Periodontal Disease on:
[Wikipedia]
[Google]
[Amazon]
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen and red and may bleed. It is considered the main cause of tooth loss for adults worldwide.V. Baelum and R. Lopez, “Periodontal epidemiology: towards
social science or molecular biology?,”Community Dentistry
and Oral Epidemiology, vol. 32, no. 4, pp. 239–249, 2004.Nicchio I, Cirelli T, Nepomuceno R, et al. Polymorphisms in Genes of Lipid Metabolism Are Associated with Type 2 Diabetes Mellitus and Periodontitis, as Comorbidities, and with the Subjects' Periodontal, Glycemic, and Lipid Profiles Journal of Diabetes Research. 2021 Jan;2021. PMCID: PMC8601849. In its more serious form, called periodontitis, the gums can pull away from the

 The primary cause of gingivitis is poor or ineffective
The primary cause of gingivitis is poor or ineffective 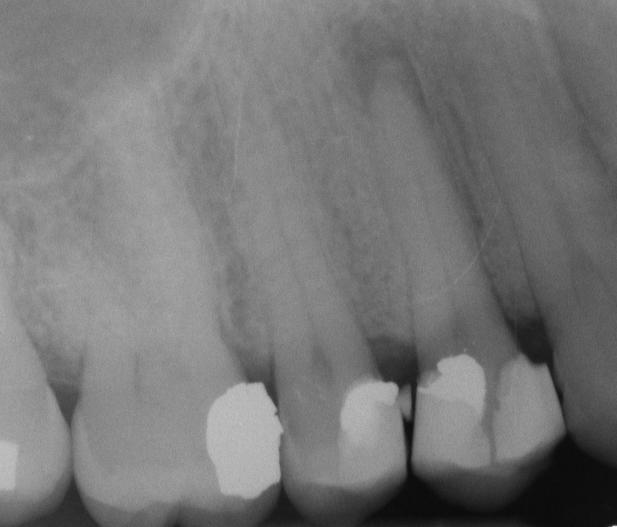
 There were several attempts to introduce an agreed-upon classification system for periodontal diseases: in 1989, 1993, 1999, and 2017.
There were several attempts to introduce an agreed-upon classification system for periodontal diseases: in 1989, 1993, 1999, and 2017.
 The cornerstone of successful periodontal treatment starts with establishing excellent
The cornerstone of successful periodontal treatment starts with establishing excellent
 Periodontitis is very common, and is widely regarded as the second most common dental disease worldwide, after dental decay, and in the United States has a
Periodontitis is very common, and is widely regarded as the second most common dental disease worldwide, after dental decay, and in the United States has a
Canadian Academy of Periodontology — What is periodontitis?
Periodontal disease and braces
Orthodontics Australia. {{Authority control Inflammations Periodontal disorders Wikipedia medicine articles ready to translate
tooth
A tooth ( : teeth) is a hard, calcified structure found in the jaws (or mouths) of many vertebrates and used to break down food. Some animals, particularly carnivores and omnivores, also use teeth to help with capturing or wounding prey, t ...
, bone can be lost, and the teeth may loosen or fall out. Bad breath may also occur.
Periodontal disease is generally due to bacteria in the mouth infecting the tissue around the teeth. Factors that increase the risk of disease include smoking
Smoking is a practice in which a substance is burned and the resulting smoke is typically breathed in to be tasted and absorbed into the bloodstream. Most commonly, the substance used is the dried leaves of the tobacco plant, which have bee ...
, diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
, HIV/AIDS
Human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), a retrovirus. Following initial infection an individual ...
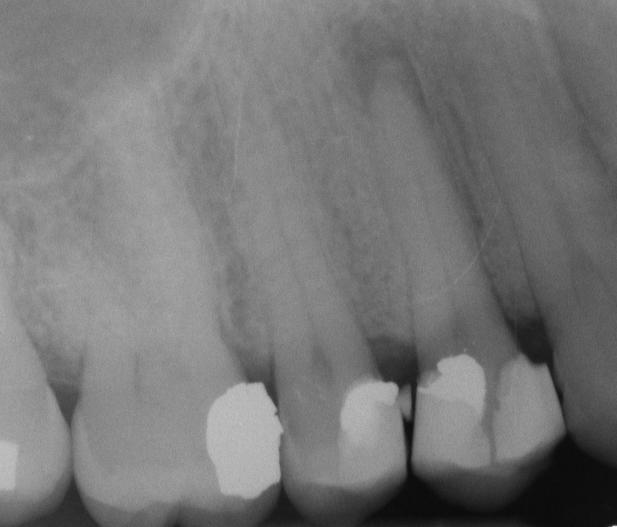
, family history, and certain medications. Diagnosis is by inspecting the gum tissue around the teeth both visually and with a probe and X-ray
X-rays (or rarely, ''X-radiation'') are a form of high-energy electromagnetic radiation. In many languages, it is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it in 1895 and named it ' ...
s looking for bone loss around the teeth.
Treatment involves good oral hygiene
Oral hygiene is the practice of keeping one's mouth clean and free of disease and other problems (e.g. bad breath) by regular brushing of the teeth (dental hygiene) and cleaning between the teeth. It is important that oral hygiene be carried out ...
and regular professional teeth cleaning. Recommended oral hygiene include daily brushing and flossing
Dental floss is a cord of thin filaments used in interdental cleaning to remove food and dental plaque from between teeth or places a toothbrush has difficulty reaching or is unable to reach. Its regular use as part of oral cleaning is designed ...
. In certain cases antibiotics
An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention ...
or dental surgery may be recommended. Clinical investigations demonstrate that quitting smoking and making dietary changes enhance periodontal health. Globally 538 million people were estimated to be affected in 2015 and has been known to affect 10-15% of the population generally. In the United States nearly half of those over the age of 30 are affected to some degree, and about 70% of those over 65 have the condition. Males are affected more often than females.
Signs and symptoms
In the early stages, periodontitis has very few symptoms, and in many individuals the disease has progressed significantly before they seek treatment. Symptoms may include: * Redness or bleeding of gums while brushingteeth
A tooth ( : teeth) is a hard, calcified structure found in the jaws (or mouths) of many vertebrates and used to break down food. Some animals, particularly carnivores and omnivores, also use teeth to help with capturing or wounding prey, te ...
, using dental floss or biting into hard food (e.g., apples) (though this may also occur in gingivitis, where there is no attachment loss gum disease )
* Gum swelling that recurs
* Spitting out blood after brushing teeth
* Halitosis, or bad breath, and a persistent metallic taste in the mouth
* Gingival recession, resulting in apparent lengthening of teeth (this may also be caused by heavy-handed brushing or with a stiff toothbrush)
* Deep pockets between the teeth and the gums ( pockets are sites where the attachment has been gradually destroyed by collagen-destroying enzymes, known as collagenases
Collagenases are enzymes that break the peptide bonds in collagen. They assist in destroying extracellular structures in the pathogenesis of bacteria such as ''Clostridium''. They are considered a virulence factor, facilitating the spread of ga ...
)
* Loose teeth, in the later stages (though this may occur for other reasons, as well)
Gingival inflammation and bone destruction are largely painless. Hence, people may wrongly assume painless bleeding after teeth cleaning is insignificant, although this may be a symptom of progressing periodontitis in that person.

Associated conditions
Periodontitis has been linked to increasedinflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
in the body, such as indicated by raised levels of C-reactive protein
C-reactive protein (CRP) is an annular (ring-shaped) pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin ...
and interleukin-6
Interleukin 6 (IL-6) is an interleukin that acts as both a pro-inflammatory cytokine and an anti-inflammatory myokine. In humans, it is encoded by the ''IL6'' gene.
In addition, osteoblasts secrete IL-6 to stimulate osteoclast formation. Sm ...
. It is associated with an increased risk of stroke, myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which ...
, atherosclerosis
Atherosclerosis is a pattern of the disease arteriosclerosis in which the wall of the artery develops abnormalities, called lesions. These lesions may lead to narrowing due to the buildup of atheromatous plaque. At onset there are usually ...
and hypertension. It also linked in those over 60 years of age to impairments in delayed memory and calculation abilities. Individuals with impaired fasting glucose and diabetes mellitus
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
have higher degrees of periodontal inflammation, and often have difficulties with balancing their blood glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, usi ...
level owing to the constant systemic inflammatory state, caused by the periodontal inflammation. Although no causal association was proven, there is an association between chronic periodontitis and erectile dysfunction
Erectile dysfunction (ED), also called impotence, is the type of sexual dysfunction in which the penis fails to become or stay erect during sexual activity. It is the most common sexual problem in men.Cunningham GR, Rosen RC. Overview of ma ...
, inflammatory bowel disease
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, Crohn's disease and ulcerative colitis being the principal types. Crohn's disease affects the small intestine and large intestine, as wel ...
, heart disease, and pancreatic cancer.
Diabetes and periodontal disease
A positive correlation between raised levels of glucose within the blood and the onset or progression of periodontal disease has been shown in the current literature. Data has also shown that there is a significant increase in the incidence or progression of periodontitis in patients with uncontrolled diabetes compared to those who do not have diabetes or have well-controlled diabetes. In uncontrolled diabetes, the formation ofreactive oxygen species
In chemistry, reactive oxygen species (ROS) are highly reactive chemicals formed from diatomic oxygen (). Examples of ROS include peroxides, superoxide, hydroxyl radical, singlet oxygen, and alpha-oxygen.
The reduction of molecular oxygen ...
can damage cells such as those in the connective tissue of the periodontal ligament, resulting in cell necrosis
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated dig ...
or apoptosis. Furthermore, individuals with uncontrolled diabetes mellitus who have frequent exposure to periodontal pathogens have a greater immune response to these bacteria. This can subsequently cause and/or accelerate periodontal tissue destruction leading to periodontal disease.
Oral cancer and periodontal disease
Current literature suggests a link between periodontal disease and oral cancer. Studies have confirmed an increase in systemic inflammation markers such as C-Reactive Protein and Interleukin-6 to be found in patients with advanced periodontal disease. The link between systemic inflammation and oral cancer has also been well established.
Both periodontal disease and cancer risk are associated with genetic susceptibility and it is possible that there is a positive association by a shared genetic susceptibility in the two diseases.
Due to the low incidence rate of oral cancer, studies have not been able to conduct quality studies to prove the association between the two, however future larger studies may aid in the identification of individuals at a higher risk.
Systemic implications
Periodontal disease (PD) can be described as an inflammatory condition affecting the supporting structures of the teeth. Studies have shown that PD is associated with higher levels of systemic inflammatory markers such as Interleukin-6 (IL-6), C-Reactive Protein (CRP) and Tumor Necrosis Factor (TNF). To compare, elevated levels of these inflammatory markers are also associated with cardiovascular disease and cerebrovascular events such as ischemic strokes.
The presence of a wide spectrum inflammatory oral diseases can increase the risk of an episode of stroke in an acute or chronic phase. Inflammatory markers, CRP, IL-6 are known risk factors of stroke. Both inflammatory markers are also biomarkers of PD and found to be an increased level after daily activities, such as mastication or toothbrushing, are performed. Bacteria from the periodontal pockets will enter the bloodstream during these activities and the current literature suggests that this may be a possible triggering of the aggravation of the stroke process.
Other mechanisms have been suggested, PD is a known chronic infection. It can aid in the promotion of atherosclerosis by the deposition of cholesterol, cholesterol esters and calcium within the subendothelial layer of vessel walls. Atherosclerotic plaque that is unstable may rupture and release debris and thrombi that may travel to different parts of the circulatory system causing embolization and therefore, an ischemic stroke. Therefore, PD has been suggested as an independent risk factor for stroke.
A variety of cardiovascular diseases can also be associated with periodontal disease. Patients with higher levels of inflammatory markers such as TNF, IL-1, IL-6 and IL-8 can lead to progression of atherosclerosis and the development and perpetuation of atrial fibrillation, as it is associated with platelet and coagulation cascade activations, leading to thrombosis and thrombotic complications.
Experimental animal studies have shown a link between periodontal disease, oxidative stress and cardiac stress. Oxidative stress favours the development and progression of heart failure as it causes cellular dysfunction, oxidation of proteins and lipids, and damage to the deoxyribonucleic acid (DNA), stimulating fibroblast proliferation and metalloproteinases activation favouring cardiac remodelling.
During SARS Covid 19 pandemic, Periodontitis was significantly associated with a higher risk of complications from COVID‐19, including ICU admission, need for assisted ventilation and death and increased blood levels of markers such as D‐dimer, WBC and CRP which are linked with worse disease outcome.
Clinical significance
Inadequate nutrition and periodontal disease
Periodontal disease is multifactorial, and nutrition can significantly affect its prognosis. Studies have shown that a healthy and well-balanced diet is crucial to maintaining periodontal health. Nutritional deficiencies can lead to oral manifestations such as those in scurvy and rickets disease. Different vitamins will play a different role in periodontal health: * Vitamin C: Deficiencies may lead to gingival inflammation and bleeding, subsequently advancing periodontal disease * Vitamin D: Deficiencies may lead to delayed post-surgical healing * Vitamin E: Deficiencies may lead to impaired gingival wound healing * Vitamin K: Deficiencies may lead to gingival bleeding Nutritional supplements of vitamins have also been shown to positively affect healing after periodontal surgery and many of these vitamins can be found in a variety of food that we eat within a regular healthy diet. Therefore, vitamin intakes (particularly vitamin C) and dietary supplements not only play a role in improving periodontal health, but also influence the rate of bone formation and periodontal regeneration. However, studies supporting the correlation between nutrition and periodontal health are limited, and more long-term research is required to confirm this.Causes
Periodontitis is an inflammation of the periodontium, i.e., the tissues that support the teeth. The periodontium consists of four tissues: *gingiva
The gums or gingiva (plural: ''gingivae'') consist of the mucosal tissue that lies over the mandible and maxilla inside the mouth. Gum health and disease can have an effect on general health.
Structure
The gums are part of the soft tissue l ...
, or gum tissue,
* cementum
Cementum is a specialized calcified substance covering the root of a tooth. The cementum is the part of the periodontium that attaches the teeth to the alveolar bone by anchoring the periodontal ligament.Illustrated Dental Embryology, Histology, ...
, or outer layer of the roots of teeth,
* alveolar bone
The alveolar process () or alveolar bone is the thickened ridge of bone that contains the tooth sockets on the jaw bones (in humans, the maxilla and the mandible). The structures are covered by gums as part of the oral cavity.
The synonymous te ...
, or the bony sockets into which the teeth are anchored, and
* periodontal ligament
The periodontal ligament, commonly abbreviated as the PDL, is a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which it sits. It inserts into root cementum one side and onto alveolar ...
s (PDLs), which are the connective tissue
Connective tissue is one of the four primary types of animal tissue, along with epithelial tissue, muscle tissue, and nervous tissue. It develops from the mesenchyme derived from the mesoderm the middle embryonic germ layer. Connective tissue ...
fibers that run between the cementum and the alveolar bone.
oral hygiene
Oral hygiene is the practice of keeping one's mouth clean and free of disease and other problems (e.g. bad breath) by regular brushing of the teeth (dental hygiene) and cleaning between the teeth. It is important that oral hygiene be carried out ...
, which leads to the accumulation of a mycotic and bacterial matrix at the gum line, called dental plaque
Dental plaque is a biofilm of microorganisms (mostly bacteria, but also fungi) that grows on surfaces within the mouth. It is a sticky colorless deposit at first, but when it forms tartar, it is often brown or pale yellow. It is commonly found be ...
. Other contributors are poor nutrition and underlying medical issues such as diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level (hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ...
. Diabetics must be meticulous with their homecare to control periodontal disease. New finger prick tests have been approved by the Food and Drug Administration
The United States Food and Drug Administration (FDA or US FDA) is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food ...
in the US, and are being used in dental offices to identify and screen people for possible contributory causes of gum disease, such as diabetes.
In some people, gingivitis progresses to periodontitis – with the destruction of the gingival fibers, the gum tissues separate from the tooth and deepened sulcus, called a periodontal pocket. Subgingival microorganisms (those that exist under the gum line) colonize the periodontal pockets and cause further inflammation in the gum tissues and progressive bone loss. Examples of secondary causes are those things that, by definition, cause microbic plaque accumulation, such as restoration overhangs and root proximity.
Smoking
Smoking is a practice in which a substance is burned and the resulting smoke is typically breathed in to be tasted and absorbed into the bloodstream. Most commonly, the substance used is the dried leaves of the tobacco plant, which have bee ...
is another factor that increases the occurrence of periodontitis, directly or indirectly, and may interfere with or adversely affect its treatment. It is arguably the most important environmental risk factor for periodontitis. Research has shown that smokers have more bone loss, attachment loss and tooth loss compared to non-smokers. This is likely due to several effects of smoking on the immune response including decreased wound healing, suppression of antibody
An antibody (Ab), also known as an immunoglobulin (Ig), is a large, Y-shaped protein used by the immune system to identify and neutralize foreign objects such as pathogenic bacteria and Viral disease, viruses. The antibody recognizes a unique m ...
production, and the reduction of phagocytosis
Phagocytosis () is the process by which a cell uses its plasma membrane to engulf a large particle (≥ 0.5 μm), giving rise to an internal compartment called the phagosome. It is one type of endocytosis. A cell that performs phagocytosis i ...
by neutrophil
Neutrophils (also known as neutrocytes or heterophils) are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying in ...
s
Ehlers–Danlos syndrome and Papillon–Lefèvre syndrome (also known as palmoplantar keratoderma) are also risk factors for periodontitis.
If left undisturbed, microbial plaque calcifies to form calculus
Calculus, originally called infinitesimal calculus or "the calculus of infinitesimals", is the mathematics, mathematical study of continuous change, in the same way that geometry is the study of shape, and algebra is the study of generalizati ...
, which is commonly called tartar. Calculus above and below the gum line must be removed completely by the dental hygienist or dentist to treat gingivitis and periodontitis. Although the primary cause of both gingivitis and periodontitis is the microbial plaque that adheres to the tooth surfaces, there are many other modifying factors. A very strong risk factor is one's genetic susceptibility. Several conditions and diseases, including Down syndrome
Down syndrome or Down's syndrome, also known as trisomy 21, is a genetic disorder caused by the presence of all or part of a third copy of chromosome 21. It is usually associated with child development, physical growth delays, mild to moderate ...
, diabetes, and other diseases that affect one's resistance to infection, also increase susceptibility to periodontitis.
Periodontitis may be associated with higher stress. Periodontitis occurs more often in people from the lower end of the socioeconomic scale than people from the upper end of the socioeconomic scale.
Genetics
Genetics is the study of genes, genetic variation, and heredity in organisms.Hartl D, Jones E (2005) It is an important branch in biology because heredity is vital to organisms' evolution. Gregor Mendel, a Moravian Augustinian friar worki ...
appear to play a role in determining the risk for periodontitis. It is believed genetics could explain why some people with good plaque control have advanced periodontitis, whilst some others with poor oral hygiene are free from the disease. Genetic factors which could modify the risk of a person developing periodontitis include:
* Defects of phagocytosis
Phagocytosis () is the process by which a cell uses its plasma membrane to engulf a large particle (≥ 0.5 μm), giving rise to an internal compartment called the phagosome. It is one type of endocytosis. A cell that performs phagocytosis i ...
: person may have hypo-responsive phagocyte
Phagocytes are cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or dying cells. Their name comes from the Greek ', "to eat" or "devour", and "-cyte", the suffix in biology denoting "cell", from the Greek ...
s.
* Hyper-production of interleukin
Interleukins (ILs) are a group of cytokines (secreted proteins and signal molecules) that are expressed and secreted by white blood cells (leukocytes) as well as some other body cells. The human genome encodes more than 50 interleukins and rela ...
s, prostaglandin
The prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids having diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are der ...
s and cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in a ...
s, resulting in an exaggerated immune response
An immune response is a reaction which occurs within an organism for the purpose of defending against foreign invaders. These invaders include a wide variety of different microorganisms including viruses, bacteria, parasites, and fungi which could ...
.
* Interleukin 1
The Interleukin-1 family (IL-1 family) is a group of 11 cytokines that plays a central role in the regulation of immune and inflammatory responses to infections or sterile insults.
Discovery
Discovery of these cytokines began with studies on ...
(IL-1) gene polymorphism: people with this polymorphism produce more IL-1, and subsequently are more at risk of developing chronic periodontitis.
Diabetes appears to exacerbate the onset, progression, and severity of periodontitis. Although the majority of research has focused on type 2 diabetes
Type 2 diabetes, formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urinati ...
, type 1 diabetes
Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when cells that make insulin (beta cells) are destroyed by the immune system. Insulin is a hormone required for the cells to use blood sugar f ...
appears to have an identical effect on the risk for periodontitis. The extent of the increased risk of periodontitis is dependent on the level of glycaemic control. Therefore, in well managed diabetes there seems to be a small effect of diabetes on the risk for periodontitis. However, the risk increases exponentially as glycaemic control worsens. Overall, the increased risk of periodontitis in diabetics is estimated to be between two and three times higher. So far, the mechanisms underlying the link are not fully understood, but it is known to involve aspects of inflammation, immune functioning, neutrophil activity, and cytokine biology.
Mechanism
As dental plaque or biofilm accumulates on the teeth near and below the gums there is somedysbiosis
Dysbiosis (also called dysbacteriosis) is characterized by a disruption to the microbiome resulting in an imbalance in the microbiota, changes in their functional composition and metabolic activities, or a shift in their local distribution. For ex ...
of the normal oral microbiome. As of 2017 it was not certain what species were most responsible for causing harm, but gram-negative
Gram-negative bacteria are bacteria that do not retain the crystal violet stain used in the Gram staining method of bacterial differentiation. They are characterized by their cell envelopes, which are composed of a thin peptidoglycan cell wa ...
anaerobic bacteria, spirochetes, and viruses have been suggested; in individual people it is sometimes clear that one or more species is driving the disease. Research in 2004 indicated three gram negative anaerobic species: ''Aggregatibacter actinomycetemcomitans
''Aggregatibacter actinomycetemcomitans'' is a Gram-negative, facultative anaerobe, nonmotile bacterium that is often found in association with localized aggressive periodontitis, a severe infection of the periodontium. It is also suspected to b ...
'', '' Porphyromonas gingivalis'', ''Bacteroides forsythus
''Tannerella forsythia'' is an anaerobic, Gram-negative bacterial species of the Bacteroidota phylum. It has been implicated in periodontal diseases and is a member of the red complex of periodontal pathogens. ''T. forsythia'' was previously n ...
'' and '' Eikenella corrodens''.
Plaque may be soft and uncalcified, hard and calcified, or both; for plaques that are on teeth the calcium comes from saliva; for plaques below the gumline, it comes from blood via oozing of inflamed gums.
The damage to teeth and gums comes from the immune system as it attempts to destroy the microbes that are disrupting the normal symbiosis between the oral tissues and the oral microbe community. As in other tissues, Langerhans cells in the epithelium take up antigens from the microbes, and present them to the immune system, leading to movement of white blood cell
White blood cells, also called leukocytes or leucocytes, are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from mult ...
s into the affected tissues. This process in turn activates osteoclasts which begin to destroy bone, and it activates matrix metalloproteinases that destroy ligaments. So, in summary, it is bacteria which initiates the disease, but key destructive events are brought about by the exaggerated response from the host's immune system.
Classification
 There were several attempts to introduce an agreed-upon classification system for periodontal diseases: in 1989, 1993, 1999, and 2017.
There were several attempts to introduce an agreed-upon classification system for periodontal diseases: in 1989, 1993, 1999, and 2017.
1999 classification
The 1999 classification system for periodontal diseases and conditions listed seven major categories of periodontal diseases, of which 2–6 are termed ''destructive'' periodontal disease, because the damage is essentially irreversible. The seven categories are as follows: * Gingivitis * Chronic periodontitis *Aggressive periodontitis Aggressive periodontitis describes a type of periodontal disease and includes two of the seven classifications of periodontitis as defined by the 1999 classification system:
# Localized aggressive periodontitis (LAP)
# Generalized aggressive periodo ...
* Periodontitis as a manifestation of systemic disease Periodontitis as a manifestation of systemic diseases is one of the seven categories of periodontitis as defined by the American Academy of Periodontology 1999 classification system and is one of the three classifications of periodontal diseases an ...
* Necrotizing ulcerative gingivitis/periodontitis
* Abscesses of the periodontium
* Combined periodontic-endodontic lesions
Moreover, terminology expressing both the extent and severity of periodontal diseases are appended to the terms above to denote the specific diagnosis of a particular person or group of people.
Severity
The "severity" of disease refers to the amount ofperiodontal ligament
The periodontal ligament, commonly abbreviated as the PDL, is a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which it sits. It inserts into root cementum one side and onto alveolar ...
fibers that have been lost, termed "clinical attachment loss". According to the 1999 classification, the severity of chronic periodontitis is graded as follows:
* Slight: of attachment loss
* Moderate: of attachment loss
* Severe: ≥ of attachment loss
Extent
The "extent" of disease refers to the proportion of the dentition affected by the disease in terms of percentage of sites. Sites are defined as the positions at which probing measurements are taken around each tooth and, generally, six probing sites around each tooth are recorded, as follows: * Mesiobuccal * Mid-buccal * Distobuccal * Mesiolingual * Mid-lingual * Distolingual If up to 30% of sites in the mouth are affected, the manifestation is classified as "localized"; for more than 30%, the term "generalized" is used.2017 classification
The 2017 classification of periodontal diseases is as follows: Periodontal health, gingival disease and conditions * Periodontal health and gingival health ** Clinical gingival health on an intact periodontium ** Clinical gingival health on an intact periodontium *** Stable periodontitis *** Non periodontitis person * Gingivitis - Dentalbiofilm
A biofilm comprises any syntrophic consortium of microorganisms in which cells stick to each other and often also to a surface. These adherent cells become embedded within a slimy extracellular matrix that is composed of extracellular ...
induced
**Associated with the dental biofilm alone
**Mediated by systemic and local risk factors
**Drug induced gingival enlargement.
* Gingival diseases - Non dental biofilm
A biofilm comprises any syntrophic consortium of microorganisms in which cells stick to each other and often also to a surface. These adherent cells become embedded within a slimy extracellular matrix that is composed of extracellular ...
induced
**Genetic/developmental disorders
**Specific infections
**Inflammatory and immune conditions
**Reactive processes
**Neoplasms
**Endocrine, nutritional and metabolic
**Traumatic lesions
**Gingival pigmentation.
Periodontitis
* Necrotizing periodontal diseases
** Necrotizing Gingivitis
**Necrotizing periodontitis
**Necrotizing stomatitis
* Periodontitis as a manifestation of systemic disease Periodontitis as a manifestation of systemic diseases is one of the seven categories of periodontitis as defined by the American Academy of Periodontology 1999 classification system and is one of the three classifications of periodontal diseases an ...
* Periodontitis
Other conditions affecting the periodontium
(Periodontal Manifestations of Systemic Diseases and Developmental and Acquired Conditions)
* Systemic disease of conditions affecting the periodontal support tissues
* Other Periodontal Conditions
** Periodontal abscesses
** Endodontic- periodontal lesion
A lesion is any damage or abnormal change in the tissue of an organism, usually caused by disease or trauma. ''Lesion'' is derived from the Latin "injury". Lesions may occur in plants as well as animals.
Types
There is no designated classif ...
s
* Mucogingival deformities and conditions
**Gingival Phenotype
**Gingival/Soft Tissue Recession
**Lack of Gingiva
**Decreased Vestibular Depth
**Aberrant Frenum/muscle position
**Gingival Excess
**Abnormal Color
**Condition of the exposed root surface
* Traumatic occlusal forces
**Primary Occlusal Trauma
**Secondary Occlusal Trauma
* Tooth and prosthesis
In medicine, a prosthesis (plural: prostheses; from grc, πρόσθεσις, prósthesis, addition, application, attachment), or a prosthetic implant, is an artificial device that replaces a missing body part, which may be lost through trau ...
related factors
** Localized tooth-related factors
** Localized dental prostheses-related factors
Peri-implant diseases and conditions
* Peri-implant health
* Peri-implant mucositis
* Peri-implantitis
* Peri-implant soft and hard tissue deficiencies
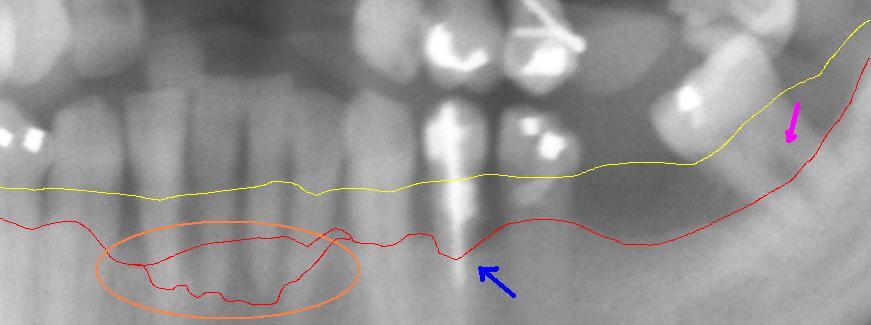
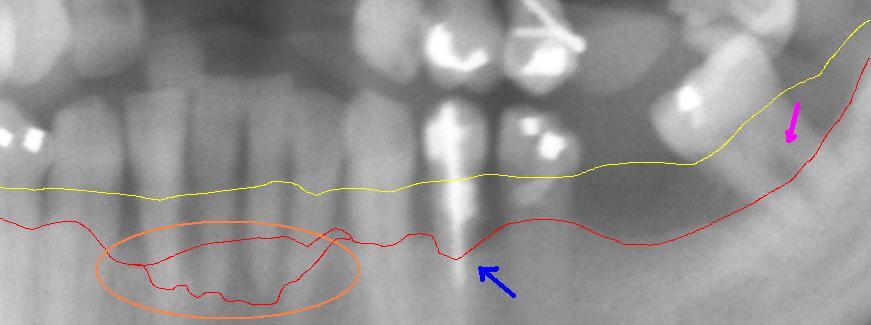
Staging
The goals of staging periodontitis is to classify the severity of damage and assess specific factors that may affect management. According to the 2017 classification, periodontitis is divided into four stages; after considering a few factors such as: * Amount and percentage bone loss radiographically * Clinical attachment loss, probing depth * Presence of furcation * Vertical bony defects * History of tooth loss related to periodontitis * Tooth hypermobility due to secondary occlusal traumaGrading
According to the 2017 classification, the grading system for periodontitis consists of three grades: *Grade A: Slow progression of disease; no evidence of bone loss over last five years *Grade B: Moderate progression; < 2mm of bone loss over last five years *Grade C: Rapid progression or future progression at high risk; ≥ 2mm bone loss over five years Risk factors affecting which grade a person is classified into include: *Smoking * DiabetesPrevention
Dailyoral hygiene
Oral hygiene is the practice of keeping one's mouth clean and free of disease and other problems (e.g. bad breath) by regular brushing of the teeth (dental hygiene) and cleaning between the teeth. It is important that oral hygiene be carried out ...
measures to prevent periodontal disease include:
* Brushing properly on a regular basis (at least twice daily), with the person attempting to direct the toothbrush bristles underneath the gumline, helps disrupt the bacterial-mycotic growth and formation of subgingival plaque.
*Flossing
Dental floss is a cord of thin filaments used in interdental cleaning to remove food and dental plaque from between teeth or places a toothbrush has difficulty reaching or is unable to reach. Its regular use as part of oral cleaning is designed ...
daily and using interdental brushes (if the space between teeth is large enough), as well as cleaning behind the last tooth, the third molar, in each quarter
*Using an antiseptic mouthwash
Mouthwash, mouth rinse, oral rinse, or mouth bath is a liquid which is held in the mouth passively or swilled around the mouth by contraction of the perioral muscles and/or movement of the head, and may be gargled, where the head is tilted back ...
: Chlorhexidine gluconate-based mouthwash in combination with careful oral hygiene may cure gingivitis, although they cannot reverse any attachment loss due to periodontitis.
*Regular dental check-ups and professional teeth cleaning as required: Dental check-ups serve to monitor the person's oral hygiene methods and levels of attachment around teeth, identify any early signs of periodontitis, and monitor response to treatment.
Typically, dental hygienists (or dentists) use special instruments to clean (debride) teeth below the gumline and disrupt any plaque growing below the gumline. This is a standard treatment to prevent any further progress of established periodontitis. Studies show that after such a professional cleaning (periodontal debridement), microbial plaque tends to grow back to precleaning levels after about three to four months. Nonetheless, the continued stabilization of a person's periodontal state depends largely, if not primarily, on the person's oral hygiene at home, as well as on the go. Without daily oral hygiene
Oral hygiene is the practice of keeping one's mouth clean and free of disease and other problems (e.g. bad breath) by regular brushing of the teeth (dental hygiene) and cleaning between the teeth. It is important that oral hygiene be carried out ...
, periodontal disease will not be overcome, especially if the person has a history of extensive periodontal disease.
Management
 The cornerstone of successful periodontal treatment starts with establishing excellent
The cornerstone of successful periodontal treatment starts with establishing excellent oral hygiene
Oral hygiene is the practice of keeping one's mouth clean and free of disease and other problems (e.g. bad breath) by regular brushing of the teeth (dental hygiene) and cleaning between the teeth. It is important that oral hygiene be carried out ...
. This includes twice-daily brushing with daily flossing
Dental floss is a cord of thin filaments used in interdental cleaning to remove food and dental plaque from between teeth or places a toothbrush has difficulty reaching or is unable to reach. Its regular use as part of oral cleaning is designed ...
. Also, the use of an interdental brush is helpful if space between the teeth allows. For smaller spaces, products such as narrow picks with soft rubber bristles provide excellent manual cleaning. Persons with dexterity problems, such as with arthritis
Arthritis is a term often used to mean any disorder that affects joints. Symptoms generally include joint pain and stiffness. Other symptoms may include redness, warmth, swelling, and decreased range of motion of the affected joints. In some ...
, may find oral hygiene to be difficult and may require more frequent professional care and/or the use of a powered toothbrush. Persons with periodontitis must realize it is a chronic inflammatory disease and a lifelong regimen of excellent hygiene and professional maintenance care with a dentist/hygienist or periodontist is required to maintain affected teeth.
Initial therapy
Removal of microbial plaque and calculus is necessary to establish periodontal health. The first step in the treatment of periodontitis involves nonsurgical cleaning below the gum line with a procedure called "root surface instrumentation" or "RSI", this causes a mechanical disturbance to the bacterial biofilm below the gumline. This procedure involves the use of specialized curettes to mechanically remove plaque and calculus from below the gumline, and may require multiple visits andlocal anesthesia
Local anesthesia is any technique to induce the absence of sensation in a specific part of the body, generally for the aim of inducing local analgesia, that is, local insensitivity to pain, although other local senses may be affected as well. I ...
to adequately complete. In addition to initial RSI, it may also be necessary to adjust the occlusion (bite) to prevent excessive force on teeth that have reduced bone support. Also, it may be necessary to complete any other dental needs, such as replacement of rough, plaque-retentive restorations, closure of open contacts between teeth, and any other requirements diagnosed at the initial evaluation. It is important to note that RSI is different to scaling and root planing: RSI only removes the calculus
Calculus, originally called infinitesimal calculus or "the calculus of infinitesimals", is the mathematics, mathematical study of continuous change, in the same way that geometry is the study of shape, and algebra is the study of generalizati ...
, while scaling and root planing removes the calculus as well as underlying softened dentin
Dentin () (American English) or dentine ( or ) (British English) ( la, substantia eburnea) is a calcified tissue of the body and, along with enamel, cementum, and pulp, is one of the four major components of teeth. It is usually covered by e ...
e, which leaves behind a smooth and glassy surface, which is not a requisite for periodontal healing. Therefore, RSI is now advocated over root planing.
Reevaluation
Nonsurgical scaling and root planing are usually successful if the periodontal pockets are shallower than . The dentist or hygienist must perform a re-evaluation four to six weeks after the initial scaling and root planing, to determine if the person's oral hygiene has improved and inflammation has regressed. Probing should be avoided then, and an analysis by gingival index should determine the presence or absence of inflammation. The monthly reevaluation of periodontal therapy should involve periodontal charting as a better indication of the success of treatment, and to see if other courses of treatment can be identified. Pocket depths of greater than which remain after initial therapy, with bleeding upon probing, indicate continued active disease and will very likely lead to further bone loss over time. This is especially true in molar tooth sites where furcations (areas between the roots) have been exposed.Surgery
If nonsurgical therapy is found to have been unsuccessful in managing signs of disease activity, periodontal surgery may be needed to stop progressive bone loss and regenerate lost bone where possible. Many surgical approaches are used in the treatment of advanced periodontitis, including open flap debridement and osseous surgery, as well as guided tissue regeneration and bone grafting. The goal of periodontal surgery is access for definitive calculus removal and surgical management of bony irregularities which have resulted from the disease process to reduce pockets as much as possible. Long-term studies have shown, in moderate to advanced periodontitis, surgically treated cases often have less further breakdown over time and, when coupled with a regular post-treatment maintenance regimen, are successful in nearly halting tooth loss in nearly 85% of diagnosed people.Local drug delivery
Local drug deliveries in periodontology has gained acceptance and popularity compared to systemic drugs due to decreased risk in development of resistant flora and other side effects. A meta analysis of local tetracycline found improvement. Local application ofstatin
Statins, also known as HMG-CoA reductase inhibitors, are a class of lipid-lowering medications that reduce illness and mortality in those who are at high risk of cardiovascular disease. They are the most common cholesterol-lowering drugs.
L ...
may be useful.
Systemic drug delivery
Systemic drug delivery in conjunction with non-surgical therapy may be used as a means to reduce the percentage of the bacterial plaque load in the mouth. Many different antibiotics and also combinations of them have been tested; however, there is yet very low-certainty evidence of any significant difference in the short and long term compared to non-surgical therapy alone. It may be beneficial to limit the use of systemic drugs, since bacteria can develop antimicrobial resistance and some specific antibiotics might induce temporary mild adverse effects, such as nausea, diarrhoea and gastrointestinal disturbances.Adjunctive systemic antimicrobial treatment
There is currently low-quality evidence suggesting if adjunctive systemic antimicrobials are beneficial for the non-surgical treatment of periodontitis. It is not sure whether some antibiotics are better than others when used alongside scaling and root planing).Maintenance
Once successful periodontal treatment has been completed, with or without surgery, an ongoing regimen of "periodontal maintenance" is required. This involves regular checkups and detailed cleanings every three months to prevent repopulation of periodontitis-causing microorganisms, and to closely monitor affected teeth so early treatment can be rendered if the disease recurs. Usually, periodontal disease exists due to poor plaque control resulting from inappropriate brushing. Therefore, if the brushing techniques are not modified, a periodontal recurrence is probable.Other
Most alternative "at-home" gum disease treatments involve injecting antimicrobial solutions, such ashydrogen peroxide
Hydrogen peroxide is a chemical compound with the formula . In its pure form, it is a very pale blue liquid that is slightly more viscous than water. It is used as an oxidizer, bleaching agent, and antiseptic, usually as a dilute solution (3% ...
, into periodontal pockets via slender applicators or oral irrigators. This process disrupts anaerobic micro-organism colonies and is effective at reducing infections and inflammation when used daily. A number of other products, functionally equivalent to hydrogen peroxide, are commercially available, but at substantially higher cost. However, such treatments do not address calculus formations, and so are short-lived, as anaerobic microbial colonies quickly regenerate in and around calculus.
Doxycycline may be given alongside the primary therapy of scaling (see § initial therapy). Doxycycline has been shown to improve indicators of disease progression (namely probing depth and attachment level). Its mechanism of action involves inhibition of matrix metalloproteinases (such as collagenase), which degrade the teeth's supporting tissues ( periodontium) under inflammatory conditions. To avoid killing beneficial oral microbes, only small doses of doxycycline (20 mg) are used.
Phage therapy
Phage therapy, viral phage therapy, or phagotherapy is the therapeutic use of bacteriophages for the treatment of pathogenic bacterial infections. This therapeutic approach emerged at the beginning of the 20th century but was progressively rep ...
may be a new therapeutic alternative.
Prognosis
Dentists and dental hygienists measure periodontal disease using a device called a periodontal probe. This thin "measuring stick" is gently placed into the space between the gums and the teeth, and slipped below the gumline. If the probe can slip more than below the gumline, the person is said to have a gingival pocket if no migration of the epithelial attachment has occurred or a periodontal pocket if apical migration has occurred. This is somewhat of a misnomer, as any depth is, in essence, a pocket, which in turn is defined by its depth, i.e., a 2-mm pocket or a 6-mm pocket. However, pockets are generally accepted as self-cleansable (at home, by the person, with a toothbrush) if they are 3 mm or less in depth. This is important because if a pocket is deeper than 3 mm around the tooth, at-home care will not be sufficient to cleanse the pocket, and professional care should be sought. When the pocket depths reach in depth, the hand instruments and ultrasonic scalers used by the dental professionals may not reach deeply enough into the pocket to clean out the microbial plaque that causes gingival inflammation. In such a situation, the bone or the gums around that tooth should be surgically altered or it will always have inflammation which will likely result in more bone loss around that tooth. An additional way to stop the inflammation would be for the person to receive subgingival antibiotics (such as minocycline) or undergo some form of gingival surgery to access the depths of the pockets and perhaps even change the pocket depths so they become 3 mm or less in depth and can once again be properly cleaned by the person at home with his or her toothbrush. If people have 7-mm or deeper pockets around their teeth, then they would likely risk eventual tooth loss over the years. If this periodontal condition is not identified and people remain unaware of the progressive nature of the disease, then years later, they may be surprised that some teeth will gradually become loose and may need to be extracted, sometimes due to a severe infection or even pain. According to the Sri Lankan tea laborer study, in the absence of any oral hygiene activity, approximately 10% will experience severe periodontal disease with rapid loss of attachment (>2 mm/year). About 80% will experience moderate loss (1–2 mm/year) and the remaining 10% will not experience any loss.Epidemiology
prevalence
In epidemiology, prevalence is the proportion of a particular population found to be affected by a medical condition (typically a disease or a risk factor such as smoking or seatbelt use) at a specific time. It is derived by comparing the number o ...
of 30–50% of the population, but only about 10% have severe forms.
Chronic periodontitis affects about 750 million people or about 10.8% of the world population as of 2010.
Like other conditions intimately related to access to hygiene and basic medical monitoring and care, periodontitis tends to be more common in economically disadvantaged populations or regions. Its occurrence decreases with a higher standard of living. In Israeli population, individuals of Yemenite, North-African, South Asian, or Mediterranean origin have higher prevalence of periodontal disease than individuals from European descent. Periodontitis is frequently reported to be socially patterned, i.e. people from the lower end of the socioeconomic scale are affected more often than people from the upper end of the socioeconomic scale.
History
An ancient hominid from 3 million years ago had gum disease. Records from China and the Middle East, along with archaeological studies, show that mankind has had periodontal disease for at least many thousands of years. In Europe and the Middle East archaeological research looking at ancient plaque DNA, shows that in the ancient hunter-gatherer lifestyle there was less gum disease, but that it became more common when more cereals were eaten. The Otzi Iceman was shown to have had severe gum disease. Furthermore, research has shown that in the Roman era in the UK, there was less periodontal disease than in modern times. The researchers suggest that smoking may be a key to this.Society and culture
Etymology
The word "periodontitis" (Greek
Greek may refer to:
Greece
Anything of, from, or related to Greece, a country in Southern Europe:
*Greeks, an ethnic group.
*Greek language, a branch of the Indo-European language family.
**Proto-Greek language, the assumed last common ancestor ...
: ) comes from the Greek ''peri'', "around", ( GEN ), "tooth", and the suffix , in medical terminology "inflammation
Inflammation (from la, wikt:en:inflammatio#Latin, inflammatio) is part of the complex biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or Irritation, irritants, and is a protective response involving im ...
". The word ''pyorrhea'' (alternative spelling: ''pyorrhoea'') comes from the Greek (), "discharge of matter", itself from , "discharge from a sore", ''rhoē'', "flow", and the suffix -''ia''. In English this term can describe, as in Greek, any discharge of pus
Pus is an exudate, typically white-yellow, yellow, or yellow-brown, formed at the site of inflammation during bacterial or fungal infection. An accumulation of pus in an enclosed tissue space is known as an abscess, whereas a visible collection ...
; i.e. it is not restricted to these diseases of the teeth.
Economics
It is estimated that lostproductivity
Productivity is the efficiency of production of goods or services expressed by some measure. Measurements of productivity are often expressed as a ratio of an aggregate output to a single input or an aggregate input used in a production proce ...
due to severe periodontitis costs the global economy about US$54 billion each year.
Other animals
Periodontal disease is the most common disease found in dogs and affects more than 80% of dogs aged three years or older. Its prevalence in dogs increases with age, but decreases with increasing body weight; i.e., toy and miniature breeds are more severely affected. Recent research undertaken at the Waltham Centre for Pet Nutrition has established that the bacteria associated with gum disease in dogs are not the same as in humans. Systemic disease may develop because the gums are very vascular (have a good blood supply). The blood stream carries these anaerobic micro-organisms, and they are filtered out by thekidney
The kidneys are two reddish-brown bean-shaped organs found in vertebrates. They are located on the left and right in the retroperitoneal space, and in adult humans are about in length. They receive blood from the paired renal arteries; bloo ...
s and liver
The liver is a major organ only found in vertebrates which performs many essential biological functions such as detoxification of the organism, and the synthesis of proteins and biochemicals necessary for digestion and growth. In humans, it ...
, where they may colonize and create microabscesses. The microorganisms traveling through the blood may also attach to the heart
The heart is a muscular organ found in most animals. This organ pumps blood through the blood vessels of the circulatory system. The pumped blood carries oxygen and nutrients to the body, while carrying metabolic waste such as carbon diox ...
valves, causing vegetative infective endocarditis
Infective endocarditis is an infection of the inner surface of the heart, usually the valves. Signs and symptoms may include fever, small areas of bleeding into the skin, heart murmur, feeling tired, and low red blood cell count. Complication ...
(infected heart valves). Additional diseases that may result from periodontitis include chronic bronchitis
Bronchitis is inflammation of the bronchi (large and medium-sized airways) in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi ...
and pulmonary fibrosis
Fibrosis, also known as fibrotic scarring, is a pathological wound healing in which connective tissue replaces normal parenchymal tissue to the extent that it goes unchecked, leading to considerable tissue remodelling and the formation of permane ...
.
Footnotes
External links
Canadian Academy of Periodontology — What is periodontitis?
Periodontal disease and braces
Orthodontics Australia. {{Authority control Inflammations Periodontal disorders Wikipedia medicine articles ready to translate