Reperfusion Therapy on:
[Wikipedia]
[Google]
[Amazon]
Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack (
 Emergency bypass surgery for the treatment of an acute myocardial infarction (MI) is less common than PCI or thrombolysis. From 1995 to 2004, the percentage of people with
Emergency bypass surgery for the treatment of an acute myocardial infarction (MI) is less common than PCI or thrombolysis. From 1995 to 2004, the percentage of people with
myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may ...
(MI)). Reperfusion therapy includes drugs
A drug is any chemical substance that causes a change in an organism's physiology or psychology when consumed. Drugs are typically distinguished from food and substances that provide nutritional support. Consumption of drugs can be via inhalat ...
and surgery
Surgery ''cheirourgikē'' (composed of χείρ, "hand", and ἔργον, "work"), via la, chirurgiae, meaning "hand work". is a medical specialty that uses operative manual and instrumental techniques on a person to investigate or treat a pat ...
. The drugs are thrombolytics
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive p ...
and fibrinolytic
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. Primary fibrinolysis is a normal body process, while secondary fibrinolysis is the breakdown of clots due to a medicine, a medical disorder, or some other c ...
s used in a process called thrombolysis
Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massive p ...
. Surgeries performed may be minimally-invasive
Minimally invasive procedures (also known as minimally invasive surgeries) encompass surgical techniques that limit the size of incisions needed, thereby reducing wound healing time, associated pain, and risk of infection. Surgery by definition ...
endovascular procedures such as a percutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(PCI), which involves coronary angioplasty
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
. The angioplasty uses the insertion of a balloon
A balloon is a flexible bag that can be inflated with a gas, such as helium, hydrogen, nitrous oxide, oxygen, and air. For special tasks, balloons can be filled with smoke, liquid water, granular media (e.g. sand, flour or rice), or light so ...
to open up the artery, with the possible additional use of one or more stent
In medicine, a stent is a metal or plastic tube inserted into the lumen of an anatomic vessel or duct to keep the passageway open, and stenting is the placement of a stent. A wide variety of stents are used for different purposes, from expandab ...
s. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.
If an MI is presented with ECG
Electrocardiography is the process of producing an electrocardiogram (ECG or EKG), a recording of the heart's electrical activity. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the hear ...
evidence of an ST elevation
ST elevation refers to a finding on an electrocardiogram wherein the trace in the ST segment is abnormally high above the baseline.
Electrophysiology
The ST segment starts from the J point (termination of QRS complex and the beginning of ST segm ...
known as STEMI
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may tr ...
, or if a bundle branch block
A bundle branch block is a defect in one the bundle branches in the electrical conduction system of the heart.
Anatomy and physiology
The heart's electrical activity begins in the sinoatrial node (the heart's natural pacemaker), which is situat ...
is similarly presented, then reperfusion therapy is necessary. In the absence of an ST elevation, a non-ST elevation MI, known as an NSTEMI
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may tra ...
, or an unstable angina
Unstable angina (UA), also called crescendo angina, is a type of angina pectoris that is irregular. It is also classified as a type of acute coronary syndrome (ACS).
It can be difficult to distinguish unstable angina from non-ST elevation (non-Q ...
may be presumed (both of these are indistinguishable on initial evaluation of symptoms). ST elevations indicate a completely blocked artery needing immediate reperfusion. In NSTEMI the blood flow is present but limited by stenosis
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
. In NSTEMI, thrombolytics must be avoided as there is no clear benefit of their use. If the condition stays stable a cardiac stress test
A cardiac stress test (also referred to as a cardiac diagnostic test, cardiopulmonary exercise test, or abbreviated CPX test) is a cardiological test that measures the heart's ability to respond to external stress in a controlled clinical environ ...
may be offered, and if needed subsequent revascularization
In medical and surgical therapy, revascularization is the restoration of perfusion to a body part or organ that has had ischemia. It is typically accomplished by surgical means. Vascular bypass and angioplasty are the two primary means of reva ...
will be carried out to restore a normal blood flow. If the blood flow becomes unstable an urgent angioplasty may be required. In these unstable cases the use of thrombolytics is contraindicated.
At least 10% of treated cases of STEMI do not develop necrosis
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated dige ...
of the heart muscle
Cardiac muscle (also called heart muscle, myocardium, cardiomyocytes and cardiac myocytes) is one of three types of vertebrate muscle tissues, with the other two being skeletal muscle and smooth muscle. It is an involuntary, striated muscle tha ...
. A successful restoration of blood flow is known as aborting the heart attack. About 25% of STEMIs can be aborted if treated within the hour of symptoms onset.
Thrombolytic therapy
Myocardial infarction
Thrombolytic therapy
Thrombolysis, also called fibrinolytic therapy, is the breakdown ( lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism (massiv ...
is indicated for the treatment of STEMI – if it can begin within 12 hours of the onset of symptoms, and the person is eligible based on exclusion criteria, and a coronary angioplasty
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
is not immediately available. Thrombolysis is most effective in the first 2 hours. After 12 hours, the risk of intracranial bleeding
Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds ( intraventricular bleeds and intraparenchymal bleeds), subarachnoid bleeds, epidural bleeds, and subdural bleeds. ...
associated with thrombolytic therapy outweighs any benefit. Because irreversible injury occurs within 2–4 hours of the infarction, there is a limited window of time available for reperfusion to work.
Thrombolytic drugs are contraindicated for the treatment of unstable angina and NSTEMI and for the treatment of individuals with evidence of cardiogenic shock
Cardiogenic shock (CS) is a medical emergency resulting from inadequate blood flow due to the dysfunction of the ventricles of the heart.Textbooks of Internal MedicinHarrison's Principles of Internal Medicine 16th Edition, The McGraw-Hill Compan ...
.
Although no perfect thrombolytic agent exists, ideally it would lead to rapid reperfusion, have a high sustained patency rate, be specific for recent thrombi, be easily and rapidly administered, create a low risk for intracerebral bleeding
Intracerebral hemorrhage (ICH), also known as cerebral bleed, intraparenchymal bleed, and hemorrhagic stroke, or haemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. It is one kind of bleed ...
and systemic bleeding, have no antigen
In immunology, an antigen (Ag) is a molecule or molecular structure or any foreign particulate matter or a pollen grain that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. ...
icity, adverse hemodynamic effects, or clinically significant drug interaction
Drug interactions occur when a drug's mechanism of action is disturbed by the concomitant administration of substances such as foods, beverages, or other drugs. The cause is often the inhibition of the specific receptors available to the drug, ...
s, and be cost effective
Cost-effectiveness analysis (CEA) is a form of economic analysis that compares the relative costs and outcomes (effects) of different courses of action. Cost-effectiveness analysis is distinct from cost–benefit analysis, which assigns a monetar ...
. Currently available thrombolytic agents include streptokinase
Streptokinase (SK) is a thrombolytic medication activating plasminogen by nonenzymatic mechanism. As a medication it is used to break down clots in some cases of myocardial infarction (heart attack), pulmonary embolism, and arterial thromboemboli ...
, urokinase
Urokinase, also known as urokinase-type plasminogen activator (uPA), is a serine protease present in humans and other animals. The human urokinase protein was discovered, but not named, by McFarlane and Pilling in 1947. Urokinase was originally i ...
, and alteplase
Alteplase (t-PA), a biosynthetic form of human tissue-type plasminogen activator (t-PA), is a thrombolytic medication, used to treat acute ischemic stroke, acute ST elevation myocardial infarction, ST-elevation myocardial infarction (a type of h ...
(recombinant tissue plasminogen activator
Tissue plasminogen activator (abbreviated tPA or PLAT) is a protein involved in the breakdown of blood clots. It is a serine protease () found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalyzes the conversion ...
, rtPA). More recently, thrombolytic agents similar in structure to rtPA such as reteplase
Reteplase, trade names include Retavase, is a thrombolytic drug, used to treat heart attacks by breaking up the clots that cause them.
Reteplase is a recombinant non-glycosylated form of human tissue plasminogen activator, which has been modifie ...
and tenecteplase
Tenecteplase, sold under the trade names TNKase, Metalyse and Elaxim, is an enzyme used as a thrombolytic drug.
Tenecteplase is a tissue plasminogen activator (tPA) produced by recombinant DNA technology using an established mammalian cell line ...
have been used. These newer agents boast efficacy at least as well as rtPA with significantly easier administration. The thrombolytic agent used in a particular individual is based on institution preference and the age of the patient.
Depending on the thrombolytic agent being used, additional anticoagulation
Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where the ...
with heparin
Heparin, also known as unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. Since heparins depend on the activity of antithrombin, they are considered anticoagulants. Specifically it is also used in the treatm ...
or low molecular weight heparin
Low-molecular-weight heparin (LMWH) is a class of anticoagulant medications. They are used in the prevention of blood clots and treatment of venous thromboembolism (deep vein thrombosis and pulmonary embolism) and in the treatment of myocardial in ...
may be of benefit. With tPa and related agents (reteplase and tenecteplase), heparin is needed to keep the coronary artery open. Because of the anticoagulant effect of fibrinogen depletion with streptokinase and urokinase treatment, it is less necessary there.
Failure
Thrombolytic therapy to abort a myocardial infarction is not always effective. The degree of effectiveness of a thrombolytic agent is dependent on the time since the myocardial infarction began, with the best results occurring if the thrombolytic is used within two hours of the onset of symptoms. Failure rates of thrombolytics can be as high as 50%. In cases of failure of the thrombolytic agent to open the infarct-related coronary artery, the person is then either treated conservatively with anticoagulants and allowed to "complete the infarction" orpercutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(and coronary angioplasty) is then performed. Percutaneous coronary intervention in this setting is known as "rescue PCI" or "salvage PCI". Complications, particularly bleeding, are significantly higher with rescue PCI than with primary PCI due to the action of the thrombolytic.
Side effects
Intracranial bleeding (ICB) and subsequentstroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
is a serious side effect
In medicine, a side effect is an effect, whether therapeutic or adverse, that is secondary to the one intended; although the term is predominantly employed to describe adverse effects, it can also apply to beneficial, but unintended, consequence ...
of thrombolytic use. The risk factor
In epidemiology, a risk factor or determinant is a variable associated with an increased risk of disease or infection.
Due to a lack of harmonization across disciplines, determinant, in its more widely accepted scientific meaning, is often use ...
s for developing intracranial bleeding include a previous episode of intracranial bleed, advanced age of the individual, and the thrombolytic regimen that is being used. In general, the risk of ICB due to thrombolytics is between 0.5 and 1 percent.
Coronary angioplasty
The benefit of prompt, primary angioplasty over thrombolytic therapy for acute STEMI is now well established. When performed rapidly, an angioplasty restores flow in the blocked artery in more than 95% of patients compared with the reperfusion rate of about 65% achieved by thrombolysis. Logistic and economic obstacles seem to hinder a more widespread application of angioplasty, although the feasibility of providing regionalized angioplasty for STEMI is currently being explored in the United States. The use of a coronary angioplasty to abort a myocardial infarction is preceded by a primarypercutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
. The goal of a prompt angioplasty is to open the artery as soon as possible, and preferably within 90 minutes of the patient presenting to the emergency room. This time is referred to as the door-to-balloon Door-to-balloon is a time measurement in emergency cardiac care (ECC), specifically in the treatment of ST segment elevation myocardial infarction (or STEMI). The interval starts with the patient's arrival in the emergency department, and ends whe ...
time. Few hospitals can provide an angioplasty within the 90 minute interval, which prompted the American College of Cardiology (ACC) to launch a national Door to Balloon (D2B) Initiative in November 2006. Over 800 hospitals have joined the D2B Alliance as of March 16, 2007.
One particularly successful implementation of a primary PCI protocol is in the Calgary Health Region under the auspices of the Libin Cardiovascular Institute of Alberta
The 'Libin Cardiovascular Institute'' is an entity of Alberta Health Services and the University of Calgary. It connects all cardiovascular research, education and clinical care in Southern Alberta. The Institute coordinates the activities of o ...
. Under this model, EMS teams responding to an emergency can transmit the ECG directly to a digital archiving system that allows emergency room staff to immediately confirm the diagnosis. This in turn allows for redirection of the EMS teams to those facilities that are ready to conduct time-critical angioplasty. This protocol has resulted in a median time to treatment of 62 minutes.
The current guidelines in the United States restrict angioplasties to hospitals with available emergency bypass surgery as a backup, but this is not the case in other parts of the world.
A PCI involves performing a coronary angiogram to determine the location of the infarcting vessel, followed by balloon angioplasty
Angioplasty, is also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclero ...
(and frequently deployment of an intracoronary stent) of the stenosed arterial segment. In some settings, an extraction catheter may be used to attempt to aspirate (remove) the thrombus prior to balloon angioplasty. While the use of intracoronary stent
In medicine, a stent is a metal or plastic tube inserted into the lumen of an anatomic vessel or duct to keep the passageway open, and stenting is the placement of a stent. A wide variety of stents are used for different purposes, from expandab ...
s do not improve the short term outcomes in primary PCI, the use of stents is widespread because of the decreased rates of procedures to treat restenosis compared to balloon angioplasty.
Adjuvant therapy
Adjuvant therapy, also known as adjunct therapy, adjuvant care, or augmentation therapy, is a therapy that is given in addition to the primary or initial therapy to maximize its effectiveness. The surgeries and complex treatment regimens used in ...
during an angioplasty includes intravenous heparin
Heparin, also known as unfractionated heparin (UFH), is a medication and naturally occurring glycosaminoglycan. Since heparins depend on the activity of antithrombin, they are considered anticoagulants. Specifically it is also used in the treatm ...
, aspirin, and clopidogrel
Clopidogrel — sold under the brand name Plavix, among others — is an antiplatelet medication used to reduce the risk of heart disease and stroke in those at high risk. It is also used together with aspirin in heart attacks and following t ...
. Glycoprotein IIb/IIIa inhibitors are often used in the setting of primary angioplasty to reduce the risk of ischemic complications during the procedure. Due to the number of antiplatelet agents and anticoagulants used during primary angioplasty, the risk of bleeding associated with the procedure is higher than during an elective procedure.
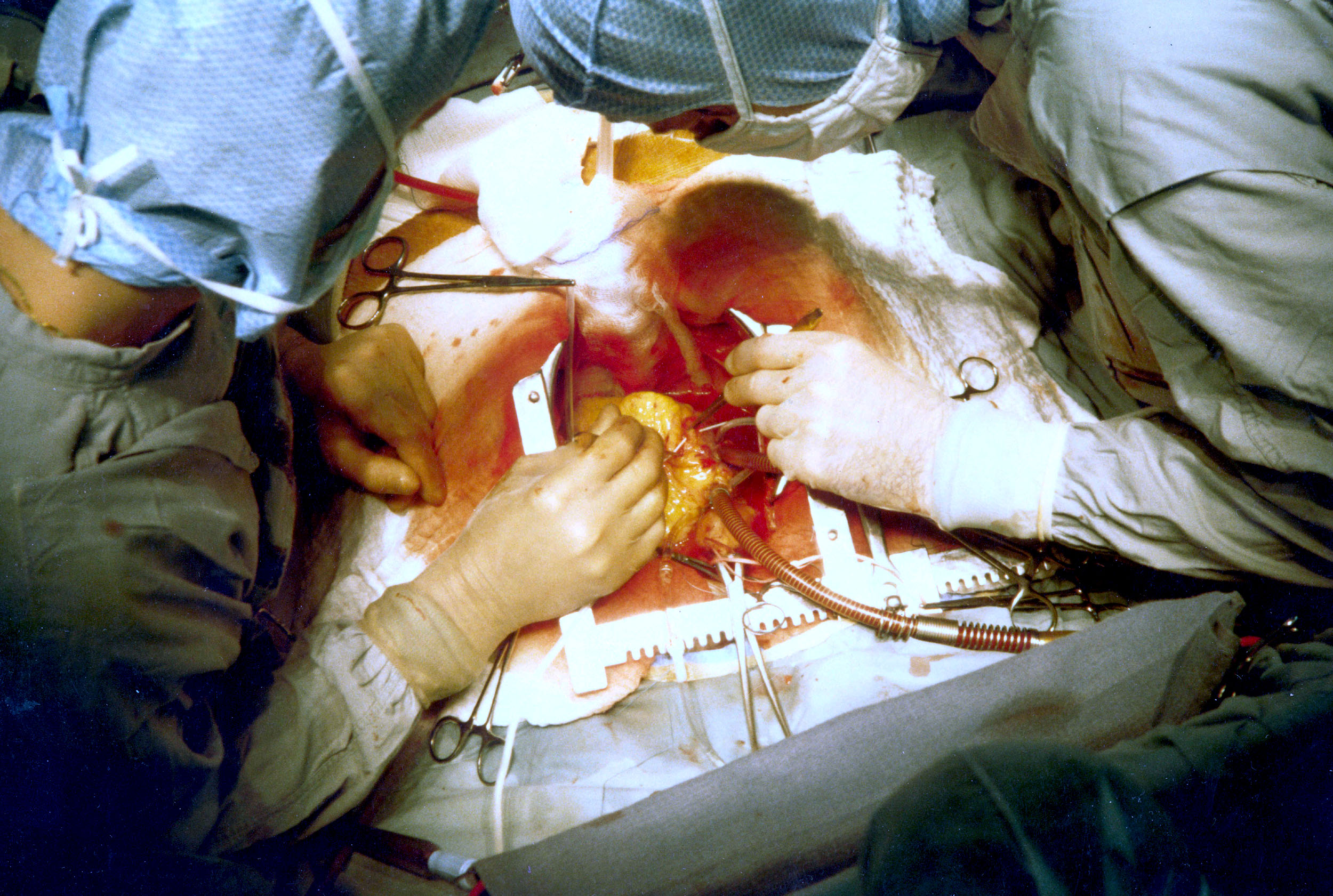
Coronary artery bypass surgery
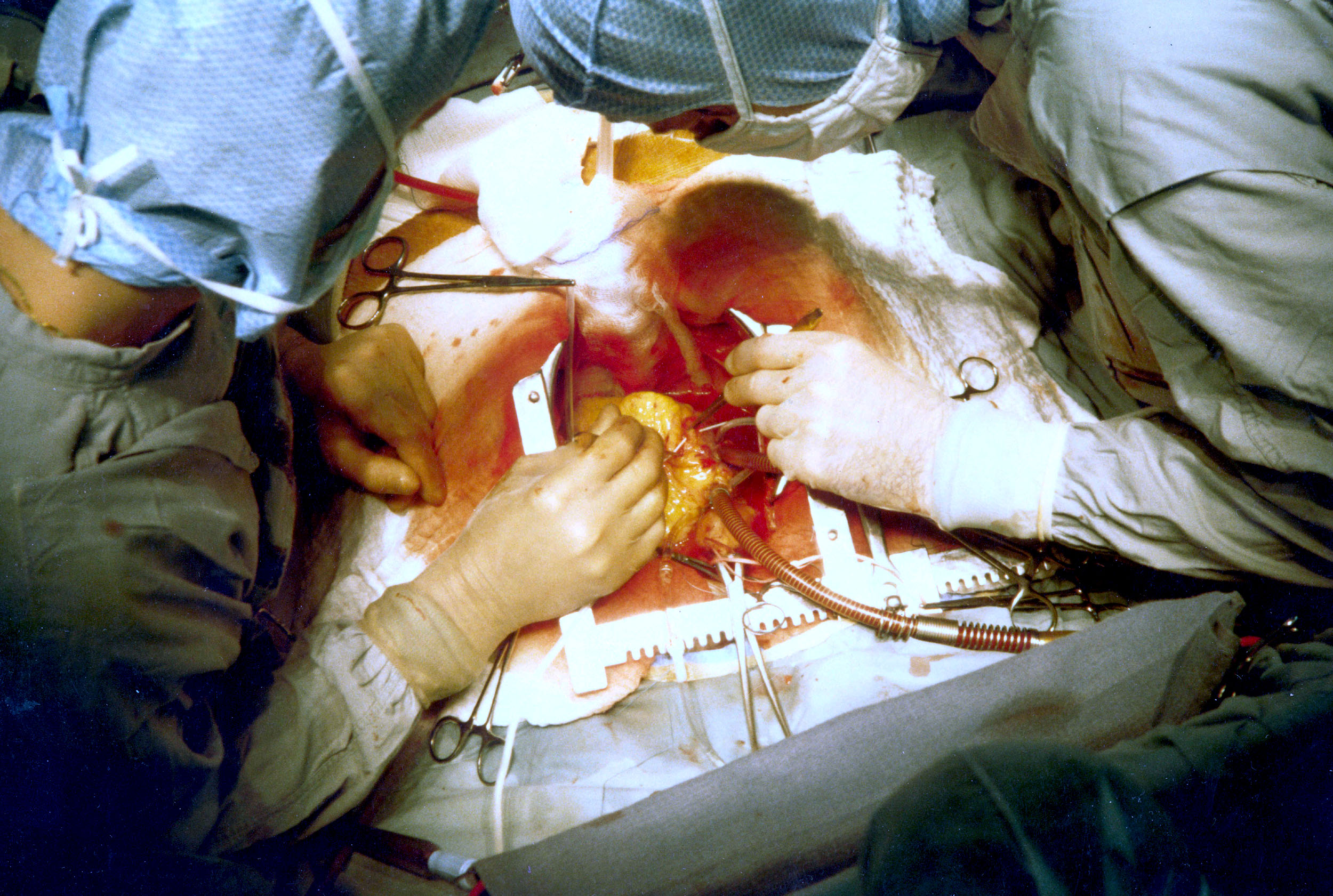 Emergency bypass surgery for the treatment of an acute myocardial infarction (MI) is less common than PCI or thrombolysis. From 1995 to 2004, the percentage of people with
Emergency bypass surgery for the treatment of an acute myocardial infarction (MI) is less common than PCI or thrombolysis. From 1995 to 2004, the percentage of people with cardiogenic shock
Cardiogenic shock (CS) is a medical emergency resulting from inadequate blood flow due to the dysfunction of the ventricles of the heart.Textbooks of Internal MedicinHarrison's Principles of Internal Medicine 16th Edition, The McGraw-Hill Compan ...
treated with primary PCI rose from 27.4% to 54.4%, while the increase in coronary artery bypass graft surgery (CABG) was only from 2.1% to 3.2%. Emergency CABG is usually undertaken to simultaneously treat a mechanical complication, such as a ruptured papillary muscle, or a ventricular septal defect, with ensuing cardiogenic shock. In uncomplicated MI, the mortality rate can be high when the surgery is performed immediately following the infarction. If this option is entertained, the patient should be stabilized prior to surgery, with supportive interventions such as the use of an intra-aortic balloon pump
The intra-aortic balloon pump (IABP) is a mechanical device that increases myocardial oxygen perfusion and indirectly increases cardiac output through afterload reduction. It consists of a cylindrical polyurethane balloon that sits in the aorta, ...
. In patients developing cardiogenic shock after a myocardial infarction, both PCI and CABG are satisfactory treatment options, with similar survival rates.
Coronary artery bypass surgery involves an artery or vein from the patient being implanted to bypass narrowings or occlusions in the coronary arteries. Several arteries and veins can be used, however internal mammary artery
In human anatomy, the internal thoracic artery (ITA), previously commonly known as the internal mammary artery (a name still common among surgeons), is an artery that supplies the anterior chest wall and the breasts. It is a paired artery, with one ...
grafts have demonstrated significantly better long-term patency rates than great saphenous vein
The great saphenous vein (GSV, alternately "long saphenous vein"; ) is a large, subcutaneous, superficial vein of the leg. It is the longest vein in the body, running along the length of the lower limb, returning blood from the foot, leg and thig ...
grafts. In patients with two or more coronary arteries affected, bypass surgery is associated with higher long-term survival rate
Survival rate is a part of survival analysis. It is the proportion of people in a study or treatment group still alive at a given period of time after diagnosis. It is a method of describing prognosis in certain disease conditions, and can be use ...
s compared to percutaneous interventions. In patients with single vessel disease, surgery is comparably safe and effective, and may be a treatment option in selected cases. Bypass surgery has higher costs initially, but becomes cost-effective in the long term. A surgical bypass graft is more invasive
Invasive may refer to:
*Invasive (medical) procedure
*Invasive species
*Invasive observation, especially in reference to surveillance
*Invasively progressive spread of disease from one organ in the body to another, especially in reference to cancer ...
initially but bears less risk of recurrent procedures (but these may be again minimally invasive).
Reperfusion arrhythmia
Accelerated idioventricular rhythm
Accelerated idioventricular rhythm is a ventricular rhythm with a rate of between 40 and 120 beats per minute. Idioventricular means “relating to or affecting the cardiac ventricle alone” and refers to any ectopic ventricular arrhythmia. Accel ...
which looks like slow ventricular tachycardia is a sign of a successful reperfusion. No treatment of this rhythm is needed as it rarely changes into a more serious rhythm.
See also
*Perfusion scanning
Perfusion is the passage of fluid through the lymphatic system or blood vessels to an organ or a tissue. The practice of perfusion scanning is the process by which this perfusion can be observed, recorded and quantified. The term perfusion scannin ...
* Reperfusion injury
* Revascularization
* TIMI
The Thrombolysis In Myocardial Infarction, or TIMI Study Group, is an Academic Research Organization (ARO) affiliated with Brigham and Women's Hospital and Harvard Medical School dedicated to advancing the knowledge and care of patients with car ...
* Ischemia-reperfusion injury of the appendicular musculoskeletal system Ischemia-reperfusion (IR) tissue injury is the resultant pathology from a combination of factors, including tissue hypoxia, followed by tissue damage associated with re-oxygenation. IR injury contributes to disease and mortality in a variety of pa ...
References
{{Reflist, 32em Cardiac procedures