally by the ...
intake (possibly included bulk forming laxatives such as psyllium), stool softeners (e.g. polyethylene glycol, and biofeedback
Biofeedback is the process of gaining greater awareness of many physiology, physiological functions of one's own body by using Electronics, electronic or other instruments, and with a goal of being able to Manipulation (psychology), manipulate t ...
retraining to coordinate pelvic floor during defecation.
Surgery may be considered, but only if non surgical treatment has failed and the symptoms are severe enough to warrant the intervention. Improvement with surgery is about 55-60%.
Ulceration may persist even when symptoms resolve.
Mucosal prolapse syndrome
A group of conditions known as Mucosal prolapse syndrome (MPS) has now been recognized. It includes SRUS, rectal prolapse, proctitis cystica profunda, and inflammatory polyps.
Epidemiology
Rectal prolapse affects less than 0.5% of the general population.
Pornography
Rosebud pornography and Prolapse pornography (or rosebudding or rectal prolapse pornography) is an anal sex practice that occurs in some extreme anal pornography wherein a pornographic actor or actress performs a rectal prolapse wherein the walls of the rectum slip out of the anus. Rectal prolapse is a serious medical condition that requires the attention of a medical professional. However, in rosebud pornography, it is performed deliberately. Michelle Lhooq, writing for VICE, argues that rosebudding is an example of producers making 'extreme' content due to the easy availability of free pornography on the internet. She also argues that rosebudding is a way for pornographic actors and actresses to distinguish themselves.
Terminology
Prolapse refers to "the falling down or slipping of a body part from its usual position or relations". It is derived from the Latin ''pro-'' - "forward" + ''labi'' - "to slide". Prolapse can refer to many different medical conditions other than rectal prolapse.
procidentia has a similar meaning to prolapse, referring to "a sinking or prolapse of an organ or part". It is derived from the Latin ''procidere'' - "to fall forward".intussusception Intussusception may refer to:
* Intussusception (medical disorder)
Intussusception is a medical condition in which a part of the intestine folds into the section immediately ahead of it. It typically involves the small bowel and less commonly t ...
s involving colon or small intestine
The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the p ...
, which can sometimes be a medical emergency. Rectal intussusception by contrast is not life-threatening.
Intussusceptum refers to the proximal
Standard anatomical terms of location are used to unambiguously describe the anatomy of animals, including humans. The terms, typically derived from Latin or Greek roots, describe something in its standard anatomical position. This position ...
section of rectal wall, which telescopes into the lumen of the distal
Standard anatomical terms of location are used to unambiguously describe the anatomy of animals, including humans. The terms, typically derived from Latin or Greek roots, describe something in its standard anatomical position. This position pro ...
section of rectum
The rectum is the final straight portion of the large intestine in humans and some other mammals, and the Gastrointestinal tract, gut in others. The adult human rectum is about long, and begins at the rectosigmoid junction (the end of the s ...
(termed the intussuscipiens).
See also
* Fecal incontinence
* Obstructed defecation
* Rectal discharge
* Anismus
References
External links
{{DEFAULTSORT:Rectal Prolapse
Colorectal surgery
Rectum
 The most widely used classification of internal rectal prolapse is according to the height on the rectal/sigmoid wall from which they originate and by whether the intussusceptum remains within the rectum or extends into the anal canal. The height of intussusception from the anal canal is usually estimated by defecography.
Recto-rectal (high) intussusception (intra-rectal intussusception) is where the intussusception starts in the rectum, does not protrude into the anal canal, but stays within the rectum. (i.e. the intussusceptum originates in the rectum and does not extend into the anal canal. The intussuscipiens includes rectal lumen distal to the intussusceptum only). These are usually intussusceptions that originate in the upper rectum or lower sigmoid.
Recto-anal (low) intussusception (intra-anal intussusception) is where the intussusception starts in the rectum and protrudes into the anal canal (i.e. the intussusceptum originates in the rectum, and the intussuscipiens includes part of the anal canal)
An Anatomico-Functional Classification of internal rectal intussusception has been described, with the argument that other factors apart from the height of intussusception above the anal canal appear to be important to predict symptomology. The parameters of this classification are anatomic descent, diameter of intussuscepted bowel, associated rectal hyposensitivity and associated delayed colonic transit:
* Type 1: Internal recto-rectal intussusception
** Type 1W Wide lumen
** Type 1N Narrowed lumen
* Type 2: Internal recto-anal intussusception
** Type 2W Wide Lumen
** Type 2N Narrowed lumen
** Type 2M Narrowed internal lumen with associated rectal hyposensitivity or early megarectum
* Type 3: Internal-external recto-anal intussusception
The most widely used classification of internal rectal prolapse is according to the height on the rectal/sigmoid wall from which they originate and by whether the intussusceptum remains within the rectum or extends into the anal canal. The height of intussusception from the anal canal is usually estimated by defecography.
Recto-rectal (high) intussusception (intra-rectal intussusception) is where the intussusception starts in the rectum, does not protrude into the anal canal, but stays within the rectum. (i.e. the intussusceptum originates in the rectum and does not extend into the anal canal. The intussuscipiens includes rectal lumen distal to the intussusceptum only). These are usually intussusceptions that originate in the upper rectum or lower sigmoid.
Recto-anal (low) intussusception (intra-anal intussusception) is where the intussusception starts in the rectum and protrudes into the anal canal (i.e. the intussusceptum originates in the rectum, and the intussuscipiens includes part of the anal canal)
An Anatomico-Functional Classification of internal rectal intussusception has been described, with the argument that other factors apart from the height of intussusception above the anal canal appear to be important to predict symptomology. The parameters of this classification are anatomic descent, diameter of intussuscepted bowel, associated rectal hyposensitivity and associated delayed colonic transit:
* Type 1: Internal recto-rectal intussusception
** Type 1W Wide lumen
** Type 1N Narrowed lumen
* Type 2: Internal recto-anal intussusception
** Type 2W Wide Lumen
** Type 2N Narrowed lumen
** Type 2M Narrowed internal lumen with associated rectal hyposensitivity or early megarectum
* Type 3: Internal-external recto-anal intussusception
 Rectal prolapse is a "falling down" of the rectum so that it is visible externally. The appearance is of a reddened, proboscis-like object through the anal sphincters. Patients find the condition embarrassing. The symptoms can be socially debilitating without treatment, but it is rarely life-threatening.
The true incidence of rectal prolapse is unknown, but it is thought to be uncommon. As most affected people are elderly, the condition is generally under-reported. It may occur at any age, even in children, but there is peak onset in the fourth and seventh decades. Women over 50 are six times more likely to develop rectal prolapse than men. It is rare in men over 45 and in women under 20. When males are affected, they tend to be young and report significant bowel function symptoms, especially obstructed defecation, or have a predisposing disorder (e.g., congenital anal atresia). When children are affected, they are usually under the age of 3.
35% of women with rectal prolapse have never had children, suggesting that pregnancy and labour are not significant factors. Anatomical differences such as the wider pelvic outlet in females may explain the skewed gender distribution.
Associated conditions, especially in younger patients include autism, developmental delay syndromes and psychiatric conditions requiring several medications.
Rectal prolapse is a "falling down" of the rectum so that it is visible externally. The appearance is of a reddened, proboscis-like object through the anal sphincters. Patients find the condition embarrassing. The symptoms can be socially debilitating without treatment, but it is rarely life-threatening.
The true incidence of rectal prolapse is unknown, but it is thought to be uncommon. As most affected people are elderly, the condition is generally under-reported. It may occur at any age, even in children, but there is peak onset in the fourth and seventh decades. Women over 50 are six times more likely to develop rectal prolapse than men. It is rare in men over 45 and in women under 20. When males are affected, they tend to be young and report significant bowel function symptoms, especially obstructed defecation, or have a predisposing disorder (e.g., congenital anal atresia). When children are affected, they are usually under the age of 3.
35% of women with rectal prolapse have never had children, suggesting that pregnancy and labour are not significant factors. Anatomical differences such as the wider pelvic outlet in females may explain the skewed gender distribution.
Associated conditions, especially in younger patients include autism, developmental delay syndromes and psychiatric conditions requiring several medications.
 The precise cause is unknown, and has been much debated. In 1912 Moschcowitz proposed that rectal prolapse was a sliding hernia through a pelvic
The precise cause is unknown, and has been much debated. In 1912 Moschcowitz proposed that rectal prolapse was a sliding hernia through a pelvic